Abstract
Background
Most users of unsupported Internet interventions visit that site only once, therefore there is a need to create interventions that can be offered as a single brief interaction with the user.
Objective
The main goal of this study was to compare the effect of a one-session unsupported Internet intervention on participants' clinical symptoms (depressive and anxiety symptoms) and related variables (mood, confidence and motivation).
Method
A total of 765 adults residing in the United States took part in a randomized controlled trial. Participants were randomly assigned to one of five brief plain text interventions lasting 5–10 min. The interventions designed to address depressive symptoms were: thoughts (increasing helpful thoughts), activities (increasing activity level), sleep hygiene, assertiveness (increasing assertiveness awareness), Own Methods (utilizing methods that were previously successful). They were followed-up one week after consenting.
Results
A main effect of time was observed for both depression (F(1, 563) = 234.70, p < 0.001) and anxiety (F(1, 551) = 170.27, p < 0.001). In all cases, regardless of assigned condition and Major Depressive Episode status, mean scores on both positive outcomes (mood, confidence and motivation) and negative outcome scores (depression and anxiety) improved over time.
Conclusions
Brief unsupported Internet interventions can improve depressive symptoms at one-week follow-up. Further outcome data and research implications will be discussed.
Keywords: Depression, Anxiety, Mood, Confidence, Motivation, Internet intervention
Highlights
-
•
Most users of Internet interventions visit that site only once.
-
•
There is a need to create interventions that can be offered as a single brief interaction with the user.
-
•
This study explores the effect of a one-session intervention on participants’ clinical symptoms and related variables.
-
•
Mean scores on depression, anxiety, mood, confidence and motivation improved over time.
-
•
Brief Internet intervention can improve depressive symptoms at one-week follow-up.
1. Introduction
Major depression is estimated to become the second largest contributor to the global burden of disease in 2020 (Murray and Lopez, 1997); with an estimated 350 million people suffering from clinical depression worldwide (World Health Organization, 2015). The economic effects of depression are estimated at $77.4 billions lost annually in the United States. Both treatment and prevention of major depressive episodes can reduce the burden of depression (Muñoz et al., 2012). However, most people with major depression do not receive adequate treatment (Kessler et al., 2003), and of those who do receive treatment one-third do not improve (Warden et al., 2007). Thus, novel models for delivering mental health services and reducing the burden of mental disorders are needed (Kazdin and Rabbitt, 2013).
Unsupported Internet interventions represent a novel model of intervention delivery that is gaining in popularity, and there is now a growing body of evidence supporting the efficacy of Internet intervention for preventing and treating major depression. Andersson and Cuijpers (2009) conducted a meta-analysis in which they concluded that Internet treatments meet the criteria for evidence-based treatments for depression. Other studies have shown that Internet programs are effective in preventing depressive episodes in adults (Holländare et al., 2011, Buntrock et al., 2016) and in adolescents (Calear and Christensen, 2010, Calear et al., 2009, Van Voorhees et al., 2009). Additionally, unsupported Internet interventions increase accessibility, patient autonomy, and are “non-consumable” (i.e., they could be scaled up at marginal costs without losing therapeutic power) (Leykin et al., 2014, Muñoz, 2010).
However, there are several limitations to unsupported Internet interventions for depression. Perhaps the most salient ones are the high rates of attrition (Eysenbach, 2005, Muñoz et al., 2015), lower adherence, and effect sizes that tend to be small to moderate (Andersson and Cuijpers, 2009). There is some emerging evidence that in some circumstances, Internet interventions for depression can produce negative effects (Schueller et al., 2013), but this topic has been has been scarcely explored in the literature (Rozental et al., 2014). Certainly, several of these limitations are not particular to unsupported Internet interventions. Whereas several groups have found that most visitors to online interventions visit the sites only one time (Clarke et al., 2002, Leykin et al., 2014), this is in fact similar to traditional psychotherapy with live providers, in which the mean of visits to mental health services tend to be between three and five visits (Hansen et al., 2002) and the modal number of visits to mental health clinics is one (Weir et al., 2008). The critique of especially poor adherence to unsupported intervention may therefore be unwarranted, and the assumed expectation of high adherence to any psychosocial treatment, including Internet interventions, may be unjustifiably optimistic. While this limitation is clear for unsupported Internet interventions, guided Internet interventions tend to yield higher adherence rates (e.g., Andersson and Hedman, 2013, Hedman et al., 2013). That most users of unsupported Internet interventions visit a site only once speaks to the need of creating interventions that can be offered as a single brief interaction with the user. Indeed, such interaction represents a unique opportunity to take advantage of the user's current interest and availability and to offer information that could potentially improve current poor mood or prevent a future poor mood. Further, if brief unsupported Internet interventions lead the user to experience positive outcomes, the user may be tempted to return to the site or to pursue additional brief (or perhaps even longer) interventions, or to recommend this intervention to other users, which will increase the societal benefit of these interventions. Brief unsupported Internet interventions that are based on specific therapeutic tools or techniques may serve as a type of a naturalistic dismantling study, allowing us to better understand the relative utility of individual components or approaches in therapy, at least insofar as they are delivered online. Further, data gathered from such brief unsupported Internet interventions could be highly useful in the development of more extensive Internet intervention packages. After testing brief interventions, researchers could optimize and improve the best performing ones, discard those with limited utility, and combine interventions into more comprehensive packages for users who wish to take advantage of further opportunities to improve their mood.
Previous studies of brief treatments were first done in the traditional face-to-face format; and in recent years a few studies have also tested the utility of brief interventions through Internet. Although there were promising outcomes, given the limited number of studies, and the wide variety of populations and intervention types, drawing firm conclusions from these studies is difficult. For instance, Ayers et al. (2015) have shown that a brief, simple online intervention can improve the mood of postnatal women by changing their negative self-beliefs; the vast majority of participants reported liking the intervention. Ahmedani et al. (2015) found in a pilot study that a brief twenty minutes intervention based on CBT and Motivational Interviewing increased treatment seeking and reduced depression scores of participants with depression and chronic pain. Christensen et al. (2006) conducted an online randomized control trial comparing different versions of a Internet CBT intervention for depression. Results indicated that a single module of intervention was not effective in reducing depression, but those who completed three modules did attain reductions of their depression scores; interestingly, longer programs were associated with higher dropout rates (Christensen et al., 2006). Finally, other studies conducted with perinatal women have demonstrated the efficacy of brief Internet interventions for substance use (Ondersma et al., 2012, 2005, 2011, 2007, 2014). Most of these studies could be included under a Low Intensity (LI) CBT paradigm which can be defined as brief interventions that seek to increase the access to efficient and effective evidenced-based treatment to individuals with mild psychological disorders who would not otherwise have access due to a lack of resources and/or time (Bennett-Levy et al., 2010). The hallmark of LI CBT is that it does not require a highly trained mental health professional (e.g., clinical psychologist) to provide treatment, making the dissemination of this form of psychotherapy more readily available (Bennett-Levy et al., 2010). Although there are several potential benefits of brief unsupported interventions, their efficacy is not yet clear. Additionally, previous studies did not examine which components of an intervention were crucial to outcomes, highlighting the need to develop short-term intervention studies specifically to understand the differential effectiveness of psychotherapeutic components (Christensen et al., 2006).
Thus, the main goal of this study was to compare the one-week impact of brief unsupported Internet interventions delivered via a randomized clinical trial on participants' clinical symptoms (depressive and anxiety symptoms) and non-clinical variables (mood, confidence and motivation). Additionally, we examined participant-rated level of usefulness of the conditions. Participants were randomly assigned to one of five very brief unsupported interventions (lasting 5–10 min). The interventions were: increasing activity level, increasing helpful thoughts, increasing sleep hygiene, increasing assertiveness, or using their own mood managing method.
2. Method
2.1. Participants
Participants were recruited via Amazon's Mechanical Turk (Buhrmester et al., 2011). The sample consisted of 765 adults residing in the United States, aged 20 to 55 years old (Mage = 35.9, SDAge = 8.7); 69.2% were female. Participants were asked to complete a follow-up survey one week after completing the intervention to which they were randomized; 464 individuals (60.65% of the original sample) completed the follow-up survey. The only eligibility criteria for the study were that participants be at least 18 years of age, live in the U.S., and provide informed consent. The Institutional Review Board (IRB) at Palo Alto University approved this study. The trial was registered at clinicaltrials.gov, ref. number: NCT02748954.
2.2. Measures
2.2.1. Demographic questionnaire
Participants indicated their gender, age, country of residence, and postal code.
2.2.2. Depression
Depression was assessed via the Patient Health Questionnaire (PHQ-9; Kroenke & Spitzer, 2002), which is a widely used 10-item measure that screens for presence of a major depressive episode as well as assesses the severity of depressive symptomatology over a 2-week period. The measure is known to have good psychometric properties (Kroenke et al., 2002, Martin et al., 2006). The presence of a major depressive episode was determined using the criteria defined in the PHQ-9 scoring instructions (based on DSM-IV criteria for MDE). Specifically, respondents must endorse either item 1 (anhedonia) or item 2 (depressed mood) with a rating of 2 (more than half the days) or higher and endorse at least 5 items with a rating of 2 or higher (with the exception of item 9 (suicidal ideation), which requires a 1 (several days) or higher in order to meet criteria for MDE).
2.2.3. Anxiety
Anxiety was measured with the 7-item Generalized Anxiety Disorder questionnaire (GAD-7; Spitzer, Kroenke, Williams, & Löwe, 2006), which is a commonly used self-report questionnaire for measuring the level of generalized anxiety symptoms over a two-week period. Just as the PHQ-9, the GAD-7 is known to have excellent psychometric properties, having been tested in a wide range of populations, settings, and manners of administration (Spitzer et al., 2006).
2.2.4. Ancillary questions
Participants were asked to answer four Likert-type questions. The first question asked, “How would you describe your mood in the last 2 weeks?” and had responses ranging from 0 = Extremely Negative to 9 = Extremely Positive. The subsequent two questions asked, (1) “How motivated are you to do something to improve your mood?” (2) “How confident are you that you are able to do something to improve your mood?” and had responses ranging from 0 = Not at all to 10 = Extremely. Finally, the last question asked, “Before you see the ideas we will be sharing with you, how likely do you think they will be useful?” and had responses ranging from 0 = Very Unlikely to 6 = Very Likely.
2.3. Procedure
Participants were recruited through Amazon's Mechanical Turk (MTurk) workforce recruitment platform. After being redirected to the online study from MTurk, participants were asked to indicate their age (to establish eligibility). Eligible participants received a link to the study, and were presented with an informed consent document; only those who signed this online form were allowed to continue with the study and asked to complete other basic demographic questions. Before starting the intervention, participants were asked the four ancillary questions, and the clinical symptoms were assessed using the Patient Health Questionnaire 9 (PHQ-9) and the Generalized Anxiety Disorder questionnaire (GAD-7). Participants were then randomized into 1 of the 5 different intervention conditions. The five conditions were:
-
(1)
Thoughts. Increasing helpful thoughts consisted of two psychoeducational segments (i.e., thoughts affect emotions, and how to manage harmful thoughts), and a list of “helpful thoughts” that participants could choose to use to increase their mood for the next week.
-
(2)
Activities. Increasing activity level included a brief description of how activities affect mood. Participants were then asked to choose the activities they could use to improve their mood from an available list of “helpful activities”; users were also able to generate their own helpful activities. Participants were also presented with examples of unhelpful activities such as staying in bed and being isolated.
-
(3)
Assertiveness. Increasing assertiveness, consisting of tips for communicating assertively, and an example of an assertive statement. Participants were asked to describe a recent conflict and apply the intervention's assertiveness techniques to address the conflict.
-
(4)
Sleep hygiene. Increasing sleep hygiene included a description on how sleep can affect mood. Participants were also asked to select from a list of helpful sleep hygiene suggestions to be practiced within the next week such as, “Don't take naps during the day” and “Use the bed/bedroom for sleep or sex only”.
-
(5)
Own Methods, wherein participants were asked to identify and use four of their own personal strategies that have helped them improve their mood in the past.
Conditions one to four included a psychoeducational segment, an activity, and a contract; they were presented in plain text, and were designed to be completed in five to ten minutes. At the end of each of the four active conditions (i.e., increasing helpful thoughts, increasing activity level, increasing assertiveness, and increasing sleep hygiene), participants were asked to fill out a contract for themselves as a commitment to exercising their assigned intervention with the following statement, “I [participant's name], commit to [assigned activity], to test whether this [assigned activity] can help me improve my mood”. The Own Methods condition did not include a contract.
Immediately post intervention, participants were again asked the following three ancillary questions: (1) How motivated are you to do something about your mood? (2) How confident are you that you are able to do something to improve your mood? (3) How useful was this? Responses were given on a Likert scale, from 0 = Not at all to 10 = Extremely. After completing the intervention, participants were informed that they would be receiving a follow-up email in one week.
One week after completing the intervention, participants were sent a follow-up survey asking if they had used mood improving techniques. Additionally, they were asked the four ancillary questions about their mood, motivation, confidence, and self rated usefulness. Finally, participants completed the PHQ-9, and the GAD-7. Because the follow-up was at one week, we altered the instructions to limit the PHQ-9 to one week, as follows: “Over the last week, how often have you been bothered by any of the following problems?”. Participants were compensated with $0.10 after completion of the intervention and $0.10 upon completion of the follow-up questions. Participants were also provided a link that allowed them to access all five of the intervention conditions. Additionally, participants were provided other resources, such as e-couch, the USA Crisis Call Center, and local help lines for other parts of the world through the Befrienders website.
2.4. Statistical analysis
The primary analysis examined differences in outcome measures among randomized conditions across time. MDE status was included in analyses of responses to the ancillary questions, to determine whether those meeting criteria for MDE responded differently to the interventions. The combination of between- and within-subjects factors resulted in a 5 (treatment condition) × 2 (baseline MDE status) × 2 or 3 (time) mixed ANOVA design. Data were analyzed as a linear mixed-effects model (SAS PROC MIXED Version 9.4; SAS Institute, 2013) that utilizes a full-information maximum likelihood approach to handle missingness in outcome responses. This approach to missing data handling has been shown to yield unbiased estimates under the assumption of missing at random (Enders, 2010, Rubin and Little, 2002), which are likely satisfied in the present data. Finally, a Compound Symmetric Heterogeneity residual covariance structure was specified to account for correlations between outcome measurements at different times, while allowing for variances to vary across measurement occasions.
3. Results
3.1. Descriptive statistics
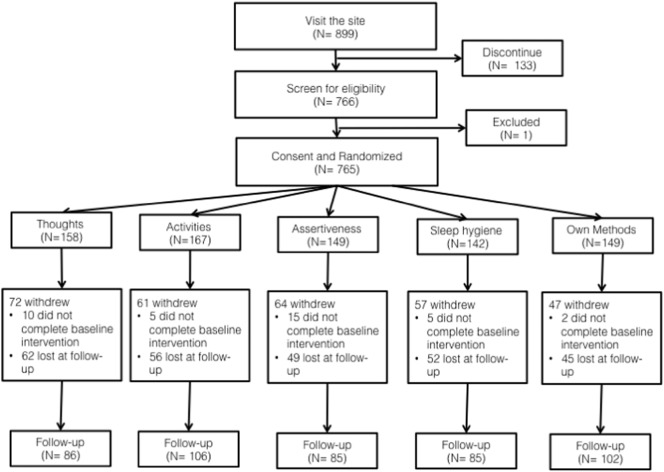
Recruitment took place from May 2015, up to June 2015, enrollment figures and follow-up samples are displayed in Fig. 1. Table 1 contains correlations for the measured outcome variables and demographic variables (age, gender). Participants who identified as female reported higher baseline anxiety (GAD-7; r(763) = 0.143, p < 0.01) and depression (PHQ-9; r(763) = 0.104, p < 0.01) scores, and younger participants tended to report lower anxiety (r(763) = − 0.147, p < 0.01) and depression (r(763) = − 0.129, p < 0.01). Motivation to improve mood was positively correlated with age (r(763) = 0.134, p < 0.01).
Fig. 1.
CONSORT diagram: progression of participants through a brief online study with a one week follow-up.
Table 1.
Pearson correlations among gender, age, and pre-intervention depression symptoms (PHQ-9 total score), anxiety symptoms (GAD-7 total score), positive mood (7-point likert scale), confidence in ability to improve mood (7-point likert scale), and motivation to improve mood (7-point likert scale). N = 765.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | M | SD |
|---|---|---|---|---|---|---|---|---|---|
| 1. Gender (female) | – | 0.041 | 0.104** | 0.143** | − 0.151** | − 0.001 | 0.019 | – | – |
| 2. Age | – | − 0.129** | − 0.147** | .033 | 0.047 | 0.134** | 35.9 | 12.5 | |
| 3. Depression | – | 0.766** | − 0.634** | − 0.408** | − 0.120** | 8.73 | 6.81 | ||
| 4. Anxiety | – | − 0.573** | − 0.343** | − 0.069 | 7.12 | 5.82 | |||
| 5. Mood | – | 0.489** | 0.196** | 5.15 | 1.94 | ||||
| 6. Confidence | – | 0.490** | 6.69 | 2.34 | |||||
| 7. Motivation | – | 7.04 | 2.10 |
Note. **p < 0.01. M = mean; SD = standard deviation.
Depression and anxiety symptoms were positively correlated with one another (r(763) = 0.766, p < 0.01), and negatively associated with self-reported positive mood (r(763) = − 0.634 and − 0.573, respectively, p < 0.01) and confidence in one's ability to improve one's own mood (r(763) = − 0.408 and − 0.343, respectively, p < 0.01). Major depression symptoms were also negatively correlated with motivation ratings (r(763) = − 0.120, p < 0.01).
Motivation was positively correlated with confidence (r(763) = 0.490, p < 0.01) and positive mood (r(763) = 0.196, p < 0.01), and confidence and positive mood ratings were also positively correlated (r(763) = 0.489, p < 0.01). Prior to completing the intervention, participants reported sub-clinical levels of anxiety symptoms, with a mean GAD-7 score of 7.11 (SD = 5.82). At follow-up, the mean GAD-7 score was 4.41 (SD = 4.96). Participants reported mild-to-moderate levels of depressive symptoms at baseline, with a mean PHQ-9 score of 8.73 (SD = 6.81). At baseline (N = 765), 23.9% (n = 183) of participants screened positive for a Major Depressive Episode. At follow-up (N = 464), the mean PHQ-9 score was 5.13 (SD = 5.56), and 10.3% (n = 48) of participants screened positive for Major Depressive Episode. There was no significant difference in follow-up completion rates between those who met criteria for MDE at baseline and those who did not meet criteria at baseline (χ2Diff(1) = 0.481, p = 0.489). In addition, no significant difference in follow-up completion rates between male and female participants (χ2Diff(1) = 0.001, p = 0.982). Participants who completed follow-up had a higher mean age, compared to those who did not complete follow-up (t(763) = − 2.526, p < 0.05, d = 0.180 [95%CI: − 4.140, − 0.519]). See Fig. 2. Examining those with data at both baseline and follow up (N = 464), 76.9% (n = 357) screened negative for MDE at baseline and of them, 96.4% (n = 344) still screened negative for MDE at one-week follow up; 23.1% (n = 107) screened positive for MDE at baseline, and of them 67.3% (n = 72) no longer screened positive for MDE at one-week follow up.
Fig. 2.
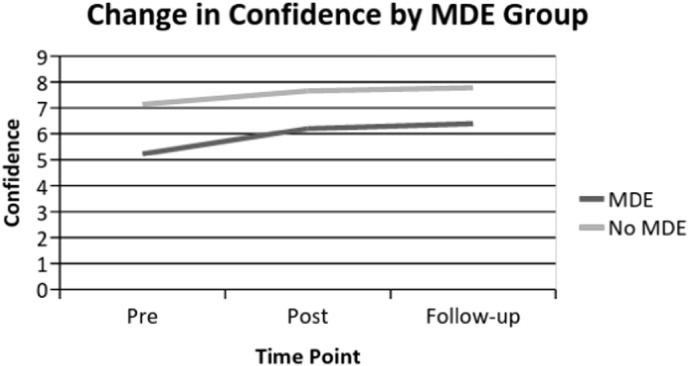
Two-way interaction between time and MDE status with confidence as the outcome.
3.2. Impact of randomized condition on outcome variables
3.2.1. Clinical outcomes
Differences between randomized conditions on reported depression (pre and follow-up) and anxiety (pre and follow-up) were assessed. The Own Methods condition was used as the control group for the other four conditions. No significant two-way interactions were observed for either outcome variable, indicating that none of the four intervention conditions differed in rates of improvement from the Own Methods condition for either depression or anxiety. A main effect of time was observed for both depression (MDiff = − 3.496, 95%CI: [− 3.944, − 3.047], F(1, 563) = 234.70, p < 0.001, d = − 0.56) and anxiety (MDiff = − 2.610, 95%CI: [− 3.003, − 2.172], F(1, 551) = 170.27, p < 0.001, d = − 0.49), suggesting that mean scores on depression and anxiety decreased from pre to follow-up across all conditions. A main effect of condition was observed for anxiety (F(4, 742) = 2.95, p < 0.05). This effect was driven by a marginally significant difference (p = 0.0718) between those in the activities condition and those in the Own Methods condition across all time points
Observed PHQ-9 scores showed that from baseline to follow-up 321 participants decreased their scores (range of decrease: 1–23 points), 66 participants maintained the same score, and 77 increased their scores (range of increase: 1–17 points). Regarding the GAD-7 score from baseline to follow-up 290 decreased their scores (range of decrease: 1–19 points), 87 participants maintained the same score, and 87 increased their scores (range of increase: 1–18 points).
3.2.2. Ancillary variables
The impact of randomized condition and MDE baseline status on reported motivation (across three time points: pre, post, and follow-up), confidence (pre, post, and follow-up), and positive mood (pre and follow-up) was assessed. A main effect of time was observed for all outcome variables, specifically: motivation (MDiff = 0.452, 95% CI:[0.258, 0.646], F(2, 1067) = 15.99, p < 0.001, d = 0.19), confidence (MDiff = 0.968, 95% CI:[0.765, 1.17], F(2, 1066) = 57.50, p < 0.001, d = 0.34), and positive mood (MDiff = 1.283, 95% CI:[1.114, 1.452], F(1, 534) = 221.84, p < 0.001, d = 0.55). In all cases, regardless of assigned condition and MDE status, mean scores on each outcome (motivation, confidence, and positive mood) improved from baseline to follow-up. A main effect of condition was noted for confidence (F(4, 741) = 3.99, p < 0.01). The effect was driven by a difference between the sleep hygiene condition (which produce the smallest change) and the assertiveness condition (which produced the highest change). Screening positive for an MDE at baseline predicted lower motivation (F(1, 747) = 14.30, p < 0.001), lower confidence (F(1743) = 93.17, p < 0.001), and lower overall mood (F(1, 693) = 170.06, p < 0.001) across all time points (see Table 2, Table 3). The two-way interaction between Time and MDE status was significant for confidence (F(2, 1066) = 7.10, p < 0.001; Fig. 2) and overall mood (F(1, 534) = 36.69, p < 0.001; Fig. 3). Those with MDE improved significantly more than those without MDE (simple comparisons presented in Table 2). However, this finding should be interpreted with caution as those with subclinical levels of depression at baseline (who reported better mood and higher confidence at baseline than those screening positive for a MDE) had less room to improve over time. The two-way interaction between Time and Condition was significant for confidence (F(8, 1062) = 2.19, p < 0.05; Fig. 4). Simple comparisons indicated at post-intervention, those in both the thoughts and activities conditions showed significantly greater confidence in their ability to improve their mood compared to those in the Own Methods condition (thoughts: MDiff = 0.694, 95%CI:[0.189, 1.200], d = 0.132; activities: MDiff = 0.610, 95%CI:[ 0.112, 1.109], d = 0.349). The three-way interaction between Time, MDE status and Condition was significant for motivation (F(8, 1063) = 2.05, p < 0.05). Specifically, at post-intervention (MDiff = − 1.350, 95%CI:[− 2.338, − 0.362], d = 0.18) and follow-up (MDiff = − 1.978, 95%CI:[ − 3.193, − 0.764], d = 0.27), those who screened positive for MDE in the thoughts condition showed significantly less improvement in motivation compared to those in the Own Methods condition (Fig. 5). From pre-intervention to follow-up, those in the activities and assertiveness who screened positive for MDE showed less improvement in motivation compared to the Own Methods condition, but the results did not reach significance (p = 0.065 and 0.069, respectively).
Table 2.
Mean motivation, confidence, and mood scores by MDE group across time.
| Motivation | Pre | Post | Follow-up |
|---|---|---|---|
| MDE | 6.55 | 7.00 | 7.02 |
| No MDE | 7.19 | 7.56 | 7.55 |
| d = − 0.307* | d = − 0.289* | d = − 0.274* | |
| Confidence | |||
| MDE | 5.23 | 6.20 | 6.40 |
| No MDE | 7.14 | 7.65 | 7.78 |
| d = − 0.874* | d = − 0.721* | d = − 0.676* | |
| Mood | |||
| MDE | 3.45 | 5.13 | |
| No MDE | 5.68 | 6.46 | |
| d = − 1.317* | d = − .0856* | ||
Note. *p < 0.05.
Table 3.
Time ∗ condition interaction for perceived usefulness of intervention.
| Pre intervention | Post intervention | Increase | |
|---|---|---|---|
| Activities | 6.02 | 7.49 | 1.47** |
| Thoughts | 5.87 | 7.07 | 1.20** |
| Assertiveness | 6.26 | 7.06 | 0.80** |
| Sleep hygiene | 5.86 | 6.26 | 0.40 |
| Own Methods | 6.13 | 6.16 | 0.03 |
Note. Significantly different from Own Methods in bold font. **p < 0.01.
Fig. 3.
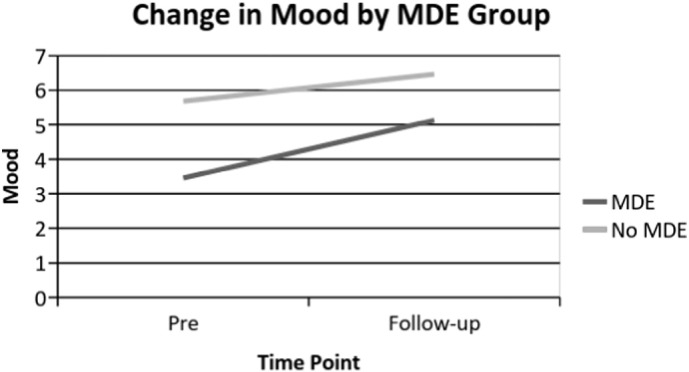
Two-way interaction between time and MDE status with mood as the outcome.
Fig. 4.
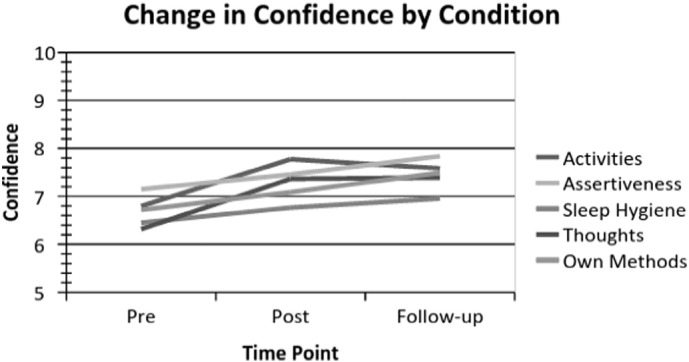
Two-way interaction between time and condition with confidence as the outcome.
Fig. 5.
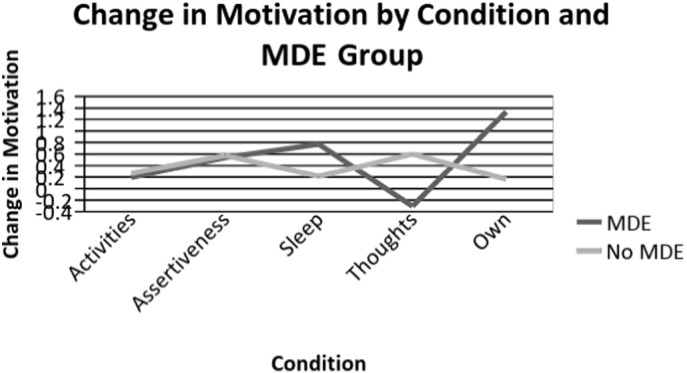
Three-way interaction between time, MDD status and condition with motivation as the outcome.
3.2.3. Perceived usefulness of micro interventions
The impact of randomized condition and MDE baseline status on perceived usefulness of the assigned intervention (pre and post) was assessed. A main effect of time was observed (MDiff = 0.812, 95%CI: [0.637, 0.988], F(1, 723) = 82.53, p < 0.001, d = 0.36), indicating that overall, participants' perception of usefulness of all interventions increased over time. A main effect of MDE was also observed (MDiff = − 0.766, 95%CI: [− 1.088, − 0.443], F(1, 746) = 21.68, p < 0.001, d = 0.40), such that after exposure to their assigned intervention, those meeting criteria for MDE reported all interventions as less useful compared to those without MDE post intervention. A significant time × condition interaction emerged (F(4, 723) = 7.74, p < 0.001). Results indicated that immediately following exposure to the intervention, those in the activities (MDiff = 1.189, 95%CI: [0.588, 1.790], d = 0.72), thoughts (MDiff = 0.684, 95%CI: [0.064, 1.303], d = 0.57), and assertiveness (MDiff = 0.920, 95%CI: [0.268, 1.572], d = 0.40) conditions rated the intervention as significantly more useful than those in the Own Methods condition (see Table 3).
4. Discussion
This study aimed to compare the impact of brief, unsupported Internet interventions on symptoms of depression and anxiety. Brief unsupported interventions represent a novel model for delivering online mental health services, especially given the high rates of attrition in full-scale unsupported Internet interventions (Eysenbach, 2005, Muñoz et al., 2015). Four brief, 5–10 min interventions (targeting activity level, thoughts, assertiveness, and sleep) were compared to a control condition (using Own Methods to manage mood) via a randomized controlled trial.
The key finding from this study is that although all non-supported interventions resulted in improvement of depression and anxiety scores over time, no intervention performed significantly better or worse than others over time, either for depression or anxiety. The degree of improvements in depression scores found in this study, as measured by effect sizes, were moderate and similar to that of previous studies with individuals with depression treated with extended unsupported Internet interventions (Andersson and Cuijpers, 2009). Other studies testing brief interventions have also yield positive effects with individuals with depression and chronic pain (Ahmedani et al., 2015), with perinatal women's mood (Ayers et al., 2015) and for smoking cessation (Ondersma et al., 2012, Ondersma et al., 2005, Ondersma et al., 2011, Ondersma et al., 2007, Ondersma et al., 2014). Interestingly, Christensen et al. (2006) reported that those who completed a single online module of a CBT intervention for depression did not show improvements, but those who completed three modules did show improvements in their depressive scores. A possible explanation for the difference between the Christensen et al. finding and ours has to do with the difference between the type of intervention. Christensen et al. module was an introduction to the core CBT concepts, which took 20 to 40 min to complete; only, a small proportion of participants completed the intervention and only 25% completed the post-test. However, in the present study, participants were taught a specific skill and were asked to sign a contract with themselves; additionally, a larger proportion of participants completed the intervention. Overall, the large reduction in prevalence of major depressive episodes (67.3% of those screening positive for MDE at baseline no longer met criteria at one-week follow-up) suggests further work is warranted examining whether brief interventions have significant impact on depression symptoms and perhaps even on the point prevalence of major depressive episodes. For example, a similar significant reduction in depression scores was reported in response to ten brief, four-minute video clips of cognitive-behavioral mood management methods shown one per day during a two-week period at the noon, 6 p.m., and 11 p.m. local television news program (Muñoz et al., 1982).
The lack of significant interaction between group and time for depression and anxiety scores was a surprising outcome. Unexpectedly, the control condition (Own Methods) appeared to be as effective as the presumed active intervention conditions. It is difficult to place this finding in context, because of the different control conditions used in previous studies on brief interventions. For example, Ayers et al. (2015) used an active comparison group exercise; Christensen et al. (2006) compared a single module to extended versions of a CBT online program; and, the Ahmedani et al. (2015) pilot study did not use a control condition. It is conceivable that being reminded about strategies that have previously been effective in improving mood and being prompted to use them was itself an effective intervention. Our finding that those who screened positive for MDE in the Own Methods condition showed the highest change in motivation supports this possibility. We have found a similar effect in a study where pregnant women were asked to have a stress-free day without explicit instructions on how to do so. Not only did they report lower levels of stress, but they also showed significant reduction in morning cortisol levels (Urizar et al., 2004, Urizar and Muñoz, 2011). Thus, drawing attention to improving mood or reducing stress may nudge people into using methods they know and achieving measurable effects.
Likewise, analysis of ancillary variables revealed that motivation, confidence, and positive mood improved over time regardless of the assigned condition and MDE status. The finding that the assertiveness condition resulted in greatest increase in confidence, and the sleep condition – in the lowest increase is an intriguing one. One possibility may be that assertiveness skills training targets internal confidence specifically, whereas sleep hygiene does not. This is further corroborated by the finding that thoughts and activities conditions showed a significant increase in confidence from pre to post intervention level compared to the Own Methods condition. As above, it is possible that teaching individuals these new, concrete skills may improve their confidence in their ability to improve their mood level. We also found that those who screen positive for MDE showed greater improvement in confidence, as well as mood, than those without MDE. Although this may suggest that brief interventions yield confidence improvement for participants with MDE, this finding should be interpreted with caution because those without MDE may have little room for improvement. However, those in the Thoughts condition who screened positive for MDE showed less improvement in motivation over time (from pre to post and from pre to follow-up) than those who did not screen positive for MDE. It may be the case that although the Thoughts condition led to a confidence gain, it may require a more intense intervention to improve motivation. It may be noteworthy, however, that those who screened positive for MDE in the Own Methods condition reported the higher change in motivation score, which might suggest that building on inner resources can be a source of motivation for individuals because they reminded themselves that they could improve their mood using methods they already knew.
Given that unsupported Internet interventions are user-driven, ensuring that users understand the utility of interventions is highly important. We found that participants perceived the interventions as more useful over time; however, participants meeting criteria for MDE reported all interventions as less useful compared to those without MDE. The activities condition was rated as the most useful intervention, followed by thoughts, assertiveness, sleep hygiene, and lastly Own Methods. This may suggest that the activities intervention could be the cornerstone of future brief Internet interventions for mood, and a target for iterative improvement. That the Own Methods condition was rated as least useful is not surprising, considering that individuals were prompted to use the strategies they are already using, without teaching them any new strategies. The sleep hygiene condition did not differ significantly from the Own Methods condition, suggesting that the effect of this condition was weak or that sleep problems may require a higher dose than the one provided in this brief intervention.
5. Limitations
This study had several limitations that should be acknowledged. First, participants were recruited through Amazon's Mechanical Turk (MTurk) and were compensated for participation. This may limit the generalizability of the results. However, evidence shows that MTurk participants may be more diverse than college samples, that realistic compensation does not affect data quality, and that data obtained could be as reliable as the one obtained in traditional methods (Buhrmester et al., 2011). Second, although the Own Methods condition was initially envisioned as a control condition, change in depression and anxiety scores in that condition were no different from those of other conditions. Though it is possible that the active conditions were not sufficiently powerful to separate from the control condition, another possible reason is that the prompt to think of and use previously effective strategies may itself be an active intervention. Future studies may benefit from using a wait list control condition to explore the specific impact of each condition versus time or changes attributable to regression to the mean effect. Third, there were some participants whose depressive score in the PHQ-9 and anxiety score from the GAD-7 worsened over time, indicating that brief interventions although potentially beneficial for most participants, may also yield negative outcomes in others. Further studies should include ways in which participants are able to report adverse events (Rozental et al., 2014).
6. Conclusions
Brief Internet interventions could benefit greater numbers of people. In the present study participants receiving a brief Internet intervention experienced a decrease in their depression and anxiety levels, and showed improvements in their motivation, confidence and positive mood. One of the most intriguing results from our study was the finding of no significant differences between all intervention conditions; whereas all interventions, including the Own Methods condition, result in depression improvements, no intervention stood out as being clearly superior or inferior. Though it is possible that, in the absence of a truly inert control condition, participants have improved merely from the passage of time, given that our effect sizes were comparable to those of other extended unsupported Internet interventions (Andersson and Cuijpers, 2009) lends partial credence to our conclusion that brief interventions could offer sufficiently positive results. Future research should specifically examine the utility of reminding individuals of the benefits of their past successful mood improvement methods. Additionally, because the activities condition was rated as most useful intervention, future studies could explore the impact of this condition vs. a non-active control to better determine the effect of brief online interventions.
The most important benefit of studying brief interventions is that, if brief interventions work, they can provide at least one skill for those that visited the site only once, or tempt the user to return to the site or to pursue additional interventions. Studies on brief interventions can also speed up the process of generating new scientific knowledge (compared to traditional studies - see Ioannidis, 1998). Developing brief interventions takes less time than designing a multifaceted treatment (which, in the case of unsupported Internet studies, most participants do not complete). Even if specific brief interventions tested fail to show significant differences, they yield this information in a short period of time, allowing us to introduce further small changes in the interventions and retest them in a short period of time, allowing researchers to “fail fast and fail better”.
Testing brief interventions through the Internet may allow recruitment of large samples with lower attrition rates than more extensive multifaceted Internet interventions. This method may facilitate creation of big data sets that could help identify more precisely who benefits from which intervention (Muñoz and Bunge, 2016). Instead of relying on population means to produce treatment recommendations, big data on several brief Internet interventions will allow us to construct personalized evidence based interventions through pattern matching. Identifying the individual interventions as well as the sequences of interventions which worked best for each individual or subgroup may lead to more customized (and precise) decisions and therapeutic practices.
References
- Ahmedani B.K., Crotty N., Abdulhak M.M., Ondersma S.J. Pilot feasibility study of a brief, tailored mobile health intervention for depression among patients with chronic pain. Behav. Med. 2015;41(1):25–32. doi: 10.1080/08964289.2013.867827. [DOI] [PubMed] [Google Scholar]
- Andersson G., Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cogn. Behav. Ther. 2009;38(4):196–205. doi: 10.1080/16506070903318960. [DOI] [PubMed] [Google Scholar]
- Andersson G., Hedman E. Effectiveness of guided internet-based cognitive behavior therapy in regular clinical settings. Verhaltenstherapie. 2013;23(3):140–148. [Google Scholar]
- Ayers S., Fitzgerald G., Thompson S. Brief online self-help exercises for postnatal women to improve mood: a pilot study. Matern. Child Health J. 2015;19(11):2375–2383. doi: 10.1007/s10995-015-1755-5. [DOI] [PubMed] [Google Scholar]
- Bennett-Levy J., Richards D.A., Farrand P., Christensen H., Griffiths K.M., Kavanagh D.J.…Proudfoot J. Low Intensity CBT Interventions. 2010. Low intensity CBT interventions: a revolution in mental health care; pp. 3–18. [Google Scholar]
- Buhrmester M., Kwang T., Gosling S.D. Amazon's mechanical Turk: a new source of inexpensive, yet high-quality, data? Perspect. Psychol. Sci. 2011;6(1):3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- Buntrock C., Ebert D., Lehr D., Smit F., Riper H., Berking M., Cuijpers P. Effect of a web-based guided self-help intervention for prevention of major depression in adults with subthreshold depression: a randomized clinical trial. JAMA. 2016;315(17):1854–1863. doi: 10.1001/jama.2016.4326. [DOI] [PubMed] [Google Scholar]
- Calear A.L., Christensen H. Review of internet-based prevention and treatment programs for anxiety and depression in children and adolescents. Med. J. Aust. 2010;192(11):S12. doi: 10.5694/j.1326-5377.2010.tb03686.x. [DOI] [PubMed] [Google Scholar]
- Calear A.L., Christensen H., Mackinnon A., Griffiths K.M., O'Kearney R. The YouthMood project: a cluster randomized controlled trial of an online cognitive behavioral program with adolescents. J. Consult. Clin. Psychol. 2009;77(6):1021–1032. doi: 10.1037/a0017391. [DOI] [PubMed] [Google Scholar]
- Christensen H., Griffiths K.M., Mackinnon A.J., Brittliffe K. Online randomized controlled trial of brief and full cognitive behaviour therapy for depression. Psychol. Med. 2006;36(12):1737–1746. doi: 10.1017/S0033291706008695. [DOI] [PubMed] [Google Scholar]
- Clarke G., Reid D.E., O'Connor E., DeBar L.L., Kelleher C., Lynch F., Nunley S. Overcoming depression on the internet (ODIN): a randomized controlled trial of an internet depression skills intervention program. J. Med. Internet Res. 2002;4(3) doi: 10.2196/jmir.4.3.e14. (Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1761939/) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders C.K. Guilford Press; New York London: 2010. Applied missing data analysis. [Google Scholar]
- Eysenbach G. The law of attrition. J. Med. Internet Res. 2005;7(1) doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen N.B., Lambert M.J., Forman E.M. The psychotherapy dose-response effect and its implications for treatment delivery services. Clin. Psychol. Sci. Pract. 2002;9(3):329–343. [Google Scholar]
- Hedman E., Ljótsson B., Rück C., Bergström J., Andersson G., Kaldo V., … Effectiveness of internet-based cognitive behaviour therapy for panic disorder in routine psychiatric care. Acta Psychiatr. Scand. 2013;128(6):457–467. doi: 10.1111/acps.12079. [DOI] [PubMed] [Google Scholar]
- Holländare F., Johnsson S., Randestad M., Tillfors M., Carlbring P., Andersson G., Engström I. Randomized trial of internet-based relapse prevention for partially remitted depression. Acta Psychiatr. Scand. 2011;124(4):285–294. doi: 10.1111/j.1600-0447.2011.01698.x. [DOI] [PubMed] [Google Scholar]
- Ioannidis J.P. Effect of the statistical significance of results on the time to completion and publication of randomized efficacy trials. JAMA. 1998;279(4):281–286. doi: 10.1001/jama.279.4.281. [DOI] [PubMed] [Google Scholar]
- Kazdin A.E., Rabbitt S.M. Novel models for delivering mental health services and reducing the burdens of mental illness. Clin. Psychol. Sci. Pract. 2013;2167702612463566 [Google Scholar]
- Kessler R.C., Berglund P., Demler O., Jin R., Koretz D., Merikangas K.R.…Wang P.S. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L. The PHQ-9: A new depression diagnostic and severity measure. Psychiatr. Ann. 2002;32:509–515. [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosom. Med. 2002;64:258–266. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- Leykin Y., Muñoz R.F., Contreras O., Latham M.D. Results from a trial of an unsupported internet intervention for depressive symptoms. Internet Interv. 2014;1(4):175–181. doi: 10.1016/j.invent.2014.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin A., Rief W., Klaiberg A., Braehler E. Validity of the brief patient health questionnaire mood scale (PHQ-9) in the general population. Gen. Hosp. Psychiatry, 2006;28:71–77. doi: 10.1016/j.genhosppsych.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Muñoz R.F. Using evidence-based internet interventions to reduce health disparities worldwide. J. Med. Internet Res. 2010;12(5) doi: 10.2196/jmir.1463. (Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3057307/) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz R.F., Bunge E.L. Prevention of depression worldwide: a wake-up call. Lancet Psychiatry. 2016 doi: 10.1016/S2215-0366(15)00555-6. [DOI] [PubMed] [Google Scholar]
- Muñoz R.F., Glish M., Soo-Hoo T., Robertson J. The San Francisco mood survey project: preliminary work toward the prevention of depression. Am. J. Community Psychol. 1982;10(3):317–329. doi: 10.1007/BF00896498. [DOI] [PubMed] [Google Scholar]
- Muñoz R.F., Beardslee W.R., Leykin Y. Major depression can be prevented. Am. Psychol. 2012;67(4):285–295. doi: 10.1037/a0027666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz R.F., Bunge E.L., Chen K., Schueller S.M., Bravin J.I., Shaughnessy E.A., Pérez-Stable E.J. Massive open online interventions a novel model for delivering behavioral-health services worldwide. Clin. Psychol. Sci. 2015;2167702615583840 [Google Scholar]
- Murray C.J., Lopez A.D. Alternative projections of mortality and disability by cause 1990–2020: global burden of disease study. Lancet. 1997;349(9064):1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- Ondersma S.J., Chase S.K., Svikis D.S., Schuster C.R. Computer-based brief motivational intervention for perinatal drug use. J. Subst. Abus. Treat. 2005;28(4):305–312. doi: 10.1016/j.jsat.2005.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ondersma S.J., Svikis D.S., Schuster C.R. Computer-based brief intervention: a randomized trial with postpartum women. Am. J. Prev. Med. 2007;32(3):231–238. doi: 10.1016/j.amepre.2006.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ondersma S.J., Grekin E.R., Svikis D. The potential for technology in brief interventions for substance use, and during-session prediction of computer-delivered brief intervention response. Subst. Use Misuse. 2011;46(1):77–86. doi: 10.3109/10826084.2011.521372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ondersma S.J., Svikis D.S., Lam P.K., Connors-Burge V.S., Ledgerwood D.M., Hopper J.A. A randomized trial of computer-delivered brief intervention and low-intensity contingency management for smoking during pregnancy. Nicotine Tob. Res. 2012;14(3):351–360. doi: 10.1093/ntr/ntr221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ondersma S.J., Svikis D.S., Thacker L.R., Beatty J.R., Lockhart N. Computer-delivered screening and brief intervention (e-SBI) for postpartum drug use: a randomized trial. J. Subst. Abus. Treat. 2014;46(1):52–59. doi: 10.1016/j.jsat.2013.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozental A., Andersson G., Boettcher J., Ebert D.D., Cuijpers P., Knaevelsrud C.…Carlbring P. Consensus statement on defining and measuring negative effects of. Internet Interv. 2014;1(1):12–19. [Google Scholar]
- Rubin D.B., Little R.J.A. J Wiley & Sons; Hoboken, NJ: 2002. Statistical analysis with missing data. [Google Scholar]
- Schueller S.M., Pérez-Stable E.J., Muñoz R.F. A mood management intervention in an internet stop smoking randomized controlled trial does not prevent depression a cautionary tale. Clin. Psychol. Sci. 2013 doi: 10.1177/2167702613484717. (2167702613484717) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Urizar G.G., Muñoz R.F. Impact of a prenatal cognitive-behavioral stress management intervention on salivary cortisol levels in low-income mothers and their infants. Psychoneuroendocrinology. 2011;36(10):1480–1494. doi: 10.1016/j.psyneuen.2011.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urizar G.G., Milazzo M., Le H.-N., Delucchi K., Sotelo R., Muñoz R.F. Impact of stress reduction instructions on stress and cortisol levels during pregnancy. Biol. Psychol. 2004;67(3):275–282. doi: 10.1016/j.biopsycho.2003.11.001. [DOI] [PubMed] [Google Scholar]
- Van Voorhees B.W., Fogel J., Reinecke M.A., Gladstone T., Stuart S., Gollan J., … Randomized clinical trial of an internet-based depression prevention program for adolescents (project CATCH-IT) in primary care: 12-week outcomes. J. Dev. Behav. Pediatr. 2009;30(1):23–37. doi: 10.1097/DBP.0b013e3181966c2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warden D., Rush A.J., Trivedi M.H., Fava M., Wisniewski S.R. The STAR* D project results: a comprehensive review of findings. Curr. Psychiatry Rep. 2007;9(6):449–459. doi: 10.1007/s11920-007-0061-3. [DOI] [PubMed] [Google Scholar]
- Weir S., Wills M., Young J., Perlesz A. La Trobe University; 2008. The Implementation of Single Session Work in Community Health. [Google Scholar]
- World Health Organization Depression. 2015. http://www.who.int/mediacentre/factsheets/fs369/en/ Retrieved January 14, 2016, from.