Abstract
The present pilot study examined the efficacy and acceptability of an internet-delivered Cognitive Behaviour Therapy (iCBT) intervention delivered in both English and Arabic languages to Arab Australians, aged 18 and over, with symptoms of depression and anxiety. Thirteen participants with at least mild symptoms of depression on the (Patient Health Questionnaire 9-item; PHQ-9; total scores ≥ 5) or anxiety (Generalised Anxiety Disorder 7-item; GAD-7; total scores ≥ 5) accessed the online Arabic Wellbeing Course, which consisted of five online lessons delivered over eight weeks with weekly clinician support. Measures of depression, anxiety, distress and disability were administered at pre-treatment, post-treatment and 3-month follow-up. Data were analysed using generalised estimation equation (GEE) modelling. Seventy-seven percent (10/13) of participants completed the five lessons over eight weeks, with 10/13 providing post-treatment and 3-month follow-up data. Participants improved significantly across all outcome measures, with large within-group effect sizes based on estimated marginal means (Cohen's d) at post-treatment (d = 1.18 to 1.62) and 3-month follow-up (d = 1.28 to 1.72). In addition, 40% and 38% of participants obtained, at least, a 50% improvement in symptoms of both anxiety and depression at 3-month follow-up respectively. Participants rated the Arabic Wellbeing Course as acceptable, and 70% of those who completed follow-up questionnaires reported accessing the course in both English and Arabic languages. Notwithstanding the limitations of an open trial design, these results are encouraging and indicate that culturally modified clinician-guided internet-delivered versions of Western psychological interventions have the potential for increasing access to treatment for Arabic-speaking Australians, and potentially other groups.
Keywords: Arabic, Arab Australians, Anxiety, Depression, Internet-delivered treatment, Transdiagnostic
Highlights
-
•
This pilot study examined the efficacy of an internet-delivered Cognitive Behaviour Therapy (iCBT) for Arab Australians.
-
•
iCBT was found to be effective and acceptable among Arab Australian participants.
-
•
Seventy percent of participants who completed follow up data reported accessing the Course in both English and Arabic languages.
-
•
iCBT has the potential for increasing access to treatment for Arabic-speaking Australians, and other groups.
1. Introduction
In the last 15 years, the size of the Arabic-speaking communities in Australia, Arab Australians, have increased by approximately 50% (Australian Bureau of Statistics, 2006, Australian Bureau of Statistics, 2011) and Arabic is now the fourth most common language in Australia (Australian Bureau of Statistics, 2011). Relatively little is known about the mental health of this population; however two small surveys (Centre for Epidemiology and Research, 2010, Kayrouz et al., 2014) indicate that the prevalence of anxiety, depression and psychological distress may be higher in this group than in the general population (Slade et al., 2009).
Unfortunately, treatment seeking rates in Arab Australians appear to be lower than in the general Australian population (Kayrouz et al., 2014, Slade et al., 2009). Barriers to treatment seeking in this population include lack of culturally appropriate services and lack of services delivered in the Arabic language (Kayrouz et al., 2014, Youssef and Deane, 2006). The latter point is particularly important as data indicate that 40% of Arab Australians have difficulty speaking English (Australian Bureau of Statistics, 2011). In addition, 38.5% of Arab Australians were born in Australia (Australian Bureau of Statistics, 2011), and may have difficulty reading Arabic. Consequently, when developing culturally-appropriate mental health services for Arab Australians, it may be beneficial to provide services in both English and Arabic, allowing Arab Australians to choose their language preference. Most research to date with Arabs living in western countries do not provide this option, either presenting materials in English or Arabic only (Kayrouz et al., 2015, Kayrouz et al., 2016a, Stenmark et al., 2013, Taloyan et al., 2013, Wagner et al., 2008).
One strategy that may reduce barriers to accessing psychological treatment and provide flexibility of choice in the preferred language is to deliver psychological interventions, such as cognitive behavioural therapy (CBT), via the internet (Andersson and Titov, 2014). Two recent surveys of Arabs living in Australia and overseas found that > 50% of the samples reported they would be willing try internet-delivered CBT (iCBT) treatments to manage symptoms of anxiety and depression (Kayrouz et al., 2014, Kayrouz et al., n.d). These findings are consistent with observations that Arab people prefer treatment that is short-term, directive, and focused on the present (Abudabbeh and Hays, 2006, Al-Krenawi and Graham, 2000, Chaleby, 1992).
Two recent feasibility pilot trials (Kayrouz et al., 2015, Kayrouz et al., 2016a) explored the efficacy and acceptability of treating symptoms of anxiety and depression in Arab people using a culturally modified version of an existing evidence-based iCBT intervention, the Wellbeing Course (Dear et al., 2015, Kirkpatrick et al., 2013, Titov et al., 2013, Titov et al., 2014, Titov et al., 2012, Titov et al., 2015a, Titov et al., 2015b). Results from these two trials were promising, and indicated the Arabic Wellbeing Course reduced symptoms of anxiety, depression and disability in Arab people, and that > 90% of participants rated the intervention as acceptable (Kayrouz et al., 2015, Kayrouz et al., 2016a). However, a limitation of these trials is that the intervention was delivered only in the English language and therefore would not be accessible to non-English speaking Arab people.
The present study aims to further extend this line of research by examining the efficacy and acceptability of the Arabic Wellbeing Course when presented in both the English and Arabic languages. Because of the absence of previous research exploring the efficacy of a translated iCBT treatment for Arab Australians experiencing depression or anxiety, an open-trial design was considered ethically appropriate to inform the power requirements of a future large randomised controlled trial. A secondary aim was to explore which language participants reported using.
2. Method
2.1. Design and hypotheses
A single-group open trial design was utilised. A GEE analysis was conducted to calculate the average group improvement in symptoms over time (Hubbard et al., 2010). This study was approved by the Human Research Ethics Committee of Macquarie University, Sydney, Australia, and registered as a clinical trial with the Australian New Zealand Clinical Trials Registry, ACTRN12163001329752.
Based on the results of a therapist-guided trial of the Arabic Wellbeing Course presented in the English language (Kayrouz et al., 2015) it was hypothesised that (1) Arabs would show a statistically and clinically significant reduction in the symptoms of depression, anxiety, distress and disability; and (2) Arabs would rate the course as worthwhile and would recommend the course to a friend or family member.
2.2. Participants
Details about the study were promoted using Facebook (FB) recruitment strategies including promoting posts on the FB public page of the eCentreClinic research clinic (www.ecentreclinic.org) (for more details see Kayrouz et al., 2016b). Two phases of recruitment occurred from 16 June 2015 to 13 July 2015 (Phase 1) and 16 July to 10 August 2016 (Phase 2). Interested adults applied online via the eCentreClinic website, which provides information about anxiety and depression, and conducts clinical research concerning internet-delivered treatment.
Over the two recruitment phases, eight participants in Phase 1 and five participants in Phase 2 provided informed consent and volunteered to participate. Inclusion criteria were: (1) living in Australia; (2) overseas-born or Australian-born person who self-identified as being of Arabic ancestry; (3) between the ages of 18 and 70 years; (4) having reliable internet access; (5) not receiving CBT elsewhere; (6) no history of a psychotic condition; (7) a Patient Health Questionnaire 9-item (PHQ-9) score ≥ 5 or a Generalised Anxiety Disorder 7-item (GAD-7) score ≥ 5 indicating, at least, mild depressive or anxiety symptoms, but not currently experiencing severe depression (defined as a total score ≥ 23 or a score = 3 on question 9 of the PHQ-9) (Kroenke et al., 2001); and (8) if taking medication for anxiety or depression, having been on a stable dose for at least one month.
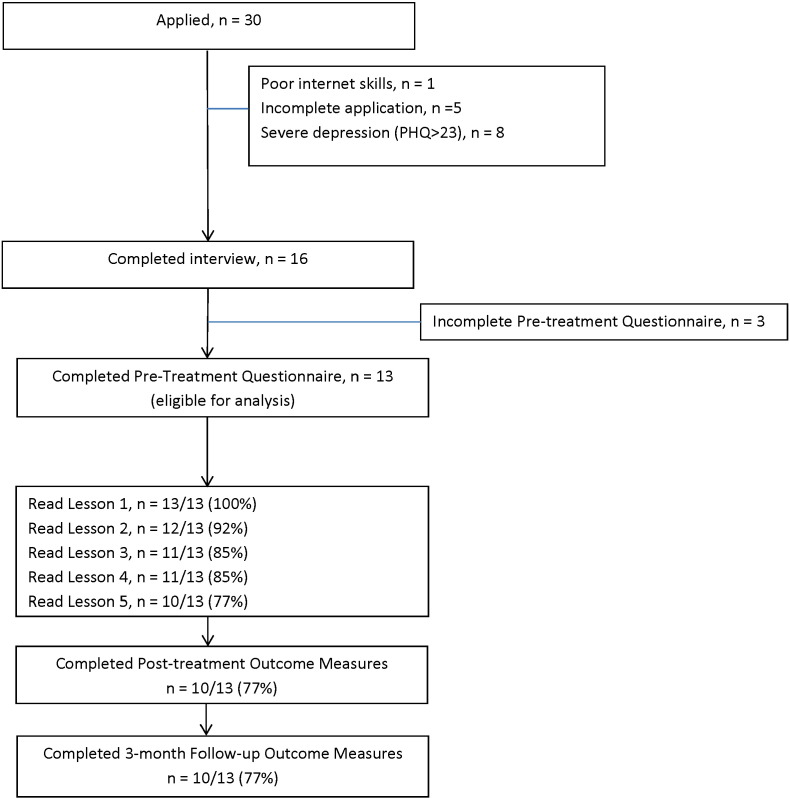
Of the 30 participants who applied to participate, 13 were eligible with 17 participants excluded at assessment (see Fig. 1). During assessment, 14/17 (82%) were excluded for the following reasons: (a) five for incomplete applications; (b) eight for experiencing very severe depression (i.e., defined as a total score ≥ 23 on the PHQ-9 or PHQ-9 Q9 > 2), and (c) one for poor internet skills and unreliable internet access. During treatment, 3/17 (18%) were excluded for not completing the pre-treatment (baseline) questionnaires. The final sample had a mean age of 37.13 years (SD = 12.48; range = 23–64) and 8/13 (62%) were males. The majority of participants were married (n = 7, 54%), with the remainder single (n = 5, 38%) or separated/divorced/other (n = 1, 8%). Fifty-four percent of the sample (n = 7) had attained at least a bachelor's degree, 31% (n = 4) attained a diploma, and 15% (n = 2) attained a trade certificate/apprentice or completed schooling, at least, up to Year 10 (approximately 15 years of age). Eight of the 13 participants (62%) reported they were in full-time or part-time employment, 3/13 (23%) unemployed, and 2/13 (15%) were full-time or part-time students. Five participants (38%) reported having had previous mental health treatment, two (15%) reported taking medication related to their symptoms, and participants reported a mean of 21.5 years of difficulties with mental health (SD = 9.2).
Fig. 1.
Participant flow.
A sample size of 15 was determined as sufficient (one-tailed test, power at 80%, and alpha at .05) to detect a within-group Cohen’s d effect size of .70; the minimum likely effect based on previous studies employing the Wellbeing Course (Kayrouz et al., 2015, Titov et al., 2013). Given the importance of the present study’s research question, the difficulties in recruitment, and how close the sample is to the target, the final sample size of 13 was used with the risk of being underpowered to detect change, and less than ideal for providing reliable and robust estimations. The sample of 13 participants, available in all three-time points, is considered minimal, but sufficient in order to estimate change over time.
3. Questionnaire measures
3.1. Primary measures
3.1.1. Patient Health Questionnaire – 9-item (PHQ-9; Kroenke et al., 2001)
The PHQ-9 is a nine-item measure of the symptoms and severity of depression that has been translated and validated in several languages (Gilbody et al., 2007), including Arabic (Al-Qadhi et al., 2014, Becker et al., 2002). It has a clinical cut-off score of 10 that predicts a DSM-IV diagnosis of depression, with higher scores indicating greater symptom severity. Internal consistency of the questionnaire is high (α = 0.74–0.89) (Kroenke et al., 2001), and the questionnaire has good clinical sensitivity to change. Cronbach's alpha in the present study was acceptable (α = 0.78).
3.1.2. Generalised Anxiety Disorder – 7-item scale (GAD-7; Spitzer et al., 2006)
The GAD-7 is a seven-item screening questionnaire that has been found to be sensitive to generalised anxiety disorder, social phobia and panic disorder, with higher scores indicating greater symptom severity (Lowe et al., 2008). It is widely used and has been translated and validated in several languages, including Arabic (e.g., Bener et al., 2013a, Bener et al., 2013b). Internal consistency of the GAD-7 scale is good (α = 0.79–0.91). The GAD-7 has good convergent and divergent validity with other anxiety and disability scales (Dear et al., 2011, Kroenke et al., 2010). A clinical cut-off score of 8 indicated a diagnosis of anxiety disorder (Dear et al., 2011, Lowe et al., 2008, Richards and Suckling, 2009). Cronbach's alpha in the present study was acceptable (α = 0.73).
4. Secondary measures
4.1. Kessler 10-Item Scale (K-10; Kessler et al., 2002)
The K-10 is a ten-item measure of general psychological distress with total scores ≥ 22 associated with a diagnosis of anxiety and depressive disorders (Andrews and Slade, 2001). The Arabic translation of the K10 has been extensively used in WHO World Mental Health Surveys (Kessler et al., 2002) and has been validated for some Arab populations (Fassaert et al., 2009). In the present sample, Cronbach's alpha was high (α = 0.81).
4.2. Sheehan Disability Scales (SDS; Sheehan, 1983)
The SDS is a three-item scale measuring functional impairment in the following domains: (1) work and studies, (2) social life, and (3) family life and home responsibilities. The SDS has been found to have high internal consistency of 0.89 (Leon et al., 1997). In the present study, Cronbach's α = 0.80. Similar to previous translations of the SDS (Molykhia and Ibrahim, 2009), the SDS was translated by a team of professional translators and reviewed and approved by the lead author.
Participants were administered English and Arabic versions of all primary and secondary questionnaires at pre-treatment, post-treatment and at 3-month follow-up, allowing them to complete questionnaires in their preferred language. English and Arabic versions of the PHQ-9 and GAD-7 were also administered weekly to monitor safety and progress of each participant.
4.3. Additional measures
At post-treatment acceptability of the course was assessed by asking two questions in English and Arabic, which required a ‘Yes’ or ‘No’ response. The questions were: (1) Would you recommend this course to a friend or family member also experiencing stress, anxiety, or low mood; and (2) Was it worth your time doing this course?
At three-month follow-up, language preferences of the course were assessed by asking two questions in English and Arabic. The first question, ‘What language did you use to read the lessons of the Arabic Wellbeing Course?’ required a response to a five-point Likert-scale (i.e., 1 - English only; 2 - English mostly; 3 - Both; 4 - Arabic mostly; and 5 - Arabic only). The second question was open-ended and asked, ‘What were the advantages or disadvantages of having the course available in both English and Arabic? Do you have any other feedback for us around this?’
4.4. Intervention
The Wellbeing Course is a five-lesson iCBT intervention targeting core symptoms of both anxiety and depression; that is, a transdiagnostic intervention (Titov et al., 2013). The Wellbeing Course is based on the Macquarie University Model (MUM) of internet-delivered psychological treatment (Titov et al., 2015b). The Wellbeing Course is a structured skills-based course that focuses on teaching practical evidence-based psychological skills (e.g., realistic thinking, assertiveness, behavioural activation and graded exposure) that assist in the management of symptoms of anxiety and depression, consistent with the aforementioned Arab preferences for psychological treatment. This course has been evaluated in several clinical trials (Kirkpatrick et al., 2013, Titov et al., 2013) with individuals of many different cultural backgrounds, including Arab Australians, and has been used in a national online public mental health service to treat > 2000 Australian adults (Titov et al., 2015a).
In addition to the five lessons, the Wellbeing Course includes: (a) a summary of each lesson with homework to apply the skills taught in that lesson, (b) automated emails that encourage adherence and reinforce progress, (c) a secure email system for communication between the therapist and participant, (d) additional online resources about skills not described in the lessons, including communication, assertiveness, and sleep-hygiene skills and (e) stories about people who have recovered from anxiety and depression.
4.5. Translation
The Arabic language version of the Arabic Wellbeing Course retained the core therapeutic components of the English version of the Arabic Wellbeing Course (Kayrouz et al., 2016a). However, modifications in the translation were made to ensure the translation was culturally syntonic; that is, expressions of language were congruent and sensitive to values and meanings of the culture (Bernal et al., 1995). In addition, images of people were changed to include more people with Arab features. Both English and Arabic versions of the lessons of the Arabic Wellbeing Course were presented in parallel, allowing the participants to choose their language of preference.
Translation of the content of the course was conducted in stages. First, a team of five professional translators from a national translation service translated the English version of the Arabic Wellbeing Course into Arabic. Second, in consultation with an independent translation team consisting of a professional translator and community mental health bilingual speaker, the translation was reviewed to ensure that the translation was culturally syntonic and could be understood by an Arab adult with Year 9 equivalent reading ability in Arabic (i.e., about 10 years of primary and secondary education). Third, all suggested changes were reviewed by the lead author (a bilingual psychologist who has worked over 15 years with the Arabic speaking community in Australia) before submitting recommended changes to the principal team of translators. Fourth, changes were discussed by all stakeholders to reach consensus on the changes.
Two examples are presented here of the challenges addressed during translation. One challenge was noted when considering the appropriate Arabic translation of the title of the intervention. The principal team translated wellbeing in Arabic as “الرفاه”, which the independent translation team suggested could be interpreted to mean material wellbeing (i.e., luxurious and wealthy). After discussion, “عافية” which means wellness, was accepted as the least stigmatising and best option. In a second example, after discussion, the term psychological health in Arabic “الصحه النفسيه” (i.e. psychological health) was not used in the title of the course because of the potential stigma of the term due to its association with madness or being possessed, as noted by other researchers in this field (Gearing et al., 2012).
4.6. Therapist
The lead author provided clinical support in Arabic and English via telephone and email to all participants. Consistent with the previous trials of the Wellbeing Course (Dear et al., 2015, Kirkpatrick et al., 2013, Titov et al., 2012, Titov et al., 2013, Titov et al., 2014, Titov et al., 2015a, Titov et al., 2015b), the therapist aimed to keep clinical contact to approximately 10 min per participant per week unless their clinical presentation indicated more time was required. During each contact, the therapist aimed to reinforce progress, summarise key skills of the course, normalise commonly experienced difficulties during treatment and encourage continued engagement. The therapist was supervised by one of the co-authors (BFD) during scheduled weekly meetings and as required. A secure log of contact was kept that included progress notes and contact time.
4.7. Statistical methods
A generalised estimation equation (GEE) modelling technique was employed to examine changes in the symptom measures over time. The GEE method enables the testing of the expected patient trajectory of improvement in symptoms following treatment. Specifically, reduction from a wide range of initial symptoms towards bounded minimal symptoms using a log link function and gamma scale. Similar to the aforementioned power analysis, the sample size requirements for the GEE were considered sufficient, though less than ideal for precision and reducing sample bias. Specifically, a sample consisting of 10 and more repeated observations can detect changes over time with power that is greater than 0.8 given change over time is large (Paik, 1988, Teerenstra et al., 2010). The GEE method was selected because it deals with key issues presented in iCBT trials such as missing data, proportionally changing symptoms and non-independent nature of the repeated measures design of the current study.
To compare the preliminary efficacy of the intervention group across time, GEE analyses were run for the overall sample comparing the primary and secondary outcome variables from pre-treatment to post-treatment and 3-month follow-up in the intervention group. An exchangeable correlation matrix was selected to reduce the cost of the degrees of freedom needed from a relatively small sample size. Pairwise contrasts were made to test additional symptom change between post-treatment and 3-month follow-up.
Missing data were addressed through a method of simulated replacement values, consistent with intention-to-treat principles. To impute missing data, Model estimates (GEE) were used to calculate imputed data, under the assumption of missing completely at random (MCAR). More sensitive replacement methods (such as MAR) were not utilised given the limited sample size.
Two additional methods (last-observation carried forward and completer only analysis) commonly used in pilot studies were employed side-by-side with GEE model-based estimation. This was done to mitigate the risk of overfit or extrapolation from statistical models in relatively small samples.
Based on dissemination studies (Richards and Suckling, 2009), an index of clinical significant remission and deterioration was calculated. The remission index was defined as the proportion of participants who at pre-treatment scored at or above the clinical cut-offs on the PHQ-9 (≥ 10) and GAD-7 (≥ 8), and then subsequently below these clinical cut-offs at post-treatment and three-month follow-up (Richards and Suckling, 2009). Negative effects of treatment (Rozental et al., 2014) were measured as deterioration, which was defined as an increase by five or more points on the PHQ-9 or GAD-7 at post-treatment or follow-up, compared to pre-treatment (Richards and Suckling, 2009). Importantly, in these analyses, the last available data (i.e., last-observation-carried-forward; LOCF) were carried forward for participants who did not complete post-treatment or three-month follow-up questionnaires to provide a conservative estimate of effect sizes and remission. All analyses were performed in SPSS version 22.0 (SPSS, Inc., Chicago, IL).
5. Results
5.1. Adherence and attrition
Ten of thirteen (77%) participants completed the course, which was defined as reading all five lessons within the eight-week period; however, 85% (11/13) read the first four lessons, which provides a proxy of minimum therapeutic dose. Ten of thirteen (77%) participants provided post-treatment and three-month follow-up data. Fig. 1 shows participant flow including adherence and attrition rates.
5.2. Outcomes and effect sizes
The outcomes and effect sizes of the trial are displayed in Table 1. The GEE analyses revealed significant main effects for time on all measures: PHQ-9 (Wald's χ2 (2, N = 13) = 31.43, p < 0.001), GAD-7 (Wald's χ2 (2, N = 13) = 21.26, p < 0.001); SDS (Wald's χ2 (2, N = 13) = 24.24, p < 0.001); and K-10 (Wald's χ2 (2, N = 13) = 32.94, p < 0.001). Pairwise comparisons revealed that PHQ-9, GAD-7, SDS and K-10 scores were significantly lower at post-treatment and 3-month follow-up than at pre-treatment (all p < 0.001). There were no significant differences on all outcome measures between post-treatment and 3-month follow-up.
Table 1.
Observed and estimated means, standard deviations, confidence intervals and effect sizes (Cohen's d) for the overall sample.
| Observed means |
Estimated marginal means |
Within group effect sizes (based on estimated means) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | 3-month follow-up | Pre-treatment | Post-treatment | 3-month follow-up | Pre-post | Pre-treatment to 3-month follow-up | Post-treatment to 3-month follow-up | |
| PHQ-9 | 12.53 (4.66) | 6.60 (4.65) | 5.70 (4.42) | 12.54 (4.48) | 6.72 (3.87) | 5.80 (3.68) | 1.39 (0.50–2.20) | 1.64 (0.71–2.47) | 0.24 (− 0.54–1.01) |
| GAD-7 | 11.15 (5.46) | 6.00 (3.37) | 5.00 (5.06) | 11.15 (5.25) | 6.06 (3.14) | 5.05 (4.21) | 1.18 (0.31–1.97) | 1.28 (0.40–2.08) | 0.27 (− 0.51–1.04) |
| SDS | 24.15 (13.37) | 8.90 (9.53) | 7.00 (7.16) | 24.15 (12.84) | 8.92 (7.93) | 6.88 (5.96) | 1.43 (0.53–2.24) | 1.72 (0.78–2.56) | 0.29 (− 0.49–1.05) |
| K10 | 29.62 (8.10) | 18.60 (6.40) | 18.90 (9.45) | 29.62 (7.78) | 18.81 (5.34) | 19.11 (7.87) | 1.62 (0.69–2.45) | 1.34 (0.45–2.15) | − 0.05 (− 0.81–0.0.72) |
Note: Standard deviations and 95% confidence intervals are shown in parentheses. Pre: pre-treatment, post: post-treatment; PHQ-9: Patient Health Questionnaire 9-Item; GAD-7: Generalised Anxiety Disorder 7-Item; SDS: Sheehan Disability Scale; K10: Kessler 10-Item.
Large pre-treatment to post-treatment and pre-treatment to 3-month follow-up effect sizes were found on all measures, using both completer and estimated-marginal means (completers: Cohen's d = 1.10 to 1.60; estimated marginal means; d = 1.18 to 1.72). Further, moderate to large effect sizes on primary measures (i.e., PHQ-9 and GAD-7) were also found when using last observation carried forward (LOCF: Cohen's d for PHQ-9 and GAD-7 were 0.89 and 0.74 respectively). Comparison of post-treatment to 3-month follow-up effect sizes indicated there were no additional improvements across all outcome measures.
5.3. Clinical significance
Table 2 displays the clinically significant remission and recovery rates on the PHQ-9 and GAD-7. For the PHQ-9, of the 10/13 (76.92%) participants who scored above the cutoff at pre-treatment, eight (8/13; 61.54%) were below this cutoff at post-treatment and 3-month follow-up. Six of 13 (46.15%) and five of 13 (38.46%) participants made a 50% or greater improvement on the PHQ-9 at post-treatment and 3-month follow-up respectively. For the GAD-7, of the 9/13 (69.23%) participants who scored above the cutoff at pre-treatment, 7/13 (53.84%) were below this cutoff at post-treatment and 3-month follow-up. Three of 13 (23.08%) and five of 13 (38.46%) participants made a 50% or greater improvement on the GAD-7 at post-treatment and 3-month follow-up respectively.
Table 2.
Proportion of participants below cut-off scores of clinical significance (remission) and proportion demonstrating at least 50% reduction in pre-treatment scores (recovery) and the average improvement of the group.
| Pre-treatment |
Post-treatment |
3-month follow-up |
|||||
|---|---|---|---|---|---|---|---|
| ≥ Clinical cut-off | ≤ Clinical cut-off | ≥ 50% improvement | Average improvement | ≤ Clinical cut-off | ≥ 50% improvement | Average improvement | |
| PHQ-9 | 10/13 (76.92%) | 8/13 (61.54%) | 6/13 (46.15%) | 33.10% | 8/13 (61.54%) | 5/13 (38.46%) | 40.38% |
| GAD-7 | 9/13 (69.23%) | 7/13 (53.84%) | 3/13 (23.08%) | 32.06% | 7/13 (53.84%) | 5/13 (38.46%) | 37.77% |
Note: Intention-to-treat model was employed with last-observation being carried forward if follow-up data was not available. The clinical cut-offs utilised for the PHQ-9 and GAD-7 were 10 and 8 respectively.
5.4. Deterioration
At post-treatment and 3-month follow-up, none of the 13 participants obtained PHQ-9 and GAD-7 scores five or more points higher compared to pre-treatment, respectively, indicating no participants met criteria for deterioration.
5.5. Acceptability
Ten of 13 respondents (77%) provided ratings of the acceptability of the course. All (10/10) of the responding participants reported both that it was ‘worth their time doing the course’, and that they would ‘recommend this course to a friend or family member with anxiety or depression’.
5.6. Language preferences
Ten of 13 respondents (77%) provided responses for language preferences. Seventy percent (7/10) reported using both English and Arabic translations of the Arabic Wellbeing, 20% (2/10) reported using English only, and 10% (1/10) reported using Arabic only.
5.7. Contact
The mean total therapist time per participant over the eight-week course was 63.54 min (SD = 28.45), which comprised an average of 53.69 min (SD = 27.56) and 9.85 min (SD = 5.44) per participant for telephone calls and secure private emails, respectively. An additional average of 13.69 min (SD = 3.53) per participant was required for administrative purposes including the screening telephone call at recruitment. The therapist made an average of 10 telephone calls (SD = 1.44; range = 6 to 11) and an average of 5.9 emails to each participant (SD = 1.46; range = 3 to 8) during the course.
6. Discussion
The primary aims of the present study were to examine the preliminary efficacy and acceptability of the Arabic Language Wellbeing Course, a culturally modified transdiagnostic iCBT program, for symptoms of anxiety and depression in Arab-speaking Australians when administered by a clinician. It was hypothesised that participants would show statistically and clinically significant reductions in symptoms of depression, anxiety, distress and disability and that they would rate the course as worthwhile and recommend the program to a friend or family member. These hypotheses were supported.
Overall, the results from this small, preliminary trial are encouraging. Large within-group effect sizes were found on the primary and secondary outcome measures including a measure of disability, indicating that improvements generalised to other domains. The available data indicated that these improvements were maintained at follow-up and were reflected in moderate levels of remission and recovery. These results are consistent with the results of previous small open trials of the English version of the Arabic Wellbeing Course with Arab people living in Australia (Kayrouz et al., 2015), and in other countries (Kayrouz et al., 2016a), and with results observed in an evaluation of the Wellbeing Course used in a clinician-guided format with a general Australian population (Dear et al., 2015, Kirkpatrick et al., 2013, Titov et al., 2013, Titov et al., 2014, Titov et al., 2012, Titov et al., 2015a, Titov et al., 2015b). In addition, high rates of participant satisfaction were observed in the present trial.
These results are also consistent with the positive results from an emerging body of work that has evaluated modified and translated versions of iCBT interventions developed for Western populations with other culturally and linguistically diverse (CALD) groups including Chinese and Arab people (Choi et al., 2012, Knaevelsrud et al., 2015, Wagner et al., 2012). This literature provides support for the position that people of different cultures share similar experiences of anxiety and depression, and may, therefore, benefit from similar treatment strategies. Notwithstanding the limitations of an open trial design, the present study extends these results by demonstrating that relatively minor modifications and translations may be sufficient to make interventions acceptable to a targeted CALD group. Importantly, since modified interventions have shown preliminary effectiveness in translated formats (Choi et al., 2012, Knaevelsrud et al., 2015), the potential for reducing the language barrier and increasing the availability of culturally appropriate mental health services for CALD communities is considerable.
An interesting and unexpected finding was that 70% of participants reported using both English and Arabic translations of the Arabic Wellbeing Course. Participants reported that presenting the course in English and Arabic improved their understanding of the content of the course. For example, one participant reported, “It was very valuable to be able to navigate through the course in Arabic when not sure about any psychology terms in English”. Consequently, further research and future dissemination of the Arabic Wellbeing Course may need to consider presenting the course in both English and Arabic.
Despite addressing a key issue relating to the language barrier, there was a relatively slow rate of recruitment. This difficulty with recruitment may reflect relatively low levels of mental health literacy of CALD populations (Adrian and Aseel, 2014). This suggests that strategies that aim to reduce barriers to care require multiple targets including appropriately translated and modified treatment materials, as well as publicly available materials that can increase mental health literacy in the target groups. Such materials could be made available not only on websites, but also social media, which appears to have the potential for increasing access among otherwise hard-to-reach groups (Kayrouz et al., 2016b, Ünlü Ince et al., 2014).
Limitations of this study include the following. First, the absence of a control group means it is not possible to determine the effect of the treatment beyond that of spontaneous remission. Second, despite the small sample size being less than ideal, statistically and clinically significant improvements in symptom levels were found, however an increased sample size would improve the accuracy and robustness of the symptom change estimation. Third, the small sample size limits the extent to which the results can be generalised and means that significant caution is needed in interpreting the results of the trial beyond conclusions about the general feasibility of iCBT for Arabs in Australia. Fourth, the relatively high educational level of the sample limits the extent to which the results can be generalised to those with lower levels of educational attainment. Fifth, the level of acculturation was not measured raising questions about the extent to which acculturation may moderate treatment outcomes. However, a large randomised controlled trial is planned, which will address several of these issues.
In summary, the translated format of the Arabic Wellbeing Course resulted in large improvements on measures of anxiety, depression, stress and disability at post-treatment, which were sustained at three-month follow-up. Moreover, participants rated the treatment as acceptable. These results also contribute to an emerging body of evidence indicating that iCBT interventions are a promising strategy that is feasible, has potential as an effective intervention, and for increasing access to treatment by CALD populations who might otherwise be unable to access mental health care.
Funding
The funding for the study was provided by Macquarie University as part of the lead author's PhD candidature. BFD is supported by a National Health and Medical Research Council Australian Public Health Fellowship. The development of the Wellbeing Course was enabled by funding from the Australian National Health and Medical Research Council Project Grant No. 630560.
Declaration of conflicting interests
The authors declare that there is no conflict of interest.
Acknowledgements
The authors wish to acknowledge all participants, service providers, Arabic speaking organisations and other agencies that supported this study.
References
- Abudabbeh N., Hays P.A. Cognitive behavioral therapy with people of Arab heritage. In: Hays P.A., Iwamasa G.Y., editors. Culturally Responsive Cognitive-Behavioral Therapy: Assessment, Practice, and Supervision. American Psychological Association; Washington, DC: 2006. pp. 141–159. [Google Scholar]
- Adrian F., Aseel H. Mental health literacy in non-Western countries: a review of the recent literature. Ment. Health Rev. J. 2014;19(2):84–98. [Google Scholar]
- Al-Krenawi A., Graham J.R. Culturally sensitive social work practice with Arab clients in mental health settings. Health Soc. Work. 2000;25(1):9–22. doi: 10.1093/hsw/25.1.9. [DOI] [PubMed] [Google Scholar]
- Al-Qadhi W., ur Rahman S., Ferwana M.S., Abdulmajeed I.A. Adult depression screening in Saudi primary care: prevalence, instrument and cost. BMC Psychiatry. 2014;14(1):190–198. doi: 10.1186/1471-244X-14-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G., Titov N. Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry. 2014;13(1):4–11. doi: 10.1002/wps.20083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G., Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10) Aust. N. Z. J. Public Health. 2001;25(6):494–497. doi: 10.1111/j.1467-842x.2001.tb00310.x. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics . ABS; Canberra: 2006. Census of Population and Housing - Fact Sheets, 2006, 2914.0. [Google Scholar]
- Australian Bureau of Statistics . ABS; Canberra: 2011. Reflecting a Nation: Stories From the 2011 Census, 2012–2013, Cat No. 2071.0. [Google Scholar]
- Becker S., Al Zaid K., Al Faris E. Screening for somatization and depression in Saudi Arabia: a validation study of the PHQ in primary care. Int. J. Psychiatry Med. 2002;32(3):271–283. doi: 10.2190/XTDD-8L18-P9E0-JYRV. [DOI] [PubMed] [Google Scholar]
- Bener A., Al-Kazaz M., Ftouni D., Al-Harthy M., Dafeeah E.E. Diagnostic overlap of depressive, anxiety, stress and somatoform disorders in primary care. Asia-Pacific Psychiatry. 2013;5(1):E29–E38. doi: 10.1111/j.1758-5872.2012.00215.x. [DOI] [PubMed] [Google Scholar]
- Bener A., Dafeeah E.E., Chaturvedi S.K., Bhugra D. Somatic symptoms in primary care and psychological comorbidities in Qatar: neglected burden of disease. Int. Rev. Psychiatry. 2013;25(1):100–106. doi: 10.3109/09540261.2012.730993. [DOI] [PubMed] [Google Scholar]
- Bernal G., Bonilla J., Bellido C. Ecological validity and cultural sensitivity for outcome research: issues for the cultural adaptation and development of psychosocial treatments with Hispanics. J. Abnorm. Child Psychol. 1995;23(1):67–82. doi: 10.1007/BF01447045. [DOI] [PubMed] [Google Scholar]
- Centre for Epidemiology and Research . NSW Department of Health; Sydney: 2010. 2006–2009 Report on Adult Health by Country of Birth From the New South Wales Population Health Survey. (Retrieved from http://www.health.nsw.gov.au/surveys/adult/Publications/hsa:0609cob.pdf) [Google Scholar]
- Chaleby K. Psychotherapy with Arab patients, toward a culturally oriented technique. Arab J. Psychiatry. 1992;3(1):16–27. (Retrieved from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=psyc3&AN=2001-16515-003) [Google Scholar]
- Choi I., Zou J., Titov N., Dear B.F., Li S., Johnston L.…Hunt C. Culturally attuned Internet treatment for depression amongst Chinese Australians: a randomised controlled trial. J. Affect. Disord. 2012;136(3):459–468. doi: 10.1016/j.jad.2011.11.003. [DOI] [PubMed] [Google Scholar]
- Dear B.F., Titov N., Sunderland M., McMillan D., Anderson T., Lorian C., Robinson E. Psychometric comparison of the Generalized Anxiety Disorder Scale-7 and the Penn State Worry Questionnaire for measuring response during treatment of generalised anxiety disorder. Cogn. Behav. Ther. 2011;40(3):216–227. doi: 10.1080/16506073.2011.582138. [DOI] [PubMed] [Google Scholar]
- Dear B.F., Staples L.G., Terides M., Karin E., Zou J., Johnston L.…Titov N. Transdiagnostic versus disorder-specific and clinician-guided versus self-guided treatment for generalised anxiety disorder: a randomised controlled trial. J. Anxiety Disord. 2015;36:63–77. doi: 10.1016/j.janxdis.2015.09.003. [DOI] [PubMed] [Google Scholar]
- Fassaert T., De Wit M.A.S., Tuinebreijer W.C., Wouters H., Verhoeff A.P., Beekman A.T.F., Dekker J. Psychometric properties of an interviewer-administered version of the Kessler Psychological Distress scale (K10) among Dutch, Moroccan and Turkish respondents. Int. J. Methods Psychiatr. Res. 2009;18(3):159–168. doi: 10.1002/mpr.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gearing R.E., Schwalbe C.S., MacKenzie M.J., Brewer K.B., Ibrahim R.W., Olimat H.S.…Al-Krenawi A. Adaptation and translation of mental health interventions in Middle Eastern Arab countries: a systematic review of barriers to and strategies for effective treatment implementation. Int. J. Soc. Psychiatry. 2012;59(7):671–681. doi: 10.1177/0020764012452349. [DOI] [PubMed] [Google Scholar]
- Gilbody S., Richards D., Brealey S., Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J. Gen. Intern. Med. 2007;22(11):1596–1602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbard A.E., Ahern J., Fleischer N.L., Laan M.V.D., Lippman S.A., Jewell N.…Satariano W.A. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology. 2010;21(4):467–474. doi: 10.1097/EDE.0b013e3181caeb90. [DOI] [PubMed] [Google Scholar]
- Kayrouz, R., Dear, B. F., Karin, E., Terides, M., Gandy, M., Fogliati, V., & Titov, N. (unpublished). Acceptability of mental health services for anxiety and depression amongst Arabs. [DOI] [PubMed]
- Kayrouz R., Dear B.F., Johnston L., Keyrouz L., Nehme E., Laube R., Titov N. Intergenerational and cross-cultural differences in emotional wellbeing, mental health service utilisation, treatment seeking preferences and acceptability of psychological treatments for Arab Australians. Int. J. Soc. Psychiatry. 2014;61(5):484–491. doi: 10.1177/0020764014553004. [DOI] [PubMed] [Google Scholar]
- Kayrouz R., Dear B.F., Johnston L., Gandy M., Fogliati V.J., Sheehan J., Titov N. A feasibility open trial of guided Internet-delivered cognitive behavioural therapy for anxiety and depression amongst Arab Australians. Internet Interv. 2015;2(1):32–38. [Google Scholar]
- Kayrouz R., Dear B.F., Karin E., Gandy M., Fogliati V.J., Terides M.D., Titov N. A pilot study of self-guided internet-delivered cognitive behavioural therapy for anxiety and depression among Arabs. Internet Interv. 2016;3:18–24. doi: 10.1016/j.invent.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayrouz R., Dear B.F., Karin E., Titov N. Facebook as an effective recruitment strategy for mental health research of hard to reach populations. Internet Interv. 2016;4:1–10. doi: 10.1016/j.invent.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.-L.T.…Zaslavsky A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002;32(06):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick T., Dear B.F., Johnston L., Titov N. A feasibility open trial of an internet-delivered cognitive-behavioural therapy (iCBT) among consumers of a non-governmental mental health organisation with anxiety. Peer J. 2013;1 doi: 10.7717/peerj.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knaevelsrud C., Brand J., Lange A., Ruwaard J., Wagner B. Web-based psychotherapy for posttraumatic stress disorder in war-traumatized Arab patients: randomized controlled trial. J. Med. Internet Res. 2015;17(3) doi: 10.2196/jmir.3582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W., Löwe B. The Patient Health Questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen. Hosp. Psychiatry. 2010;32(4):345–359. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- Leon A.C., Olfson M., Portera L., Farber L., Sheehan D.V. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. Int. J. Psychiatry Med. 1997;27:93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD. [DOI] [PubMed] [Google Scholar]
- Lowe B., Decker O., Muller S., Brahler E., Schellberg D., Herzog W., Herzberg P.Y. Validation and standardization of the Generalized Anxiety Disorder screener (GAD-7) in the general population. Med. Care. 2008;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Molykhia T., Ibrahim S. A comparative study of disability among patients suffering social anxiety disorder and comorbid depressive disorders. Egypt. J. Psychiatry. 2009;29(1):27–33. [Google Scholar]
- Paik M.C. Repeated measurement analysis for nonnormal data in small samples. Commun. Stat. Simul. Comput. 1988;17(4):1155–1171. [Google Scholar]
- Richards D.A., Suckling R. Improving access to psychological therapies: phase IV prospective cohort study. Br. J. Clin. Psychol. 2009;48(4):377–396. doi: 10.1348/014466509X405178. [DOI] [PubMed] [Google Scholar]
- Rozental A., Andersson G., Boettcher J., Ebert D.D., Cuijpers P., Knaevelsrud C.…Carlbring P. Consensus statement on defining and measuring negative effects of Internet interventions. Internet Interv. 2014;1(1):12–19. [Google Scholar]
- Sheehan D.V. Charles Scribner and Sons; New York: 1983. The Anxiety Disease. [Google Scholar]
- Slade T., Johnston A., Oakley Browne M.A., Andrews G., Whiteford H. 2007 National Survey of Mental Health and Wellbeing: methods and key findings. Aust. N. Z. J. Psychiatry. 2009;43(7):594–605. doi: 10.1080/00048670902970882. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stenmark H., Catani C., Neuner F., Elbert T., Holen A. Treating PTSD in refugees and asylum seekers within the general health care system. A randomized controlled multicenter study. Behav. Res. Ther. 2013;51(10):641–647. doi: 10.1016/j.brat.2013.07.002. [DOI] [PubMed] [Google Scholar]
- Taloyan M., Alinaghizadeh H., Löfvander M. Short-term cognitive-behavioral treatment in multicultural primary care of patients with longstanding backache. Scand. J. Psychol. 2013;54(5):371–375. doi: 10.1111/sjop.12061. [DOI] [PubMed] [Google Scholar]
- Teerenstra S., Lu B., Preisser J.S., van Achterberg T., Borm G.F. Sample size considerations for GEE analyses of three-level cluster randomized trials. Biometrics. 2010;66(4):1230–1237. doi: 10.1111/j.1541-0420.2009.01374.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N., Dear B.F., Johnston L., Terides M. Transdiagnostic internet treatment for anxiety and depression. Spanish J. Clin. Psychol. 2012;17(3):237–260. [Google Scholar]
- Titov N., Dear B.F., Johnston L., Lorian C., Zou J., Wootton B.…Rapee R.M. Improving adherence and clinical outcomes in self-guided internet treatment for anxiety and depression: randomised controlled trial. PLoS One. 2013;8(7) doi: 10.1371/journal.pone.0062873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N., Dear B.F., Johnston L., McEvoy P., Wootton B., Terides M.…Rapee R. Improving adherence and clinical outcomes in self-guided internet treatment for anxiety and depression: a 12-month follow-up of a randomised controlled trial. PLoS One. 2014;9(2) doi: 10.1371/journal.pone.0089591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N., Dear B.F., Staples L.G., Bennett-Levy J., Klein B., Rapee R.M.…Nielssen O.B. MindSpot Clinic: an accessible, efficient, and effective online treatment service for anxiety and depression. Psychiatr. Serv. 2015;66(10):1043–1050. doi: 10.1176/appi.ps.201400477. [DOI] [PubMed] [Google Scholar]
- Titov N., Dear B.F., Staples L.G., Terides M.D., Karin E., Sheehan J.…McEvoy P.M. Disorder-specific versus transdiagnostic and clinician-guided versus self-guided treatment for major depressive disorder and comorbid anxiety disorders: a randomized controlled trial. J. Anxiety Disord. 2015;35:88–102. doi: 10.1016/j.janxdis.2015.08.002. [DOI] [PubMed] [Google Scholar]
- Ünlü Ince B., Cuijpers P., van 't Hof E., Riper H. Reaching and recruiting Turkish migrants for a clinical trial through Facebook: a process evaluation. Internet Interv. 2014;1(2):74–83. [Google Scholar]
- Wagner R., Derrick S., Claire M., Jackie J. Impact of culture on the experience of panic symptoms in Arab and Australian patients at a psychology clinic. Aust. Psychol. 2008;43(2):127–131. [Google Scholar]
- Wagner B., Schulz W., Knaevelsrud C. Efficacy of an Internet-based intervention for posttraumatic stress disorder in Iraq: a pilot study. Psychiatry Res. 2012;195(1–2):85–88. doi: 10.1016/j.psychres.2011.07.026. [DOI] [PubMed] [Google Scholar]
- Youssef J., Deane F.P. Factors influencing mental-health help-seeking in Arabic-speaking communities in Sydney, Australia. Ment. Health Relig. Cult. 2006;9(1):43–66. [Google Scholar]