Abstract
Background
Insomnia is highly prevalent in breast cancer (BRC) patients, but non-pharmacological treatment is not widely available. The aim of this preliminary study was to investigate whether guided cognitive behavioral therapy via the Internet (I-CBT) is a feasible and effective solution for this undertreated condition in BRC patients, and to investigate who benefits most.
Methods
An existing evidence based I-CBT sleep intervention (I-Sleep) was adapted for BRC patients. An open mixed methods design was used including qualitative interviews and pre- and post-test questionnaires measuring sleep, fatigue, daily functioning, and psychological distress.
Results
100 of the 171 participants (59%) completed the intervention fully and participants highly valued the intervention (7.5 out of 10). Large to small pre-post effect sizes were found on insomnia severity (d = 1.33) fatigue (d = 0.24), and daytime functioning (d = 0.30). Younger patients and patients with more severe insomnia at baseline benefited most from the intervention.
Conclusion
The I-CBT intervention I-Sleep is feasible, well-accepted, and effective for BRC patients who suffer from insomnia, especially for younger patients and those with more severe insomnia.
Keywords: Breast cancer, Insomnia, E-health, Internet, CBT, Web-based intervention
1. Introduction
Insomnia is common in the general population, but even more prevalent among cancer patients. About two thirds of all the women who have been treated for breast cancer (BRC) experience insomnia symptoms. About one third of them fulfill the criteria for an insomnia disorder (Savard et al., 2011a). This is defined by (a) dissatisfaction with sleep quantity or quality (sleep onset latency or wake after sleep onset or early morning awakening ≥ 30 min), (b) for 3 or more nights a week, (c) for at least 3 months, (d) causing clinically significant impairment in day-time functioning, (e) which cannot be explained by other sleep disorders or by drugs (American Psychiatric Association, 2013).
About three-quarter of all people who visit a physician for insomnia receive medication, mostly benzodiazepines (Benca, 2005, Knuistingh et al., 2005). Although medication is effective in the short term, it has negative side effects and significant risks (Buscemi et al., 2007). The preferred treatment for insomnia is cognitive behavioral therapy (CBT; Edinger and Wohlgemuth, 1999). CBT is as effective as medication in the short term and more effective in the long term (Berger et al., 2009, Espie et al., 2008, Matthews et al., 2014, Morin et al., 2006, Neylan, 2011). However, the availability of CBT is limited because of a lack of qualified therapists. Moreover, accessibility is hampered by geographic distances, and personal limitations on travel and costs. For these reasons Internet-CBT (I-CBT) has been developed.
A number of different studies have demonstrated the effectiveness of internet based treatment for insomnia among otherwise healthy patients (van Straten and Cuijpers, 2009, Jernelöv et al., 2012, Zachariae et al., 2016, Seyffert et al., 2016). The Dutch CBT intervention I-Sleep, which is used in the current study, is an example of this (van Straten et al., 2013).
Many BRC patients don't seek help for their insomnia because they often think that insomnia is a normal and temporary consequence of cancer treatment (Berger et al., 2009). Nevertheless, the body of evidence that CBT can effectively reduce insomnia in BRC patients is growing (Fiorentino and Ancoli-Israel, 2006, Savard et al., 2005a, Espie et al., 2008). Furthermore, the first studies on self-administered CBT for insomnia in cancer patients (video- or web-based) also showed promising results (Savard et al., 2011b, Ritterband et al., 2012, Savard et al., 2014). The question remains whether or not it is feasible to implement an online insomnia intervention for BRC patients in routine care: do they want to use it and do they complete the program? Next, it is unknown if the effects which are established in RCTs are similar to those obtained in routine care. Therefore, the aims of the present study on our adapted guided I-Sleep intervention are:
-
1)
How feasible is a guided web-based intervention in routine care: is there a need for this type of program (do BRC patients want to participate), do patients adhere to it, and do they feel that the intervention is worthwhile?
-
2)
Is the guided web-based intervention effective? Do BRC patients experience less symptoms after the guided I-CBT in comparison to pre-treatment levels and how do these improvements in terms of effect sizes compare to those obtained in previous RCTs?
-
3)
Which BRC patients benefit the most from the guided I-CBT? What demographic, clinical and treatment characteristics are associated with treatment outcomes?
2. Methods/design
2.1. Study design
An open mixed methods design was used with web-based pre- and post-treatment questionnaires and semi-structured telephone interviews. The Medical Ethics Committee confirmed that the “Medical Research Involving Human Subjects Act” (WMO) does not apply to the study (registration number 2013.254). The study protocol is also approved by the faculty Ethical Committee and the Scientific Committees of the participating hospitals. All participants provided web-based informed consent, and therewith approved the study procedures and data storage.
2.2. Recruitment
We collaborated with three hospital-based BRC care units in and around the city of Amsterdam. Specialized nurses directed possibly eligible patients to the Internet site (www.slaapproblemen-na-borstkanker.nl). On this public website, the study goals and procedures were explained and participants could express their interest in the treatment. Recruitment of participants was also done by advertising on BRC social media sites.
2.3. Inclusion criteria
BRC patients were eligible to participate if they met the following criteria: 1) self-reported insomnia, 2) surgery, chemotherapy and/or radiation treatment for BRC finished three months to five years before inclusion, 3) 18 years or older, 4) sufficient mastery of Dutch language, and 5) access to the internet.
2.4. Guided I-CBT intervention
The I-Sleep intervention comprises six sessions. Each session contains information, a daily sleep diary, exercises, and examples of other BRC patients going through insomnia CBT. Each session covers a different theme: 1) psycho-education on sleep and insomnia, 2) sleep hygiene and behaviors that can hinder or promote sleep, 3) sleep restriction and stimulus control – starting a new sleep rhythm with fixed (restricted) times for going to bed at night and getting out of bed in the morning, 4) relaxation techniques, 5) dysfunctional thoughts about sleep and 6relapse prevention.
The I-Sleep intervention was adapted for BRC patients based on in-depth interviews with five BRC patients with insomnia, and the available literature on specific characteristics of insomnia related to BRC. Information on postoperative pain, early menopause and hot flushes was added to the psycho-education in the first lesson. Furthermore, three examples of BRC patients with insomnia, representing different situations in terms of age, cancer treatment, and types of sleep difficulties were described and added. The five interviewed patients evaluated and approved the adapted intervention.
After completing the pre-treatment questionnaire and providing informed consent, a coach was assigned to a participant. The coaches were trained psychologists and mental health nurses. They provided weekly online feedback on the assignments in order to provide more explanation if needed and to encourage participants to adhere to the assignments.
2.5. Procedures
The online pre-treatment questionnaire was sent before the start of the web-based intervention. The post-treatment questionnaire was sent 9 weeks later. A representative subsample of participants was chosen for the semi-structured interviews, selected using the following criteria: younger and older age, (dis)satisfaction with treatment, level of adherence to the treatment, and severity of insomnia symptoms at the start of the treatment. Interviews were conducted until saturation was reached, hence when no new topics were brought up by the patients.
2.6. Within group effects
The primary outcome measure was insomnia severity. Secondary outcome measures were fatigue, daily functioning and symptoms of anxiety and depression.
Insomnia severity was measured with the Insomnia Severity Index (ISI): A 7-item questionnaire with a total score ranging from 0 to 28 (Morin, 1993) and can be divided into: 0–7 = no clinically significant insomnia, 8–14 = sub threshold insomnia, 15–21 = clinical insomnia (moderate severity) and 22–28 = clinical insomnia (severe). The ISI is validated for web delivery (Thorndike et al., 2011) and cancer patients (Savard et al., 2005b).
Fatigue was measured with the Fatigue Severity Scale (FSS): A 9-item questionnaire with a total scoring ranging from 9 to 63 (Krupp et al. 1989). Higher scores indicate greater fatigue.
Daily functioning was measured with the Work and Social Adjustment Scale (WSAS): A 4-item questionnaire rated on an 8-point Likert scale (0 = not at all impaired, 8 = very severely impaired). Each item measures a domain of functioning: household, work, friendship and social functioning (Marks, 1986).
Symptoms of anxiety and depression were measured with the Hospital Anxiety and Depression scales (HADS): A 14-item questionnaire (Zigmond and Snaith, 1983) with two 7-item subscales: depression (HADS-D) and anxiety (HADS-A), both with a total score range of 0–21. Scores 0–7 excludes a depression or anxiety disorder, scores 8–10 indicate a possible depression or anxiety disorder, scores 11–21 indicate a probable depression or anxiety disorder.
Demographic characteristics in the questionnaire included age, nationality, marital status, educational level and work status. Clinical characteristics included sick leave from work in the previous month, sleep medication use and BRC treatment received (surgery, radiotherapy, chemotherapy, and hormonal therapy).
2.7. Feasibility
To measure feasibility, we examined the number of lessons finished by the patients. We also evaluated treatment satisfaction with 14 items developed by the research group. Each item was rated on a 3-point Likert scale (0 = fully agree, 1 = neutral, 2 = fully disagree.
The semi-structured interviews aimed at discussing the following topics: motivation for treatment, preferences for web-based or face-to-face treatment, experiences with adaptations made for breast cancer, experiences with coaching, and suggestions for improvement. The interview was conducted by a master student in psychology and took approximately 45 min.
2.8. Data analysis
First, we described the characteristics of the study population with regard to demographic factors, the history of cancer, insomnia severity, and level of functioning. We investigated potential selective drop-out by comparing the completers of the intervention, with the participants that did not complete the intervention. To test the effect of the intervention we calculated Cohen's d by dividing the difference in pre- and post-test scores of participants by the pooled standard deviation for each outcome measure (Cohen, 1988). A Cohen's d of 0.00–0.32 is considered as small, 0.33–0.55 as medium, and > 0.56 as large (Lipsey, 1990, Lipsey and Wilson, 1993). We performed intention to treat analyses on our primary outcome measure. Missing post-test scores were imputed using a multiple imputation procedure. For the imputation procedure we included all baseline clinical variables (ISI, FSS, Hads anxiety, Hads depression, WSAS functioning) as well as age, education and number of days between randomisation and start intervention.
Satisfaction with the intervention was assessed with the 14 statements (% agreed). The semi-structured interviews were transcripted and the information was categorised within the themes. For every theme we summarized the main findings.
Finally, in order to identify characteristics of BRC patients who might benefit most from the intervention we performed univariate and multivariate regression analyses on the insomnia improvement scores. We included the following independent variables in the model: demographic characteristic, characteristics on illness history, severity of insomnia, severity of anxiety and depression, and level of functioning.
3. Results
3.1. Baseline characteristics
The mean age of the 171 women who accessed to the guided internet intervention was 49 years (range 21 to 76, median 50). Most of them were living with their partner or were married (79%). Most women had a paid job (79%), but almost half of those were on sick leave. Most of the women had been treated for BRC with chemotherapy (77.8%) and with hormonal therapy (76%). The mean time between surgery and admission to the intervention was 2.3 years. 51 patients suffered from subthreshold insomnia (ISI score 8–14), 104 patients from clinical insomnia with moderate severity (ISI score 15–21) while the remaining 16 patients suffered from severe clinical insomnia (ISI score > 21). Most of the women were self-referred to the intervention by information on the internet (66.5%), and 33.5% of the women were referred by routine care procedures. We additionally examined the differences between routine care recruitment and internet recruitment, and found that higher educated women were referred significantly more by medical staff (64.9% vs 46.9%, p = 0.03).
We compared the baseline scores of the 100 women who completed the intervention with the 71 women who did not complete the intervention. Non-completers suffered significantly more often from daytime fatigue (p < 0.01), and were more often on sick leave (p < 0.02) (Table 1).
Table 1.
Demographic and baseline characteristics of 171 women who applied to the internet course.
| Total N = 171; 100% |
Treatment completed N = 100 (58.5%) |
Treatment not completed N = 71 (42.5%) |
p | |
|---|---|---|---|---|
| Demographic characteristics | ||||
| % Women | 100% | 100% | 100% | NA |
| Age mean (SD) | 49.4 (8.7) | 50.1 (9.0) | 48.3 (8.0) | 0.17 |
| % Born in the Netherlandsa | 84.2% | 85.0% | 83.1% | 0.74 |
| % Higher education | 53.2% | 59.0% | 45.1% | 0.07 |
| % Living together | 78.9% | 79.0% | 78.9% | 0.98 |
| % In a paid job | 78.9% | 80.0% | 77.5% | 0.69 |
| % On sick leave | 47.4% | 38.8% | 60.0% | 0.02 |
| Type of treatment | ||||
| % Complete breast amputation | 60.8% | 64.0% | 56.3% | 0.31 |
| Years between operation and admission to intervention, mean (SD) | 2.3 (2.1) | 2.4 (2.2) | 2.2 (2.0) | 0.62 |
| % Radiotherapy | 65.5% | 66.0% | 64.8% | 0.87 |
| % Chemotherapy | 77.8% | 77.0% | 78.9% | 0.77 |
| % Hormonal therapy | 76.0% | 76.0% | 76.1% | 0.99 |
| % With lymphe oedemia | 46.8% | 41.0% | 54.9% | 0.07 |
| Sleep characteristics | ||||
| Insomnia severity index, mean (SD) | 16.5 (3.6) | 16.1 (3.4) | 17.0 (3.9) | 0.11 |
| Fatigue Severity Scale, mean (SD) | 39.3 (11.1) | 37.3 (11.1) | 42.2 (10.6) | < 0.01 |
| % With sleep medication | 45.0% | 48.0% | 40.8% | 0.35 |
| % Insomnia before breast cancer | 38.0% | 41.0% | 33.8% | 0.34 |
| % Sleep medication in history | 25.7% | 29.0% | 21.1% | 0.25 |
| % Other sleep treatment in history | 7.6% | 8.0% | 7.0% | 0.82 |
| Psychological symptoms and functioning | ||||
| HADS-anxiety | 7.6 (3.7) | 7.6 (3.7) | 7.6 (3.8) | 0.95 |
| HADS-depression | 5.5 (3.7) | 5.2 (3.5) | 5.9 (4.0) | 0.20 |
| WSAS functioning (total) | 16.2 (9.7) | 15.4 (9.6) | 17.3 (9.7) | 0.20 |
| WSAS household | 3.9 (2.8) | 3.5 (2.6) | 4.5 (2.9) | 0.12 |
| WSAS work | 4.5 (3.1) | 4.4 (3.1) | 4.6 (3.2) | 0.63 |
| WSAS friendship | 3.8 (2.8) | 3.7 (2.7) | 4.0 (2.8) | 0.46 |
| WSAS social functioning | 4.0 (2.7) | 3.9 (2.7) | 4.2 (2.8) | 0.48 |
| % Medical referral | 33.5% | 33.0% | 34.5% | 0.86 |
Participant + both parents were born in the Netherlands.
3.2. Feasibility: response and adherence
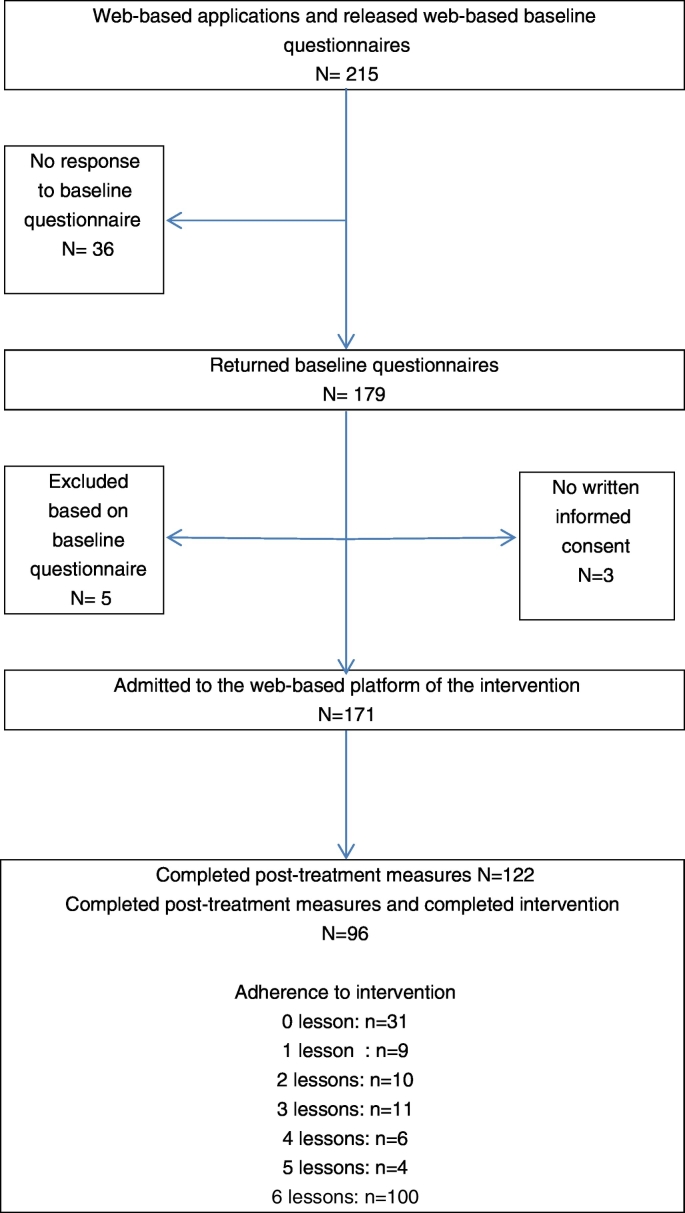
During the inclusion period of 9 months 215 patients subscribed, of which 179 (83%) returned the pre-treatment questionnaire (Fig. 1). Five of those were excluded because they did not meet the inclusion criteria, and 3 did not provide informed consent, leaving 171 included women. This exceeded our expectations which implied that we had to train more therapists than we had planned beforehand.
Fig. 1.
Flow diagram of participants' progress though the study phases: pre- and post-treatment measurement, and intervention adherence.
Of the 171 women registered to the intervention, 31 (18%) never started. Another 19 (11%) completed only 1 or 2 lessons, 21 (12%) carried out a substantial part of the intervention (3, 4 or 5 lessons) while the remaining 100 (59%) completed the whole course of 6 lessons. Of the 171 women, 122 (71%) returned the post-treatment questionnaire. Finally, 96 women (56%) completed the intervention as well as the pre- and post-measurements.
3.3. Feasibility: experiences of participants
On average, the 122 patients who returned the post-test questionnaire were satisfied with the intervention (value of 7.5 on a scale from 1 to 10). Most of the women (87%) liked the fact that they could work independently on the exercises, and almost all (94%) appreciated the support of the coaches (Table 2). Coaches received a satisfaction score of 7.8 (scale 1–10). The majority (85%) appreciated the information provided in the intervention, although a substantial part (41%) of the women indicted that they had seen some of this information before. Most of the women appreciated the exercises (77%).
Table 2.
Opinions on the internet intervention of 122 participants.
| Statement | (Fully) agree% | Neutral % | (Fully) disagree % |
|---|---|---|---|
| The intervention contained much new information | 59% | 31% | 10% |
| I appreciated the information on the internet site | 85% | 13% | 2% |
| I found the exercises useful | 77% | 18% | 5% |
| I valued the fact that feedback was provided | 94% | 4% | 2% |
| The feedback of the coach was useful | 83% | 14% | 3% |
| The feedback was motivating | 75% | 18% | 7% |
| The internet site was clearly structured | 84% | 15% | 2% |
| I was easy to find my way on the internet site | 78% | 17% | 5% |
| The site was well readable (font, color, etc) | 94% | 6% | – |
| The design of the site was nice | 85% | 15% | – |
| I liked to work independently on my sleep problems | 87% | 7% | 6% |
| The exercises were meaningful | 74% | 17% | 9% |
| The intervention has given me new insights into my sleep problems | 72% | 20% | 9% |
| The intervention taught me to cope with my sleep problems | 72% | 20% | 8% |
During the 19 qualitative interviews the following advantages of the web-based intervention were mentioned by the patients: that the intervention was especially designed for BRC patients (the recognition of not being the only one with this problem), that they could carry out the treatment in their own time and place (especially since they already had spent a lot of travel time for their cancer treatment) and that coaching was provided. The feedback was perceived as highly personalized and the women felt well understood. Also the coaching had an important role in encouraging and reminding the women in completing their homework. According to the women, the intervention could be improved by providing more in-depth information on the specific relation between BRC and insomnia, on coping with hot flushes and shoulder pain.
3.4. Within-group effects
We analysed the scores of the 171 women who were admitted to the intervention (Table 3).
Table 3.
Improvements between baseline and post-test (n = 171; intention to treat analysis).
| Mean scores (SD) |
||||
|---|---|---|---|---|
| Before | After | Effect size (95% confidence interval)a | p | |
| Insomnia severity index | 16.5 (3.6) | 9.2 (4.9) | 1.33 (1.13/1.54) | < 0.01 |
| Fatigue severity scale | 39.3 (11.1) | 35.9 (13.2) | 0.24 (0.08/0.39) | < 0.01 |
| HADS-anxiety | 7.6 (3.7) | 6.0 (3.7) | 0.44 (0.28/0.60) | < 0.01 |
| HADS-depression | 5.5 (3.7) | 4.3 (3.4) | 0.37 (0.22/0.53) | < 0.01 |
| WSAS - functioning | 16.2 (9.7) | 12.6 (10.1) | 0.30 (0.14/0.45) | < 0.01 |
Cohen's d = the difference in pre- and post-test scores of participants by the pooled standard deviation.
The mean Insomnia Severity Index (ISI) score improved significantly from 16 at pre-treatment to 8 at post-treatment, which corresponds to a large effect size of 1.33 (p < 0.01). This means that, on average, there was a shift from moderately severe clinical insomnia (score 15–21) to subthreshold insomnia (score 8–14). Daytime fatigue also improved significantly with a small effect size of 0.24 (p < 0.01). Daily functioning improved significantly as well: women were more capable of functioning (Cohen's d = 0.30; p < 0.01; Table 3). There were also significant improvements on anxiety (Cohen's d = 0.44; p < 0.01) and depression (Cohen's d = 0.37; p < 0.01).
3.5. Characteristics associated with sleep improvements
We analysed the association between sleep improvement (ISI scores) and several patient and clinical characteristics using data of the 96 patients who completed the intervention and the questionnaires (Table 4). Univariate linear regression analyses revealed three factors that were significantly associated with sleep improvement: younger age (p < 0.01), higher baseline insomnia severity (p < 0.01), and higher baseline daily fatigue (< 0.05). However, daily fatigue was no longer associated with sleep improvements in the multivariate model. BRC patients who were younger (p < 0.05) and had higher baseline insomnia levels (p < 0.01) benefited the most from the intervention. These two variables explained 28% of the total variance in ISI scores reduction.
Table 4.
Association between improvement in sleep complaints (ISI score) and other variables (linear regression analysis (a positive score indicates improvement).
| Univariate beta coefficient (95% CI) | Multivariate beta coefficient (95% CI) | |
|---|---|---|
| Demographic characteristics | ||
| Higher age | − 0.13 (− 0.23/− 0.4)⁎⁎ | − 0.09 (− 0.18/− 0.03)⁎ |
| Born in the Netherlands | − 0.16 (− 2.7/2.4) | – |
| Higher education | 0.44 (− 1.4/2.3) | – |
| Living together | 1.47 (− 0.8/3.7) | – |
| Not in a paid job | 0.44 (− 1.9/2.7) | – |
| On sick leave | 1.55 (− 0.4/3.5) | – |
| Type of treatment | ||
| Tumorectomy | − 0.8 (− 2.7/1.0) | – |
| Years between operation and admission to intervention | 0.01 (− 0.4/0.4) | – |
| Radiotherapy | 1.7 (− 0.2/3.6) | – |
| Chemotherapy | 1.49 (− 0.6/3.6) | – |
| Hormonal therapy | 0.07 (− 2.0/2.2) | – |
| with lymphe oedemia | 0.43 (− 1.4/2.3) | |
| Sleep Problems | ||
| More severe sleep problems (ISI) | 0.65 (0.42/0.89)⁎⁎ | 0.61 (0.37/0.84)⁎⁎ |
| More fatigue (FSS) | 0.09 (0.01/0.17)⁎ | Non significant |
| With sleep medication | 0.53 (− 1.29/2.35) | – |
| Sleep problems before breast cancer | 0.87 (− 0.96/2.70) | – |
| Sleep medication in history | 0.21 (− 1.79/2.21) | – |
| Other sleep treatment in history | − 0.83 (− 4.11/2.46) | – |
| Psychological symptoms and functioning | ||
| More severe HADS-anxiety | 0.19 (− 0.05/0.43) | – |
| More severe HADS-depression | 0.14 (− 0.13/0.40) | – |
| WSAS household | 0.07 (− 0.29/0.42) | – |
| WSAS work | 0.08 (− 0.21/0.38) | – |
| WSAS friendship | − 0.17 (− 0.51/0.16) | – |
| WSAS social functioning | − 0.14 (− 0.49/0.20) | – |
⁎ < 0.05; ⁎⁎ < 0.01.
4. Discussion
In this study we examined the feasibility and effects of a guided web-based CBT for insomnia in BRC patients. We demonstrated that the intervention is feasible because we had a high registration rate, a reasonable good adherence rate, and high treatment satisfaction scores. Those who completed the intervention and returned the post-test questionnaire (response rate 56%) improved on average 8 points on the Insomnia Severity Index which corresponds to a significant and large effect size (ITT d = 1.33). There were also significant improvements on all the secondary outcomes (fatigue, daytime functioning, anxiety and depression) although these effects were in the small to moderate range (between d = 0.24 and d = 0.44). Finally, we showed that younger women and women with more severe insomnia at baseline improved most.
The adherence rate of 59% is reasonably high, but lower than the adherence rate of 73% for the same internet intervention for insomnia in a non-cancer population (van Straten et al., 2013). However, the treatment satisfaction scores were in the same range (7.5 vs 7.3). These findings suggest that completion of the insomnia intervention is more difficult for BRC patients. Possibly, we should adjust our treatment even more to the specific needs of BRC patients as was also suggested in the qualitative interviews.
The results of our study are in line with findings published previously in randomized controlled trials on self-administered treatment for insomnia in BRC patients (Savard et al., 2014, Ritterband et al., 2012). First, our patients seemed to be comparable with respect to demographical characteristics as well as insomnia severity at baseline. Second our within effect size for insomnia severity (ITT d = 1.33) is in the same range as obtained in these two studies (d = 2.24 and d = 1.29, respectively).
Most of the women that were referred by routine care procedures were higher educated compared to women that were self-referred. Possibly, professionals assume that higher education is a necessary condition for participating in an internet intervention.
Our internet intervention was offered with coaching from a professional. This was highly appreciated by the patients. The women felt well understood and the coaching helped her to adhere to the treatment. In general, Internet interventions demonstrate higher effect sizes for guided interventions than for non-guided interventions (Spek et al., 2007, Lancee et al., 2013). Despite the patients' appreciation of the support provided by the coaches, our effect size was not higher than in the other two studies which offered the interventions without any personal guidance. There might be several explanations for this. First, our study is not a RCT. It might be possible that our intervention would yield higher between group effect sizes in a RCT than the between group effect sizes in the other 2 studies. Secondly, our coaching might not have been properly conducted. This seems unlikely however since we used similar types of coaches and similar training procedures than other successful internet based studies we performed. Thirdly, it may be that the automated feedback in the other two interventions was as effective as the feedback of a professional. Further research into the additional effects of personal and automated guidance is warranted.
We tailored our I-Sleep intervention for breast cancer patients by adding psycho-education about breast cancer and insomnia, about hot flashes and insomnia, and about pain and insomnia. Furthermore, the case examples were based on real stories of BRC patients undergoing insomnia treatment. We assumed that all of this would lead to lower drop-out rates, which in turn would lead to greater effects. However, there is still little empirical data on the impact of tailoring of treatments to specific target groups and their effectiveness and most clinical studies conducted in cancer patients have not importantly adapted CBT-I to this specific population. Although our participants appreciated these adjustments, these adjustments may not be a necessary condition for improving sleep. On the other hand, some of the participants mentioned that they would have liked the intervention to be even more specific for BRC patients. This raises the question as to whether and to what extent we have to tailor web-based interventions for insomnia to specific subpopulations. Hypothetically the adjustments are mainly important in order to make the intervention more attractive for different subpopulations. In a systematic review by Schubart et al. (2011) on the factors that enhance user engagement of internet interventions, the importance of an individualized program is stated. Therefore, the personally tailored advice in the feedback of the coaches may be of more importance for adherence than the tailoring of the intervention itself.
Our results showed that younger patients with more severe insomnia benefited the most from the intervention. Nevertheless, the fact that 59% of the BRC patients who started the intervention also completed the intervention (and put in considerable effort in completing the exercises) indicates that the intervention was appreciated by a majority of BRC patients.
A limitation of this study was that the insomnia diagnoses were not assessed by clinical interviews. Hence, some patients may not have suffered from an insomnia disorder or they may have suffered from another sleep disorder (e.g. sleep apnea). According to the ISI, about 70% of our sample suffered from moderate to severe clinical insomnia. The lack of a control group is an important limitation as well as it is unclear whether the effects obtained are truly due to the treatment or to some non-specific factors (e.g., passage of time). However, the effect sizes obtained were of a similar magnitude as previous studies.
The conclusion of this study is that a guided web-based CBT intervention is a valuable addition in supportive cancer care, especially for younger patients and those with more severe insomnia.
Declaration of interest
None.
Authors' contributions
AS obtained funding for this study. ED coordinated the recruitment of health care organisations, patients and the data collection. AS and ED were responsible for the overall design of the intervention and supervision of the coaches. AS analysed the data. ED wrote the manuscript. All authors read, contributed and approved the final manuscript.
Acknowledgments
We thank Jitske Bongers for her efforts on the recruitment of patients and the support on the data collection. Also, we are grateful for the financial support we received from Fund Pink Ribbon (2012.PS13.C149) to develop the intervention and to carry out this study.
References
- American Psychiatric Association . American Psychiatric Association; Washington, D.C: 2013. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. [Google Scholar]
- Benca R.M. Diagnosis and treatment of chronic insomnia. Psychiatr. Serv. 2005;56(3):332–343. doi: 10.1176/appi.ps.56.3.332. [DOI] [PubMed] [Google Scholar]
- Berger A.M., Kuhn B.R., Farr L.A., Lynch J.C., Agrawal S., Chamberlain J., Von Essen S.G. Behavioral therapy intervention trial to improve sleep quality and cancer-related fatigue. Psychooncology. 2009;18(6):634–646. doi: 10.1002/pon.1438. [DOI] [PubMed] [Google Scholar]
- Buscemi N., Vandermeer B., Friesen C., Bialy L., Tubman M., Ospina M., Klassen T.P., Witmans M. The efficacy and safety of drug treatments for chronic insomnia in adults: a meta-analysis of RCTs. J. Gen. Intern. Med. 2007;22(9):1335–1350. doi: 10.1007/s11606-007-0251-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. second ed. New York; Lawrence Erlbaum Associates: 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- Edinger J.D., Wohlgemuth W.K. The significance and management of persistent primary insomnia: the past, present and future of behavioral insomnia therapies. Sleep Med. Rev. 1999;3(2):101–118. doi: 10.1016/s1087-0792(99)90018-7. [DOI] [PubMed] [Google Scholar]
- Espie C.A., Fleming L., Cassidy J., Samuel L., Taylor L.M., White C.A., Paul J. Randomized controlled clinical effectiveness trial of cognitive behavior therapy compared with treatment as usual for persistent insomnia in patients with cancer. J. Clin. Oncol. 2008;26(28):4651–4658. doi: 10.1200/JCO.2007.13.9006. [DOI] [PubMed] [Google Scholar]
- Fiorentino L., Ancoli-Israel S. Insomnia and its treatment in women with breast cancer. Sleep Med. Rev. 2006;10(6):419–429. doi: 10.1016/j.smrv.2006.03.005. (Dec) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jernelöv S., Lekander M., Blom K., Rydh S., Ljótsson B., Axelsson J., Kaldo V. Efficacy of a behavioral self-help treatment with or without therapist guidance for co-morbid and primary insomnia-a randomized controlled trial. BMC Psychiatry. 2012;12(1):5. doi: 10.1186/1471-244X-12-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knuistingh Neven A., Lucassen P.L.B.J., Bonsema K., Teunissen H., Verduin M.M., Bouma (2005). NHG-standaard Slaapproblemen en slaapmiddelen (eerste herziening). Huisarts Wet. 48(8):402-15.
- Krupp L.B., LaRocca N.G., Muir-Nash J., Steinberg A.D. The fatigue severity scale: application to patients with multiple sclerosis and systemic lupus erythematosus. Arch. Neurol. 1989;46(10):1121–1123. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- Lancee J., van den Bout J., Sorbi M.J., van Straten A. Motivational support provided via email improves the effectiveness of internet-delivered self-help treatment for insomnia: a randomized trial. Behav. Res. Ther. 2013;51(12):797–805. doi: 10.1016/j.brat.2013.09.004. (Dec) [DOI] [PubMed] [Google Scholar]
- Lipsey M.W. SAGE Publications Inc.; Newbury Park, CA: 1990. Design Sensitivity. Statistical Power for Experimental Research. [Google Scholar]
- Lipsey M.W., Wilson D.B. The efficacy of psychological, educational, and behavioral treatment. Confirmation from meta-analysis. Am. Psychol. 1993;48:1181–1209. doi: 10.1037//0003-066x.48.12.1181. [DOI] [PubMed] [Google Scholar]
- Marks I.M. John Wright; Bristol: 1986. Behavioural Psychotherapy. [Google Scholar]
- Matthews E.E., Berger A.M., Schmiege S.J., Cook P.F., McCarthy M.S., Moore C.M., Aloia M.S. Oncology Nursing Forum. Vol. 41, No. 3. Oncology Nursing Society; 2014. Cognitive behavioral therapy for insomnia outcomes in women after primary breast cancer treatment: a randomized, controlled trial; pp. 241–253. [DOI] [PubMed] [Google Scholar]
- Morin C.M. Guilford Press; New York: 1993. Insomnia: Psychological Assessment and Management. [Google Scholar]
- Morin C.M., Bootzin R.R., Buysse D.J., Edinger J.D., Espie C.A., Lichstein K.L. Psychological and behavioral treatment of insomnia: update of the recent evidence (1998–2004) Sleep-New York Westchester. 2006;29(11):1398. doi: 10.1093/sleep/29.11.1398. [DOI] [PubMed] [Google Scholar]
- Neylan T.C. Time to disseminate cognitive behavioral treatment of insomnia: comment on “efficacy of brief behavioral treatment for chronic insomnia in older adults”. Arch. Intern. Med. 2011;171(10):895–896. doi: 10.1001/archinternmed.2010.526. [DOI] [PubMed] [Google Scholar]
- Ritterband L.M., Bailey E.T., Thorndike F.P., Lord H.R., Farrell-Carnahan L., Baum L.D. Initial evaluation of an internet intervention to improve the sleep of cancer survivors with insomnia. Psychooncology. 2012;21(7):695–705. doi: 10.1002/pon.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savard J., Simard S., Ivers H., Morin C.M. Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part I: sleep and psychological effects. Am. Soc. Clin. Oncol. 2005;23(25) doi: 10.1200/JCO.2005.09.548. (9 1, 6097-106y) [DOI] [PubMed] [Google Scholar]
- Savard M.H., Savard J., Simard S., Ivers H. Empirical validation of the insomnia severity index in cancer patients. Psychooncology. 2005;14:429–441. doi: 10.1002/pon.860. [DOI] [PubMed] [Google Scholar]
- Savard J., Ivers H., Villa J., Caplette-Gingras A., Morin C.M. Natural course of insomnia comorbid with cancer: an 18-month longitudinal study. J. Clin. Oncol. 2011;29:3580–3586. doi: 10.1200/JCO.2010.33.2247. [DOI] [PubMed] [Google Scholar]
- Savard J., Villa J., Simard S., Ivers H., Morin C.M. Feasibility of a self-help treatment for insomnia comorbid with cancer. Psychooncology. 2011;20(9):1013–1019. doi: 10.1002/pon.1818. [DOI] [PubMed] [Google Scholar]
- Savard J., Ivers H., Savard M.-H., Morin C.M. Is a video-based cognitive-behavioral therapy for insomnia as efficacious as a professionally-administered treatment in breast cancer? Results of a randomized controlled trial. Sleep. 2014;37:1305–1314. doi: 10.5665/sleep.3918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubart J.R., Stuckey L., Ganeshamoorty A.B.S., Sciamannan Chronic health conditions and internet behavioral interventions: a review of factors to enhance user engagement CIN: computers, informatics. Nursing. 2011;29(2):81–92. doi: 10.1097/NCN.0b013e3182065eed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seyffert M., Lagisetty P., Landgraf J., Chopra V., Pfeiffer P.N. Internet-delivered cognitive behavioral therapy to treat insomnia: a systematic review and meta-analysis. PLoS One. 2016;11(2) doi: 10.1371/journal.pone.0149139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spek V., Cuijpers P., Nyklícek I., Riper H., Keyzer J., Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol. Med. 2007;37(3):319–328. doi: 10.1017/S0033291706008944. (Mar) [DOI] [PubMed] [Google Scholar]
- van Straten A., Cuijpers P. Selfhelp therapy for insomnia: a meta-analysis. Sleep Med. Rev. 2009;13:61–71. doi: 10.1016/j.smrv.2008.04.006. [DOI] [PubMed] [Google Scholar]
- van Straten A., Emmelkamp J., de Wit J., Lancee J., Andersson G., van Someren E.J.W., Cuijpers P. Guided internet-delivered cognitive behavioural treatment for insomnia: a randomized trial. Psychol. Med. 2013 doi: 10.1017/S0033291713002249. (Available on CJO 2013) [DOI] [PubMed] [Google Scholar]
- Thorndike F.P., Ritterband L.M., Saylor D.K., Magee J.C., Gonder-Frederick L.A., Morin C.M. Validation of the insomnia severity index as a web-based measure. Behav. Sleep Med. 2011;9(4):216–223. doi: 10.1080/15402002.2011.606766. [DOI] [PubMed] [Google Scholar]
- Zachariae R., Lyby M.S., Ritterband L.M., O'Toole M.S. Efficacy of internet-delivered cognitive-behavioral therapy for insomnia - A systematic review and meta-analysis of randomized controlled trials. Sleep Med. Rev. 2016;30:1–10. doi: 10.1016/j.smrv.2015.10.004. Epub 2015 Oct 24. Review. [DOI] [PubMed] [Google Scholar]
- Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]