Abstract
Chronic pain is a major health problem and behavioral based treatments have been shown to be effective. However, the availability of these kinds of treatments is scarce and internet-based treatments have been shown to be promising in this area. The objective of the present systematic review is to evaluate internet-based interventions for persons with chronic pain. The specific aims are to do an updated review with a broad inclusion of different chronic pain diagnoses and to assess disability and pain and also measures of catastrophizing, depression and anxiety. A systematic search identified 891 studies and 22 trials were selected as eligible for review. Two of the selected trials included children/youth and five included individuals with chronic headache and/or migraine. The most frequently measured domain reflected in the primary outcomes was interference/disability, followed by catastrophizing. Result across the studies showed a number of beneficial effects. Twelve trials reported significant effects on disability/interference outcomes and pain intensity. Positive effects were also found on psychological variable such as catastrophizing, depression and anxiety. Several studies (n = 12) were assessed to have an unclear level of risk bias. The attrition levels ranged from 4% to 54% where the headache trials had the highest drop-out levels. However, findings suggest that internet-based treatments based on cognitive behavioural therapy (CBT) are efficacious measured with different outcome variables. Results are in line with trials in clinical settings. Meta-analytic statistics were calculated for interference/disability, pain intensity, catastrophizing and mood ratings. Results showed that the effect size for interference/disability was Hedge's g = − 0.39, for pain intensity Hedge's g = − 0.33, for catastrophizing Hedge's g = − 0.49 and for mood variables (depression) Hedge's g = − 0.26.
Keywords: Chronic pain, Internet, Cognitive behavioral therapy, Headache, Pediatric pain, Self-help
Highlights
-
•
Chronic pain is a depleting health problem, however the availability of effective treatments are scarce.
-
•
Internet based interventions have the potential to overcome several practical barriers
-
•
The results of this systematic review are in line with previous reviews with small to moderate overall effects.
-
•
The present review has a broader inclusion of studies with studies on headache and children/youth.
-
•
Meta-analytic statistics were calculated for disability/interference, catastrophizing, pain intensity and mood variables.
1. Introduction
Chronic pain is a major health problem with a large impact on the emotional, physical and social functioning of persons as well as society. An estimation of 10–30% adults suffer from chronic pain (Reid et al., 2011). Empirical support has been found for cognitive behavioural therapy (CBT) and acceptance and commitment therapy (ACT), which is a form of CBT, for a variety of chronic pain problems compared to wait-list controls and alternative active treatments (Eccleston et al., 2013, Hann and McCracken, 2014). Unfortunately, the availability of CBT and ACT for chronic pain is poor for many individuals suffering from chronic pain. It is essential to increase the accessibility of evidence-based treatments such as CBT to chronic pain suffers. For the last decade researchers across the world have investigated the power of the internet to create internet-based prevention and treatment programmes (Andersson, 2014, Andersson, 2009). Different methods are used to administer the interventions and to encourage the participants. Guided internet-based programmes provide instructions for behavioural change to the participants while being monitored by a therapist. In contrast, unguided internet-based interventions are websites that are fully automated. Furthermore, there are a great number of apps (downloadable programmes designed to run on the smart phone) relating to pain, but there is no regulatory body evaluating and approving the release of health-care apps (Rosser and Eccleston, 2011).
Several systematic reviews have been performed the last five years, more specific 2010, 2012 and 2014, indicating the rapid development in this area. In a review conducted by Macea et al. (2010), 11 studies were assessed to quantify the efficacy of internet-based CBT (iCBT) for chronic pain. The studies included were randomized controlled trials. The main outcome used in the meta-analysis was pain, and results showed small reductions in pain compared to waiting-list control groups. High dropout rates were reported with an average of 26%, which is higher than in traditional CBT interventions (14%). In another review (Bender et al., 2011) 17 articles that evaluated iCBT for chronic pain were included. The total sample analysed consisted of 2503 individuals with different chronic pain syndromes including headache, back pain, musculoskeletal pain, abdominal pain and fibromyalgia. Results showed that iCBT was associated with improvements in pain, activity limitation, and costs associated with treatment. The effects on depression and anxiety were less consistent. A more recent review included fifteen studies with a total sample of 2012 adults with chronic pain. The researchers found positive effects regarding pain intensity, disability, depression and anxiety at post-treatment. It was found that there is insufficient evidence to make conclusions regarding the efficacy of internet-based psychological treatments in participants with headache conditions (Eccleston et al., 2014).
The rapid increase of internet-based studies for chronic pain for adults and children/youth and the technical development and increasing trials for different pain diagnoses including headache motivate a review with a broader perspective on internet-based treatment. The present review aims to do an updated review with a broad inclusion of different chronic pain diagnoses and to include studies with children/youth with chronic pain. The more specific aims are to assess disability and pain and also outcomes of catastrophizing, depression and anxiety are of interest. Furthermore, risk of bias was assessed for the different trials and meta-analytic statistics were calculated for the different outcome variables.
2. Methods
2.1. Identification of studies
This review includes published journal articles describing randomized controlled trials of internet-based CBT for chronic pain. Studies were identified using different sources. Existing systematic reviews in the field were used (Bender et al., 2011, Eccleston et al., 2014, Macea et al., 2010). Furthermore, a search of MEDLINE, PsychINFO, CINAHL and The Cochrane Library was conducted (1990 to March 2015). All searches were carried out on the 23rd of February and 5th of March 2015. Unpublished literature was not sought for the review.
The titles, abstracts and keyword were searched for the following terms: cognitive, cognitive behavioral therapy, CBT, acceptance, ACT, acceptance and commitment therapy, combined with chronic pain, fibromyalgia, FM, persistent pain, back pain, CLBP, musculoskeletal pain, rheumatoid arthritis, chronic headache, headache, and persistent headache and further combined with internet, online, self-help, web-based and also combined with control trial, RCT, and control trial. The aim was to capture efficiently the maximum number of published trials in the field.
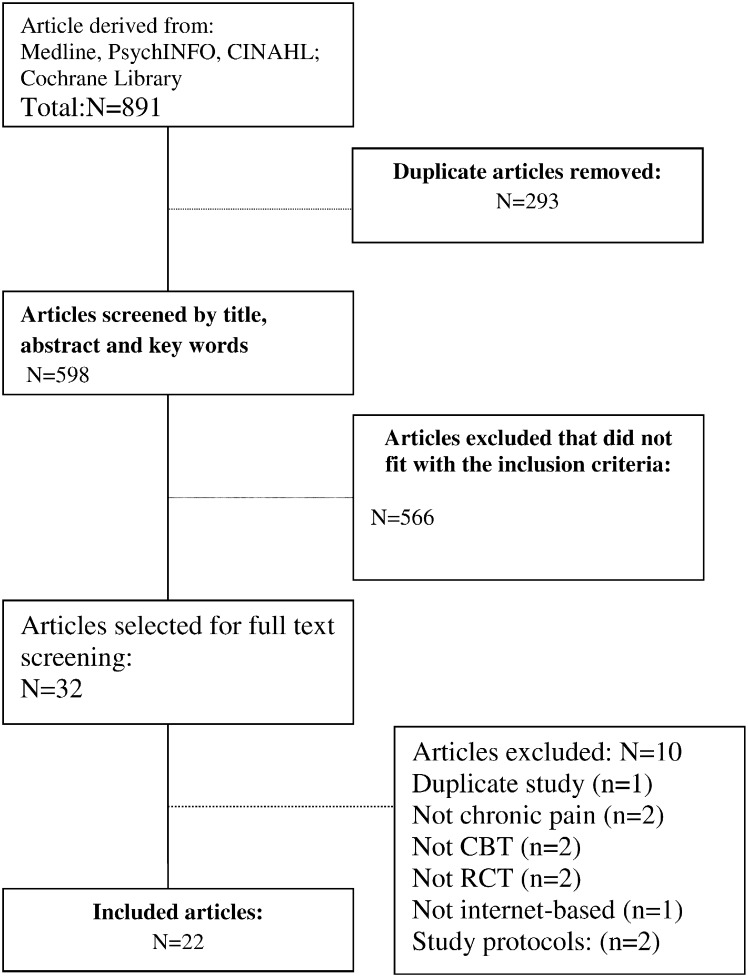
2.2. Study selection
Study selection was carried out by the first author and agreed by the other authors. Fig. 1 shows a flow diagram of the study selection process for the review. Inclusion criteria adopted was: 1) randomized controlled trial; 2) article written in English; 3) web-based or mobile phone intervention for the treatment of chronic pain of different types; 4) measurement of disability level and/or pain; 6) treatments that were based on CBT- or ACT principles; and 7) a comparison between an intervention group and a waiting-list control or other treatment. The search yielded a total of 891 articles. When the duplicated articles and the ones that did not fulfill the inclusion criteria were removed, 32 remained. After the full text selection ten articles were excluded since they did not fulfill the inclusion criteria; two were not randomized controlled trials (Kristjánsdóttir et al., 2011, Ljótsson et al., 2014); two studies included samples with pain but not chronic pain (Del Pozo-Cruz et al., 2012, Irvine et al., 2015); two trials were not CBT-based interventions but peer support (Lorig et al., 2008, Lorig et al., 2002); on study did not include a web-based intervention only telephone administered behavioral treatment (Cottrell et al., 2007); one trial (Fales et al., 2014) included a sample reported in an study already included (Palermo et al., 2009) and two were study protocols (Hayes et al., 2014, Lin et al., 2014) leaving 22 articles that were included. For further information see Fig. 1.
Fig. 1.
Flow chart.
2.3. Data extraction
The first and last authors reviewed independently the full text of articles meeting the eligibility criteria. Data were extracted by the first author and reviewed and agreed by the last one. Data extracted included details of participants' pain condition, sample size, design characteristics, outcome measures, information about the intervention, mean age of participants, educational level of the participants, pain duration, percentage of women, method of treatment delivery, period of treatment, the type of control condition used for comparison, the participants' attrition rate and the results of the outcomes. Primary and secondary outcome information was extracted.
2.4. Data management
The time point for the collection of data was direct after the intervention. Furthermore, the studies' methodological quality was assessed by the reviewers using an adapted Cochrane Collaboration tool for the risk of bias within randomized trials (Higgins et al., 2011).
We relied primarily on guidelines for application of the Cochrane Collaboration tool to assess five areas of potential bias: selection bias, detection bias, attrition bias, reporting bias and other sources of bias. Performance bias was removed since it is difficult to conceal CBT-based treatment from the participants or the therapist. The different areas of potential bias are described in the Results section.
We used the program Comprehensive Meta-Analysis (version 2.2.021; CMA) to calculate pooled mean effect sizes using random effects models. We also calculated the I2-statistic as an indicator of heterogeneity in percentages (with 0% indicating no observed heterogeneity, 25% low, 50% moderate, and 75% high heterogeneity). Publication bias was tested by inspecting funnel plots and Egger's test (Egger et al., 1997), using the procedures implemented in CMA.
3. Results
3.1. Study characteristics
Table 1 shows the characteristics of the included studies. A total of 2354 persons with chronic pain were randomized to internet-based interventions across the 22 trials. The sample sizes ranged from 44 to 305. Most trials were conducted in USA (n = 9, 40.9%) and Sweden (n = 9, 40.9%), followed by the Netherlands (n = 2, 9.0%), Australia (n = 1, 4.5%) and Norway (n = 1, 4.5%). Two of the included studies involved children/youth with chronic pain (Hicks et al., 2006, Palermo et al., 2009). The mean age across studies ranged from 36.7 to 65.8 years old, excluding the children/youth trials. The majority of the participants were females; the percentage ranged from 52.1–95%. One study only included women (Kristjánsdóttir et al., 2013a). In the trials including adults the education level was defined in different ways but in 54.5% (n = 12) of the studies, the majority of the participants had some level of higher education level. In the articles where the education level was lower (n = 3) the recruitment was from clinical settings (Buhrman et al., 2013a, Buhrman et al., 2013b, de Boer et al., 2014). In one study the participants with university education were as many as those with non-university degree (Dear et al., 2013). Four trials lacked information about education levels (Andersson et al., 2003, Brattberg, 2006, Devineni and Blanchard, 2005, Ström et al., 2000).
Table 1.
Study characteristics.
| Study/country | Health condition | Women (%) | Age group (age range) | Study groups | N recruitment method | Control condition | Interventiona | Guidance | Period of treatment | Education level | Pain duration |
|---|---|---|---|---|---|---|---|---|---|---|---|
|
Andersson et al. (2003) Sweden |
Headache | 81.8% (n = 36) | 40.3 (range: 18–59) | Adults | 44 (advertisement) | Web-based treatment with telephone support or web-based only | CBT | Yes (psychologists) | 6 weeks | No information | Headache duration: 05–1 year: n = 2 1–5 years: n = 14 6–10: n = 5 > 10: n = 23 |
|
Berman et al. (2009) USA |
Mixed chronic pain conditions | 87.2% females in total sample (n = 78) 87,8% in intervention group (n = 41) and 86,5% in WLC (n = 37) |
65,8 years (range: 55–91) | Older adults | 78 (through public service) | Intervention or WLC | CBT and mind–body intervention, 6 weeks. | Yes (research assistant) | 6 weeks | 38.5% college graduation, 29.5 some college, 23.1% graduated school. | No information |
|
Brattberg (2006, 2007), Sweden |
Chronic pain and burnout | 89.1% (n = 49) |
Treatment group: 47 (sd = 8; range 32–62 years) WLC: 47 (sd = 6; range 34–61) |
Adults | 55 (advertisement) | Intervention or WLC | CBT | Yes (researcher and an expert patient) | 20 weeks | No information | No information |
|
Bromberg et al. (2012) USA |
Chronic migraine | 89% (n = 165) females | Mean age = 42.6 (sd = 11.5) (range 20–66) | Adults | 189 (advertisement) | Intervention or TAU | CBT | NO (only reminders) | 4 weeks | < 11th grade: 0.56% (n = 1) High school or general education diploma: 17.22% (n = 31) 2 years of college/AA degree/technical school training: 22.22% (n = 40) College graduate (BA or BS): 33.89% (n = 61) Master's degree: 20% (n = 36) Doctoral/medical/law degree: 11% (n = 6.11) |
Average baseline headache duration: 2.47 h per day (sd = 1.44) |
|
Buhrman et al. (2013a) Sweden |
Mixed chronic pain conditions | 72.2% (52) | 40.1 (sd = 8.94) | Adults | 72 (clinical setting) | Intervention or active control group (moderated online discussion forum) | CBT | Yes (graduate students) | 8 weeks | University education: 33.3% (n = 24); upper secondary school: 54.1% (n = 39) and nine-year compulsory school: 12.5% (n = 9) | Pain duration in years M (SD):6.2 (2.07) |
|
Buhrman et al. (2013b) Sweden |
Mixed chronic pain condition | 59.2%(45) | 49.1 (sd = 10.34) | Adults | 76 (clinical setting) | Intervention or active control group (moderated online discussion forum) | ACT | Yes (graduate students) | 7 weeks | University education: 43.4% (n = 33); upper secondary school: 47.4% (n = 36) and nine-year compulsory school: 9.2% (n = 7) | Pain duration in years M (SD):15.3 (11.65) |
|
Buhrman et al. (2015) Sweden |
Mixed chronic pain conditions | 85%(44) | 50.69 (sd = 12.72) | Adults | 52 (clinical setting) | Intervention or active control group (moderated online discussion forum) | CBT | Yes (graduate students) | 8 weeks | Nine-Year compulsory school: 19% (n = 10) Upper secondary school: 23% (n = 12) University education < 2 years: 6% (n = 3) University education > 2 years: 52% (27) |
3 months-5 year: 33% (n = 17) 5–10 years: 13% (n = 7) 10 years and more: 54% (n = 28) |
|
Buhrman et al. (2004) Sweden |
Back pain | 62.5% (35) | 44.6 (sd = 10.4) | Adults | 56 (advertisement) | Intervention or WLC | CBT with some physical components | Yes, (graduate students) with weekly structured telephone calls | 6 weeks | University education: 57.1% (n = 32); upper secondary school: 25% (n = 14) and nine-year compulsory school: 17.9% (n = 10) | Pain duration in years M (SD):10.1 (9.2) |
|
Buhrman et al. (2011) Sweden |
Back pain | 68.5% (37) | 43.2 (sd = 9.8) | Adults | 54 (advertisement) | Intervention or WLC | CBT | Yes (clinical psychologists), contacted once by telephone | 8 weeks | University education: 53.7% (n = 29); upper secondary school: 40.7% (n = 22)and nine-year compulsory school: 5.6% (n = 3) | Pain duration in years M (SD):12.1 (8.5) |
|
Carpenter et al. (2012) USA |
Chronic lower back pain | 83% | 42.5 (21–74) (sd = 10.3) | Adults | 141 (advertisement) | Intervention or WLC | CBT | No (only reminders) | 3 weeks | 54% no more than 2 years of college or technical school | 6-516 months (M = 103.7, SD = 94.1) |
|
Chiauzzi et al. (2010) USA |
Back pain | 67% | 46.14 (sd = 11.99; range = 18–79)) | Adults | 209 (through advertisement through professional, patient contacts the American chronic pain association website) | Intervention or active control condition that received text-based material | CBT | No | 4 weeks | < 11th grade: 2(1.01) HS1 or GED2: 50 (25.25) Partial college/AA:63 (31.82) BA or BS: 55 (27.78) Master's: 26 (13.13) PhD/MD: 2 (1.01) 1 = High school 2 = General Educational Development Diploma |
No information |
|
de Boer et al. (2014) The Netherlands |
Mixed chronic pain | Females n = 32 (64%) (internet n = 15, 68,2%; face-to-face n = 17, 60.7%) | 52.1 (sd = 11.2) | Adults | Randomized n = 72, started the program n = 50 (clinical setting) | Internet intervention vs face-to-face group intervention | CBT 7 weeks + 1 week two months after the last module. | Yes (trained psychologist). | 7 weeks + 1 week | Tertiary education n = 10, 20%; higher secondary education n = 20, 40%; lower secondary education n = 18, 36% and primary education n = 2, 7.1%. | Mean (sd): 102 (98.4) in months. Range 8–365. Internet: 1182 (121.7) Range: 8–365 Group: 90.0 (77.1) Range 12–300- |
|
Dear et al. (2013) Australia |
Mixed chronic pain conditions | 85% (n = 53) | 49 (20–91) | Adults | 63 (advertisement) | Intervention or WLC | CBT | Yes, (clinical psychologist with postgraduate qualification) | 8 weeks | University education 40% (n = 25) Certificate/diploma/other 40% (n = 25) |
M = 7.36(sd = 8.10) |
|
Devineni and Blanchard (2005) USA |
Chronic headache | 79.1% (= 110) | Treatment: 43.6 (sd = 12.0); wlc: 41.0 (sd = 11.8); dropout 39.2 (sd = 14.7) | Adults | 139 (through internet websites) | Internet-based treatment or symptom monitoring waitlist control | CBT | Yes (researchers) | 4 weeks | No information | No information |
|
Hedborg and Muhr (2011) Sweden |
Chronic migraine | 69.9% females | Group intervention + handmassage: mean = 49.4 (range 22–65); group intervention without handmassage mean = 44.8 (23–61) and control group mean = 49.0 (27–65) | Adults | 83 (advertisement) | Intervention MBT without hand-massage, intervention with hand-massage and control group 3 arms |
CBT with multidisciplinary components | No | 11 months for the intervention groups, and 8 months for the control group. | College/university/post-graduate studies: Intervention group with hand massage: 68%; intervention group without hand massage: 66.7% and control group: 48.1% Upper secondary school: 24,25,40.7% respectively. Nine year compulsory school/elementary 8, 8.3, 11,1% respectively. | Migraine frequency during baseline recording: Group with hand massage: 10.1 (range 1–27), tension-type headache 32, Aura 48. Intervention group without hand-massage: mean = 13.9 (range 1–33); tension type headache: 41.7; aura 29.2. Control group: migraine mean: 10.0 (range 2–33); tension type: 37; aura: 51.9 |
|
Hicks et al. (2006) USA |
Pediatric recurrent pain | 63.8% (n = 30) | 11.7 (sd = 2.1) | Youth (9–16 years old) | 47 | Intervention (internet-based treatment) or standard medical care waitlist | CBT | Yes (researchers) | 7 weeks | - | Median duration of pain problem in years (minimum/maximum): 3.0 (0.25/11) |
|
Kristjánsdóttir et al. (2013a) Norway |
Women with chronic widespread pain (CWP) | 100% females | Intervention group (n = 69) 44.59 (sd = 11.13) and the control group n = 65 43.80 (sd = 11.20) |
Women adults | 135 (clinical setting) | Intervention or WLC | CBT/ACT smartphone 4 weeks | Yes (therapist) | 4 weeks | 43.5% (n = 30) in the intervention group college/university and 34.8% (n = 23) in the control group. Total 39.26% (n = 53). High school 36.30% (n = 49). Elementary 15.56% (n = 21). |
In the treatment group M = 13.133 (sd = 8.78) and in the control group M = 15.47 (sd = 12.09) |
|
Palermo et al. (2009) USA |
Mixed chronic pain conditions |
72.9% | 14.8 (sd = 2.0) | Children and adolescents and their parent. | 48 | Intervention or WLC | CBT and social learning | Yes (phd doctoral student) | 8 weeks for children and parents. | Parents' educational level 40.4% vocational school or some college; 34.0% college degree. | No information |
|
Ruehlman et al. (2012) USA |
Mixed chronic pain conditions | 64.3% (n = 196) |
44.93 (range: 19–78) | Adults | 305 (information on pain sites) | Online self-management program or wait list control with TAU | CBT | No | 6 weeks | 10.5% high school degree; 70.8% reported attending at least some college, 18.4% had advance degrees | 89.5% reported having pain for more than 2 years |
|
Ström et al. (2000) Sweden |
Recurrent headache | 67.6% (n = 69) | 36.7 (range: 19–62) | Adults | 102 (advertisement) | Intervention or WLC | CBT | Yes (graduate students) | 6 weeks | No information | Headache duration: 05-1 year: n = 5 1–5 years: n = 41 > 5: n = 52 |
|
Trompetter et al. (2015) The Netherlands |
Mixed chronic pain conditions | 75.3–76.8% on different conditions | 52.9 (ACT), 52.3 (EW)& 53.2 (WLC) (sd = 13.3, 11.8; 120) | Adults | 238 (advertisement) | 3-conditions: Intervention; control condition expressive writing or WLC | ACT | Yes (graduate psychology students) | 9 modules which could be worked through in 9–12 weeks. | High level of education 45.1% (ACT); 44.3 (EW) & 42.9 (WLC).Low 19.5 (ACT); 19.0 (EW); 22.1 (WLC). | Duration > 5 years: 58.5–69.66% |
|
Williams et al. (2010) USA |
Fibromyalgia | 95% females | 50 years (sd = 11.5) | Adults | 118 (clinical setting) |
Standard care or experimental intervention consisted of standard care plus web-enhanced behavioral self-management program (WEB-SM) | CBT | No | 6 months | 40% college training, 30% college degree, 12% processing education extending beyond college graduation and 18% being high school graduates or less. | The average participant had held a diagnosis of FM for 9.4 year (sd = 6.5) |
CBT = cognitive behavior therapy, ACT = acceptance and commitment therapy.
3.2. Health conditions
Several studies (n = 9, 40.9%) targeted people with mixed chronic pain conditions (Berman et al., 2009, Brattberg, 2006, Buhrman et al., 2015, Buhrman et al., 2013a, Buhrman et al., 2013b, de Boer et al., 2014, Dear et al., 2013, Ruehlman et al., 2012, Trompetter et al., 2015) and two (9%) studies specifically included persons with fibromyalgia/widespread pain (Kristjánsdóttir et al., 2013a, Williams et al., 2010). The two studies (9%) that included children and youth included mixed chronic pain problems (Hicks et al., 2006, Palermo et al., 2009). Four trials involved individuals with back pain (Buhrman et al., 2004, Buhrman et al., 2011, Carpenter et al., 2012, Chiauzzi et al., 2010). Five studies (22.7%) targeted persons with chronic headache and/or migraine (Andersson et al., 2003, Bromberg et al., 2012, Devineni and Blanchard, 2005, Hedborg and Muhr, 2011, Ström et al., 2000).
3.3. Interventions and control conditions
As seen in Table 1 all studies evaluated behavioral-based treatments. Most of the studies (n = 19, 86.36%) stated that the intervention was CBT-based (Andersson et al., 2003, Berman et al., 2009, Brattberg, 2006, Bromberg et al., 2012, Buhrman et al., 2011, Buhrman et al., 2015, Buhrman et al., 2004, Buhrman et al., 2013a, Carpenter et al., 2012, Chiauzzi et al., 2010, de Boer et al., 2014, Dear et al., 2013, Devineni and Blanchard, 2005, Hedborg and Muhr, 2011, Hicks et al., 2006, Palermo et al., 2009, Ruehlman et al., 2012, Ström et al., 2000, Williams et al., 2010) while two were ACT interventions (Buhrman et al., 2013b, Trompetter et al., 2015). One intervention (Kristjánsdóttir et al., 2013a) used an intervention based on both CBT and ACT. However, several interventions described ACT-influenced techniques such as mindfulness (Buhrman et al., 2015, Buhrman et al., 2011, Carpenter et al., 2012). Four interventions (Buhrman et al., 2004, Buhrman et al., 2013a, Hedborg and Muhr, 2011, Kristjánsdóttir et al., 2013a) also included multidisciplinary components. The intervention period ranged from three weeks (Carpenter et al., 2012) to 11 months (Hedborg and Muhr, 2011).
Control conditions varied; 14 (63.6%) trials used wait-list control conditions (Berman et al., 2009, Brattberg, 2006, Buhrman et al., 2004, Buhrman et al., 2011, Carpenter et al., 2012, Dear et al., 2013, Devineni and Blanchard, 2005, Hayes et al., 2014, Hicks et al., 2006, Ström et al., 2000) or active control conditions (Buhrman et al., 2015, Buhrman et al., 2013a, Buhrman et al., 2013b, Chiauzzi et al., 2010). Three studies compared the experimental conditions with treatment as usual (Bromberg et al., 2012, Ruehlman et al., 2012, Williams et al., 2010). One study used a face-to-face control condition (de Boer et al., 2014), and two trials (Andersson et al., 2003, Kristjánsdóttir et al., 2013a) compared an internet-based intervention with telephone/smartphone support to an only internet-based treatment. In addition, one trial for individuals with chronic headache used three conditions; one consisted of an internet-based intervention, one of an internet-intervention and hand massage and the third condition was a wait-list-control (Hedborg and Muhr, 2011). Another study for adults with mixed chronic pain diagnoses also allocated participants to one of three conditions: internet-based intervention, expressive writing condition and wait-list control (Trompetter et al., 2015).
3.4. Guidance
An important aspect of web-based interventions is how interactive they are, i.e. how much the participant participates within the program e.g. uses self-assessment and self-monitoring tools. All internet-based treatments require that participants act by themselves but the type and degree of feedback offered vary. The degree of feedback differs from self-guided programs that not offer supportive feedback or provides automated feedback to guided programs that offers tailored feedback (Andersson and Cuijpers, 2009, Marks et al., 2009).
77.27% (n = 17) of the included trials were guided. In six (Buhrman et al., 2015, Buhrman et al., 2013b, Buhrman et al., 2004, Buhrman et al., 2013a, Ström et al., 2000, Trompetter et al., 2015) of the studies the online therapists were graduate students who received supervision of clinical psychologists. In several trials (n = 4) the researchers were the therapists (Andersson et al., 2003, Devineni and Blanchard, 2005, Hicks et al., 2006, Kristjánsdóttir et al., 2013a). One trial was guided by a research assistant that also was a nurse (Berman et al., 2009). In another study, in addition to the researcher, an expert patient was used to guide the participants (Brattberg, 2006). In three trials the therapists consisted of clinical psychologists (Buhrman et al., 2011, de Boer et al., 2014, Dear et al., 2013). In Palermo et al. (2009) the participants were guided by a Ph D psychology postdoctoral fellow.
3.5. Outcomes
Focus in the present review is post-intervention data. Seven (31.8%) (Andersson et al., 2003, Berman et al., 2009, Buhrman et al., 2011, Hedborg and Muhr, 2011, Ruehlman et al., 2012, Ström et al., 2000, Williams et al., 2010) of the 22 trials did not include follow-up data. All the outcomes used in the different trials are presented in Table 2.
Table 2.
Outcomes and results in the included trials.
| Trial | Outcome measures | Functioning Pre-post (interaction effects when nothing else specified) |
Pain Pre-post (interaction effects when nothing else specified) |
Psychological/psychosocial variables Pre-post (interaction effects when nothing else specified) |
Follow-up | Drop-out rate at post-treatment |
|---|---|---|---|---|---|---|
| Andersson et al. (2003) | No primary outcome defined. Outcome measures: Headache diary, HADS, PSS, HDI, CSQ |
HDI: decreased significantly for both the sole internet intervention and the internet intervention with telephone support a main effect of time was found. | Pain duration: Post-hoc test showed that the self-help plus telephone group had a significantly decreased duration. In the self-help plus telephone group, 29% reached a clinically significant improvement and in the self-help only group, 23%. The difference was however not statistically significant | Main effect were found on the: HADS-depression subscale, PSS-stress scale, CSQ-reinterpreting pain sensations and CSQ-catastrophizing Interaction effects in favour of the internet group with telephone support were found on the subscales CSQ-ignore pain and CSQ-coping self-statements. Post hoc analyses confirmed the difference in CSQ-ignore pain. |
No FU | 31.9% |
| Berman et al. (2009) | No primary outcomes defined. Outcome measures: BPI, PSEQ: PSEQ,; CES-D 10; STAI-6 |
BPI: NS | BPI-pain intensity: NS . |
PAQ (awareness of responses to pain): interaction effect was found. CES-D (depression): NS STAI: NS PSEQ (pain self-efficacy):NS |
No FU | 12.0% |
| Brattberg (2006) | No primary outcome defined. Outcome measures: SF-36, HADS, a stress barometer |
SF-36- physical functional scale: NS However, thirteen of 23 individuals (57%) increased their work capacity. More individuals in the treatment group had increased their work capacity when compared to the waiting list group. | SF-36- bodily pain. | HADS-depression scale. In an intent-to-treat analysis, the NNT was calculated for anxiety and depression. The number needed to treat regarding recovering from anxiety and depression was 2. For increased work capacity, the number needed to treat was 3 | 1 year (Brattberg, 2007) | 8.3% |
| Bromberg et al. (2012) | No primary outcomes defined. Daily headache record; MIDAS; CPCI-42, HSES, PCS, Headache-specific locus of control, DASS-21, PGIC. |
Migraine-related disability: NS | No information. | Interaction effects were found in the scales: PCS-helplessness scale, PCS-magnification scale: PCS-rumination scale, PCS-total scale, DASS-depression scale, DASS-stress scale; CPCI-exercise, CPCI-persistence, CPCI-relaxation, CPCI-social support and HSES-Self-efficacy. Post-hoc tests revealed that participants who used the website reported a significantly greater decrease in depression, as compared with the control condition. |
3 and 6 months follow-up | 16.4% |
| Buhrman et al. (2013a) | Primary outcome: CSQ Secondary outcomes: HADS, MPI, PAIRS; QOLI |
PAIRS | MPI-Pain severity: NS | Interaction effects were found in the scales: CSQ-diverting attention subscale; CSQ-catastrophizing scale; HADS-anxiety scale; HADS-depression scale; MPI-life control scale; MPI-affective distress scale and MPI-punishing responses scale | 6 months | 22.2% |
| Buhrman et al. (2013b) | Primary outcome: CPAQ Secondary outcomes: HADS, MPI, PAIRS, QOLI |
MPI- interfering | MPI-Pain severity: NS | Interaction effects were found in the scales: CPAQ-activity engagement scale; CPAQ- pain willingness scale; CPAQ-total scale; HADS-anxiety scale; HADS-depression scale: CSQ-catastrophizing subscale; CSQ-praying and hoping subscale; MPI-affective distress subscale. |
6 months | 19.7% |
| Buhrman et al. (2015) | Primary outcomes; MADRS-S, BAI, PDI Secondary outcome measures: ASI, PCS, CPAQ, CSQ, MPI, QOLI. |
PDI | MPI-Pain severity: NS | Interaction effects were found in the scales: MADRS-S, BAI, CPAQ-activity engagement subscale. The difference was clinical significant for the completers. Significant effects were also found on the CSQ-catastrophizing subscale and PCS-total scale. |
1 year | 17.3% |
| Buhrman et al. (2004) | Primary outcome: CSQ Secondary outcomes: MPI, HADS, PAIRS, Pain diary. |
MPI-Interference: NS | MPI-Pain severity: NS | Interaction effects were found in the scales: CSQ-catastrophizing; CSQ-control over pain and CSQ-ability to decrease pain. For the catastrophizing scale 39% (n = 10) showed a reliable improvement, and in the control group 14% (n = 4), a difference that was statistically significant. | 3 months | 8.0% |
| Buhrman et al. (2011) | Primary outcome: CSQ Secondary outcomes: HADS, MPI, PAIRS; QOLI |
MPI-Interference: NS | MPI-Pain severity: NS | An interaction effect was found in the CSQ-catastrophizing scale. A post hoc test on the pre to post change scores confirmed a difference between the groups at posttest. Reliable Change Index was calculated for catastrophizing scale in the CSQ, 58% (15/26) of the treated participants showed a reliable improvement, and in the control group 18% (5/28). This difference that was statistically significant. A significant interaction effect was also found in QOLI, and this was explained by a decrease in the control group and an increase of QOLI scores in the treatment group confirmed by a post hoc test. |
No Fu | 7.4% |
| Carpenter et al. (2012) | Primary outcome: SOPA Secondary outcomes: PCS, RMDQ, FABQ, NMRS, SES. |
RMDQ | Pain rating-average pain; pain rating—highest pain and pain rating—lowest pain: NS | Interaction effect were found on: Pain Catastrophizing Scale (PCS); PCS-rumination; PCS-magnification; PCS-helplessness and negative mood regulation scale. | 6 weeks | 7.1% |
| Chiauzzi et al. (2010) | No primary outcome defined. Outcome measures: BPI, ODQ, DASS, PGIC, CPCI-42, PCS, PSEQ, FABQ. |
ODQ: NS | BPI-worst pain scale: participants recruited online in the internet-group showed a greater mean decrease from baseline to post-test while no significant difference were found for the participants recruited from the clinical settings. 12.3% in internet-group decreased in current pain comparing with 7% in the control condition. | Website participants showed clinically significant reductions in DASS-depression; DASS-anxiety and DASS-stress. | 3 and 6 months | 7.5% |
| de Boer et al. (2014) | Primary outcome: PCS. Secondary outcomes: VAS-pain intensity, PCCL (5 subscales), RAND-36 (9 subscales). Additionally cost-effectiveness was assessed. |
VAS interference and fatigue: NS ITT and completers-analyses showed significant main effects on the subscales physical functioning, social functioning, pain and perceived health change. | VAS-pain intensity: NS . |
Main effects for time on both the internet intervention and the live intervention were found on PCS (ITT-analyses) and PCCL. An interaction effect was found on PCS (Completers-analyses) in favour of the internet group. |
2 months | 20.6% |
| Dear et al. (2013) | Primary outcomes: PHQ-9; GAD-7; RMDQ Secondary outcomes: WBPQ, pain intensity, PSEQ, TSK, PRSS |
RMDQ. | An interpain (average pain) Clinical significance on all primary outcomes except average pain. |
Interaction effect were found on: PHQ-9 (depression); PSEQ (self-efficacy); TSK and PRSS (catastrophizing). | 3 months | 4.0% |
| Devineni and Blanchard (2005) | No primary outcome defined. Outcome measures: Headache diary, HSQ, CES-D, STAI, HDI. |
A significant reduction was found on HDI. The total treated sample (N = 49) showed a significant reduction on medication index scores from baseline to post-treatment. |
Interaction effects were found on: Headache index and Headache Index within the aggregate treated sample. The percentage of treatment completers showing clinically significant improvement, defined as a 50% or greater reduction in Headache Index scores without a corresponding increase in overall medication consumption, was 38.5%. Article in press | CES-D (depression): NS STAI: NS |
2 months | 38.1% |
| Hedborg and Muhr (2011) | No primary outcome defined. Outcome measures: PQ23, MADRS-S; diary of migraine frequency, physical activity lasting 30 min or more, and intake of migraine medications. |
No information | Migraine frequency: 50% greater, reduction was found in 40% and 42% participants of the two groups receiving MBT (with and without hand massage respectively) comparing to 15% in the control group. No significant difference in reduction of migraine was seen between the two treatment groups. Preliminary data indicate that migraine medication decreased in the intervention groups but not in the control group. | MADRS-S: NS PQ23-Perceived work performance (8 months versus start): significant improvement in the intervention group MBT with hand massage. |
No FU | 8.4% |
| Hicks et al. (2006) | Primary outcome: Pain Index in pain diary, NRS Secondary outcome measures: PedsQL, VAS- how much they expected treatment to help them, VAS- evaluations of treatment and perceived benefit of treatment. |
No information. | Significant effects were found on the Pain diary in both pain frequency and pain intensity at 1-month follow-up. The number of pain-free days increased significantly more in the treatment group than the control group at 1-month follow-up. For pain free days, the nonparametric test did not detect the between group differences. 71 and 72% of the treatment group achieved clinically significant improvement at the 1- and 3-month follow-ups, respectively, whereas only 19 and 14% of the control group achieved the criterion | PedsQL: NS | 1 and 3 months | 21.3% |
| Kristjánsdóttir et al. (2013a) | Primary outcome: PCS Secondary outcomes: CPVI, VAS for pain, fatigue and sleep disturbance, FIQ, SF-8, CPAQ, GHQ, feasibility of the smartphone intervention was assessed with single questions post-intervention. |
FIQ | VAS- pain level: NS | Interactions effects were found on: PCS (ITT); PCS (per protocol); CPAQ; SF8-mental and CPVI. | 5 months. 1 year follow-up (Kristjánsdóttir et al., 2013b) |
17.0% |
| Palermo et al. (2009) | Primary outcomes: CALI, pain intensity-NRS, RCADs Secondary outcomes: MDD, ARCS, TEISF |
Interaction effects were found on: CALI-prospective scale (online) and CALI-prospective scale (retrospective) | An interaction effect was found on pain intensity. Retrospective ratings of pain: NS. The mean percent pain reduction in the treatment group was 33.2%. The rate of clinically significant improvement in pain intensity was greater in children in the treatment group for the ITT-sample (38.5% vs 13.6%). |
RCADS (emotional functioning): NS ARCS (parental responses): NS | 3 months | 8.4% |
| Ruehlman et al. (2012) | No primary outcome defined. Outcome measures: CES-D, Depression anxiety stress scales, test of pain knowledge that assessed a wide range of topics addressed within the program, PCP-S, PCP-EA. |
Pain interference in 10 areas of daily functioning (social, sex, sleep, recreation, household chores, work, self-care, parenting, physical activities, and exercise. | Significant interaction effects on pain severity | Interaction effects were found on the scales: CES- depression; DASS-stress: DASS-anxiety: DASS-depression; emotional burden and PCP-EA catastrophizing subscale. | No FU | 7.6% |
| Ström et al. (2000) | No primary outcome defined. Outcome measures: Headache and medication index, BDI, HDI. |
HDI: NS | Interaction effects were found on the Headache index; frequency of headache days and Peak intensity. Among the participants in the treatment condition, 50% showed a clinically significant improvement | BDI: NS | No FU | 56% |
| Trompetter et al. (2015) | Primary outcome: MPI-pain interference Secondary outcomes: PCS, MHC-SF, PDI, HADS, FFMQ, PIPS, Pain-NRS |
A treatment effect was found on MPI-Interference in favor for ACT comparing to Expressive Writing. ACT vs WL: NS |
Significant results were found in Pain intensity in favor for ACT comparing to EW. | An interaction effect was found on PCS in favor for ACT comparing to WLC. An interaction effect was found on PIPS in favor of ACT comparing to EW and to WLC. |
3 months | 27.7% |
| Williams et al. (2010) | Primary outcomes: BPI, SF-36 Physical Functioning Scale. Secondary outcomes: MFI; MOS Sleep scale; CES-D, STPI, PGIC |
An interaction effect was found on SF-36-physical functional scale. The WEB-SM group demonstrated more individual improving 31% vs 6%, NNT 5. PGIC: available for only half of the sample (standard care = 33, WEB-SM n = 35) there was a statistically significant difference in the numbers of individuals reporting at least minimal improvement 57% vs 21%). |
An interaction effect was found on BPI-average pain intensity. Additionally, the proportion of patient reporting a 30% decrease in the mean pain score from baseline to endpoint was significantly greater in the WEB-SM group (29% vs 8%) NNT for the 30% responder rater was 5. | MOS-sleep scale: NS MFI (fatigue): NS CES-Depression: NS STPI (anxiety): NS |
No FU | 10.2% |
NS = no significance; SOPA = The Survey of Pain Attitudes; FABQ = Fear Avoidance Beliefs Questionnaire, PCS = Pain Catastrophizing Scale, NMRS = Negative Mood Regulation Scale, RMDQ = Roland-Morris Disability Questionnaire, SES = Pain self-efficacy Scale, PDI = Pain Disability Index, MPI = Multidimensional Pain Inventory, HADS = Hospital Anxiety Depression Scale, FFMQ = Five Facet Mindfulness Questionnaire, PIPS = Psychological Inflexibility in Pain Scale, ELS = Engaged Living Scale, MHC-SF = Mental Health Continuum-Short Form, PHQ-9 = Patient Health Questionnaire 9-item, GAD-7 = Generalized Anxiety Disorders 7-item, WBQ = Wisconsin Brief Pain Questionnaire, PSEQ = Pain Self-efficacy Questionnaire, TSK = TAMPA Scale of Kinesiophobia, PRSS = Pain Responses Self-Statements, CALI = Child Activity Limitations Interview, Pain NRS = Numerical Rating Scale, RCADS = Revised Child Anxiety Depression Scale, ARCS = Adult Responses to Children's Symptoms, TEISF = Treatment Evaluation Inventory-Short Form, CSQ = The Coping Strategies Questionnaire, PAIRS = Pain Impairment Relationship Scale, QOLI = Quality of Life Inventory, CPAQ = Chronic Pain Acceptance Questionnaire, MADRS-S = Montgomery–Åsberg Depression Rating Scale-Swedish version, BAI = Beck Anxiety Inventory, ASI = Anxiety Sensitivity Index, BPI = Brief Pain Inventory-Short Form, PSEQ = Pain Self-efficacy Questionnaire, CES-D = Center Epidemiologic studies Short Depression Scale, STAI-6 = State–Trait Anxiety Inventory, MIDAS = Migraine disability assessment questionnaire, CPCI-42 = Chronic Pain Coping Inventory-42, HSES = Headache management self-efficay scale, DASS-21 = Depression Anxiety Stress Scales, PGIC = Patient Global Impression of Change, ODQ = Oswestry Disability Questionnaire, HDI = Headache Disability Inventory, HSQ = Headache Symptom Questionnaire, PQ23 = Quality of life questionnaire, BDI = Beck depression inventory, PSS = The Perceived Stress Scale, PCP-S = Profile of Chronic Pain-Screen, PCP-EA = Profile of Chronic Pain Extended Assessment, SF-36 = SF-36 Physical Functioning Scale, MFI = Multidimensional Fatigue Inventory, STPI = State–Trait Personality Inventory, SF-36 = Medical Outcomes 36-Item Short-Form Health Survey, CPVI = The Chronic Pain Values Inventory, VAS = Visual analog scales, FIQ = Fibromyalgia Impact Questionnaire, SF-8 = Short form health survey, GHQ = General Health Questionnaire, PedsQL = Pediatric Quality of Life Inventory, PCCL = Pain Coping and Cognition List, RAND36 = Global health-related quality of life.
3.6. Primary outcomes
The most frequently measured domain reflected in the primary outcomes was interference/disability (in six of the trials) (Berman et al., 2009, Dear et al., 2013, Hicks et al., 2006, Palermo et al., 2009, Trompetter et al., 2015, Williams et al., 2010), followed by catastrophizing (in five of the studies) (Buhrman et al., 2004, Buhrman et al., 2013a, Buhrman et al., 2011, de Boer et al., 2014, Kristjánsdóttir et al., 2013a). Pain intensity/severity was the primary outcome in four of the trials (Berman et al., 2009, Hicks et al., 2006, Palermo et al., 2009, Williams et al., 2010). One study (Carpenter et al., 2012) used a survey of pain attitudes (SOPA) as a primary outcome and psychological variables such as depression and anxiety domains were primary outcomes in three trials (Buhrman et al., 2015, Dear et al., 2013, Palermo et al., 2009). Other included primary outcomes were quality of life (Hedborg and Muhr, 2011) and self-efficacy (Berman et al., 2009).
3.7. Secondary outcomes
Secondary outcomes were reported in 14 of the trials. These outcomes were pain severity, self-efficacy, catastrophizing, fear of movement and re-injury, emotional functioning, disability, acceptance, pain attitudes and beliefs. For more details see Table 2.
3.8. Uncategorized domain and measures
Eight (Andersson et al., 2003, Brattberg, 2006, Bromberg et al., 2012, Chiauzzi et al., 2010, Devineni and Blanchard, 2005, Hedborg and Muhr, 2011, Ruehlman et al., 2012, Ström et al., 2000) of which five (Andersson et al., 2003, Bromberg et al., 2012, Devineni and Blanchard, 2005, Hedborg and Muhr, 2011, Ström et al., 2000) were headache and/or migraine trials of the 22 studies listed a variety of outcomes but did not specify whether any of these were considered primary or secondary. The domains measured were emotional functioning such as depression and anxiety, pain severity, interference, catastrophizing, pain attitudes and beliefs, headache and medication index and coping strategies.
3.9. Effect of internet-based CBT-based interventions
Result across the studies showed a number of beneficial effects. In the present review, effects from the primary analyses are focused. As mentioned earlier several (n = 10) of the included trials included inactive control condition while four used active control groups (Buhrman et al., 2015, Buhrman et al., 2013a, Buhrman et al., 2013b, Chiauzzi et al., 2010). Two trials (Hedborg and Muhr, 2011, Trompetter et al., 2015) included three conditions and three (Bromberg et al., 2012, Ruehlman et al., 2012, Williams et al., 2010) used treatment as usual. Three trials used active treatments, one used internet-based treatment with the addition of telephone support (Andersson et al., 2003), one internet-based treatment without smartphone (Kristjánsdóttir et al., 2013a) and the third trial compared the internet-based treatment with face-to-face group intervention (de Boer et al., 2014). For an overview of the results see Table 2.
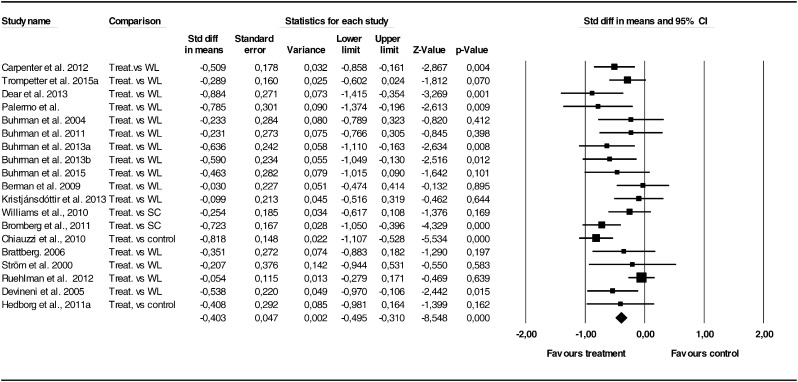
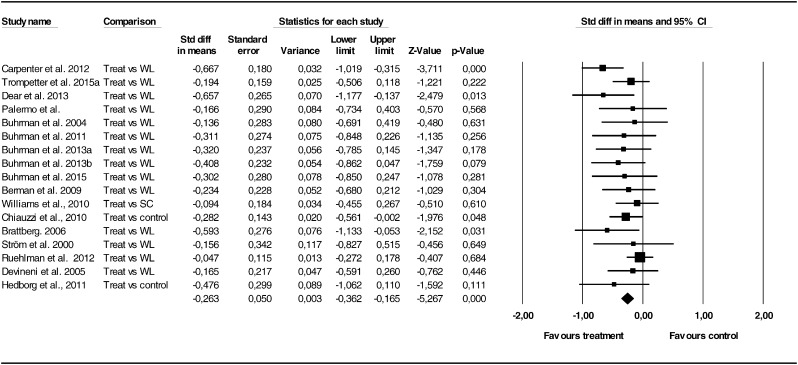
3.10. Interference and disability
We calculated effect sizes for the interference/disability measures based on the means and standard deviations at post-treatment. For the studies where the comparison group was either waiting list or treatment as usual the overall random effects effect size in the 15 pain studies was Hedge's g = − 0.42 (95% CI: − 0.55 to − 0.28), in the direction of favouring treatment but with a significant heterogeneity (I2 = 53.5%). Publication bias was not present as assessed by Egger's test (p = .24). Guidance did not moderate this effect (g = − 0.39 for guided vs. − 0.37 for unguided treatments). The effect size for the four headache trials was Hedge's g = − 0.52 (95% CI: − 0.74 to − 0.30), in the direction of favouring treatment and with a non-significant heterogeneity (I2 = 30.0%). Publication bias was not present from the Egger's test (p = .07). For the three trials in which internet treatment had been compared against an active control condition (e.g., face-to-face) the results showed an advantage for the comparison condition Hedge's g = − 0.33 (95% CI: − 0.58 to − 0.008), with no heterogeneity I2 = 0.0%) or publication bias. A forest plot for the pain and headache studies combined is presented in Fig. 2. We included the waitlist and treatment as usual control groups (N = 19). Here the effect size was Hedge's g = − 0.41 (95% CI: − 0.55 to − 0.27), with a significant heterogeneity (I2 = 50.0%), but no indication of publication bias.
Fig. 2.
Forest plot of studies comparing internet treatment against no treatment or treatment as usual control conditions for pain and headache using pain interference/disability ratings.
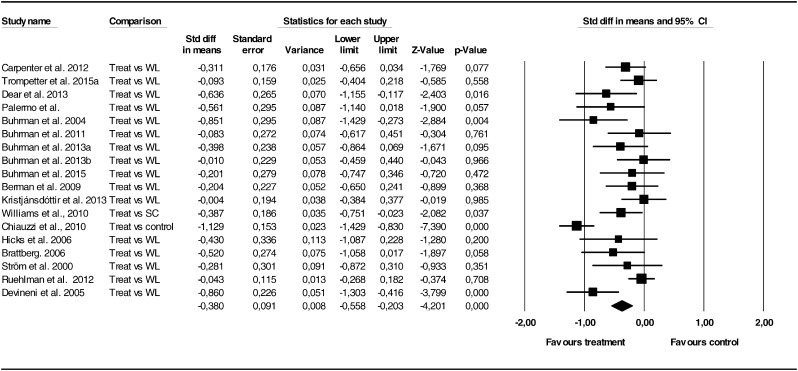
3.11. Pain
Effect sizes were calculated for the pain severity measures. For the studies where the comparison group was either waiting list or treatment as usual the overall random effects effect size in 16 pain studies was Hedge's g = − 0.35 (95% CI: − 0.54 to − 0.17), in the direction of favouring treatment but with a significant heterogeneity (I2 = 68.6%). Publication bias was not present as assessed by Egger's test (p = .25). Removing outliers (Chiauzzi et al., 2010) reduced the effect (g = − 0.25), but the overall effect remained statistically significant. Guidance did not moderate the effect (with only three studies being unguided). We did not calculate the effect size for the headache studies as there were only two studies in which pain data were provided for the waitlist condition. This was also the case for the active control comparisons with only two trials. The overall effect for pain ratings (both pain and headache compared against waitlist or regular care) involved 18 trials and the effect was Hedge's g = − 0.38 (95% CI: − 0.56 to − 0.23) in the direction of favouring treatment but with a large significant heterogeneity (I2 = 67.9%). Publication bias was not present as assessed by Egger's test (p = .22). A forest plot for the pain and headache studies combined is presented in Fig. 3.
Fig. 3.
Forest plot of studies comparing internet treatment against no treatment or treatment as usual control conditions for pain and headache using pain severity ratings.
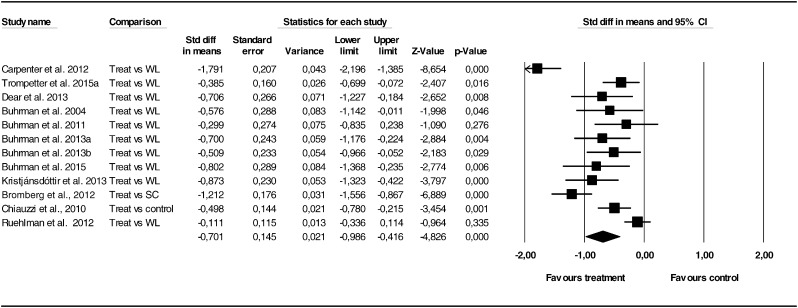
3.12. Catastrophizing
We calculated meta-analytic statistics for the catastrophizing outcomes. For the studies where the comparison group was either waiting list of treatment as usual the overall random effects effect size for the 11 pain studies was Hedge's g = − 0.65 (95% CI: − 0.95 to − 0.36), in the direction of favouring treatment but with a significant heterogeneity (I2 = 82.2%). Publication bias was not present as assessed by Egger's test (p = .12). As the Carpenter et al. (2012) trial had a substantially higher effect size (g = − 1.79) we recalculated the effect with this trial removed, which resulted in a lower but still significant effect (g = − 0.49). Adding the only controlled headache trial (Bromberg et al., 2012) did not change the results (g = − 0.70) compared to the overall findings. For an overview for the effects see Fig. 4.
Fig. 4.
Forest plot of studies comparing internet treatment against no treatment or treatment as usual control conditions for pain and headache using catastrophizing ratings.
3.13. Depression and anxiety
We calculated meta-analytic statistics for the mood ratings (mainly depression). For the 14 pain studies the effect size when comparing against waitlist/treatment as usual was Hedge's g = − 0.27 (95% CI: − 0.38 to − 0.16), in the direction of favouring treatment and without significant heterogeneity (I2 = 7.9%). Publication bias was not present as assessed by Egger's test (p = .10). Adding the three headache trials did not change the result (Hedge's g = − 0.26). See Fig. 5 for forest plot.
Fig. 5.
Forest plot of studies comparing internet treatment against no treatment or treatment as usual control conditions for pain and headache using depression ratings.
3.14. Risk of bias within studies
Assessment of the studies was made using an adapted Cochrane Collaboration tool for the risk of bias within randomized trials (Higgins et al., 2011). Five areas of potential bias were assessed: selection bias, detection bias, attrition bias, reporting bias and other bias. Selection bias focus is on the description on the method used to generate the allocation sequence. To assess detection bias description of all used measures was observed and whether there was an intended blinding. Authors need to describe the completeness of outcome data for each main outcome, including attrition and exclusions from the analysis for a low attrition bias. Reporting bias concerns the reporting of the prespecified outcomes. Other bias assesses if any important concerns about bias, not covered in the other domains in the tool are present. An overall assessment of bias was made, where a low overall assessment required low assessments in all the five areas. Table 3 provides a summary of the risk of bias assessment. More than half (n = 14) of the trials reported sufficient descriptions of participant randomization, which leads to comparable groups. In eight of the studies, selection bias was unclear since the method of randomization was not described in sufficient detail (Andersson et al., 2003, Carpenter et al., 2012, Chiauzzi et al., 2010, Dear et al., 2013, Devineni and Blanchard, 2005, Hicks et al., 2006, Ruehlman et al., 2012, Ström et al., 2000). Five of the trials did not clearly demonstrate how data was collected (Brattberg, 2006, Chiauzzi et al., 2010, Hicks et al., 2006, Kristjánsdóttir et al., 2013a, Ström et al., 2000). In the remaining trials (n = 17) it was reported that data was collected online and blinded for the researchers. Most trials (n = 17) reported adequate information about attrition. However, four studies (Brattberg, 2006, Carpenter et al., 2012, Chiauzzi et al., 2010, Hicks et al., 2006) did not report attrition clearly enough or no reasons for participants withdrawing were given. Reporting bias was found low in most trials (n = 16) since the pre-specified outcomes were reported. Three trials (Bromberg et al., 2012, Carpenter et al., 2012, Ström et al., 2000) were assessed high risk of reporting bias since not all outcome measures were made available for analyses. In one study (Ström et al., 2000) one outcome variable was not included in the analyses. In three trials (Andersson et al., 2003, Brattberg, 2006, Devineni and Blanchard, 2005) reporting bias was judged unclear since no intention-to-treat analyses were made. Overall ten trials (Berman et al., 2009, Buhrman et al., 2015, Buhrman et al., 2013a, Buhrman et al., 2013b, Buhrman et al., 2011, Buhrman et al., 2004, de Boer et al., 2014, Hedborg and Muhr, 2011, Palermo et al., 2009, Trompetter et al., 2015) were assessed having a low risk of bias and the remaining 12 were judged having unclear risk of bias.
Table 3.
Risk of bias within studies.
| Reference | Selection bias | Selection bias argument | Detection bias | Detections bias argument | Attrition bias | Attrition bias argument | Reporting bias | Reporting bias argument | Other bias | Other bias argument | Overall assessment of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Andersson et al. (2003) | Unclear | Randomization method unclear | Low | All outcomes are described and administered online | Low | Attrition is well described and analyses between completers and non-completers are made. | Unclear | No ITT-analyses. | Low | Study appears to be free of other sources of bias | Unclear |
| Berman et al. (2009) | Low | Participants were randomly assigned to either the intervention or WLC via a simple coin toss. | Low | Assessments described and taken online | Low | Imputed score for standardized scales that were missing no less than 10% of the responses, with the exception of the CES-D 10. | Low | All results are reported | Low | Study appears to be free of other sources of bias. | Low |
| Brattberg (2006) | Low | Lottery draw by a study leader who was blindfolded. | Unclear | Outcomes are scarcely described and are administered both by regular mail and e-mail. | Unclear | Attrition is explained. Unclear drop-out analyses. | Unclear | Outcomes are presented. No ITT analyses. | Low | Study appears to be free of other sources of bias | Unclear |
| Bromberg et al. (2012) | Low | Random number table was used for group assignment | Low | All outcomes are described and administered online | High | One outcome measure was not available for analysis. | High | All outcomes are not included, due to a data management error. | Low | Study appears to be free of other sources of bias. | Unclear risk |
| Buhrman et al. (2013a) | Low | Randomization was made by an independent person through a randomization page using at true random number service. | Low | All outcomes are described and administered online | Low | Attrition is well explained and drop-out analyses were made. | Low | All data presented using ITT analyses. | Low | Study appears to be free of other sources of bias. | Low |
| Buhrman et al. (2013b) | Low | Randomization was made through a randomization page using at true random number service. | Low | All outcomes are described and administered online | Low | Attrition is explained and drop-out analyses were made. | Low | All data presented using ITT analyses. | Low | Study appears to be free of other sources of bias. | Low |
| Buhrman et al. (2015) | Low | Randomization was made through a randomization page using at true random number service. | Low | All outcomes are described and administered online | Low | Attrition is explained and drop-out analyses were made. | Low | All data presented using ITT analyses. | Low | Study appears to be free of other sources of bias. | Low |
| Buhrman et al. (2004) | Low | Randomization was done with a dice | Low | All outcomes are described and administered online | Low | Attrition well described. Differences between completers and non-completers are reported. | Low | All outcomes are reported and missing data is imputed. | Low | Study seems to be free of other sources of bias | Low |
| Buhrman et al. (2011) | Low | Randomization was made by an independent person through a randomization page. | Low | All outcomes are described and administered online | Low | Attrition described and analyses of completer and non-completers was made. | Low | All outcome measures were presented according the ITT principle. | Low | Study seems to be free of other sources of bias | Low |
| Carpenter et al. (2012) | Unclear | Eligibility criteria changed during allocation (age). Randomization through random number table. No more information given. | Low | All measures described, participants and administered online | Unclear | No information about why participants dropped out. | High | No ITT-data presented | Low | Study appears to be free of other sources of bias. | Unclear |
|
Chiauzzi et al. (2010) USA |
Unclear | Participants were randomized using an adaptive or “stratified” randomization that ensures group equivalence on preselected variables that may relate to outcome across conditions. The method is not described. No information about allocation concealment insufficient. |
Unclear | No information about how the outcomes were administered. | Unclear | Attrition was described but difference between completers and non-completers is missing. | Low | All pre-specified outcomes were presented | Low | Study appears to be free of other sources of bias. | Unclear |
| de Boer et al. (2014) | Low | Permuted block randomization (ration 1:1; block size of 14). For allocation sequence was concealed from the researcher enrolling and assessing participants in sequential numbered sealed envelopes. | Low | All measures described, participants unidentified. | Low | Attrition was adequately explained and missing data appeared to have been imputed using appropriate methods. | Low | Published report includes data for all expected outcomes | Low | Study appears to be free of other sources of bias. | Low |
| Dear et al. (2013) | Unclear | Randomization via a permuted randomization process. No information of method. Groups differed in the PRSS. | Low | All measures described, participants unidentified | Low | Completers described. Attrition described. ITT (LCOF) |
Low | All pre-specified outcomes were presented | Low | Study appears to be free of other sources of bias. | Unclear |
| Devineni and Blanchard (2005) | Unclear risk | Randomization method unclear | Low | All outcomes are described and administered online | Low | Attrition is well described and dropout predictors are reported | Unclear | All post-data is reported however is not all FU data reported. | Low | Study appears to be free of other sources of bias | Unclear risk |
|
Hedborg and Muhr (2011) Sweden |
Low | Randomization procedure: a sequence of random numbers was generated in statistical package for the social sciences 18.0 (SPSS) software, stratified by gender. Based on magnitude these numbers were arranged into three equal-sized groups, which translated into the three study groups. Blinded randomization. | Low | Outcomes well described and administered online. | Low | Attrition well described and analyses of completers and no-completers reported. | Low | All data reported. ITT for main variables. | Low | Study appears to be free of other sources of bias | Low |
| Hicks et al. (2006) | Unclear risk | Randomization method unclear | Unclear risk | Outcomes were mailed out but unclear how participants sent their responses. | Unclear | ITT analyses were conducted. No information about why participants dropped out. | Low | All expected data is reported | Low | Study appears to be free of other sources of bias. | Unclear risk |
|
Kristjánsdóttir et al. (2013a) Norway |
Low | A computer generated sequence list with the 2 groups randomized in blocks of 4 used for practical reasons to ensure similar numbers in each group at each time point. | Unclear risk | Questionnaires were administered in paper. No description given if outcome assessors were blinded. Outcomes described. | Low | Attrition is described and differences between completers and non-completers are reported. | Low | Published report includes data for all expected outcomes. ITT analyses. | Low | Study appears to be free of other sources of bias | Unclear |
| Palermo et al. (2009) | Low | Fixed allocation randomization scheme was used. Blocked randomization with blocks of 10. An online random number generator was used. Comparable groups | Low | All measures described, participants unidentified. | Low | Completers described. Attrition described. ITT |
Low | All pre-specified outcomes were presented | Low | Study appears to be free of other sources of bias. | Low |
| Ruehlman et al. (2012) | Unclear risk | Randomization method unclear | Low | All outcomes are described and administered online | Low | Attrition was adequately explained and missing data appeared to have been imputed using appropriate methods. | Low | All prespecified outcomes were presented | Low | Study appears to be free of other sources of bias | Unclear |
| Ström et al. (2000) | Unclear | Randomization method unclear | Unclear risk | Some outcomes administered online while other on paper. Unclear if blinding was possible. All outcomes described. | Low | Attrition described and differences between completers and non-completers reported. | High | MLPC not reported in the results. No ITT analyses. | Low | Study appears to be free of other sources of bias | Unclear |
| Trompetter et al. (2015) | Low | Allocation to conditions was performed by sequential block wise randomization using an electronically written key, with stratification on gender, age, and educational level. | Low | All measures described, participants unidentified | Low | Completers described. Attrition described. ITT |
Low | All outcomes were presented. ITT mixed model. | Low | Study appears to be free of other sources of bias. | Low |
|
Williams et al. (2010) USA |
Low | Randomization used 1:1 ratio. A computerized randomization program assisted in the development of the allocation sequence for study. Allocation concealment was utilized to prevent selection bias. | Low | All outcomes adequately described and taken online. | Unclear | Attrition is described but differences between completers and non-completers is not reported | Low | Published report includes data for all expected outcomes ITT analyses. |
Low | Study appears to be free of other sources of bias | Unclear |
3.15. Attrition
Drop-out rates in internet-based trials vary significantly. In a review they were reported to range from 2 to 83% (Melville et al., 2010). A common approach classifies drop-out based on non-completion of one or more assessment or treatment components (i.e. pre-treatment assessments, treatment sessions, post-treatment assessments) (Melville et al., 2010). The drop-out rates ranged from 4% (Dear et al., 2013) to 56 % (Ström et al., 2000). It seems that attrition is a bigger problem in unguided internet-based treatments than guided ones (Baumeister et al., 2014). However, in the present review this difference is not clear. In the present review the majority of the trials were guided (72 %). The five unguided trials have drop-out rates that range from 7.1% to 16.4%. The three studies with highest drop-out rates were headache trials and they reported values of 31.9% (Andersson et al., 2003), 38.1 % (Devineni and Blanchard, 2005) and 56% (Ström et al., 2000). For more information see Table 2.
Different trials have used different methods to prevent high drop-out numbers. Several trials used telephone support (Andersson et al., 2003, Buhrman et al., 2013a, Buhrman et al., 2004, Dear et al., 2013, Hedborg and Muhr, 2011, Hicks et al., 2006). Andersson et al. (2003) did not find evidence of an effect of the telephone calls regarding the drop-out rate. All guided trials used personalized reminders and feedback instead of impersonal automatic reminders with the exception of one guided study (Dear et al., 2013) that employed regular automatic e-mails that reinforced the participants. Several trials also included some live meetings (Berman et al., 2009, Brattberg, 2006, Hedborg and Muhr, 2011, Kristjánsdóttir et al., 2013a). In five trials, participants were paid for completing assessments (Berman et al., 2009, Bromberg et al., 2012, Carpenter et al., 2012, Chiauzzi et al., 2010, Ruehlman et al., 2012). The financial incentive varied from a total sum of $75–$200. Participants received a financial benefit per measurement point except in one trial (Berman et al., 2009) where participants received $100 for their participation in the study project. Four of these trials were unguided (Bromberg et al., 2012, Carpenter et al., 2012, Chiauzzi et al., 2010, Ruehlman et al., 2012).
3.16. Software
The trials included in this review report different security levels to the websites. Four trials (Buhrman et al., 2015, Buhrman et al., 2013b, Buhrman et al., 2013a, Trompetter et al., 2015) describe secure websites that require double identification and all communication takes place on enclosed secure websites. Two unguided studies (Carpenter et al., 2012, Williams et al., 2010) report using secure servers with unique user-id. Most trials used user-name and password to log in to the websites and communication took place through e-mails (Andersson et al., 2003, Berman et al., 2009, Brattberg, 2006, Bromberg et al., 2012, Buhrman et al., 2004, Buhrman et al., 2011, Chiauzzi et al., 2010, de Boer et al., 2014, Devineni and Blanchard, 2005, Kristjánsdóttir et al., 2013a, Palermo et al., 2009, Ström et al., 2000). Two trials (Dear et al., 2013, Ruehlman et al., 2012) lacked information regarding inlog to the internet-based treatments. One trial (Kristjánsdóttir et al., 2013a) used smartphones as the main source to the treatment in addition to a website; information about the security of the inlog is scarce.
3.17. Time spent on the participants
Several of the guided trials reported time spent on the participants. Ström et al. (2000) described that the sum of time that the therapist spent per participant was 40 min. Furthermore, a cost-efficient analysis was conducted and the authors conclude that their treatment is as cost-efficient as minimal therapist contact treatment and 12 times as cost-efficient as traditional clinical treatment. In the trial by de Boer et al. (2014) a cost-effectiveness analysis was made and showed that in the internet course the costs were €199 lower compared to the group course however, no information of times spent on participants was reported. Palermo et al. (2009) reported that 30 min per participant was spent; Dear et al. (2013) described that the total time spent per participant on average was 81.54 min (sd = 30.91) and Hicks et al. (2006) reported that the mean time spent was 189 min (telephone calls constituted the majority of the contact time). One trial (Devineni and Blanchard, 2005) estimated the time to be 78 min per participant. Andersson et al. (2003) described the time the telephone calls lasted, 5–20 min (mean time 10 min) per call of a total of 6 calls. However, no information about the time spent on the internet group without telephone calls is given. Several trials (n = 10) did not report the time spent on the participants (Berman et al., 2009, Brattberg, 2006, Buhrman et al., 2015, Buhrman et al., 2013b, Buhrman et al., 2004, Buhrman et al., 2013a, Buhrman et al., 2011, Hedborg and Muhr, 2011, Kristjánsdóttir et al., 2013a, Trompetter et al., 2015).
4. Discussion
This review included 22 randomized controlled trials of which two included children/youth and five included individuals with chronic headache and/or migraine. Overall, the literature on internet treatments for pain and headache is heterogeneous and the effects (as assessed by meta-analysis) are small to moderate. The results of this review are thus in line with previous reviews with small to moderate overall effects. However, the present review had broader inclusion of studies including trials on headache and children/youth. The most frequent primary outcome was interference/disability followed by catastrophizing. In the five trials including chronic headache and/or migraine no primary outcomes were defined. Several of the included trials had small sample sizes and reported power issues (Andersson et al., 2003, Brattberg, 2006, Buhrman et al., 2015, Buhrman et al., 2004, Buhrman et al., 2011, Dear et al., 2013, Hicks et al., 2006, Palermo et al., 2009, Ström et al., 2000). Many studies (n = 12) were assessed as having an unclear level of risk bias. The main focus in the present review was interference/disability and pain but there was also an interest in the measures of catastrophizing, and depression/anxiety.
Most trials (91%) included measures of interference or disability. The majority (n = 12) reported significant results in favor of the internet-based treatment of which two (Andersson et al., 2003, Devineni and Blanchard, 2005) included individuals with headache. Effect sizes ranged from small to large and a couple (Andersson et al., 2003, Williams et al., 2010) of the trials showed clinical significant effects. However, the overall effect was small (Hedge's g = − 0.39). Only one trial did not report pain intensity or pain frequency (Bromberg et al., 2012). Twelve trials reported significant results on pain intensity and/or pain frequency of which four (of five headache trials) included chronic headache and/or migraine and two paediatric pain. The effect sizes ranged from small to medium, even if not all trials reported effect sizes. When we calculated effect sizes we found a small average effect (Hedge's g = − 0.33). Thus, for both pain interference/disability and pain severity effects are modest which is in line with the effects of CBT in face-to-face trials (Eccleston et al., 2013).
Catastrophizing has been found to be important to target in the treatment of chronic pain since it is associated with several negative consequences in a person's life such as psychosocial dysfunction and greater health care utilization (Linton and Bergbom, 2011, Turner et al., 2000). The findings of the present review show that catastrophizing is a common measure since the majority of the trials (n = 14) included some catastrophizing scale. Among the trials that did not measure catastrophizing three included participants with chronic headache and/or migraine and one included paediatric pain. Significant reductions in catastrophizing were found in 13 trials of the 14 studies with effect sizes ranging from small to large. When we calculated meta-analytic statistics the average effect was moderate (Hedge's g = − 0.65), and somewhat lower when one outlier was removed (g = − 0.49). Thus, we conclude that internet-based CBT has the potential to reduce catastrophizing even if larger studies are needed and the effects are moderate.
Emotional distress in terms of depression and anxiety was included in 90% (n = 20) of the trials and significant results were found in the depression scales in favour of the internet-based treatments in 11 studies. Effect sizes range from small to moderate in the six trials that reported effect sizes. Six studies reported significant results in anxiety scales with modest effect sizes. Two of the included trials that showed significant results in both depression and anxiety (Buhrman et al., 2015, Dear et al., 2013) used these scales as primary outcomes since the interventions targeted emotional distress in chronic pain adults. The effect size we calculated was small (Hedge's g = − 0.26), leaving much room for improvement.
Attrition can be a big problem in internet-based treatments and it is therefore important to engage and involve the user in the treatment which can motivate the person to learn and progress through the program (Andersson, 2014). A recent systematic review concluded that although guidance is a beneficial feature of internet-based interventions, its effect is smaller than reported before when compared to unguided interventions (Baumeister et al., 2014). Interestingly the difference in attrition in the present review was not obvious between the guided and unguided trials as proposed by research (Baumeister et al., 2014). However, the majority of the included trials (n = 17) were guided. The range in attrition levels was considerable, from 4% to 54%. The studies with highest drop-out levels were the chronic headache trials with drop-out rates between 31.9%–56%. Since, drop-out is a common problem in internet-based intervention different methods were used to prevent this problem such as telephone support, personalized reminders and feedback, and financial incitements. It is unclear how much these methods were helpful.
There are limitations that need to be mentioned. First, we need to acknowledge the fact that we reviewed a broad range of studies, which is reflected in a wide variety of outcomes, different treatment formats, lengths of treatment and many other aspects. Pain is a broad construct and it is possible that we may have missed studies and the decision not to include related problems such as irritable bowel syndrome is a potential limitation as well. Second, as we do not have enough studies yet it is hard to conduct moderator analyses to discern what works (Andersson et al., 2009). For example, we had very few studies on unguided internet-based CBT treatments which are common forms of treatment but usually not as effective as guided treatments. Furthermore, the quality of the trials could have been better and there is a need for better trials with larger samples that are described in more detail. For example, it can be hard to grasp how the intervention looks like without screenshots that are rarely available for the reader of a paper. Given the public health implications of chronic pain conditions (including headache) it is crucial that new treatments and formats (e.g., internet delivery) are carefully investigated and described before they are disseminated. As a third limitation, we acknowledge the fact that most of the studies we reviewed are not conducted in clinical regular settings which calls for studies that are more representative for regular health care settings (so-called effectiveness studies). Fourth, as mentioned earlier more than half of the included trials had an overall unclear risk of bias. However, to be assessed as low risk of bias all five criteria needed to be rated as low risk. Fifth, few of the included studies conducted a proper cost-effectiveness analysis. Future studies should include this kind of data. Another important topic to investigate is the possibility of negative and harmful effects (Rozental et al., 2014). Furthermore, it is important to compare the internet-based interventions with credible alternative treatments. The majority of the included trial in the present review used wait-list controls, which can be justified when there is no alternative treatment available but still leaves the question of how the treatment works against alternative treatments. It is difficult to conclude regarding the results in the headache and/or migraine trials; more studies are needed. One trial (Kristjánsdóttir et al., 2013a) in the present review included smartphone communication for women with widespread pain. Probably, smartphones and apps will increase as complements or as a sole intervention in the area of self-help. A recent systematic review (Wallace and Dhingra, 2014) showed that most of the pain-related apps included in their review not only lacked evidence of health care professionals input regarding development but also contained few evidence-based pain management features. There is room for improvement in this area.
There are however, also some strengths to consider. Internet offers several advantages: reducing costs and increasing convenience for users, reducing health service costs, and reaching isolated groups, furthermore it can offer a treatment opportunity avoiding stigmatization and persons have often timeless access to internet and thereby to the treatment. For being a fairly recent format for delivery of pain treatment there are many controlled trials and at the very least the findings are promising. In addition, the findings of the included trials are comparable with the effects of CBT in general for chronic pain (Eccleston et al., 2013). Hopefully, new trials will help us improve the outcomes and better tailor interventions to the needs of the patients.
References
- Andersson G. Using the Internet to provide cognitive behaviour therapy. Behav. Res. Ther. 2009;47:175–180. doi: 10.1016/j.brat.2009.01.010. [DOI] [PubMed] [Google Scholar]
- Andersson G. Boca Raton CRS Press; 2014. The Internet and CBT: A Clinical Guide. [Google Scholar]
- Andersson G., Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cogn. Behav. Ther. 2009;38:196–205. doi: 10.1080/16506070903318960. [DOI] [PubMed] [Google Scholar]
- Andersson G., Lundström P., Ström L., Lundstrom P., Strom L. Internet-based treatment of headache: does telephone contact add anything? Headache. 2003;43:353–361. doi: 10.1046/j.1526-4610.2003.03070.x. [DOI] [PubMed] [Google Scholar]
- Andersson G., Carlbring P., Berger T., Almlöv J., Cuijpers P. What makes internet therapy work? Cogn. Behav. Ther. 2009;38:55–60. doi: 10.1080/16506070902916400. [DOI] [PubMed] [Google Scholar]
- Baumeister H., Reichler L., Munzinger M., Lin J. The impact of guidance on internet-based mental health interventions — a systematic review. Internet Interv. 2014;1:205–215. [Google Scholar]
- Bender J.L., Radhakrishnan A., Diorio C., Englesakis M., Jadad A.R. Can pain be managed through the Internet? A systematic review of randomized controlled trials. Pain. 2011;152:1740–1750. doi: 10.1016/j.pain.2011.02.012. [DOI] [PubMed] [Google Scholar]
- Berman R.L.H., Iris M.a., Bode R., Drengenberg C. The effectiveness of an online mind–body intervention for older adults with chronic pain. J. Pain. 2009;10:68–79. doi: 10.1016/j.jpain.2008.07.006. [DOI] [PubMed] [Google Scholar]
- Brattberg G. Internet-based rehabilitation for individuals with chronic pain and burnout: a randomized trial. Int. J. Rehabil. Res. 2006;29:221–227. doi: 10.1097/01.mrr.0000210055.17291.f5. [DOI] [PubMed] [Google Scholar]
- Brattberg G. Internet-based rehabilitation for individuals with chronic pain and burnout II: a long-term follow-up. Int. J. Rehabil. Res. 2007;30:231–234. doi: 10.1097/MRR.0b013e32829fa545. [DOI] [PubMed] [Google Scholar]
- Bromberg J., Wood M.E., Black R.a., Surette D.a., Zacharoff K.L., Chiauzzi E.J. A randomized trial of a web-based intervention to improve migraine self-management and coping. Headache. 2012;52:244–261. doi: 10.1111/j.1526-4610.2011.02031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhrman M., Fältenhag S., Ström L., Andersson G. Controlled trial of internet-based treatment with telephone support for chronic back pain. Pain. 2004;111:368–377. doi: 10.1016/j.pain.2004.07.021. [DOI] [PubMed] [Google Scholar]
- Buhrman M., Nilsson-Ihrfeldt E., Jannert M., Strom L., Andersson G. Guided internet-based cognitive behavioural treatment for chronic back pain reduces pain catastrophizing: a randomized controlled trial. J. Rehabil. Med. 2011;43:500–505. doi: 10.2340/16501977-0805. [DOI] [PubMed] [Google Scholar]
- Buhrman M., Fredriksson A., Edstrom G., Shafiei D., Tarnqvist C., Ljotsson B., Hursti T., Gordh T., Andersson G., Buhrman M., Fredriksson A., Edstrom G., Shafiei D., Tarnqvist C., Ljotsson B., Hursti T., Gordh T., Andersson G. Guided internet-delivered cognitive behavioural therapy for chronic pain patients who have residual symptoms after rehabilitation treatment: randomized controlled trial. Eur. J. Pain (United Kingdom) 2013 doi: 10.1002/j.1532-2149.2012.00244.x. [DOI] [PubMed] [Google Scholar]
- Buhrman M., Skoglund A., Husell J., Bergstrom K., Gordh T., Hursti T., Bendelin N., Furmark T., Andersson G. Guided internet-delivered acceptance and commitment therapy for chronic pain patients: a randomized controlled trial. Behav. Res. Ther. 2013;51 doi: 10.1016/j.brat.2013.02.010. [References] [DOI] [PubMed] [Google Scholar]
- Buhrman M., Syk M., Burvall O., Hartig T., Gordh T., Andersson G. Individualized guided internet-delivered cognitive-behavior therapy for chronic pain patients with comorbid depression and anxiety: a randomized controlled trial. Clin. J. Pain. 2015;31:504–516. doi: 10.1097/AJP.0000000000000176. [DOI] [PubMed] [Google Scholar]
- Carpenter K.M., Stoner S.A., Mundt J.M., Stoelb B. An online self-help CBT intervention for chronic lower back pain. Clin. J. Pain. 2012;28:14–22. doi: 10.1097/AJP.0b013e31822363db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiauzzi E., Pujol L.a., Wood M., Bond K., Black R., Yiu E., Zacharoff K. painACTION-back pain: a self-management website for people with chronic back pain. Pain Med. 2010;11:1044–1058. doi: 10.1111/j.1526-4637.2010.00879.x. [DOI] [PubMed] [Google Scholar]
- Cottrell C., Drew J., Gibson J., Holroyd K., O'Donnell F. Feasibility assessment of telephone-administered behavioral treatment for adolescent migraine. Headache. 2007;47:1293–1302. doi: 10.1111/j.1526-4610.2007.00804.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Boer M.J., Versteegen G.J., Vermeulen K.M., Sanderman R., Struys M.M.R.F. A randomized controlled trial of an internet-based cognitive-behavioural intervention for non-specific chronic pain: an effectiveness and cost-effectiveness study. Eur. J. Pain (United Kingdom) 2014:1–12. doi: 10.1002/ejp.509. [DOI] [PubMed] [Google Scholar]
- Dear B.F., Titov N., Nicholson K., Johnston L., Wootton B.M., Terides M.D., Rapee R.M., Hudson J.L. The pain course: a randomised controlled trial of a clinician-guided internet-delivered cognitive behaviour therapy program for managing chronic pain and emotional well-being. Pain. 2013;154:942–950. doi: 10.1016/j.pain.2013.03.005. [DOI] [PubMed] [Google Scholar]
- Del Pozo-Cruz B., Parraca J.a., Del Pozo-Cruz J., Adsuar J.C., Hill J.C., Gusi N. An occupational, internet-based intervention to prevent chronicity in subacute lower back pain: a randomized controlled trial. J. Rehabil. Med. 2012;44:581–587. doi: 10.2340/16501977-0988. [DOI] [PubMed] [Google Scholar]
- Devineni T., Blanchard E.B. A randomized controlled trial of an internet-based treatment for chronic headache. Behav. Res. Ther. 2005;43:277–292. doi: 10.1016/j.brat.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Eccleston C., Williams A.C.d.C., Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst. Rev. 2013 doi: 10.1002/14651858.CD007407.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccleston C., Fisher E., Craig L., Duggan G.B., Rosser B.A., Keogh E. Psychological therapies (internet-delivered) for the management of chronic pain in adults. Cochrane database Syst. Rev. 2014;2 doi: 10.1002/14651858.CD010152.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M., Davey Smith G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fales J., Palermo T.M., Law E.F., Wilson A.C. Sleep outcomes in youth with chronic pain participating in a randomized controlled trial of online cognitive-behavioral therapy for pain management. Behav. Sleep Med. 2014;13:37–41. doi: 10.1080/15402002.2013.845779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hann K.E.J., McCracken L.M. A systematic review of randomized controlled trials of acceptance and commitment therapy for adults with chronic pain: outcome domains, design quality, and efficacy. J. Context. Behav. Sci. 2014;3:1–39. [Google Scholar]
- Hayes S., Hogan M., Dowd H., Doherty E., O′Higgins S., Nic Gabhainn S., MacNeela P., Murphy A.W., Kropmans T., ONeill C., Newell J., McGuire B.E. Comparing the clinical-effectiveness and cost-effectiveness of an internet-delivered Acceptance and Commitment Therapy (ACT) intervention with a waiting list control among adults with chronic pain: study protocol for a randomised controlled trial. BMJ Open. 2014;2 doi: 10.1136/bmjopen-2014-005092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedborg K., Muhr C. Multimodal behavioral treatment of migraine: an internet-administered, randomized, controlled trial. Ups. J. Med. Sci. 2011;116:169–186. doi: 10.3109/03009734.2011.575963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks C.L., von Baeyer C.L., McGrath P.J. Online psychological treatment for pediatric recurrent pain: a randomized evaluation. J. Pediatr. Psychol. 2006;31:724–736. doi: 10.1093/jpepsy/jsj065. [DOI] [PubMed] [Google Scholar]
- Higgins J.P.T., Altman D.G., Gotzsche P.C., Juni P., Moher D., Oxman a.D., Savovic J., Schulz K.F., Weeks L., Sterne J.a.C. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irvine A.B., Russell H., Manocchia M., Mino D.E., Cox Glassen T., Morgan R., Gau J.M., Birney A.J., Ary D.V. Mobile-web app to self-manage low back pain: randomized controlled trial. J. Med. Internet Res. 2015;17 doi: 10.2196/jmir.3130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristjánsdóttir Ó.B., Fors E.A., Eide E., Finset A., van Dulmen S., Wigers S.H., Eide H., Dulmen S.V., Wigers S.H., Eide H. Written online situational feedback via mobile phone to support self-management of chronic widespread pain: a usability study of a web-based intervention. BMC Musculoskelet. Disord. 2011;12:51. doi: 10.1186/1471-2474-12-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristjánsdóttir Ó.B., Fors E.a., Eide E., Finset A., Stensrud T.L., Van Dulmen S., Hørven Wigers S., Eide H. A smartphone-based intervention with diaries and therapist-feedback to reduce catastrophizing and increase functioning in women with chronic widespread pain: randomized controlled trial. J. Med. Internet Res. 2013;15:1–28. doi: 10.2196/jmir.2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristjánsdóttir Ó.B., Fors E.A., Eide E., Finset A., Stensrud T.L., van Dulmen S., Wigers S.H., Eide H. A smartphone-based intervention with diaries and therapist feedback to reduce catastrophizing and increase functioning in women with chronic widespread pain. part 2: 11-month follow-up results of a randomized trial. J. Med. Internet Res. 2013;15:e72. doi: 10.2196/jmir.2442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J., Lüking M., Ebert D.D., Buhrman M., Andersson G., Baumeister H. Effectiveness and cost-effectiveness of a guided and unguided internet-based acceptance and commitment therapy for chronic pain: study protocol for a three-armed randomised controlled trial. Internet Interv. 2014;2:7–16. [Google Scholar]
- Linton S.J., Bergbom S. Understanding the link between depression and pain. Scand. J. Pain. 2011;2:47–54. doi: 10.1016/j.sjpain.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Ljótsson B., Atterlöf E., Lagerlöf M., Andersson E., Jernelöv S., Hedman E., Kemani M., Wicksell R.K. Internet-delivered acceptance and values-based exposure treatment for fibromyalgia: a pilot study. Cogn. Behav. Ther. 2014;43:93–104. doi: 10.1080/16506073.2013.846401. [DOI] [PubMed] [Google Scholar]
- Lorig K.R., Laurent D.D., Deyo R.a., Marnell M.E., Minor M.a., Ritter P.L. Can a back pain e-mail discussion group improve health status and lower health care costs?: a randomized study. Arch. Intern. Med. 2002;162:792–796. doi: 10.1001/archinte.162.7.792. [DOI] [PubMed] [Google Scholar]
- Lorig K.R., Ritter P.L., Laurent D.D., Plant K. The internet-based arthritis self-management program: a one-year randomized trial for patients with arthritis or fibromyalgia. Arthritis Care Res. 2008;59:1009–1017. doi: 10.1002/art.23817. [DOI] [PubMed] [Google Scholar]
- Macea D.D., Gajos K., Daglia A. The efficacy of web-based cognitive behavioral interventions for chronic pain: a systematic review and meta-analysis. J. Pain. 2010;11:917–929. doi: 10.1016/j.jpain.2010.06.005. [DOI] [PubMed] [Google Scholar]
- Marks I.M., Cuijpers P., Cavanagh K., van Straten A., Gega L., Andersson G. Meta-analysis of computer-aided psychotherapy: problems and partial solutions. Cogn. Behav. Ther. 2009;38:83–90. doi: 10.1080/16506070802675239. [DOI] [PubMed] [Google Scholar]
- Melville K.M., Casey L.M., Kavanagh D.J. Dropout from internet-based treatment for psychological disorders. Br. J. Clin. Psychol. 2010;49:455–471. doi: 10.1348/014466509X472138. [DOI] [PubMed] [Google Scholar]
- Palermo T.M., Wilson A.C., Peters M., Lewandowski A., Somhegyi H. Randomized controlled trial of an internet-delivered family cognitive-behavioral therapy intervention for children and adolescents with chronic pain. Pain. 2009;146:205–213. doi: 10.1016/j.pain.2009.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid K.J., Harker J., Bala M.M., Truyers C., Kellen E., Bekkering G.E., Kleijnen J. Epidemiology of chronic non-cancer pain in Europe: narrative review of prevalence, pain treatments and pain impact. Curr. Med. Res. Opin. 2011;27:449–462. doi: 10.1185/03007995.2010.545813. [DOI] [PubMed] [Google Scholar]
- Rosser B.a., Eccleston C. Smartphone applications for pain management. J. Telemed. Telecare. 2011;17:308–312. doi: 10.1258/jtt.2011.101102. [DOI] [PubMed] [Google Scholar]
- Rozental A., Andersson G., Boettcher J., Ebert D.D., Cuijpers P., Knaevelsrud C., Ljótsson B., Kaldo V., Titov N., Carlbring P. Consensus statement on defining and measuring negative effects of internet interventions. Internet Interv. 2014;1:12–19. [Google Scholar]
- Ruehlman L.S., Karoly P., Enders C. A randomized controlled evaluation of an online chronic pain self management program. Pain. 2012;153:319–330. doi: 10.1016/j.pain.2011.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ström L., Pettersson R., Andersson G. A controlled trial of self-help treatment of recurrent headache conducted via the internet. J. Consult. Clin. Psychol. 2000;68:722–727. [PubMed] [Google Scholar]
- Trompetter H.R., Bohlmeijer E.T., Veehof M.M., Schreurs K.M.G. Internet-based guided self-help intervention for chronic pain based on acceptance and commitment therapy: a randomized controlled trial. J. Behav. Med. 2015;66–80 doi: 10.1007/s10865-014-9579-0. [DOI] [PubMed] [Google Scholar]
- Turner J.A.J.A., Jensen M.P.M.P., Romano J.M.J.M. Do beliefs, coping, and catastrophizing independently predict functioning in patients with chronic pain? Pain. 2000;85:115–125. doi: 10.1016/s0304-3959(99)00259-6. [DOI] [PubMed] [Google Scholar]
- Wallace L.S., Dhingra L.K. A systematic review of smartphone applications for chronic pain available for download in the United States. J. Opioid Manag. 2014;10:63–68. doi: 10.5055/jom.2014.0193. [DOI] [PubMed] [Google Scholar]
- Williams D.A., Kuper D., Segar M., Mohan N., Sheth M., Clauw D.J. Internet-enhanced management of fibromyalgia : a randomized controlled trial. Pain. 2010;151:694–702. doi: 10.1016/j.pain.2010.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]