Abstract
The aim of this pilot study was to examine if a personalized web-based multi-platform nutrition, exercise, and lifestyle coaching program, supported weight loss and the reduction of chronic disease risk factors in overweight or obese women. Twenty-eight women completed the program, which represented 50% of those who provided baseline data. The program consisted of a one-year curriculum with daily exercise, nutritional habits, and health behaviour lessons along with access to a one-on-one coach. The workouts, habits, and lessons were available via computer, tablet, and mobile device which, along with coaching, facilitated self-monitoring and accountability. At baseline and 12-months, weight, waist circumference, fat mass, muscle mass, blood pressure, total cholesterol, low density lipoproteins, high density lipoproteins, triglycerides, C reactive protein, and fasting glucose were collected. Over the 12 months, women who completed the program, (average age 49.64 (SD 10.99) years), lost 16.52 (SD 13.63) lbs (P < 0.001), and reduced waist circumference by 3.56 (SD 2.31) in (P < 0.0001). Diastolic blood pressure decreased by 3.77 (SD 7.25) mm Hg (P = 0.02) and high density lipoproteins increased by 0.16 (SD 0.28) mmol/L (P = 0.01). No other risk factors changed significantly. Compliance was a significant predictor of weight loss (P < 0.01). In conclusion, women who completed the web-based program experienced significant weight loss (8.62% of initial body weight) coming predominantly from body fat. Chronic disease risk factors also improved.
Keywords: Physical activity, Internet, Intervention, Weight loss, Behaviour change, Nutrition
Highlights
-
•
We examined the effects of a web-based intervention on weight loss in overweight or obese women.
-
•
Study completers experienced weight loss and saw an improvement in disease-related risk factors.
-
•
Women who reported greater program compliance experienced greater weight loss.
1. Introduction
Overweight and obesity are universally recognized as a risk factor for numerous health conditions such as type 2 diabetes, hypertension, some types of cancer, cardiovascular disease, poor quality of life, functional limitations, and mental health concerns (Dixon, 2010, Luo et al., 2007). Although it is well established that a reduction in weight of 5–10% substantially decreases the risk of morbidity and premature mortality (Obes. Res., 1998, Mokdad et al., 2003, Poirier et al., 2006), adherence to weight loss interventions is generally poor (Coons et al., 2012). Consequently, a reduction in obesity and/or obesity-related health conditions remains a serious challenge, in particular to primary care providers who receive limited training and support in obesity management but who are expected to counsel and treat the condition (Flodgren et al., 2010).
Multi-platform interventions, which are web-based and can be accessed on a mobile device, a tablet, and/or a computer, may present a promising opportunity to provide innovative, engaging, and effective support to adults seeking assistance with obesity management when developed using best practice recommendations and evidence. These types of interventions have the ability to reach individuals world-wide, including those in rural or remote locations or those with transportation limitations, provide support that is convenient and accessible 24-hours per day, offer multiple options for peer and health professional support, and be offered at a low cost (Neve et al., 2010, PWC, 2012).
Although there is evidence to suggest that interventions based on the web are successful in promoting weight loss, well-designed and evaluated weight loss interventions of this nature are sparse (Coons et al., 2012, Neve et al., 2010). Further, many of the interventions evaluated to date fail to include all of the key components associated with successful weight loss and weight loss maintenance, which include self-monitoring (e.g., nutrition, exercise, specific habits), goal-setting, behaviour change psychology, access to coaching from a health professional (including regular tailored feedback), a multi-component approach (including dietary counselling, exercise and healthy lifestyle habit promotion, and behaviour change), utilization of multiple channels to deliver messages (such as email, social media, discussion forum), and an adequate duration (minimum six months in length) (Coons et al., 2012, Neve et al., 2010, Kirk et al., 2012, Korda and Itani, 2013). Thus, evidence of the effectiveness of a comprehensive, web-based and multi-platform weight loss intervention is needed. Assessing the effectiveness of programs like this is imperative as it would be a logical and feasible method of reaching adults worldwide who struggle with weight management. Additionally, if demonstrated effective in the reduction of morbidity and mortality, a web-based multi-platform intervention would provide primary care providers with a safe and accessible treatment option for their patients.
The aim of this pilot study was to examine the changes after a web-based multi-platform nutrition, exercise, and lifestyle coaching program in anthropometrics and body composition (weight, waist circumference, body fat mass, muscle mass), blood pressure, and blood chemistry (total cholesterol, low density lipoprotein (LDL), high density lipoproteins (HDL), triglycerides, C reactive protein (CRP), fasting glucose) of overweight or obese adults. This program was one year in duration and included detailed exercise programming, progressive nutritional habits, daily lessons utilizing behaviour change psychology, and one-on-one coaching to achieve individualized goals.
2. Methods
2.1. Participants
During June and July of 2014, adults aged 18–65 years living in British Columbia, Canada with a Body Mass Index (BMI) > 24.9 kg/m2 were recruited from Festubert Family Practice in Duncan, British Columbia by a primary care physician. Inclusion criteria were as follows: men and women aged 18–65 years of age with a BMI > 24.9 kg/m2, daily access to the Internet, basic fitness equipment or access to a fitness facility, and the ability to participate in moderate-to-vigorous physical activity. Individuals were excluded if inclusion criteria were not met as well as females who were pregnant or wanting to become pregnant over the course of the study period, and an inability to communicate in English. Ethical approval was obtained from Quorum Review IRB; one of the largest independent review boards providing ethics review to the human clinical trials industry.
2.2. Study design
This study utilized an observational design to explore whether a web-based multi-platform nutrition, exercise, and lifestyle coaching program resulted in changes to anthropometrics and body composition, blood pressure, and blood chemistry in overweight or obese adults. Potential participants were identified by a chart review completed by a primary care physician and then approached via phone call or during a regular appointment. After being identified, each participant completed a brief questionnaire to screen for conditions that would limit his or her ability to safely participate in moderate-to-vigorous physical activity or commit to a year-long program (e.g., Do you currently have any injuries that might restrict or limit your ability to work out?). If a limiting condition was identified, the participant was not invited to participate further. At the baseline measurement session, each participant met with the physician to ensure there were no contraindications to participation in the program. Informed consent was obtained from each participant after a full explanation of the study was provided by the primary care physician.
All eligible participants were enrolled in the one-year web-based multi-platform Precision Nutrition Coaching Program. This included two study visits (baseline and 12 months) to obtain anthropometric and body composition measurements, blood pressure, and fasting blood work. Participants also completed an online demographics and medical history questionnaire at baseline and 12 months. The Precision Nutrition Coaching Program is a commercially available program. Participants were charged a monthly fee to be involved.
Both men and women were recruited to participate in this study (n = 9 and n = 68, respectively) however, only 3 men completed the one-year program (Fig. 1). Therefore, only women were included in the analysis. Twelve participants were lost between recruitment and baseline due to the identification of a limiting condition (i.e., an injury that would prevent participation in moderate-to-vigorous physical activity) or acknowledgement that commitment to a one-year program was not feasible. Participants who formally opted out of the program (n = 15) indicated the following reasons for leaving: 1) the program was not working for them, 2) no reason, 3) health-related reasons, 4) too busy, 5) were not following the program. Twenty-eight women completed the full 12-month program and provided follow-up data.
Fig. 1.
Participant flow chart.
2.3. Intervention
The Precision Nutrition Coaching Program curriculum consists of three main components: 1) an exercise program, 2) daily nutritional habits, and 3) daily health behaviour lessons. Participants were provided with individual login information and were able to access the complete program via desktop/laptop computer, tablet, or mobile phone (http://www.precisionnutrition.com/). See Fig. 2 for screen shots of the program and Table 1 for program details. Each day, participants recorded whether or not they completed the workout and habit, which was used to determine program compliance (program compliance = (total number of days that both the habit and workout were completed/total number of days in the full program)∗ 100%). Additionally, participants had access to a coach, a certified health and fitness professional trained in motivational interviewing techniques, who provided tailored advice. Each participant received two team messages per month and one individual message approximately every three weeks from the coach. The coach also created a private forum on a social media site (i.e., Facebook) to enable participants to communicate with each other. Participants were encouraged to reach out to the coach as needed for further support.
Fig. 2.
Screen shots of the online Precision Nutrition Coaching Program.
Table 1.
Description of the Precision Nutrition Coaching Program curriculum.
| Section | Details |
|---|---|
| Home page | The landing page for the Precision Nutrition Coaching Program, presents personalized information, access to all aspects of the program including progress reports, daily workout and lesson, compliance scores, coach contact information, and archived information from previous days. |
| Daily exercise | An overview of the entire workout phase is available in a downloadable document, along with an overview of the workout for the day, detailed written instructions about each exercise in the workout, and access to online videos of each exercise. Written modifications for each exercise are provided so participants with movement or equipment limitations could safely complete the workout. |
| Daily lesson / habit | Each day a written and audio version of the lesson is available. Assignments associated with the lesson are also accessed from the page. Habits, which change every 2 weeks, are also displayed here. The daily lesson compliments the nutritional habit being worked on. |
| Progress report | Access to progress related to completion of daily habits, workouts, and assignments are provided along with changes in weight, girth measurements, and photos. |
| Discussion forum (i.e. Facebook group) | Access to posts and threads from the coach and team, a blog, recommended books, coaching chats, and Precision Nutrition related information are provided on this page. |
| Coach contact | This page provides the opportunity to connect privately with your designated coach. |
| Your info | Access to your individual profile, and settings are available here. |
The exercise program (Table 1) consisted of a detailed daily workout that progressed in intensity over time; the year was divided into 11 phases that were 4–6 weeks in duration. Each workout session began with a warm-up and then moved into the main exercise portion. Each week included two days of cardiovascular interval training, three days of weight training, one day of active recovery (e.g., walking), and one day of complete rest.
Nutritional modifications were made through the practice of health habits, which were designed to gradually introduce change. Participants focused on a specific nutritional habit for a two-week period. For example, one nutritional habit was to eat at least five servings of vegetables each day. The daily lessons compliment the nutritional habits by providing participants with tools and/or information to follow the habit while also explaining why the habit is important. For example, a lesson on food preparation and storage (with a focus on vegetables) would complement the habit of consuming at least five servings of vegetables each day. Often, daily lessons included short written assignments to encourage participants to apply the lesson to their own situation. The lessons utilize principles of cognitive behavioural therapy for optimal behaviour change.
2.4. Measurements
2.4.1. Questionnaire
Participants completed an online questionnaire (made available through their personal login on the intervention website) at baseline and 12 months that included demographic information, medical history, medication use, injury history, exercise habits, dietary habits, allergy information, and goals related to health and fitness.
2.4.2. Anthropometric and body composition measurements
Height was measured using a stadiometer and body weight using a calibrated, digital scale (Seca 876 scale, Seca corporation, Hamburg Germany). BMI was calculated by dividing weight(kg)/height(m)2. Body girth measurements including neck, shoulder, chest, arm, waist, hip, and calf were taken using a research grade measuring tape and were completed as per the Canadian Physical Activity, Fitness, & Lifestyle Approach procedure manual (CSEP, 2003). On a weekly basis, participants also self-reported their weight and waist circumference and were given detailed instructions from the procedure manual to follow. Total girth was calculated by summing all measurements and was used in the analysis. Body fat mass (lbs) and muscle mass (lbs) was determined using the Inbody R20 Bioelectrical Impedance Analyzer device (Dolezal et al., 2013). All anthropometric and body composition measurements were taken by a trained professional at baseline and 12 months while participants were shoeless and wearing light clothing.
2.4.3. Blood pressure
Blood pressure was taken with participants seated comfortably with feet flat on the floor by a trained professional at baseline and 12 months. An automated BPI device (Omron HEM 907XL IntelliSense Professional Digital Blood Pressure Monitor, Omron, Kyoto Japan) was used. This device takes three consecutive measures 1 min apart (after a two-minute waiting period prior to the first measurement) and then takes an average.
2.4.4. Blood chemistry
Blood chemistry (total cholesterol, LDL, HDL, triglycerides, CRP, fasting glucose) was conducted at LifeLabs by a trained technician at baseline and 12 months. Participants were required to fast for at least 8 h prior to having blood work completed. Standard laboratory protocols were employed to acquire blood chemistry values (LifeLabs® Medical Laboratory Services, www.lifelabs.com).
2.4.5. Statistics
All analyses were performed using SAS version 9.4 (Release 9.4 Cary, NC; SAS Institute Inc.). Baseline characteristics of the study population were calculated using the means procedure and described as mean (standard deviation (SD)). Independent sample t-tests were used to compare the baseline measures between study completers (i.e., those who completed both the baseline and 12-month data collection) and non-completers (i.e., those who completed baseline data collection but not 12-month data collection). For study completers (n = 28), baseline and 12 month repeated measures, including weight, waist circumference, body fat mass, muscle mass, blood pressure (systolic and diastolic), total cholesterol, LDL, HDL, triglycerides, CRP, and fasting glucose, were compared using paired sample t-tests. Bivariate regressions were completed to look at the relationship between weight change and compliance. Age was initially included in the model as a confounding variable however, since it was not a significant contributor (P > 0.1) to the model and did not significantly change the magnitude of the relationship between weight change and compliance, it was removed.
3. Results
Participant characteristics are shown in Table 2. Women who enrolled in the study were on average aged 49.64 (SD 10.99) years with a waist circumference of 40.49 (SD 5.14) in. In general, women had blood pressure and blood chemistry values that fall within healthy ranges (Table 2). Women defined as non-completers had a higher baseline weight, fat mass, and muscle mass and were also younger compared to women who completed the study (Table 3).
Table 2.
Baseline and 12 month measures for participants who completed the program.
| N | Baseline (Mean (SD)) | 12 Months (Mean (SD)) | |
|---|---|---|---|
| Demographics | |||
| Age (years) | 28 | 49.64 (10.99) | – |
| Height (cm) | 28 | 164.30 (2.58) | – |
| Weight (lbs)a | 28 | 191.67 (36.84) | 175.15 (31.39) |
| Anthropometrics and body composition | |||
| BMI (kg/m2) | 27 | 32.20 (6.70) | 31.23 (10.68) |
| Waist circumference (in)a | 28 | 40.49 (5.14) | 36.93 (5.01) |
| Total girth (in)a | 28 | 241.52 (21.88) | 228.34 (21.20) |
| Fat mass (lbs)b | 27 | 73.23 (29.49) | 61.43 (28.40) |
| Muscle mass (lbs) | 27 | 63.49 (9.44) | 62.61 (6.80) |
| Blood pressure | |||
| Systolic (mmHg) | 27 | 120.31 (14.18) | 117.26 (11.18) |
| Diastolic (mmHg)b | 27 | 74.14 (8.49) | 70.37 (10.37) |
| Blood chemistry | |||
| Total cholesterol (mmol/L) | 27 | 5.00 (1.00) | 5.04 (0.99) |
| HDL cholesterol (mmol/L)b | 27 | 1.51 (0.40) | 1.67 (0.47) |
| LDL cholesterol (mmol/L) | 26 | 2.87 (0.72) | 2.84 (0.78) |
| Triglycerides (mmol/L) | 27 | 1.36 (0.85) | 1.43 (1.74) |
| CRP (μmol/L) | 24 | 3.41 (6.37) | 2.77 (5.79) |
| Fasting glucose (mmol/L) | 27 | 5.70 (1.55) | 5.46 (0.80) |
BMI – Body Mass Index, HDL – High Density Lipoprotein, LDL – Low Density Lipoprotein, CRP – C Reactive Protein, SD – Standard Deviation.
Denotes significant difference between baseline and 12-month measure (P < 0.0001).
Denotes significant difference between baseline and 12-month measure (P < 0.05).
Table 3.
Baseline comparison between study completers and non-completers.
| N | Completers (Mean (SD)) | N | Non-completers (Mean (SD)) | |
|---|---|---|---|---|
| Demographics | ||||
| Age (years)a | 28 | 49.64 (10.99) | 28 | 44.17 (9.88) |
| Height (cm) | 28 | 164.30 (2.58) | 28 | 167.3 (5.54) |
| Weight (lbs)a | 28 | 191.67 (36.84) | 28 | 216.4 (47.61) |
| Anthropometrics and body composition | ||||
| BMI (kg/m2) | 27 | 32.20 (6.70) | 28 | 34.98 (6.91) |
| Waist circumference (in) | 28 | 40.49 (5.14) | 28 | 42.70 (5.93) |
| Total girth (in) | 28 | 241.52 (21.88) | 28 | 253.30 (24.86) |
| Fat mass (lbs)a | 27 | 73.23 (29.49) | 28 | 93.47 (34.66) |
| Muscle mass (lbs)a | 27 | 63.49 (9.44) | 28 | 69.04 (9.82) |
| Blood pressure | ||||
| Systolic (mmHg) | 27 | 120.31 (14.18) | 28 | 118.60 (12.49) |
| Diastolic (mmHg) | 27 | 74.14 (8.49) | 28 | 75.21 (7.47) |
| Blood chemistry | ||||
| Total cholesterol (mmol/L) | 27 | 5.00 (1.00) | 26 | 5.03 (0.91) |
| HDL cholesterol (mmol/L) | 27 | 1.51 (0.40) | 28 | 1.47 (0.37) |
| LDL cholesterol (mmol/L) | 26 | 2.87 (0.72) | 28 | 3.12 (0.92) |
| Triglycerides (mmol/L) | 27 | 1.36 (0.85) | 27 | 1.30 (0.48) |
| CRP (μmol/L) | 24 | 3.41 (6.37) | 27 | 5.57 (7.12) |
| Fasting glucose (mmol/L) | 27 | 5.70 (1.55) | 28 | 5.22 (0.35) |
Denotes significant difference between completers and non-completers (P < 0.05).
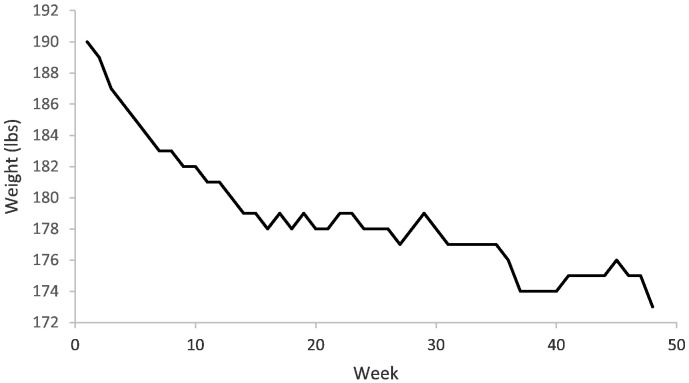
Women who completed the program lost an average of 16.52 (SD 13.63) lbs of weight (P < 0.001) or experienced an 8.62 (SD 5.84) % weight loss over 12 months, which was largely attributable to the loss of fat mass (P = 0.03), not muscle mass (P = 0.64; Table 2). Fig. 3 depicts the weight loss trajectory experienced by participants over the 12-month period. Consequent to the loss in weight was a 3.56 (SD 2.31) in reduction in waist circumference (P < 0.0001). Fig. 4 shows the change in weight and waist circumference experienced by each individual participant. There was a significant reduction in diastolic blood pressure of 3.77 (SD 7.25) mm Hg (P = 0.02) and increase in HDL cholesterol of 0.16 (SD 0.28) mmol/L (P = 0.01) however no other markers changed significantly (Table 2).
Fig. 3.
Weight loss trajectory over the 12-month Precision Nutrition Coaching Program for those participants who completed the full program.
Fig. 4.
A change in (Δ) weight and B Change in (Δ) waist circumference (WC) by individual participant over the 12-month Precision Nutrition Coaching Program.
Compliance in the study completers was 77.5 (SD 22.6) % and was a significant negative predictor of weight change (parameter estimate − 0.28731, P < 0.01). Stated differently, women who reported greater compliance experienced greater weight loss.
No serious adverse events attributable to weight loss or study participation were reported during the 12-month program.
4. Discussion
4.1. Principle findings
The primary finding of this study was that women who completed The Precision Nutrition Coaching Program, a web-based multi-platform nutrition, exercise, and lifestyle coaching program for weight management, experienced significant weight loss (between 5 and 10%) coming predominantly from body fat. This finding supports the guidelines that suggest weight management interventions be multi-faceted and include self-monitoring, goal setting, behaviour change psychology, and coaching from a health professional (including regular tailored feedback).
To our knowledge, this study describes the first web-based multi-platform program to incorporate all key components suggested in systematic reviews to be included in weight management programs (Coons et al., 2012, Neve et al., 2010, Kirk et al., 2012, Korda and Itani, 2013). Specifically, this program was one year in duration and included detailed exercise programming, progressive nutritional habits, daily lessons utilizing behaviour change psychology, self-monitoring, goal setting, multiple communication platforms, and one-on-one coaching to achieve individualized goals. According to a group of primary care providers, this online program also meets almost all features of an ideal online weight loss program; it has a structured curriculum, goal-setting assistance, self-monitoring tools, psychologically oriented content, peer support, and reports (Hwang et al., 2012).
4.2. Comparisons with prior work
In this study, issues commonly reported in the literature were also noted, particularly the high rate of attrition at 12 months; approximately 50% of the participants recruited at baseline completed the full program. In a review of technology interventions to curb obesity, Coons et al. (Coons et al., 2012) reported attrition rates ranging from 25 to 43% whereas Rao et al. (Rao et al., 2011) reported attrition rates of 20 to 80% in their review of emerging weight management strategies. As well, despite 9 men agreeing to participate (compared to 68 women) only 3 finished the study. Similarly, other studies report a much higher percentage of women enrolling in both technology-based and face-to-face weight management programs (Neve et al., 2010, Finkelstein and Kruger, 2014, Jebb et al., 2011). This indicates a service gap and begs further exploration as approximately 30% of men in North America are classified as being obese (Flegal et al., 2012, Twells et al., 2014) and at risk of or exhibiting obesity-related health complications.
Despite the high attrition rate, women who completed 12 months of this program lost between 5 and 10% of their initial body weight, the percentage weight loss recommended for significant reductions in morbidity and mortality (Obes. Res., 1998, Mokdad et al., 2003, Poirier et al., 2006). More importantly, this loss in body weight consisted primarily of fat loss and not muscle loss. Loss of fat mass, particularly that in the abdominal region (indicated by waist circumference in this study) is associated with substantive reductions in cardiovascular risk factors (Ross et al., 2004) whereas loss of muscle mass is unfavourable as it is the most significant contributor to basal metabolic rate and consequently, its loss may be associated with reduced metabolism (Elisa, 1992).
In this study, individuals reporting the highest compliance with daily habits and exercise experienced the greatest weight loss. This is not surprising given prior reports stating the association between weight loss and compliance with an online intervention (Neve et al., 2010, Thomas et al., 2015). Due to the variability in the definition of compliance with a web- or phone-based intervention, it is difficult to compare results across studies. However, in general, compliance is low (Neve et al., 2010). For example, Thomas et al. (Thomas et al., 2015) found that participants recorded their activities on the website on at least 5 days of the week for only 6.7 weeks of the 12-week program.
Compliance aside, in this study, women progressively lost body weight, maintaining a lower body mass for the full duration of the program (Fig. 3). Unlike the weight loss trajectory seen in this study, it is more common for participants in other interventions to lose weight for the first 3 to 6 months and then gradually regain weight as time goes on (Butryn et al., 2011).
Although we detected few significant changes in the health indicators collected for this study, many of the women presented with baseline values that fell within normal healthy ranges. Thus, it was not surprising that we detected little improvements at follow up. However, it is noteworthy that the changes detected in diastolic blood pressure, HDL, and waist circumference may confer significant reductions in disease risk. For example, Cook et al. (Cook et al., 1995) reported that, in the general population, a 2 mm Hg reduction in diastolic blood pressure, which is comparable to the change detected in this study, could decrease the number of coronary heart disease events by 6%. Another investigation suggested that for every 0.025 mmol/L increase in HDL there is a 5% reduction of cardiovascular disease risk in men (Gordon et al., 1986). While this is not directly comparable to our female program participants, it can be inferred that the women in this study would experience substantial health benefit. Finally, it has been reported that reductions in abdominal obesity are associated with significant improvements in cardiometabolic risk factors (Janiszewski et al., 2008), suggesting that positive health changes may also be detected due to the decrease in waist circumference noted in participants of this study. It is important to note that, with increasing numbers of risk factors present, individuals experience a step-wise increase in risk for cardiovascular disease or coronary heart disease mortality (Malik et al., 2004, McNeill et al., 2005). Additionally, there is some evidence to suggest that specific chronic disease risk factors, such as hypertension and HDL cholesterol, confer greater risk for cardiovascular disease compared to other chronic disease risk factors, such as triglycerides (McNeill et al., 2005, Alexander et al., 2003, Hunt et al., 2004), however a reduction in any one (or multiple) chronic disease risk factor would impart meaningful health benefit to an individual.
Recent evidence suggests that participants who complete a commercial weight loss program lose more weight compared to those receiving standard weight management support in a primary care setting (5.06 kg versus 2.25 kg, respectively) (Jebb et al., 2011). Reasons for this could be that primary care providers often do not receive substantial training and support in weight management, often do not have sufficient clinic time to address a complex issue such as weight management, and perceive an inability to change patient behaviour (Jay et al., 2008, Kushner, 1995, Maheux et al., 1987). Another recent systematic review and meta-analysis of 23 studies (9632 participants) exploring self-help weight loss programs concluded that there was no significant weight loss at 12 months (Hartmann-Boyce et al., 2015). These findings, combined with the evidence illustrating the enormous health risk and economic burden associated with obesity (An, 2015) point to the need for widely available and effective weight management programs for primary care providers to refer their patients to.
4.3. Limitations
There are limitations with this study. First, this study was observational in nature and did not include a standard care control group. Thus, we are not able to determine causality. We also noted significant attrition. Further, generalizability of our results are limited as the population studied is a small sample of middle-aged, female Caucasian patients from one city. Longitudinal studies and randomized controlled trials in heterogeneous populations are needed to corroborate our findings and further examine the utility of web-based multi-platform interventions. Despite these limitations, our study lends support for the use of web-based multi-platform weight management interventions following published recommendations and guidelines.
4.4. Conclusion
Participation in the web-based multi-platform nutrition, exercise, and lifestyle coaching program for weight management, can support middle-aged women in experiencing significant weight loss and reducing disease-related risk factors. Thus, this intervention may be a viable treatment option for individuals who are seeking support with weight management and who have similar characteristics to those in this pilot study.
Abbreviations
- BMI
Body mass index
- CRP
C Reactive Protein
- HDL
High density lipoprotein
- LDL
Low density lipoprotein
- SD
Standard deviation
- WC
waist circumference
Authors' contributions
MW, JMB and MH conceived and designed the study; MH and MW collected data; MH analyzed the data; KAM wrote manuscript draft; MH and KAM interpreted results; all authors revised, and approved the manuscript.
Conflict of interest
Authors declare financial support for submitted work by Precision Nutrition. Authors MH and JMB declare receiving salary from Precision Nutrition. Precision Nutrition is a commercial company.
Acknowledgements
This work was supported by Precision Nutrition.
References
- Alexander C.M., Landsman P.B., Teutsch S.M., Haffner S.M., Third National H., Nutrition Examination S., National Cholesterol Education P NCEP-defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older. Diabetes. 2003;52:1210–1214. doi: 10.2337/diabetes.52.5.1210. (PMID: 12716754) [DOI] [PubMed] [Google Scholar]
- An R. Health care expenses in relation to obesity and smoking among U.S. adults by gender, race/ethnicity, and age group: 1998–2011. Public Health. 2015;129:29–36. doi: 10.1016/j.puhe.2014.11.003. [DOI] [PubMed] [Google Scholar]
- Butryn M.L., Webb V., Wadden T.A. Behavioral treatment of obesity. Psychiatr. Clin. North Am. 2011;34:841–859. doi: 10.1016/j.psc.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults–the evidence report. National Institutes of HealthObes. Res. 1998;6(Suppl. 2):51S–209S. (PMID: 9813653) [PubMed] [Google Scholar]
- Cook N.R., Cohen J., Hebert P.R., Taylor J.O., Hennekens C.H. Implications of small reductions in diastolic blood pressure for primary prevention. Arch. Intern. Med. 1995;155:701–709. (PMID: 7695458) [PubMed] [Google Scholar]
- Coons M.J., Demott A., Buscemi J., Duncan J.M., Pellegrini C.A., Steglitz J., Pictor A., Spring B. Technology interventions to curb obesity: a systematic review of the current literature. Curr. Cardiovasc. Risk Rep. 2012;6:120–134. doi: 10.1007/s12170-012-0222-8. (PMID: 3471367) [DOI] [PMC free article] [PubMed] [Google Scholar]
- CSEP . Health Canada; Ottawa, Ontario: 2003. The Canadian Physical Activity, Fitness & Lifestyle Approach —- Third Edition. (ISBN: 1–896900-16-X) [Google Scholar]
- Dixon J.B. The effect of obesity on health outcomes. Mol. Cell. Endocrinol. 2010;316:104–108. doi: 10.1016/j.mce.2009.07.008. [DOI] [PubMed] [Google Scholar]
- Dolezal B.A., Lau M.J., Abrazada M., Storer T.W., Cooper C.B. Validity of two commercial grade bioelectrical impedance analyzers for measurement of body fat percentage. JEP Online. 2013;16:74–83. [Google Scholar]
- Elisa M. Energy expenditure in the whole body. In: Kinney J.T., editor. Energy Metabolism: Tissue Determinants and Cellular Corollaries. New York; Raven Press: 1992. pp. 19–60. (ISBN: 0–88167–871-6) [Google Scholar]
- Finkelstein E.A., Kruger E. Meta- and cost-effectiveness analysis of commercial weight loss strategies. Obesity. 2014;22:1942–1951. doi: 10.1002/oby.20824. [DOI] [PubMed] [Google Scholar]
- Flegal K.M., Carroll M.D., Kit B.K., Ogden C.L. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- Flodgren G., Dickinson H.O., Kirk S.F., Alberti H., Beyer F.R., Brown J.G., Penney T.L., Summerbell C.D., Eccles M.P. The Cochrane Collaboration. 2010. Interventions to change the behaviour of health professionals and the organisation of care to promote weight reduction in overweight and obese adults (review) pp. 1–106. (PMID: 20238311) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon D.J., Knoke J., Probstfield J.L., Superko R., Tyroler H.A. High-density lipoprotein cholesterol and coronary heart disease in hypercholesterolemic men: the lipid research clinics coronary primary prevention trial. Circulation. 1986;74:1217–1225. doi: 10.1161/01.cir.74.6.1217. (PMID: 3536151) [DOI] [PubMed] [Google Scholar]
- Hartmann-Boyce J., Jebb S.A., Fletcher B.R., Aveyard P. Self-help for weight loss in overweight and obese adults: systematic review and meta-analysis. Am. J. Public Health. 2015;105:e43–e57. doi: 10.2105/AJPH.2014.302389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt K.J., Resendez R.G., Williams K., Haffner S.M., Stern M.P., San Antonio Heart S National cholesterol education program versus World Health Organization metabolic syndrome in relation to all-cause and cardiovascular mortality in the San Antonio heart study. Circulation. 2004;110:1251–1257. doi: 10.1161/01.CIR.0000140762.04598.F9. [DOI] [PubMed] [Google Scholar]
- Hwang K.O., Stuckey H.L., Chen M.C., Kraschnewski J.L., Forjuoh S.N., Poger J.M., McTigue K.M., Sciamanna C.N. Primary care providers' perspectives on online weight-loss programs: a big wish list. J. Med. Internet Res. 2012;14:e16. doi: 10.2196/jmir.1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janiszewski P.M., Kuk J.L., Ross R. Is the reduction of lower-body subcutaneous adipose tissue associated with elevations in risk factors for diabetes and cardiovascular disease? Diabetologia. 2008;51:1475–1482. doi: 10.1007/s00125-008-1058-0. [DOI] [PubMed] [Google Scholar]
- Jay M., Gillespie C., Ark T., Richter R., McMacken M., Zabar S., Paik S., Messito M.J., Lee J., Kalet A. Do internists, pediatricians, and psychiatrists feel competent in obesity care?: using a needs assessment to drive curriculum design. J. Gen. Intern. Med. 2008;23:1066–1070. doi: 10.1007/s11606-008-0519-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jebb S.A., Ahern A.L., Olson A.D., Aston L.M., Holzapfel C., Stoll J., Amann-Gassner U., Simpson A.E., Fuller N.R., Pearson S., Lau N.S., Mander A.P., Hauner H., Caterson I.D. Primary care referral to a commercial provider for weight loss treatment versus standard care: a randomised controlled trial. Lancet. 2011;378:1485–1492. doi: 10.1016/S0140-6736(11)61344-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk S.F., Penney T.L., McHugh T.L., Sharma A.M. Effective weight management practice: a review of the lifestyle intervention evidence. Int. J. Obes. 2012;36:178–185. doi: 10.1038/ijo.2011.80. [DOI] [PubMed] [Google Scholar]
- Korda H., Itani Z. Harnessing social media for health promotion and behavior change. Health Promot. Pract. 2013;14:15–23. doi: 10.1177/1524839911405850. [DOI] [PubMed] [Google Scholar]
- Kushner R.F. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev. Med. 1995;24:546–552. doi: 10.1006/pmed.1995.1087. [DOI] [PubMed] [Google Scholar]
- Luo W., Morrison H., de Groh M., Waters C., DesMeules M., Jones-McLean E., Ugnat A.M., Desjardins S., Lim M., Mao Y. The burden of adult obesity in Canada. Chronic Dis. Can. 2007;27:135–144. (PMID: 17623559) [PubMed] [Google Scholar]
- Maheux B., Pineault R., Beland F. Factors influencing physicians' orientation toward prevention. Am. J. Prev. Med. 1987;3:12–18. (PMID: 3452333) [PubMed] [Google Scholar]
- Malik S., Wong N.D., Franklin S.S., Kamath T.V., L'Italien G.J., Pio J.R., Williams G.R. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation. 2004;110:1245–1250. doi: 10.1161/01.CIR.0000140677.20606.0E. [DOI] [PubMed] [Google Scholar]
- McNeill A.M., Rosamond W.D., Girman C.J., Golden S.H., Schmidt M.I., East H.E., Ballantyne C.M., Heiss G. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care. 2005;28:385–390. doi: 10.2337/diacare.28.2.385. (PMID: 15677797) [DOI] [PubMed] [Google Scholar]
- Mokdad A.H., Ford E.S., Bowman B.A., Dietz W.H., Vinicor F., Bales V.S., Marks J.S. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–79. doi: 10.1001/jama.289.1.76. (PMID: 12503980) [DOI] [PubMed] [Google Scholar]
- Neve M., Morgan P.J., Jones P.R., Collins C.E. Effectiveness of web-based interventions in achieving weight loss and weight loss maintenance in overweight and obese adults: a systematic review with meta-analysis. Obes. Rev. 2010;11:306–321. doi: 10.1111/j.1467-789X.2009.00646.x. [DOI] [PubMed] [Google Scholar]
- Poirier P., Giles T.D., Bray G.A., Hong Y., Stern J.S., Pi-Sunyer F.X., Eckel R.H. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss. Arterioscler. Thromb. Vasc. Biol. 2006;26:968–976. doi: 10.1161/01.ATV.0000216787.85457.f3. [DOI] [PubMed] [Google Scholar]
- PWC . 2012. Intelligent Healthcare through mHealth. [Google Scholar]
- Rao G., Burke L.E., Spring B.J., Ewing L.J., Turk M., Lichtenstein A.H., Cornier M.A., Spence J.D., Coons M., American Heart Association Obesity Committee of the Council on Nutrition PA, Metabolism, Council on Clinical C, Council on Cardiovascular N, Council on the Kidney in Cardiovascular D, Stroke C New and emerging weight management strategies for busy ambulatory settings: a scientific statement from the American Heart Association endorsed by the Society of Behavioral Medicine. Circulation. 2011;124:1182–1203. doi: 10.1161/CIR.0b013e31822b9543. [DOI] [PubMed] [Google Scholar]
- Ross R., Janssen I., Dawson J., Kungl A.M., Kuk J.L., Wong S.L., Nguyen-Duy T.B., Lee S., Kilpatrick K., Hudson R. Exercise-induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Obes. Res. 2004;12:789–798. doi: 10.1038/oby.2004.95. [DOI] [PubMed] [Google Scholar]
- Thomas J.G., Leahey T.M., Wing R.R. An automated internet behavioral weight-loss program by physician referral: a randomized controlled trial. Diabetes Care. 2015;38:9–15. doi: 10.2337/dc14-1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twells L.K., Gregory D.M., Reddigan J., Midodzi W.K. Current and predicted prevalence of obesity in Canada: a trend analysis. CMAJ open. 2014;2:E18–E26. doi: 10.9778/cmajo.20130016. [DOI] [PMC free article] [PubMed] [Google Scholar]