Abstract
The aim of this pilot study was to explore the effects of an early and customized CBT intervention, mainly delivered via internet, for adolescents with coexisting recurrent pain and emotional distress (low mood, worry, and/or distress). The intervention was based on a transdiagnostic approach, to concurrently target pain and emotional distress. A single case experimental design (SCED) was employed with six participants, 17–21 years old, who were recruited via school health care professionals at the student health care team at an upper secondary school in a small town in Sweden. The intervention consisted of 5–9 modules of CBT, delivered via internet in combination with personal contacts and face to face sessions. The content and length of the program was customized depending on needs. The effects of the program were evaluated based on self-report inventories, which the participants filled out before and after the intervention and at a six month follow-up. They did also fill out a diary where they rated symptoms on a daily basis. The results were promising, at least when considering changes during the intervention as well as pre- and posttest ratings. However, the results were more modest when calculating the reliable change index (RCI), and most of the treatment effects were not sustained at the follow-up assessment, which raises questions about the durability of the effects. Taken together, this study indicates that this type of program is promising as an early intervention for adolescents with pain and concurrent emotional distress, although the outcomes need to be explored further, especially in terms of long-term effects.
Keywords: Adolescents, Pain, CBT, Emotional distress
Highlights
-
•
I-CBT has not been used as an early intervention for adolescents with coexisting pain and emotional distress
-
•
The aim of this pilot study was to explore the effects of early I-CBT for adolescents with pain and emotional distress
-
•
The intervention consisted of 5-9 modules of customized I-CBT combined with personal support
-
•
The effects were quite modest and larger studies are needed to further explore the outcomes
1. Introduction
Recurrent pain is a common complaint in youth, affecting up to 50% of Swedish adolescents (Fichtel and Larsson, 2002), and among half of these suffer from functional impairments such as poor sleep (Haraldstad et al., 2011) and school absence (Korterink et al., 2015). Headache, abdominal pain, and muscle pain are frequently reported, and about 40% of pain sufferers convey several pain locations (Larsson and Sund, 2007). Adolescents with frequent pains report higher levels of disability as well as anxiety and depressive symptoms (Fichtel and Larsson, 2002, Hoftun et al., 2012). They are also at risk of developing future emotional and behavioral problems, such as reduced leisure time activities and somatic complaints other than pain (Larsson and Sund, 2007). Suffering from frequent pain in adolescence is thus closely linked to emotional distress such as anxiety and depressive symptoms both concurrently and in the future, and it is important to address coexisting pain and emotional problems early on.
Cognitive behavioral therapy (CBT) for adolescents with chronic pain has shown significant effects in reducing pain intensity and improving function (for reviews, see Fisher et al., 2014, Eccleston et al., 2013, Palermo et al., 2010). Although internet-based CBT (I-CBT) for pain mainly has been tested out on adults, there is also evidence that it may be beneficial for adolescents with recurrent pain (e.g., Palermo et al., 2009, Palermo et al., 2016, Trautmann and Kröner-Herwig, 2010, Hicks et al., 2006; for a review, see Bender et al., 2011). I-CBT may particularly fit this age group, considering that adolescents are often used to modern technology, and the treatment is easily accessible. I-CBT may be extra effective if applied early on, for preventing future disability. Early interventions have the advantage of targeting problems before they get too severe, and have shown to be effective for reducing anxiety and depressive symptoms in youth (see e.g. Mrazek and Haggerty, 1994, Mychailyszyn et al., 2012). To our knowledge, I-CBT has not been used as an early intervention for adolescents with coexisting pain and emotional distress.
One explanation of the high levels of comorbidity between pain and emotional distress is that they share essential maintaining processes (Linton, 2013). Based on the transdiagnostic perspective, treatments should target shared processes to achieve improvements in co-morbid problems such as pain and depressive symptoms. One core transdiagnostic process is avoidance; both overt, such as avoidance of social and physical activities, and covert, such as avoidance of negative thoughts and feelings (Barlow et al., 2010). To our knowledge, only one earlier study, which was a case report of two adolescents, has used a transdiagnostic approach to target pain and concurrent anxiety and depression in this age group (Allen et al., 2012). In the current study, we developed an intervention where the main content focused on transdiagnostic processes such as avoidance, to simultaneously target coexisting pain and emotional distress. Additional modules targeting specific problem areas were added to optimize the treatment and promote engagement. Similar approaches have been applied to younger children and adolescents, with encouraging results, both individually (e.g. Warner et al., 2011), and in group format (Logan and Simons, 2010). However, an entirely new aspect in our study was to deliver a transdiagnostic intervention via internet, a delivery mode which particularly may fit this specific age group.
Promoting engagement is extra important in adolescents, since there is a heightened risk for drop-outs (de Haan et al., 2013). Customizing the treatment content to fit the needs of the individual is one way of promoting engagement. In comparison to other internet-based interventions for pain in this age group, the customization of content and length of the intervention is a new feature in our study. Keeping personal contact through e-mails, phone calls or sms is another way of engaging youth. In the current project, we developed a unique intervention which was specifically adapted to suit adolescents, based on modern technology in combination with personal contacts. The main content focused on transdiagnostic processes, and additional components targeting specific problem areas were added depending on needs of the adolescent. As the participants partly had different emotional symptoms (e.g. with or without anxiety, depressive symptoms), the program was customized based on their problem description. The purpose of this pilot study was to explore the effects of an early and customized school-based CBT intervention, mainly delivered via internet, for adolescents with coexisting recurrent pain and emotional distress.
2. Method
2.1. Design
A single case experimental design (SCED) was employed with six participants. SCED is recommended when new treatments are developed and evaluated (Kazdin, 2014). SCED provides an intensive study of the individual, which includes systematic observation, manipulation of variables, repeated measurement before and during the intervention, and mainly visual data analysis. One advantage with SCED is that it gives detailed information about how the intervention works for each participant.
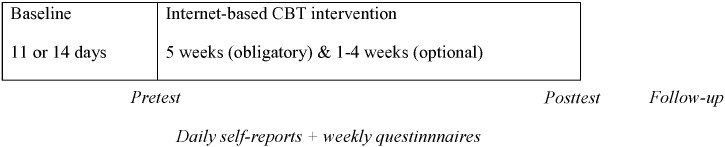
As shown in Fig. 1, the participants started to fill out daily reports before the intervention started (i.e. baseline) and continued throughout the intervention. The intervention was initiated at different time points for each participant. In this study the participants were randomized into two different baselines: 11 and 14 days. Validated self-report questionnaires were completed weekly during the intervention as well as at pretest, posttest and at a six months follow-up. The study was approved by the Regional Ethical Review Board in Uppsala (Dnr 2013/516).
Fig. 1.
Basic design of the study.
2.2. Recruitment
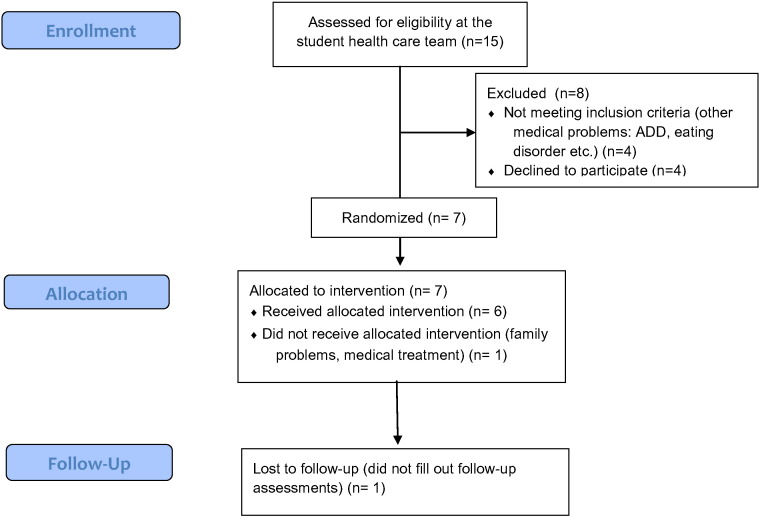
The participants were recruited via school health care professionals (two social workers and two nurses) at the student health care team at an upper secondary school in a small town in Sweden. The inclusion criteria were (1) adolescents enrolled in upper secondary school at a national program, (2) recurrent problems with pain (musculoskeletal pain, stomach pain or headache) in combination with self-reported problems with low mood, worry and/or distress, and (3) willingness to participate in the study. The exclusion criteria were (1) severe medical conditions (based on assessments by nurse or physician), (2) severe psychiatric conditions, e.g. eating disorder, psychosis (based on screening interview with psychologist), that required psychiatric care. Seven adolescents fulfilled the inclusion criteria and were included in the study. One of the participants dropped out during the treatment. Fig. 2 presents the recruitment process and reasons for exclusion and drop-out.
Fig. 2.
Recruitment process.
2.3. Participants
Six adolescents, 17–21 years old, participated in the study and completed the intervention. Table 1 presents an overview of the participants. None of the participants were on medication or had an ongoing contact with specialized health care services.
Table 1.
Overview of participants.
| Year in upper secondary school | Age | Gender | Pain duration | Pain localization | How often have you experienced pain during the last month (0 = never; 10 = always) | Problem description | Number of modules completed | |
|---|---|---|---|---|---|---|---|---|
| Participant 1 | 1 | 17 | Female | + 52 weeks | Back, head | 8 | Pain, sleep difficulties, anxiety, rumination | 6 |
| Participant 2 | 1 | 17 | Female | 4–5 weeks | Abdomen, head | 7 | Pain, anxiety, worry | 6 + one extra face to face session |
| Participant 3 | 2 | 18 | Male | 24–35 weeks | Shoulders, abdomen | 3 | Chest pain, anxiety, low mood | 5 |
| Participant 4 | 1 | 17 | Female | + 52 weeks | Neck, shoulders, back, abdomen, head | 8 | Pain, worry, rumination, low mood, anxiety | 9 + one extra face to face session |
| Participant 5 | 1 | 20 | Female | + 52 weeks | Neck, shoulders, back | 7 | Pain, low mood, sleep difficulties, rumination | 9 + one extra face to face session |
| Participant 6 | 4 | 21 | Female | + 52 weeks | Neck, shoulders, back, head | 8 | Pain, anxiety, low mood | 4 |
2.4. Procedure
The school health care personnel informed potential participants about the study and provided written information about the project at ordinary health care controls or when the adolescents applied for help at the school health care center. Adolescents who were interested in participating were invited to a screening interview with a psychologist. At the interview, the adolescents were informed about the purpose of the study, the content of the intervention and the assessments, and inclusion- and exclusion criteria were verbally assessed. Informed written consents were obtained. Electronic access to the web-platform was ensured with an electronic password that was sent to the participants' personal mobile phone. Five psychologists from the research team conducted the intervention. Participants were randomly assigned to therapists. The intervention as well as the pretest and posttest were administered through a web platform. Daily ratings and weekly questionnaires were coded and sent out to the participants via ordinary mail, and were returned on a weekly basis in pre-paid envelopes. The participants received a voucher à 10 Euro for each weekly assessment they returned. After completing the intervention, an independent person interviewed the participants individually following a semi structured protocol in order to evaluate the overall impression of the intervention.
2.5. Intervention
The intervention consisted of 5–9 modules of CBT, delivered via internet in combination with personal contacts and two obligatory face to face sessions: one at the beginning (Module 1) and one at the end (Module 9). The content of the program was customized depending on the needs of the adolescent, and included five obligatory modules (Module 1–4 and Module 9) and four optional modules (Module 5–8). The optional modules were recommended to participants based on daily ratings of symptoms after the initial four obligatory modules. If the adolescent scored above 5 on one or more of the symptoms, the modules targeting these symptoms were recommended. The order of the optional modules was decided in discussions with the adolescent. Table 2 presents a summary of the content of the program. The participants had contact with the psychologist via the platform 1–3 times per week. The adolescents were free to contact the psychologists via sms or e-mail if they had difficulties in completing the tasks or if they had questions about the material. Phone calls and additional face to face sessions were set up if the adolescents were in need of extra help to complete the material. Furthermore, face to face sessions could be added because of the following reasons:
-
-
Need of exposure in vivo related to any of the areas that were covered in the program
-
-
Need of extra tasks in any of the areas that were covered in the program.
Table 2.
Summary of the CBT program.
| Module | Content | Example of exercises |
|---|---|---|
| 1; Kick-off Obligatory |
Psychoeducation Goal setting |
Set up goals in terms of activities and function |
| 2 Obligatory |
Behavioral activation | Scheduling activities that are positively reinforced |
| 3 Obligatory |
Behavioral activation Behavioral experiment |
Continue with behavioral activation Set up a behavioral experiment |
| 4 Obligatory |
Positive psychology techniques | Savoring techniques Three good things (ref) |
| 5–8 Optional/recommended |
Sleep | Sleep hygiene |
| Coping with stress | Scheduling activities for recovering from stress | |
| Dealing with pain | Self-exposure | |
| Techniques for targeting worry | Concreteness training (ref) | |
| 9; Ending Obligatory |
Relapse prevention | Identify potential problems, maintain improvement |
Adolescents were asked to log on to the web-platform at least once a week during the program, and to complete homework assignments within a week. The psychologists sent out reminders via sms or e-mail if the participants had not completed a module within a week. The psychologists responded to each assignment with written feedback via the platform to evaluate progress, solve potential problems and provide positive reinforcement to the adolescent. The participants completed the program in 4–13 weeks. Table 1 contains information about how many modules each of the participants completed, as well as extra face to face sessions, in addition to the obligatory two face to face sessions (module #1 and module #9).
2.6. Measures
The participants were evaluated using self-report inventories (1) on a daily basis, (2) at pretest and posttest and (3) at a six month follow-up.
2.6.1. Daily ratings
The participants were asked to think about their present day when filling out the daily ratings, which consisted of five questions as displayed in Table 3. Four of the questions were taken from World Health Organization inventory (WHO, World Health Organization, 2001) in order to assess levels of pain, perceived stress, depressive symptoms and sleep difficulties. The fifth question was a self-constructed item about the level of worry and/or rumination. Answers were given on eleven-point numerical scales with 0 and 10 as endpoints (labels depending on question).
Table 3.
Items used for daily ratings.
| How much pain did you experience today? |
| How stressed or tense have you felt today? |
| To what extent have you experienced low mood today? |
| How well did you sleep last night? |
| To what extent have you been worried or dwelt on things today? |
2.6.2. Pre, post and follow-up
The following measures were used for assessments at pretest, posttest, and follow-up. Swedish versions of all scales were used.
2.6.2.1. Pain Catastrophizing Scale-Children (PCS-C)
The Pain Catastrophizing Scale-Children (PCS-C) was used to assess pain-related catastrophizing (Crombez et al., 2003). The PCS-C describes 13 thoughts and feelings that children and adolescents may have when experiencing pain, and is divided into three subscales: magnification (e.g. “I keep thinking of other painful events”), rumination (e.g. “I can't seem to keep it out of my mind”), and helplessness (e.g.” I feel I can't go on”). Respondents are asked to what extent they experience each thought and feeling on a five-point scale (0 = not at all; 4 = all the time). The PCS-C has shown satisfactory psychometric properties (Crombez et al., 2003).
2.6.2.2. Functional Disability Inventory (FDI)
The Functional Disability Inventory (FDI) was used to assess level of impairment in physical and psychosocial functioning (Walker and Greene, 1991). The scale is developed for children and adolescents with chronic pain and consists of 15 items with no subscales. The respondents are asked about their difficulty to do different activities (e.g. “Being at school the whole day”;” Doing something with a friend”). Answers are given on a five-point scale (0 = no problem and 4 = impossible). The psychometric properties of the FDI has shown to be good (Claar and Walker, 2006). The Swedish version of the FDI has been used in earlier research (e.g., Wicksell et al., 2009).
2.6.2.3. Hospital Anxiety and Depression Scale (HADS)
The Hospital Anxiety and Depression Scale (HADS) (Zigmond and Snaith, 1983) was used to assess depressive symptoms and anxiety. The HADS is divided into two subscales with seven items each, aiming at capture common symptoms of depression (e.g. “I have lost interest in my appearance”) and anxiety (e.g. “I feel tense and wound up”). Responders rate to what extent they agree with each statement on a four-point scale (0 = not at all; 3 = very much indeed). The HADS has shown satisfactory psychometric properties (Bjelland et al., 2002, Herrmann, 1997), including the Swedish version (Lisspers et al., 1997).
2.6.2.4. Insomnia Severity Index (ISI)
The Insomnia Severity Index (ISI) (Yang et al., 2009) was used to assess sleep difficulties. The scale consists of seven items to assess perceived symptoms and consequences of insomnia (e.g. “How satisfied/dissatisfied are you with your current sleep pattern?”) as well as the degree of distress associated with sleeping difficulties (e.g. “How worried/distressed are you about your current sleep problem?”). Respondents answer each item on a five-point scale, labels depending on question. The scale has shown adequate psychometric properties (Bastien et al., 2001). The Swedish version of the ISI has repeatedly been used in earlier research (e.g., Jansson-Fröjmark, 2014).
2.6.2.5. Perseverative Thinking Questionnaire (PTQ)
The Perseverative Thinking Questionnaire (PTQ) (Ehring et al., 2011) was used to assess repetitive negative thinking such as worry and rumination. The PTQ consists of 15 statements (e.g. “Thoughts intrude into my mind”; “I can't stop dwelling on them”). The respondents answer to what degree each statement is true for them on a five-point scale (0 = never true; 4 = almost always). The PTQ has shown good psychometric properties (Ehring et al., 2011).
2.7. Analysis
The daily ratings are presented in graphs to enable visual inspection. To facilitate evaluation, the daily ratings of each symptom were summarized on a weekly basis, and the mean score for each week is presented in the graphs. This method is referred to as “blocking data”, and may be used for facilitating evaluation of data with large fluctuation (Kazdin, 2011). The effects are evaluated mainly by inspecting changes between phases: baseline vs. intervention. Descriptive data is presented for pretest, posttest and follow-up. To facilitate evaluation of changes from pretest to posttest, Reliable Change Index (RCI) was calculated on all measured included in the pre and post assessments, as an indicator of clinical significant change. The RCI equals the difference between a participant's pretest and posttest scores, divided by the standard error of the difference (Jacobson and Truax, 1991).
3. Results
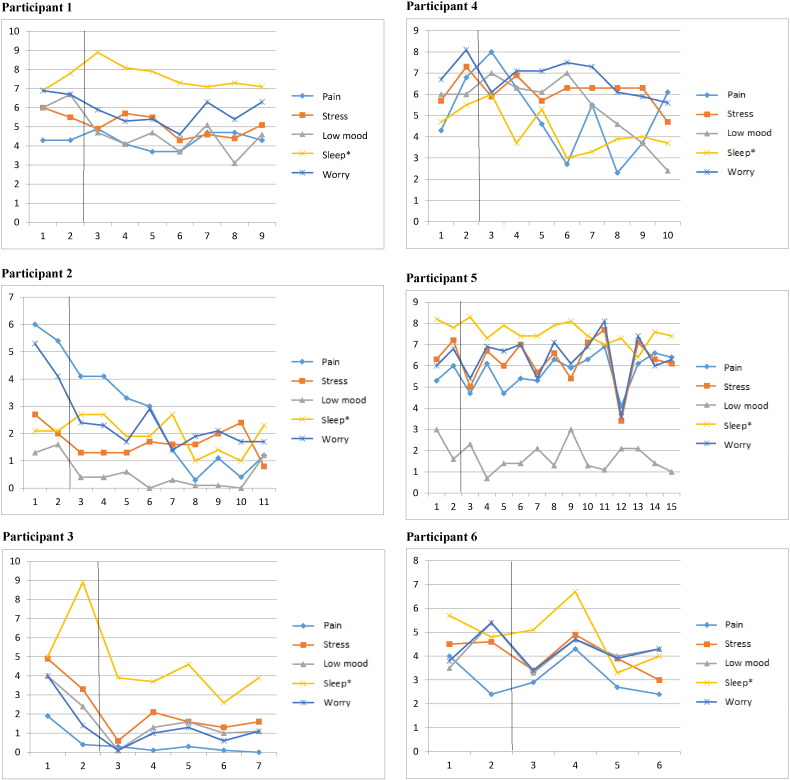
3.1. Daily ratings
Fig. 3 presents daily ratings for the participants throughout the study. In each graph, the area to the left represents scorings during baseline, and the area to the right displays scorings during the intervention. The horizontal line at the bottom of the graph illustrates for how many weeks the intervention lasted for each participant. As can be seen, participant 1 improved in mood and perceived stress during the intervention, whereas the other variables remained constant. Participant 2 improved notably in pain, worry and perceived stress. However, it should be noted that the improvements begun already during baseline. Sleep and mood remained stable for this participant. Participant 3 improved on all variables, although all improvements except for sleep begun already during baseline. Participant 4 has fairly mixed scorings. There was a large improvement in mood, and moderate improvements in worry, perceived stress and sleep, although ratings of sleep varied a lot throughout the intervention. Ratings of pain also varied with no clear trend. Participants 5 basically did not change at all throughout the intervention. Participant 6 improved on sleep and perceived stress, whereas the other variables remained stable.
Fig. 3.
Daily ratings for the participants during baseline and throughout the intervention. Note. *The ratings of sleep has been reversed, so that high scores indicate poor sleep.
3.2. Pre, post and follow-up
Table 4 presents scorings on pretest, posttest and follow-up for all participants. As can be seen, participant 1 improved on measures of anxiety and sleep from pretest to posttest, and improved somewhat on measures of pain catastrophizing, depressive symptoms and repetitive negative thinking, whereas disability remained stable. However, at follow-up, anxiety and depressive symptoms were worse than at baseline, whereas the improvements on sleep, catastrophizing and repetitive negative thinking remained. Participant 2 improved on measures of disability from pretest to posttest, and remained fairly stable on the other measures. The improvements remained stable to follow-up. Participant 3 improved on measures of anxiety and depressive symptoms from pretest to posttest, whereas the other measures remained fairly stable on constantly low levels. The improvements did not remain to follow-up. Participant 4 improved on measures of disability from pretest to posttest whereas the other variables remained fairly stable. At follow-up, disability had decreased, but not to the baseline levels. Participant 5 improved on measures of disability and depressive symptoms from pretest to posttest, and remained fairly stable on the other measures. Participant 6 improved clearly on all measures from pretest to posttest. However, when calculating the reliable change index (RCI), the results were more modest. Only two of the participants had reliable improvements, namely participant 6 who improved on four out of six measures, and participant 1, who improved on the measure of sleep.
Table 4.
Pre, post and follow-up ratings for all participants.
| Measure | Participant 1 | Participant 2 | Participant 3 | Participant 4 | Participant 5 | Participant 6 |
|---|---|---|---|---|---|---|
| PCS-C Pre |
31 | 28 | 5 | 32 | 21 | 19 |
| PCS-C Post |
26 | 28 | 11 | 28 | 22 | 7 |
| PCS-C Follow-up |
25 | 13 | 25 | 30 | 17 | – |
| FDI Pre |
38 | 10 | 3 | 20 | 35 | 20 |
| FDI Post |
38 | 0 | 2 | 5 | 30 | 3 |
| FDI Follow-up |
41 | 0 | 0 | 14 | 23 | – |
| HADS-A Pre | 10 | 9 | 8 | 19 | 8 | 14 |
| HADS-A Post | 6 | 10 | 4 | 18 | 7 | 4⁎ |
| HADS-A Follow-up |
14 | 7 | 8 | 21 | 7 | – |
| HADS-D Pre | 6 | 2 | 7 | 9 | 7 | 11 |
| HADS-D Post | 4 | 2 | 2 | 8 | 3 | 0⁎ |
| HADS-D Follow-up |
9 | 2 | 6 | 11 | 7 | – |
| ISI Pre |
20 | 5 | 7 | 13 | 20 | 11 |
| ISI Post |
11⁎ | 8 | 4 | 12 | 18 | 2⁎ |
| ISI Follow-up |
12 | 7 | 7 | 10 | 21 | – |
| PTQ Pre |
52 | 32 | 26 | 40 | 33 | 34 |
| PTQ Post |
49 | 29 | 25 | 46 | 31 | 15⁎ |
| PTQ Follow-up |
45 | 19 | 27 | 55 | 34 | – |
Reliable change according to the Reliable Change Index (RCI).
Note. Follow-up data for participant 6 is missing because of non-completion.
PCS-C: Pain Catastrophizing Scale-Children; FDI: Functional Disability Inventory; HADS-A: Hospital Anxiety and Depression Scale-Anxiety subscale; HADS-D: Hospital Anxiety and Depression Scale-Depression subscale; ISI: Insomnia Severity Index; PTQ: Perseverative Thinking Questionnaire.
3.3. Summary of the results
According to the daily ratings, all participants improved during the intervention, except for participant 6. However, two of the participants (# 2 and 3) improved somewhat already during baseline. The most consistent improvements were on the measure of perceived stress, where improvements were seen in all participants. Furthermore, half of the participants improved on the measures of mood, and half of the participants improved on the measure of worry. Altogether, this indicates that the intervention may be promising for tackling problems with perceived stress and mild mood disturbances. On the pre and post assessments, the most consistent improvements were on the measure of disability, where four of the participants improved (# 2, 4, 5 and 6). On the other measures, findings were mixed with improvements on some measures, and there were no clear deteriorations. One of the participants (# 6) clearly improved on all the measures. However, few of the changes were of a reliable size; only participant 6 had reliable improvements on the majority of measures. Unfortunately, follow-up data is missing for this participant. The results do not indicate any negative effects of the intervention.
4. Discussion
The aim of this pilot study was to explore the effects of an early and customized CBT intervention, mainly delivered via internet, for adolescents with coexisting recurrent pain and emotional distress. To our knowledge, this is the first study exploring the effects of an early customized I-CBT intervention for adolescents with pain and concurrent emotional distress. Taken together, the results were promising, at least when considering changes during the intervention as well as pre- and posttest ratings. All participants except for one (# 5) improved on daily ratings of symptoms, and the most consistent improvements were on measures of perceived stress, where all participants improved somewhat. Based on raw scores on pre and post assessments, all participants improved on some of the measures, and one of the participants improved on all measures (# 6). The most consistent improvements were on measures of disability, where four out of six participants improved. However, most improvements were not statistically reliable according to the reliable change index (RCI), and most of them did not remain to the follow-up assessment. The RCI was added as an indicator of improvements that were beyond changes that could be due to measurement errors. It appears as most of the changes in raw scores may in fact be due to measurement errors as opposed to real improvements. The drawback is that the RCI relies on quite stringent criteria, and in our study some fairly large improvements in terms of absolute scores failed to reach the level of significance according to the RCI.
Taken together, the effect of the intervention was quite modest, and one explanation for this may be high pre-treatment symptom severity. Even though pain is strikingly common in this age group, recent data on about 3000 Swedish adolescents suggests that it is only a few percentage who suffer from frequent and intense pain at multiple sites, and these report significantly higher levels of emotional difficulties than peers (Boersma and Flink, 2015). The symptom severity in our sample was comparable to those of chronic samples (Fisher et al., 2014). Aiming at being an early intervention, this means that our sample had comparable high levels of symptom severity. This was also reflected in that the participants required quite a lot of extra support, mainly reminders via sms, and yet the intervention had little effect on outcome. Nevertheless, the participants did not actively seek help at primary care or at a pain clinic because of their pain problem, and therefore our intervention may still be framed as an indicated preventive intervention (Mrazek and Haggerty, 1994), one subcategory of early interventions.
There are several new aspects in this intervention which are worth mentioning. First, the content and length of the program was based on needs of the adolescent. This resulted in large differences between individuals; the program lasted from 4 to 13 weeks, and three of the participants received an extra face to face session whereas the others did not. Although the program had various variations and it might be difficult to say what the intervention really entailed, this flexibility might also be a strength, as the program was individually tailored based on expressed needs. Secondly, our intervention aimed at concurrently treating pain and emotional distress, and to our knowledge there is only one published study, a case report with two adolescents, using a similar approach in this age group (Allen et al., 2012). It is common that adolescents with pain suffer from concurrent anxiety and/or depressive symptoms. One part of the high comorbidity may be due to somatic symptoms related to psychiatric conditions (e.g. generalized anxiety disorder). In the pain literature, it has been put forward that pain and emotional symptoms are closely related and intertwined; it is often difficult to tease out what is what (Linton, 2013). Based on contemporary theories around pain and co-existing emotional distress, one explanation of the high levels of comorbidity is that these problems share essential maintaining transdiagnostic processes (Linton, 2013). This was the theoretical basis for our intervention. The obligatory parts of the intervention consisted of components targeting transdiagnostic processes such as avoidance, for instance by using behavioral activation. This is a technique which has shown to be effective, both for patients with pain (e.g., Hlobil et al., 2007), and for those suffering from emotional distress (e.g., Dimidjian et al., 2006). The results from this pilot study preliminary supports the idea of targeting transdiagnostic processes in adolescents suffering from pain and comorbid emotional distress, although larger studies are warranted to further explore the effects.
Another new feature in our intervention is that it was run in cooperation with the school-health care personnel. It turned out that the recruitment procedure worked well; the school health personnel quite easily recruited a group of participants, and the personnel reported that they perceived the recruitment as proceeding smoothly. Only one of the participants dropped out during the program, and this was due to external factors (family situation and medical treatment), and not to the program itself. Altogether, this indicates that the setup worked, and that the school health care might serve as a base for this type of programs.
Poor adherence is a well-known problem in treatment studies for youth (de Haan et al., 2013).Our strategy for tackling this was to provide as much personal support as the adolescents needed and asked for. Indeed, this strategy worked for preventing drop-outs, as only one adolescent dropped out. However, it implies difficulties of determining how time-consuming the program is for personnel, as well as estimating cost-effectiveness. Unfortunately, we did not collect data of how many reminders etc. the adolescents got during the intervention. Future studies should preferably monitor more carefully how much time is dedicated to each adolescent, in order to evaluate cost-effectiveness.
One potential drawback is that there might have been a bias in recruitment of participants. The instructions for the school health personal were to consecutively invite adolescents who fulfilled the inclusion criteria, when the adolescents either applied on their own to the school health care center, or to ask them at the ordinary health care controls. The personnel only kept track of how many adolescents they asked, not of the ones that were left out, which raises questions about a potential selection bias, which may have influenced our results. With this in mind it is even more important to underscore that this was a pilot study, the results should be regarded as preliminary, and we do not know whether it is possible to generalize them to other settings.
Another obvious shortcoming is that the results are fairly modest. Regarding the daily ratings it is difficult to draw conclusions, as several of the baselines were not stable when the intervention was initiated. However, we did not consider it feasible with longer baseline periods in this age group. Furthermore, to guarantee quality of the data of daily ratings, the participants would preferably have filled them out electronically, but of technical reasons this did not work. Taken together, although promising, it is still questionable whether it really is an effective intervention for this group, not at least in terms of long-lasting effects. This implies a need for further developing methods to enhance durability, for instance by following adolescents with these problems for a longer period of time, and provide booster sessions. Problems with pain and emotional distress tend to be cyclic (Mense et al., 2001), and it may be important to provide support when a new episode of either pain or emotional distress appear. Future programs would preferably include boosters after a few weeks, to explore whether this may enhance improvements that last over time.
5. Conclusions
The results from pilot study preliminary endorse further development of an early and customized school-based transdiagnostic CBT intervention, mainly delivered via internet, for adolescents with coexisting recurrent pain and emotional distress. However, the results were modest, which underscores the need for more studies to further explore the effects of the intervention.
Conflict of interest
The authors have no conflicts of interest in relation to this study.
Acknowledgments
The authors sincerely want to thank Martin Arvidsson and Maria Lind for their expert help in delivering the program, the school health care personnel at Lindeskolan for recruitment, and Steven J. Linton for the inspiration and support during the whole project. We also want to thank the Academic Hospital in Uppsala, Sweden, and especially Monica Buhrman, for getting access to their web platform.
References
- Allen L.B., Tsao J.C.I., Seidman L.C., Ehrenreich-May J., Zeltzer L.K. A unified, transdiagnostic treatment for adolescents with chronic pain and comorbid anxiety and depression. Cogn. Behav. Pract. 2012;19(1):56–67. doi: 10.1016/j.cbpra.2011.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow D.H., Farchione T.J., Fairholme C.P., Ellard K.K., Boisseau C.L., Allen L.B., May J.T.E. Oxford University Press; USA: 2010. Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: Therapist Guide. [Google Scholar]
- Bastien C.H., Vallières A., Morin C.M. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Bender J.L., Radhakrishnan A., Diorio C., Englesakis M., Jadad A.R. Can pain be managed through the Internet? A systematic review of randomized controlled trials. Pain. 2011;152(8):1740–1750. doi: 10.1016/j.pain.2011.02.012. [DOI] [PubMed] [Google Scholar]
- Bjelland I., Dahl A.A., Haug T.T., Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J. Psychosom. Res. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- Boersma K., Flink I.K. Open Paper Presentation at the 45th Annual EABCT Congress, Jerusalem, Israel, August 31–September 3. 2015. Investigating the role of emotion regulation in relation to co-occurring pain-, emotional-, and interpersonal problems in adolescents. [Google Scholar]
- Claar R.L., Walker L.S. Functional assessment of pediatric pain patients: psychometric properties of the functional disability inventory. Pain. 2006;121(1–2):77–84. doi: 10.1016/j.pain.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crombez G., Bijttebier P., Eccleston C., Mascagni T., Mertens G., Goubert L., Verstraeten K. The child version of the pain catastrophizing scale (PCS-C): a preliminary validation. Pain. 2003;104(3):639–646. doi: 10.1016/S0304-3959(03)00121-0. [DOI] [PubMed] [Google Scholar]
- de Haan A.M., Boon A.E., de Jong J.T.V.M., Hoeve M., Vermeiren R.J.M. A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clin. Psychol. Rev. 2013;33(5):698–711. doi: 10.1016/j.cpr.2013.04.005. [DOI] [PubMed] [Google Scholar]
- Dimidjian S., Hollon S.D., Dobson K.S., Schmaling K.B., Kohlenberg R.J., Addis M.E.…Jacobson N.S. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J. Consult. Clin. Psychol. 2006;74(4):658. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- Eccleston C., Tm P., Acdc W., Lewandowski A., Morley S., Fisher E., Law E. Psychological therapies for the management of chronic and recurrent pain in children and adolescents (review) Cochrane Database Syst. Rev. 2013;12 doi: 10.1002/14651858.CD003968.pub3. (Online) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehring T., Zetsche U., Weidacker K., Wahl K., Schönfeld S., Ehlers A. The perseverative thinking questionnaire (PTQ): validation of a content-independent measure of repetitive negative thinking. J. Behav. Ther. Exp. Psychiatry. 2011;42(2):225–232. doi: 10.1016/j.jbtep.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fichtel A., Larsson B. Psychosocial impact of headache and comorbidity with other pains among Swedish school adolescents. Headache J. Head and Face Pain. 2002;42(8):766–775. doi: 10.1046/j.1526-4610.2002.02178.x. [DOI] [PubMed] [Google Scholar]
- Fisher E., Heathcote L., Palermo T.M., Eccleston C. Systematic review and meta-analysis of psychological therapies for children with chronic pain. J. Pediatr. Psychol. 2014;39(8):763–782. doi: 10.1093/jpepsy/jsu008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haraldstad K., Sørum R., Eide H., Natvig G.K., Helseth S. Pain in children and adolescents: prevalence, impact on daily life, and parents' perception, a school survey. Scand. J. Caring Sci. 2011;25(1):27–36. doi: 10.1111/j.1471-6712.2010.00785.x. [DOI] [PubMed] [Google Scholar]
- Herrmann C. International experiences with the Hospital Anxiety and Depression Scale—a review of validation data and clinical results. J. Psychosom. Res. 1997;42(1):17–41. doi: 10.1016/s0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- Hicks C.L., Von Baeyer C.L., McGrath P.J. Online psychological treatment for pediatric recurrent pain: a randomized evaluation. J. Pediatr. Psychol. 2006;31(7):724–736. doi: 10.1093/jpepsy/jsj065. [DOI] [PubMed] [Google Scholar]
- Hlobil H., Uegaki K., Staal J.G., de Bruyne M.C., Smid T., Van Mechelen W. Substantial sick-leave costs savings due to a graded activity intervention for workers with non-specific sub-acute low back pain. Eur. Spine J. 2007;16(7):919–924. doi: 10.1007/s00586-006-0283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoftun G.B., Romundstad P.R., Rygg M. Factors associated with adolescent chronic non-specific pain, chronic multisite pain, and chronic pain with high disability: the Young–HUNT Study 2008. J. Pain. 2012;13(9):874–883. doi: 10.1016/j.jpain.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Jacobson N.S., Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 1991;59(1):12. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jansson-Fröjmark M. The work and social adjustment scale as a measure of dysfunction in chronic insomnia: reliability and validity. Behav. Cogn. Psychother. 2014;42(2):186–198. doi: 10.1017/S135246581200104X. [DOI] [PubMed] [Google Scholar]
- Kazdin A.E. Oxford University Press; 2011. Single-case Research Designs: Methods for Clinical and Applied Settings. [Google Scholar]
- Kazdin Alan E. Allyn and Bacon; Boston, MA: 2014. Research Design in Clinical Psychology. (4. uppl) [Google Scholar]
- Korterink J.J., Diederen K., Benninga M.A., Tabbers M.M. Epidemiology of pediatric functional abdominal pain disorders: a meta-analysis. PLoS One. 2015;10(5) doi: 10.1371/journal.pone.0126982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsson B., Sund A.M. Emotional/behavioural, social correlates and one‐year predictors of frequent pains among early adolescents: influences of pain characteristics. Eur. J. Pain. 2007;11(1):57. doi: 10.1016/j.ejpain.2005.12.014. [DOI] [PubMed] [Google Scholar]
- Linton S.J. A transdiagnostic approach to pain and emotion. J. Appl. Biobehav. Res. 2013;18:82–103. doi: 10.1111/jabr.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisspers J., Nygren A., Söderman E. Hospital Anxiety and Depression Scale (HADS): some psychometric data for a Swedish sample. Acta Psychiatr. Scand. 1997;96(4):281–286. doi: 10.1111/j.1600-0447.1997.tb10164.x. [DOI] [PubMed] [Google Scholar]
- Logan D.E., Simons L.E. Development of a group intervention to improve school functioning in adolescents with chronic pain and depressive symptoms: a study of feasibility and preliminary efficacy. J. Pediatr. Psychol. 2010;35(8):823–836. doi: 10.1093/jpepsy/jsq008. [DOI] [PubMed] [Google Scholar]
- Mense S., Simons D.G., Russell I.J. Lippincott Williams & Wilkins; 2001. Muscle Pain: Understanding Its Nature, Diagnosis, and Treatment. [Google Scholar]
- Mrazek P.J., Haggerty R.J. National Academy Press; Washington, DC: 1994. Reducing Risks for Mental Disorders. [PubMed] [Google Scholar]
- Mychailyszyn M.P., Brodman D.M., Read K.L., Kendall P.C. Cognitive-behavioral school-based interventions for anxious and depressed youth: a meta-analyses of outcomes. Clin. Psychol. Sci. Pract. 2012;19(2):129–153. [Google Scholar]
- Palermo T.M., Wilson A.C., Peters M., Lewandowski A., Somhegyi H. Randomized controlled trial of an internet-delivered family cognitive-behavioral therapy intervention for children and adolescents with chronic pain. Pain. 2009;146(1–2):205–213. doi: 10.1016/j.pain.2009.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo T.M., Eccleston C., Lewandowski A.S., Williams A.C.D.C., Morley S. Randomized controlled trials of psychological therapies for management of chronic pain in children and adolescents: an updated meta-analytic review. Pain. 2010;148(3):387–397. doi: 10.1016/j.pain.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo T.M., Law E.F., Fales J., Bromberg M.H., Jessen-Fiddick T., Tai G. Internet-delivered cognitive-behavioral treatment for adolescents with chronic pain and their parents: a randomized controlled multicenter trial. Pain. 2016;157(1):174–185. doi: 10.1097/j.pain.0000000000000348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trautmann E., Kröner-Herwig B. A randomized controlled trial of Internet-based self-help training for recurrent headache in childhood and adolescence. Behav. Res. Ther. 2010;48(1):28–37. doi: 10.1016/j.brat.2009.09.004. [DOI] [PubMed] [Google Scholar]
- Walker L.W., Greene J.W. The functional disability inventory: measuring a neglected dimension of child health status. J. Pediatr. Psychol. 1991;16:39–58. doi: 10.1093/jpepsy/16.1.39. [DOI] [PubMed] [Google Scholar]
- Warner C.M., Colognori D., Kim R.E., Reigada L.C., Klein R.G., Browner‐Elhanan K.J.…McFarlane‐Ferreira Y.B. Cognitive‐behavioral treatment of persistent functional somatic complaints and pediatric anxiety: an initial controlled trial. Depress. Anxiety. 2011;28(7):551–559. doi: 10.1002/da.20821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO, World Health Organization The world health report 2001: mental health: new understanding, new hope. 2001. http://www.who.int/whr/2001/en/whr01_en.pdf (Extracted May 13, 2014, from)
- Wicksell, Melin, Lekander, Olsson Evaluating the effectiveness of exposure and acceptance strategies to improve functioning and quality of life in longstanding pediatric pain — a randomized controlled trial. Pain. 2009;141(3):248–257. doi: 10.1016/j.pain.2008.11.006. [DOI] [PubMed] [Google Scholar]
- Yang M., Morin C.M., Schaefer K., Wallenstein Interpreting score differences in the Insomnia Severity Index: using health-related outcomes to define the minimally important difference. Curr. Med. Res. Opin. 2009;25(10):2487–2494. doi: 10.1185/03007990903167415. [DOI] [PubMed] [Google Scholar]
- Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]