Abstract
Ample studies have demonstrated that internet-based cognitive behavioural therapy (iCBT) for anxiety disorders is effective and acceptable in controlled settings. Studies assessing the clinical effectiveness of iCBT for anxiety disorders among routine care populations are, however, not as numerous. The purpose of this study was to assess the effectiveness of iCBT among anxiety patients, who were on a waiting list for intensive outpatient treatment, in a specialised routine care clinic.1
A randomised controlled pilot trial was conducted. Recruited patients were on a waiting list and had a primary diagnosis of either social phobia or panic disorder. Participants were randomised into either receiving iCBT with minimal therapist contact (received access to the programme FearFighter® (FF) and received support from a clinician via telephone) or no treatment (stayed on the waiting list). The primary outcome was self-reported symptomatic change of anxiety on Beck Anxiety Inventory (BAI). The secondary outcomes were comorbid depression measured on Beck Depression Inventory (BDI-II) and quality of life measured with the EuroQol one-item visual-analogue scale (EQ-vas). All results were analysed by intention-to-treat analyses using a mixed-effects approach. N = 158 patients were assessed for eligibility of which N = 67 met all eligibility inclusion criteria, signed informed consent forms, and were randomised. Post-treatment assessment was completed by N = 47 (70%). In the intervention group, N = 11 (31%) completed all modules of FF. No significant differences of change of symptomatic levels were found between the intervention and control group for anxiety (BAI: mean diff. = 2.42; 95% CI − 1.03 to 5.86; p = 0.17; d = 0.06) or for depression (BDI-II: mean diff. 1.87; 95% CI − 2.25 to 6.00; p = 0.37; d = 0.02). A large and significant effect was found in self-reported quality of life in favour of the experimental group (EQ-vas: mean diff. − 20.88; 95% CI − 30.64 to − 11.11; p < 0.001; d = 0.81).
This study was not able to document statistically significant clinical effect of iCBT with minimal therapist contact compared to a waiting list control group in a specialised anxiety clinic in routine care. However, a large and significant effect was seen on self-reported quality of life. Although these results offer an interesting perspective on iCBT in specialised care, they should be interpreted with caution, due to the limitations of the study. A large scale fully powered RCT is recommended.
Keywords: Internet, Computer, Internet-based, Cognitive behavioural therapy, CBT, iCBT, cCBT, RCT, Randomised controlled trial, Anxiety, Social phobia, Panic disorder, Specialised care, Secondary care, Self-help
Highlights
-
•
Effectiveness of iCBT for anxiety was investigated in specialised care
-
•
67 adult anxiety patients were randomised to either waiting-list or iCBT
-
•
No significant difference was found post treatment on symptomatic levels of anxiety
-
•
A large and significant difference was found on self-reported quality of life
1. Introduction
Panic disorder and social phobia are common, debilitating disorders characterised respectively by an excessive anxiety response when experiencing either normal bodily symptoms such as small palpitations or when confronted with social situations (American Psychiatric Association, 2000). A large epidemiological survey estimated a 12-month prevalence rate of 2.7% for adult panic disorder (with or without agoraphobia) and 6.8% for adult social phobia (Kessler et al., 2005). Onset is typically between the ages of 13–15 for social phobia and 24–40 for panic disorder. If untreated these disorders often become chronic (Bruce et al., 2005). They are associated with negative consequences such as impaired career trajectories, absenteeism from work, reduced work performance, impaired romantic relationships, impaired quality of life, elevated medical utilisation and high societal costs (Katon, 1996, Wittchen et al., 2000, Batelaan et al., 2007, Olatunji et al., 2007, Konnopka et al., 2009).
There is now substantial evidence to support internet-based cognitive behavioural therapy with minimal support (iCBT) as being effective for panic disorder and social phobia compared to non-intervening (Spek et al., 2007, Barak et al., 2008, Andrews et al., 2010, Andersson et al., 2014) with large effect sizes (e.g. Carlbring et al., 2006, Berger et al., 2009).
iCBT even seems to offer treatment results comparable to those of traditional face-to-face therapy. For example, in a randomised study by Hedman et al. (Hedman et al., 2011) no difference was found between iCBT and group face-to-face CBT for social phobia on the Liebowitz Social Anxiety Scale (non-inferiority randomised design, where the lower-bound of the 95% CI of the mean difference fell within 10 LSASS points). Similarly, Kiropoulos et al. (Kiropoulos et al., 2008), found support for iCBT to be equally effective as face-to-face CBT for panic disorder in a randomised study (post-treatment assessment for Panic Disorder Severity Scale: iCBT (N = 45): M = 9.92 SD = 5.88; CBT (N = 35): M = 9.24 SD = 5.65; ANOVA analysis on group effect p = .88). And in a meta-analysis of studies comparing iCBT with face-to-face CBT for depression and anxiety disorders, Cuijpers et al. (Cuijpers et al., 2010) did not find support for iCBT to yield smaller effect sizes than traditional face-to-face CBT.
However, most studies have been conducted under controlled conditions and have primarily included self-referred patients. To our knowledge, only a few studies had been conducted on patients in routine care settings. Cavanagh et al. (Cavanagh et al., 2006) conducted a naturalistic, open, non-controlled study of adult anxiety and/or depression using the programme Beating the Blues. N = 219 was included of which, N = 84 (38%) dropped out, and N = 104 (47%) completed post-treatment outcome measures. A significant change was found using intention-to-treat analyses on the Clinical Outcomes in Routine Evaluation-Outcome Measure (p < 0.001; d = 0.5) and on the Work and Social Adjustment scale (p < 0.001; d = 0.26). Similarly, in a specialised CBT clinic Learmonth et al. (Learmonth et al., 2008) conducted a naturalistic, open, non-controlled study on adult anxiety and/or depression using the programme Beating the Blues as well. N = 555 participants were included, and almost three quarters (N = 394 ≈ 71%) concluded all modules in the programme. A significant improvement was seen (p < 0.001) on Beck Depression Inventory (d = 0.72) and on Beck Anxiety Inventory (d = 0.5) using intention-to-treat analyses. Even though these studies were uncontrolled, a positive effect was indicated for the use of iCBT in routine care.
Since more research on this topic was needed and due to long waiting lists for anxiety treatment, it was decided to conduct a pilot RCT on iCBT for these disorders using a waiting list population in an outpatient clinic for anxiety disorders2 in a Danish specialised care setting. No studies had been conducted on iCBT in routine care in Denmark up to this point.
The intervention chosen was the programme FearFighter® (FF). This online self-help programme is specifically designed for panic disorders and phobias and is completed over 9 steps. Two previous randomised controlled trials (RCT) had investigated the effectiveness of FF on adult populations with positive results being indicated. The first RCT was conducted by its original developer Isaac Marks et al. (Marks et al., 2004) on a population (N = 93) of mainly self-referred patients who answered notices in general practitioner (GP) offices or self-help groups. FF with minimal guidance was compared to face-to-face therapy and relaxation in a three-arm trial in a 2:2:1 ratio. On the Fear Questionnaire Global Phobia scale a significant difference was found between FF and relaxation (mean diff. − 1.2; 95% CI − 2.4 to − 0.1; p < 0.001) but no significant difference was found between FF and face-to-face therapy (mean diff. − 0.2; 95% CI − 1.2 to 0.8), which indicated FF to be effective. The second RCT was conducted by Schneider et al. (Schneider et al., 2005) on a population (N = 68) referred to a self-help clinic. This RCT compared FF to a minimal form of iCBT referred to as ‘anxiety management’ in a 2:1 ratio. Both groups received minimal guidance in equal doses. In both groups a significant improvement was seen (FF: d = 0.5–5.1; MA: d = 0.5–5.1; p < 0.01), but no significant between-group effect was seen (p > 0.3). There was, however, a tendency in favour of FF compared to anxiety management after 14 weeks. Given the relatively small sample size (N = 68), the active control condition, and the significant within group results in both groups, the authors conclude that this might also indicate FF to be an effective treatment.
2. Methods
2.1. Trial design
For the present study, the trial was designed as a pilot two-arm randomised controlled trial. The experimental group was given access to FearFighter® (FF) (ST Solutions Ltd., Birmingham, England) with minimal therapist contact. The control group was placed on a waiting list for face-to-face CBT as part of normal routine practice and received no psychological treatment.
2.2. Patients and recruitment
Inclusion criteria were: a primary DSM-IV diagnosis of panic disorder with or without agoraphobia or social phobia, mastery of the Danish language (written and spoken) and access to a computer with a broadband Internet connection. Exclusion criteria were: developmental disorders or other cognitive disabilities or Axis II disorders other than cluster C (avoidant, dependent, obsessive–compulsive), suicidal plans, bipolar disorder or depressive psychotic features.
Patients referred to the clinic first underwent a diagnostic assessment as part of routine practice to establish diagnosis. They were diagnosed by use of (a) the Anxiety Disorders Interview Schedule (Brown et al., 1994) a reliable, structured interview for anxiety disorders and related conditions, (b) Structured Clinical Interview for DSM-IV Axis II Personality Disorders (First et al., 1997) to establish possible axis II disorders, and (c) an anamnestic interview which is a comprehensive interview of the patient and is standard care practice throughout the Central Region of Denmark. Such an interview includes the patient's social background and context; history of the disorder e.g. time of onset and circumstances surrounding that; and other relevant diseases and disorders e.g. neurological disorders. All interviews were conducted by trained, experienced clinicians (five clinical psychologists and one psychotherapist). After this diagnostic assessment, eligible patients were asked to participate in the study. Provided that they still wanted it, the patients were informed that they would still be able to receive the treatment they were promised even if the iCBT programme helped them.
Prior to participation all patients signed informed consent documents; additionally, they received both spoken and written information, which explained their rights. The trial was approved by the Danish Research Ethics Committee (ref. nr. M-20110143).
Within the permitted timeframe of the study (9 months for the clinical trial running from September 2011 through July 2012), a total of N = 158 patients were referred to the clinic. N = 75 patients met the inclusion criteria and were invited to participate in the study.
2.3. Intervention
In the intervention group, patients used the therapist-assisted, self-help Internet intervention FearFighter® (FF). FF is an iCBT treatment and self-management programme for panic disorder and phobic disorders (Marks et al., 2004). It includes weekly screening of symptoms by use of questionnaires supported by a database to keep track of progress. The programme gives feedback to the patient as well as the supporting clinician about whether symptom levels are constant, rising or falling. An alarm message is given if the patient scores over a pre-set threshold on a one-item suicidal score. When this occurs, the patient is contacted for a suicidal assessment interview and referred to an acute ward if needed. The dose of treatment is nine weekly modules (steps). The patient can prolong the time intervals between the steps; however, a time lock prevents the patients from proceeding to the next step within a shorter time span. The patients were allowed to use as much time with the programme as they wished while they were still on the waiting list. The core clinical elements in the programme are: psycho education, cognitive restructuring, interoceptive and in vivo exposure exercises, applied relaxation, restructuring of maladaptive schemas and relapse prevention. The programme includes interactive exercises and uses a range of multimedia channels, including audio/video of a therapist, case and exercise demonstration, text on screen as slides next to the therapist in the videos, printout summaries, exercise descriptions and material for non-professional helpers, automated email reminders, graphics and animations (Kenwright et al., 2004). The programme was translated to Danish. Small cultural adaptations were made to fit the Danish context of the study. These adaptations included videos and pictures, which were taken in locations familiar to the Danish population. Additionally, Interoceptive exposure was added and included: hyperventilation, spinning on an office chair and running on the spot.
Unique usernames and passwords were used to protect the participants' privacy, and all saved data were securely transferred and encrypted.
By use of 10-minute telephone calls, all participants in the intervention group received synchronous support weekly or biweekly from either a clinical psychologist or a psychotherapist trained in CBT. The calls were initiated by the clinicians and were prescheduled. The support included technical assistance and problem solving regarding any difficulties or lack of progress with the therapy. Participants were also encouraged to continue the treatment.
The participants were advised to ask a friend or a family member for support through the programme. Information about the role of a helper, which the patient could provide the helper with, was given to the patient as a downloadable pdf file.
The support staff consisted of the same experienced CBT clinicians (five clinical psychologists and one psychotherapist) who were responsible for the intake. They all went through a one-day training course which included instructions in using the clinician side of the programme and training in providing support to the participants in the format of 10 min telephone calls as required for the present study. As preparation for the training, they had all gone through the FearFighter® programme.
Patients in the control condition received no psychological treatment.
2.4. Outcome measures
2.4.1. Primary outcome measure
The Beck Anxiety Inventory (BAI) is a 21-item self-report instrument for assessing the severity of anxiety in psychiatric patients (Beck et al., 1988a). It has a high internal consistency with a Cronbach's alpha of 0.92 and test retest reliability of r = 0.75 (Beck et al., 1988a).
2.4.2. Secondary outcome measures
The Beck Depression Inventory (BDI-II) is a 21-item self-report measure used to determine the presence and severity of depressive symptoms (Beck et al., 1988b). Internal consistency of the original BDI is excellent with a Cronbach's alpha of 0.86, and test–retest reliability is also high (Beck et al., 1988b). In the present study the BDI-II, which has been shown to have similar properties, is used (Beck et al., 1996).
The Panic Disorder Severity Scale (PDSS) is a seven-item scale that was used to assess symptoms of panic disorder (Houck et al., 2002). It has been found to have excellent inter-rater reliability on all scale items ranging from r = 0.74 to 0.87, moderate internal consistency with Cronbach's alpha of 0.65 and favourable levels of validity and sensitivity to change (Shear et al., 1997). In the present study the self-report version was used.
The Liebowitz Social Anxiety Scale (LSAS) is comprised of 24 social situations that are each rated for level of fear over the past week (Liebowitz, 1987). In the present study it was used in the self-report format. LSAS has shown a high test–retest reliability over 12 weeks with an r = 0.83 (Fresco et al., 2001). LSAS-SR has a high internal consistency with a Cronbach's alpha = 0.95 (Baker et al., 2002).
Finally, patients scored their health-related quality of life on the EuroQol visual analogue scale (EQ-vas) (EuroQol Group, 1990). This is a one-item visual-analogue scale on which the patient scores his or her subjective experience of general state of health on a continuous line with scores ranging from 0 to 100.
2.5. Sample size
Previous studies of FF (Marks et al., 2004) have found medium to large effect sizes between FF and control conditions. Following Cohen (Cohen, 1992), to detect a medium difference between two independent sample means (d = .50) at alpha = .05 and power of .80 requires N = 64 in each group.
2.6. Randomisation
Randomisation was performed using a computer-generated string of 100 binary random numbers (www.random.org) placed sequentially in concealed envelopes. A secretary not involved in the study administered the randomisation.
2.7. Statistical analyses
We used descriptive statistics to compare the intervention group with controls on various baseline characteristics. This allowed us to check for the presence of confounding variables. We used a two-sided student's t-test for the comparison of variables of continuous nature, such as age, while for the categorical variables we used a chi-squared test of proportions. In addition to this, we compared the intervention group with controls on outcome measures at baseline as well as follow-up using a two-sided student's t-test. Furthermore, we reported the mean and standard deviation of duration and number of telephone calls as well as number of steps completed in the FearFighter® programme for the intervention group.
The analyses of change conducted were intention-to-treat (ITT) linear regression using a mixed effects approach with a random intersection at subject level. We used all observations available for these analyses. Since difference of change over time between intervention group and controls was the main interest of the analysis, an interaction term was added to the model. Standardised effect sizes in the form of Cohen's d were calculated for all mean differences of change between intervention group and controls.
All outcome measures were checked for normality by visual inspection of the quantile-normal plots.
A p-value lower than 0.05 was considered statistically significant. The statistical package STATA version 13 was used for all analyses.
3. Results
3.1. Inclusion
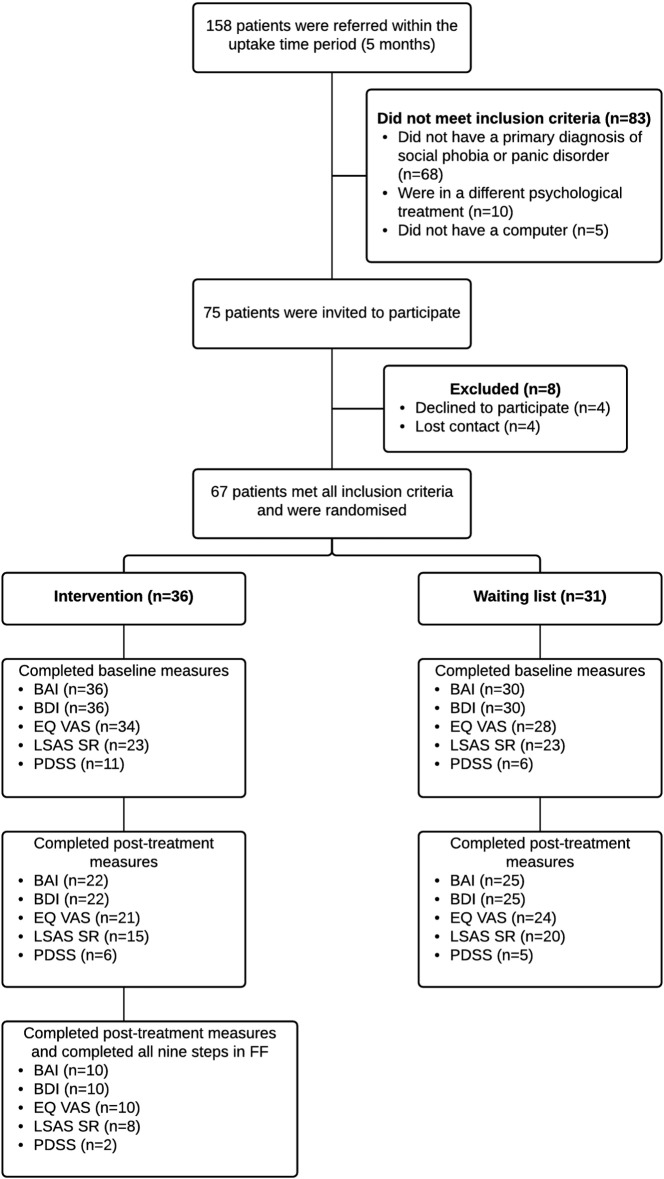
As can be seen in Fig. 1, 158 patients were referred to the clinic during the study period. 75 patients met all inclusion criteria for the study and were invited to participate. 8 were excluded because they either declined to participate (N = 4) or contact was lost (N = 4). Thus, a total of 67 patients were randomised whereof 36 were randomly allocated to the intervention group and 31 to the control group.
Fig. 1.
Patient flow.
BAI: Beck Anxiety Inventory; BDI-II: Beck Depression Inventory II; LSAS-SR: Liebowitz Social Anxiety Scale — Self Report version; PDSS-SR: Panic Disorder Severity Scale — Self Report version; EQ-VAS: EuroQol visual analogue scale.
3.2. Adherence and support given
All 36 participants assigned to the intervention group completed baseline measurements and 22 (61%) completed post-treatment measurements. Only 11 (31%) out of the 36 allocated participants concluded the programme in its entirety whereof 1 did not submit post-treatment data. 14 (39%) counted as dropped out of the study either because they began other treatment (N = 8) or they never started (N = 6). Of the 31 participants allocated to the control group, 30 (97%) completed baseline measurements and 25 (81%) completed the post-measurements.
Participants in the control group were rated after four months (122 days), whereas a wide variation was seen in the days spent with the programme in the intervention group (m = 123 days, sd = 59.94).
Support was provided as short prescheduled telephone calls initiated by the clinicians. A mean of M = 10.7 min was spent per call.3 A mean of M = 55.9 min (SD = 32.2; range: [20–149]) was spent per patient. Results of duration of support calls could only be obtained from 18 participants (50%) most likely caused by forgetfulness of the therapists due to the stressed reality of clinical practice(Table 1).
Table 1.
Adherence and support.
| Mean | SD | N | |
|---|---|---|---|
| Number of telephone calls pr. participant | 5.22 | 1.59 | 18 |
| Total length of telephone calls in minutes | 72.17 | 38.64 | 18 |
| Length of telephone calls pr. participant | 55.9 | 32.2 | 18 |
| Number of steps completed in the FearFighter programme | 5.28 | 3.27 | 36 |
| Number of days spend with the programme | 123 | 59.94 | 36 |
3.3. Baseline characteristics
Baseline characteristics for both groups are seen in Table 2. There were no statistically significant differences between the two groups on any measure at baseline except for depression. In the experimental condition a higher number of participants (N = 21) were diagnosed with a comorbid depressive disorder when compared to the control group (N = 8), based on the clinical assessment interview (p < 0.01). For this reason we controlled for comorbid affective disorder in all analyses. Furthermore, when the participants were split into degrees of severity based on BDI-II scores, more than twice the number of patients scored over the cut-off for severe depression (BDI-II score ≥ 30) in the intervention group. However, there was no statistically significant difference in the distribution of degrees of depression severity between the two groups (p = 0.24).
Table 2.
Baseline characteristics.
| Intervention group | Control group | p-Value | |||
|---|---|---|---|---|---|
| Gender (N, %) | |||||
| Female | 23 | 63.89 | 18 | 60.00 | |
| Male | 13 | 36.11 | 12 | 40.00 | 0.7457 |
| Age at baseline (mean, SD) | 32.39 | 12.30 | 29.23 | 8.81 | 0.2441 |
| Psychotropic drugs (N, %) | |||||
| Yes | 26 | 72.22 | 18 | 60.00 | |
| No | 10 | 27.78 | 12 | 40.00 | 0.2943 |
| Primary diagnosis (N, %) | |||||
| PD | 12 | 33.33 | 7 | 23.33 | |
| SP | 24 | 66.67 | 23 | 76.67 | 0.3716 |
| Comorbid Affective (N, %) | |||||
| Yes | 21 | 58.33 | 8 | 26.67 | |
| No | 15 | 41.67 | 22 | 73.33 | 0.0099 |
| BDI II 14–19 | 5 | 41.67 | 8 | 61.11 | |
| BDI II 20–28 | 10 | 13.89 | 7 | 22.22 | |
| BDI II 29–63 | 13 | 27.78 | 6 | 19.44 | 0.2390 |
| Comorbid Personality (N, %) | |||||
| Yes | 9 | 25.00 | 8 | 26.67 | |
| No | 27 | 75.00 | 22 | 73.33 | 0.8775 |
| Employed/student (N, %) | |||||
| Yes | 14 | 38.89 | 15 | 50.00 | |
| No | 22 | 61.11 | 15 | 50.00 | 0.3651 |
| Alcohol consumption per week (N, %) | |||||
| Never drink | 12 | 33.33 | 8 | 26.67 | |
| 0–5 | 23 | 63.89 | 15 | 50.00 | |
| 5–10 | 0 | 0.00 | 4 | 13.33 | |
| 10–20 | 1 | 2.78 | 3 | 10.00 | 0.0720 |
PD: panic disorder; SP: social phobia.
3.4. Outcome
The observed means and standard deviations of the outcome measures at baseline as well as follow-up for both the intervention group and the controls are shown in Table 3. The mean differences of outcomes between the two groups at both time points are likewise shown in Table 3. No statistically significant differences between the groups were found as has been showed in Table 3.
Table 3.
Observed means of outcome measures.
| Mean intervention group (SD) | Mean control group (SD) | Mean difference | 95% CI | p-Value | N intervention | N control | ||
|---|---|---|---|---|---|---|---|---|
| Observed mean of outcome measures at baseline | ||||||||
| BAI | 22.86 (10.41) | 22.23 (8.54) | 0.63 | − 4.12 | 5.37 | 0.7923 | 36 | 30 |
| BDI-II | 22.72 (10.66) | 20.17 (10.68) | 2.56 | − 2.71 | 7.82 | 0.3361 | 36 | 30 |
| EQ-vas | 49.26 (19.14) | 49.18 (19.64) | 0.09 | − 9.80 | 9.97 | 0.9862 | 34 | 28 |
| Observed mean of outcome measures at follow-up | ||||||||
| BAI | 16.00 (10.12) | 19.68 (9.56) | − 3.68 | − 9.47 | 2.11 | 0.2067 | 22 | 25 |
| BDI-II | 17.36 (11.77) | 18.68 (9.87) | − 1.32 | − 7.67 | 5.04 | 0.6787 | 22 | 25 |
| EQ-vas | 63.52 (19.10) | 45.04 (20.83) | 18.48 | 6.40 | 30.56 | 0.0035 | 21 | 24 |
BAI: Beck Anxiety Inventory; BDI-II: Beck Depression Inventory II; EQ-VAS: EuroQol visual analogue scale.
As can be seen in Table 4, the results of the intention-to-treat linear regression analysis (ITT) on the primary measure of symptoms of anxiety (BAI) reported no statistically significant difference of change between the groups (mean diff. = 2.42; 95% CI − 1.03 to 5.86; p = 0.17; d = 0.06).
Table 4.
Linear regression analyses of between-group change over time.
| Change intervention group | p-Value | Change control group | p-Value | Mean diff. of change over time | 95% CI | p-Value | Std. effect size | ||
|---|---|---|---|---|---|---|---|---|---|
| BAI | − 5.293 | 0.0000 | − 2.873 | 0.0217 | 2.415 | − 1.033 | 5.863 | 0.1699 | 0.06 |
| BDI-II | − 3.504 | 0.0247 | − 1.533 | 0.2788 | 1.873 | − 2.253 | 5.998 | 0.3737 | 0.02 |
| EQ-vas | 16.276 | 0.0000 | − 4.391 | 0.2076 | − 20.876 | − 30.644 | − 11.107 | 0.0000 | 0.81 |
BAI: Beck Anxiety Inventory; BDI-II: Beck Depression Inventory II; EQ-VAS: EuroQol visual analogue scale.
Likewise, we found no statistically significant difference of change on the secondary outcome measure of symptomatic levels of depression (BDI-II) when comparing the intervention group to the control group (mean diff. 1.87; 95% CI − 2.25 to 6.00; p = 0.37; d = 0.02). There was, however, a small statistically significant favourable within-group change in the intervention group on the BDI-II (mean diff. − 3.70; p = 0.02) but not in the control group (mean diff. − 1.53; p = 0.28). A large and statistically significant between-group beneficial difference of change was seen on the EQ-vas (mean diff. − 20.88; 95% CI − 30.64 to − 11.11; p < 0.001; d = 0.81).
4. Discussion and conclusion
The present pilot study examined whether it was feasible to conduct an iCBT trial in routine practice in Denmark and whether it was an effective treatment for social phobia and panic disorder when delivered to patients on a waiting list for CBT treatment in comparison to a non-intervening control condition in routine care in a specialised anxiety clinic. The programme FearFighter® was used since it had, in previous RCT's, been shown to be an effective treatment for these disorders (Marks et al., 2004).
Results show that we were able to recruit patients from the waiting list (N = 67). We did, however, not find a significant difference of change in favour of the experimental group on symptomatic levels of neither anxiety (BAI: mean diff. = 2.42; 95% CI − 1.03 to 5.86; p = 0.17; d = 0.06) nor depression (BDI-II: mean diff. 1.87; 95% CI − 2.25 to 6.00; p = 0.37; d = 0.02).
These results resembles those of a recent study by Kok et al. (Kok et al., 2014) in which a different, but functionally equivalent iCBT intervention was investigated in an RCT recruiting from specialised anxiety clinics in routine care in the Netherlands. They did find a significant, though small, effect (N = 210; d = 0.35; p = 0.02) on the primary outcome measure of symptomatic levels of phobia using the Fear Questionnaire. Nonetheless, no significant difference between the groups was found on the secondary measure of BAI (p = 0.5). Given the fact that the previous studies of FF used the Fear Questionnaire, which could seem to be more sensitive to change, this may shed some light on the presumably different results between the present and the previous RCT's of FF.
Also, the previous RCT's on FF were conducted on patient groups with less severe comorbidity. In the study from 2004, Marks et al. compared FF with clinician-guided self-exposure and applied relaxation. In the population studied (N = 90), few had comorbid psychiatric disorders (7%) compared with the present study (affective disorders FF = 58%, Control = 27%; personality disorders FF = 25%, Control = 27%). In the study from 2005, Schneider, Mataix-Cols et al. demonstrated significant treatment effect in a self-help clinic. There was no clear description of baseline characteristics and the presence of comorbid disorders was not reported. Yet, while the exclusion criteria for the most part resembled those adopted in the present study, severe depression was excluded. By comparison 28% (N = 19) of the participants in the present study reported severe depression at baseline. This was particularly true in the intervention group whereof 36% reported severe depression at baseline (n = 13). From these observations it could be speculated that high degrees of comorbidity and, perhaps particularly, severe depression might reduce the clinical effectiveness of iCBT when delivered in a format with minimal therapist contact as it has been indicated to be the case in some studies (Chambless et al., 1997, Collimore and Rector, 2012).
The results did show a large and statistically significant beneficial effect on the self-reported quality of life (EQ-vas). Though this may seem contradictory to the apparent lack of treatment effect, it may be due to the participants appreciating being able to do something themselves to change their situations and that the programme induced hope and a sense of control. It can also be speculated that receiving information about their conditions enabled the patients to distance themselves from their illnesses. All of these explanations were indicated by participant comments during the supporting telephone calls.
This was a pilot trial with a number of limitations. It is possible that the explanation for the lack of treatment effect lies in the study's lack of power. Our power calculations stated that 64 participants were needed in each group, while we were only able to recruit N = 67 in total during the pre-specified time period of the study. However, in addition to high p-values, the results also showed very low standardised effect sizes for most of the scores. This could indicate that the statistically insignificant results were due to more than low power. Moreover, some of the estimated effects are likely explained by the phenomena “regression to the mean”. Another explanation for the statistically insignificant effect of the clinical outcome measures may be due to the fact that only 11 participants actually completed all nine steps in the FearFighter® programme. A completers analysis may give more insight to whether this was the case; however, such an analysis in the current study would be greatly underpowered. Furthermore, the participants in the control group were rated after precisely four months (122 days), whereas a wide variation was seen in the days spent with the programme in the intervention group (m = 123 days, sd = 59.94). Additionally, the participants were referred to the clinic with the promise of face-to-face treatment and it was clear from interviews conducted after the treatment, that many patients did not regard the iCBT as the “real” intervention but rather as a sort of training or preparation for “the real treatment”. This was in spite of the fact that the patients were told otherwise. This might have compromised the patients expectancy of treatment effect of the iCBT and damaged the working alliance which might have compromised treatment outcome (Waller and Gilbody, 2009, Ritterband et al., 2010, Preschl et al., 2011). Finally, the EQ-VAS is a one-item measurement scale. The use of one item scales have been criticised for being scientifically weak because of poor reliability, validity, and responsiveness due to the scales' lack of a general reference frame. For this reason, each respondent may answer the question from a different frame of reference and thus render the underlying construct measured too wide. Consequently, the answers can be ambiguous (Hobart et al., 2007). However, there is evidence to support that there is a satisfactory correlation between the EQ5D-5L index score and the EQ-VAS score (Konig et al., 2010, Feng et al., 2014).
In conclusion, we were able to conduct a study on iCBT and to recruit patients from the waiting list of a specialised care clinic. The intervention did even seem to improve the participants' quality of life significantly. However, no statistically significant difference in symptomatic change of anxiety or depression was seen from pre to post treatment measurements between the intervention group and the control group. These results should, though, be interpreted with great caution due to the limitations of the study.
Further research is needed to explore this topic. An RCT conducted in routine care with sufficient power to detect a small effect size would be recommended. Also, a study of iCBT in a blended care format in specialised care would be recommended.
Conflict of interest
The authors have no conflicts of interests.
Acknowledgements
The authors would like to thank the Fund for Welfare Technology (1087) and the Danish Agency for Digitisation for their funding and support. Also, our deepest appreciation for the dedication and hard-work from all involved in the project.
Footnotes
Clinic for OCD and Anxiety disorders, Aarhus University Hospital, DK.
Clinic for OCD and Anxiety disorders, Aarhus University Hospital, Aarhus, DK.
The standard deviation of time spent on individual phone calls could not be calculated, as only the sum of minutes spent on each patient was available to the research team.
References
- American Psychiatric Association . Washington DC; Amercian Psychiatric Association: 2000. Diagnostic and Statistical Manual of Metal Disorders (4. ed. TR) [Google Scholar]
- Andersson G., Cuijpers P., Carlbring P., Riper H., Hedman E. Guided internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiatry. 2014;13:288–295. doi: 10.1002/wps.20151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G., Cuijpers P., Craske M.G., Mcevoy P., Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis. PLoS One. 2010;5:e13196. doi: 10.1371/journal.pone.0013196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker S.L., Heinrichs N., Kim H.-J., Hofmann S.G. The Liebowitz social anxiety scale as a self-report instrument: a preliminary psychometric analysis. Behav. Res. Ther. 2002;40:701–715. doi: 10.1016/s0005-7967(01)00060-2. [DOI] [PubMed] [Google Scholar]
- Barak A., Hen L., Boniel-Nissim M., Shapira N.A. A comprehensive review and a meta-analysis of the effectiveness of internet-based psychotherapeutic interventions. J. Technol. Hum. Serv. 2008;26:109–160. [Google Scholar]
- Batelaan N., Smit F., De Graaf R., Van Balkom A., Vollebergh W., Beekman A. Economic costs of full-blown and subthreshold panic disorder. J. Affect. Disord. 2007;104:127–136. doi: 10.1016/j.jad.2007.03.013. [DOI] [PubMed] [Google Scholar]
- Beck A.T., Epstein N., Brown G., Steer R.A. An inventory for measuring clinical anxiety: psychometric properties. J. Consult. Clin. Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck A.T., Steer R.A., Garbin M.G. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin. Psychol. Rev. 1988;8:77–100. [Google Scholar]
- Beck A.T., Steer R.A., Ball R., Ranieri W.F. Comparison of Beck Depression Inventories–IA and –II in psychiatric outpatients. J. Pers. Assess. 1996;67:588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Berger T., Hohl E., Caspar F. Internet-based treatment for social phobia: a randomized controlled trial. J. Clin. Psychol. 2009;65:1021–1035. doi: 10.1002/jclp.20603. [DOI] [PubMed] [Google Scholar]
- Brown T.A., Dinardo P.A., Barlow D.A. Graywind Publication; New York: 1994. Anxiety Interview Schedule for DSM-IV: Adult Version. [Google Scholar]
- Bruce S.E., Yonkers K.A., Otto M.W., Eisen J.L., Weisberg R.B., Pagano M., Shea M.T., Keller M.B. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12-year prospective study. Am. J. Psychiatry. 2005;162:1179–1187. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlbring P., Bohman S., Brunt S., Buhrman M., Westling B.E., Ekselius L., Andersson G. Remote treatment of panic disorder: a randomized trial of internet-based cognitive behavior therapy supplemented with telephone calls. Am. J. Psychiatry. 2006;163(2119):2119–‐2125. doi: 10.1176/ajp.2006.163.12.2119. [DOI] [PubMed] [Google Scholar]
- Cavanagh K., Shapiro D.A., Van Den Berg S., Swain S., Barkham M., Proudfoot J. The effectiveness of computerized cognitive behavioural therapy in routine care. Br. J. Clin. Psychol. 2006;45:499–514. doi: 10.1348/014466505X84782. [DOI] [PubMed] [Google Scholar]
- Chambless D.L., Tran G.Q., Glass C.R. Predictors of response to cognitive-behavioral group therapy for social phobia. J. Anxiety Disord. 1997;11:221–240. doi: 10.1016/s0887-6185(97)00008-x. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychol. Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Collimore K.C., Rector N.A. Symptom and cognitive predictors of treatment response in CBT for social anxiety disorder. Int. J. Cogn. Ergon. Ther. 2012;5:157–169. [Google Scholar]
- Cuijpers P., Donker T., Van Straten A., Li J., Andersson G. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychol. Med. 2010;40:1943–1957. doi: 10.1017/S0033291710000772. [DOI] [PubMed] [Google Scholar]
- Euroqol Group EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- Feng Y., Parkin D., Devlin N.J. Assessing the performance of the EQ-VAS in the NHS PROMs programme. Qual. Life Res. 2014;23:977–989. doi: 10.1007/s11136-013-0537-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M., Gibbon M., Spitzer R., Williams J., LS. B. American Psychiatric Press, Inc.; Washington DC.: 1997. Structured Clinical Interview for DSM-IV Axis II Personality Disorders, (SCID-II) [Google Scholar]
- Fresco D.M., Coles M.E., Heimberg R.G., Liebowitz M.R., Hami S., Stein M.B., Goetz D. The Liebowitz social anxiety scale: a comparison of the psychometric properties of self-report and clinician-administered formats. Psychol. Med. 2001;31:1025–1035. doi: 10.1017/s0033291701004056. [DOI] [PubMed] [Google Scholar]
- Hedman E., Andersson G., Ljótsson B., Andersson E., Rück C., Mörtberg E., Lindefors N. Internet-based cognitive behavior therapy vs. cognitive behavioral group therapy for social anxiety disorder: a randomized controlled non-inferiority trial. PLoS One. 2011:6. doi: 10.1371/journal.pone.0018001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobart J.C., Cano S.J., Zajicek J.P., Thompson A.J. Rating scales as outcome measures for clinical trials in neurology: problems, solutions, and recommendations. Lancet Neurol. 2007;6:1094–1105. doi: 10.1016/S1474-4422(07)70290-9. [DOI] [PubMed] [Google Scholar]
- Houck P.R., Speigel D.A., Shear M.K., Rucci P. Reliability of the self-report version of the panic disorder severity scale. Depress. Anxiety. 2002;15:183–185. doi: 10.1002/da.10049. [DOI] [PubMed] [Google Scholar]
- Katon W. Panic disorder: relationship to high medical utilization, unexplained physical symptoms, and medical costs. J. Clin. Psychiatry. 1996;57:11–18. [PubMed] [Google Scholar]
- Kenwright M., Marks I., Gega L., Mataix-Cols D. Computer-aided self-help for phobia/panic via internet at home: a pilot study. Br. J. Psychiatry. 2004;184:448–449. doi: 10.1192/bjp.184.5.448. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Chiu W.T., Demler O., Walters E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiropoulos L.A., Klein B., Austin D.W., Gilson K., Pier C., Mitchell J., Ciechomski L. Is internet-based CBT for panic disorder and agoraphobia as effective as face-to-face CBT? J. Anxiety Disord. 2008;22:1273–1284. doi: 10.1016/j.janxdis.2008.01.008. [DOI] [PubMed] [Google Scholar]
- Kok R.N., Straten A., Beekman A.T.F., Cuijpers P. Short-term effectiveness of web-based guided self-help for phobic outpatients: randomized controlled trial. J. Med. Internet Res. 2014;16 doi: 10.2196/jmir.3429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konig H.H., Born A., Gunther O., Matschinger H., Heinrich S., Riedel-Heller S.G., Angermeyer M.C., Roick C. Validity and responsiveness of the EQ-5D in assessing and valuing health status in patients with anxiety disorders. Health Qual. Life Outcomes. 2010;8:47. doi: 10.1186/1477-7525-8-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konnopka A., Leichsenring F., Leibing E., König H.-H. Cost-of-illness studies and cost-effectiveness analyses in anxiety disorders: a systematic review. J. Affect. Disord. 2009;114:14–31. doi: 10.1016/j.jad.2008.07.014. [DOI] [PubMed] [Google Scholar]
- Learmonth D., Trosh J., Rai S., Sewell J., Cavanagh K. The role of computer-aided psychotherapy within an NHS CBT specialist service. Couns. Psychother. Res. 2008;8:117–123. [Google Scholar]
- Liebowitz M.R. Social phobia. Mod. Probl. Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Marks I.M., Kenwright M., Mcdonough M., Whittaker M., Mataix-Cols D. Saving clinicians' time by delegating routine aspects of therapy to a computer: a randomized controlled trial in phobia/panic disorder. Psychol. Med. 2004;34:9–18. doi: 10.1017/s003329170300878x. [DOI] [PubMed] [Google Scholar]
- Olatunji B.O., Cisler J.M., Tolin D.F. Quality of life in the anxiety disorders: a meta-analytic review. Clin. Psychol. Rev. 2007;27:572–581. doi: 10.1016/j.cpr.2007.01.015. [DOI] [PubMed] [Google Scholar]
- Preschl B., Maercker A., Wagner B. The working alliance in a randomized controlled trial comparing online with face-to-face cognitive-behavioral therapy for depression. BMC Psychiatry. 2011;11 doi: 10.1186/1471-244X-11-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritterband L., Thorndike F., Vásquez D., Saylor D. Oxford Guide to Low Intensity CBT Interventions. Oxford University Press; New York, NY: 2010. Treatment credibility and satisfaction with internet interventions. [Google Scholar]
- Schneider A.J., Mataix-Cols D., Marks I.M., Bachofen M. Internet-guided self-help with or without exposure therapy for phobic and panic disorders. Psychother. Psychosom. 2005;74:154–164. doi: 10.1159/000084000. [DOI] [PubMed] [Google Scholar]
- Shear M.K., Brown T.A., Barlow D.H., Money R. Multicenter collaborative panic disorder severity scale. Am. J. Psychiatry. 1997;154:1571–1575. doi: 10.1176/ajp.154.11.1571. [DOI] [PubMed] [Google Scholar]
- Spek V., Cuijpers P., Nyklicek I., Riper H., Keyzer J., Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol. Med. 2007;37:319–328. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- Waller R., Gilbody S. Barriers to the uptake of computerized cognitive behavioural therapy: a systematic review of the quantitative and qualitative evidence. Psychol. Med. 2009;39:705–712. doi: 10.1017/S0033291708004224. [DOI] [PubMed] [Google Scholar]
- Wittchen H.U., Fuetsch M., Sonntag H., Müller N., Liebowitz M. Disability and quality of life in pure and comorbid social phobia. findings from a controlled study. Eur. Psychiatry. 2000;15:46–58. doi: 10.1016/s0924-9338(00)00211-x. [DOI] [PubMed] [Google Scholar]