Abstract
The mental health of young people is decreasing. It is therefore important to develop early interventions for young people with mental health problems. One previous randomized controlled trial on tailored Internet-based treatment for young adults with minimal therapist guidance has shown promising results for anxiety symptoms. The purpose of this study was to investigate the effects of tailored internet-administered CBT for young adults (16–25 years old) with anxiety, depression and possible comorbidity in regular care. Participants were recruited from a youth health care centre (n = 15). Screening consisted of online questionnaires followed by a semi-structured interview. A total of 10 participants completed pre and post measurement. The treatment consisted of individually prescribed CBT text modules with online therapist guidance. All dependent measures improved significantly immediately following treatment and the within-group effect based on pre- to post measurement on the primary outcome measure, the Beck Anxiety Inventory, was d = 1.50, the within-group effect on the secondary outcome measures, Montgomery Åsberg Depression Rating Scale-Self-Rated, Clinical Outcomes in Routine Evaluation and Quality of Life Inventory showed large improvement. Tailored internet-based treatment can be an approach in the treatment of anxiety symptoms and comorbid depressive symptoms in youth care.
1. Introduction
Swedish children and young people's mental health has decreased during the 1990s and 2000s and the latest data from 2011 show a continued decrease and is thus a growing public health problem (Swedish National Board of Health and Welfare, 2013). During the time period of 1994 to 2006 the proportion of young adults aged 16–29 years who reported severe anxiety more than doubled. In the age group 18–24 years, 7% of men in the population had contact with the psychiatric outpatient or inpatient care, or used psychotropic drugs. The corresponding numbers for women were 10%. Young people with anxiety have an increased risk of not completing school and are at increased risk for other mental health problems, substance abuse, unemployment and suicidality (Murray et al., 2012). In the age group 15–24, 176 people took their lives in 2013, 123 men and 53 women (Swedish National Board of Health and Welfare, 2014). Untreated anxiety disorders have a relatively chronic course and in adult studies it has been found that anxiety disorders often have its onset in childhood or adolescence (Wenar and Kerig, 2008). Serious long-term effects can be developed as a result of initially mild anxiety disorders and it is therefore important with early interventions for young people with anxiety problems. Wenemark et al. (2006) showed that young adults in the age group of 18–29 were affected to a larger extent in regard to mental illness than other age groups. These results lead to the establishment of Youth Health Care Centres in Sweden where young adults could easily access psychological treatment (Halje et al., 2015). One way to increase access to treatment is via internet-based cognitive behavioural therapy (ICBT). ICBT interventions are one way of disseminating evidence-based treatment in primary care settings while maintaining treatment fidelity (Craske et al., 2009). The first-line psychological treatment for youth anxiety disorders is CBT (Kendall and Peterman, 2015). Although CBT principles are evidence based and standardized, clinicians are encouraged to use “flexibility within fidelity,” tailoring treatment to the youth's individual presentation (Kendall et al., 2008). Numerous studies have been conducted to examine CBT for anxiety disorders and anxiety symptoms in youth, and taken together; these studies provide the empirical support necessary to make CBT the psychological treatment identified to date as an evidence-based treatment (Seligman and Ollendick, 2011). Young adults use the internet daily, making this a setting well suited for information, psychoeducation and treatment for young adults. This group is more heterogeneous than adults and the need to develop different kinds of treatment and ways to convey them becomes larger. For young adults, ICBT has been proven effective for students with social phobia (Tillfors et al., 2011), for students with anxiety, depression and stress (Day et al., 2013) and for young adults with anxiety and depression (Sethi et al., 2010). Travers and Benton (2014) examined young adults' attitudes towards internet administered treatment and 34% reported an interest towards internet administered treatment instead of conventional treatment. There are however few studies on the effectiveness of ICBT which warrants for this study.
This study is part of a lager ongoing project to tailor ICBT for anxiety and depression for adolescents, young adults, adults and older adults. The individually tailored ICBT intervention aims to address the participant's needs and symptoms. Previous trials have been conducted on adolescents (Silfvernagel et al., 2015) and young adults and adults (Silfvernagel et al., 2012).
The purpose of this study was to determine whether tailored ICBT is a feasible approach in the treatment of anxiety symptoms and comorbid anxiety and depressive symptoms in a clinical setting, a Youth Health Care Centre.
2. Method
2.1. Participants and procedure
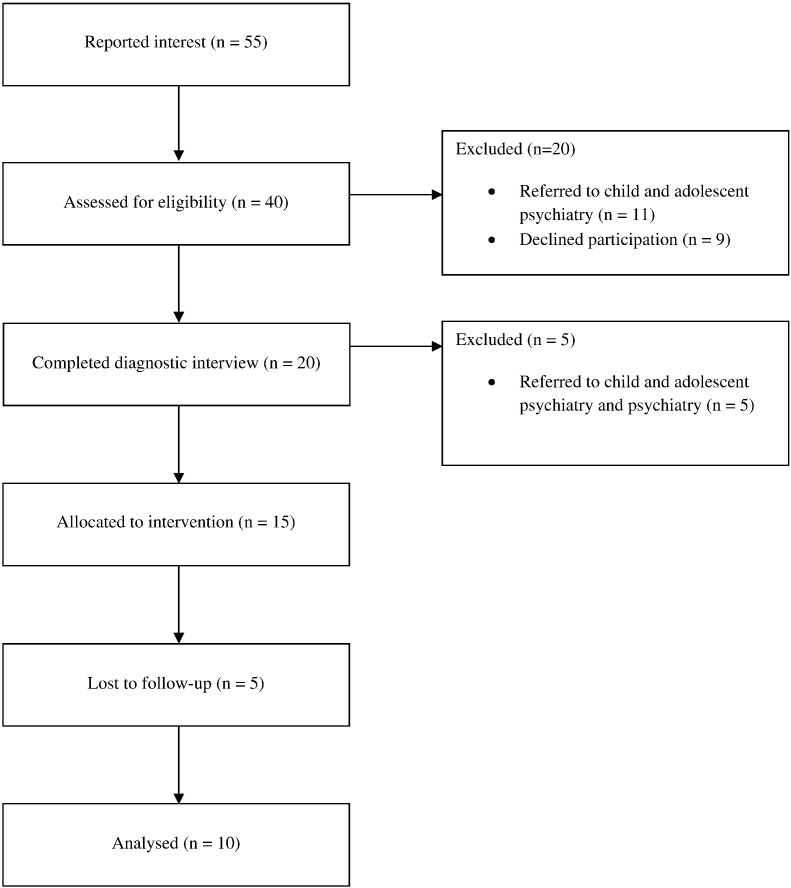
This interventional study with a single group design took place in a Youth Health Care Centre in Sweden. It was approved by the regional ethics committee in Linköping and registered at ClinicalTrials.gov (NCT01402258). Participants were recruited from the Centre. Information about all psychological treatment offered at the Centre was presented on the Youth Health Care Centre website. The Centre uses self-referral, which means that the young adults apply for treatment via telephone to a nurse or a therapist. Participants interested in internet-based CBT applied to the treatment via an early version of the online platform developed by the research group (Vlaescu et al., 2016). The platform contained information about the trial, how to register, and how to submit written informed consent. Screening consisted of the following questionnaires administered via the Internet: Beck Anxiety Inventory (BAI; Beck et al., 1988) (primary outcome measure); Montgomery-Åsberg Depression Scale-Self-rated (MADRS-S; Svanborg and Åsberg, 1994); Clinical Outcomes in Routine Evaluation-Outcome Measure (CORE-OM; Barkham et al., 2001); Quality of Life Inventory (QOLI; Frisch et al., 1992); Alcohol Use Disorders Identification Test (AUDIT; Saunders et al., 1993); and additional questions with reference to demographic variables. If the participants met the initial inclusion criteria they underwent further screening consisting of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I; First et al., 2002), conducted by licensed psychologists employed at the Youth Health Care Centre. The licensed psychologists then presented their clinical assessment to the main author and a psychiatrist before the participants were enrolled in the trial. This procedure was repeated at post treatment with the exception of AUDIT. The participants had to be between the ages of 16–25 years old (young adults), and suffer from recurrent anxiety symptoms to be included. The participants did not have to fulfil diagnostic criteria for an anxiety disorder in order to be included in the study. Participants were also assessed for the presence of comorbid major depression. Individuals with major depression as primary condition were not to be included. The participants had to have a score of < 4 points on item 9 (suicidal thoughts) on MADRS-S; not currently be in psychotherapy; and not be at risk of alcohol abuse or fulfilling the criteria for current alcohol addiction. Fifty-five individuals expressed an interest in the trial, of which 40 filled in all the self-assessment forms. Eleven were referred to child and adolescent psychiatry after this initial screening and 9 declined to participate. Twenty were assessed with SCID-I, 5 individuals were referred to child and adolescent psychiatry and psychiatry and 15 participants were included the study (see Fig. 1). For a demographic description of the participants, see Table 1.
Fig. 1.
Flowchart of study participants.
Table 1.
Demographic description of the participants at pre-treatment.
| Treatment group (n = 15) | |
|---|---|
| Gender, n (%) | |
| Male | 1 (6.7%) |
| Female | 14 (93.3%) |
| Age (years) | |
| Mean (SD) | 21.5 (1.8) |
| Minimum–maximum | 18–24 |
| Marital status, n (%) | |
| Single | 7 (46.7%) |
| Living together with a partner | 6 (40%) |
| Living with parents | 2 (13.3%) |
| Highest educational level, n (%) | |
| Secondary school | 10 (66.7%) |
| College/university (not completed) | 5 (33.3%) |
| Psychotherapy, n (%) | |
| No experience | 7 (46.7%) |
| Previous experience | 8 (53.3%) |
| Anxiolytic and/or antidepressant, n (%) | |
| Ongoing | 3 (20%) |
| Completed | 2 (13.3%) |
| No experience | 10 (66.7%) |
| Employment status, n (%) | |
| Employed | 6 (40%) |
| Unemployed | 1 (6.7%) |
| Student | 7 (46.7%) |
| Sick leave | 1 (6.7%) |
| SCID-I diagnosis, n (%) | |
| Generalized anxiety disorder | 4 (26.7%) |
| Panic disorder | 3 (20%) |
| Panic disorder + agoraphobia | 5 (33.3%) |
| Social phobia | 1 (6.7%) |
| Obsessive-compulsive disorder | 1 (6.7%) |
| Posttraumatic stress disorder | 3 (20%) |
| Anxiety disorder not otherwise specified | 1 (6.7%) |
| Major depression | 6 (40%) |
SCID-I = Structured Clinical Interview for DSM-IV Axis I Disorders.
2.2. Treatment
The treatment consisted of tailored internet-administered CBT, with 22 modules and accompanying homework assignments. The modules were between 9 and 45 pages long, with an average length of 19.7 pages. The modules were derived from previous studies on tailored treatment for anxiety and depression (Carlbring et al., 2011, Johansson et al., 2012, Bergman Nordgren et al., 2014, Silfvernagel et al., 2012). They were adapted for young adults both with regard to language and with clinical examples. The modules are all based on established and evidence-based CBT principles and included psychoeducation, exposure exercises, behavioural experiments and homework assignments. The treatment was individually tailored for each participant based on the results of the clinical assessment based on the questioners and the SCID-I interview. The first module (introduction) and the last module (relapse prevention) were fixed, and the following were available for the psychologist to prescribe: cognitive restructuring (2 modules); panic disorder (2 modules); panic symptoms (1 module); agoraphobia (1 module); social anxiety (2 modules); trauma (2 modules); setting boundaries (1 module); behavioural activation (2 modules); procrastination (1 module); worrying (1 module); generalized anxiety (3 modules); applied relaxation (1 module); and establish a better sleep pattern (1 module). For a more detailed description of the modules, see Silfvernagel et al. (2015). Licensed and experienced psychologists employed at the Youth Health Care Centre provided therapist guidance and there were no automatic messages.
2.3. Statistical analyses
Changes in questionnaire scores between pre- and post-treatment were evaluated using paired sample t-tests. The within-group effect sizes (Cohen's d) were calculated from the observed means and observed pooled standard deviations from pre- to post-measurement. Non-response was handled based on the principle Complete Cases (Salim et al., 2008), which means that only data from the participants who completed the survey were included in the analysis. Also examined was the percentage of participants who no longer met the criteria for a diagnosis after treatment.
3. Results
The effect of treatment was examined using the outcome measures BAI, MADRS-S CORE-OM and QOLI. The results from these are presented in the form of means, standard deviations and the within group effect size in Table 2. Distribution of diagnoses post-treatment assessed with the SCID interview and treatment adherence is presented with the number and average of finished modules.
Table 2.
Immediate results, means, standard deviations and within group effects (n = 10).
| Measure | Pre-treatment | Post-treatment | Within group effect |
|---|---|---|---|
| BAI | 26.90 (9.01) | 16.00 (5.52) | d = 1.50 |
| MADRS-S | 20.60 (6.13) | 13.60 (4.53) | d = 1.31 |
| CORE-OM | 20.17 (4.47) | 12.59 (4.99) | d = 1.60 |
| QOLI | 0.67 (1.83) | 1.93 (1.04) | d = 0.88 |
BAI = Beck Anxiety Inventory, MADRS-S = Montgomery Åsberg Depression Rating Scale-Self Rated, CORE-OM = Clinical Outcomes in Routine Evaluation - Outcome Measure, QOLI = Quality of Life Inventory.
3.1. Results
Paired sample t-tests showed significant results across all outcome measures, primary and secondary, with large within-group effect sizes: BAI (t9 = 5.35, p < 0.001, d = 1.50), MADRS-S (t9 = 4.67, p < 0.001, d = 1.31), CORE-OM (t9 = 7.61, p < 0.001, d = 1.60) and QOLI (t9 = 3.53, p < 0.05, d = 0.88). According to the assessment of the SCID interview after treatment 7 of 10 participants no longer met the criteria for a diagnosis.
3.2. Treatment adherence
Of the 15 participants who were included in the study, 9 completed all prescribed modules with the associated homework assignments (8–12) with a mean of 10.1 modules. One participant announced after five of the eight planned modules that they desired to end treatment because they were feeling much improved and thereafter participated in post-measurement. The 5 who discontinued treatment prematurely finished a mean of 3.4 modules. Out of the 5 who discontinued ICBT treatment, 2 wanted to receive face-to-face CBT at the clinic and 3 did not want to participate in the post-measurement.
4. Discussion
The aim of this pilot effectiveness study was to evaluate the effects of individually tailored ICBT for anxiety disorders with comorbid depressive symptoms for young adults (16–25). Large treatment effects were found for all dependent measures immediately following treatment. The results of this study are consistent with previous trials of individually tailored ICBT conducted in a clinical setting for adolescents (Silfvernagel et al., 2015), that was conducted at the same time as this study, and a previous efficacy trial on young adults with anxiety symptoms (Silfvernagel et al., 2012). The results are also in line with Halje et al. (2015) who examined CBT treatment at Youth Health Care Centres within the same county where this study took place. The results should be viewed with caution due to a small sample size and the lack of randomization; however this was a pilot effectiveness study with psychologists employed at the Centre who administrated the treatment which strengthens the validity. The psychologist received supervision in both CBT and ICBT during the study. The psychologists conducted the interviews and the treatment after training on the SCID-I and ICBT offered by the research group led by Professor Gerhard Andersson. The use of standardized diagnostic interviews is not common practice at Youth Health Care Centres in the county (Halje et al., 2015) but was implemented after the trial.
A further strength in comparison with (Silfvernagel et al., 2012) is that the participants were recruited from within the Youth Health Care Centre and not via national recruitment, enhancing the possibility that the population for this trial was representative for the clinical setting where the study took place.
The results of the SCID-I interview shows that 7 out of 10 no longer met diagnostic criteria for their initial diagnosis. Of the 15 participants who were included in the study, 9 completed their planned treatment. This can be compared to patients seeking psychological treatment in primary care and psychiatry, were just over a third are improved regarding the condition they were seeking help for (Hansen et al., 2002). Up to 8% deteriorate, and the rest, more than half, remain unchanged. Treatment adherence can be viewed as high in this small study in comparison with Halje et al. (2015) and Tillfors et al. (2011).
An essential aspect is how well the sample in the study represents the population studied. The treatment was tested in regular care with a patient population that is common and representative for young adults seeking first-line psychological treatment. Within this setting, young adults, between the ages 16 and 25 can receive psychological treatment for anxiety and depression via self-referral. Inclusion criteria in this study were liberal with few restrictions in terms of comorbidity, which mimics a clinical population and probably enhances the external validity for this study. However the results must be followed up in with larger samples. This effectiveness pilot study examined whether tailored ICBT would work in a real-world settings and in situations that clinicians encounter in their daily routine practice. Andersson and Hedman (2013) reviewed the literature and showed that internet-administered CBT can work well in regular care but that more research was needed to see how the treatment works in the different contexts and in different target groups i.e. young adults.
With the help of technical progress, the boundaries between internet administered treatment and therapy can become more fluent in the future. The internet can be used for self-assessment within clinical settings, be used to record behaviours live, to deliver psychoeducation, and by combining treatment modules with support face-to-face.
5. Conclusions
The tentative conclusion based on the results from this small effectiveness trial is that tailoring ICBT can be a feasible approach in the treatment of anxiety symptoms and comorbid depressive symptoms in youth care. Further research should however be conducted on a larger scale to draw conclusions if said treatment should be implemented within this setting, preferably in comparison with face-to-face CBT.
Conflict of interest
The authors have no conflict of interest to report.
Acknowledgments
This trial was funded by a grant from Medical Research Council of Southeast Sweden (FORSS-150291). The authors would like to thank the therapists Miriam Fohlin, Malin Larsson and Åsa Johansson along with the participants in this trial for their involvement. PhD Robert Johansson provided valuable comments on an early version of the manuscript.
Footnotes
Trial Registration:Clinicaltrials.gov NCT01402258.
References
- Andersson G., Hedman E. Effectiveness of guided internet-based cognitive behavior therapy in regular clinical settings. Verhaltenstherapie. 2013;23:140–148. [Google Scholar]
- Barkham M., Margison F., Leach C., Lucock M., Mellor-Clark J., Evans C., Benson L., Connell J., Audin K., McGrath G. Service profiling and outcomes benchmarking using the CORE-OM: toward practice-based evidence in the psychological therapies. Clinical Outcomes in Routine Evaluation-Outcome Measures. J. Consult. Clin. Psychol. 2001;69(2):184–196. doi: 10.1037//0022-006x.69.2.184. [DOI] [PubMed] [Google Scholar]
- Beck A.T., Epstein N., Brown G., Steer R.A. An inventory for measuring clinical anxiety: psychometric properties. J. Consult. Clin. Psychol. 1988;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Bergman Nordgren L., Hedman E., Etienne J., Bodin J., Kadowaki Å., Eriksson S., Lindkvist E., Andersson G., Carlbring P. Effectiveness and cost-effectiveness of individually tailored Internet-delivered cognitive behavior therapy for anxiety disorders in a primary care population: a randomized controlled trial. Behav. Res. Ther. 2014;59:1–11. doi: 10.1016/j.brat.2014.05.007. [DOI] [PubMed] [Google Scholar]
- Carlbring P., Maurin L., Törngren C., Linna E., Eriksson T., Sparthan E., Strååt M., Marquez von Hage C., Bergman Nordgren L., Andersson G. Individually-tailored, internet-based treatment for anxiety disorders: a randomized controlled trial. Behav. Res. Ther. 2011;49:18–24. doi: 10.1016/j.brat.2010.10.002. [DOI] [PubMed] [Google Scholar]
- Craske M.G., Rose R.D., Lane A., Shaw Welch S., Campbell-Sills L., Sullivan G., Sherbourne C., Bystrisky A., Stein M.B., Roy-Byrne P.P. Computer-assisted delivery of cognitive behavioral therapy for anxiety disorders in primary-care settings. Depress. Anxiety. 2009;26:235–242. doi: 10.1002/da.20542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day V., McGrath P.J., Wojtowicz M. Internet-based guided self-help for university students with anxiety, depression and stress: a randomized controlled clinical trial. Behav. Res. Ther. 2013;51(7):344–351. doi: 10.1016/j.brat.2013.03.003. [DOI] [PubMed] [Google Scholar]
- First M.B., Spitzer R.L., Gibbon M., Williams J. Biometrics Research, New York State Psychiatric Institute; New York: 2002. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P) (November) [Google Scholar]
- Frisch M.B., Cornell J., Villanueva M., Retzlaff P.J. Clinical validation of the quality of life inventory: a measure of life satisfaction for use in treatment planning and outcome assessment. Psychol. Assess. 1992;4(1):92–101. [Google Scholar]
- Halje K., Timpka T., Tylestedt P., Adler A.-K., Fröberg L., Schyman T., Johansson, Dahl K. Self-referral psychological treatment centre for young adults: a 2-year observational evaluation of routine practice before and after treatment. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2015-008030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen N.B., Lambert M.J., Forman E.V. The psychotherapy dose-response effect and its implications for treatment delivery services. Clin. Psychol. Sci. Pract. 2002;9:329–343. [Google Scholar]
- Johansson R., Sjöberg E., Sjögren M., Johnsson E., Carlbring P., Andersson T., Rousseau A., Andersson G. Tailored vs. standardized internet-based cognitive behavior therapy for depression and comorbid symptoms: a randomized controlled trial. PLoS One. 2012;7 doi: 10.1371/journal.pone.0036905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall P.C., Peterman J.S. CBT for adolescents with anxiety: mature yet still developing. Am. J. Psychiatr. 2015;172:519–530. doi: 10.1176/appi.ajp.2015.14081061. [DOI] [PubMed] [Google Scholar]
- Kendall P.C., Gosch E., Furr J.M., Sood E. Flexibility within fidelity. J. Am. Acad. Child Adolesc. Psychiatry. 2008;47:987–993. doi: 10.1097/CHI.0b013e31817eed2f. [DOI] [PubMed] [Google Scholar]
- Murray C.J., Vos T., Lozano R. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- Salim A., Mackinnon A., Christensen H., Griffiths K. Comparison of data analysis strategies for intent-to-treat analysis in pre-test–post-test designs with substantial dropout rates. Psychiatry Res. 2008;160:335–345. doi: 10.1016/j.psychres.2007.08.005. [DOI] [PubMed] [Google Scholar]
- Saunders J.B., Aasland O.G., Babor T.F., de la Fuente J.R., Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Seligman L.D., Ollendick T.H. Cognitive behavioral therapy for anxiety disorders in youth. Child Adolesc. Psychiatr. Clin. N. Am. 2011;20(2):217–238. doi: 10.1016/j.chc.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sethi S., Campbell A.J., Ellis L.A. The use of computerized self-help packages to treat adolescent depression and anxiety. J. Technol. Hum. Serv. 2010;28:144–160. [Google Scholar]
- Silfvernagel K., Carlbring P., Kabo J., Edström S., Eriksson J., Månson L., Andersson G. Individually tailored internet-based treatment for young adults and adults with panic attacks: randomized controlled trial. J. Med. Internet Res. 2012;14:32–44. doi: 10.2196/jmir.1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silfvernagel K., Gren-Landell M., Emanuelsson M., Carlbring P., Andersson G. Individually tailored internet-based cognitive behavior therapy for adolescents with anxiety disorders: a pilot effectiveness study. Internet Interv. 2015;2:297–302. doi: 10.1016/j.invent.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svanborg P., Åsberg M. A new self-rating scale for depression and anxiety states based on the Comprehensive Psychopathological Rating Scale. Acta Psychiatr. Scand. 1994;89(1):21–28. doi: 10.1111/j.1600-0447.1994.tb01480.x. [DOI] [PubMed] [Google Scholar]
- Swedish National Board of Health . Dödsorsaker 2013. Artikelnummer 2014-8-5. 2014. Socialstyrelsen. (Stockholm 2014) [Google Scholar]
- Swedish National Board of Health and Welfare . Psykisk ohälsa bland unga. Underlagsrapport till Barns och ungas hälsa, vård och omsorg 2013. 2013. Socialstyrelsen. (Stockholm 2013) [Google Scholar]
- Tillfors M., Andersson G., Ekselius L., Furmark T., Lewenhaupt S., Karlsson A., Carlbring P. A randomized trial of internet-delivered treatment for social anxiety disorder in high school students. Cogn. Behav. Ther. 2011;40:147–157. doi: 10.1080/16506073.2011.555486. [DOI] [PubMed] [Google Scholar]
- Travers M.F., Benton S.A. The acceptability of therapist-assisted, internet-delivered treatment for college students. J. Coll. Stud. Psychother. 2014;28:35–46. [Google Scholar]
- Vlaescu G., Alasjö A., Miloff A., Carlbring P., Andersson G. Features and functionality of the Iterapi platform for internet-based psychological treatment. Internet Interv. 2016;6:107–114. doi: 10.1016/j.invent.2016.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenar C., Kerig P. fifth ed. McGraw Hill International Edition; New York: 2008. Developmental Psychopathology. From Infancy Through Adolescence. [Google Scholar]
- Wenemark M., Fornander L., Borgstedt-Risberg M. Folkhälsovetenskapligt centrum; Linköping: 2006. Östgötens psykiska hälsa. Om unga vuxna. Rapport 2006:4. [Google Scholar]