Abstract
Recent developments in mobile technology, sensor devices, and artificial intelligence have created new opportunities for mental health care research. Enabled by large datasets collected in e-mental health research and practice, clinical researchers and members of the data mining community increasingly join forces to build predictive models for health monitoring, treatment selection, and treatment personalization. This paper aims to bridge the historical and conceptual gaps between the distant research domains involved in this new collaborative research by providing a conceptual model of common research goals. We first provide a brief overview of the data mining field and methods used for predictive modeling. Next, we propose to characterize predictive modeling research in mental health care on three dimensions: 1) time, relative to treatment (i.e., from screening to post-treatment relapse monitoring), 2) types of available data (e.g., questionnaire data, ecological momentary assessments, smartphone sensor data), and 3) type of clinical decision (i.e., whether data are used for screening purposes, treatment selection or treatment personalization). Building on these three dimensions, we introduce a framework that identifies four model types that can be used to classify existing and future research and applications. To illustrate this, we use the framework to classify and discuss published predictive modeling mental health research. Finally, in the discussion, we reflect on the next steps that are required to drive forward this promising new interdisciplinary field.
Highlights
-
•
Clinical researchers and computer scientists increasingly join forces to build predictive models to improve online based mental health treatment.
-
•
We introduce a conceptual framework that helps to classify applications of predictive modeling in the mental health domain.
-
•
The framework can bridge the conceptual gap between mental health and data mining researchers.
1. Introduction
Mental health problems have huge impacts on those affected, their social network, and society at large (Centre for Mental Health, 2010). By 2030, global mental health costs are expected to rise to about 6 trillion dollars per year, which by then will be more than the predicted health costs related to cancer, diabetes and respiratory diseases combined (Bloom et al., 2011). Ample research has been devoted to understanding the underlying causes of (specific) mental health problems, the factors that play a role in recovery, as well as the effectiveness of various therapies. This evidence-based movement has led to substantial improvements in mental health care. At the same time, however, there is a consensus that improvements should be made to more effectively address the global burden of mental health conditions.
E-mental health, the application of information technology in mental health care for the prevention and treatment of psychological disorders, may provide an answer to the global burden of mental health problems. The number of online treatment applications is increasing and can provide help to people who otherwise would remain untreated (Robinson et al., 2010; Titov et al., 2015). Recent advancements in computer and communication science have resulted in a rapid development of the field, which has led to new research opportunities and treatment models. Based on data that clients generate when using an online treatment, predictive models can be developed which support clients as well as therapists.
An example of a development fueled by the technological advancements includes so-called Ecological Momentary Assessments (EMA). Using EMA, a wealth of coarse- and fine-grained data is collected, from heart-rate sensors, physical activity sensors, and other mobile applications, to assess the dynamics of symptoms, affect, behavior and cognition over time, in the natural habitat of the patient (Trull and Ebner-Priemer, 2013). Initially designed as a pen and paper measurement, currently, EMA measures are dominantly collected using electronic devices such as the users' smartphone. EMA enables researchers to measure the users' current state and behavior while engaged in their daily routine (Shiffman et al., 2008; Wichers et al., 2011). Such type of data, however, is also partially collected when users engage into an online based treatment. This information allows to provide users with situational and personalized interventions (Burns et al., 2011) that are tailored to specific user needs. To analyze EMA data and other fine-grained types of data (e.g. log-level data), it is not straight forward to employ traditional statistical approaches such as t-tests, Analysis of Variance, or Ordinary Least Squares (OLS) regression. Although these methods allow to understand the relationship among measures and their influence on the treatment outcome, they neither account for the specific temporal (or sequential) nature of the data nor do they consider complex interaction effects among various measures. This is where new analytical methods come into play.
Promising methods include predictive modeling techniques such as Decision Trees, Bayesian approaches (Langley et al., 1992), Support Vector Machines (Cortes and Vapnik, 1995), and Artificial Neural Networks (Haykin, 2009). In order to apply these methods to the type of sequential data collected in e-mental health applications, the data has to be pre-processed (Hoogendoorn and Funk, 2017). The main objective of this pre-processing step is to derive meaningful variables that can then be used in predictive modeling. To succeed in leveraging the potential of predictive models for the purpose of developing effective interventions, each of the steps requires goal setting, understanding the data, construction of such models, as well as interpretation of the models, understanding user perception of these models, and finally deployment of the models developed. To fulfill all these requirements, an intense interdisciplinary collaboration between clinical researchers and computer scientists is mandatory.
The data science community has to understand therapists' needs, their work process with clients, and decision points. On the other hand, therapists have to understand the technical capabilities, what data might be beneficial and what type of predictions can be derived from it. Only when both sides can communicate effectively, the potential of predictive modeling in improving treatment outcomes can be realized. The success of this collaboration will stand or fall with the development of a common language that we think is necessary to successfully plan new research studies and implement more sophisticated online treatments, which incorporates predictive modeling that utilizes the assessed data during the treatment process, in routine practice. Note that predictive modeling based on observational data should only be used to generate hypothesis on causal effects. Whether these causal effects really exist and could inform clinical decision making has to be studied in subsequent, carefully designed experiments.
In this paper, we introduce a conceptual framework that aims to categorize predictive modeling e-mental health research. In Section 2, we introduce predictive modeling methods and techniques. Section 3 presents the framework, which categorizes the various uses of predictive modeling in mental health research into four classes. In Section 4, we discuss illustrative examples of each model type from the existing literature. Finally, in the discussion, we reflect on identified research gaps, the way in which the framework may help to address these gaps, and expected future challenges.
2. Methods in predictive modeling
In this section, we provide a short introduction to the predictive modeling domain. We define basic terminology, briefly describe supervised learning and evaluation methods to access the performance of such models.
2.1. Terminology
Predictive modeling can be positioned under the broader umbrella term “statistical modeling” (Shmueli, 2010). While traditional statistical approaches focus on explaining data in terms of causality or identify relations, predictive modeling strives to find the model that provides the most accurate predictions. Predictions are derived from so-called attributes or features that are derived from observations. These features are not unlike the variables utilized in traditional statistical approaches. However, traditional statistical approaches, focusing on high explanatory power, do not necessarily lead to a high predictive power (Dawes, 1979; Forster and Sober, 1994).
2.2. Supervised learning approaches
Building predictive models is often done through so-called supervised learning. Fig. 1 provides a general overview of the procedure of this approach. Supervised learning requires “historical” data providing predictive attributes and a target value (e.g. the occurrence of a depressive episode), that we want to predict from new data, where the attributes, but not the target values, are known. Targets can either be continuous values (referred to as regression) or categorical (classification). Data is commonly pre-processed to derive appropriate features from the raw attributes and to compose a training and test set. In addition, an assumption is made on the type of function that may describe the relationship between the features and the target. The set of all possible functions that can explain the observed data is called the hypothesis space. Next, a learning algorithm is applied that uses the training dataset in combination with an error metric to select a final hypothesis from the set of all hypotheses. To estimate the generalizability of this final hypothesis, it is evaluated against a test dataset that was not used in the learning process.
Fig. 1.
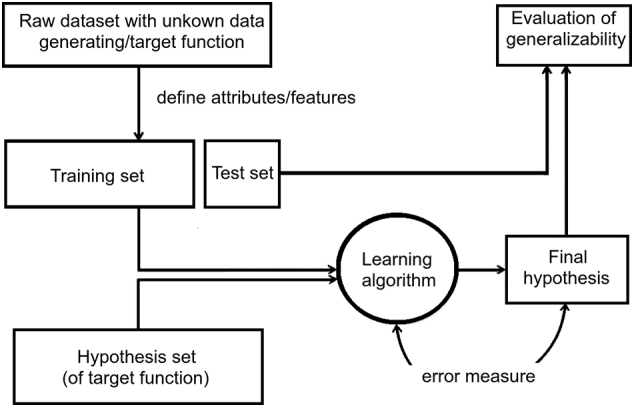
Generic model of a supervised learning approach based on Abu-Mostafa (2013).
Various learning techniques and types of target functions exist. We follow the categorization of Witten and Frank (2005). They distinguish between (1) probabilistic modeling methods such as Naïve Bayes classifiers (see, e.g., Langley et al., 1992), (2) divide-and-conquer modeling methods such as decision trees (Safavian and Landgrebe, 1991), (3) (extended) linear modeling methods such as generalized linear models (e.g. logistic regression), support vector machines (Cortes and Vapnik, 1995), or artificial neural networks (see Haykin, 2009), and (4) instance-based learning methods such as k-nearest neighbors (Altman, 1992). A discussion of these methods is beyond the scope of this paper, but the references provide a good starting point for detailed information.
Supervised learning is a so-called bottom-up approach as it is driven by the data. It is complemented by the top-down approach, which is knowledge-driven. In the latter approach, existing theories are formalized into computational models that connect theoretical concepts from a domain to executable code. Therefore, the top-down approach starts from a theory and typically utilizes model structures that are based on theoretical and empirical insights into the problem domain. There are a multitude of techniques ranging from more mathematical types of modeling such as systems of differential equations (Zeigler et al., 2000) to rule-based or agent-based systems (Van der Hoek and Wooldridge, 2008).
2.3. Evaluating predictive models
The purpose of predictive modeling is to find a model that generalizes well beyond the training data. Evaluation methods are different for regression and classification models. When evaluating regression models, two objective functions that are often used are the mean absolute error (MAE) and the mean squared error (MSE). The right type of error measure is dependent on what type of result is most desirable. The MAE is more suitable if you do not want your performance measure to be highly sensitive to outliers, and the MSE is more suitable if large errors are particularly undesirable.
For evaluating classification models, a great variety of measures such as accuracy (percentage of correctly classified cases), precision (fraction of correct classifications out of all cases attributed to a certain class by the predictive model), or recall (fraction of cases correctly found to be in that class out of all elements in the data that were in the class) are used. When the classification performance of a model depends on a threshold value, as is often the case, the receiver operating characteristic (ROC) curve and the Area Under the Curve (AUC) can be used as performance measures (see e.g. Hanley and McNeil, 1982).
As mentioned, the generalizability of models is often tested on a test dataset, which is kept apart from the training set used to fit the model. When data is limited, a validation method called cross-validation can be used. The method divides the original sample set into k subsets, where k − 1 subsets are used as training samples and one subset is used as a validation and/or test sample. The process is repeated k times, where each of the subsets acts as the test set once, and the performance results are averaged (Olson and Delen, 2008).
3. Framework
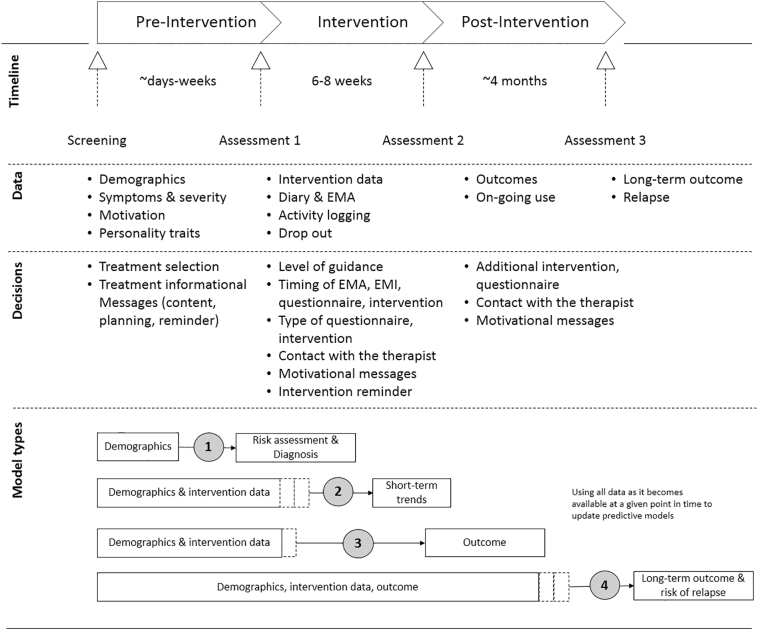
To describe and categorize existing applications of predictive modeling within the mental health domain, we propose a framework. The framework (Fig. 2) provides a common language for researchers and forms the basis for informing treatment decisions and designing new interventions and experiments. The framework has four major elements, which are described below: time (phases), data, decisions, and model types.
Fig. 2.
Proposed framework to categorize predictive modeling in e-mental-health.
3.1. Time
Predictive modeling in mental health naturally tries to uncover meaningful predictive sequential relationships. Hence, the framework is arranged along core phases of the timeline of the psychological intervention. We refer to these phases using the generic, yet recognizable, terms pre-intervention, intervention, and post-intervention to make them applicable across a wide range of mental health settings.
3.2. Data
Along the different phases, the framework identifies different types of data that are collected from participating clients, therapists and the technical systems involved. To predict states related to an individual, not only the data related to that individual could be relevant, but possibly the data from other individuals who have gone through this (or a similar) intervention can also hold predictive power.
Different data are collected in the different phases. In the pre-intervention phase questionnaires or interviews are used to determine the severity of past and current problems. Additionally, socio-demographic data, personality traits, motivation and attitude towards the treatment can be assessed as part of this assessment process.
The largest amount of data is usually collected in the intervention phase. This encompasses, for example, the client's text responses to exercises in the interventions, their logins to the health systems, and other system interactions including technical loggings. Daily diaries are an option for recording the client's development during the intervention (e.g., Bolger et al., 1989; Burton et al., 2009; Jacelon and Imperio, 2005). Smartphone-based EMA enables clients to regularly report relevant variables a few times a day (Wichers et al., 2011). Smartphones can also serve as a rich source of data when usage data, such as call logs and app usage, and sensor data, such as GPS and accelerometer data, are collected (e.g. Lane et al., 2010; Eagle et al., 2009). The high sampling frequency can quickly lead to a large amount of data per client. Whether and when more data leads to better predictive models is the subject of debate (Stange and Funk, 2016). The intervention often ends with a final screening, which can consist of a variety of questionnaires to estimate the remaining symptom severity and to evaluate the improvement of the client.
The post-intervention phase can consist of follow-up screenings and additional or repeated interventions to reduce the risk of relapse (Kessler et al., 2005; Vittengl et al., 2009).
3.3. Decisions
The data described in the previous subsection fuel recommendations and therapeutic decisions. These decisions may influence the course of the treatment and the client's adherence and should aim to improve the therapeutic outcome.
In the pre-intervention phase, one has to decide what intervention and what level of guidance would best suit the client's needs. With moderate symptoms, for example, the client might be best of with a preventive self-help intervention without any personal guidance. When symptoms are severe or the when problems are complex, a guided or blended intervention would perhaps be more appropriate.
During the intervention phase, earlier decisions may need to be corrected on the basis of new information. For instance, the level of guidance might be increased if a client is at risk of dropping out. Keeping the intervention relevant for the client by personalizing it based on his or her behavior could prevent this. The right timing of EMA (Armey et al., 2015; Moskowitz and Young, 2006; Smyth and Stone, 2003) and Ecological Momentary Intervention (EMI) (Heron and Smyth, 2010; Runyan et al., 2013) also represent important decisions during the intervention phase. An optimal timing can minimize the intrusiveness and enhance the client's perception of the intervention.
In the post-treatment phase, additional interventions can be scheduled to maintain the outcome and prevent relapse (Kessler and Chiu, 2005; Vittengl et al., 2009). Usually, Internet-based treatment during this phase also consists of symptom screening and interventions to guide clients after their active treatment (Kok et al., 2014; Lord et al., 2016). Decisions that are seen in all phases are adherence measures that include motivational messages and feedback as well as reminders or contact to the therapist.
3.4. Model types
Predictive models can serve a variety of purposes. Traditionally, predictive models have been limited to prediction based on the data of a certain stage (e.g. at the pre-intervention) to predict what is going to happen in the next stage (e.g. success of the intervention). However, given the higher granularity and quality of the current assessments, more detailed models have become available that may enable predictions over shorter time periods. These models can drive personalized interventions that are fully tailored to observations collected from a specific client. The framework recognizes this by distinguishing four model types. It arranges the model types on the basis of the phase of treatment, the type of data that is available to the models, and the clinical decisions that are made on the basis of the model output. Table 1 presents an overview of the four model types.
Table 1.
Proposed model types of the framework.
| Model type | Predictors | Purpose | Usage |
|---|---|---|---|
| 1 | Pre-intervention | Risk assessment and diagnosis | Identify clients at risk for mental health problems Support diagnostic process Support selection of intervention Estimate level of guidance, EMA, EMI |
| 2 | Pre-intervention and intervention | Short-term trends | Support selection of therapy by therapist Facilitate personalized therapy Support selection of individual decisions, such as next intervention, screening, motivation and level of guidance Identify risk of drop-out Adapt intervention to maximize short-term outcomes Track therapeutic progress |
| 3 | Pre-intervention and intervention | Predict therapy outcome | Support selection of therapy by therapist Facilitate personalized therapy Support selection of individual decisions, such as next intervention, screening, motivation and level of guidance Adapt intervention to maximize treatment outcomes |
| 4 | Pre-intervention, intervention, post-intervention | Stabilize results, prevent relapse | Identifying clients with high relapse risk Facilitate personalized after-care Adapt after-care to maximize long-term outcomes |
Type 1 models predict risk of mental illness and can be used to identify best treatment options. There is extensive research on the predictive power of variables with respect to risk assessment and diagnosis, focusing on a wide variety of variables related to socio-demographic characteristics (see e.g. Tovar et al., 2014; Mittendorfer-Rutz et al., 2014), personality traits (see e.g. Magidson et al., 2014), and illness characteristics (see e.g. Otto et al., 2001; Wade et al., 1998). In the past, this type of research has often employed standard statistical methods like OLS regression and logistic regression. Data available to Type 1 models can be collected through questionnaires, EMA assessments, or shared electronic health records. The time-span of the data collection varies from 1 h (one-time screening instrument administrations), to days (e.g., a one-week diary), or weeks (e.g., EMA assessments).
Type 2 models predict short-term changes of the health status and treatment adherence to optimize treatment and treatment progress. As clients progress through the intervention, more data becomes available, as illustrated in Fig. 2 by the little-dotted boxes. Whenever new data arrive, the client-specific model can be updated, which, on average, increases the power to predict the short-term evolution of key concepts such as the valence of mood or rumination. Based on predicted short-term changes, the next steps of the intervention can be planned. Furthermore, such models might contribute to the client's adherence to the intervention. When the current engagement level is understood and the predicted probability for drop-out is high, motivational interventions can be applied, such as direct contact with the therapist, or a reminding message.
Type 3 models predict the outcome of the intervention phase, based on available data such as socio-demographic data and observations made during the intervention phase. Here, models that estimate and minimize dropout risk are also relevant, but in this case, the focus should be on drop-out over a longer term (which may require qualitatively different interventions than those deployed to reduce short-term drop-out).
Type 4 models aim to predict relapse. This class of models uses data from the pre-intervention phase and the intervention phase to provide a prediction of relapse risk (Kessing, 1999). Type 4 models can help to determine whether patients need after-care, or to decide on an optimal assessment schedule to regularly assess the stability of short-term treatment results.
4. Applying the framework to published research
In this section, we use the introduced framework to categorize published e-mental health research in which predictive models were applied, to illustrate that 1) the framework works in an insightful way and is useful, and 2) the framework covers work done within the field. Discussed papers, their key characteristics, and the relationship to the framework are summarized in Table 2.
Table 2.
Predictive models used in e-mental health.
| Model type | Studya | Data | Prediction | Method | Comment |
|---|---|---|---|---|---|
| 1 | Ankarali et al. (2007) | Social-demographic data | Postpartum depression | Classification tree, logistic regression | Estimation of risk for postpartum depression in women. |
| 1 | Van der Werf et al. (2006) | Time-to-event data | Estimation of recovery probability | Sequential-phase model | Models transitions from non-depressed to depressed states in the general population. Identifies factors that lead to depression. |
| 1 | Gittelman et al. (2015) | Facebook likes | Life expectancy is estimated from Facebook likes | Principal Component Analysis, linear regression | Facebook likes indicate habits and activities, which are used to predict life expectancy. |
| 1 | Pestian and Nasrallah (2010) | Suicide notes | Possible suicide | Support vector machine | The genuinely of suicide notes is estimated. |
| 1 | Burns et al. (2011) | EMA | EMA ratings are inferred from the collected smartphone data | Various types of regression trees | Provides EMI to the user in stressful situations. |
| 1 | Saeb et al. (2015) | GPS movement data | Correlation between GPS and phone usage | K-means for location clustering, and elastic net regularization for prediction of depressive symptoms | The relationship among mobile phone GPS sensor features, EMA ratings, and the PHQ-9 scores is analyzed. |
| 1 | Kim et al. (2015) | Activity measures | Estimation of mood | Hierarchical model | Mood is inferred from physical activity. |
| 1 | Doryab et al. (2014) | Noise level, movement and location data, light intensity, phone usage | Correlation between depression and phone usage and sleep behavior | Tertius algorithm (see Flach and Lachiche, 2001) | Preliminary study on detection of behavior change in people with depression. |
| 1 | Mestry et al. (2015) | Smartphone measures | Estimation of mental state | Correlation | Smartphone data is analyzed for correlation with the mental state such as depression, anxiety or stress. |
| 1 | Demirci et al. (2015) | Pittsburgh Sleep Quality Index, Beck Depression Inventory, Beck Anxiety Inventory | Sleep quality, depression and anxiety score | Correlation | Smartphone use correlates with sleep quality and symptoms of anxiety and depression. |
| 1 | Ma et al. (2012) | Smartphone measures | Estimation of mood | Factor graph | Mood is inferred from data recorded by the personal smartphone. |
| 1 | Likamwa et al. (2013) | Smartphone measures | Estimation of mood | Regression model | Mood is inferred from data recorded by the personal smartphone. |
| 1 | Panagiotakopoulos et al. (2010) | EMA rating and contextual Information | Mental state | Bayesian network | Mental states such as depression, anxiety and stress are estimated from contextual data. |
| 1 | Lu et al. (2012) | Voice samples | Stress estimation from voice samples | Mixture of hidden Markov models | Stress level can be estimated from voice-based features. |
| 1 | Chang et al. (2011) | Speech samples | Emotion recognition | Support vector machine | Library that runs on a smartphone and estimates emotion from speech samples. |
| 1 | Van der Sluis et al. (2012) | Speech samples | Stress estimation | Regression | Stress level of post-traumatic stress disorder patients is estimated from voice samples. |
| 1 | Asselbergs et al. (2016) | Smartphone measures | Estimation of mood | Regression model | Failed replication of Likamwa et al. (2013) |
| 2 | Daugherty et al. (2009) | Mood measures | Estimation of mood swing cycles and treatment influence | Dynamic model | Simulation of treatment and coupling behavior for bipolar individuals. |
| 2 | Both et al. (2010), Both and Hoogendoorn (2011), Both, Hoogendoorn and Klein (2012) | EMA | Simulates client's symptom trajectory | Dynamic model | Allows predictions about the client's recovery curve and simulates the influence of various therapy forms. |
| 2 | Touboul et al. (2010) | EMA | Estimation of recovery curve and relapse risk | Dynamic model | The identification of underlying model parameters allow client specific predictions. |
| 2 | Demic and Cheng (2014) | EMA, clinical data | Prediction of depressive episodes and recovery chance | Finite-state machine, dynamical system | Modeling of occurrence of depressive episodes, and influence of treatment. |
| 2 | Noble (2014) | Questionnaires | Scheduling of face-to-face interventions | Control-theoretic model | Control-theoretic scheduling of psychotherapy based on client individual data. |
| 2 (4) | Patten (2005) | Depression score | Estimated recovery curves | Markov model | Prevalence and recovery from major depressive episodes are estimated with a Markov model |
| 2 | Becker et al. (2016) | Phone usage data, EMA data | Mood of the next day | Lasso Regression, Support Vector Machines, linear regression, Bayesian Hierarchical Regression | Try to predict the mood level of the next day based on reported EMA data and phone usage data |
| 2 | van Breda et al. (2016) | EMA data | Mood of the next day | Linear regression with a bagging approach | Predict the mood of the next day by means of EMA data collected during previous days. Optimize the historical period used for predictions. |
| 2 | Bremer et al. (2017) | Diary data | Current mood | Text mining and Bayesian regression | Clients' activity diary data is used to infer the current mood. |
| 2 | Osmani et al. (2013) | Smartphone measures | Depressive state | Correlation | Smartphone measured of the activity are correlated to the depressive state of bipolar individuals. |
| 3 | Karyotaki et al. (2015) | Demographics | Estimation of drop-out risk factors | Hierarchical Poisson regression modeling | Individual Patient Data Meta-Analysis: raw data from various trials were analyzed to identify drop-out risk factors for web-based interventions. |
| 3 | Kegel and Flückiger (2014) | Self-esteem, mastery, clarification, global Alliance | Treatment dropout | Hierarchical regression | Clients with lower levels of self-esteem, fewer clarifying experiences, and absence of therapeutic alliance are more likely to dropout. |
| 3 | Meulenbeek et al. (2015) | Socio-demographic, personal, and illness-related variables | Treatment dropout | Logistic regression | Dropout estimation for clients with mild panic disorder. |
| 3 | Proudfoot et al. (2013) | Perceived self-efficacy questionnaire | Symptom improvement | Correlation | Perceived self-efficacy reported at the beginning of web-based treatment indicates outcome. |
| 3 | Van et al. (2008) | Hamilton Rating Scale for Depression | Treatment failure | Logistic regression | Early improvement can be used to predict therapy outcome. |
| 3 | Priebe et al. (2011) | Therapeutic relationship | Treatment outcome | χ2 Analysis | Outcome of 9 studies was compared to estimate the predictive capability of therapeutic relationship. |
| 3 | Donkin et al. (2013) | Application usage data | Completion of interventions | Logistic regression | Usage data and its influence on the outcome. |
| 3 | Van Gemert-Pijnen et al. (2014) | Login frequency | Prediction of outcome after therapy | Linear regression model | Client login frequency was correlated with improvement after the therapy. |
| 3 | Whitton et al. (2015) | Collected data about used program features | Outcome prediction | Correlation | Usage of (some) program features was correlated with treatment outcome. |
| 3 | Bennett et al. (2011) | Session based outcome questionnaire | Treatment outcome | Various methods | Treatment outcome estimation based on session based questionnaires. |
| 3 | Perlis (2013) | Socio-demographics, self-reported clinical data | Treatment resistance | Naïve Bayes, logistic regression, support vector machine, random forest | Treatment resistance is predicted based on self-reported data. |
| 3 | Hoogendoorn et al. (2017) | Socio-demographics, emails sent by patient | Treatment success | Logistic regression, decision tree, random forest | Treatment success is predicted based on the text contained in the emails sent by the patient to the therapist. |
| 4 | Kessing (1999) | ICD-10 Depression rating | Relapse risk, suicide risk | Cox-regression | The risk of relapse is significantly related to the severity of baseline and post-treatment depression. |
| 4 | Busch et al. (2012) | Demographics, medication, clinical data | Predict one year follow up outcome | Hierarchical logistic regression | The outcome of bipolar clients at one year follow up is predicted using clinical data. |
| 4 | Farren and McElroy (2010) | Demographics, previous drinking characteristics, comorbidity | Alcoholic relapse risk | Logistic regression | Relapse after 3 or 6 months of clients with alcohol-dependence and depression or bipolar disorder. |
| 4 | Farren et al. (2013) | Demographics, previous drinking characteristics, comorbidity | Alcoholic relapse risk | Logistic regression | Longitudinal outcome after 2 years of clients with alcohol-dependence and depression or bipolar disorder. |
| 4 | Pedersen and Hesse (2009) | Demographics, previous drinking characteristics | Alcoholic relapse risk | Logistic regression | Based on demographics and previous drinking behavior the alcoholic relapse risk is predicted. |
| 4 | van Voorhees et al. (2008) | Mood, social and cognitive vulnerability | relapse risk | Regression trees | Estimation of depression relapse risk. |
| 4 | Gustafson et al. (2014) | GPS position | Trigger EMI | Previously entered locations | EMI is triggered in locations where alcohol was obtained in the past. |
| 4 | Chih et al. (2014) | Weekly assessed EMA ratings | Predict relapse risk in coming week | Bayesian network model | Bases on weekly surveys, the relapse risk in the coming week of previously alcohol-dependent clients is predicted. |
| 4 | Aziz et al. (2009) | Ambient measures | Triggers EMI, notifies family members or supervisors | Temporal trace langue rules | A support agent that triggers EMI or notifies medical staff based on monitoring techniques designed to identify risk of relapse. |
Studies are listed in the order in which they were presented in the main text.
4.1. Model Type 1: risk assessment
Type 1 models aim for the prediction of mental health problems. One way of achieving this goal is to apply data mining techniques to (re-)analyze existing epidemiological data, to identify illness risk factors that might not be easily detected with more traditional statistical techniques. For example, Ankarali et al. (2007) compared the performance of classification trees, a supervised modeling technique, to standard logistic regression in determining social-demographic risk factors for postpartum depression in women. The classification tree identified six risk factors, while the logistic regression model found only three. Another example is the study by Van der Werf et al. (2006) who used a large Dutch epidemiological database to create a mathematical model of the recovery from depression in the general population.
Relevant data for identifying people with health risks can also be collected through popular social media, such as Facebook and Twitter. In a study conducted by Gittelman et al. (2015), for example, Facebook “likes” were collected to predict mortality, using Principal Component Analysis (to reduce the high-dimensional predictor space), followed by Bootstrap Regression (a regression technique that is less vulnerable to violations of statistical assumptions). The model with Facebook likes and basic demographic features was better than either one alone. In this context, advances in automated text analysis are also promising. For example, Pestian and Nasrallah (2010) explored whether text mining techniques could be used to identify genuine suicide notes. In their study, the predictive model proved to be better in this task than mental health professionals (78% vs. 63%, respectively).
Technological progress allows to continuously acquire data on an individual level. For example, several studies suggest that depressive symptoms could possibly be monitored unobtrusively, without explicit user input, using predictive models built from smartphone log-file data. Building on a pilot study of Burns et al. (2011), Saeb et al. (2015) analyzed the connection between users' daily movement patterns, estimated from their phones' GPS records, and the presence of depressive symptoms. Various features of the users' movements were derived from these data, such as the variance in location visits. To determine client-specific locations of importance, Saeb et al. (2015) used a variant of the K-means clustering algorithm (Arthur and Vassilvitskii, 2007), an unsupervised learning technique that finds optimal partitions of multivariate data. Patterns in location cluster visits were found to be correlated with depressive symptoms as assessed by a self-report questionnaire. As a result, the presence of clinical levels of depression could be detected with a high degree of accuracy. The relevance of mobility and activity monitoring was further demonstrated in studies of Kim et al. (2015) and Osmani et al. (2013).
Several other studies explored the usefulness of smartphone logfiles to detect mental health problems in healthy participants. Doryab et al. (2014) used phone call logs and phone light sensor data as proxies of users' social and sleeping behavior. Findings suggested that clear changes in outgoing calls were associated with changes in depressive symptoms. Similar findings were reported by Mestry et al. (2015), who concluded that predicting a possible range of depression, stress and anxiety is more feasible than predicting absolute values. Demirci et al. (2015) investigated the relationship between smartphone usage and sleep quality, depression, and anxiety in a student sample. Increased smartphone usage was found to be related to more symptoms of depression, anxiety, and lower sleep quality. Similar results were reported by Ma et al. (2012) and Likamwa et al. (2013), who were able to predict mood scores with an accuracy of 50% and 93%, respectively, based on variables that were collected on the smartphone.
The predictive accuracy of the models may be further increased by capturing contextual information, either through unobtrusive assessment or through prompted self-report questionnaires. Panagiotakopoulos et al. (2010) collected such data from 27 anxiety clients over 30 days, five times a day (allowing participants to make additional ratings freely at any time). Using Bayesian networks, they were able to infer stress levels from EMA data with an average accuracy of 84%.
Voice recordings, which can be unobtrusively sampled through the microphones of smartphones, might provide another source for health screening applications. Lu et al. (2012) analyzed voice recordings to estimate stress levels and found changes in pitch to be correlated with stress levels. Chang et al. (2011) showed that voice analysis programs can estimate current affection or stress levels, using smartphone-based voice analysis software. Van der Sluis et al. (2012) found that, in addition to pitch, other speech features such as amplitude, zero crossings, power, and high-frequency power are also useful predictors of stress levels of patients with post-traumatic stress disorder (PTSD).
As suggested by the studies discussed, Type 1 models most probably will find their way into future e-mental health in the form of smartphone applications. For this, it is important that the promising preliminary findings, which are often based on small-sample pilot studies, are corroborated by adequately powered independent replication studies. The findings of Likamwa et al. (2013), for example, could not be replicated in a follow-up study (Asselbergs et al., 2016).
4.2. Model Type 2: short-term predictions during treatment
Type 2 models target the prediction of patients' states as they evolve during the intervention. Studies have shown that tracking patients' states can improve treatment adherence and treatment outcomes by providing a feedback cycle (Lambert, 2010; Miller et al., 2006). For this, traditional self-report questionnaires can be administered regularly, for instance, every two weeks. If necessary, these coarse-grained assessments can be complemented by more fine-grained daily smartphone-based assessments (Torous et al., 2015). The distinction between Type 1 and Type 2 models is not always clear-cut. When Type 1 models and applications are used during treatment to make short-term predictions of health states to inform decisions on the course of treatment, the models should be classified as Type 2. Type 2 models can also be more advanced, since more detailed data from the ongoing treatment is available to inform the modeling process (i.e., log-data of web-based treatment platforms, therapist input, and extensive diagnostic data)
Type 2 models explicitly consider the patient in the context of treatment. Daugherty et al. (2009) used oscillating differential equations to predict hypomanic, stable, and depressive episodes in patients diagnosed with bipolar disorder. Their model incorporates the effects of medication treatment and behavior coupling between patients. Medication treatment slows the rapid mood changes and dampens the amplitude of mood oscillations. Patients with a similar cycle synchronize over time, whereas patients with an opposite cycle remain in an opposite cycle.
Becker et al. (2016) exploit phone usage data and previous EMA measurements to predict the reported value for mood for an experiment with a group of students. For phone usage data they include app usage, activity levels, number of phone calls, and number of text messages sent. They apply a variety of data mining techniques including Support Vector Machines, Lasso and Linear regression, and Bayesian Hierarchical Regression. They create a general model as well as user level models and are able to achieve a root mean squared error of 0.83 using the Lasso Regression approach with the user level approach.
Similarly, van Breda et al. (2016) try to predict mood for the next day using self-reported EMA data of depressed patients during previous days. They optimize the number of days taken into account in their features to predict the mood value for the next day. They build individual patient models and use a combination of linear regression models (using a so-called bagging approach).
Another possibility to understand clients' mood trajectories are online diaries that are part of online interventions. Bremer et al. (2017) demonstrate that the clients' mood on a specific day can be inferred based on their diary data. In a 2-phase modeling approach, they employ techniques from text mining to first extract activities that were likely described in the diary entries by the user. In the subsequent step, the set of relevant activities is used to successfully predict the clients' mood using an ordered logit model.
Another clear Type 2 model is the ‘virtual patient’ model of Both et al. (2010). This model describes the relationships between different client states such as mood, thoughts, and coping skills as a system of differential equations, which allows simulation of the development of patient states over time. As discussed in our overview of predictive modeling approaches, such a model is developed using a top-down approach, where domain knowledge is formalized in a computational model. With the model, the development of internal states can be simulated to predict mood during treatment. The model incorporates hypothesized working mechanisms of different therapeutic interventions, such as activity scheduling or cognitive behavior therapy (CBT), to enable simulations of the potential effects of these interventions, which in turn could be used to identify the intervention that could benefit the patient the most (Both and Hoogendoorn, 2011). To do this effectively, additional model states are necessary to account for external variables that are not controllable by the client (Both, Hoogendoorn and Klein, 2012). Similar approaches, using different computational techniques, have been proposed by Touboul et al. (2010), Demic and Cheng (2014), Noble (2014), and Patten (2005).
4.3. Model Type 3: predicting treatment outcome
Type 3 models predict treatment outcome (including drop-out) during active treatment. Rather than focusing on the relationship between short-term symptom dynamics and treatment decisions, these models aim to predict the outcome of the full therapeutic process (i.e., the post-test results) from data that are collected before and during treatment. This outcome has two aspects: 1) the change in health symptoms (which is typically known as the vector of continuous mental health questionnaire scores), and 2) whether or not treatment was provided as intended (which is typically a binary variable, flagging the treatment as drop-out for patients who did not complete a predetermined minimum percentage of treatment).
Using regression techniques, clinical researchers have been exploring Type 3 models, using predictors that were collected at baseline (pre-test) assessments (e.g., DeRubeis et al., 2014; Huibers et al., 2015; Karyotaki et al., 2015; Kegel and Flückiger, 2014; Meulenbeek et al., 2015), mental health questionnaire responses that were collected during treatment (e.g., Proudfoot et al., 2013; Van et al., 2008), or repeated measures of the therapeutic relationship between the patient and the therapists (e.g., Priebe et al., 2011). In these studies, researchers tend to focus more on the importance of individual predictors on a population level (i.e., risk factors), rather than on the predictive power of the model as a whole.
Recent studies suggest that logfiles of electronic treatment delivery systems might also provide useful detailed predictors of treatment outcome. The number of logins, actions per login, completed modules, and time spent are metrics that can identify differences between adherers and non-adherers (Donkin et al., 2013). Van Gemert-Pijnen et al. (2014), for example, found user login frequency to be correlated with depressive symptoms after treatment. Whitton et al. (2015) examined the correlation between the usage of program features and outcomes in a study of a web-based self-help intervention for symptoms of depression and anxiety. The usage of diary functions and SMS reminding was not correlated with outcome, nor did the number of interventions (both started and completed) have an impact on symptom reduction. The symptom tracking functionality, which enabled users to track their improvement, also had no influence on the final treatment result. However, the use of the reminder function of the symptom tracking tool had a positive influence on the outcome.
Advanced data mining techniques have been used to build Type 3 models as well. For example, Bennett et al. (2011) used (naïve) Bayesian classifiers and Random Forest decision trees (see Breiman et al., 1984) to predict treatment outcomes from health questionnaires that were collected at each treatment session. Early reductions in symptom levels were found to be a significant predictor of treatment outcome. Using 10-fold cross-validation, the predictive accuracy of the various classification models varied between 60% and 76%.
Early detection of clients at high risk for treatment resistance could also be helpful, for example, to decide on the optimal level of therapist guidance in a web-based treatment. Perlis (2013) used self-reported socio-demographic and clinical variables to predict treatment resistance. With multivariate models such as logistic regression, naïve Bayes and Support Vector Machines, the authors achieved an AUC of 0.71, indicating fair predictive performance.
An approach that utilizes free text written by patients is proposed in Hoogendoorn et al. (2017). They extracted features from the text messages sent by patients suffering from an anxiety disorder to their therapist as part of an anxiety treatment. Features included word usage, sentiment, response rate, length of email, phrasing of the emails, and topics that patients wrote about in their emails. They were aimed at predicting a reliable improvement in the so-called Social Phobia Measure and were able to achieve AUCs of around 0.83 halfway through the therapy and similar scores at the end, which is significantly better than using baseline data only.
4.4. Model Type 4: models for relapse prediction
Type 4 models focus on predicting the risk of relapse, that is, the re-occurrence of symptoms in the long term. Typically, the relapse risk determines the amount of aftercare required. The design of interventions and treatment platforms for relapse prevention training is similar to that of treatment platforms and interventions used in regular treatment (Barnes et al., 2007; Holländare et al., 2013; Lobban et al., 2015). To stabilize the condition of patients, aftercare can be provided in the form of screenings and interventions.
As with Type 3 models, clinical researchers have used traditional regression techniques such as logistic regression to predict relapse in patients diagnosed with a variety of disorders, including depression (e.g., Kessing, 1999), bipolar depression (Busch et al., 2012), and alcohol misuse (Farren and McElroy, 2010; Pedersen and Hesse, 2009). More advanced statistical techniques have also been applied. For instance, Patten (2005) analyzed data from several clinical depression trials to estimate the parameters of a Markov model, and Van Voorhees et al. (2008) identified risk factors through regression tree modeling.
Type 4 models can support mental health specialists to assess the risk of relapse in their patients, to scale-up after-care when needed. More likely, however, is that these models will find their way into mobile self-help applications. If so, these models will probably perform better because the models will then be able to take current contextual information of the patient into account, resulting in more options to personalize interventions. According to Juarascio et al. (2015), context-aware interventions are expected to appear for treatment and relapse prevention for a variety of health problems, due to the rapid developments in sensor technology and mobile applications. Gustafson et al. (2014) and Chih et al. (2014) implemented Bayesian network modeling in an EMA/EMI smartphone application aimed at reducing relapse for recovering alcohol-dependent individuals. In this app, relapse-prevention interventions are triggered when the risk of relapse occurrence is estimated to be high based on the EMA ratings (including unobtrusive contextual variables). In a validation study, the model achieved an AUC of 0.91 in predicting relapse in the following week. A similar EMA/EMI approach was proposed by Aziz et al. (2009), who developed a rule-based support agent that monitors client conditions to trigger EMI when the risk of relapse is predicted to be high, based on the client's mental health state, social interactions, estimated substance use, and physiological conditions.
5. Discussion
In this paper, we provided a brief introduction to predictive modeling methods, introduced a common framework for understanding applications of predictive modeling in mental health, and applied the framework to categorize published mental health research in which predictive modeling techniques were applied. Doing so, we aimed to contribute to the development of a common language between clinical researchers and members of the data mining community.
With this framework, opportunities can be identified to extend and improve an emerging field. For instance, our preliminary literature review suggests that e-mental health researchers should perhaps focus more on the validity of model predictions rather than the more traditional goal of identifying specific predictors. Demonstrating the relevance of a specific predictor has theoretical relevance. However, single predictors rarely provide a basis for predictions of variables that are relevant to clinical practice. In practice, often only a fraction of the variance of the target variable of interest is explained. In comparison with clinical researchers, data miners are more used (and more tolerant) to focusing on the accurate prediction of high-value target variables while focusing less on the specific predictors that play a role in this prediction. It would be interesting to learn more about the relative merits of this approach in e-mental health applications.
We also identified room for improvement in the proper application of predictive modeling methodology. We found that several studies do not use independent test sets to evaluate experimental modeling techniques. Proper testing (validation) of models is of utmost importance to investigate the generalizability of proposed models. Patterns in available data can often be modeled well, but more importantly testing a model on to unseen data is critical to test generalizability, as explained in the first section of this paper. The current wealth of data collected in e-mental health applications provides many opportunities to use test sets for model validation, and we urge researchers to apply this technique more. Furthermore, utilization of predictive modeling can have pitfalls such as estimation of a spurious correlation due to an involuntarily introduced bias or a systematic error during study design (Pearl, 2009; Sjölander, 2009). Especially, with the larger amount of data collected during online intentions this effect can magnify (Khoury and Ioannidis, 2014).This emphasis the need for a common language and understanding of the subject.
Some identified studies, relevant to mental health care, could not be readily classified with the proposed framework. These studies focused on the modeling of mental processes, without explicit links to psychotherapeutic intervention. By focusing on the therapeutic purpose of the modeling, the framework stresses the need for empirical validation of model performance in clinical settings, which is more stringent (i.e., prediction errors are more serious when they provide the basis for clinical treatment decisions). Nonetheless, these studies apply predictive modeling to processes that are relevant to mental health care. The framework may need to be extended to incorporate this type of research more easily.
We would like to stress that our review of available predictive modeling mental health research should not be considered exhaustive. Although we feel that the papers identified are representative for the field, we cannot rule out that important publications were missed, especially since the number of modeling studies seems to be rising each month. In our view, this illustrates the need for conceptual frameworks such as the one proposed in this paper, so that the growing body of research initiatives can be more easily understood, categorized, and evaluated.
In this paper, we could only provide a brief overview of data mining methods. While our framework should promote a shared understanding of high-level research goals, we also acknowledge that productive collaboration in this field requires researchers to gain a deeper and better understanding of data mining methods. To promote this, we suggest that authors make a deliberate effort to thoroughly explain core aspects of data mining methods applied when they publish predictive modeling mental health care research (i.e., to contribute to the development of a common language by providing basic descriptions of core methods to which clinical researchers may be less familiar).
E-mental health is a rich interdisciplinary research field that enables many new research approaches, of which predictive modeling appears to be most promising. The framework proposed in this paper might serve to bridge the conceptual gap between psychologists and predictive modelers. The framework provides a common language for classifying predictive modeling mental health research, which may help to promote constructive and productive interdisciplinary research and to identify new research opportunities.
Conflict of interest
There are no conflicts of interest.
References
- Abu-Mostafa Y. Caltech. AMLBook; 2013. Learning From Data.http://work.caltech.edu/lectures.html Retrieved from. [Google Scholar]
- Altman N.S. An introduction to kernel and nearest-neighbor nonparametric regression. Am. Stat. 1992;46(3):175–185. [Google Scholar]
- Ankarali H., Canan A., Akkus Z. Comparison of logistic regression model and classification tree: an application to postpartum depression data. Expert Syst. Appl. 2007;32(4):987–994. [Google Scholar]
- Armey M.F., Schatten H.T., Haradhvala N., Miller I.W. Ecological momentary assessment (EMA) of depression-related phenomena. Curr. Opin. Psychiatry. 2015;4:21–25. doi: 10.1016/j.copsyc.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arthur D., Vassilvitskii S. Presented at: Annual ACM-SIAM Symposium on Discrete Algorithms. 2007. K-means++: the advantages of careful seeding; pp. 1027–1035. (Philadelphia, PA, USA) [Google Scholar]
- Asselbergs J., Ruwaard J., Ejdys M., Schrader N., Sijbrandij M., Riper H. Mobile phone-based unobtrusive ecological momentary assessment of day-to-day mood: an explorative study. J. Med. Internet Res. 2016;18(3) doi: 10.2196/jmir.5505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aziz A.A., Klein M.C.A., Treur J. Proceedings - 2009 IEEE/WIC/ACM International Conference on Web Intelligence and Intelligent Agent Technology - Workshops, WI-IAT Workshops 2009. vol. 3. 2009. Modeling an ambient agent to support depression relapse prevention; pp. 335–340. [Google Scholar]
- Barnes C., Harvey R., Mitchell P., Smith M., Wilhelm K. Evaluation of an online relapse prevention program for bipolar disorder. Dis. Manag. Health Out. 2007;15(4):215–224. [Google Scholar]
- Becker D., Bremer V., Funk B., Asselbergs J., Riper H., Ruwaard J. Americas Conference on Information Systems! AMCIS 2016: San Diego. 2016. How to predict mood? Delving into features of smartphone-based data; p. 2016. [Google Scholar]
- Bennett C., Doub T., Bragg A., Luellen J., Van Regenmorter C., Lockman J., Reiserer R. Proceedings - 2011 1st IEEE International Conference on Healthcare Informatics, Imaging and Systems Biology, HISB 2011. 2011. Data mining session-based patient reported outcomes (PROs) in a mental health setting: toward data-driven clinical decision support and personalized treatment; pp. 229–236. [Google Scholar]
- Bloom D.E., Cafiero E.T., Jané-Llopis E., Abrahams-Gessel S., Bloom L.R., Fathima S., Feigl A.B., Gaziano T., Mowafi M., Pandya A., Prettner K., Rosenberg L., Seligman B., Stein A.Z., Weinstein C. World Economic Forum; Geneva: 2011. The Global Economic Burden of Noncommunicable Diseases. [Google Scholar]
- Bolger N., DeLongis A., Kessler R.C., Schilling E.A. Effects of daily stress on negative mood. J. Pers. Soc. Psychol. 1989;57(5):808–818. doi: 10.1037//0022-3514.57.5.808. [DOI] [PubMed] [Google Scholar]
- Both F., Hoogendoorn M. Neural Information Processing. 2011. Utilization of a virtual patient model to enable tailored therapy for depressed patients; pp. 700–710.http://link.springer.com/chapter/10.1007/978-3-642-24965-5_79 Retrieved from. [Google Scholar]
- Both F., Hoogendoorn M., Klein M.C.A., Treur J. Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics) 2010. Computational modeling and analysis of therapeutical interventions for depression. [Google Scholar]
- Both F., Hoogendoorn M., Klein M.C.A. In Proceedings - 2012 IEEE/WIC/ACM International Conference on Intelligent Agent Technology, IAT 2012. Vol. 2. 2012. Validation of a model for coping and mood for virtual agents; pp. 382–389. [Google Scholar]
- Breiman L., Friedman J., Stone C.J., Olshen R.A. CRC Press; 1984. Classification and Regression Trees. [Google Scholar]
- Bremer V., Becker D., Funk B., Lehr D. Proceedings of the Twenty-Fifth Conference on Information Systems (ECIS 2017) 2017. Predicting the individual mood level based on diary data. [Google Scholar]
- Burns M.N., Begale M., Duffecy J., Gergle D., Karr C.J., Giangrande E., Mohr D.C. Harnessing context sensing to develop a mobile intervention for depression. J. Med. Internet Res. 2011;13(3) doi: 10.2196/jmir.1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton C., Weller D., Sharpe M. Functional somatic symptoms and psychological states: an electronic diary study. Psychosom. Med. 2009;71(1):77–83. doi: 10.1097/PSY.0b013e31818f2acb. [DOI] [PubMed] [Google Scholar]
- Busch A.B., Neelon B., Zelevinsky K., He Y., Normand S.T. Accurately predicting bipolar disorder mood outcomes. Med. Care. 2012;50(4):311–319. doi: 10.1097/MLR.0b013e3182422aec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centre for Mental Health . Centre for Mental Health; London: 2010. Economic and Social Costs of Mental Health Problems in 2009/10.https://www.centreformentalhealth.org.uk/Handlers/Download.ashx?IDMF=6a98a6da-b9f5-4a07-b88a-067976a0bf5b Retrieved from. [Google Scholar]
- Chang K., Fisher D., Canny J. Proceedings of PhoneSense. 2011. Ammon: a speech analysis library for analyzing affect, stress, and mental health on mobile phones.http://www.cs.berkeley.edu/~jfc/papers/11/AMMON_phonesense.pdf Retrieved from. [Google Scholar]
- Chih M.Y., Patton T., McTavish F.M., Isham A.J., Judkins-Fisher C.L., Atwood A.K., Gustafson D.H. Predictive modeling of addiction lapses in a mobile health application. J. Subst. Abuse Treat. 2014;46(1):29–35. doi: 10.1016/j.jsat.2013.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortes C., Vapnik V. Support-vector networks. Mach. Learn. 1995;20(3):273–297. [Google Scholar]
- Daugherty D., Roque-Urrea T., Urrea-Roque J., Troyer J., Wirkus S., Porter M.a. Mathematical models of bipolar disorder. Commun. Nonlinear Sci. Numer. Simul. 2009;14(7):2897–2908. [Google Scholar]
- Dawes R.M. The robust beauty of improper linear models in decision making. Am. Psychol. 1979;34(7):571–582. [Google Scholar]
- Demic S., Cheng S. Modeling the dynamics of disease states in depression. PLoS One. 2014;9(10) doi: 10.1371/journal.pone.0110358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demirci K., Akgönül M., Akpinar A. Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. J. Behav. Addict. 2015;4(2):85–92. doi: 10.1556/2006.4.2015.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeRubeis R.J., Cohen Z.D., Forand N.R., Fournier J.C., Gelfand L.A., Lorenzo-Luaces L. The personalized advantage index: translating research on prediction into individualized treatment recommendations. A demonstration. PLoS One. 2014;9(1):1–8. doi: 10.1371/journal.pone.0083875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donkin L., Hickie I.B., Christensen H., Naismith S.L., Neal B., Cockayne N.L., Glozier N. Rethinking the dose-response relationship between usage and outcome in an online intervention for depression: randomized controlled trial. J. Med. Internet Res. 2013;15(10) doi: 10.2196/jmir.2771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doryab A., Min J.K., Wiese J., Zimmerman J., Hong J.I. Proceedings of 20017 AAAI Workshop on Modern Artificial Intelligence for Health Analytics (MAIHA) 2014. Detection of behavior change in people with depression. [Google Scholar]
- Eagle N., Pentland A.S., Lazer D. Inferring friendship network structure by using mobile phone data. Proc. Natl. Acad. Sci. 2009;106(36):15274–15278. doi: 10.1073/pnas.0900282106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farren C.K., McElroy S. Predictive factors for relapse after an integrated inpatient treatment programme for unipolar depressed and bipolar alcoholics. Alcohol Alcohol. 2010;45(6):527–533. doi: 10.1093/alcalc/agq060. [DOI] [PubMed] [Google Scholar]
- Farren C.K., Snee L., Daly P., McElroy S. Prognostic factors of 2-year outcomes of patients with comorbid bipolar disorder or depression with alcohol dependence importance of early abstinence. Alcohol Alcohol. 2013;48(1):93–98. doi: 10.1093/alcalc/ags112. [DOI] [PubMed] [Google Scholar]
- Flach P.A., Lachiche N. Confirmation-guided discovery of first-order rules with Tertius. Mach. Learn. 2001;42(1–2):61–95. [Google Scholar]
- Forster M., Sober E. How to tell when simpler, more unified, or less ad hoc theories will provide more accurate predictions. Br. J. Philos. Sci. 1994;45(1):1–35. [Google Scholar]
- Gittelman S., Lange V., Crawford C.A.G., Okoro C.A., Lieb E., Dhingra S.S., Trimarchi E. A new source of data for public health surveillance: Facebook likes. J. Med. Internet Res. 2015;17(4) doi: 10.2196/jmir.3970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson D.H., McTavish F.M., Chih M., Atwood A.K., Johnson R.A., Boyle M.G., Levy M.S., Driscoll H., Chisholm S.M., Dillenburg L., Isham A., Shah D. A smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA Psychiat. 2014;71(5):566–572. doi: 10.1001/jamapsychiatry.2013.4642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanley J.A., McNeil B.J. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- Haykin S.S. vol. 3. Pearson Education; Upper Saddle River: 2009. Neural Networks and Learning Machines. [Google Scholar]
- Heron K.E., Smyth J.M. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behavior treatments. Br. J. Health Psychol. 2010;15(1):1–39. doi: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holländare F., Anthony S.A., Randestad M., Tillfors M., Carlbring P., Andersson G., Engström I. Two-year outcome of internet-based relapse prevention for partially remitted depression. Behav. Res. Ther. 2013;51(11):719–722. doi: 10.1016/j.brat.2013.08.002. [DOI] [PubMed] [Google Scholar]
- Hoogendoorn M., Funk B. Springer; 2017. Machine Learning for the Quantified Self. [Google Scholar]
- Hoogendoorn M., Berger T., Schulz A., Stolz T., Szolovits P. Predicting social anxiety treatment outcome based on therapeutic email conversations. IEEE J. Biom. Health Inform. 2017;21(5):1449–1459. doi: 10.1109/JBHI.2016.2601123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huibers M.J.H., Cohen Z.D., Lemmens L.H.J.M., Arntz A., Peeters F.P.M.L., Cuijpers P., DeRubeis R.J. Predicting optimal outcomes in cognitive therapy or interpersonal psychotherapy for depressed individuals using the personalized advantage index approach. PLoS One. 2015;10(11) doi: 10.1371/journal.pone.0140771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacelon C.S., Imperio K. Participant diaries as a source of data in research with older adults. Qual. Health Res. 2005;15(7):991–997. doi: 10.1177/1049732305278603. [DOI] [PubMed] [Google Scholar]
- Juarascio A.S., Manasse S.M., Goldstein S.P., Forman E.M., Butryn M.L. Review of smartphone applications for the treatment of eating disorders. Eur. Eat. Disord. Rev. 2015;23(1):1–11. doi: 10.1002/erv.2327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karyotaki E., Kleiboer A., Smit F., Turner D.T., Pastor A.M., Andersson G., Cuijpers P. Predictors of treatment dropout in self-guided web-based interventions for depression: an “individual patient data” meta-analysis. Psychol. Med. 2015;45(13):2717–2726. doi: 10.1017/S0033291715000665. [DOI] [PubMed] [Google Scholar]
- Kegel A.F., Flückiger C. Predicting psychotherapy dropouts: a multilevel approach. Clin. Psychol. Psychother. 2014 doi: 10.1002/cpp.1899. [DOI] [PubMed] [Google Scholar]
- Kessing L.V. Severity of depressive episodes according to ICD ^10: prediction of risk of relapse and suicide. Br. J. Psychiatry. 1999;184(2):153–156. doi: 10.1192/bjp.184.2.153. [DOI] [PubMed] [Google Scholar]
- Kessler R., Chiu W. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Arch. Gen. Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Berglund P., Demler O., Jin R., Merikangas K.R., Walters E.E. Lifetime prevalence and age-of-onset distributions of. Arch. Gen. Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Khoury M.J., Ioannidis J.P.A. Big data meets public health. Science. 2014;346(6213):1054–1055. doi: 10.1126/science.aaa2709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J., Nakamura T., Kikuchi H., Yoshiuchi K., Sasaki T., Yamamoto Y. Covariation of depressive mood and spontaneous physical activity in major depressive disorder: toward continuous monitoring of depressive mood. IEEE J. Biomed. Health Inform. 2015;19(4):1347–1355. doi: 10.1109/JBHI.2015.2440764. [DOI] [PubMed] [Google Scholar]
- Kok G., Bockting C., Burger H., Smit F., Riper H. Mobile cognitive therapy: adherence and acceptability of an online intervention in remitted recurrently depressed patients. Internet Interventions. 2014;1(2):65–73. [Google Scholar]
- Lambert M. Yes, it is time for clinicians to routinely monitor treatment outcome. In: Duncan Barry L., Miller Scott D., Wampold Bruce E., Hubble Mark A., editors. The Heart and Soul of Change: Delivering What Works in Therapy. 2nd ed. American Psychological Association; Washington, DC, US: 2010. pp. 239–266. [Google Scholar]
- Lane N.D., Miluzzo E., Lu H., Peebles D., Choudhury T., Campbell A.T. A survey of mobile phone sensing. IEEE Commun. Mag. 2010;48(9):140–150. [Google Scholar]
- Langley P., Iba W., Thompson K. vol. 90. AAAI; 1992. An Analysis of Bayesian Classifiers; pp. 223–228. [Google Scholar]
- Likamwa R., Liu Y., Lane N.D., Zhong L. MobiSys '13 Proceeding of the 11th Annual International Conference on Mobile Systems, Applications, and Services. 2013. MoodScope: building a mood sensor from smartphone usage patterns; pp. 389–402. [Google Scholar]
- Lobban F., Dodd A.L., Dagnan D., Diggle P.J., Griffiths M., Hollingsworth B., Jones S. Feasibility and acceptability of web-based enhanced relapse prevention for bipolar disorder (ERPonline): trial protocol. Contemp. Clin. Trials. 2015;41:100–109. doi: 10.1016/j.cct.2015.01.004. [DOI] [PubMed] [Google Scholar]
- Lord S., Moore S.K., Ramsey A., Dinauer S., Johnson K. Implementation of a substance use recovery support mobile phone app in community settings: qualitative study of clinician and staff perspectives of facilitators and barriers. JMIR Ment. Health. 2016;3(2) doi: 10.2196/mental.4927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu H., Frauendorfer D., Rabbi M., Mast M.S., Chittaranjan G.T., Campbell A.T., Choudhury T. Proceedings of the 2012 ACM Conference on Ubiquitous Computing. ACM; 2012. Stresssense: detecting stress in unconstrained acoustic environments using smartphones; pp. 351–360. [Google Scholar]
- Ma Y., Xu B., Bai Y., Sun G., Zhu R. Wearable and Implantable Body Sensor Networks (BSN), 2012 Ninth International Conference on. 2012. Daily mood assessment based on mobile phone sensing; pp. 142–147. [Google Scholar]
- Magidson J.F., Roberts B.W., Collado-Rodriguez A., Lejuez C.W. Theory-driven intervention for changing personality: expectancy value theory, behavioral activation, and conscientiousness. Dev. Psychol. 2014;50:1442–1450. doi: 10.1037/a0030583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mestry M., Mehta J., Mishra A., Gawande K. Communication, Information Computing Technology (ICCICT), 2015 International Conference. 2015. Identifying associations between smartphone usage and mental health during depression, anxiety and stress; pp. 1–5. [Google Scholar]
- Meulenbeek P., Seeger K., ten Klooster P.M. Dropout prediction in a public mental health intervention for sub-threshold and mild panic disorder. Cogn. Behav. Ther. 2015;8(January) [Google Scholar]
- Miller Scott D., Duncan Barry L., Brown Jeb, Sorrell R., Chalk M.B., Miller S.D.…Sorrell R. Using Formal Client Feedback to Improve Retention and Outcome: Making Ongoing, Real-time Assessment Feasible. J. Brief Ther. 2006;5(1):5–22. [Google Scholar]
- Mittendorfer-Rutz E., Härkänen T., Tiihonen J., Haukka J. Association of socio-demographic factors, sick-leave and health care patterns with the risk of being granted a disability pension among psychiatric outpatients with depression. PLoS One. 2014;9(6) doi: 10.1371/journal.pone.0099869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz D.S., Young S.N. Ecological momentary assessment: what it is and why it is a method of the future in clinical psychopharmacology. J. Psychiatry Neurosci. 2006;31(1):13–20. [PMC free article] [PubMed] [Google Scholar]
- Noble S.L. Control-theoretic scheduling of psychotherapy and pharmacotherapy for the treatment of post traumatic stress disorder. IET Control Theory Appl. 2014;8(13):1196. [Google Scholar]
- Olson D., Delen D. Springer-Verlag; 2008. Advanced Data Mining Techniques. [Google Scholar]
- Osmani V., Maxhuni A., Grünerbl A., Lukowicz P., Haring C., Mayora O. Proceedings of International Conference on Advances in Mobile Computing and Multimedia - MoMM '13. 2013. Monitoring activity of patients with bipolar disorder using smart phones; pp. 85–92. [Google Scholar]
- Otto M.W., Tuby K.S., Gould R.a., McLean R.Y.S., Pollack M.H. An effect-size analysis of the relative efficacy and tolerability of serotonin selective reuptake inhibitors for panic disorder. Am. J. Psychiatr. 2001;158(12):1989–1992. doi: 10.1176/appi.ajp.158.12.1989. [DOI] [PubMed] [Google Scholar]
- Panagiotakopoulos T.C., Lyras D.P., Livaditis M., Sgarbas K.N., Anastassopoulos G.C., Lymberopoulos D.K. A contextual data mining approach toward assisting the treatment of anxiety disorders. IEEE Trans. Inf. Technol. Biomed. 2010;14(3):567–581. doi: 10.1109/TITB.2009.2038905. [DOI] [PubMed] [Google Scholar]
- Patten S.B. Markov models of major depression for linking psychiatric epidemiology to clinical practice. Clin. Pract. Epidemiol. Ment. Health. 2005;1(1):2. doi: 10.1186/1745-0179-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl J. Technical Report. 2009. Myth, confusion, and science in causal analysis. [Google Scholar]
- Pedersen M.U., Hesse M. A simple risk scoring system for prediction of relapse after inpatient alcohol treatment. Am. J. Addict. 2009;18(6):488–493. doi: 10.3109/10550490903205983. [DOI] [PubMed] [Google Scholar]
- Perlis R.H. A clinical risk stratification tool for predicting treatment resistance in major depressive disorder. Biol. Psychiatry. 2013;74(1):7–14. doi: 10.1016/j.biopsych.2012.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pestian J., Nasrallah H. Suicide note classification using natural language processing: a content analysis. Biomed. Inform. Insights. 2010;3:19–28. doi: 10.4137/BII.S4706. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3107011/ Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priebe S., Richardson M., Cooney M., Adedeji O., McCabe R. Does the therapeutic relationship predict outcomes of psychiatric treatment in patients with psychosis? A systematic review. Psychother. Psychosom. 2011;80(2):70–77. doi: 10.1159/000320976. [DOI] [PubMed] [Google Scholar]
- Proudfoot J., Clarke J., Birch M.-R., Whitton A.E., Parker G., Manicavasagar V.…Hadzi-Pavlovic D. Impact of a mobile phone and web program on symptom and functional outcomes for people with mild-to-moderate depression, anxiety and stress: a randomised controlled trial. BMC Psychiatry. 2013;13(1):312. doi: 10.1186/1471-244X-13-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Titov N., Andrews G., McIntyre K., Schwencke G., Solley K. Internet treatment for generalized anxiety disorder: a randomized controlled trial comparing clinician vs. technician assistance. PLoS One. 2010;5(6) doi: 10.1371/journal.pone.0010942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runyan J.D., Steenbergh T.a., Bainbridge C., Daugherty D.a., Oke L., Fry B.N. A smartphone ecological momentary assessment/intervention “app” for collecting real-time data and promoting self-awareness. PLoS One. 2013;8(8) doi: 10.1371/journal.pone.0071325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeb S., Zhang M., Karr C.J., Schueller S.M., Corden M.E., Kording K.P., Mohr D.C. Mobile phone sensor correlates of depressive symptom severity in daily-life behavior: an exploratory study. J. Med. Internet Res. 2015;17(7) doi: 10.2196/jmir.4273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safavian S.R., Landgrebe D. A survey of decision tree classifier methodology. IEEE Trans. Syst. Man Cybern. 1991;21(3):660–674. [Google Scholar]
- Shiffman S., Stone A.A., Hufford M.R. Ecological momentary assessment. Annu. Rev. Clin. Psychol. 2008;4(5):1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Shmueli G. To explain or to predict? Stat. Sci. 2010;25(3):289–310. [Google Scholar]
- Sjölander A. Propensity scores and M-structures. Stat. Med. 2009;28(9):1416–1420. doi: 10.1002/sim.3532. [DOI] [PubMed] [Google Scholar]
- Smyth J.M., Stone A. Ecological momentary assessment research in behavioral medicine. J. Happiness Stud. 2003;4:35–52. [Google Scholar]
- Stange M., Funk B. Business Science Reference; Hershey: 2016. How Big Does Big Data Need to be? Enterprise Big Data Engineering, Analytics, and Management. (S. 1–12) [Google Scholar]
- Titov N., Dear B.F., Staples L.G., Bennett-Levy J., Klein B., Rapee R.M., Shann C., Richards D., Andersson G., Ritterband L., Purtell C., Bezuidenhout G., Johnston L., Nielssen O.B. MindSpot clinic: an accessible, efficient, and effective online treatment service for anxiety and depression. Psychiatr. Serv. 2015;66(10):1043–1050. doi: 10.1176/appi.ps.201400477. [DOI] [PubMed] [Google Scholar]
- Torous J., Staples P., Onnela J.-P. Realizing the potential of mobile mental health: new methods for new data in psychiatry. Curr. Psychiatry Rep. 2015;17(8):61. doi: 10.1007/s11920-015-0602-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Touboul J., Romagnoni A., Schwartz R. On the dynamic interplay between positive and negative affects, 1–31. 2010. http://arxiv.org/abs/1004.4856 Retrieved from.
- Tovar A., Boulos R., Sliwa S., Must A., Gute D.M., Metayer N., Economos C. Baseline socio-demographic characteristics and self-reported diet and physical activity shifts among recent immigrants participating in the randomized controlled lifestyle intervention:“live well”. J. Immigr. Minor. Health. 2014;16(3):457–465. doi: 10.1007/s10903-013-9778-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull T.J., Ebner-Priemer U. Ambulatory assessments. Annu. Rev. Clin. Psychol. 2013;9:151–176. doi: 10.1146/annurev-clinpsy-050212-185510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Breda W., Hoogendoorn M., Eiben A.E., Andersson G., Riper H., Ruwaard J., Vernmark K. Computational Intelligence (SSCI), 2016 IEEE Symposium Series on. IEEE; 2016. A feature representation learning method for temporal datasets; pp. 1–8. (December) [Google Scholar]
- Van der Hoek W., Wooldridge M. Multi-agent systems. Found. Artif. Intell. 2008;3:887–928. [Google Scholar]
- Van der Sluis F., Dijkstra T., Van den Broek E.L. Proceedings of the International Conference on Health Informatics, HealthInf 2012, 01–04 Feb 2012, Vilamoura, Algarve, Portugal. SciTePress - Science and Technology Publications; 2012. Computer aided diagnosis for mental health care: on the clinical validation of sensitive machines; pp. 493–498. [Google Scholar]
- Van der Werf S.Y., Kaptein K.I., De J.P., Spijker J., De G.R., Korf J. Major depressive episodes and random mood. Arch. Gen. Psychiatry. 2006;63(5):509–518. doi: 10.1001/archpsyc.63.5.509. (May) [DOI] [PubMed] [Google Scholar]
- Van Gemert-Pijnen J.E.W.C., Kelders S.M., Bohlmeijer E.T. Understanding the usage of content in a mental health intervention for depression: an analysis of log data. J. Med. Internet Res. 2014;16(1) doi: 10.2196/jmir.2991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Voorhees B., Paunesku D., Gollan J., Kuwabara S., Reinecke M., Basu A. Predicting future risk of depressive episode in adolescents: the Chicago Adolescent Depression Risk Assessment (CADRA) Ann. Fam. Med. 2008:503–511. doi: 10.1370/afm.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van H.L., Schoevers R. a, Kool S., Hendriksen M., Peen J., Dekker J. Does early response predict outcome in psychotherapy and combined therapy for major depression? J. Affect. Disord. 2008;105(1–3):261–265. doi: 10.1016/j.jad.2007.04.016. [DOI] [PubMed] [Google Scholar]
- Vittengl J.R., Clark L.A., Dunn T.W., Jarrett R.B. Reducing relapse and recurrence in unipolar depression: a comparative meta-analysis of cognitive–behavioral therapy's effects. J. Consult. Clin. Psychol. 2009;75(3):475–488. doi: 10.1037/0022-006X.75.3.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade W., Treat T., Stuart G.L. Transporting an empirically supported treatment for panic disorder to a service clinic setting: a benchmarking strategy. J. Consult. Clin. Psychol. 1998;66(2):231–239. doi: 10.1037//0022-006x.66.2.231. [DOI] [PubMed] [Google Scholar]
- Whitton A.E., Proudfoot J., Clarke J., Birch M.R., Parker G., Manicavasagar V., Hadzi-Pavlovic D. Breaking open the black box: isolating the most potent features of a web and mobile phone-based intervention for depression, anxiety, and stress. JMIR Ment. Health. 2015;2(1) doi: 10.2196/mental.3573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichers M., Simons C.J.P., Kramer I.M.A., Hartmann J.A., Lothmann C., Myin-Germeys I., van Os J. Momentary assessment technology as a tool to help patients with depression help themselves. Acta Psychiatr. Scand. 2011;124(4):262–272. doi: 10.1111/j.1600-0447.2011.01749.x. [DOI] [PubMed] [Google Scholar]
- Witten I.H., Frank E. Second edition. Morgan Kaufmann Publishers Inc.; San Francisco, CA, USA: 2005. Data mining: practical machine learning tools and techniques. (Morgan Kaufmann Series in Data Management Systems). [Google Scholar]
- Zeigler B.P., Praehofer H., Kim T.G. Academic Press; San Diego: 2000. Theory of Modeling and Simulation: Integrating Discrete Event and Continuous Complex Dynamic Systems. [Google Scholar]