Abstract
Background
Procrastination affects a large number of individuals and is associated with significant mental health problems. Despite the deleterious consequences individuals afflicted with procrastination have to bear, there is a surprising paucity of well-researched treatments for procrastination. To fill this gap, this study evaluated the efficacy of an easy-to-use smartphone-based treatment for procrastination.
Method
N = 31 individuals with heightened procrastination scores were randomly assigned to a blended smartphone-based intervention including two brief group counseling sessions and 14 days of training with the mindtastic procrastination app (MT-PRO), or to a waitlist condition. MT-PRO fosters the approach of functional and the avoidance of dysfunctional behavior by systematically utilizing techniques derived from cognitive bias modification approaches, gamification principles, and operant conditioning. Primary outcome was the course of procrastination symptom severity as assessed with the General Procrastination Questionnaire.
Results
Participating in the smartphone-based treatment was associated with a significantly greater reduction of procrastination than was participating in the control condition (η2 = .15).
Conclusion
A smartphone-based intervention may be an effective treatment for procrastination. Future research should use larger samples and directly compare the efficacy of smartphone-based interventions and traditional interventions for procrastination.
Keywords: Procrastination, Intervention, Treatment, Smartphone, Mobile health
Highlights
-
•
We evaluated a smartphone-based treatment targeting procrastination (MT-PRO) in an adult sample (n = 31).
-
•
MT-PRO fosters utilizes techniques derived from cognitive bias modification approaches, gamification principles, and operant conditioning.
-
•
MT-PRO led to a significantly greater reduction of procrastination than was participating in the control condition (η2 = .15).
-
•
Effects were stable over 4-weeks follow-up.
1. Introduction
Deferring commitments is a ubiquitous phenomenon that is not necessarily associated with significant psychological distress. For some people, however, initially harmless dallying can turn into a persistent behavioral pattern of voluntarily postponing important tasks, referred to as procrastination (Rozental and Carlbring, 2013). Instead of working to meet important deadlines, procrastinators engage in activities that take their minds of the task at hand and, hence, lead to a short term-relief of the undesired feelings associated with approaching this task (Dryden, 2000, Pychyl et al., 2012). According to Badri Gargari et al. (2011), procrastination comprises cognitive, affective, or behavioral components. Depending on the individual’s specific characteristics these components can lead to a variety of manifestations such as academic, decisional, neurotic, or compulsive procrastination.
Prevalence rates for procrastination ranging between 15%–20% in the general adult population prove as evidence for the frequency of this phenomenon (Day et al., 2000, Ferrari et al., 2005). Amongst the afflicted, university students represent the population most frequently affected by procrastination. Here, estimates indicate that approximately 40% of university students engage in significant procrastinatory behavior (Ferrari et al., 2005, Harriott and Ferrari, 1996, Mahasneh et al., 2016, Özer et al., 2009) and almost 50% procrastinate consistently and problematically (Haycock et al., 1998, Onwuegbuzie, 2000, Solomon and Rothblum, 1984). In academic procrastination, affected students experience the pervasive and permanent desire to delay their academic obligations, causing them to spend over 30% of their daily activities in the engagement of procrastinatory behavior such as sleeping during daytime, playing, or TV watching (Pychyl et al., 2012).
Procrastination is a failure of self-regulation that is associated with various mental health problems. Studies found links between procrastination and low self-esteem (e.g., Stead et al., 2010, Steel, 2007) and poor individual well-being as measured by high levels of stress and physical illness (e.g., Tice and Baumeister, 1997). Moreover, people who procrastinate show a heightened risk for the development, maintenance, and exacerbation of mental disorders such as depression and anxiety disorders (e.g., Rozental and Carlbring, 2013). Furthermore, studies examining university students show that academic procrastination is systematically linked to poor task-performance, depression, social anxiety, and self-handicapping behavior (Ferrari et al., 1992, Tice and Baumeister, 1997), thus having a negative impact on the psychological well-being of the afflicted and their academic success. Finally, several authors point out the link between procrastination and deficits in the successful application of emotion regulation (ER) skills (Höcker et al., 2013, Rebetez et al., 2015).
Treatments for procrastination and related problems often utilize well-researched strategies stemming from cognitive behavior therapy (CBT) such as goal-setting, time-management, modeling, success spiral, and learned industriousness (Steel, 2007, Uzun Ozer et al., 2013). Although informative and useful, these strategies are not well-researched in the context of procrastination as most of the few available studies lack crucial components such as validated outcome measures, randomization, long-term follow-ups, and mostly consist of single-case designs (Dryden, 2012, Karas and Spada, 2009, Neenan, 2008, Pychyl and Flett, 2012). Taken together, it is surprising that despite the alarmingly high prevalence rates and the negative impact of procrastinatory behavior on various health domains, clinical trials examining the efficacy of treatments for procrastination are scarce and available studies often lack fundamental quality criteria (Rozental and Carlbring, 2014). Thus, unlike it is the case for most mental health issues, there is no “gold standard” treatment for procrastination (Glick and Orsillo, 2015).
In recent years, computer-based therapy approaches have made their way into therapeutic research and practice. Computer-based therapy has been shown to be highly effective by delivering treatment in high-dosages while simultaneously providing efficacious, cost-effective, scalable, and patient friendly interventions that can easily be disseminated (Barak et al., 2009). Even more promising are results from a meta-analysis by Andersson et al. (2014), suggesting that computer-based CBT and face-to-face treatment produce equivalent overall effects. Computer-based interventions targeting procrastination, however, are scarce. Our review of the literature yielded just one study on the effects of computer-based CBT on procrastination. Here, in a randomized controlled trial, Rozental et al. (2015) evaluated the effects of a computer-based self-help intervention targeting procrastination, and found that participants in both intervention groups (guided and unguided) experienced greater reduction in procrastination than did the wait-list control group with between-group effect sizes ranging from d = 0.70 to d = 0.81. Despite their proven effectiveness in various domains, computer-based therapy, however, has several limitations including the lack of assimilation into the user's daily life (e.g., Martell et al., 2010), limited accessibility, and its dependence from both time and location (e.g., Mattila et al., 2008).
Mental health apps and computer-based therapy share most of the advantages of modern technology mentioned above. However, treatment programs run on smartphone apps hold additional benefits as smartphones (a) are ubiquitous and almost constantly available (e.g., Ben-Zeev et al., 2015), (b) cause almost no maintenance costs (e.g., Ly et al., 2012), (c) are already owned by a large number of people and therefore easy to disseminate (e.g., Juarascio et al., 2015), (d) are able to interact with the user allowing data input using multiple input channels (e.g., Porta, 2007), and (e) are generally designed to be easy to use (e.g., Mattila et al., 2008). Moreover, several studies have shown that adherence and dropout rates in traditional therapy can be improved using smartphones when used as technological adjuncts to traditional therapy (e.g., Clough and Casey, 2011, McTavish et al., 2012). Because of these advantages, smartphone-based interventions are recently becoming increasingly popular for the treatment of mental health problems.
Research is needed to verify if the aforementioned advantages can be used for the treatment of psychological problems. Promising results for the evidence of mental health apps come from a systematic review of several studies producing evidence for smartphone-based mental health interventions (Donker et al., 2013), showing that apps can be effective in the reduction of symptoms of anxiety, depression, stress, and substance use. Corroborating these findings are studies showing that smartphone-based treatment programs can significantly reduce depressive symptoms as well as stress, anxiety, and overall psychological distress (Ahmedani et al., 2015, Harrison et al., 2011), decrease state and trait anxiety while simultaneously increasing self-efficacy and functional impairment (Grassi et al., 2007), and improve symptoms in patients with substance-use disorders (Garrison et al., 2015). However, research on smartphone-based interventions targeting mental health problems is still scarce. Available studies focus predominantly on the development and feasibility of mental health apps (Bush et al., 2015, Jiménez-Serrano et al., 2015, Prada et al., 2016). Moreover, our review of the literature yielded no studies examining smartphone-based interventions for procrastination.
To fill this gap, the aim of the present pilot study was to develop and evaluate a smartphone-based intervention protocol that reduces procrastination utilizing (a) an approach-avoidance training based on cognitive bias modification (CBM), (b) computer gaming principles, and (c) operant conditioning. CBM approaches are not only effective in measuring implicit bias (e.g., racial bias; Kawakami et al., 2007) but can also be used to improve treatment outcomes when used as systematic trainings using disorder-specific stimulus material (e.g., the Approach Avoidance Task, a computer-based program that asks participants to push or pull stimuli towards/away from themselves using a joystick which in turn led to a reduction in relapse rates in alcoholics; Wiers et al., 2011). Moreover, CBM approaches were shown to have an effect on brain regions (e.g. medial prefrontal cortex) associated with maladaptive approach biases (e.g., Wiers et al., 2015). The use of electronic gaming in psychotherapy has a strong research base (e.g., Horne-Moyer et al., 2014, Kauer et al., 2012, Merry et al., 2012) and smartphones are recently gaining popularity as gaming devices (Feijoo et al., 2012). Hence, it is surprising that current smartphone-based interventions only seldom utilize gamification principles to systematically enhance treatment outcomes (e.g., Franklin et al., 2016, Miloff et al., 2015). In most cases, smartphone apps for mental health problems focus on areas such as providing instructions, offering strategies for self-help, reminders and other components like a mobile diary or simple mood ratings but without making use of more innovative options and features offered by modern smartphone technology. Finally, Siang and Rao (2003) argued that learning principles such as operant conditioning are crucial in games by molding unconditioned user responses and eventually improving games by maintaining high user motivation.
Our app MT-PRO aims to reduce procrastination by systematically targeting users’ motivations to approach/avoid stimuli relevant for procrastinatory behavior. The app asks users to either actively avoid dysfunctional stimulus material (e.g., pictures showing typical alternative activities such as a student sitting in a study environment engaging in social media activities; negative study-related statements) or to actively approach functional material (e.g., a student sitting in a study environment engaging in academic tasks; positive study-related statements). Thereby, MT-PRO aims at training attitude-contrary behavior and thus promoting a change of relevant attitudes in a particular domain. In MT-PRO, users are asked to decidedly wipe away pictures showing engagement in typical alternative activities and negative statements related to procrastination which appear on their smartphone screen and to determinedly wipe pictures of study environments and positive statements related to procrastination towards them, thereby fostering avoidance and approach. The stimuli are first small and then become larger until they fill almost the entire screen. MT-PRO includes gaming principles by making users gain stars for every five correct answers given. Finally, MT-PRO aims at systematically reinforcing possible training effects by providing immediate feedback using mechanisms from operant conditioning. When processing a stimulus correctly, a smiling emoticon and the word “Correct!” appear on the screen, whereas a frowning emoticon, the words “That’s wrong!”, and a short vibration of the smartphone occurs upon every wrong answer.
In this study, we evaluated a blended smartphone-based intervention for procrastination conducting a randomized controlled trial using a waitlist group. We hypothesized MT-PRO to reduce procrastination in an academic context and expected effects to be stable at one month follow-up. We also used mediation analyses to test presumed mechanisms of change.
2. Method
2.1. Design, participants and procedures
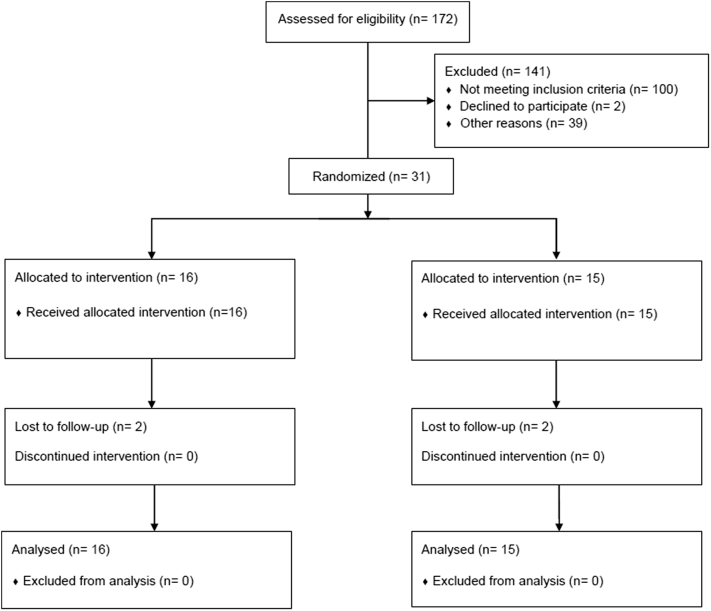
We evaluated the efficacy of a blended smartphone-based treatment program consisting of MT-PRO and two group counseling sessions in a two-arm, prospective, randomized controlled trial. Participants were recruited through the university's website, flyers on various campus pin boards, and announcements in several social media channels. To assess inclusion criteria, interested individuals were asked to complete an online screening questionnaire. Eligible participants had to meet the following criteria: (a) informed consent, (b) heightened procrastination score with values > 60th percentile on the APROF, (c) sufficient German language skills, (d) age 18 or above, and (e) access to a smartphone using Android (version 4.0 or above). The cut-off for the APROF was chosen as prevalence studies indicate that on average about 40 % of students significantly procrastinate (Ferrari et al., 2005, Harriott and Ferrari, 1996, Mahasneh et al., 2016, Özer et al., 2009) and recruitment for this study focused on students predominately. To maximize external validity there were no other exclusion criteria. Of the 172 potential participants we assessed for eligibility, 100 of these individuals did not meet the inclusion criteria (with 9 individuals being younger than 18 years, 40 failing to complete the screening assessment, and 51scoring below the 60th percentile on the APROF). Participants meeting all inclusion and none of the exclusion criteria were contacted by e-mail and received additional written information about study procedures.
In this pilot study, we included a total of 31 participants that were then randomized to either the intervention or wait list group. Block randomization of size two was used to ensure similar sample sizes across conditions. Randomization was conducted by a master's degree student (not otherwise involved in the study) via randomization.org. The student generated the assignment sequence and enrolled participants. The treatment group (n = 16) was compared to a waitlist group (n = 15). All participants in the intervention group completed the counseling sessions. On average, participants in this group used the app at 11.69 days (SD = 2.73, range 5–14) over a time period of 50.49 min total (SD = 28.09 min, range = 14.53–114.18). During this time period they played an average of 20.62 games (SD = 14.99, range = 5–57). Between post and follow-up assessment a total of 4 participants dropped out, with two dropouts each in the intervention and the wait list group. Participants were predominately female (83.9%) with an average age of 22.03 years (SD = 3.63) and the age ranging from 18 to 30 years. Fig. 1 illustrates the participant flow through the study.
Fig. 1.
CONSORT flow diagram.
Data were assessed at pre-treatment, post-treatment and 1-month follow-up. The 6-week study took place in the middle of the academic term. For statistical analyses we used completer analysis. The treatment was free of charge and every participant automatically took part in a draw for a shopping gift card. Additionally, student participants received course credits. Participants, students administering the two group counseling sessions, and students assessing the outcomes were aware of the condition assignments at all times. All study procedures complied with the human research guidelines of the Helsinki Protocol and were approved by the ethics committee of the German Psychological Society. For socio-demographics of study participants see Table 1.
Table 1.
Sample characteristics.
| Treatment group (n = 16) | Control group (n = 15) | Test statistic | p | |
|---|---|---|---|---|
| Age (years) M (SD) |
21.63 (3.56) | 22.47 (3.78) | t(29) = 0.64 | .528 |
| Gender n (%) female |
12 (75) | 14 (93.3) | Fisher’s exact test | .333 |
| Education n (%) |
||||
| High school | 13 (81.25) | 14 (93.33) | Fisher's exact test | .600 |
| University degree | 3 (18.75) | 1 (6.67) | ||
| Occupation n (%) |
||||
| Student | 14 (87.50) | 15 (100) | Fisher's exact test | .484 |
| Other | 2 (12.50) | 0 (0) | ||
| Standard period of study n (%) | ||||
| Surpassed | 1 (18.75) | 4 (26.67) | Fisher's exact test | .330 |
| Not surpassed | 13 (81.25) | 11 (73.33) |
2.1.1. Intervention group
Participants in the intervention group were invited to use MT-PRO daily on their own smartphones for 14 days. As part of the intervention, two group-based face-to-face sessions were scheduled. The first session was scheduled one day before the start of the two-week training. The second session was scheduled one day after the 2-week training period had been completed. Before the start of treatment, participants completed pre-treatment assessment and were then invited to participate in a brief group counseling in which they were provided with information on the development and maintenance of procrastination and opportunities for change. The brief counseling included two steps. First, participants received a psychoeducation in which they learned about the Rubicon model (Heckhausen and Gollwitzer, 1987). Here, participants were asked to present idiosyncratic situations in which they procrastinate and ultimately, engage in alternative activities. Secondly, therapists repeatedly used the metaphor “per aspera ad astra”, (“through hardships to the stars”) to point out the importance of continuing effort to overcome procrastination. Group sessions were delivered by three intensively trained master's degree students in laboratory rooms of the Friedrich-Alexander-University Erlangen-Nuremberg. Two graduate psychologists provided training and supervision at regular intervals to ensure adherence to the treatment protocol.
At the end of the group session MT-PRO was installed on participants' smartphones and participants were introduced to the app and instructed in its handling. Participants were then told that the app would include 80 procrastination-related stimuli. As an attempt to individualize the app material, they were asked to create 40 stimuli (statements) themselves and to choose another 40 stimuli (both statements and pictures) from a pool provided by the therapists. For the first 40 stimuli, therapists encouraged participants to word each 20 positive (e.g. “I will not be distracted from important tasks”) and 20 negative statements (e.g. “Instead of studying I rather plan my night out”) related to procrastination. Regarding the remaining 40 stimuli, and in case participants were not able to come up with all of the first 40 stimuli themselves, therapists provided a pool consisting of 78 negative and positive procrastination-related statements and pictures showing academic activities and alternative situations participants would likely perceive as more pleasant (e.g., engaging in social activities, media, sports, household). This pool was specifically created for this study by a psychologist supervised by a professor in clinical psychology. Following the notion that regulatory failures play an important role in procrastination, several of the stimuli we provided systematically addressed particular ER skills in the domains of acceptance, tolerance, and readiness to confront distressing situations believed to be important in procrastination. In the second session participants first completed post-treatment questionnaire assessment and were then interviewed and asked to give feedback concerning the app (changes they realized during the last 14 days, positive and negative features of the app, and possible problems encountered while using the app). Follow-up questionnaire assessment was conducted using an online tool.
2.1.2. Waitlist group
Participants in the waitlist group waited and were offered to participate in the intervention (two brief consultation sessions and MT-PRO) after the follow-up assessment. To obtain self-report questionnaire assessment at pre-treatment, post-treatment and follow-up, participants in the waitlist group completed online self-report assessments.
2.2. Measures
2.2.1. Primary outcome
Primary outcome was the rate of change in procrastination symptomatology as assessed by the General Procrastination Questionnaire (Allgemeiner Prokrastinationsfragebogen; APROF; Höcker et al., 2013). The APROF is an 18-item-scale that assesses general procrastination, task adversity, and preferences for alternative activities on a seven-point Likert-type scale. In the present study, the APROF showed good internal consistencies with (α = .89).
2.2.2. Secondary outcome measures
Academic procrastination was assessed using the Academic Procrastination State Inventory (APSI; Schouwenburg, 1995). The APSI is a 33-item scale assessing fluctuations in academic procrastination, behavior and thoughts that asks respondents to rate the frequency of their engaging in the items during the last seven days on a five-point Likert-type scale. The self-report instrument contains three subscales (academic procrastination, fear of failure, and lack of motivation) with coefficient alphas ranging from .82–.89 (Höcker et al., 2013). Cronbach alphas in the present research ranged from .76 to .88.
To explore to what extent MT-PRO would have a positive impact on participants’ motivation to change, we assessed the latter with a seven-item scale relating the transtheoretical model of change (DiClemente et al., 1991) to procrastination. Exemplary items are “Do you want to improve your procrastinatory behavior?” and “Do you intent to actively change your procrastinatory behavior?” All items were rated on a on a five-point Likert-type scale (0 = not at all to 4 = almost always). The mean score of these items was used for further analyses. The internal consistency of this indicators of motivation to change measure was good (α = .79).
Finally, we utilized self-reports of adaptive responses to challenging feelings experienced during procrastination to explore whether increases in specific ER skills would possibly mediate changes in procrastination. To this end, we used a modified version of the Emotion Regulation Skills Questionnaire (ERSQ; Berking and Znoj, 2008). The ERSQ is a 27-item self-report instrument that utilizes a five-point Likert-type scale (0 = not at all to 4 = almost always) to assess respondents' adaptive ER skills in the previous week. Good reliability and validity of the ERSQ have been demonstrated in previous studies (Berking et al., 2011, Berking et al., 2013). The procrastination version of the ERSQ (ERSQ-P; unpublished, a copy can be obtained from the first author) showed good internal consistency in the present study (α = .89).
2.3. Statistical analyses
We conducted two-way ANOVAs to test whether there was a statistically significant interaction between group membership and time. As effect sizes we report η2. According to commonly used conventions (Cohen, 1988) we defined η2 = 0.01/0.06/0.14 as small/moderate/large effects. Within-group differences from pre- to post-treatment and from post-treatment to follow-up were analyzed through pairwise t-tests. As effect sizes we report d (0.20 = small effect, 0.50 = medium, 0.80 = large). Group differences in sociodemographic variables were analyzed by computing several Fisher exact tests. To determine whether randomization was successful, the researchers examined group differences in primary and secondary outcomes at pre-treatment by computing several one-way ANOVAs. For these analyses, alpha was set at .05.
To explore whether changes on three subscales of the ERSQ (acceptance, readiness to confront distressing situations, and tolerance) would mediate the effects of the intervention on self-reported general procrastination, we used the path model depicted in Fig. 2.
Fig. 2.
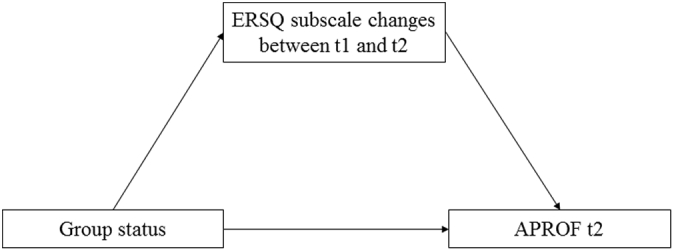
Path model.
As suggested by Hayes (2013), we tested indirect (i.e., mediation) effects with the help of bias-corrected bootstrapped 95% confidence intervals (number of bootstrap draws = 1000).
3. Results
Preliminary analyses confirmed that all statistical assumptions (independence, normality, and homoscedasticity) for using the ANOVA were met. Regarding both general and academic procrastination as measured by the APROF and the APSI, respectively, there was no group difference at baseline. ANOVA results for the APROF were (F(1,29) = 0.16; η2 = .01, 95%-CI = .00–.15) and results for the APSI were (F(1,29) = 1.03; η2 = .03, 95%-CI = .00–.22). Analyses on all further secondary outcome measures indicated that there were no significant group differences at baseline, as well. Descriptive data for both procrastination outcomes at pre-treatment, post-treatment, and follow-up in the intervention group and waitlist group are displayed in Table 2.
Table 2.
ANOVAS and repeated-measures-ANOVAs.
| n | t1 | t2 | t3 | Between group ANOVA |
Repeated-measures ANOVA |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| t1 |
t2 (after 2 weeks) |
t3 (after 6 weeks) |
Measurement-point |
Group-membership*measurement-point |
Group-membership |
|||||||||||
| F (1,29) | η2 (95%-CI) | F (df) | η2 (95%-CI) | F (df) | η2 (95%-CI) | F (df) | η2 (95%-CI) | F (df) | η2 (95%-CI) | F (df) | η2 (95%-CI) | |||||
| APROF | 0.16 | .01 (.00–.15) | 2.98 (1,25) | .11 (.00–.34) | 5.14 (1,25) | .17 (.00–.41) | 8.15 (1.45, 34.80) | .25 (.04–.45) | 4.11 (1.50, 34,80) | .01 (.00–.08) | 1.75 (1,24) | .05 (.00–.30) | ||||
| INT | 12 | 5.44 (0.65) | 4.92 (0.75) | 4.46 (0.89) | ||||||||||||
| CTR | 14 | 5.28 (0.49) | 5.33 (0.57) | 5.10 (0.76) | ||||||||||||
| APSI | 1.03 | .03 (.00–.22) | 3.81 (1,25) | .13 (.00–.37) | 3.09 (1,25) | .1 (.00–.34) | 6.83 (1.53, 36.79) | .22 (.02–.41) | 6.28 (1.50, 40.40) | .19 (.03–.34) | 1.95 (1,24) | .08 (.00–.30) | ||||
| INT | 12 | 3.29 (0.42) | 2.80 (0.54) | 2.72 (0.47) | ||||||||||||
| CTR | 14 | 3.18 (0.59) | 3.25 (0.53) | 3.12 (0.57) | ||||||||||||
3.1. Primary outcome
To test the effect of treatment we used repeated-measures-ANOVA with group-membership as between-subjects-factor. We used Greenhouse-Geisser corrections because sphericity was not given. These analyses resulted in a significant effect for the interaction of time and group on the sum score of the APROF (F(1.5,34.8) = 4.11; η2 = .15, 95%-CI = .00–.35). T-tests showed that participants in the intervention group reported a significantly greater reduction of procrastination from pre- to post-treatment (t(13) = 3.95; d = 0.75, 95%-CI = 0.41–1.15; than participants in the control group (t(12) = − 0.53; d = − 0.14, 95%-CI = − 0.40–0.16). These statistics are displayed in Table 3.
Table 3.
t-Tests.
| Change t1–t2 |
Change t2–t3 |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| n | t | df | d (95%-CI) | n | t | df | d (95%-CI) | ||
| APROF | Intervention | 14 | 3.95⁎⁎ | 13 | 0.75 (0.41–1.15) | 14 | 1.52⁎ | 13 | 0.59 (0.20–1.06) |
| Control | 13 | − 0.53 | 12 | − 0.14 (− 0.40–0.16) | 12 | 1.86 | 11 | 0.36 (0.04–0.79) | |
p < .05.
p < .01.
3.2. Secondary outcomes
For academic procrastination, the two-way repeated-measures ANOVA indicated that there was a significant interaction of time and group for the APSI (F(1.5,40.4) = 6.28; η2 = .19, 95%-CI = .02–.37). We found a significant effect of group in favor of the intervention group at post-treatment for the APSI (F(1,25) = 3.81; η2 = .13, 95%-CI = .00–.37), as well.
When testing motivation to change, we used the Wilcoxon-test because the assumption of normality was violated. The test showed no differences either for the intervention group (U = 0.40, p = .69) or the control-group (U = − 1.09, p = .28).
3.3. Follow-up analyses
Follow-up analyses on general procrastination symptoms indicated that the superiority of the intervention over the control group was sustained at the end of the 4-week follow-up assessment. We conducted a repeated-measures-ANOVA over post- and follow-up-assessment showing a significant group-effect (F(1,24) = 4.65; η2 = .16, 95%-CI = .00–.40) and no significant time and time*group effects (all ps > .05). Furthermore, the intervention group showed no significant changes of treatment gains over the follow-up period (t(13) = 1.52; d = 0.59, 95%-CI = 0.20–1.06) and no significant changes were observed in the control condition (t(11) = 1.86; d = 0.36, 95%-CI = 0.04–0.79).
3.4. Mediation analysis
Mediation analysis showed a significant association of group status and changes in acceptance (b = .610; SE = .223; p < .05), readiness to confront distressing situations (b = .628; SE = .200; p < .01), but not tolerance (b = .518; SE = .305; p = .10). The mediation analyses resulted in non-significant indirect effects for all potential mediators (acceptance: b = −.215; SE = .310; 95%-CI = − 1.06–.24; readiness to confront distressing situations: b = −.090, SE = .172; 95%-CI = −.54–.16; tolerance: b = .051; SE = .183; 95%-CI = −.26–.50). Thus, there was some evidence for the effect of the intervention on ER, but no evidence for the assumed mediational relationship between ER skills and general procrastination.
4. Discussion
In this study we aimed at evaluating a smartphone-based intervention for procrastination in a sample of afflicted adults. Results indicate that taking part in the intervention group significantly reduced both general and academic procrastination symptoms compared to the control group at post-treatment. Follow-up analyses showed that results were sustained over a 1-month period. Results also showed that MT-PRO not only positively affected general procrastination, it also improved academic procrastination with effects being stable at the 4-week follow-up assessment, as well. Moreover, playing MT-PRO resulted in significant improvements in adaptive ER. The observed between-group effect sizes of the intervention on both indicators of procrastination are comparable to those reported in other studies that evaluated interventions targeting procrastination (average about d = .80; see Höcker et al., 2013). On the APROF this corresponds with a change in the intervention group of 0.98 points from pre- to follow-up-assessment on a scale that assesses the occurrence of procrastinatory behavior ranging from 1 (= never) to 7 (= always). Possibly the (non-significant) increase of procrastination in the control group results from an increase in academic tasks over the course of the study (as the study progressed in time, student participants moved closer to final exams and/or faced other academic obligations). If this hypothesis was correct, it would indicate that the intervention (over-)compensated these effects.
Should the findings of the current study be replicated in future research, they would have important implications for clinical research and practice. Firstly, by adding to the literature by providing further evidence for the efficacy of digitalized psychological interventions and, thus, the important role of mobile mental health interventions. Secondly, results from this pilot study suggest that principles of approach and avoidance training can be successfully utilized on smartphones, thus advancing the field of mobile mental health interventions. Thirdly, this study supports the idea that utilization and dissemination of mobile mental health games can be instrumental in improving psychotherapeutic treatments for a variety of psychological problems. Finally, it can be argued that MT-PRO helps reducing procrastination by being a putatively more rewarding activity but, at the same time, also a helpful alternative behavior itself, in which procrastinators can engage in when procrastinating. Given that the average smartphone user checks his/her device as often as 150 times a day, smartphone apps like MT-PRO are capable of generating, rewarding, and maintaining strong positive habits such as the regular use of appealing apps offering help for a variety of psychological and mental health problems. In summary, this pilot study provides preliminary evidence that a blended low dosage intervention consisting of group counseling and the MT-PRO app can effectively reduce procrastination, supporting the notion that psychological interventions utilized on smartphone apps may very well pose as valuable supplements to traditional psychotherapy.
Although the investigated intervention seems to hold merit, further research needs to address the limitations of the present study. Major limitations of this study include: (a) the use of a small sample size, (b) absence of a sham control condition, (c) the absence of a MT-PRO only group that does not include face-to-face psychoeducation, and (d) the absence of experimental manipulation of potential mechanisms of change. Given the small sample size, results of this study should be interpreted with caution as the small and homogenous sample may have led to an overestimation of effect sizes (Howard et al., 2009, Ioannidis, 2008). Future studies should use larger and more heterogeneous samples. The use of a blended intervention consisting of two brief group counselling sessions (CBT-based) and the subsequent 14-days MT-PRO training (using an approach-avoidance rationale mixed with techniques of operant conditioning) in this study makes it particularly challenging to assign the effects of treatment to a particular change mechanism. Although we used regression analysis to test for possible mediators in this study, future studies should use a more elaborated research design helping to disentangle these techniques in order to pinpoint to what degree each of the mechanisms induces change. Thus, an experimental manipulation (e.g., comparing a group exclusively receiving the CBM paradigm to a group receiving the combination of CBM and operant conditioning) could help clarify to what extent systematic CBM (or other factors such as operant conditioning) are responsible for the effects of the intervention. Future studies should also work clarify whether findings from the present study generalize to time periods further away or closer to important exams.
Conflict of interest statement
There are no conflicts of interest to the best of my knowledge.
I confirm that the manuscript has been read and approved by me and my co-authors and that there are no other persons who satisfied the criteria for authorship but are not listed.
I confirm that I have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing I confirm that I have followed the regulations of institutions concerning intellectual property.
I understand that the Corresponding Author is the sole contact for the Editorial process (including Editorial Manager and direct communications with the office). He is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs. I confirm that I have provided a current, correct email address which is accessible by the Corresponding Author and which has been configured to accept email from:
Acknowledgments
We acknowledge support by Deutsche Forschungsgemeinschaft and Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU) within the funding pogramme Open Access Publishing.
References
- Ahmedani B.K., Crotty N., Abdulhak M.M., Ondersma S.J. Pilot feasibility study of a brief, tailored mobile health intervention for depression among patients with chronic pain. Behav. Med. 2015;41(1):25–32. doi: 10.1080/08964289.2013.867827. [DOI] [PubMed] [Google Scholar]
- Andersson G., Cuijpers P., Carlbring P., Riper H., Hedman E. Guided internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiatry. 2014;13(3):288–295. doi: 10.1002/wps.20151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badri Gargari R., Sabouri H., Norzad F. Academic procrastination: the relationship between causal attribution styles and behavioral postponement. Iran. J. Psychiatr. Behav. Sci. 2011;5(2):76–82. [PMC free article] [PubMed] [Google Scholar]
- Barak A., Klein B., Proudfoot J.G. Defining internet-supported therapeutic interventions. Ann. Behav. Med. 2009;38(1):4–17. doi: 10.1007/s12160-009-9130-7. [DOI] [PubMed] [Google Scholar]
- Ben-Zeev D., Schueller S.M., Begale M., Duffecy J., Kane J.M., Mohr D.C. Strategies for mHealth research: lessons from 3 mobile intervention studies. Admin. Pol. Ment. Health. 2015;42(2):157–167. doi: 10.1007/s10488-014-0556-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berking M., Znoj H. Entwicklung und Validierung eines Fragebogens zur standardisierten Selbsteinschätzung emotionaler Kompetenzen (SEK-27) [Development and validation of the Emotion-regulation Skills Questionnaire (ERSQ-27)] Z. Psychiatr. Psychol. Psychother. 2008;56:141–152. [Google Scholar]
- Berking M., Margraf M., Ebert D., Wuppermann P., Hofmann S., Junghanns K. Emotion regulation skills as a predictor of relapse during and after treatment of alcohol dependence. J. Consult. Clin. Psychol. 2011;79:307–318. doi: 10.1037/a0023421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berking M., Ebert D., Cuijpers P., Hofmann S.G. Emotion-regulation skills training enhances the efficacy of cognitive behavioral therapy for major depressive disorder. Psychother. Psychosom. 2013;82:234–245. doi: 10.1159/000348448. [DOI] [PubMed] [Google Scholar]
- Bush N.E., Dobscha S.K., Crumpton R., Denneson L.M., Hoffman J.E., Crain A.…Kinn J.T. A virtual hope box smartphone app as an accessory to therapy: proof-of-concept in a clinical sample of veterans. Suicide Life Threat. Behav. 2015;45(1):1–9. doi: 10.1111/sltb.12103. [DOI] [PubMed] [Google Scholar]
- Clough B.A., Casey L.M. Technological adjuncts to enhance current psychotherapy practices: a review. Clin. Psychol. Rev. 2011;31(3):279–292. doi: 10.1016/j.cpr.2010.12.008. [DOI] [PubMed] [Google Scholar]
- Cohen J. 2nd ed. Lawrence Erlbaum; Hillsdale, NJ: 1988. Statistical Power Analyses for the Behavioral Sciences. [Google Scholar]
- Day V., Mensink D., O’Sullivan M. Patterns of academic procrastination. J. Coll. Read. Learn. 2000;30:120–134. [Google Scholar]
- DiClemente C.C., Prochaska J.O., Fairhurst S.K., Velicer W.F., Velasquez M.M., Rossi J.S. The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change. J. Consult. Clin. Psychol. 1991;59(2):295–304. doi: 10.1037//0022-006x.59.2.295. [DOI] [PubMed] [Google Scholar]
- Donker T., Petrie K., Proudfoot J., Clarke J., Birch M.-R., Christensen H. Smartphones for smarter delivery of mental health programs: a systematic review. J. Med. Internet Res. 2013;15(11) doi: 10.2196/jmir.2791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dryden W. Sheldon Press; London, England: 2000. Overcoming Procrastination. [Google Scholar]
- Dryden W. Dealing with procrastination: the REBT approach and a demonstration session. J. Ration. Emot. Cogn. Behav. Ther. 2012;30(4):264–281. [Google Scholar]
- Feijoo C., Gómez-Barroso J.-L., Aguado J.-M., Ramos S. Mobile gaming: industry challenges and policy implications. Telecommun. Policy. 2012;36(3):212–221. [Google Scholar]
- Ferrari J.R., Parker J.T., Ware C.B. Vol. 7. 1992. Academic Procrastination: Personality Correlates With Myers-Briggs Types, Self-efficacy, and Academic Locus of Control; pp. 495–502. [Google Scholar]
- Ferrari J.R., O’Callghan J., Newbegin I. Prevalence of procrastination in the United States, United Kingdom, and Australia: arousal and avoidance delays among adults. N. Am. J. Psychol. 2005;7(1):1. [Google Scholar]
- Franklin J.C., Fox K.R., Franklin C.R., Kleiman E.M., Ribeiro J.D., Jaroszewski A.C.…Nock M.K. A brief mobile app reduces nonsuicidal and suicidal self-injury: evidence from three randomized controlled trials. J. Consult. Clin. Psychol. 2016;84(6):544–557. doi: 10.1037/ccp0000093. [DOI] [PubMed] [Google Scholar]
- Garrison K.A., Pal P., Rojiani R., Dallery J., O’Malley S.S., Brewer J.A.…Tsang J. A randomized controlled trial of smartphone-based mindfulness training for smoking cessation: a study protocol. BMC Psychiatry. 2015;15(1):83. doi: 10.1186/s12888-015-0468-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glick D.M., Orsillo S.M. An investigation of the efficacy of acceptance-based behavioral therapy for academic procrastination. J. Exp. Psychol. Gen. 2015;144(2):400–409. doi: 10.1037/xge0000050. [DOI] [PubMed] [Google Scholar]
- Grassi A., Preziosa A., Villani D., Riva G. A relaxing journey: the use of mobile phones for well-being improvement. Ann. Rev. CyberTher. Telemed. 2007;5:123–131. [Google Scholar]
- Harriott J., Ferrari J.R. Prevalence of procrastination among samples of adults. Psychol. Rep. 1996;78(2):611–616. [Google Scholar]
- Harrison V., Proudfoot J., Wee P.P., Parker G., Pavlovic D.H., Manicavasagar V. Mobile mental health: review of the emerging field and proof of concept study. J. Ment. Health. 2011;20(6):509–524. doi: 10.3109/09638237.2011.608746. [DOI] [PubMed] [Google Scholar]
- Haycock L.A., McCarthy P., Skay C.L. procrastination in college students: the role of self-efficacy and anxiety. J. Couns. Dev. 1998;76(3):317–324. [Google Scholar]
- Hayes A.F. Guilford Press; New York: 2013. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-based Approach. [Google Scholar]
- Heckhausen H., Gollwitzer P.M. Thought contents and cognitive functioning in motivational versus volitional states of mind. Motiv. Emot. 1987;11(2):101–120. [Google Scholar]
- Höcker A., Engberding M., Rist F. Hogrefe Verlag GmbH & Co. KG; Göttingen: 2013. Prokrastination – Ein Manual zur Behandlung des pathologischen Aufschiebens. [Google Scholar]
- Horne-Moyer H.L., Moyer B.H., Messer D.C., Messer E.S. The use of electronic games in therapy: a review with clinical implications. Curr. Psychiatry Rep. 2014;16(12):520. doi: 10.1007/s11920-014-0520-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard G.S., Hill T., Maxwell S.E., Coulter-Kern M., Coulter-Kern R. What's wrong with research literatures? And how to make them right. Rev. Gen. Psychol. 2009;13:146–166. [Google Scholar]
- Ioannidis J. Why most discovered true associations are inflated. Epidemiology. 2008;19:640–647. doi: 10.1097/EDE.0b013e31818131e7. [DOI] [PubMed] [Google Scholar]
- Jiménez-Serrano S., Tortajada S., García-Gómez J.M. A mobile health application to predict postpartum depression based on machine learning. Telemed. E-Health. 2015;21(7):567–574. doi: 10.1089/tmj.2014.0113. [DOI] [PubMed] [Google Scholar]
- Juarascio A.S., Manasse S.M., Goldstein S.P., Forman E.M., Butryn M.L. Review of smartphone applications for the treatment of eating disorders. Eur. Eat. Disord. Rev. 2015;23(1):1–11. doi: 10.1002/erv.2327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karas D., Spada M.M. Brief cognitive-behavioural coaching for procrastination: a case series. Coaching. 2009;2(1):44–53. [Google Scholar]
- Kauer S.D., Reid S.C., Crooke A.H.D., Khor A., Hearps S.J.C., Jorm A.F.…Patton G. Self-monitoring using mobile phones in the early stages of adolescent depression: randomized controlled trial. J. Med. Internet Res. 2012;14(3) doi: 10.2196/jmir.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawakami K., Phills C.E., Steele J.R., Dovidio J.F. (Close) distance makes the heart grow fonder: improving implicit racial attitudes and interracial interactions through approach behaviors. J. Pers. Soc. Psychol. 2007;92(6):957–971. doi: 10.1037/0022-3514.92.6.957. [DOI] [PubMed] [Google Scholar]
- Ly K.H., Dahl J., Carlbring P., Andersson G. Vol. 1. SpringerPlus; 2012. Development and Initial Evaluation of a Smartphone Application Based on Acceptance and Commitment Therapy; p. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahasneh A.M., Bataineh O.T., Al-Zoubi Z.H. The relationship between academic procrastination and parenting styles among Jordanian undergraduate university students. Open Psychol. J. 2016 [Google Scholar]
- Martell C.R., Dimidjian S., Herman-Dunn R. Guilford Press; 2010. Behavioral Activation for Depression: A Clinician's Guide. [Google Scholar]
- Mattila E., Pärkkä J., Hermersdorf M., Kaasinen J., Vainio J., Samposalo K.…Korhonen I. Mobile diary for wellness management—results on usage and usability in two user studies. IEEE Trans. Inf. Technol. Biomed. 2008;12(4):501–512. doi: 10.1109/TITB.2007.908237. [DOI] [PubMed] [Google Scholar]
- McTavish F.M., Chih M.-Y., Shah D., Gustafson D.H. How patients recovering from alcoholism use a smartphone intervention. J. Dual Diagn. 2012;8(4):294–304. doi: 10.1080/15504263.2012.723312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merry S.N., Stasiak K., Shepherd M., Frampton C., Fleming T., Lucassen M.F.G. The effectiveness of SPARX, a computerised self help intervention for adolescents seeking help for depression: randomised controlled non-inferiority trial. BMJ. 2012;344(7) doi: 10.1136/bmj.e2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miloff A., Marklund A., Carlbring P. The challenger app for social anxiety disorder: new advances in mobile psychological treatment. Internet Interv. 2015;2(4):382–391. [Google Scholar]
- Neenan M. Tackling procrastination: an REBT perspective for coaches. J. Ration. Emot. Cogn. Behav. Ther. 2008;26(1):53–62. [Google Scholar]
- Onwuegbuzie A.J. Academic procrastinators and perfectionistic tendencies among graduate students. J. Soc. Behav. Pers. 2000;15:103–109. [Google Scholar]
- Özer B.U., Demir A., Ferrari J.R. Exploring academic procrastination among Turkish students: possible gender differences in prevalence and reasons. J. Soc. Psychol. 2009;149(2):241–257. doi: 10.3200/SOCP.149.2.241-257. [DOI] [PubMed] [Google Scholar]
- Porta M. Human-computer input and output techniques: an analysis of current research and promising applications. Artif. Intell. Rev. 2007;28(3):197–226. [Google Scholar]
- Prada P., Zamberg I., Bouillault G., Jimenez N., Zimmermann J., Hasler R.…Perroud N. EMOTEO: a smartphone application for monitoring and reducing aversive tension in borderline personality disorder patients, a pilot study. Perspect. Psychiatr. Care. 2016 doi: 10.1111/ppc.12178. [DOI] [PubMed] [Google Scholar]
- Pychyl T.A., Flett G.L. Procrastination and self-regulatory failure: an introduction to the special issue. J. Ration. Emot. Cogn. Behav. Ther. 2012;30(4):203–212. [Google Scholar]
- Pychyl T.A., Lee J.M., Thibodeau R., Blunt A. Five days of emotion: an experience sampling study of undergraduate student procrastination. J. Soc. Behav. Pers. 2012;15(5):239–254. [Google Scholar]
- Rebetez M.M.L., Rochat L., Billieux J., Gay P., Van der Linden M. Do emotional stimuli interfere with two distinct components of inhibition? Cognit. Emot. 2015;29(3):559–567. doi: 10.1080/02699931.2014.922054. [DOI] [PubMed] [Google Scholar]
- Rozental A., Carlbring P. Internet-based cognitive behavior therapy for procrastination: study protocol for a randomized controlled trial. JMIR Res. Protoc. 2013;2(2) doi: 10.2196/resprot.2801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozental A., Carlbring P. Understanding and treating procrastination: a review of a common self-regulatory failure. Psychology. 2014;05(13):1488–1502. [Google Scholar]
- Rozental A., Forsell E., Svensson A., Andersson G., Carlbring P. Internet-based cognitive—behavior therapy for procrastination: a randomized controlled trial. J. Consult. Clin. Psychol. 2015;83(4):808–824. doi: 10.1037/ccp0000023. [DOI] [PubMed] [Google Scholar]
- Schouwenburg H.C. Academic procrastination: theoretical notions, measurement and research. In: Ferrari J.R., Johnson J.L., McCown W.G., editors. Procrastination and Task Avoidance: Theory, Research, and Treatment. Plenum Press; New York: 1995. pp. 71–96. [Google Scholar]
- Siang A.C., Rao Radha Krishna. Fifth International Symposium on Multimedia Software Engineering, 2003. Proceedings. IEEE; 2003. Theories of learning: a computer game perspective; pp. 239–245. [Google Scholar]
- Solomon L.J., Rothblum E.D. Academic procrastination: frequency and cognitive-behavioral correlates. J. Couns. Psychol. 1984;31(4):503–509. [Google Scholar]
- Stead R., Shanahan M.J., Neufeld R.W.J. “I'll go to therapy, eventually”: Procrastination, stress and mental health. Personal. Individ. Differ. 2010;49(3):175–180. [Google Scholar]
- Steel P. The nature of procrastination: a meta-analytic and theoretical review of quintessential self-regulatory failure. Psychol. Bull. 2007;133(1):65–94. doi: 10.1037/0033-2909.133.1.65. [DOI] [PubMed] [Google Scholar]
- Tice D.M., Baumeister R.F. Longitudinal study of procrastination, performance, stress, and health: the costs and benefits of dawdling. Psychol. Sci. 1997;8(6):454–458. [Google Scholar]
- Uzun Ozer B., Demir A., Ferrari J.R. Reducing academic procrastination through a group treatment program: a pilot study. J. Ration. Emot. Cogn. Behav. Ther. 2013;31(3):127–135. [Google Scholar]
- Wiers R.W., Eberl C., Rinck M., Becker E.S., Lindenmeyer J. Retraining automatic action tendencies changes alcoholic patients’ approach bias for alcohol and improves treatment outcome. Psychol. Sci. 2011;22(4):490–497. doi: 10.1177/0956797611400615. [DOI] [PubMed] [Google Scholar]
- Wiers C.E., Ludwig V.U., Gladwin T.E., Park S.Q., Heinz A., Wiers R.W.…Bermpohl F. Effects of cognitive bias modification training on neural signatures of alcohol approach tendencies in male alcohol-dependent patients. Addict. Biol. 2015;20(5):990–999. doi: 10.1111/adb.12221. [DOI] [PubMed] [Google Scholar]