Abstract
Skin cancers are the most common form of cancer in humans. They can largely be categorized into Melanoma and Non-melanoma skin cancers. The latter mainly includes Squamous Cell Carcinoma (SCC) and Basal Cell Carcinoma (BCC), and have a higher incidence than melanomas. There has been a recent emergence of interest in the role of non-coding RNA's in pathogenesis of skin cancers. The transcripts which lack any protein coding capacity are called non-coding RNA. These non-coding RNA are further classified based on their length; small non-coding RNA (<200 nucleotides) and long non-coding RNA (>200 nucleotides). ncRNA They are involved at multiple transcriptional, post transcriptional and epigenetic levels, modulating cell proliferation, angiogenesis, senescence and apoptosis. Their expression pattern has also been linked to metastases, drug resistance and long term prognosis. They have both diagnostic and prognostic significance for skin cancers, and can also be a target for future therapies for cutaneous malignancies. More research is needed to further utilize their potential as therapeutic targets.
Keywords: Skin cancer, Non-coding RNA's, miRNA, Cell proliferation, Invasion, Metastasis
1. Introduction
Skin cancers are the most common form of cancer in humans. They can largely be categorized into Melanoma and Non-melanoma skin cancers. The latter mainly includes Squamous Cell Carcinoma (SCC) and Basal Cell Carcinoma (BCC), and have a higher incidence than melanomas [1]. There has been a recent emergence of interest in the role of non-codingRNA's (ncRNAs) in pathogenesis of skin cancers. Majority of the studies focus on the role of ncRNA in epigenetics of melanoma and there is only limited amount of information available on non-melanoma skin cancers. Herein, we attempt to review the role of non-coding RNA in pathogenesis as well as potential therapeutic targets for skin cancers.
Recent advances in sequencing technologies have questioned the possible roles of entities that were previously considered to have minimal or insignificant contribution in disease pathogenesis and epigenetics. Although >75% of human genome is selectively transcribed, only a small portion (1–2%) of transcripts are eventually translated into proteins. The transcripts which lack any protein coding capacity are called non-coding RNA. These non-coding RNA are further classified based on their length; small non-coding RNA(<200 nucleotides) and long non-coding RNA (>200 nucleotides). Small non-codingRNA largely consists of microRNA (<20 nucleotides) and small nucleolar RNA. MicroRNAs are the most extensively studied group of RNAs which function in negative regulation of gene expression by binding to target mRNA leading to induction of degradation or inhibition of its translation. Long non-coding RNAs also possess functional capacity owing to their longer lengths and additional ability to fold upon themselves forming tertiary structures [2], [3].
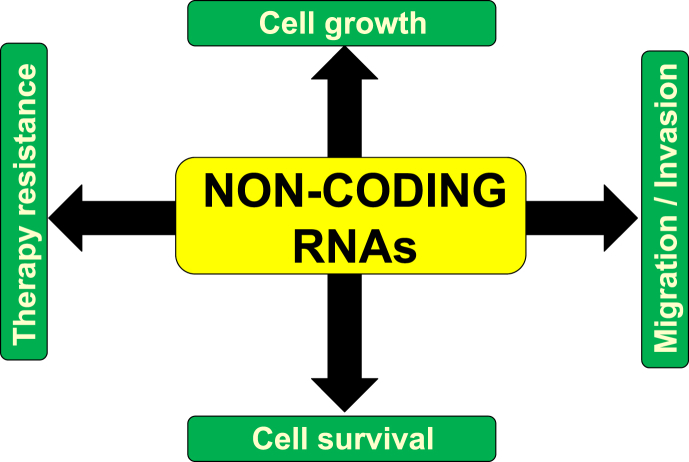
The growing body of evidence suggests that ncRNA regulate key tumor pathways and have shown to be involved in almost all human tumors. They are involved at multiple transcriptional, post transcriptional and epigenetic levels, modulating cell proliferation, angiogenesis, senescence and apoptosis (See Fig. 1). Their expression pattern has also been linked to metastases, drug resistance and long term prognosis [4], [5], [6], [7], [8], [9]. Resistance of cancers to chemotherapeutic agents is the main clinical barrier to cure and improve treatment outcomes. Therefore, better understanding of the role of non-coding RNA will help us improve treatment and prognosis of skin cancers.
Fig. 1.
Role of ncRNAs in cancers.
2. Role of ncRNA in skin cancers
Skin cancers are becoming a leading cause of morbidity and mortality worldwide. Non-melanoma skin cancers are more common than melanomas but the latter is a major cause of skin cancer related deaths. Early detection of melanoma is very important in improving survival rates. Treatment options for advanced melanoma are limited and needs more innovative strategies and targets. Pathogenesis of melanoma is very complex and involves interaction between a network of genes, regulatory mechanisms and various signaling pathways. Non-codingRNAs have garnered huge interest in the recent years regarding their role in tumorigenesis, not limited to melanomas. Their potential role in pathogenesis and as an early prognostic indicator needs further elucidation.
Melanocytes are pigment producing cells that are derived from neural crest cells. A series of steps ultimately lead to melanoblast formation and transport as melanosomes to keratinocytes. A number of melanocyte-specific proteins are expressed on melanocytes such as: Tyrosinase, Tyrosinase Protein 1 and 2, Melanosomal Matrix Protein and Microphthalmia Transcription Factor (MITF) [10]. Other genes including MITF, SOX 10, PAX3, [11], [12], [13] members of the Wnt and notch pathways [14], [15], [16], KIT and cyclins [17] all play important roles in stepwise metamorphosis of melanocytes. In addition to the contribution of protein coding genes, many non-coding genes also have a vital contribution to the signaling process. Small and long non-codingRNAs are discussed in detail pertaining to their role in melanocyte biology and cancer formation. Most commonly implicated miRNAs in skin cancers have been described in Table 1.
Table 1.
List of non-coding RNAs currently implicated in skin cancers.
| Non-coding RNA | Target gene | Type of non-coding RNA | Expression | Skin Cancer association | References |
|---|---|---|---|---|---|
| miR-211 | BRN2, KCNMA1, NFAT5, TGFBR2 | microRNA | Downregulated | Melanoma | [20], [21], [23], [45] |
| miR-200c | ZEB1, DEF1, Nil-2-A | microRNA | Downregulated | Melanoma | [46] |
| miR-210 | PTPN1 TP53I11, HOXA1 | microRNA | Upregulated | Melanoma | [27], [47], [48] |
| miR-196a | HOX-B7, bFGF, BMP-4 | microRNA | Downregulated | Melanoma | [25] |
| miR-30b | GALNT7 | microRNA | Upregulated | Melanoma | [26], [49] |
| Let-7a | Integrin beta 3 | microRNA | Downregulated | Melanoma, BCC | [50], [51] |
| SPRY4-IT1 | n/a | Antisense long non-coding RNA | Upregulated | Melanoma | [52], [53] |
| BANCR | CXC11 | Long intergenic noncoding RNA (lincRNA) | Upregulated | Melanoma | [54] |
| LlME23 | PSF | Long intergenic noncoding RNA (lincRNA) | Upregulated | Melanoma | [55] |
| ANRIL | n/a | Long intergenic noncoding RNA (lincRNA) | Upregulated | Melanoma | [56] |
| HOTAIR | HOXC | Long intergenic noncoding RNA (lincRNA) | Upregulated | Melanoma | [57] |
| miR-21 | PTEN, BCL2 | microRNA | Upregulated | BCC, SCC, Melanoma | [51], [58], [59], [60] |
| miR-29c | DNMT3A and DNMT3B | microRNA | Downregulated | BCC | [61] |
| miR-124 | ERK2 | microRNA | Downregulated | SCC | [62] |
| miR-130a | BCL-2 | microRNA | Upregulated | BCC | [61] |
2.1. MicroRNAs (miRNA) in melanocyte biology and immune response
miRNAs are small noncoding RNA (<200 nucleotides) that are involved in fine tuning of more than 60% of proteins [18], [19]. Several studies have confirmed the aberrant expression of miRNAs in melanoma cells specifically miR-211. Several groups have demonstrated that miR-211 as the most common miRNA expressed differentially in normal vs melanoma cells. Ectopic expression of miR-211 results in inhibition of growth and invasion of melanoma cells suggesting their role as tumor suppressor gene [20], [21]. This miR-211 is encoded by a region in the sixth intron of TRPM1 (Transient Receptor Potential cation channel subfamily Member M) [22]. The level of miR-211 expression in melanoma cells has been found to be inversely proportional to the invasive potential of melanomas – with melanomas exhibiting reduced expression of miR-211 being highly invasive and vice versa [20], [21], [23], [24]. Bell et al. have identified a new miR-211 target, NUAK1 which promotes melanoma cell adhesion [23]. Another miRNA, namely miR-196a was also shown to exhibit tumor suppressor properties as its expression was significantly reduced in malignant melanoma cells [25] (see Fig. 1).
Conversely, overexpression of several miRNA's (miR-210, miR-30b and miR-30) was seen to be upregulated in melanomas. These miRNAs are linked to stimulation of an immunosuppressive environment through cell-lysis by antigen-specific cytotoxic T lymphocytes (CTLs), changes in glycosylating proteins and increased synthesis of immunosuppressive molecules [26], [27].
2.2. Role of miRNA in melanoma cell cycle and cell proliferation
Undifferentiated and uncontrolled cell proliferation is a hallmark of skin cancer. Cyclin dependent kinases and EF2 transcription factors are the main cell cycle regulators. Other proteins such as asc-myc, p27 and pTEN upregulate the CDKs and indirectly function as cell cycle regulators. Non-coding RNAs particularly miRNA directly targetthese cell cycle regulators [28], [29], [30]. let-7b is a miRNA that decreases cell proliferation by targeting cell cycle regulators by acting as a tumor suppressor gene [31]. Another miRNA-193b downregulates cyclins D1 and D2 which are responsible for uncontrolled cell growth and invasion [32]. Some miRNAs are shown to indirectly control the cell cycle through p27 and p53 tumor suppressor genes. A few studies have shown that miR221/222 directly inhibit p27and lead to increased proliferation of melanoma cells. It has also been postulated that miR221/222 also inhibit c-kit, PTEN and TIMP3 tumor suppressor genes [33], [34]. Other miRNAs such as miR205, miR149, miR18b, miR21, miR203 and miR26a have been shown to regulate cell cycle proteins through a cyclin independent manner [35].
2.3. Role of miRNA in tumor invasion
Multiple factors are responsible for cell migration and tumor invasion including BSG, FSCN1, β3integrin, MARKS, GALANT 7, c-met and NFK-b. Like other regulatory processes, miRNA have been shown to actively regulate the above-mentioned proteins. In a study by Segura et al., it was demonstrated that miR182 was differentially expressed in melanoma vs benign melanocytes, directly targeting proteins such as FOXO3 and MITF which contribute to migration and invasion of melanoma cells. Animal studies have demonstrated that miR182 can serve as a therapeutic target as its expression was linked to metastasis of cancer in various mouse models [36]. Another miRNA 145 is shown to downregulate FSCN1 (fascin acting bundling protein 1) which is a known regulator of cell migration and invasion [37], [38].
2.4. Role of long ncRNA in melanoma
Long non-coding RNA are transcribed by RNA polymerase II as an initial step which leads to formation of pri-ln cRNA. This is subjected to further processing via splicing and polyadenylation which ultimately results in formation of mature-lnc RNA. These mature-lncRNAs possess an intrinsic ability to interact with RNA, DNA and proteins as they can serve as tethers, decoys and scaffolds owing to their tertiary structure with surface interaction properties. Thus, lncRNA play an important role in cell regulation, proliferation and apoptosis [39], [40], [41], [42]. Previously considered to be junk RNA, there is growing evidence of their role in skin cancers. Unlike miRNA, lncRNA has not been studied extensively and more research is needed to elucidate their specific role in cancers.
2.5. Role of ncRNA in non-melanoma skin cancers
Early evidence suggests that microRNA also has a role in pathogenesis of non-melanoma skin cancers, including Basal Cell Carcinoma (BCC) and cutaneous squamous cell carcinoma (cSCC) – the most common and the second most common forms of human cancers respectively. The expression levels of miRNA machinery (Drosha, DGCR8, AGO1, AGO2, PACT, and TARBP1) have been shown to be significantly higher in BCC and cSCC when compared to healthy controls [43].
The role of long non-coding RNA has also been studied in several cancers. Anticancer drug resistance has been shown to be associated with changes in expression of long non-coding RNA, suggesting a novel pathway to identify and possible reverse tumor drug resistance [44].
3. Conclusion
Skin cancers especially melanoma is resistant to many chemotherapeutic agents which is the main clinical barrier to improving treatment outcomes and reducing melanoma related mortality. With the increase in worldwide incidence of melanoma, it is important to find new and effective therapeutic targets. As described in this article, non-coding RNAs play a very crucial role in the pathology of skin cancers. They have both diagnostic and prognostic significance for skin cancers, and can also be a target for future therapies for cutaneous malignancies. Early diagnosis of melanoma remains the key to better treatment outcomes. There is sufficient evidence suggesting the key role of miRNA and lncRNA was early diagnostic markers. More research is needed to further utilize their potential as therapeutic targets.
References
- 1.Bath-Hextall F., Nalubega S., Evans C. The needs and experiences of skin cancer patients: a qualitative systematic review with meta-synthesis. Br. J. Dermatol. 2016 doi: 10.1111/bjd.15148. [DOI] [PubMed] [Google Scholar]
- 2.Djebali S., Davis C.A., Merkel A., Dobin A., Lassmann T., Mortazavi A. Landscape of transcription in human cells. Nature. 2012;489(7414):101–108. doi: 10.1038/nature11233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deniz E., Erman B. Long noncoding RNA (lincRNA), a new paradigm in gene expression control. Funct. Integr. Genomics. 2016 doi: 10.1007/s10142-016-0524-x. [DOI] [PubMed] [Google Scholar]
- 4.Feng S., Yao J., Chen Y., Geng P., Zhang H., Ma X. Expression and functional role of reprogramming-related long noncoding RNA (lincRNA-ROR) in glioma. J. Mol. Neurosci. 2015;56(3):623–630. doi: 10.1007/s12031-014-0488-z. [DOI] [PubMed] [Google Scholar]
- 5.Hu L., Wu Y., Tan D., Meng H., Wang K., Bai Y. Up-regulation of long noncoding RNA MALAT1 contributes to proliferation and metastasis in esophageal squamous cell carcinoma. J. Exp. Clin. Cancer Res. 2015;34:7. doi: 10.1186/s13046-015-0123-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prensner J.R., Chinnaiyan A.M. The emergence of lncRNAs in cancer biology. Cancer Discov. 2011;1(5):391–407. doi: 10.1158/2159-8290.CD-11-0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang X., Xie X., Xiao Y.F., Xie R., Hu C.J., Tang B. The emergence of long non-coding RNAs in the tumorigenesis of hepatocellular carcinoma. Cancer Lett. 2015;360(2):119–124. doi: 10.1016/j.canlet.2015.02.035. [DOI] [PubMed] [Google Scholar]
- 8.Chen F., Tian Y., Pang E.J., Wang Y., Li L. MALAT2-activated long noncoding RNA indicates a biomarker of poor prognosis in gastric cancer. Cancer Gene Ther. 2015 doi: 10.1038/cgt.2015.6. [DOI] [PubMed] [Google Scholar]
- 9.Han L., Zhang E.B., Yin D.D., Kong R., Xu T.P., Chen W.M. Low expression of long noncoding RNA PANDAR predicts a poor prognosis of non-small cell lung cancer and affects cell apoptosis by regulating Bcl-2. Cell Death Dis. 2015;6:e1665. doi: 10.1038/cddis.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maddodi N., Setaluri V. Role of UV in cutaneous melanoma. Photochem Photobiol. 2008;84(2):528–536. doi: 10.1111/j.1751-1097.2007.00283.x. [DOI] [PubMed] [Google Scholar]
- 11.Wegner M. Secrets to a healthy Sox life: lessons for melanocytes. Pigment. Cell Res. 2005;18(2):74–85. doi: 10.1111/j.1600-0749.2005.00218.x. [DOI] [PubMed] [Google Scholar]
- 12.Verastegui C., Bille K., Ortonne J.P., Ballotti R. Regulation of the microphthalmia-associated transcription factor gene by the Waardenburg syndrome type 4 gene, SOX10. J. Biol. Chem. 2000;275(40):30757–30760. doi: 10.1074/jbc.C000445200. [DOI] [PubMed] [Google Scholar]
- 13.Medic S., Ziman M. PAX3 expression in normal skin melanocytes and melanocytic lesions (naevi and melanomas) PLoS One. 2010;5(4):e9977. doi: 10.1371/journal.pone.0009977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weeraratna A.T., Jiang Y., Hostetter G., Rosenblatt K., Duray P., Bittner M. Wnt5a signaling directly affects cell motility and invasion of metastatic melanoma. Cancer Cell. 2002;1(3):279–288. doi: 10.1016/s1535-6108(02)00045-4. [DOI] [PubMed] [Google Scholar]
- 15.Balint K., Xiao M., Pinnix C.C., Soma A., Veres I., Juhasz I. Activation of Notch1 signaling is required for beta-catenin-mediated human primary melanoma progression. J. Clin. Invest. 2005;115(11):3166–3176. doi: 10.1172/JCI25001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zabierowski S.E., Baubet V., Himes B., Li L., Fukunaga-Kalabis M., Patel S. Direct reprogramming of melanocytes to neural crest stem-like cells by one defined factor. Stem Cells. 2011;29(11):1752–1762. doi: 10.1002/stem.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grichnik J.M., Burch J.A., Burchette J., Shea C.R. The SCF/KIT pathway plays a critical role in the control of normal human melanocyte homeostasis. J. Invest. Dermatol. 1998;111(2):233–238. doi: 10.1046/j.1523-1747.1998.00272.x. [DOI] [PubMed] [Google Scholar]
- 18.Friedman R.C., Farh K.K., Burge C.B., Bartel D.P. Most mammalian mRNAs are conserved targets of microRNAs. Genome Res. 2009;19(1):92–105. doi: 10.1101/gr.082701.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.John B., Enright A.J., Aravin A., Tuschl T., Sander C., Marks D.S. Human MicroRNA targets. PLoS Biol. 2004;2(11):e363. doi: 10.1371/journal.pbio.0020363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mazar J., DeYoung K., Khaitan D., Meister E., Almodovar A., Goydos J. The regulation of miRNA-211 expression and its role in melanoma cell invasiveness. PLoS One. 2010;5(11):e13779. doi: 10.1371/journal.pone.0013779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Levy C., Khaled M., Iliopoulos D., Janas M.M., Schubert S., Pinner S. Intronic miR-211 assumes the tumor suppressive function of its host gene in melanoma. Mol. Cell. 2010;40(5):841–849. doi: 10.1016/j.molcel.2010.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Valdes-Rodriguez R., Kaushik S.B., Yosipovitch G. Transient receptor potential channels and dermatological disorders. Curr. Top. Med. Chem. 2013;13(3):335–343. doi: 10.2174/15680266112129990090. [DOI] [PubMed] [Google Scholar]
- 23.Bell R.E., Khaled M., Netanely D., Schubert S., Golan T., Buxbaum A. Transcription factor/microRNA axis blocks melanoma invasion program by miR-211 targeting NUAK1. J. Invest. Dermatol. 2014;134(2):441–451. doi: 10.1038/jid.2013.340. [DOI] [PubMed] [Google Scholar]
- 24.Margue C., Philippidou D., Reinsbach S.E., Schmitt M., Behrmann I., Kreis S. New target genes of MITF-induced microRNA-211 contribute to melanoma cell invasion. PLoS One. 2013;8(9):e73473. doi: 10.1371/journal.pone.0073473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mueller D.W., Bosserhoff A.K. MicroRNA miR-196a controls melanoma-associated genes by regulating HOX-C8 expression. Int. J. Cancer. 2011;129(5):1064–1074. doi: 10.1002/ijc.25768. [DOI] [PubMed] [Google Scholar]
- 26.Gaziel-Sovran A., Segura M.F., Di Micco R., Collins M.K., Hanniford D., Vega-Saenz de Miera E. miR-30b/30d regulation of GalNAc transferases enhances invasion and immunosuppression during metastasis. Cancer Cell. 2011;20(1):104–118. doi: 10.1016/j.ccr.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Noman M.Z., Buart S., Romero P., Ketari S., Janji B., Mari B. Hypoxia-inducible miR-210 regulates the susceptibility of tumor cells to lysis by cytotoxic T cells. Cancer Res. 2012;72(18):4629–4641. doi: 10.1158/0008-5472.CAN-12-1383. [DOI] [PubMed] [Google Scholar]
- 28.Mateyak M.K., Obaya A.J., Sedivy J.M. c-Myc regulates cyclin D-Cdk4 and -Cdk6 activity but affects cell cycle progression at multiple independent points. Mol. Cell Biol. 1999;19(7):4672–4683. doi: 10.1128/mcb.19.7.4672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Walter K.A., Hossain M.A., Luddy C., Goel N., Reznik T.E., Laterra J. Scatter factor/hepatocyte growth factor stimulation of glioblastoma cell cycle progression through G(1) is c-Myc dependent and independent of p27 suppression, Cdk2 activation, or E2F1-dependent transcription. Mol. Cell Biol. 2002;22(8):2703–2715. doi: 10.1128/MCB.22.8.2703-2715.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mamillapalli R., Gavrilova N., Mihaylova V.T., Tsvetkov L.M., Wu H., Zhang H. PTEN regulates the ubiquitin-dependent degradation of the CDK inhibitor p27(KIP1) through the ubiquitin E3 ligase SCF(SKP2) Curr. Biol. 2001;11(4):263–267. doi: 10.1016/s0960-9822(01)00065-3. [DOI] [PubMed] [Google Scholar]
- 31.Schultz J., Lorenz P., Gross G., Ibrahim S., Kunz M. MicroRNA let-7b targets important cell cycle molecules in malignant melanoma cells and interferes with anchorage-independent growth. Cell Res. 2008;18(5):549–557. doi: 10.1038/cr.2008.45. [DOI] [PubMed] [Google Scholar]
- 32.Chen J., Feilotter H.E., Pare G.C., Zhang X., Pemberton J.G., Garady C. MicroRNA-193b represses cell proliferation and regulates cyclin D1 in melanoma. Am. J. Pathol. 2010;176(5):2520–2529. doi: 10.2353/ajpath.2010.091061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Igoucheva O., Alexeev V. MicroRNA-dependent regulation of cKit in cutaneous melanoma. Biochem. Biophys. Res. Commun. 2009;379(3):790–794. doi: 10.1016/j.bbrc.2008.12.152. [DOI] [PubMed] [Google Scholar]
- 34.Felicetti F., Errico M.C., Bottero L., Segnalini P., Stoppacciaro A., Biffoni M. The promyelocytic leukemia zinc finger-microRNA-221/-222 pathway controls melanoma progression through multiple oncogenic mechanisms. Cancer Res. 2008;68(8):2745–2754. doi: 10.1158/0008-5472.CAN-07-2538. [DOI] [PubMed] [Google Scholar]
- 35.Dar A.A., Majid S., de Semir D., Nosrati M., Bezrookove V., Kashani-Sabet M. miRNA-205 suppresses melanoma cell proliferation and induces senescence via regulation of E2F1 protein. J. Biol. Chem. 2011;286(19):16606–16614. doi: 10.1074/jbc.M111.227611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Segura M.F., Hanniford D., Menendez S., Reavie L., Zou X., Alvarez-Diaz S. Aberrant miR-182 expression promotes melanoma metastasis by repressing FOXO3 and microphthalmia-associated transcription factor. Proc. Natl. Acad. Sci. U. S. A. 2009;106(6):1814–1819. doi: 10.1073/pnas.0808263106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dynoodt P., Speeckaert R., De Wever O., Chevolet I., Brochez L., Lambert J. miR-145 overexpression suppresses the migration and invasion of metastatic melanoma cells. Int. J. Oncol. 2013;42(4):1443–1451. doi: 10.3892/ijo.2013.1823. [DOI] [PubMed] [Google Scholar]
- 38.Shonukan O., Bagayogo I., McCrea P., Chao M., Hempstead B. Neurotrophin-induced melanoma cell migration is mediated through the actin-bundling protein fascin. Oncogene. 2003;22(23):3616–3623. doi: 10.1038/sj.onc.1206561. [DOI] [PubMed] [Google Scholar]
- 39.Ip J.Y., Nakagawa S. Long non-coding RNAs in nuclear bodies. Dev. Growth Differ. 2012;54(1):44–54. doi: 10.1111/j.1440-169X.2011.01303.x. [DOI] [PubMed] [Google Scholar]
- 40.Brockdorff N. Noncoding RNA and polycomb recruitment. RNA. 2013;19(4):429–442. doi: 10.1261/rna.037598.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beltran M., Puig I., Pena C., Garcia J.M., Alvarez A.B., Pena R. A natural antisense transcript regulates Zeb2/Sip1 gene expression during Snail1-induced epithelial-mesenchymal transition. Genes Dev. 2008;22(6):756–769. doi: 10.1101/gad.455708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gong C., Maquat L.E. lncRNAs transactivate STAU1-mediated mRNA decay by duplexing with 3' UTRs via Alu elements. Nature. 2011;470(7333):284–288. doi: 10.1038/nature09701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sand M., Sand D., Altmeyer P., Bechara F.G. MicroRNA in non-melanoma skin cancer. Cancer Biomark. 2012;11(6):253–257. doi: 10.3233/CBM-2012-0274. [DOI] [PubMed] [Google Scholar]
- 44.Deng H., Zhang J., Shi J., Guo Z., He C., Ding L. Role of long non-coding RNA in tumor drug resistance. Tumour Biol. 2016;37(9):11623–11631. doi: 10.1007/s13277-016-5125-8. [DOI] [PubMed] [Google Scholar]
- 45.Boyle G.M., Woods S.L., Bonazzi V.F., Stark M.S., Hacker E., Aoude L.G. Melanoma cell invasiveness is regulated by miR-211 suppression of the BRN2 transcription factor. Pigment. Cell Melanoma Res. 2011;24(3):525–537. doi: 10.1111/j.1755-148X.2011.00849.x. [DOI] [PubMed] [Google Scholar]
- 46.Hurteau G.J., Spivack S.D., Brock G.J. Potential mRNA degradation targets of hsa-miR-200c, identified using informatics and qRT-PCR. Cell Cycle. 2006;5(17):1951–1956. doi: 10.4161/cc.5.17.3133. [DOI] [PubMed] [Google Scholar]
- 47.Lu X., Malumbres R., Shields B., Jiang X., Sarosiek K.A., Natkunam Y. PTP1B is a negative regulator of interleukin 4-induced STAT6 signaling. Blood. 2008;112(10):4098–4108. doi: 10.1182/blood-2008-03-148726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Medgyesi D., Hobeika E., Biesen R., Kollert F., Taddeo A., Voll R.E. The protein tyrosine phosphatase PTP1B is a negative regulator of CD40 and BAFF-R signaling and controls B cell autoimmunity. J. Exp. Med. 2014;211(3):427–440. doi: 10.1084/jem.20131196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brockhausen I. Mucin-type O-glycans in human colon and breast cancer: glycodynamics and functions. EMBO Rep. 2006;7(6):599–604. doi: 10.1038/sj.embor.7400705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Muller D.W., Bosserhoff A.K. Integrin beta 3 expression is regulated by let-7a miRNA in malignant melanoma. Oncogene. 2008;27(52):6698–6706. doi: 10.1038/onc.2008.282. [DOI] [PubMed] [Google Scholar]
- 51.Heffelfinger C., Ouyang Z., Engberg A., Leffell D.J., Hanlon A.M., Gordon P.B. Correlation of global MicroRNA expression with basal cell carcinoma subtype. G3 Bethesda. 2012;2(2):279–286. doi: 10.1534/g3.111.001115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Khaitan D., Dinger M.E., Mazar J., Crawford J., Smith M.A., Mattick J.S. The melanoma-upregulated long noncoding RNA SPRY4-IT1 modulates apoptosis and invasion. Cancer Res. 2011;71(11):3852–3862. doi: 10.1158/0008-5472.CAN-10-4460. [DOI] [PubMed] [Google Scholar]
- 53.Mazar J., Zhao W., Khalil A.M., Lee B., Shelley J., Govindarajan S.S. The functional characterization of long noncoding RNA SPRY4-IT1 in human melanoma cells. Oncotarget. 2014;5(19):8959–8969. doi: 10.18632/oncotarget.1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Flockhart R.J., Webster D.E., Qu K., Mascarenhas N., Kovalski J., Kretz M. BRAFV600E remodels the melanocyte transcriptome and induces BANCR to regulate melanoma cell migration. Genome Res. 2012;22(6):1006–1014. doi: 10.1101/gr.140061.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wu C.F., Tan G.H., Ma C.C., Li L. The non-coding RNA llme23 drives the malignant property of human melanoma cells. J. Genet. Genomics. 2013;40(4):179–188. doi: 10.1016/j.jgg.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 56.Pasmant E., Sabbagh A., Vidaud M., Bieche I. ANRIL, a long, noncoding RNA, is an unexpected major hotspot in GWAS. Faseb J. 2011;25(2):444–448. doi: 10.1096/fj.10-172452. [DOI] [PubMed] [Google Scholar]
- 57.Tang L., Zhang W., Su B., Yu B. Long noncoding RNA HOTAIR is associated with motility, invasion, and metastatic potential of metastatic melanoma. Biomed. Res. Int. 2013;2013:251098. doi: 10.1155/2013/251098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Di Cristofano A., Pandolfi P.P. The multiple roles of PTEN in tumor suppression. Cell. 2000;100(4):387–390. doi: 10.1016/s0092-8674(00)80674-1. [DOI] [PubMed] [Google Scholar]
- 59.Satzger I., Mattern A., Kuettler U., Weinspach D., Niebuhr M., Kapp A. microRNA-21 is upregulated in malignant melanoma and influences apoptosis of melanocytic cells. Exp. Dermatol. 2012;21(7):509–514. doi: 10.1111/j.1600-0625.2012.01510.x. [DOI] [PubMed] [Google Scholar]
- 60.Dziunycz P., Iotzova-Weiss G., Eloranta J.J., Lauchli S., Hafner J., French L.E. Squamous cell carcinoma of the skin shows a distinct microRNA profile modulated by UV radiation. J. Invest. Dermatol. 2010;130:2686–2689. doi: 10.1038/jid.2010.169. United States. [DOI] [PubMed] [Google Scholar]
- 61.Sand M., Skrygan M., Sand D., Georgas D., Hahn S.A., Gambichler T. Expression of microRNAs in basal cell carcinoma. Br. J. Dermatol. 2012;167(4):847–855. doi: 10.1111/j.1365-2133.2012.11022.x. [DOI] [PubMed] [Google Scholar]
- 62.Yamane K., Jinnin M., Etoh T., Kobayashi Y., Shimozono N., Fukushima S. Down-regulation of miR-124/-214 in cutaneous squamous cell carcinoma mediates abnormal cell proliferation via the induction of ERK. J. Mol. Med. Berl. 2013;91(1):69–81. doi: 10.1007/s00109-012-0935-7. [DOI] [PubMed] [Google Scholar]