A new, safe, and effective vaccine against poliovirus is urgently needed not only to complete the eradication of the virus but also to be used in the future to prevent possible virus reemergence in a postpolio world. Currently, new formulations of the oral vaccine, as well as improvements to the inactivated vaccine, are being explored. In this study, we designed a viral vector with mucosal tropism that expresses poliovirus capsid proteins. Thus, poliovirus VLPs are produced in vivo, in the cells of a vaccine recipient, and are presented to the immune system in the context of vector virus replication, stimulating the development of systemic and mucosal immune responses. Such an approach allows the development of an affordable and safe vaccine that does not rely on the full-length poliovirus genome at any stage.
KEYWORDS: Newcastle disease virus, eradication, immunization, poliovirus, vectored vaccine
ABSTRACT
The poliovirus eradication initiative has spawned global immunization infrastructure and dramatically decreased the prevalence of the disease, yet the original virus eradication goal has not been met. The suboptimal properties of the existing vaccines are among the major reasons why the program has repeatedly missed eradication deadlines. Oral live poliovirus vaccine (OPV), while affordable and effective, occasionally causes the disease in the primary recipients, and the attenuated viruses rapidly regain virulence and can cause poliomyelitis outbreaks. Inactivated poliovirus vaccine (IPV) is safe but expensive and does not induce the mucosal immunity necessary to interrupt virus transmission. While the need for a better vaccine is widely recognized, current efforts are focused largely on improvements to the OPV or IPV, which are still beset by the fundamental drawbacks of the original products. Here we demonstrate a different design of an antipoliovirus vaccine based on in situ production of virus-like particles (VLPs). The poliovirus capsid protein precursor, together with a protease required for its processing, are expressed from a Newcastle disease virus (NDV) vector, a negative-strand RNA virus with mucosal tropism. In this system, poliovirus VLPs are produced in the cells of vaccine recipients and are presented to their immune systems in the context of active replication of NDV, which serves as a natural adjuvant. Intranasal administration of the vectored vaccine to guinea pigs induced strong neutralizing systemic and mucosal antibody responses. Thus, the vectored poliovirus vaccine combines the affordability and efficiency of a live vaccine with absolute safety, since no full-length poliovirus genome is present at any stage of the vaccine life cycle.
IMPORTANCE A new, safe, and effective vaccine against poliovirus is urgently needed not only to complete the eradication of the virus but also to be used in the future to prevent possible virus reemergence in a postpolio world. Currently, new formulations of the oral vaccine, as well as improvements to the inactivated vaccine, are being explored. In this study, we designed a viral vector with mucosal tropism that expresses poliovirus capsid proteins. Thus, poliovirus VLPs are produced in vivo, in the cells of a vaccine recipient, and are presented to the immune system in the context of vector virus replication, stimulating the development of systemic and mucosal immune responses. Such an approach allows the development of an affordable and safe vaccine that does not rely on the full-length poliovirus genome at any stage.
INTRODUCTION
Poliovirus, a prototype member of the Enterovirus genus of the Picornaviridae family of positive-strand RNA viruses, normally replicates in the gut and is transmitted via the fecal-oral route. Most poliovirus infections are asymptomatic or cause mild distress, but in <1% of infections, the virus invades the central nervous system via an unknown mechanism. Its replication in motor neurons may induce a spectrum of neurological symptoms, from temporary weakness to permanent paralysis of limbs and muscles controlling breathing, occasionally leading to death (1). Humans are the only natural host of poliovirus, and there are three poliovirus serotypes, all of which can cause paralysis.
The success of the Global Polio Eradication Initiative, which brought down the number of poliovirus-induced cases of paralysis from ∼380,000 in 1988, when it started, to <50 in 2016 (2), is due to an oral poliovirus vaccine (OPV). For almost the entire campaign, the vaccine was deployed in its original formulation, developed by Albert Sabin in the late 1950s. It contains a mixture of attenuated strains that ensures the development of robust immune responses to all three serotypes of poliovirus. The most important advantages of this vaccine, which proved crucial for the success of global vaccination campaigns, are (i) the ability to induce a strong mucosal immune response, necessary for the interruption of viral transmission, and (ii) the low cost of its production and administration. The propagation of attenuated vaccine strains requires minimal biosafety precautions, and the oral vaccine can be easily administered by virtually any person without special training. Yet this vaccine has important drawbacks, which became critical as the transmission of wild-type (wt) viruses was diminishing. First, replication of vaccine strains may cause the disease in roughly one in a million primary vaccine recipients (vaccine-associated paralytic poliomyelitis [VAPP]). Second, replicating viruses rapidly lose attenuating mutations and undergo recombination with other enteroviruses, thus regaining a neuropathological phenotype indistinguishable from that of wt polioviruses (3, 4). These vaccine-derived polioviruses (VDPV) can establish circulation in human populations and have caused numerous outbreaks of paralytic poliomyelitis (5, 6). Finally, at least several cases have been documented in which recipients of the Sabin vaccine became chronically infected with poliovirus without developing the disease, and in some cases, they have been excreting the virus for decades (7–9). In recent years, several attempts have been made to minimize the negative impact of immunization with live vaccine, such as the introduction of vaccines covering only selected serotypes, as well as the development of vaccine strains with a reduced propensity for recombination and a more-stable attenuated phenotype (10, 11). Still, the intrinsic genetic instability of positive-strand RNA viruses does not permit the development of a strain completely lacking the potential for reversion, and the administration of live vaccine inevitably releases polioviruses into the environment, making achievement of the eradication goal impossible.
To circumvent the negative consequences of live vaccine while maintaining an adequate level of population protection, the road map of the eradication campaign calls for the cessation of live-vaccine use and a global switch to an inactivated poliovirus vaccine (IPV) by 2020 (12, 13). Yet the inactivated vaccine has serious limitations of its own, the most important of which are inadequate induction of the mucosal immune response and a high cost. The original IPV, developed by Jonas Salk in the 1950s, is based on formalin-inactivated wt viruses. Thus, the production of such a vaccine requires the handling of large quantities of pathogenic viruses, which significantly inflates the cost of the final product due to strict biosecurity measures, making it unaffordable for low-income nations. Attempts to replace the original strains in the vaccine formulation with less-pathogenic strains have encountered mixed success, largely due to the instability of the epitopes required for the induction of neutralizing antibodies during the long inactivation process (14). Recently, virus-like particles (VLPs) have been proposed as an alternative to vaccines based on the inactivation of infectious virions. Poliovirus is a nonenveloped virus, and its capsid proteins are produced by the processing of the capsid protein precursor P1 by the viral protease 3CD (15). Coexpression of P1 and 3CD in different systems has been shown to efficiently generate VLPs, which can induce a protective antibody response (16–20). While VLP-based vaccines eliminate biosafety concerns, since live polioviruses are not involved at any stage of production, the traditional approach based on administration of purified VLPs does not seem to be practical in the case of poliovirus. Poliovirus VLPs are unstable and easily convert from a protective D-antigen to an inactivated C- or H-antigen conformation, which does not induce neutralizing antibodies (21). Even if the antigenic stability of VLPs can be increased by introducing mutations into the capsid protein sequence (22), purified VLPs are incapable of inducing a mucosal immune response, just like the original IPV, and scaling up the experimental systems of VLP production and purification to the industrial level may represent a formidable challenge.
Here we present a novel design for an antipoliovirus vaccine that combines the benefits of a live vaccination approach with the absolute safety of VLPs. The main idea is to express poliovirus VLPs in the organisms of vaccine recipients by use of a viral vector with mucosal tropism. Such a system does not require purification and stabilization of labile VLPs, and the VLPs are presented to the immune system in the context of active viral replication, which serves as a natural adjuvant and promotes the development of strong mucosal and systemic immune responses. We introduced sequences coding for the poliovirus capsid protein precursor P1 and for protease 3CD, which is necessary for P1 processing, into the genome of a nonpathogenic strain of Newcastle disease virus (NDV), an avian single-strand negative-sense RNA virus. NDV is a member of the Avulavirus genus of the family Paramyxoviridae, and its genome contains six genes encoding seven proteins (23). The viral genes are transcribed as independent units, allowing simple construction of expression modules for foreign sequences. NDV has been demonstrated to be a promising vaccine vector for many human and veterinary pathogens. There is no preexisting immunity to NDV in the human population, and its replication in human hosts is safe and self-limiting (24, 25). NDV is easily administered via the nasal and oral routes and has been shown to elicit strong systemic and mucosal immune responses, including gut mucosal immunity in murine and nonhuman primate models (26–31).
Cells infected with the recombinant NDV expressed poliovirus capsid proteins at a level comparable to or higher than that observed in poliovirus-infected cells, and these proteins efficiently assembled into VLPs with the antigenic properties of infectious virions. Intranasal immunization of guinea pigs induced strong neutralizing and mucosal antipoliovirus antibody responses. Importantly, the recombinant vector replicated to high titers and was stable for at least 10 passages in embryonated chicken eggs, an established vaccine production system. Taken together, our data validate a novel approach to the design of a superior antipoliovirus vaccine, which can be adopted with minimal modifications to combat other picornavirus infections.
RESULTS
Construction of an NDV vector expressing poliovirus proteins.
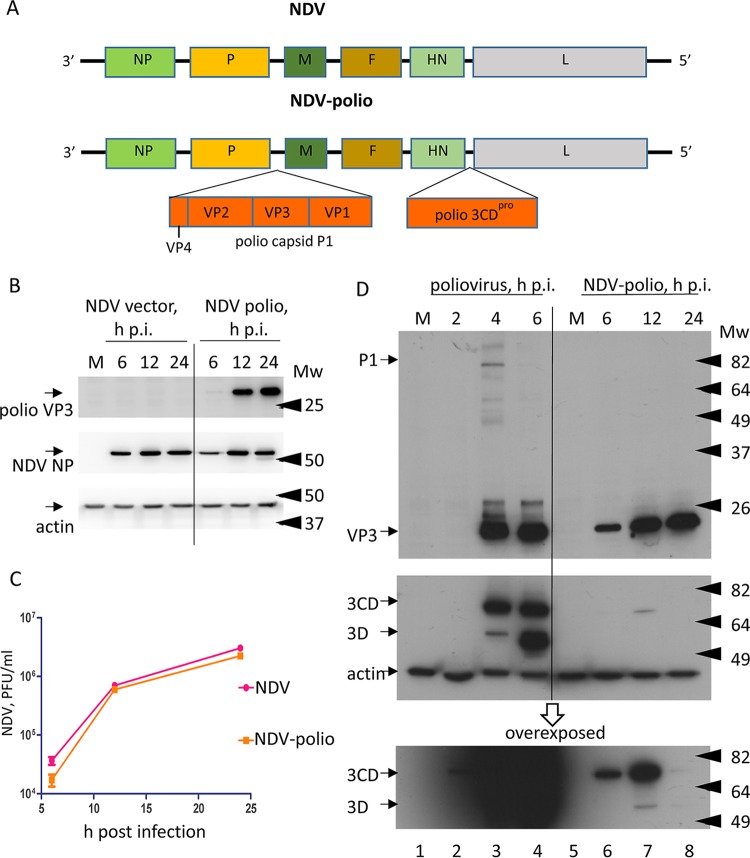
The NDV genome contains six genes in the order 3′-NP-P-M-F-HN-L-5′ (Fig. 1A). The transcription of each gene is controlled by start and stop signals so that the viral RNA-dependent RNA polymerase performs consecutive transcription initiation-termination cycles moving from the 3′ end of the genome. Since reinitiation efficiency is not absolute, this strategy results in a transcription gradient where the genes located closer to the 3′ end of the genome are expressed at a higher level than those closer to the 5′ end. We introduced the sequence coding for the poliovirus type 1 Mahoney capsid protein precursor P1 between the P and M genes, and the sequence coding for poliovirus protease 3CD between the HN and L genes, of the nonpathogenic LaSota strain of NDV (Fig. 1A). Both poliovirus inserts were engineered to be flanked by NDV transcription start and stop signals. This design was chosen to provide a high level of expression of the structural protein precursor P1 and a relatively low level of expression of 3CD protease, minimizing its possible toxic effect on cellular metabolism (32). Recombinant NDV was successfully rescued and demonstrated growth properties similar to those of the original virus without poliovirus inserts (Fig. 1B and C). To characterize the level of poliovirus protein expression, HeLa cells were infected with 10 PFU/cell of the recombinant NDV with poliovirus inserts (NDV-polio), and the lysates were collected at 6, 12, and 24 h postinfection (p.i.). By 24 h p.i., an NDV-induced cytopathic effect (CPE) became prominent, and the cells began to die extensively. For comparison, we used lysates from HeLa cells infected with 10 PFU/cell of poliovirus type 1 Mahoney, collected at 2, 4, and 6 h p.i.; by 6 h, the replication of poliovirus in HeLa cells is complete. The amounts of VP3 and 3CD produced by recombinant NDV reached their maximum levels by 12 h p.i. Interestingly, the level of the capsid protein remained the same in the sample collected at 24 h p.i., while that of 3CD decreased significantly, so that only traces of the protein could be detected at 24 h p.i. (Fig. 1D, NDV-polio). This peculiar pattern may reflect the position of the 3CD gene close to the 5′ end of the genome, so that the regulation of 3CD expression may be similar to that for its neighboring L gene, encoding a viral RNA-dependent RNA polymerase. It is likely that expression of the polymerase is inhibited toward the end of infection. The pattern may also be due to different stabilities of structural poliovirus proteins assembled into stable VLPs and the 3CD protein. The level of 3CD expression from recombinant NDV was much lower than that in poliovirus-infected cells, as predicted from the design of the recombinant construct (Fig. 1D, 3CD panels). Interestingly, this lower level of 3CD was sufficient for complete processing of P1 in NDV-polio-infected cells even at the earliest time point sampled, while in poliovirus-infected samples, the unprocessed P1 precursor and numerous cleavage products could be detected in spite of a much higher level of 3CD expression (Fig. 1D). Thus, the poliovirus capsid precursor P1 and protease 3CD can be efficiently coexpressed as separate genes from a recombinant NDV vector, resulting in robust processing of P1 into individual capsid proteins.
FIG 1.
Recombinant NDV efficiently expresses poliovirus proteins. (A) Schemes of the wt NDV negative-strand RNA genome and the recombinant virus with poliovirus inserts. (B) Western blots showing expression of the NDV protein NP and the poliovirus protein VP3 from the original NDV vector and NDV-polio. M, mock infection; Mw, molecular weight (in KDa). (C) Time course of replication of the original NDV vector and NDV-polio. (D) (Top) Western blots showing expression of the poliovirus capsid protein VP3 in cells infected with poliovirus (lanes 1 to 4) or recombinant NDV-polio (lanes 5 to 8) at the indicated times postinfection. (Center) The same membrane was probed with antibodies against poliovirus 3D which also recognize 3CD. Actin was used as a loading control. (Bottom) The same Western blot as in the center panel after longer exposure to enable better visualization of 3CD expression in cells infected with the recombinant virus NDV-polio.
Poliovirus capsid proteins expressed by recombinant NDV are fully functional and assemble into VLPs.
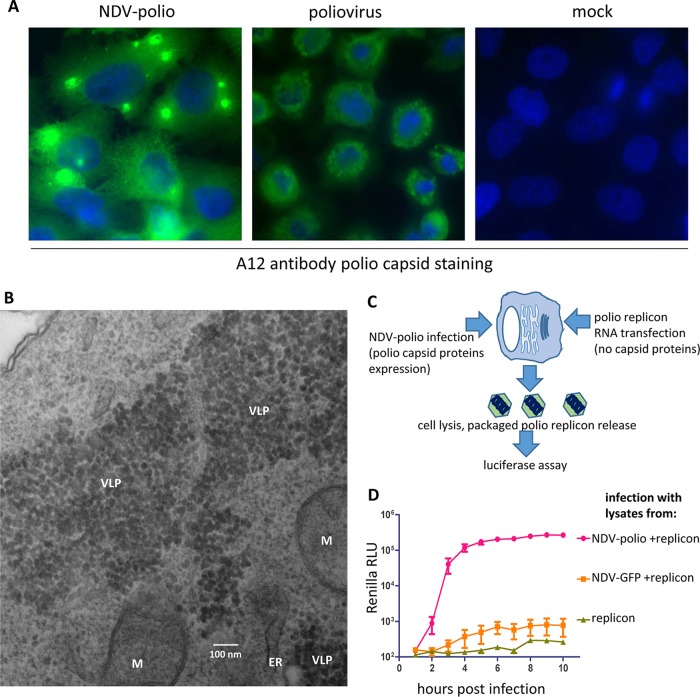
To see if poliovirus capsid proteins assemble into VLPs, we performed immunofluorescent assays of NDV-polio-infected cells with monoclonal antibody A12, which recognizes a conformational epitope present only in fully assembled poliovirus capsids (33, 34). HeLa cells infected with NDV-polio were fixed at 12 h p.i.; for a control, we used poliovirus-infected HeLa cells fixed at 6 h p.i. Cells infected with recombinant NDV-polio demonstrated a massive A12-specific signal, indicating strong accumulation of the relevant poliovirus antigen (Fig. 2A). While in control poliovirus-infected cells the capsid signal was localized in perinuclear rings, typical for the localization of replication complexes, in recombinant-NDV-infected cells the staining was more diffuse, occupying the whole cell volume, and was often highly concentrated in several spots per cell (Fig. 2A). Electron microscopy (EM) examination of cells infected with NDV-polio revealed large clusters of poliovirus VLPs in the cytoplasm, which likely correspond to the bright spots detected in the immunofluorescence assay (Fig. 2B).
FIG 2.
Poliovirus VLPs are efficiently produced in cells infected with the recombinant virus NDV-polio. (A) Immunofluorescent staining using monoclonal antibody A12, recognizing a conformational epitope in the fully formed poliovirus capsid in cells infected with the recombinant virus NDV-polio (left) or poliovirus (center) and in mock-infected cells (right). Nuclei were visualized with the DNA stain Hoechst 33342. (B) Transmission EM image of a HeLa cell infected with NDV-polio. M, mitochondrion; ER, endoplasmic reticulum. (C) Scheme of the poliovirus replicon trans-encapsidation experiment using capsid proteins expressed from the recombinant virus NDV-polio. (D) Renilla luciferase kinetics curves showing strong poliovirus replication only in samples treated with lysates of cells infected with NDV-polio and transfected with poliovirus replicon RNA, confirming effective trans-encapsidation of the replicon RNA by poliovirus capsid proteins expressed from the recombinant virus NDV-polio.
To observe if poliovirus capsid proteins expressed from recombinant NDV could form functional poliovirus capsids, we performed a trans-encapsidation assay of poliovirus replicon RNA. Poliovirus capsid proteins, encoded in the 5′ end of the genome RNA, are dispensable for RNA replication. The capsid protein coding sequence can be replaced with a reporter protein gene so that such an RNA will be fully functional in replication but incapable of forming infectious virions, unless functional capsid proteins are provided in trans (35). We infected HeLa cells with 10 PFU/cell of NDV-polio and transfected them with a poliovirus replicon RNA with the Renilla luciferase gene in place of the capsid coding sequence (36). In control samples, the cells were infected with NDV-GFP, a recombinant NDV expressing green fluorescent protein instead of poliovirus inserts, or were transfected with the poliovirus replicon RNA alone. About 20 h after transfection with the poliovirus replicon RNA, the cells were freeze-thawed three times to release any packaged replicon (Fig. 2B). To assess the presence of a packaged replicon, these lysates were used to infect HeLa cell monolayers, and the Renilla luciferase signal was monitored over 12 h. The strong replication signal confirmed that infectious virions containing poliovirus replicon RNA were efficiently formed in cells infected with NDV-polio and transfected with replicon RNA (Fig. 2D). Collectively, these data demonstrate that coexpression of the poliovirus capsid protein precursor P1 and protease 3CD from a recombinant NDV vector produces a high level of poliovirus VLPs with the antigenic properties of fully functional virions.
Propagation and stability of recombinant NDV in embryonated chicken eggs.
An important characteristic of a recombinant vaccine vector is the ability to retain the foreign insert(s) over multiple replication cycles. To determine the stability profile of the NDV-polio construct, we first plaque-purified 10 individual clones of NDV-polio and individually passaged clone 1 and a mixture of all 10 clones 10 times in embryonated eggs. To assess the percentage of viruses expressing poliovirus VLPs, HeLa cells were infected at a low multiplicity of infection (MOI) of ∼0.5 PFU/cell with the viruses from passages 1 and 10, so that the individually infected cells would be clearly separated from each other. The nonpathogenic LaSota strain of NDV, which was used as a backbone for the recombinant construct, cannot form infectious virions in the absence of exogenously added proteases and can spread only to cells in direct contact with the originally infected cell, producing foci of a few adjacent infected cells. The next day, the cells were fixed and were double stained with antibodies specific for an NDV antigen and antibody A12, recognizing a conformational epitope in the poliovirus capsid (Fig. 3A). In cells infected with either individual clone 1 or pooled clones, expression of poliovirus capsid proteins was detected in ∼95% of NDV-positive cells, and this percentage remained essentially the same after 10 passages (Fig. 3B). We also compared the expression of poliovirus capsid protein VP3 by Western blot analysis of HeLa cells infected with individual clone 1 or pooled clones passaged once or 10 times in embryonated eggs. The level of VP3 expression did not change significantly, nor did we observe any other VP3-positive bands that might indicate possible rearrangements/deletions within the poliovirus inserts (Fig. 3C). Finally, to characterize possible mutations upon serial passages, the viral RNA isolated from the pooled material at passages 2 and 11 (we performed additional passages for the propagation of a sufficient amount of material for RNA isolation) was subjected to next-generation sequencing (NGS). Analysis of NGS data with the HIVE software package (37) did not reveal any significant accumulation of point mutations or viral genomes with deletions/rearrangements of the poliovirus inserts, in agreement with the findings of the biochemical and cytological assays.
FIG 3.
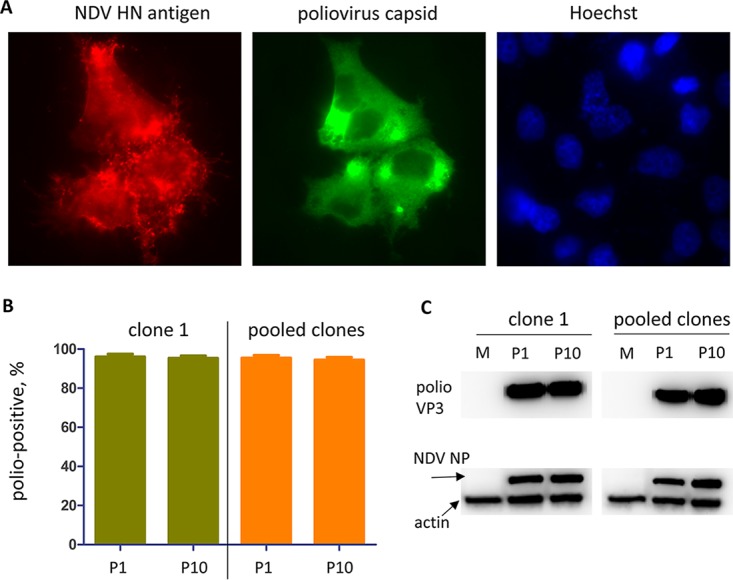
The recombinant virus NDV-polio is stable upon propagation in embryonated eggs. (A) Double immunostaining of NDV-polio-infected cells with a mouse monoclonal antibody recognizing an NDV antigen, HN, and the chimpanzee-human hybrid monoclonal antibody A12, recognizing a conformational epitope in the fully assembled poliovirus capsid. Nuclei are visualized with the DNA stain Hoechst 33342. (B) Quantitation of double-positive cells as shown in panel A, indicative of accumulation of correctly assembled poliovirus capsids in cells infected with the recombinant virus NDV-polio propagated for 10 passages in embryonated chicken eggs. Several fields containing at least 100 cells together were quantified. P, passage. (C) Western blots of lysates from HeLa cells infected at an MOI of 10 PFU/cell with the recombinant virus NDV-polio propagated for 1 or 10 passages in embryonated chicken eggs. Expression of the poliovirus capsid protein VP3 and the NDV protein NP is shown. M, mock infection. Actin was used as a loading control.
These data show that the recombinant NDV-polio construct is highly stable upon propagation in embryonated chicken eggs, an established and economically attractive system of vaccine production.
Intranasal administration of NDV-polio induces neutralizing and mucosal antipoliovirus antibodies in guinea pigs.
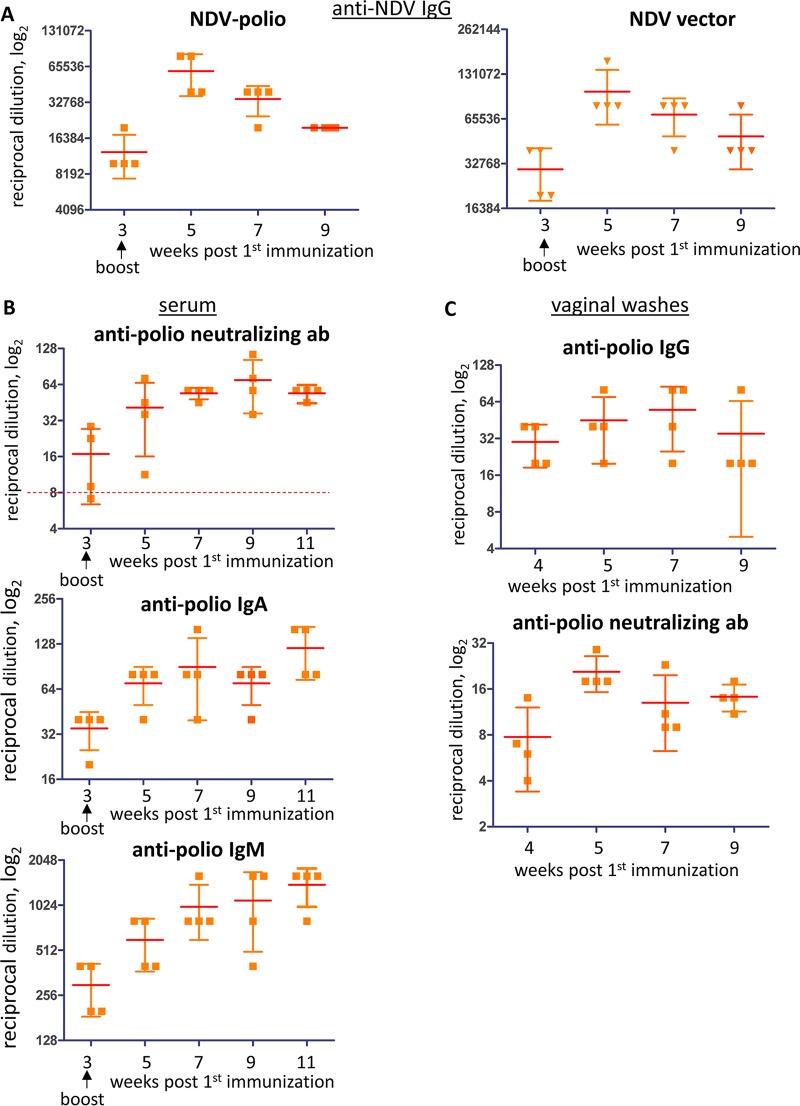
To evaluate the efficacy of antipoliovirus vaccination with the NDV-polio construct, we performed intranasal immunization of guinea pigs. Previous research indicates that the immune response of guinea pigs to NDV vector-based vaccines resembles that observed in primate models (31, 38, 39). Four animals in each group were immunized with either NDV-polio or the NDV vector without poliovirus inserts. Booster immunization was performed 3 weeks after the first immunization, and both blood serum and vaginal wash samples were collected before immunization and at weeks 3, 4, 5, 7, 9, and 11 postimmunization. The animals did not show any adverse effects associated with immunization, as was observed previously even for multiple cycles of administration of NDV-based vaccines (40). Replication of NDV was confirmed in all animals, as evidenced by the development of a serum anti-NDV IgG response. The levels and the dynamics of accumulation of anti-NDV antibodies were similar in all animals, with a clear boost after the second immunization, indicating that NDV with poliovirus inserts is not compromised relative to the parental virus in vivo (Fig. 4A).
FIG 4.
Intranasal immunization with the recombinant virus NDV-polio induces systemic and mucosal antipoliovirus responses. (A) Development of an anti-NDV IgG response upon intranasal immunization of guinea pigs with either the recombinant virus NDV-polio or NDV strain LaSota without poliovirus inserts. (B) Development of an antipoliovirus neutralizing antibody (ab) response or antipoliovirus IgM and IgA in guinea pigs immunized intranasally with the recombinant virus NDV-polio. Titers are expressed as reciprocals of serum dilutions, shown on a log2 scale. The dashed red line in the neutralizing-antibody graph indicates a 1:8 serum titer, considered sufficient for antipoliovirus protection. (C) Development of antipoliovirus IgG and neutralizing antibodies in vaginal wash samples of guinea pigs immunized with the recombinant virus NDV-polio. Titers are expressed as reciprocals of serum dilutions, shown on a log2 scale.
To assess the level of neutralizing antipoliovirus antibodies, we performed a microneutralization assay, which is a standard tool for evaluation of the efficacy of antipoliovirus vaccination. All the animals immunized with NDV-polio showed the development of a neutralizing antibody response. One serum sample collected at week 3, before the booster immunization, showed a level of neutralizing antibodies slightly below the 1:8 threshold, which is generally accepted as sufficient for protection against poliomyelitis (41). Nevertheless, the levels of neutralizing antibodies in samples collected at week 7 and later were well above the protective threshold in all the animals (Fig. 4B, top). The highest serum dilutions exhibiting neutralizing activities ranged from ∼1:35 to ∼1:100 in different animals and remained relatively stable at least until week 11 postimmunization (Fig. 4B, top).
To evaluate the development of a mucosal immune response, we first measured the levels of IgM and IgA antibodies in the sera of immunized animals. IgM is the first antibody class to appear during the development of an immune response and also contributes to mucosal immunity, and IgA is the main antibody class expressed on mucosal surfaces (42). The presence of IgM and IgA in serum has been shown to correlate with mucosal immune responses, including that in the gut in many systems (43–45). The serum was assessed for the presence of antibodies capable of binding poliovirus type 1 virions from a standard IPV preparation bound to a nitrocellulose membrane. Samples from animals immunized with NDV-polio showed steady accumulation of antipoliovirus IgM and IgA, which reached a peak at 7 weeks postimmunization and stayed relatively stable after that (Fig. 4B, center and bottom). As expected, no neutralizing or mucosal antipoliovirus antibody response was detected in the control group immunized with NDV without poliovirus inserts.
To assess the development of a bona fide mucosal antipoliovirus response, we evaluated the levels of poliovirus-specific antibodies in vaginal wash samples. For correct comparison, the protein concentrations in vaginal wash samples collected at different time points and from different animals were adjusted to the same level with phosphate-buffered saline (PBS) before titration. Some vaginal wash samples contained very little protein, likely because of an estrous cycle stage (46), and were excluded from the analysis. Since anti-guinea pig IgA, used as a conjugated secondary antibody, gave a very high background with vaginal wash samples, we assessed the levels of secreted antipoliovirus IgG; these antibodies are among the most abundant in urogenital tract secretions (42). They peaked in samples collected at weeks 4 and 5 postimmunization and decreased significantly in samples from all but one animal by week 9 (Fig. 4C). In a microneutralization assay, antipoliovirus neutralizing activity was detected in vaginal wash samples from all animals immunized with NDV-polio, but not from the control group immunized with NDV without poliovirus inserts. Levels of antipoliovirus neutralizing antibodies peaked at week 5 and remained relatively stable up to week 9 (Fig. 4C). Thus, intranasal immunization with the recombinant virus NDV-polio induces robust protective antipoliovirus systemic and mucosal responses.
DISCUSSION
The endgame strategy for poliovirus eradication calls for cessation of the use of live poliovirus vaccine in the year 2020, and the development of a vaccine that can substitute for it on a global scale is a high priority. Currently, two major approaches are being pursued. One is the development of an inactivated vaccine based on nonpathogenic poliovirus strains; the other, more ambitious, is focused on making purified VLP-based vaccines, which would not include a poliovirus propagation step at any stage of production. While both approaches address the safety concerns that drive up the cost of manufacturing the original IPV, which relies on the propagation of large quantities of pathogenic poliovirus strains, they both include tedious purification processes and face significant problems of stabilizing labile poliovirus epitopes required for the induction of protective neutralizing antibodies (22, 47, 48). Moreover, the nonreplicating vaccines are deficient in the induction of the mucosal immune response, which is critical for the interruption of poliovirus transmission. Recently, extensive circulation of wt polioviruses has been documented in Israel, in spite of almost complete vaccination coverage with IPV (49). To stop virus transmission, a mass vaccination campaign using live poliovirus vaccine had to be reimplemented, effectively reversing the poliovirus eradication strategy (50). It is likely that such undetected transmission of polioviruses would represent a constant threat of virus reemergence in a posteradication world, since surveillance based on cases of acute flaccid paralysis inevitably misses most transmission events, and global environmental surveillance is unrealistic. Yet, in this case, the option of stopping transmission by vaccination with live poliovirus vaccine will not be available.
In this study, we investigated an alternative approach to designing a safe and effective antipoliovirus vaccine. We introduced sequences coding for the poliovirus capsid protein precursor P1 and protease 3CD, required for its processing, into the genome of NDV, a negative-strand RNA virus with mucosal tropism. We reasoned that such an approach would address the major hurdles in the development of a next-generation antipoliovirus vaccine. First, the vectored vaccine is absolutely safe in terms of reintroduction of poliovirus in the environment, since the construct contains only fragments of the poliovirus genome and is in principle incapable of recombination with circulating enteroviruses. Second, poliovirus proteins are expressed and assemble into VLPs in vivo, upon replication of the recombinant virus, thus eliminating the problem of the isolation and stabilization of labile VLPs. Indeed, our data show that poliovirus capsid proteins produced in NDV-polio-infected cells assemble into VLPs with the antigenic structure of poliovirus virions. They were recognized by antibody A12, which binds a conformational epitope present only in functional virions (33, 34); they were able to trans-encapsidate a replicon RNA into functional virions; and most importantly, they were capable of inducing a neutralizing antibody response (see below). Furthermore, poliovirus VLPs are presented to the immune system in the context of active NDV replication on mucosal surfaces, serving as a natural adjuvant and stimulating the development of both systemic and mucosal immune responses. Finally, NDV-based vaccines are delivered via intranasal spray, thus retaining one of the major advantages of live poliovirus vaccine, which is administered orally by personnel without medical training.
Our data demonstrate robust development of neutralizing antipoliovirus antibodies upon two intranasal immunizations of guinea pigs. We chose guinea pigs as a model for the evaluation of this vaccine rather than mice expressing poliovirus receptor for several reasons. While mice expressing poliovirus receptor are available, they are susceptible to oral poliovirus infection, necessary for evaluation of the development of gut mucosal immunity, only in the background of alpha/beta interferon receptor knockout; thus, their immune response to vaccination cannot be informative (51). Mice expressing poliovirus receptor in the wt background can be infected with poliovirus only via intramuscular inoculation, intraperitoneal inoculation, or direct inoculation into the central nervous system and essentially allow measurement of neutralizing antibody in the serum, a parameter that can be quantitatively assessed in the microneutralization assay (52). Guinea pigs, on the other hand, due to their larger size, allow better control of intranasal vaccine delivery and the collection of larger blood samples, necessary for thorough evaluation of the immune response. Moreover, the immune response of guinea pigs to immunization with NDV-based vaccines has been shown previously to better recapitulate that observed in primate models and to include a strong mucosal component (26–31). Due to the limitations of the guinea pig model, it was impossible to test if our vaccine is capable of inducing gut immunity sufficient to interrupt poliovirus transmission. However, we observed accumulation of antipoliovirus IgM and IgA antibodies in the blood serum, as well as antipoliovirus neutralizing and specific IgG antibodies in vaginal wash samples, strongly indicative of the development of a protective mucosal immune response (45). The mucosal membranes in the body are involved in constant immunological communication and, in many cases, may be considered a unified immunological site (53). Indeed, recent research indicates that intranasal administration of different antigens can elicit gut mucosal immunity, including the development of a protective response against human Norwalk virus, an enteric pathogen with a life cycle similar to that of poliovirus (54–57). Further analysis of the performance of the vectored antipoliovirus vaccine in primates is necessary in order to fully evaluate its potential.
Is NDV the best backbone for an antipoliovirus vaccine? Two considerations are very important for the development of a live vectored vaccine. First, the preexisting immunity to the vector should not interfere with vaccine performance. Second, not only should the vector itself be safe for vaccine recipients, but there should be no safety concern in case of its inevitable release into the environment. Humans generally do not have preexisting immunity to NDV, although sporadic cases of NDV infections have been described in poultry industry workers or people handling infected birds. The infections were quickly self-resolving; they either were asymptomatic or manifested as mild conjunctivitis or laryngitis; and no cases of human-to-human transmission have been observed (58–60). Moreover, NDV has been explored as an oncolytic virus and demonstrated an excellent safety profile in clinical trials, even when high doses of the virus were administered intravenously to individuals with compromised immune systems (30). NDV and related viruses infect a broad spectrum of bird species, and pathogenic strains of NDV can cause devastating epizootics in poultry. In this study, we utilized the nonpathogenic LaSota strain of NDV, which is broadly used as a live vaccine in the poultry industry and has never been documented to develop a pathogenic phenotype (61, 62). Thus, production and administration of a vectored vaccine based on the LaSota backbone should not raise any safety concerns. Importantly, the virus replicates to high titers in embryonated chicken eggs, an established system, and one of the most effective, for vaccine production.
An important property of the viruses of the order Mononegavirales, which includes NDV, is the virtual nonexistence of recombination, leading to much higher genome stability than that of other groups of RNA viruses (63, 64). Indeed, in our analysis of the stability of the poliovirus inserts upon the propagation of plaque-purified NDV-polio, we did not observe any significant changes in poliovirus protein expression, nor did NGS analysis of the viral RNA reveal any accumulation of mutations during at least 10 passages in embryonated eggs. It should be noted that each passage in eggs entails multiple cycles of viral replication. Anyway, the production of modern vaccines employs a seed virus system that only allows a manufacturing process involving one or two passages from the seed virus stock. Therefore, the stability of a vectored NDV-based antipoliovirus vaccine should be sufficient for industrial propagation.
To develop vaccine candidates covering all three poliovirus serotypes, it may be necessary to explore the possibility of using other, antigenically distinct avian paramyxovirus (APMV) types as backbones for the expression of poliovirus VLPs of different serotypes. This will allow the administration of vaccines against all three serotypes of poliovirus in different combinations, or in any temporal succession, so that one vectored vaccine does not interfere with the performance of the other. The advantage of APMVs as vectors is that there are at least 15 APMV types with properties similar to those of NDV (APMV type 1) that are not pathogenic to poultry and can be explored as backbones for vectored vaccines (65, 66). Even though the current construct expressed poliovirus proteins to levels similar to those observed in poliovirus-infected cells, it is realistic to increase it even further. One approach is to optimize the translation initiation capacity of the RNA coding for the poliovirus capsid protein precursor; another is to place the poliovirus capsid insert closer to the 3′ end of the NDV genome, between the N and P genes of NDV, to increase the level of transcription. Collectively, these data indicate that NDV is a highly promising vector for the development of a safe, effective, and affordable antipoliovirus vaccine.
Probably the major hurdle facing any new antipoliovirus vaccine that significantly deviates from the established OPV or IPV designs is regulatory approval. The current high level of immunization coverage with conventional antipoliovirus vaccines and the low incidence of the disease make clinical trials of vaccine efficacy challenging. Still, correlates of protection, such as the induction (boost) of neutralizing and/or mucosal antibodies, can be used to evaluate vaccine potential. The recent rapid deployment and success of a vesicular stomatitis virus (VSV)-based vectored vaccine against Ebola virus demonstrates that such an approach to vaccine evaluation is warranted and proves the clinical relevance of a vectored vaccine with a design similar to that described in this study (67, 68). Collectively, our data demonstrate that an NDV-based antipoliovirus vaccine combines important benefits of IPV and OPV without their inherent drawbacks, which may be critical for the final phase of the poliovirus eradication campaign, and especially for a postpolio world.
MATERIALS AND METHODS
Cells and viruses.
The human cervical carcinoma cell line HeLa was received from the laboratory of E. Ehrenfeld, NIH; the HeLa derivative cell line HEp-2 and the DF-1 chicken embryo fibroblast cell line were from the ATCC. HeLa cells were maintained in high-glucose Dulbecco's modified Eagle medium (DMEM) supplemented with pyruvate and 10% fetal bovine serum (FBS). HEp-2 cells were grown in MEM supplemented with 10% FBS. DF-1 cells were maintained in DMEM supplemented with 10% FBS. Poliovirus type 1 Mahoney was propagated in HeLa cells, and the viral titer was either determined by a plaque assay and expressed as PFU per milliliter (for experiments where expression of poliovirus proteins was assessed) or determined by the terminal dilution method and expressed as 50% tissue culture infective doses per milliliter, calculated by Kärber's formula (69) for the assessment of neutralizing antibodies. Recombinant Newcastle disease virus (NDV) was rescued using a reverse genetics system as described in references 70 and 71, with minor modifications. Briefly, HEp-2 cells were infected with vaccinia virus expressing T7 RNA polymerase and were transfected using the Mirus 2020 transfection reagent with three plasmids coding for the NDV NP, P, and L genes (polymerase complex), as well as the plasmid coding for the full-length NDV genome with the poliovirus inserts, under the control of the T7 promoter. The cells were incubated in MEM supplemented with 10% fresh allantoic fluid for 2 days posttransfection. After that, the cells were subjected to three cycles of freeze-thawing, and the medium was collected, clarified from the cellular debris by low-speed centrifugation, and used to inoculate the allantoic cavities of 9-day-old chicken embryos. After 48 h, allantoic fluid was collected and tested for the presence of hemagglutinating (HA) activity, indicative of NDV propagation. The virus titer was determined by a plaque assay on DF-1 cells overlaid with methylcellulose-solidified growth medium supplemented with 10% fresh allantoic fluid for 3 days.
Plasmids.
The pLaSota plasmid, carrying the full-length cDNA of the LaSota strain of NDV, and the plasmids carrying the LaSota N, P, and L polymerase complex genes under the control of the T7 promoter are described in reference 71. Plasmid pXpA, carrying the full-length cDNA of poliovirus type 1 Mahoney, is described in reference 72. Plasmid pNDV-polio was constructed by inserting PCR-amplified fragments coding for the poliovirus capsid protein precursor P1 and protease 3CD into the PmeI site located between the P and M genes and the SnaBI site located between the HN and L genes of the LaSota sequence, respectively. The poliovirus P1 and 3CD inserts were designed to be flanked with transcription initiation and termination signals for LaSota polymerase. The details of primer design and other cloning considerations are available upon request.
Antibodies.
The mouse monoclonal antibody against poliovirus VP3 was a gift from Kurt Benz; rabbit polyclonal antibodies against poliovirus 3D are described in reference 73; and the humanized antibody A12 against the poliovirus capsid conformation epitope is described in references 33 and 34. Rabbit polyclonal antibodies against NDV NP protein have been described previously (74), and mouse monoclonal antibodies against NDV HN were a kind gift from Shin-Hee Kim (University of Maryland). An anti-actin mouse monoclonal antibody conjugated with horseradish peroxidase (HRP) was obtained from Sigma-Aldrich. Secondary antibodies conjugated with Alexa fluorescent dyes were from Molecular Probes. HRP-conjugated rabbit anti-guinea pig IgM, goat anti-guinea pig IgG, and sheep anti-guinea pig IgA antibodies were from Bioss, Invitrogen, and ICL, respectively.
Immunofluorescence assay.
For immunofluorescence, cells grown on a coverslip were fixed with 4% formaldehyde in PBS for 20 min, washed with PBS, and permeabilized with 0.2% Triton X-100 for 5 min. Primary and secondary antibodies were diluted in PBS with 3% ECL blocking reagent (Amersham), and the same solution was used for blocking nonspecific antibody binding sites. Images were taken with a Zeiss Axiovert 200M epifluorescence microscope equipped with a digital camera. Digital images were processed using Adobe Photoshop software, and the same parameters were applied to the whole image area.
Poliovirus replicon replication assay.
The poliovirus replicon replication assay was performed essentially as described previously (75), except that instead of being transfected with replicon RNA, HeLa cells were infected with replicon RNA trans-encapsidated in poliovirus capsid proteins expressed during the replication of the recombinant virus NDV-polio. Briefly, HeLa cells grown in a 96-well plate were incubated with lysates of cells from the trans-encapsidation experiment for 1 h, washed, and incubated in a growth medium supplemented with 30 μM EnduRen (Promega), a cell-permeant Renilla luciferase substrate. Measurements of Renilla luciferase activity, indicative of poliovirus RNA replication, were performed automatically every hour using a Tecan M1000 plate reader.
Next-generation sequencing.
NDV-polio propagated in embryonated chicken eggs was purified from allantoic fluid by centrifugation through a 30% sucrose cushion in PBS at 75,000 × g for 2.5 h. The viral RNA was isolated with a QiaAmp viral RNA isolation kit (Qiagen) using a protocol without carrier RNA. To prepare a 250-nucleotide (nt) DNA library for Illumina sequencing, 0.5 μg of total RNA was fragmented using a Focused-ultrasonicator (Covaris) to generate fragments of 300 to 500 nt. The DNA libraries from the RNA fragments were prepared using the NEBNext mRNA Library Prep master mix set for Illumina (New England BioLabs) according to the manufacturer's protocol. Briefly, the fragmented RNA was reverse transcribed, and the DNA second strand was synthesized. The resulting DNA fragments were first ligated to Illumina paired-end (PE) adaptors, then amplified using 12 cycles of PCR with multiplex indexed primers, and finally purified by magnetic beads (Agencourt AMPure PCR purification system; Beckman Coulter). After analysis of the DNA libraries for size and quality (BioAnalyzer; Agilent Technologies, Inc.), deep sequencing was performed using MiSeq (Illumina) producing 250-nt PE reads. The raw sequencing reads were analyzed by the HIVE software package (37).
Immunization of guinea pigs.
All animals were handled in accordance with established guidelines, and the procedures were performed according to the University of Maryland Institutional Animal Care and Use Committee (IACUC)-approved protocol. Five-week-old female Hartley guinea pigs were divided into 2 groups of 4 animals each, which were immunized with 10E5 PFU of either the recombinant virus NDV-polio or vector NDV without poliovirus inserts. The allantoic fluid collected from 1 egg provides ∼500 to ∼1,000 such immunization doses. For immunization, allantoic fluid diluted in PBS was administered intranasally (100 μl/nostril). Boost immunization was performed similarly at 3 weeks after the first immunization. Blood from the thoracic vein was collected at weeks 0 (prebleed), 3 (before the boost immunization), 5, 7, 9, and 11. Vaginal wash samples were collected at the same time as the blood samples. Animal-feeding needles (Fisher Scientific) were used to flush the vaginal cavity 4 to 6 times with 100 μl of PBS containing protease inhibitor cocktail (Sigma). Vaginal wash samples were clarified by centrifugation at 10,000 rpm for 15 min in a minicentrifuge to remove cellular debris, and supernatants were collected and stored at −70°C. Prior to the antibody assay and microneutralization test, the protein concentrations of vaginal wash samples were determined by the Bradford protocol (76). Samples with protein concentrations lower than 0.4 μg/μl were excluded from the analysis.
Poliovirus microneutralization assay.
Titers of antipoliovirus neutralizing antibodies in serum and vaginal wash samples of immunized guinea pigs were determined using a microneutralization assay in a 96-well plate format (77). Briefly, heat-inactivated serum, or vaginal wash samples adjusted to the same protein concentration with PBS, and poliovirus type 1 Mahoney were diluted in DMEM supplemented with 2% FBS. Fifty microliters of serial serum dilutions were incubated with 50 μl of medium containing 100 TCID50 of poliovirus for 3 h, after which 50 μl of a HeLa cell suspension (30,000 cells/well) was added, and the plate was incubated for 4 days in a cell culture incubator. Staining with crystal violet was performed at the end of incubation period to determine virus-induced CPE. All experiments included a virus titration control and a neutralization control with an in-house standard, rabbit antipoliovirus serum.
Anti-NDV IgG assay.
For the assessment of serum anti-NDV IgG antibodies, a commercial NDV antibody test kit from Affinitech was used. Briefly, serial dilutions of sera in PBS were incubated in 96-well plates with preadsorbed NDV antigens. The plates were processed for a colorimetric assay using HRP-linked goat anti-guinea pig IgG antibodies and the reagents provided in the kit with a 2,2′-azinobis(3-ethylbenzthiazoline-6-sulfonic acid) diammonium salt (ABTS) peroxidase substrate solution (Synbiotics Corporation), according to the manufacturer's protocol. The highest serum dilution producing a signal >2 times that of the prebleed control serum is plotted.
Antipoliovirus IgM, IgA, and IgG assays.
For the assessment of antipoliovirus IgM and IgA in serum and antipoliovirus IgG in vaginal wash samples, 10 μl of type 1 inactivated poliovirus vaccine (IPV) (containing formalin-inactivated whole virions) diluted 1:100 in PBS was spotted onto nitrocellulose membrane using a 96-well manifold (Schleicher & Schuell). The nonspecific binding sites were blocked by 1 h of incubation in 2% ECL blocking reagent (Amersham) in Tris-buffered saline supplemented with 0.002% Tween 20 (TBS-T). The same solution was used for serial serum dilutions, for dilutions of vaginal wash samples previously adjusted to the same protein concentration with PBS, and for dilution of secondary anti-guinea pig antibodies conjugated with horseradish peroxidase. The membrane was developed using the ECL Select detection reagent (GE Healthcare), and the signal was recorded using an Azure C300 chemiluminescent reader. The signal was quantified using Image Studio Lite software (Li-Cor). The highest serum dilution producing a signal >2 times that of the prebleed control serum is plotted.
Ethics statement.
Animal protocols were designed according to the Guide for the Care and Use of Laboratory Animals (78). The guinea pig immunization protocol (R-16-57) was approved by the University of Maryland—College Park IACUC (IBC no. 14-12). Hartley guinea pigs and 9-day-old embryonated chicken eggs were purchased from Charles River Laboratories.
Data availability.
NGS data and raw sequencing reads, as analyzed with the HIVE software package (37), are deposited at https://hive.biochemistry.gwu.edu/review/NDV_LaSota_strain_PV.
ACKNOWLEDGMENTS
We are grateful to Raul Andino for his ideas on trans-encapsidation of poliovirus replicon RNA using the NDV-expressed capsid proteins. We are deeply indebted to Ashleigh Palmer for editorial assistance.
The work was supported by NIH grant R21 AI115383.
REFERENCES
- 1.Racaniello VR. 2006. One hundred years of poliovirus pathogenesis. Virology 344:9–16. doi: 10.1016/j.virol.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 2.Cochi SL, Hegg L, Kaur A, Pandak C, Jafari H. 2016. The Global Polio Eradication Initiative: progress, lessons learned, and polio legacy transition planning. Health Affairs 35:277–283. doi: 10.1377/hlthaff.2015.1104. [DOI] [PubMed] [Google Scholar]
- 3.Stern A, Yeh MT, Zinger T, Smith M, Wright C, Ling G, Nielsen R, Macadam A, Andino R. 2017. The evolutionary pathway to virulence of an RNA virus. Cell 169:35–46. doi: 10.1016/j.cell.2017.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dowdle WR, De Gourville E, Kew OM, Pallansch MA, Wood DJ. 2003. Polio eradication: the OPV paradox. Rev Med Virol 13:277–291. doi: 10.1002/rmv.401. [DOI] [PubMed] [Google Scholar]
- 5.Anonymous. 2012. Update on vaccine-derived polioviruses detected worldwide, April 2011–June 2012. Wkly Epidemiol Rec 87:358–368. [PubMed] [Google Scholar]
- 6.Minor P. 2009. Vaccine-derived poliovirus (VDPV): impact on poliomyelitis eradication. Vaccine 27:2649–2652. doi: 10.1016/j.vaccine.2009.02.071. [DOI] [PubMed] [Google Scholar]
- 7.MacLennan C, Dunn G, Huissoon AP, Kumararatne DS, Martin J, O'Leary P, Thompson RA, Osman H, Wood P, Minor P, Wood DJ, Pillay D. 2004. Failure to clear persistent vaccine-derived neurovirulent poliovirus infection in an immunodeficient man. Lancet 363:1509–1513. doi: 10.1016/S0140-6736(04)16150-3. [DOI] [PubMed] [Google Scholar]
- 8.Weil M, Shulman LM, Heiman S, Stauber T, Alfandari J, Weiss L, Silberstein I, Indenbaum V, Mendelson E, Sofer D. 2016. Prolonged excretion of type-2 poliovirus from a primary immune deficient patient during the transition to a type-2 poliovirus-free world, Israel, 2016. Euro Surveill 21:30408. doi: 10.2807/1560-7917.ES.2016.21.47.30408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dunn G, Klapsa D, Wilton T, Stone L, Minor PD, Martin J. 2015. Twenty-eight years of poliovirus replication in an immunodeficient individual: impact on the Global Polio Eradication Initiative. PLoS Pathog 11:e1005114. doi: 10.1371/journal.ppat.1005114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lauring AS, Jones JO, Andino R. 2010. Rationalizing the development of live attenuated virus vaccines. Nat Biotechnol 28:573–579. doi: 10.1038/nbt.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vignuzzi M, Wendt E, Andino R. 2008. Engineering attenuated virus vaccines by controlling replication fidelity. Nat Med 14:154–161. doi: 10.1038/nm1726. [DOI] [PubMed] [Google Scholar]
- 12.Patel M, Cochi S. 2017. Addressing the challenges and opportunities of the polio endgame: lessons for the future. J Infect Dis 216:S1–S8. doi: 10.1093/infdis/jix117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fahmy K, Hampton LM, Langar H, Patel M, Mir T, Soloman C, Hasman A, Yusuf N, Teleb N. 2017. Introduction of inactivated polio vaccine, withdrawal of type 2 oral polio vaccine, and routine immunization strengthening in the Eastern Mediterranean region. J Infect Dis 216:S86–S93. doi: 10.1093/infdis/jix133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sutter RW, Okayasu H, Kieny MP. 2017. Next generation inactivated poliovirus vaccine: the future has arrived. Clin Infect Dis 64:1326–1327. doi: 10.1093/cid/cix116. [DOI] [PubMed] [Google Scholar]
- 15.Ypma-Wong MF, Dewalt PG, Johnson VH, Lamb JG, Semler BL. 1988. Protein 3CD is the major poliovirus proteinase responsible for cleavage of the P1 capsid precursor. Virology 166:265–270. doi: 10.1016/0042-6822(88)90172-9. [DOI] [PubMed] [Google Scholar]
- 16.Hummeler K, Anderson TF, Brown RA. 1962. Identification of poliovirus particles of different antigenicity by specific agglutination as seen in the electron microscope. Virology 16:84–90. doi: 10.1016/0042-6822(62)90205-2. [DOI] [PubMed] [Google Scholar]
- 17.Pfister T, Pasamontes L, Troxler M, Egger D, Bienz K. 1992. Immunocytochemical localization of capsid-related particles in subcellular fractions of poliovirus-infected cells. Virology 188:676–684. doi: 10.1016/0042-6822(92)90522-Q. [DOI] [PubMed] [Google Scholar]
- 18.Ansardi DC, Porter DC, Morrow CD. 1991. Coinfection with recombinant vaccinia viruses expressing poliovirus P1 and P3 proteins results in polyprotein processing and formation of empty capsid structures. J Virol 65:2088–2092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bräutigam S, Snezhkov E, Bishop DH. 1993. Formation of poliovirus-like particles by recombinant baculoviruses expressing the individual VP0, VP3, and VP1 proteins by comparison to particles derived from the expressed poliovirus polyprotein. Virology 192:512–524. doi: 10.1006/viro.1993.1067. [DOI] [PubMed] [Google Scholar]
- 20.Urakawa T, Ferguson M, Minor PD, Cooper J, Sullivan M, Almond JW, Bishop DH. 1989. Synthesis of immunogenic, but non-infectious, poliovirus particles in insect cells by a baculovirus expression vector. J Gen Virol 70(Part 6):1453–1463. doi: 10.1099/0022-1317-70-6-1453. [DOI] [PubMed] [Google Scholar]
- 21.Basavappa R, Syed R, Flore O, Icenogle JP, Filman DJ, Hogle JM. 1994. Role and mechanism of the maturation cleavage of VP0 in poliovirus assembly: structure of the empty capsid assembly intermediate at 2.9 Å resolution. Protein Sci 3:1651–1669. doi: 10.1002/pro.5560031005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fox H, Knowlson S, Minor PD, Macadam AJ. 2017. Genetically thermo-stabilised, immunogenic poliovirus empty capsids; a strategy for non-replicating vaccines. PLoS Pathog 13:e1006117. doi: 10.1371/journal.ppat.1006117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lamb RA, Parks GD. 2007. Paramyxoviridae: the viruses and their replication, p 1449–1496. In Knipe DM, Howley PM, Griffin DE, Lamb RA, Martin MA, Roizman B, Straus SE (ed), Fields virology, 5th ed Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 24.Kim SH, Samal SK. 2016. Newcastle disease virus as a vaccine vector for development of human and veterinary vaccines. Viruses 8:E183. doi: 10.3390/v8070183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Samal SK. 2011. The biology of paramyxoviruses, p 69–114. Caister Academic Press, Norfolk, United Kingdom. [Google Scholar]
- 26.DiNapoli JM, Kotelkin A, Yang L, Elankumaran S, Murphy BR, Samal SK, Collins PL, Bukreyev A. 2007. Newcastle disease virus, a host range-restricted virus, as a vaccine vector for intranasal immunization against emerging pathogens. Proc Natl Acad Sci U S A 104:9788–9793. doi: 10.1073/pnas.0703584104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DiNapoli JM, Yang L, Suguitan A Jr, Elankumaran S, Dorward DW, Murphy BR, Samal SK, Collins PL, Bukreyev A. 2007. Immunization of primates with a Newcastle disease virus-vectored vaccine via the respiratory tract induces a high titer of serum neutralizing antibodies against highly pathogenic avian influenza virus. J Virol 81:11560–11568. doi: 10.1128/JVI.00713-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.DiNapoli JM, Nayak B, Yang L, Finneyfrock BW, Cook A, Andersen H, Torres-Velez F, Murphy BR, Samal SK, Collins PL, Bukreyev A. 2010. Newcastle disease virus-vectored vaccines expressing the hemagglutinin or neuraminidase protein of H5N1 highly pathogenic avian influenza virus protect against virus challenge in monkeys. J Virol 84:1489–1503. doi: 10.1128/JVI.01946-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DiNapoli JM, Yang L, Samal SK, Murphy BR, Collins PL, Bukreyev A. 2010. Respiratory tract immunization of non-human primates with a Newcastle disease virus-vectored vaccine candidate against Ebola virus elicits a neutralizing antibody response. Vaccine 29:17–25. doi: 10.1016/j.vaccine.2010.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Freeman AI, Zakay-Rones Z, Gomori JM, Linetsky E, Rasooly L, Greenbaum E, Rozenman-Yair S, Panet A, Libson E, Irving CS, Galun E, Siegal T. 2006. Phase I/II trial of intravenous NDV-HUJ oncolytic virus in recurrent glioblastoma multiforme. Mol Ther 13:221–228. doi: 10.1016/j.ymthe.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 31.Bukreyev A, Huang ZH, Yang LJ, Elankumaran S, St Claire M, Murphy BR, Samal SK, Collins PL. 2005. Recombinant Newcastle disease virus expressing a foreign viral antigen is attenuated and highly immunogenic in primates. J Virol 79:13275–13284. doi: 10.1128/JVI.79.21.13275-13284.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sharma R, Raychaudhuri S, Dasgupta A. 2004. Nuclear entry of poliovirus protease-polymerase precursor 3CD: implications for host cell transcription shut-off. Virology 320:195–205. doi: 10.1016/j.virol.2003.10.020. [DOI] [PubMed] [Google Scholar]
- 33.Chen ZC, Fischer ER, Kouiavskaia D, Hansen BT, Ludtke SJ, Bidzhieva B, Makiya M, Agulto L, Purcell RH, Chumakov K. 2013. Cross-neutralizing human anti-poliovirus antibodies bind the recognition site for cellular receptor. Proc Natl Acad Sci U S A 110:20242–20247. doi: 10.1073/pnas.1320041110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen ZC, Chumakov K, Dragunsky E, Kouiavskaia D, Makiya M, Neverov A, Rezapkin G, Sebrell A, Purcell R. 2011. Chimpanzee-human monoclonal antibodies for treatment of chronic poliovirus excretors and emergency postexposure prophylaxis. J Virol 85:4354–4362. doi: 10.1128/JVI.02553-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Porter DC, Ansardi DC, Wang J, McPherson S, Moldoveanu Z, Morrow CD. 1998. Demonstration of the specificity of poliovirus encapsidation using a novel replicon which encodes enzymatically active firefly luciferase. Virology 243:1–11. doi: 10.1006/viro.1998.9046. [DOI] [PubMed] [Google Scholar]
- 36.Belov GA, Habbersett C, Franco D, Ehrenfeld E. 2007. Activation of cellular Arf GTPases by poliovirus protein 3CD correlates with virus replication. J Virol 81:9259–9267. doi: 10.1128/JVI.00840-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Simonyan V, Chumakov K, Dingerdissen H, Faison W, Goldweber S, Golikov A, Gulzar N, Karagiannis K, Vinh Nguyen Lam P, Maudru T, Muravitskaja O, Osipova E, Pan Y, Pschenichnov A, Rostovtsev A, Santana-Quintero L, Smith K, Thompson EE, Tkachenko V, Torcivia-Rodriguez J, Voskanian A, Wan Q, Wang J, Wu TJ, Wilson C, Mazumder R. 2016. High-performance integrated virtual environment (HIVE): a robust infrastructure for next-generation sequence data analysis. Database (Oxford) 2016:baw022. doi: 10.1093/database/baw022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khattar SK, Manoharan V, Bhattarai B, LaBranche CC, Montefiori DC, Samal SK. 2015. Mucosal immunization with Newcastle disease virus vector coexpressing HIV-1 Env and Gag proteins elicits potent serum, mucosal, and cellular immune responses that protect against vaccinia virus Env and Gag challenges. mBio 6(4):e01005. doi: 10.1128/mBio.01005-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Khattar SK, Samal S, DeVico AL, Collins PL, Samal SK. 2011. Newcastle disease virus expressing human immunodeficiency virus type 1 envelope glycoprotein induces strong mucosal and serum antibody responses in guinea pigs. J Virol 85:10529–10541. doi: 10.1128/JVI.05050-11. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 40.Khattar SK, DeVico AL, LaBranche CC, Panda A, Montefiori DC, Samal SK. 2016. Enhanced immune responses to HIV-1 envelope elicited by a vaccine regimen consisting of priming with Newcastle disease virus expressing HIV gp160 and boosting with gp120 and SOSIP gp140 proteins. J Virol 90:1682–1686. doi: 10.1128/JVI.02847-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Anonymous. 1997. Poliomyelitis prevention in the United States: introduction of a sequential vaccination schedule of inactivated poliovirus vaccine followed by oral poliovirus vaccine. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 46:1–25. [PubMed] [Google Scholar]
- 42.Cerutti A, Chen K, Chorny A. 2011. Immunoglobulin responses at the mucosal interface. Annu Rev Immunol 29:273–293. doi: 10.1146/annurev-immunol-031210-101317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grimwood K, Lund JCS, Coulson BS, Hudson IL, Bishop RF, Barnes GL. 1988. Comparison of serum and mucosal antibody responses following severe acute rotavirus gastroenteritis in young children. J Clin Microbiol 26:732–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Panyasing Y, Goodell CK, Gimenez-Lirola L, Kittawornrat A, Wang C, Schwartz KJ, Zimmerman JJ. 2013. Kinetics of influenza A virus nucleoprotein antibody (IgM, IgA, and IgG) in serum and oral fluid specimens from pigs infected under experimental conditions. Vaccine 31:6210–6215. doi: 10.1016/j.vaccine.2013.10.040. [DOI] [PubMed] [Google Scholar]
- 45.Pasetti MF, Simon JK, Sztein MB, Levine MM. 2011. Immunology of gut mucosal vaccines. Immunol Rev 239:125–148. doi: 10.1111/j.1600-065X.2010.00970.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gonzalez G. 2016. Determining the stage of the estrous cycle in female mice by vaginal smear. Cold Spring Harb Protoc doi: 10.1101/pdb.prot094474. [DOI] [PubMed] [Google Scholar]
- 47.Shimizu H. 2016. Development and introduction of inactivated poliovirus vaccines derived from Sabin strains in Japan. Vaccine 34:1975–1985. doi: 10.1016/j.vaccine.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 48.Adeyemi OO, Nicol C, Stonehouse NJ, Rowlands DJ. 2017. Increasing type 1 poliovirus capsid stability by thermal selection. J Virol 91:e01586-. doi: 10.1128/JVI.01586-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shulman LM, Gavrilin E, Jorba J, Martin J, Burns CC, Manor Y, Moran-Gilad J, Sofer D, Hindiyeh MY, Gamzu R, Mendelson E, Grotto I; Genotype–Phenotype Identification Group. 2014. Molecular epidemiology of silent introduction and sustained transmission of wild poliovirus type 1, Israel, 2013. Euro Surveill 19:20709. doi: 10.2807/1560-7917.ES2014.19.7.20709. [DOI] [PubMed] [Google Scholar]
- 50.Kopel E, Kaliner E, Grotto I. 2014. Lessons from a public health emergency—importation of wild poliovirus to Israel. N Engl J Med 371:981–983. doi: 10.1056/NEJMp1406250. [DOI] [PubMed] [Google Scholar]
- 51.Ohka S, Igarashi H, Nagata N, Sakai M, Koike S, Nochi T, Kiyono H, Nomoto A. 2007. Establishment of a poliovirus oral infection system in human poliovirus receptor-expressing transgenic mice that are deficient in alpha/beta interferon receptor. J Virol 81:7902–7912. doi: 10.1128/JVI.02675-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Koike S, Nagata N. 2016. A transgenic mouse model of poliomyelitis. Methods Mol Biol 1387:129–144. doi: 10.1007/978-1-4939-3292-4_7. [DOI] [PubMed] [Google Scholar]
- 53.Bienenstock J, McDermott M, Befus D, O'Neill M. 1978. A common mucosal immunologic system involving the bronchus, breast and bowel. Adv Exp Med Biol 107:53–59. doi: 10.1007/978-1-4684-3369-2_7. [DOI] [PubMed] [Google Scholar]
- 54.Ciabattini A, Pettini E, Arsenijevic S, Pozzi G, Medaglini D. 2010. Intranasal immunization with vaccine vector Streptococcus gordonii elicits primed CD4+ and CD8+ T cells in the genital and intestinal tracts. Vaccine 28:1226–1233. doi: 10.1016/j.vaccine.2009.11.021. [DOI] [PubMed] [Google Scholar]
- 55.Ruane D, Brane L, Reis BS, Cheong C, Poles J, Do Y, Zhu HF, Velinzon K, Choi JH, Studt N, Mayer L, Lavelle EC, Steinman RM, Mucida D, Mehandru S. 2013. Lung dendritic cells induce migration of protective T cells to the gastrointestinal tract. J Exp Med 210:1871–1888. doi: 10.1084/jem.20122762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ramirez K, Wahid R, Richardson C, Bargatze RF, El-Kamary SS, Sztein MB, Pasetti MF. 2012. Intranasal vaccination with an adjuvanted Norwalk virus-like particle vaccine elicits antigen-specific B memory responses in human adult volunteers. Clin Immunol 144:98–108. doi: 10.1016/j.clim.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 57.El-Kamary SS, Pasetti MF, Mendelman PM, Frey SE, Bernstein DI, Treanor JJ, Ferreira J, Chen WH, Sublett R, Richardson C, Bargatze RF, Sztein MB, Tacket CO. 2010. Adjuvanted intranasal Norwalk virus-like particle vaccine elicits antibodies and antibody-secreting cells that express homing receptors for mucosal and peripheral lymphoid tissues. J Infect Dis 202:1649–1658. doi: 10.1086/657087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Keeney AH, Hunter MC. 1951. Human infection with the Newcastle virus of fowls. AMA Arch Ophthalmol 46:94–95. doi: 10.1001/archopht.1951.01700020099011. [DOI] [PubMed] [Google Scholar]
- 59.Evans AS. 1955. Pathogenicity and immunology of Newcastle disease virus (NVD) in man. Am J Public Health Nations Health 45:742–745. doi: 10.2105/AJPH.45.6.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mustaffa-Babjee A, Ibrahim AL, Khim TS. 1976. A case of human infection with Newcastle disease virus. Southeast Asian J Trop Med Public Health 7:622–624. [PubMed] [Google Scholar]
- 61.Kapczynski DR, King DJ. 2005. Protection of chickens against overt clinical disease and determination of viral shedding following vaccination with commercially available Newcastle disease virus vaccines upon challenge with highly virulent virus from the California 2002 exotic Newcastle disease outbreak. Vaccine 23:3424–3433. doi: 10.1016/j.vaccine.2005.01.140. [DOI] [PubMed] [Google Scholar]
- 62.Yang HM, Zhao J, Xue J, Yang YL, Zhang GZ. 2017. Antigenic variation of LaSota and genotype VII Newcastle disease virus (NDV) and their efficacy against challenge with velogenic NDV. Vaccine 35:27–32. doi: 10.1016/j.vaccine.2016.11.048. [DOI] [PubMed] [Google Scholar]
- 63.Han GZ, Worobey M. 2011. Homologous recombination in negative sense RNA viruses. Viruses 3:1358–1373. doi: 10.3390/v3081358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chare ER, Gould EA, Holmes EC. 2003. Phylogenetic analysis reveals a low rate of homologous recombination in negative-sense RNA viruses. J Gen Virol 84:2691–2703. doi: 10.1099/vir.0.19277-0. [DOI] [PubMed] [Google Scholar]
- 65.Huang Z, Elankumaran S, Panda A, Samal SK. 2003. Recombinant Newcastle disease virus as a vaccine vector. Poultry Sci 82:899–906. doi: 10.1093/ps/82.6.899. [DOI] [PubMed] [Google Scholar]
- 66.Nakaya T, Cros J, Park MS, Nakaya Y, Zheng H, Sagrera A, Villar E, Garcia-Sastre A, Palese P. 2001. Recombinant Newcastle disease virus as a vaccine vector. J Virol 75:11868–11873. doi: 10.1128/JVI.75.23.11868-11873.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Henao-Restrepo AM, Camacho A, Longini IM. 2017. Efficacy and effectiveness of an rVSV-vectored vaccine in preventing Ebola virus disease: final results from the Guinea ring vaccination, open-label, cluster-randomised trial (Ebola Ca Suffit!). Lancet 389:505–518. doi: 10.1016/S0140-6736(16)32621-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Garbutt M, Liebscher R, Wahl-Jensen V, Jones S, Moller P, Wagner R, Volchkov V, Klenk HD, Feldmann H, Stroher U. 2004. Properties of replication-competent vesicular stomatitis virus vectors expressing glycoproteins of filoviruses and arenaviruses. J Virol 78:5458–5465. doi: 10.1128/JVI.78.10.5458-5465.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kärber G. 1931. Beitrag zur kollektiven Behandlung pharmakologischer Reihenversuche. Naunyn-Schmiedebergs Arch Exp Pathol Pharmakol 162:480–483. doi: 10.1007/BF01863914. [DOI] [Google Scholar]
- 70.Panda A, Elankumaran S, Krishnamurthy S, Huang ZH, Samal SK. 2004. Loss of N-linked glycosylation from the hemagglutinin-neuraminidase protein alters virulence of Newcastle disease virus. J Virol 78:4965–4975. doi: 10.1128/JVI.78.10.4965-4975.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Huang ZH, Krishnamurthy S, Panda A, Samal SK. 2001. High-level expression of a foreign gene from the most 3′-proximal locus of a recombinant Newcastle disease virus. J Gen Virol 82:1729–1736. doi: 10.1099/0022-1317-82-7-1729. [DOI] [PubMed] [Google Scholar]
- 72.Herold J, Andino R. 2000. Poliovirus requires a precise 5′ end for efficient positive-strand RNA synthesis. J Virol 74:6394–6400. doi: 10.1128/JVI.74.14.6394-6400.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Belov GA, Kovtunovych G, Jackson CL, Ehrenfeld E. 2010. Poliovirus replication requires the N-terminus but not the catalytic Sec7 domain of ArfGEF GBF1. Cell Microbiol 12:1463–1479. doi: 10.1111/j.1462-5822.2010.01482.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Samuel AS, Subbiah M, Shive H, Collins PL, Samal SK. 2011. Experimental infection of hamsters with avian paramyxovirus serotypes 1 to 9. Vet Res 42:38. doi: 10.1186/1297-9716-42-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Belov GA, Feng Q, Nikovics K, Jackson CL, Ehrenfeld E. 2008. A critical role of a cellular membrane traffic protein in poliovirus RNA replication. PLoS Pathog 4:e1000216. doi: 10.1371/journal.ppat.1000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bradford MM. 1976. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72:248–254. [DOI] [PubMed] [Google Scholar]
- 77.Anonymous. 1997. Manual for the virological investigation of polio. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 78.National Research Council. 2011. Guide for the care and use of laboratory animals, 8th ed National Academies Press, Washington, DC. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
NGS data and raw sequencing reads, as analyzed with the HIVE software package (37), are deposited at https://hive.biochemistry.gwu.edu/review/NDV_LaSota_strain_PV.