Abstract
Background
At current prognostication of low grade glioma remains suboptimal and might be improved with additional markers. These may guide treatment decisions, in particular on early adjuvant therapy versus wait and see after surgery.
Methods
We used a targeted Next-Generation Sequencing panel to assess mutational and copy number status of selected genes and chromosomes in a consecutive series of adult grade II supratentorial glioma, and assessed the impact of molecular markers of interest on overall survival.
Results
207 IDH mutated grade II glioma samples were analyzed with a median follow-up of 6.9 years. Loss of region 9p21.3 did not show a correlation with outcome in IDH mutated 1p/19q-codeleted oligodendroglioma or IDH mutated astrocytoma. We found a significant shorter overall survival with univariable analysis in IDH mutated astrocytoma patients with trisomy of chromosome 7 (Log rank P = 0.044) and in IDH mutated 1p/19q-codeleted oligodendroglioma patients with a PTEN mutation (Log rank P = 0.033). We could not validate these findings in multivariate analysis or in the TCGA dataset.
Conclusions
Loss of 9p21.3 is not associated with outcome in a molecularly defined cohort of grade II glioma and therefore it remains unclear if loss of 9p21.3 can be used as additional marker of anaplasia or to guide treatment decisions. Trisomy of chromosome 7 in IDH mutated astrocytoma and PTEN mutations in IDH mutated oligodendroglioma are potential markers of poor prognosis, but require confirmation in larger series.
Electronic supplementary material
The online version of this article (10.1007/s11060-018-2867-8) contains supplementary material, which is available to authorized users.
Keywords: Glioma, Low-grade, Molecular markers, IDH, 9p21.3, 7q
Introduction
In 2016 the World Health Organization Classification of Tumors of the Central Nervous System (WHO) was updated, resulting in a major change in the classification of diffuse gliomas [1]. The 2016 WHO classification provides an integrated diagnosis of glioma by combining histopathological with genotypic features. Moreover, in the case of discrepancy between genotypic and histopathological features, the genotypic features are leading in classifying a glioma subtype. As a result the 2016 CNS WHO markedly improved the objectivity of classification and prognosis estimation as compared to the previous version [1–3].
Three clinically relevant subgroups of diffuse low-grade (grade II) gliomas are identified and recognized by the WHO 2016 classification based on two molecular markers: (1) oligodendroglioma, IDH mutant and 1p/19q-codeleted (IDH1/2 mutation in combination with presence of a co-deletion of the entire 1p and 19q chromosomal arms), (2) diffuse astrocytoma, IDH mutant; (IDH1/2 mutation without 1p19q co-deletion), and (3) diffuse astrocytoma, IDH1/2 wildtype. Other frequently reported genetic changes in glioma are CIC, FUBP1, TP53, ATRX, TERT promoter mutations and copy number changes of chromosome 7, 9, and 10 [1, 2, 4, 5]. Although the 2016 CNS WHO update is robust and provides a more accurate prognosis estimation, there is still variation in outcome within the different entities and the grading of glioma is still depending on histological features. Prognostication might be further improved if additional molecular markers can be identified that correlate with prognosis. These markers may facilitate treatment decisions, in particular for early radiotherapy and adjuvant chemotherapy versus a wait and watch policy after surgery. This is in particular relevant, as the currently used criteria (age of 40, less than gross total resection) are quite arbitrary, and in some patients that are 40 years or older with a less than gross total resection, a wait and watch period of years is possible [6–8]. Thus, molecular factors showing a clinically significant relation with outcome would be highly welcome.
Several studies have tried to further stratify molecularly defined glioma, most of them in anaplastic glioma. For example, some studies showed that loss of chromosome 9p or specifically the 9p21.3 region is associated with a worse prognosis in various subtypes of grade III and IV glioma [9–11]. This could however not be validated in a recently published large cohort of grade II and III glioma [12]. In the present study we aimed to identify molecular prognostic markers for grade II IDH mutated astrocytoma (in particular loss of 10q, trisomy of chromosome 7, PTEN mutations) and in grade II IDH mutated 1p19q-codeleted oligodendroglioma (in particular loss of 9p21.3, CIC, FUBP1, and PTEN mutations). To our knowledge there are no published studies that investigated prognostic impact of these markers specifically in molecularly defined grade II glioma. Therefore, in a well-defined cohort of histologically proven supratentorial adult grade II glioma we used a targeted Next-Generation Sequencing panel for molecular classification and evaluated the prognostic value of glioma specific molecular markers.
Methods
Patient selection
For this study we used a cohort of patients from a project on extent of resection in grade II glioma [13]. Adult patients (age ≥ 18 years) with histopathologically confirmed supratentorial grade II glioma were included. Tissue samples were collected in two Dutch hospitals (Erasmus MC Cancer Institute, Rotterdam; and Elisabeth-TweeSteden Hospital, Tilburg). Histopathological diagnosis and low grade was confirmed by a dedicated neuropathologist (J.M.K.). Time-window of patient inclusion was 2003–2016. For clinical factors, age, KPS, type of surgery, and treatment after surgery were collected. This study was approved by the medical ethics committee of Erasmus MC.
DNA extraction
DNA was isolated from formalin-fixed-paraffin-embedded (FFPE) tissue blocks. Tissue areas with high percentage of neoplastic cells (preferably > 70%, but at least 50%) were manually macrodissected from 10 µm sections. Macrodissected tissue was digested using Proteinase K incubation at 56 °C overnight in presence of 5% Chelex 100 resin (Bio-Rad). After overnight incubation, proteinase K was inactivated at 90 °C for 10 min. Next, dissolved DNA was separated from Chelex resin and cell debris by centrifugation at 20 g for 5 min. DNA concentration was measured using the Qubit 3.0 Fluorometer according to manufacturer’s protocol (Life Technologies).
Next-Generation-Sequencing
We used Next-Generation Sequencing to assess mutational and copy number status of selected genes and chromosomes. The primer panel consisted of primers for glioma specific genes of interest (hot spot regions, or whole gene) and primers for highly polymorphic single nucleotide polymorphisms to detect large genomic alterations in chromosomes of interest. Chromosomal imbalances and loss of heterozygosity (LOH) were estimated as described previously [3]. An overview of the targeted hotspots/whole genes and chromosomes is shown in Supplementary Table 1. Sequencing was performed with the Ion Torrent Personal Genome Machine or Ion S5 (Life Technologies). TERT promoter mutational status (C228T and C250T mutation) was assessed in a separate assay as described before (SNaPshot, Life Technologies) [3].
Survival
All patients were followed until death or censored at date of last follow-up. Overall survival (OS) was measured from the date of diagnostic scan until date of death or censorship. Date of death was provided by patient records or the Municipal Personal Records Database. The database was developed and maintained at Erasmus MC, and locked on March 21st 2018.
Statistical analysis
All analyses were performed using R (3.3.2) and RStudio (1.0.44). Overall survival was measured as time between date of diagnostic scan and date of death or censorship. Overall survival is shown in Kaplan–Meier plots (ggplot2 package in R). Univariable analyses were performed using the Log-rank test and multivariable analyses with Cox proportional-hazards models. Categorical data were analyzed with Pearson’s Chi square test or Fisher’s exact test when assumptions of the Chi square test were violated (as indicated in the respective tables). Kruskal–Wallis test was used for continuous data. All calculations were two-sided tests, with a P value < 0.05 considered as statistically significant.
Results
We identified 246 patients with a pathologically confirmed grade II glioma with available FFPE material. Of these, 2 patients were excluded due to insufficient DNA yield and no remaining tissue for DNA isolation, and 14 were excluded from analysis due to sequencing failure (very low coverage and/or uniformity for most amplicons after two attempts). At the time of analysis, 53 patients were reported dead, 15 of the 95 IDH mutated 1p/19q-codeleted oligodendroglioma patients and 38 of the 112 IDH mutated astrocytoma patients.
Molecular classification
As we were interested in additional markers for IDH mutated grade II glioma, 23 patient samples that were classified as IDH wildtype were excluded from further analyses. 207 patients were included in final analyses with a median follow-up of 6.9 years (range 0.4–21.7 years). Clinical characteristics are shown in Table 1. An oncoprint plot with all mutations and copy number alterations for the 207 patients is shown in Fig. 1. Mutation frequencies per molecular subgroup are shown in Table 2. Median overall survival per CNS WHO 2016 molecular subgroup was consistent with literature (Supplementary Fig. 1).
Table 1.
Patient characteristics
| Characteristics | Oligodendroglioma | Astrocytoma IDHmt | P | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Patients (n) | 95 | 112 | |||
| Sex | 0.149 | ||||
| Male | 49 | 51.6 | 71 | 63.4 | |
| Female | 46 | 48.4 | 41 | 36.6 | |
| Age | < 0.0001 | ||||
| Median (IQR) | 45 | (37–52) | 37 | (29–45) | |
| Type of 1st surgery | 0.002† | ||||
| Awake craniotomy | 51 | 53.7 | 54 | 48.2 | |
| Normal resection | 23 | 24.2 | 49 | 43.8 | |
| Open biopsy | 7 | 7.4 | 2 | 1.8 | |
| Stereotactic biopsy | 14 | 14.7 | 7 | 6.2 | |
| Preoperative KPS | 0.064 | ||||
| Median (IQR) | 100 | (100–100) | 100 | (90–100) | |
| Histopathological diagnosis | |||||
| Grade II astrocytoma | 8 | 8.4 | 87 | 77.7 | |
| Grade II oligodendroglioma | 77 | 81.1 | 9 | 8.0 | |
| Grade II oligo-astrocytoma | 10 | 10.5 | 16 | 14.3 | |
| Treatment after 1st surgery | < 0.0001 | ||||
| Wait and scan | 52 | 54.7 | 52 | 46.4 | |
| Chemotherapy | 24 | 25.3 | 5 | 4.5 | |
| Radiotherapy | 16 | 16.8 | 42 | 37.5 | |
| Chemoradiation | 3 | 3.2 | 13 | 11.6 | |
| Follow-up (years) | |||||
| Median (range) | 8.0 | (0.9–21.7) | 6.1 | (0.4–16.7) | |
†Fisher’s exact test
Fig. 1.
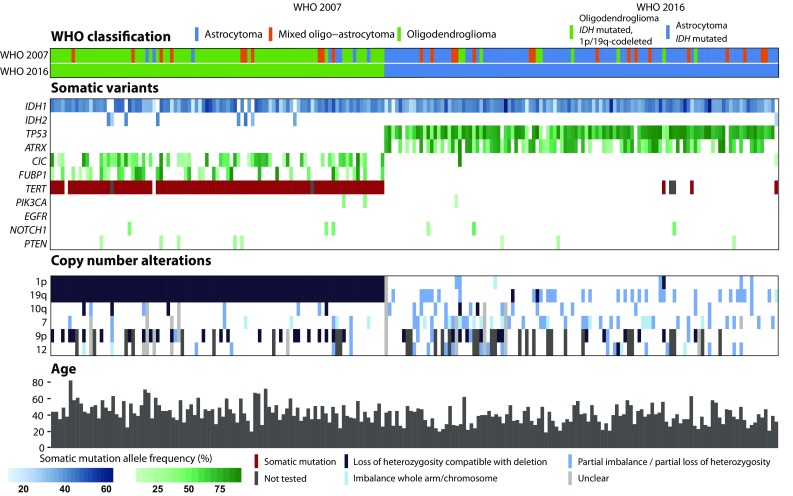
Oncoprint plot with overview of somatic alterations per patient. At the top of the figure the WHO 2007 and WHO 2016 classification are shown. In the middle part all somatic variants and copy number alterations are shown. Patients are separated based on the WHO 2016 classification. IDH mutated 1p/19q-codeleted patients are depicted in the left part of the figure and IDH mutated astrocytoma patients on the right part of the figure. The bottom part of the figure shows the clinical characteristic age per patient
Table 2.
Frequencies of gene mutations per WHO subgroup
| Gene | IDH mutated astrocytoma | IDH mutated 1p/19q-codeleted oligodendroglioma | ||
|---|---|---|---|---|
| N | % | N | % | |
| IDH1 | 111 | 99.1 | 87 | 91.6 |
| IDH2 | 1 | 0.9 | 8 | 8.4 |
| TP53 | 105 | 93.8 | 0 | 0 |
| ATRX | 75 | 67 | 0 | 0 |
| CIC | 2 | 1.8 | 52 | 54.7 |
| FUBP1 | 0 | 0 | 36 | 37.9 |
| TERT | 3 | 2.7 | 91 | 95.8 |
| PIK3CA | 1 | 0.9 | 2 | 2.1 |
| EGFR | 0 | 0 | 0 | 0 |
| NOTCH1 | 3 | 2.7 | 3 | 3.2 |
| PTEN | 3 | 2.7 | 5 | 5.3 |
IDH mutated astrocytoma
107 of the 112 IDH mutated astrocytomas could be reliably evaluated for imbalance of chromosome 7: 13 samples showed imbalance compatible with trisomy of the entire chromosome 7. In univariable analysis trisomy of chromosome 7 was significantly associated with shorter overall survival (Log rank P = 0.044). However, this survival difference lost significance when correcting for age and KPS (HR 2.22; 95% CI 0.95–5.20; P = 0.066). Only two samples showed loss of entire chromosomal arm 10q, both with a relatively poor overall survival of less than 8 years (Fig. 2). Loss of 9p21.3 (n = 18) was not associated with outcome. Out of the 18 patients with loss of 9p21.3, 13 showed loss of the entire 9p chromosomal arm, which was also not associated with outcome. A PTEN mutation was detected in 3 patients (all three no loss of 10q) and did not show an impact on outcome (Fig. 2).
Fig. 2.
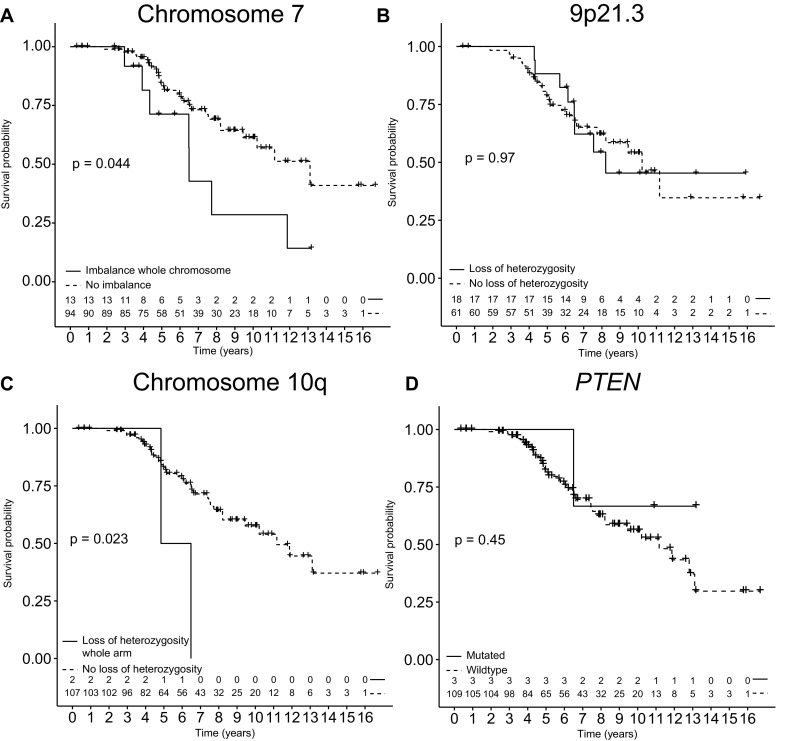
Kaplan–Meier plots with overall survival of IDH mutated astrocytoma patients. Kaplan–Meier plots with overall survival of IDH mutated astrocytoma patients stratified for presence of a imbalance pattern consistent with trisomy of chromosome 7, b loss of 9p21.3 region, c loss of chromosomal arm 10q, d and presence of a PTEN mutation
IDH mutated 1p/19q-codeleted oligodendroglioma
In IDH mutated 1p/19q-codeleted oligodendroglioma, both CIC and FUBP1 mutations were frequent events, but neither was associated with prognosis (Fig. 3). In 27 out of the 77 patients that could be reliably evaluated for copy number changes on chromosome 9p, loss of 9p21.3 was found. Of these, 23 showed loss of entire chromosomal arm 9p. No homozygous deletions or mutations of CDKN2A were detected. Loss of 9p21.3 did not have significant impact on overall survival (Log rank P = 0.12) (Fig. 3). Additional analysis for impact of loss of entire 9p did not show different results. Trisomy of chromosome 7 and loss of chromosomal arm 10q were present in a few samples, both without impact on overall survival (Fig. 3). Five patients were PTEN mutated and showed a significantly shorter OS in univariable analysis (Log rank P = 0.033). This survival difference was not significant anymore when correcting for age and KPS (HR 3.73; 95% CI 0.78–17.76; P = 0.097).
Fig. 3.
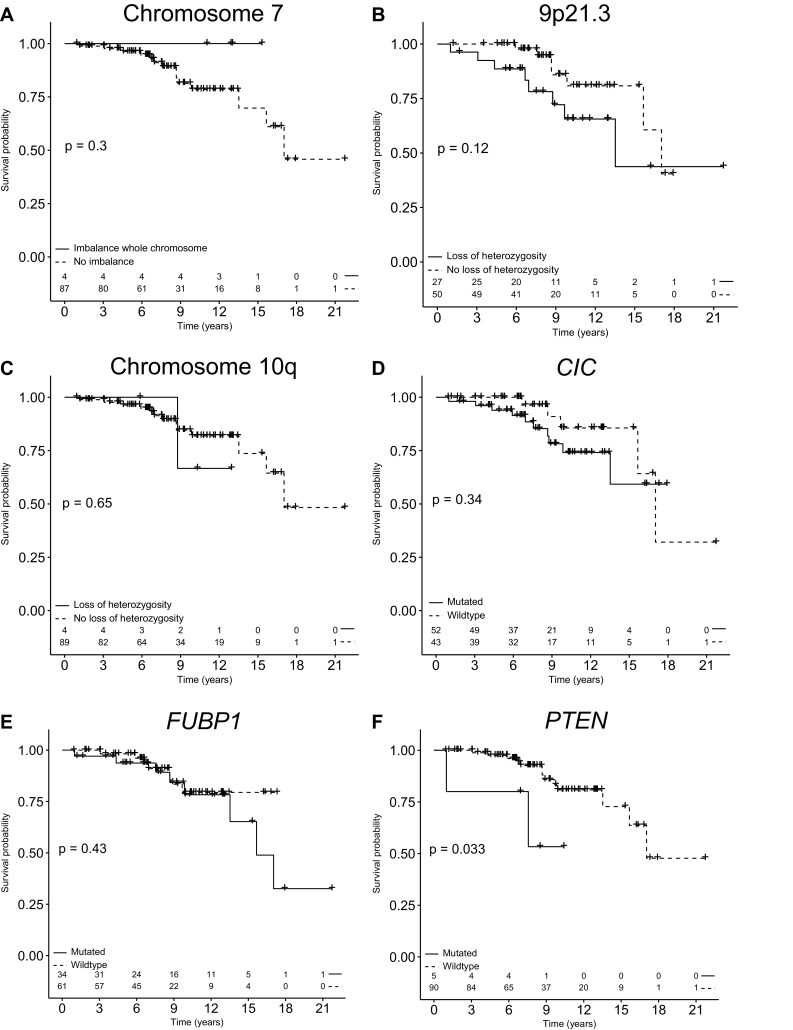
Kaplan–Meier plots with overall survival of IDH mutated 1p/19q-codeleted oligodendroglioma patients. Kaplan–Meier plots with overall survival of IDH mutated 1p/19q-codeleted oligodendroglioma patients stratified for presence of a Imbalance pattern consistent with trisomy of chromosome 7, b loss of 9p21.3 region, c loss of chromosomal arm 10q, d presence of CIC mutation, e presence of FUBP1 mutation, f and presence of a PTEN mutation
Exploratory analyses
On further exploratory analyses, we found no other molecular markers that significantly impact on overall survival in molecularly defined LGG with the targeted sequencing panel we used.
Validation of findings in the TCGA
We aimed to validate our findings in the publically available dataset The Cancer Genome Atlas (TCGA). In the TCGA dataset, 9 out of 72 grade II IDH mutated astrocytoma showed trisomy of chromosome 7, but this was not significantly associated with a difference in overall survival in univariate analysis (Log rank P = 0.3). We also analyzed the TCGA dataset for presence of loss of 10q in grade II IDH mutated astrocytoma. Only one sample showed loss of 10q, with a poor survival (1.75 years). Among the 47 grade II IDH mutated 1p/19q-codeleted oligodendroglioma samples in the TCGA dataset, there were no samples with a PTEN mutation, confirming the rarity of this event.
Discussion
In this study we aimed to investigate the prognostic impact of additional molecular markers in grade II IDH mutated astrocytoma and grade II IDH mutated 1p/19q-codeleted oligodendroglioma. We used a targeted NGS panel to investigate genes that are frequently mutated in glioma and to investigate regions that are frequently reported to have copy number changes.
Loss of chromosome 9p or in particular the 9p21.3 region is a frequently reported copy number variation in all glioma subtypes [2, 9–11]. Several studies investigated the impact of loss of 9p/9p21.3 on prognosis. A meta-analysis published in 2015 pooled the data of 13 different studies that were published between 2002 and 2013 [10]. Although most individual studies in this meta-analysis did not show a survival difference, the pooled data showed that loss of 9p was significantly associated with a poorer prognosis. However, most studies in this analysis did not take into account confounding factors such as IDH1/2 mutational status, and a subgroup analysis of types of gliomas showed that impact of loss of 9p on overall survival was particularly present in the glioblastoma subtype. A recent study specifically focused on the impact of 9p loss in grade II and III glioma and found that loss of 9p is an independent prognostic factor in IDH mutated glioma, however, the effect was most clear in IDH mutated astrocytomas [11]. In opposite, Alentorn et al. found loss of 9p to be a poor prognostic marker in anaplastic oligodendroglioma [9]. A later study by Aoki et al. did not confirm this finding however [12]. Our study is the first that specifically focusses on the impact of loss of 9p21.3 and entire 9p in histologically defined grade II glioma. We could not confirm impact of loss of 9p21.3 region or entire 9p on prognosis in IDH mutated astrocytoma nor in IDH mutated 1p/19q-codeleted oligodendroglioma. However, a trend towards shorter overall survival in IDH mutated 1p/19q-codeleted oligodendroglioma with loss of 9p21.3 is visible, and longer follow-up and larger sample size is necessary for final conclusions. Exact comparison of our data with previous literature is difficult, because of different selection criteria in the different cohorts. Therefore, it is yet unclear if in grade II IDH mutated glioma loss of 9p21.3 region can be used as marker of anaplasia or to guide more aggressive treatment strategies.
Trisomy of chromosome 7 is also frequently reported in glioma [2, 14, 15]. In combination with loss of 10q it is considered an early event in glioblastoma IDH wildtype and is correlated with dismal prognosis in grade II and III IDH wildtype glioma [2, 15–17]. Trisomy of chromosome 7 is also described in lower grade glioma, though less frequently. The impact of trisomy of 7 on overall survival in IDH mutated low grade glioma is not clear. To our knowledge no large series are published. Wessels et al. reported that polysomy of 7 was associated with a poorer prognosis in grade II astrocytoma, but this report antedates the discovery of the role IDH mutations in glioma [14]. In our cohort we found that trisomy of chromosome 7 might be a marker of poor prognosis in IDH mutated astrocytoma. However, this could not be validated in multivariate analysis nor in the TCGA data, and this observation requires validation in a larger independent cohort to define the clinical value.
CIC and FUBP1 mutations are frequently mutated in IDH mutated 1p/19q-codeleted oligodendroglioma and the prognostic impact has been investigated in several series. One study by Gleize et al. reported that inactivating CIC mutations in IDH mutated glioma correlate with poorer outcome. In other cohorts this effect was not observed [3, 18–20]. In our cohort we also did not find a correlation between CIC nor FUBP1 mutation and prognosis.
Our study has several limitations. The retrospective nature comes with the risk of a selection bias. We tried to avoid selection bias by analyzing a consecutive cohort of all grade II gliomas undergoing surgery within a specified period. Also due to the retrospective nature, treatment was heterogeneous. Furthermore, we may have missed smaller region copy number alterations and other mutations in regions not covered by our NGS panel. We used a diagnostically validated [21] and targeted NGS panel that consists of highly polymorphic SNPs that cover whole chromosomes of interest with roughly 1 SNP per 3 MB. Large scale copy number variations of whole chromosomes or large parts of chromosomes can therefore be reliably detected, but small region or subclonal copy number variations are potentially missed. However, the aim of this study was to validate the impact of large region copy number variations which were described before and that are considered to be early events, and these can be reliably detected with the panel used [21]. Also, it is known that lengthy follow-up in studies on low-grade glioma is necessary for definitive conclusions, so longer of follow up of this dataset is necessary.
In conclusion, in univariable analysis we found a significant shorter overall survival in IDH mutated astrocytoma patients with trisomy of chromosome 7, and in IDH mutated 1p/19q-codeleted oligodendroglioma patients with a PTEN mutation. However, we could not confirm these findings in multivariate analysis or in the TCGA validation set and therefore these findings require validation in other larger series. We could not confirm the impact on OS of LOH of 9p21.3 (the CDKN2A region) which is frequently reported as a progression marker particularly in higher grade glioma. However, we need lengthy follow-up for definitive conclusions. Also, other strategies should be pursued to identify prognostic relevant molecular markers within these IDH mutant glioma subgroups, like methylation patterns and total number of chromosomal aberrations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
MMJW, PJF, CMFD, AJPEV, and MJvdB contributed to the conception and design of the work. All authors contributed to the acquisition and interpretation of the data. MMJW, PJF, and MJVDB wrote the initial draft of the report. All authors critically reviewed each draft and provided feedback and intellectual content, and provided final approval to submit for publication.
Conflict of interest
Martin J. van den Bent reports personal fees from Roche, Novartis, BMS, MSD, Actelion, Blue Earth Diagnostics, and personal fees and grants from Abbvie, all outside the submitted work. All other authors report no disclosures.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. This study was approved by the medical ethics committee of Erasmus MC.
References
- 1.Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016;131:803–820. doi: 10.1007/s00401-016-1545-1. [DOI] [PubMed] [Google Scholar]
- 2.Cancer Genome Atlas Research N. Brat DJ, Verhaak RG, Aldape KD, Yung WK, Salama SR, Cooper LA, Rheinbay E, Miller CR, Vitucci M, Morozova O, Robertson AG, Noushmehr H, Laird PW, Cherniack AD, Akbani R, Huse JT, Ciriello G, Poisson LM, Barnholtz-Sloan JS, Berger MS, Brennan C, Colen RR, Colman H, Flanders AE, Giannini C, Grifford M, Iavarone A, Jain R, Joseph I, Kim J, Kasaian K, Mikkelsen T, Murray BA, O’Neill BP, Pachter L, Parsons DW, Sougnez C, Sulman EP, Vandenberg SR, Van Meir EG, von Deimling A, Zhang H, Crain D, Lau K, Mallery D, Morris S, Paulauskis J, Penny R, Shelton T, Sherman M, Yena P, Black A, Bowen J, Dicostanzo K, Gastier-Foster J, Leraas KM, Lichtenberg TM, Pierson CR, Ramirez NC, Taylor C, Weaver S, Wise L, Zmuda E, Davidsen T, Demchok JA, Eley G, Ferguson ML, Hutter CM, Mills Shaw KR, Ozenberger BA, Sheth M, Sofia HJ, Tarnuzzer R, Wang Z, Yang L, Zenklusen JC, Ayala B, Baboud J, Chudamani S, Jensen MA, Liu J, Pihl T, Raman R, Wan Y, Wu Y, Ally A, Auman JT, Balasundaram M, Balu S, Baylin SB, Beroukhim R, Bootwalla MS, Bowlby R, Bristow CA, Brooks D, Butterfield Y, Carlsen R, Carter S, Chin L, Chu A, Chuah E, Cibulskis K, Clarke A, Coetzee SG, Dhalla N, Fennell T, Fisher S, Gabriel S, Getz G, Gibbs R, Guin R, Hadjipanayis A, Hayes DN, Hinoue T, Hoadley K, Holt RA, Hoyle AP, Jefferys SR, Jones S, Jones CD, Kucherlapati R, Lai PH, Lander E, Lee S, Lichtenstein L, Ma Y, Maglinte DT, Mahadeshwar HS, Marra MA, Mayo M, Meng S, Meyerson ML, Mieczkowski PA, Moore RA, Mose LE, Mungall AJ, Pantazi A, Parfenov M, Park PJ, Parker JS, Perou CM, Protopopov A, Ren X, Roach J, Sabedot TS, Schein J, Schumacher SE, Seidman JG, Seth S, Shen H, Simons JV, Sipahimalani P, Soloway MG, Song X, Sun H, Tabak B, Tam A, Tan D, Tang J, Thiessen N, Triche T, Jr, Van Den Berg DJ, Veluvolu U, Waring S, Weisenberger DJ, Wilkerson MD, Wong T, Wu J, Xi L, Xu AW, Yang L, Zack TI, Zhang J, Aksoy BA, Arachchi H, Benz C, Bernard B, Carlin D, Cho J, DiCara D, Frazer S, Fuller GN, Gao J, Gehlenborg N, Haussler D, Heiman DI, Iype L, Jacobsen A, Ju Z, Katzman S, Kim H, Knijnenburg T, Kreisberg RB, Lawrence MS, Lee W, Leinonen K, Lin P, Ling S, Liu W, Liu Y, Liu Y, Lu Y, Mills G, Ng S, Noble MS, Paull E, Rao A, Reynolds S, Saksena G, Sanborn Z, Sander C, Schultz N, Senbabaoglu Y, Shen R, Shmulevich I, Sinha R, Stuart J, Sumer SO, Sun Y, Tasman N, Taylor BS, Voet D, Weinhold N, Weinstein JN, Yang D, Yoshihara K, Zheng S, Zhang W, Zou L, Abel T, Sadeghi S, Cohen ML, Eschbacher J, Hattab EM, Raghunathan A, Schniederjan MJ, Aziz D, Barnett G, Barrett W, Bigner DD, Boice L, Brewer C, Calatozzolo C, Campos B, Carlotti CG, Jr, Chan TA, Cuppini L, Curley E, Cuzzubbo S, Devine K, DiMeco F, Duell R, Elder JB, Fehrenbach A, Finocchiaro G, Friedman W, Fulop J, Gardner J, Hermes B, Herold-Mende C, Jungk C, Kendler A, Lehman NL, Lipp E, Liu O, Mandt R, McGraw M, McLendon R, McPherson C, Neder L, Nguyen P, Noss A, Nunziata R, Ostrom QT, Palmer C, Perin A, Pollo B, Potapov A, Potapova O, Rathmell WK, Rotin D, Scarpace L, Schilero C, Senecal K, Shimmel K, Shurkhay V, Sifri S, Singh R, Sloan AE, Smolenski K, Staugaitis SM, Steele R, Thorne L, Tirapelli DP, Unterberg A, Vallurupalli M, Wang Y, Warnick R, Williams F, Wolinsky Y, Bell S, Rosenberg M, Stewart C, Huang F, Grimsby JL, Radenbaugh AJ, Zhang J. Comprehensive, integrative genomic analysis of diffuse lower-grade gliomas. N Engl J Med. 2015;372:2481–2498. doi: 10.1056/NEJMoa1402121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dubbink HJ, Atmodimedjo PN, Kros JM, French PJ, Sanson M, Idbaih A, Wesseling P, Enting R, Spliet W, Tijssen C, Dinjens WN, Gorlia T, van den Bent MJ. Molecular classification of anaplastic oligodendroglioma using Next-Generation Sequencing: a report of the prospective randomized EORTC Brain Tumor Group 26951 phase III trial. Neuro Oncol. 2016;18:388–400. doi: 10.1093/neuonc/nov182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weller M, Weber RG, Willscher E, Riehmer V, Hentschel B, Kreuz M, Felsberg J, Beyer U, Loffler-Wirth H, Kaulich K, Steinbach JP, Hartmann C, Gramatzki D, Schramm J, Westphal M, Schackert G, Simon M, Martens T, Bostrom J, Hagel C, Sabel M, Krex D, Tonn JC, Wick W, Noell S, Schlegel U, Radlwimmer B, Pietsch T, Loeffler M, von Deimling A, Binder H, Reifenberger G. Molecular classification of diffuse cerebral WHO grade II/III gliomas using genome- and transcriptome-wide profiling improves stratification of prognostically distinct patient groups. Acta Neuropathol. 2015;129:679–693. doi: 10.1007/s00401-015-1409-0. [DOI] [PubMed] [Google Scholar]
- 5.Eckel-Passow JE, Lachance DH, Molinaro AM, Walsh KM, Decker PA, Sicotte H, Pekmezci M, Rice T, Kosel ML, Smirnov IV, Sarkar G, Caron AA, Kollmeyer TM, Praska CE, Chada AR, Halder C, Hansen HM, McCoy LS, Bracci PM, Marshall R, Zheng S, Reis GF, Pico AR, O’Neill BP, Buckner JC, Giannini C, Huse JT, Perry A, Tihan T, Berger MS, Chang SM, Prados MD, Wiemels J, Wiencke JK, Wrensch MR, Jenkins RB. Glioma groups based on 1p/19q, IDH, and TERT promoter mutations in tumors. N Engl J Med. 2015;372:2499–2508. doi: 10.1056/NEJMoa1407279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ryken TC, Parney I, Buatti J, Kalkanis SN, Olson JJ. The role of radiotherapy in the management of patients with diffuse low grade glioma: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2015;125:551–583. doi: 10.1007/s11060-015-1948-1. [DOI] [PubMed] [Google Scholar]
- 7.Soffietti R, Baumert BG, Bello L, von Deimling A, Duffau H, Frenay M, Grisold W, Grant R, Graus F, Hoang-Xuan K, Klein M, Melin B, Rees J, Siegal T, Smits A, Stupp R, Wick W, European Federation of Neurological S Guidelines on management of low-grade gliomas: report of an EFNS-EANO Task Force. Eur J Neurol. 2010;17:1124–1133. doi: 10.1111/j.1468-1331.2010.03151.x. [DOI] [PubMed] [Google Scholar]
- 8.Schiff D. Low-grade gliomas. Continuum. 2017;23:1564–1579. doi: 10.1212/CON.0000000000000537. [DOI] [PubMed] [Google Scholar]
- 9.Alentorn A, Dehais C, Ducray F, Carpentier C, Mokhtari K, Figarella-Branger D, Chinot O, Cohen-Moyal E, Ramirez C, Loiseau H, Elouahdani-Hamdi S, Beauchesne P, Langlois O, Desenclos C, Guillamo JS, Dam-Hieu P, Ghiringhelli F, Colin P, Godard J, Parker F, Dhermain F, Carpentier AF, Frenel JS, Menei P, Bauchet L, Faillot T, Fesneau M, Fontaine D, Motuo-Fotso MJ, Vauleon E, Gaultier C, Le Guerinel C, Gueye EM, Noel G, Desse N, Durando X, Barrascout E, Wager M, Ricard D, Carpiuc I, Delattre JY, Idbaih A, Network P. Allelic loss of 9p21.3 is a prognostic factor in 1p/19q codeleted anaplastic gliomas. Neurology. 2015;85:1325–1331. doi: 10.1212/WNL.0000000000002014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang T, Li S, Yang Z, Liu J, Han Y. Loss of heterozygosity of 9p Is associated with poorer survival in patients with gliomas. Mol Neurobiol. 2016;53:6407–6412. doi: 10.1007/s12035-015-9523-5. [DOI] [PubMed] [Google Scholar]
- 11.Roy DM, Walsh LA, Desrichard A, Huse JT, Wu W, Gao J, Bose P, Lee W, Chan TA. Integrated genomics for pinpointing survival loci within arm-level somatic copy number alterations. Cancer Cell. 2016;29:737–750. doi: 10.1016/j.ccell.2016.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aoki K, Nakamura H, Suzuki H, Matsuo K, Kataoka K, Shimamura T, Motomura K, Ohka F, Shiina S, Yamamoto T, Nagata Y, Yoshizato T, Mizoguchi M, Abe T, Momii Y, Muragaki Y, Watanabe R, Ito I, Sanada M, Yajima H, Morita N, Takeuchi I, Miyano S, Wakabayashi T, Ogawa S, Natsume A. Prognostic relevance of genetic alterations in diffuse lower-grade gliomas. Neuro Oncol. 2017 doi: 10.1093/neuonc/nox132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wijnenga MMJ, French PJ, Dubbink HD, Dinjens WNM, Atmodimedjo PN, Kros JM, Smits M, Gahrmann R, Rutten GJ, Verheul JB, Fleischeuer R, Dirven CMF, Vincent AJPE, van den Bent MJ. The impact of surgery in molecularly defined low-grade glioma: an integrated clinical, radiological and molecular analysis. Neuro Oncol. 2017 doi: 10.1093/neuonc/nox176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wessels PH, Twijnstra A, Kessels AG, Krijne-Kubat B, Theunissen PH, Ummelen MI, Ramaekers FC, Hopman AH. Gain of chromosome 7, as detected by in situ hybridization, strongly correlates with shorter survival in astrocytoma grade 2. Genes Chromosomes Cancer. 2002;33:279–284. doi: 10.1002/gcc.10029. [DOI] [PubMed] [Google Scholar]
- 15.van den Bent MJ, Weller M, Wen PY, Kros JM, Aldape K, Chang S. A clinical perspective on the 2016 WHO brain tumor classification and routine molecular diagnostics. Neuro Oncol. 2017;19:614–624. doi: 10.1093/neuonc/now277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aibaidula A, Chan AK, Shi Z, Li Y, Zhang R, Yang R, Li KK, Chung NY, Yao Y, Zhou L, Wu J, Chen H, Ng HK. Adult IDH wild-type lower-grade gliomas should be further stratified. Neuro Oncol. 2017;19:1327–1337. doi: 10.1093/neuonc/nox078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wijnenga MMJ, Dubbink HJ, French PJ, Synhaeve NE, Dinjens WNM, Atmodimedjo PN, Kros JM, Dirven CMF, Vincent A, van den Bent MJ. Molecular and clinical heterogeneity of adult diffuse low-grade IDH wild-type gliomas: assessment of TERT promoter mutation and chromosome 7 and 10 copy number status allows superior prognostic stratification. Acta Neuropathol. 2017;134:957–959. doi: 10.1007/s00401-017-1781-z. [DOI] [PubMed] [Google Scholar]
- 18.Wesseling P, van den Bent M, Perry A. Oligodendroglioma: pathology, molecular mechanisms and markers. Acta Neuropathol. 2015;129:809–827. doi: 10.1007/s00401-015-1424-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan AK, Pang JC, Chung NY, Li KK, Poon WS, Chan DT, Shi Z, Chen L, Zhou L, Ng HK. Loss of CIC and FUBP1 expressions are potential markers of shorter time to recurrence in oligodendroglial tumors. Mod Pathol. 2014;27:332–342. doi: 10.1038/modpathol.2013.165. [DOI] [PubMed] [Google Scholar]
- 20.Jiao Y, Killela PJ, Reitman ZJ, Rasheed AB, Heaphy CM, de Wilde RF, Rodriguez FJ, Rosemberg S, Oba-Shinjo SM, Nagahashi Marie SK, Bettegowda C, Agrawal N, Lipp E, Pirozzi C, Lopez G, He Y, Friedman H, Friedman AH, Riggins GJ, Holdhoff M, Burger P, McLendon R, Bigner DD, Vogelstein B, Meeker AK, Kinzler KW, Papadopoulos N, Diaz LA, Yan H. Frequent ATRX, CIC, FUBP1 and IDH1 mutations refine the classification of malignant gliomas. Oncotarget. 2012;3:709–722. doi: 10.18632/oncotarget.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dubbink HJ, Atmodimedjo PN, van Marion R, Krol NM, Riegman PH, Kros JM, van den Bent MJ, Dinjens WN. Diagnostic detection of allelic losses and imbalances by Next-Generation Sequencing: 1p/19q co-deletion analysis of gliomas. J Mol Diagn. 2016;18:775–786. doi: 10.1016/j.jmoldx.2016.06.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


