Abstract
Background
Health checks for cardiometabolic diseases could play a role in the identification of persons at high risk for disease. To improve the uptake of these health checks in primary care, we need to know what barriers and facilitators determine participation.
Methods
We used an iterative search strategy consisting of three steps: (a) identification of key-articles; (b) systematic literature search in PubMed, Medline and Embase based on keywords; (c) screening of titles and abstracts and subsequently full-text screening. We summarised the results into four categories: characteristics, attitudes, practical reasons and healthcare provider-related factors.
Results
Thirty-nine studies were included. Attitudes such as wanting to know of cardiometabolic disease risk, feeling responsible for, and concerns about one’s own health were facilitators for participation. Younger age, smoking, low education and attitudes such as not wanting to be, or being, worried about the outcome, low perceived severity or susceptibility, and negative attitude towards health checks or prevention in general were barriers. Furthermore, practical issues such as information and the ease of access to appointments could influence participation.
Conclusion
Barriers and facilitators to participation in health checks for cardiometabolic diseases were heterogeneous. Hence, it is not possible to develop a ‘one size fits all’ approach to maximise the uptake. For optimal implementation we suggest a multifactorial approach adapted to the national context with special attention to people who might be more difficult to reach. Increasing the uptake of health checks could contribute to identifying the people at risk to be able to start preventive interventions.
Keywords: Health check, cardiometabolic disease, cardiovascular disease, diabetes, prevention, primary care, general practitioner, attendance, participation
Introduction
Cardiometabolic diseases (CMDs) including cardiovascular disease (CVD), diabetes and chronic kidney disease remain the number one cause of death worldwide.1 To a large extent, CMDs are caused by an unhealthy lifestyle, with smoking, unhealthy diet and physical inactivity as the most important risk factors.2–5 With the increasing rates of obesity and insufficient physical activity,6 in combination with smoking and the ageing population,7 there is an urgent need for stimulating CMD prevention programmes. Studies have shown that as much as 80% of CVD could be prevented or postponed if risk factors in lifestyle and behaviour could be eliminated.8 To be able to do this, it is necessary to find the people with risk factors in lifestyle and behaviour. Selective prevention,9 defined as the identification of people at high risk for CMD among those without established CMD, combined with interventions to help prevent or delay the onset of disease therefore represents a good starting point for CMD prevention. The first step of selective prevention, CMD risk assessment, can be done by a health check. This health check could be organised in several ways, such as a questionnaire that can be completed on the Internet or a more detailed health check performed by a doctor and with (laboratory) tests. On the one hand, health checks have not been shown to be effective to reduce mortality10 and screening and lifestyle counselling in the general population has been shown to have no effect on the development of ischaemic heart disease.11 On the other hand, it has been shown that health checks in primary care led to an improvement in surrogate outcomes such as total cholesterol, blood pressure and body mass index (BMI)12 and a health check followed by tailored lifestyle advice led to both increased physical activity and healthier eating habits.13 Furthermore, improved control of modifiable risk factors in primary care, in patients with multiple risk factors, was shown to decrease cardiovascular events.14
The European Society of Cardiology (ESC) guideline on CVD prevention (2016) recommends performing a health check for CVD risk assessment in men above 40 years and in women above 50 years of age at least every five years.8 Given the longstanding and continuous relationship of patients with their general practitioner (GP) and the presence of up to date medical records,15 GPs have an unique opportunity to identify people at high risk for CMD among people without established CVD, and in assessing their eligibility for intervention.8 Different examples of health checks in primary care already exist for example in the United Kingdom (UK),16 Czech Republic17 and in the Netherlands.18 To be able to assess individuals' eligibility, however, it is important that people participate in health checks. The uptake of health checks in primary care varies widely, with response rates ranging from 1.2% for an online risk estimation19 to 84.1% for fasting plasma glucose measurement as screening for type 2 diabetes.20 To improve the uptake of health checks for CMD in primary care, we need to know what barriers and facilitators determine participation in health checks.
Primary care seems to be a promising setting for CMD health checks, therefore we will focus on this setting with a broad view on barriers and facilitators including both characteristics and reasons related with participation. So far, reviews did not select on characteristics and reasons related to participation just in primary care but in different settings.21,22
In this study we aim to identify characteristics and barriers and facilitators of people for participation in health checks for CMD in a primary healthcare setting.
Methods
Data collection
We performed a systematic search and review23 within the framework of the SPIMEU (Determinants of sucessful implementation of selective prevention of CMDs across Europe) project, which is a European Commission co-funded project and aims to identify determinants of successful implementation of selective prevention of CMD in primary care across Europe.24
The purpose of this review was explorative and aimed to provide a broad overview of barriers and facilitators for participation in health checks. Since a broad search, including all synonyms related to this subject, yielded more than 35,000 articles, we decided to apply a three-step method to search for articles using an iterative method described by Zwakman et al.25
As the first step we defined the research question and identified five key articles related to the aim of our review (e.g. about CMD, health checks or barriers and facilitators for participation).26–30 Step two consisted of a backward and forward citation search based on these five key articles. The backward citation search identified articles through the reference list of the key articles, and the forward citation search identified articles citing one of the key articles using Google Scholar. This yielded 30 articles (the ‘golden bullets’) which we used to identify important keywords and index terms to build the search including ‘barriers and facilitators’, ‘health check’, ‘cardiometabolic diseases’, ‘primary care’ and their synonyms.
Subsequently we used the search string based on the keywords from the golden bullets to search in Medline (Ovid), Embase (embase.com), Cinahl (Ebsco) and PubMed. This search strategy included both free-text and MeSH (Medical Subject Headings) terms, and was initially created in Medline and later adapted to the other databases with corresponding vocabularies. The searches were conducted by two librarians at the University Library at Karolinska Institute in March 2016. We performed a combined search for both barriers and facilitators for professionals and patients. The results regarding the professionals are reported elsewhere.31 The complete search strategies are available in Supplementary Material File 1.
In step three, all titles and abstracts were screened according to the eligibility criteria (see below) by either ACC, MJH or AKW using the screening program Rayyan.32 Selected articles were assessed for eligibility by at least two authors (PW, AKW, MJH or ACC).
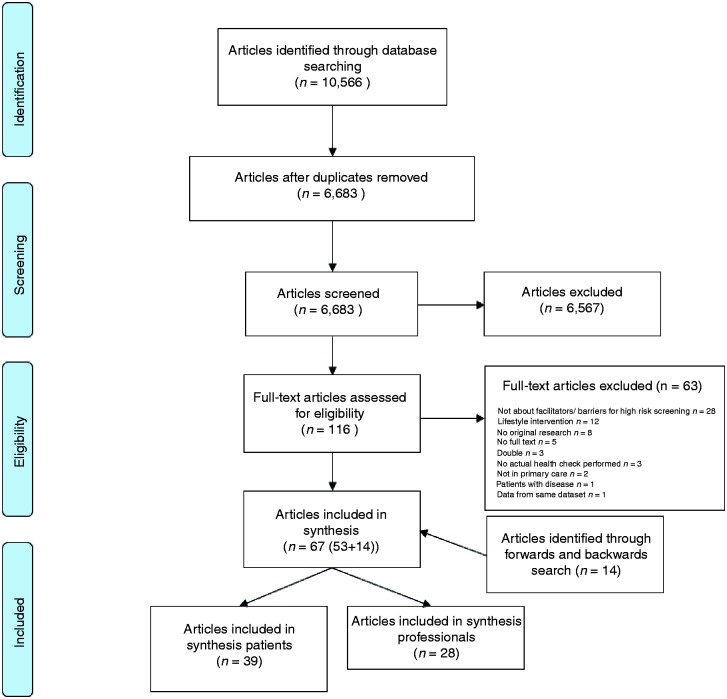
If there was any uncertainty as to whether particular articles should be included or not, they were discussed among the four authors that did the screening to reach a final decision based on the eligibility criteria. Reference lists of included articles were also searched and articles citing the already included studies were identified through Google Scholar searches until no new articles were identified anymore (Figure 1). Selected articles were assessed for inclusion based on full text by at least two authors (PW, AKW, MJH or ACC).
Figure 1.
Flow-chart of studies.
Eligibility criteria
We used the following eligibility criteria:
Thematic focus on prevention of cardiometabolic diseases.
Regarding adult people (18+) without established CMD, so all studies performed only in patients already diagnosed with cardiovascular disease (or taking medication for hypertension or dyslipidaemia), diabetes mellitus or chronic renal failure were excluded.
Performed in a primary care setting.
Data on barriers and facilitators to (not) participate in a health check.
Health check that started with an invitation for a health check for CMD (not hypothetical willingness to participate or intention to attend).
Original research (no opinion papers such as editorials).
Language: English, Swedish, German or Dutch.
We defined a health check as the first step in a prevention programme: inviting people for a risk assessment to identify people at high risk. A health check could be part of a prevention programme which, according to our definition, also includes the next step: interventions to decrease the risk in people who are identified in the health check as being at increased risk. In this current review, we only included information on barriers and facilitators to participation in the health check if possible. If information was given only about the whole prevention programme including the intervention then we used this information.
Assessment of study quality
Our review has an explorative nature and the intervention and outcome are heterogeneous. Furthermore, the research question can be answered using different study designs; quantitative, qualitative and mixed-methods studies could give insight in barriers and facilitators for participation. To our knowledge, no specific quality assessment instrument is available for this type or review. Therefore, we decided to limit the quality assessment to two criteria: (a) adequate number of participants: at least 100 participants and (b) control group comparison: studies directly comparing participants with non-participants. We used these criteria separately to see whether the identified barriers and facilitators changed when only good quality studies were considered compared to all studies.
Data analysis
Data extraction from the articles was performed by AKW. The identified papers included were heterogeneous in design (qualitative and quantitative), in population (from different contexts) and in facilitators and barriers described. We therefore decided to use a more narrative synthesis approach which has been used in previous research.21,22
To structure the data we divided the results into four different themes: (a) personal characteristics; (b) attitude towards the outcome of health checks and prevention in general; (c) practical issues; and (d) barriers and facilitators for people related with the healthcare provider. Part of this structure was derived from the study of Burgess et al.33 and adapted based on the results from the articles included in our review.
We then categorised factors into (a) barriers; (b) facilitators; or (c) neutral, the latter meaning that the factor was studied, but was not identified in the study as a barrier or facilitator. To target the most commonly reported findings in the articles, we decided to pay attention in the text to factors only reported in more than 10 articles and which were identified as a barrier or facilitator in at least two-thirds (67%) of these articles.
Since the studies reported their findings in a different manner, we used the following criteria to be able to report the results in this review in a uniform way. In the studies with a direct comparison between participants and non-participants, factors which significantly differed between these groups were included in the tables. If a multivariable analysis was performed then the results of this analysis were used. If no significance level was reported, we included the factors with an absolute difference between the group of attenders and non-attenders of 5% or more. If this was not reached, we described the factor as neutral. In studies which only described one group, either participants or non-participants, the factors which were indicated as facilitators or barriers in 5% or more of the studied population were reported. We chose this low percentage because we did not want to miss a potential barrier or facilitator.
Some health checks consisted of several steps: for example, an online health risk assessment as the first step and a complete risk assessment as the second step.20 We chose to report the barriers and facilitators for both these steps, since they are both part of the health check.
Results
Study selection and study characteristics
In total, the search identified 6683 unique articles of which titles and abstracts were screened.
After screening for eligibility and quality, 40 articles remained. Two articles described the results based on the same dataset.34,35 We included only one of the two studies34 which directly compared non-attenders with attenders. The flowchart is shown in Figure 1 and the characteristics of the 39 included studies are summarised in Tables 1–3. The included articles were published between 1988–2016. Twenty-six studies (67%) were conducted in the United Kingdom (UK), of which 10 reported barriers and facilitators about the National Health Service (NHS) health check, which is a health check for people aged 40–74 years in the UK.16 The other studies were from the Netherlands (five), Denmark (three), Sweden (three), China (one) and Germany (one).
Table 1.
Characteristics of studies describing attenders of health checks of cardiometabolic diseases in primary care.
| Year | First author | Country, programme | Number of participants (P) | Inclusion (in) and exclusion (ex) | Method | |
|---|---|---|---|---|---|---|
| 62 | 1991 | Norman | UK | P: 159 | In: age 30–50 years | Questionnaire about views health check and way of invitation Semi-structured interview (n = 11) |
| 46 | 1994 | Ochera | UK | P: 1712 | In: age 30–65 years, part had health check <12 months, part randomly selected Ex: patients who had moved or died | Registry data and questionnaire |
| 67 | 2010 | Harkins | UK, HaHP | P: 13 | In: age 45–60 years, registered with a GP, socio-economically disadvantaged people who attended follow-up after 6 months Ex: history of heart disease | Focus group discussions |
| 70 | 2012 | Hardy | UK, PhyHWell | P: 5 | In: age: 25, 47, 48, 52, 76 years Severe mental illness (bipolar disorder, schizophrenia) | Interview |
| 64 | 2014 | Baker | UK, NHS health check | P: 1011 | In: age 40–74 years | Survey with quantitative and qualitative (open-ended) questions |
| 29 | 2015 | Ismail | UK, NHS health check | P: 45 baseline, 38 follow-up | In: age 40–74 years | Semi-structured qualitative interviews + 1 year follow up interview |
| 36 | 2015 | Ligthart | The Netherlands, pre-DIVA trial | P: 15 | In: age 76–82 years Ex: dementia or conditions likely to hinder successful follow-up | Semi-structured interviews |
| 65 | 2015 | Riley | UK, NHS health check | P: 28 | In: age 40–74 years Patients who attended <6 months Ex: existing CVD | Semi-structured interviews |
| 68 | 2015 | Zhong | China, Dutch- Chinese prevention consultation | Unknown | In: age>35 years | Questionnaire |
| 49 | 2016 | Robson | UK, NHS health check | P: 214295 (2009–2012) | In: age 40–74 years Ex: pre-existing vascular disease | Registry data |
CVD: cardiovascular disease; GP: general practitioner; HaHP: Have a Heart Paisley; NHS: National Health Service; pre-DIVA: prevention of dementia by intensive vascular care; UK: United Kingdom.
Table 2.
Characteristics of studies describing non-attenders of health checks of cardiometabolic diseases in primary care.
| Year | First author | Country, programme | Number of non-participants (NP) | Inclusion (in) and exclusion (ex) | Method | |
|---|---|---|---|---|---|---|
| 58 | 1988 | Pill (The views) | UK | NP: 259 | In: age 20–45 years | Semi-structured interview |
| 59 | 2004 study 1991 | Nielsen | Denmark | NP: 18 | In: age 30–50 years | Guided qualitative interview |
| 60 | 2015 | Ellis | UK, NHS health check | NP: 41 | In: age 40–74 years | Semi-structured interviews |
NHS: National Health Service; NP: non-participant; UK: United Kingdom.
Table 3.
Characteristics of studies describing attenders compared to non-attenders of health checks of cardiometabolic diseases in primary care.
| Year | First author | Country, programme | Number of participants (P), non-participants (NP) | Inclusion (in) and exclusion (ex) | Method | |
|---|---|---|---|---|---|---|
| 38 | 1988 | Pill (comparison) | UK | P: 216 NP: 259 | In: age 20–45 years | Questionnaire using semi-structured interview |
| 48 | 1990 | Waller | UK | P: 963, NP: 495 | In: age 35–64 years | Medical record audit and questionnaire |
| 39 | 1993 | Jones | UK | P: 2,402, NP: 98 | In: age 25–55 years, patients with and without a history of CHD. | Questionnaire and health data |
| 66 | 1993 | Norman | UK | P/NP: 150 | In: middle aged | Health belief questionnaires before invitation |
| 40 | 1993 | Thorogood | UK | P: 2205, NP: 473 | In: age 35–64 years, also patients with angina and MI included | Postal health belief questionnaire before invitation to health check |
| 55 | 1994 | Davies | UK British Family Heart Study | P: 2315 NP:141 | Age 40–59 years | Questionnaire |
| 41 | 1994 | Griffiths | UK | P: 113, NP: 137 | In: age>16 years | Questionnaire |
| 34 | 1995 | Christensen | Denmark | P: 1272, NP: 423 | In: age 40–49 years, men | Questionnaire |
| 42 | 1997 | Weinehall | Sweden, Västerbotten program | P: 14,188 NP: 10,682 | In: age 30, 40, 50 or 60 years | Registry data |
| 43 | 2004 | Wall | Sweden, Ockelbo project | P: 237, NP: 67 | In: age 35 or 40 years | Questionnaire or telephone interview (with non responders questionnaire) |
| 44 | 2009 | Dalsgaard | Denmark, ADDITION study | P: 879, NP: 1100 | In: age 40–69 years with high-risk score Ex: known diabetes | Questionnaire + registry data |
| 52 | 2010 | Marteau | UK, DICISION trial | P: 721, NP: 551 | In: age 40–69 years, at risk for diabetes (risk score practice registers) Many were obese or used anti-hypertensive drugs Ex: known diabetes | Questionnaire (willingness to change lifestyle) |
| 50 | 2011 | Dalton | UK, NHS health check | P: 2370, NP: 2924 | In: age 35–74 years with >20% 10-year risk on CVD (GP records) incl. people with hypertension or using statins Ex: CVD (CHD, stroke/TIA) or diabetes | Electronic medical record |
| 69 | 2012 | Eborall | UK, MY-WAIST | P: 13 NP: 84 | In: age 40–70 years (30–70 South Asian and African-Caribbean origin) | Semi-structured interviews or reply slip with open-ended questions |
| 20 | 2012 | Klijs | The Netherlands | P: 4457, NP: 848 | In: age 40–74 years, self-measured waist circumference ≥80 cm (women) ≥84 cm (men) Ex: known diabetes | Registry data |
| 56 | 2011 | Lambert | UK, deadly trio-programme | P: 5871, NP: 18,295 | In: age >40 years, men from Birmingham inner city Ex: already in a disease register | Routine data |
| 37 | 2012 | Norberg | Sweden, Västerbotten | P: 96,560 observations NP: 61,622 observations | In: 40th, 50th, and 60th birthdays, all inhabitants | Registry data |
| 19 | 2013 | Van der Meer | The Netherlands | P: 617 NP: 142 | In: age 45–70 years | Registry data, questionnaire |
| 33 | 2014 | Burgess | UK, NHS health check | P: 17, NP: 10 | In: age 40–74 years, invited for NHS health check Ex: already in care-path, did not receive invitation for health check | Semi-structured interviews |
| 47 | 2014 | Hoebel | Germany, GEDA study | P: 13,328 NP: 13,227 | In: age >35 years, respondents with statutory health insurance | GEDA = national telephone health interview survey |
| 51 | 2015 | Attwood | UK, NHS | P: 373, NP: 1007 | In: age 40–74 years | Registry data |
| 53 | 2015 | Groenenberg (Response) | The Netherlands | Step 1 HRA P: 308, NP: 440 Step 2 Prev. c. P: 123, NP: 84 | In: age 45–70 years (35 for Hindustani and Surinamese) | Electronic medical record |
| 61 | 2015 | Jenkinson | UK, NHS health check | P: 17, NP: 10 | In: age 40–74 years, invited for NHS health check | Semi-structured interviews |
| 54 | 2014 | Krska | UK, NHS health check | P: 434, NP: 210 | In: age 40–74 years, people with estimated risk on CVD > 20% from medical records | Cross-sectional postal survey |
| 45 | 2016 | Groenenberg (Determinants) | The Netherlands | HRA P: 696, NP: 196 | In: age 45–70 years and low SES | Questionnaire |
| 57 | 2016 | Lang | UK | P: 2339 NP: 3127 | In: age 50–74 years, no CVD diagnosis | Primary care electronic health records |
CHD: coronary heart disease; CVD: cardiovascular disease; GEDA: German Health Update; HRA: health risk assessment; MI: myocardial infarction; NHS: National Health Service; NP: non-participant; P: participant; Prev c.: Prevention consultation; SES: socio-economic status; TIA: Transient ischemic attack; UK: United Kingdom.
Almost all studies included people in the age range between 30–75 years, except for one study from the Netherlands which focused on elderly people between 76–82 years of age.36 Attendance rates for health checks ranged from 1.2%19 to 84.1%.20 Quantitative methods for data collection were used in 27 studies, (e.g. questionnaire and registry data), qualitative methods were used in 11 studies (e.g. focus groups and semi-structured interviews) and one study used both quantitative and qualitative methods for data collection.
Barriers and facilitators
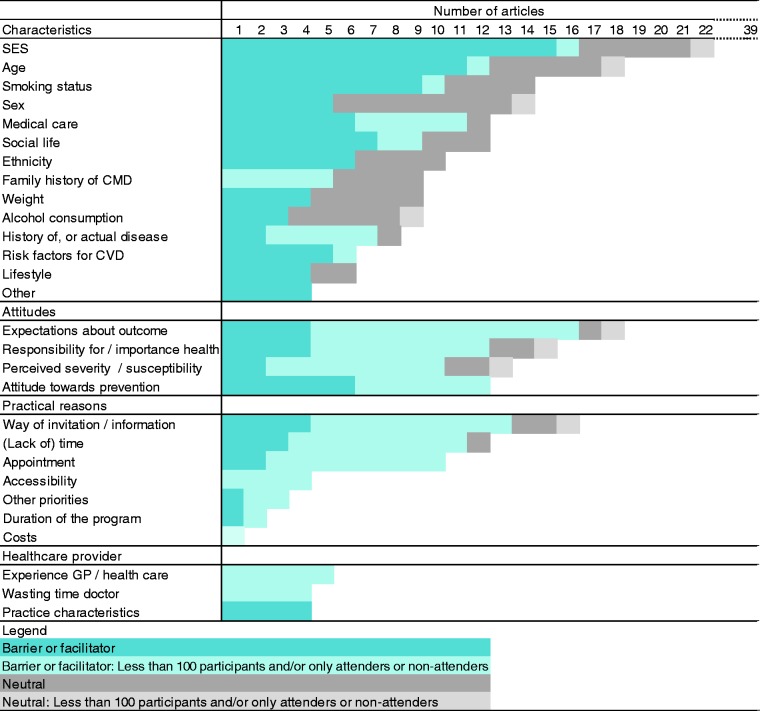
The factors related to participation (facilitators), non-participation (barriers) and neutral factors are summarised in Figure 2, more detailed results can be found in Supplementary Material Files 2(a) and (b).
Figure 2.
Barriers and facilitators for people to participate in a health check for cardiometabolic disease (CMD). CVD: cardiovascular disease; GP: general practitioner; SES: socioeconomic status.
Personal characteristics
Socio-economic status (SES), age, social life, smoking status, and receiving medical care were studied more than 10 times and were reported in at least two-thirds of the studies as a barrier or facilitator (Figure 2). In total, 22 (56%) of the studies reported about SES, of which 16 (73%) reported it as a barrier or facilitator (Figure 2). Different characteristics were classified as SES: educational level, occupation, income level and ownership of a house or car. Low educational level was reported as a barrier in one study37 and middle or higher educational level was a facilitator in two studies.37,38 However in eight studies education was neither a facilitator nor a barrier.19,20,39–44 Overall, low SES was reported to be both a barrier and a facilitator,45,46 and higher SES to be a facilitator.47
In total, 18 studies (46%) reported about age, of which 12 (67%) reported it as a barrier or facilitator. Higher age was a barrier in one study39 and a facilitator in six studies,20,44,48–51 and lower age was a barrier in four studies.37,42,50,52 In six studies, age was neither barrier nor facilitator (Supplementary Material File 2).19,38,40,41,53,54
Smoking status was reported in 14 studies (36%), of which 10 (71%) reported it as barrier or facilitator. Smoking was a barrier for participation and not smoking was a facilitator in 10 studies.20,40,41,43,47–49,55–57 Smoking was a neutral factor in five studies.19,39,50,54,55
Receiving medical care was a barrier or facilitator in 11 out of 12 studies (92%). Being under medical care, or being recently examined, were reported as a barrier for participation in six studies.39,43,44,58–61 In contrast, frequently consulting a doctor was described as a facilitator in four studies38,40,47,48,62 and as a neutral factor in one study.19
Factors related to social life were a barrier or facilitator in nine out of 12 studies (36%). Being single, unmarried or being responsible for a young child (<5 years) or other dependants were reported as barriers in four studies.37,40,41,58 Being married or cohabitating, having no responsibility for young children or dependants and strong social support were reported as facilitators.20,34,38,47,48
Attitudes
Attitude towards the outcome of the health check, the feeling of being responsible for one’s own health, perceived severity and susceptibility, and attitudes towards prevention in general were studied more than 10 times and were reported in at least two-thirds of the studies as a barrier or facilitator. Perceived severity was defined as ‘an individual’s belief about the seriousness of the threat’ and perceived susceptibility as ‘individual’s beliefs about his or her chances of experiencing the threat’.63
In total 18 studies (46%) reported about the attitude towards the outcome of the health check. Barriers were not wanting to know CMD risk19,33,59 and being worried about the outcome of the check and its possible consequences.39,58–61 On the other hand, wanting to know CMD risk,45 wanting to be reassured,29,33,36,58,61,64,65 and not having fear for the outcome36,58 were facilitators.
In total 14 studies (36%) reported about feelings of responsibility towards one’s own health. Facilitators for participation were: feeling responsible for one’s own health, finding health important or believing to be able to influence one’s health status.29,34,38,40,45,66 Factors related with susceptibility and severity of disease were reported in 13 studies (33%). Barriers for participation were experiencing less severity or susceptibility of disease or feeling healthy,33,39,43,58,60,67–69 whereas concerns about health were facilitating for participation.64 The attitude of people towards prevention or towards health checks was reported in 12 studies (31%). In general a negative attitude towards prevention or health checks was a barrier for participation,45,54,59 whereas a positive attitude was a facilitator33,60,65,66,70 or a neutral factor.54
Practical reasons
The practical reasons that were studied more than 10 times and reported as barrier or facilitator in at least two-thirds of the studies were: the kind of invitation and information provision, time constraints and appointment related issues.
In total, 17 studies (44%) described factors related with the kind of invitation and information for a health check of which 14 (82%) described this as a barrier or facilitator. Not receiving the invitation38,39,61,67,68 and not being familiar with the health check19,33 were identified as barriers. Clear information about the health check,29,67 an invitation by the GP or health centre36,68 and additional effort for invitation such as an additional phone call after the invitation,45 or the use of outreach workers,67 were identified as facilitators.
A barrier was lack of time, including being busy with, for example, work or family.19,33,43,45,58–61,67,69 Being retired and working flexible hours were identified as facilitators in one study.33 Difficulties with arranging the appointment, for example no time slot available outside working hours,60 were identified as barriers, whereas health checks with no appointment needed and easy access were identified as facilitators.62,67,68
Healthcare provider–related factors
Barriers and facilitators for people related to their healthcare provider were not often described. All factors within this category, such as experience with the GP (five studies) and practice characteristics (four studies), were described less than 10 times, so less often than the minimum number we reported on.
Quality assessment
In total 28 articles (72%) reported results based on studies with more than 100 participants. These studies were all quantitative studies. Focus on these studies alone did not change the results within the category of personal characteristics and factors that were identified both as barriers and facilitators were comparable. Attitudes and practical issues were less often described in the studies with more than 100 participants. In total, 26 studies (67%) directly compared participants and non-participants. These studies were mostly quantitative studies and only including these studies did not change the results within the category of personal characteristics. Attitudes and practical issues were less often described in studies with direct comparison of participants and non-participants. In Figure 2 and Supplementary Material File 2(a), the studies that were still included after applying both the quality criteria are shown in darker colours (Figure 2) and in bold (Supplementary Material File 2(a)).
Discussion
Summary of the results
Barriers and facilitators for people to participate or not in health checks for CMD in primary care are heterogeneous. Lower age, lower education, smoking and living alone seemed to be barriers for participation but the results were not univocal. Wanting to know one’s CMD risk (reassurance), feeling responsible for one’s own health and concerns about health were facilitators for participation, whereas not wanting to know the risk, being worried about the outcome, feeling healthy, or low perceived severity or susceptibility of disease were barriers. Furthermore, practical issues for people to participate, such as the kind of invitation to the health check, providing sufficient information, requested time investment for the participants and possibilities for easy appointment play an important role in the acceptance. Overall, we conclude that for a good uptake of health checks, a multifactorial approach is necessary.
Discussion in the light of the literature
The characteristics and reasons to (or not to) participate in CVD health checks in different settings were previously explored in two reviews.21,22 Dryden et al. identified several characteristics and attitudes of people that were related to non-participation. Non-participants were, for example, more often men, had a lower income or SES, were younger, single, smokers and had more cardiovascular risk factors. Furthermore, they felt less in control over their health, valued health less strongly and were less likely to believe in the efficacy of health checks.21
Stol et al. focused more on the reasons for participation in cardiovascular health checks. They identified a broad range of reasons for participation, which were related to health improvement, for example, wanting to know health status, health monitoring, for example, reassurance and practical issues such as a convenient location with wide opening times. On the other hand, they also identified reasons for non-participation which were also related to health improvement, for example, feeling healthy and considering risk as low. Furthermore having no faith in screening, and not wanting to know the outcome of the health check, practical issues such as lack of time and lack of knowledge and poor accessibility were reasons for non-participation. The reasons for (non-)participation were comparable to our findings which could be partly due to some overlap of the included articles (11/39 overlapping articles), although our study was focused on primary care.
We expected that we would be able to find personal characteristics that would be specific for participation in a health check for CMD. From the literature we know that people with the largest need for medical care are the least likely to receive it, which is known as the ‘inverse care law’.71 Furthermore, women receive less satisfactory preventative management than men, especially when the GP is a man.72 Also people with a lower SES are less likely to receive preventive care.73 This was confirmed by the review of Dryden et al.: the people at higher risk for CVD were less likely to participate in a health check21 and health checks are more likely to serve the ‘worried well’. Our review did partly confirm these results. Smoking, lower education and a higher age seemed to hamper participation. However, these factors were not unanimously identified as barriers.
Given the longstanding and continuous relationship of patients with their GP and the presence of up to date medical records,15 GPs have a unique opportunity to identify people at high risk for CMD among people without established CVD, and to assess their eligibility for intervention.8 Therefore our review focused on health checks performed in primary care. In practice, however, it is not necessarily the GP him/herself that performs all tasks in the health check. For example, in the Västerbotten programme people were invited to their primary healthcare centre, but the district nurse played a crucial role in the actual execution of the tasks in the health check.37 Also in the NHS Health Check the programme is largely delivered by nurses.74
Strengths and limitations
A strength of our study is that we were able to identify multiple articles on the subject using a rigorous search, including a backward and forward citation search until no further studies were identified. We believe that this scrutiny was sufficient and that no relevant articles were missed. Furthermore, we were able to collect multiple articles regarding health checks focused specifically on the situation in primary care and general practice. This review gives a broad overview of different categories of barriers and facilitators for participation, including a clear overview about the factors that have been studied and have been most frequently identified as a facilitator or a barrier.
The studies that we included in this review were very heterogeneous as well as the outcome measure ‘barriers and facilitators’. We ended up with a broad range of results which were difficult to quantify, count or summarise. Therefore, we decided to only report the factors that were studied more than 10 times and reported barriers or facilitators in more than two-thirds of the studies. Furthermore, we decided to include factors that were significant, or if no significance level was reported, we included the factors with an absolute difference between the group of attenders and non-attenders of 5% or more. We do realise that this is not optimal, since significance also relates to the power of the study, and not merely with the strength of the effect. However, in this way we were able to use a consistent method for data extraction from the mix of qualitative and quantitative studies that we included in the review. These were both pragmatic decisions, and other options for reporting could also be considered. However, since the results were diverse and we did not find factors that were consistently identified as a barrier or a facilitator, we expect that the results will not change drastically when other methods for describing the results would have been applied.
Our review had a descriptive aim, which was to provide an overview about barriers and facilitators. Therefore we did not want to narrow down the described intervention and outcome, as is usually done in systematic reviews, for example when using a PICO (Patient, Intervention, Comparison, Outcome) method to describe a study. Methodologically, we were not able to find a validated instrument to assess the risk of bias or study quality for the studies included in this review. As we have noted, the studies were very heterogeneous and each study reported multiple outcomes in both quantitative and qualitative ways. We applied two criteria to the studies which, in our view, selected the studies with more robust results. We acknowledge that individual studies that we included have several types of bias, and that the bias of each included study might influence the validity of reported barriers and facilitators. However, we believe that if a barrier of facilitator is frequently reported, and reported in studies which included more participants, the likelihood of it being valid is greater.
Most of the studies in our review (26 out of 39 studies in total) were from the UK. In the UK, the GP has a strong position in the healthcare system, including a gatekeeper role.75 The other studies were mainly from the Netherlands, and Denmark in which the GP also has a strong position, and primary healthcare is mostly reimbursed for the patient. One study from Denmark showed that the attendance rate for a health check was much higher when it was offered for free compared with costs of around US$40.35 Overall, costs did not seem to be an important barrier for participation in the studies included in this review, which may be due to the fact that most studies reported on the NHS Health Check, which is fully reimbursed by the government for the patient.
Three studies were conducted in Sweden, where the GP has a somewhat weaker position. Therefore, our results may not be generalisable to other, especially non-Western countries with different (primary) healthcare systems and a less strong position of the GP. Furthermore, it may be less generalisable to countries where people have to pay for the health check, however, based on our review it is not possible to draw firm conclusions about this.
Clinical impact of this study
The overview of barriers and facilitators in this systematic review could be used for future development of selective prevention programmes for CMD in primary care. To improve uptake, attention could be paid to different aspects, as described in this review such as personal characteristics, attitude and practical aspects. First of all, special attention could be paid to people who are less motivated to participate, such as smokers, younger people and people with a lower level of education. Secondly, uptake of health checks might be improved by providing good information to the people about the aims and benefits of the health check, and making them aware of their possible risk to develop disease. Third the organisation of the health check could be performed in such a way that makes it as easy as possible for people to participate. For example, a clear invitation that actually reaches the people, a location that is easy to reach and easy access to appointments. By improving the uptake for health checks, especially the people at high risk, interventions could be started to decrease their risk.
Since healthcare systems differ between countries, and the organisation of health checks such as inviting people usually takes place on a local level, we suggest the adaptation of the planning of the health check to the national situation and the actual implementation to the local situation.
Conclusion
The barriers and facilitators for people to participate in health checks for CMD are very heterogeneous. Hence, it is not possible to develop a ‘one size fits all’ approach for CMD health checks. Personal characteristics, practical reasons and attitudes of people towards prevention and health checks should be taken into account to improve the uptake of health checks for CMD in primary care. For the development and implementation of CMD health checks, we suggest a multifactorial approach and take into account both the national and local context. To increase uptake for health checks, special attention should be paid to groups of people that might be harder to reach, such as those with low SES, smokers and people with a negative attitude towards health checks and prevention. Increasing the uptake of health checks could contribute to identifying the people who are at risk for CMD to be able to start interventions to decrease their risk.
Supplemental Material
Supplemental material for Barriers and facilitators to participation in a health check for cardiometabolic diseases in primary care: A systematic review by Anne-Karien M de Waard, Per E Wändell, Martin J Holzmann, Joke C Korevaar, Monika Hollander, Carl Gornitzki, Niek J de Wit, François G Schellevis, Christos Lionis, Jens Søndergaard, Bohumil Seifert, Axel C Carlsson and on behalf of the SPIMEU Research Group in European Journal of Preventive Cardiology
Acknowledgements
The authors would like to thank René Spijker for his contribution to the iterative search method.
SPIMEU project group collaborators
The SPIMEU research group includes: Anne-Karien M de Waard, Per E Wändell, Martin J Holzmann, Joke C Korevaar, Monika Hollander, Carl Gornitzki, Niek J de Wit, François G Schellevis, Christos Lionis, Jens Sondergaard, Bohumil Seifert, Axel C Carlsson, Norbert Král, Anders Sonderlund and Agapi Angelaki.
Author contribution
AKW, PW, MJH, JCK, MH and ACC contributed to conception, design, analysis, interpretation and drafting the manuscript. CL, NJW, FGS, JS, BS, NK, AS and AA contributed to conception. CG contributed to the analysis. All authors critically revised the manuscript and gave final approval.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This review is part of the project/joint action ‘663309/SPIM EU’ which has received funding from the European Union’s Health Programme (2014–2020). The content of this review represents the views of the authors only and is their sole responsibility; it can not be considered to reflect the views of the European Commission and/or the Consumers, Health, Agriculture and Food Executive Agency or any other body of the European Union. The European Commission and the Agency do not accept any responsibility for use that may be made of the information it contains.
References
- 1.World Health Organization (WHO). Cardiovascular diseases, http://www.who.int/mediacentre/factsheets/fs317/en/ (2016, accessed 24 February 2017).
- 2.James WP. The epidemiology of obesity: The size of the problem. J Intern Med 2008; 263: 336–352. [DOI] [PubMed] [Google Scholar]
- 3.Yusuf S, Reddy S, Ounpuu S, et al. Global burden of cardiovascular diseases: Part I: General considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 2001; 104: 2746–2753. [DOI] [PubMed] [Google Scholar]
- 4.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010; 87: 4–14. [DOI] [PubMed] [Google Scholar]
- 5.Deaton C, Froelicher ES, Wu LH, et al. The global burden of cardiovascular disease. Eur J Cardiovasc Nurs 2011; 10: S5–S13. [DOI] [PubMed] [Google Scholar]
- 6.WHO. Obesity and overweight, http://www.who.int/mediacentre/factsheets/fs311/en/ (2017, accessed 8 November 2017).
- 7.WHO. World population ageing 1950–2050, http://www.un.org/esa/population/publications/worldageing19502050/ (2002, accessed 24 February 2017).
- 8.Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016; 23: NP1–NP96. [DOI] [PubMed] [Google Scholar]
- 9.Mrazek PJ, Haggerty RJ, eds Institute of Medicine. 1994. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research, Washington, DC: National Academies Press, 1994. DOI: 10.17226/2139. [DOI] [PubMed] [Google Scholar]
- 10.Krogsboll LT, Jorgensen KJ, Gronhoj Larsen C, et al. General health checks in adults for reducing morbidity and mortality from disease. Cochrane Database Syst Rev. 2012; 10: CD009009. [DOI] [PubMed] [Google Scholar]
- 11.Jorgensen T, Jacobsen RK, Toft U, et al. Effect of screening and lifestyle counselling on incidence of ischaemic heart disease in general population: Inter99 randomised trial. BMJ. 2014. DOI: 10.1136/bmj.g3617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Si S, Moss JR, Sullivan TR, et al. Effectiveness of general practice-based health checks: A systematic review and meta-analysis. Br J Gen Pract 2014; 64: e47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van den Brekel-Dijkstra K, Rengers AH, Niessen MA, et al. Personalized prevention approach with use of a web-based cardiovascular risk assessment with tailored lifestyle follow-up in primary care practice - a pilot study. Eur J Prev Cardiol. 2015. DOI: 2047487315591441. [DOI] [PubMed] [Google Scholar]
- 14.Avanzini F, Marzona I, Baviera M, et al. Improving cardiovascular prevention in general practice: Results of a comprehensive personalized strategy in subjects at high risk. Eur J Prev Cardiol. 2016. DOI: 10.1177/2047487315613664. [DOI] [PubMed] [Google Scholar]
- 15.WHO Regional Office for Europe. Action plan for implementation of the European Strategy for the Prevention and Control of Noncommunicable Diseases 2012−2016, http://www.euro.who.int/en/publications/abstracts/action-plan-for-implementation-of-the-european-strategy-for-the-prevention-and-control-of-noncommunicable-diseases-20122016 (2012, accessed 24 February 2017).
- 16.NHS Choices. What is an NHS health check?, http://www.nhs.uk/Conditions/nhs-health-check/Pages/NHS-Health-Check.aspx (2016, accessed 3 October 2017).
- 17.Všeobecná zdravotní pojišťovna [general health insurance company]. Všeobecná preventivní prohlídka [General preventive surveillance], https://www.vzp.cz/pojistenci/prevence/preventivni-prohlidky/vseobecna-preventivni-prohlidka (accessed 3 October 2017).
- 18.Dekker JM, Alssema M, Janssen PGH, et al. The prevention consultation, cardiometabolic risk module. Huisarts en wetenschap 2011; 54: 138.
- 19.Van der Meer V, Nielen MM, Drenthen AJ, et al. Cardiometabolic prevention consultation in the Netherlands: Screening uptake and detection of cardiometabolic risk factors and diseases–a pilot study. BMC Fam Pract 2013; 14: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Klijs B, Otto SJ, Heine RJ, et al. Screening for type 2 diabetes in a high-risk population: Study design and feasibility of a population-based randomized controlled trial. BMC Public Health 2012. 12: 671. DOI: 10.1186/1471-2458-12-671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dryden R, Williams B, McCowan C, et al. What do we know about who does and does not attend general health checks? Findings from a narrative scoping review. BMC Public Health 2012; 12: 723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stol YH, Asscher EC, Schermer MH. Reasons to participate or not to participate in cardiovascular health checks: A review of the literature. Public Health Ethics 2015; 9: 301–311. [Google Scholar]
- 23.Grant MJ, Booth A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Info Libr J 2009; 26: 91–108. [DOI] [PubMed] [Google Scholar]
- 24.SPIMEU Research Team. Website SPIMEU project, www.spimeu.org (2017, accessed 04 2017).
- 25.Zwakman M, Verberne LM, Kars MC, et al. Introducing PALETTE: an iterative method for conducting a literature search for a review in palliative care. BMC Palliat Care 2018; 17: 82. [DOI] [PMC free article] [PubMed]
- 26.Godefrooij M, Spigt M, van der Minne W, et al. Implementing cardiometabolic health checks in general practice: A qualitative process evaluation. BMC Fam Pract 2014; 15: 132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ismail H, Kelly S. Lessons learned from England’s Health Checks Programme: Using qualitative research to identify and share best practice. BMC Fam Pract 2015; 16: 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Naslund GK, Fredrikson M, Hellenius ML, et al. Characteristics of participating and nonparticipating men in a randomized, controlled diet and exercise intervention trial. Scand J Prim Health Care 1994; 12: 249–254. [DOI] [PubMed] [Google Scholar]
- 29.Ismail H, Atkin K. The NHS Health Check programme: Insights from a qualitative study of patients. Health Expect 2016. DOI: 10.1111/hex.12358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koopmans B, Fau NM, Fau SF, et al. Non-participation in population-based disease prevention programs in general practice. BMC Public Health 2012; 12: 856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wandell PE, de Waard AM, Holzmann MJ, et al. Barriers and facilitators among health professionals in primary care to prevention of cardiometabolic diseases: A systematic review. Fam Pract 2018. DOI: 10.1093/fampra/cmx137. [DOI] [PubMed] [Google Scholar]
- 32.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan–a web and mobile app for systematic reviews. Syst Rev 2016. DOI: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burgess C, Wright AJ, Forster AS, et al. Influences on individuals’ decisions to take up the offer of a health check: A qualitative study. Health Expect. 2015. DOI: 10.1111/hex.12212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Christensen B. Characteristics of attenders and non-attenders at health examinations for ischaemic heart disease in general practice. Scand J Prim Health Care 1995; 13: 26–31. [DOI] [PubMed] [Google Scholar]
- 35.Christensen B. Payment and attendance at general practice preventive health examinations. Fam Med 1995; 27: 531–534. [PubMed] [Google Scholar]
- 36.Ligthart SA, van den Eerenbeemt KD, Pols J, et al. Perspectives of older people engaging in nurse-led cardiovascular prevention programmes: A qualitative study in primary care in the Netherlands. Br J Gen Pract. 2015; 65: e41–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Norberg M, Blomstedt Y, Lonnberg G, et al. Community participation and sustainability – evidence over 25 years in the Vasterbotten Intervention Programme. Glob Health Action. 2012; 5: 19166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pill R, French J, Harding K, et al. Invitation to attend a health check in a general practice setting: Comparison of attenders and non-attenders. J R Coll Gen Pract 1988; 38: 53–56. [PMC free article] [PubMed] [Google Scholar]
- 39.Jones A, Cronin PA, Bowen M. Comparison of risk factors for coronary heart disease among attenders and non-attenders at a screening programme. Br J Gen Pract 1993; 43: 375–377. [PMC free article] [PubMed] [Google Scholar]
- 40.Thorogood M, Coulter A, Jones L, et al. Factors affecting response to an invitation to attend for a health check. J Epidemiol Community Health 1993; 4: 224–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Griffiths C, Cooke S, Toon P. Registration health checks: Inverse care in the inner city? Br J Gen Pract 1994; 44: 201–204. [PMC free article] [PubMed] [Google Scholar]
- 42.Weinehall L, Hallgren CG, Westman G, et al. Reduction of selection bias in primary prevention of cardiovascular disease through involvement of primary health care. Scand J Prim Health Care 1998; 16: 171. [DOI] [PubMed] [Google Scholar]
- 43.Wall M, Teeland L. Non-participants in a preventive health examination for cardiovascular disease: Characteristics, reasons for non-participation, and willingness to participate in the future. Scand J Prim Health Care 2004; 22: 248–251. [DOI] [PubMed] [Google Scholar]
- 44.Dalsgaard E, Lauritzen T, Christiansen T, et al. Socioeconomic factors related to attendance at a Type 2 diabetes screening programme. Diabetic Med 2009; 26: 518–525. [DOI] [PubMed] [Google Scholar]
- 45.Groenenberg I, Crone MR, van Dijk S, et al. Determinants of participation in a cardiometabolic health check among underserved groups. Prev Med Rep. 2016; 4: 33–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ochera J, Hilton S, Bland JM, et al. Patients’ experiences of health checks in general practice: A sample survey. Fam Pract 1994; 11: 26–34. [DOI] [PubMed] [Google Scholar]
- 47.Hoebel J, Starker A, Jordan S, et al. Determinants of health check attendance in adults: Findings from the cross-sectional German Health Update (GEDA) study. BMC Public Health 2014; 14: 913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Waller D, Agass M, Mant D, et al. Health checks in general practice: Another example of inverse care? BMJ 1990; 300: 1115–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Robson J, Dostal I, Sheikh A, et al. The NHS Health Check in England: An evaluation of the first 4 years. BMJ Open. 2016; 6: e008840. DOI: 10.1136/bmjopen-2015-008840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dalton AR, Bottle A, Okoro C, et al. Uptake of the NHS Health Checks programme in a deprived, culturally diverse setting: Cross-sectional study. J Public Health (Oxf). 2011; 33: 422–429. [DOI] [PubMed] [Google Scholar]
- 51.Attwood S, Morton K, Sutton S. Exploring equity in uptake of the NHS Health Check and a nested physical activity intervention trial. J Public Health (Oxf) 2016; 38: 560–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Marteau TM, Mann E, Prevost AT, et al. Impact of an informed choice invitation on uptake of screening for diabetes in primary care (DICISION): Randomised trial. BMJ. 2010; 340: c2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Groenenberg I, Crone MR, van Dijk S, et al. Response and participation of underserved populations after a three-step invitation strategy for a cardiometabolic health check. BMC Public Health. 2015; 15: 854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Krska J, du Plessis R, Chellaswamy H. Views and experiences of the NHS Health Check provided by general medical practices: Cross-sectional survey in high-risk patients. J Public Health (Oxf). 2015; 37: 210–217. [DOI] [PubMed] [Google Scholar]
- 55.Davies G, Pyke S, Kinmonth AL. Effect of non-attenders on the potential of a primary care programme to reduce cardiovascular risk in the population. Family Heart Study Group. BMJ 1994; 309: 1553–1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lambert AM, Burden AC, Chambers J, et al. Cardiovascular screening for men at high risk in Heart of Birmingham Teaching Primary Care Trust: The ‘Deadly Trio’ programme. J Public Health (Oxf). 2012; 34: 73–82. [DOI] [PubMed] [Google Scholar]
- 57.Lang SJ, Abel GA, Mant J, et al. Impact of socioeconomic deprivation on screening for cardiovascular disease risk in a primary prevention population: A cross-sectional study. BMJ Open. 2016; 6: e009984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pill R, Stott N. Invitation to attend a health check in a general practice setting: The views of a cohort of non-attenders. J R Coll Gen Pract 1988; 38: 57–60. [PMC free article] [PubMed] [Google Scholar]
- 59.Nielsen KD, Dyhr L, Lauritzen T, et al. You can’t prevent everything anyway: A qualitative study of beliefs and attitudes about refusing health screening in general practice. Fam Pract 2004; 21: 28–32. [DOI] [PubMed] [Google Scholar]
- 60.Ellis N, Gidlow C, Cowap L, et al. A qualitative investigation of non-response in NHS health checks. Arch Public Health. 2015; 73: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jenkinson CE, Asprey A, Clark CE, et al. Patients’ willingness to attend the NHS cardiovascular health checks in primary care: A qualitative interview study. BMC Fam Pract. 2015; 16: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Norman P, Fitter M. Patients’ views on health screening in general practice. Fam Pract 1991; 8: 129–132. [DOI] [PubMed] [Google Scholar]
- 63.Witte K. Putting the fear back into fear appeals: The extended parallel process model, Communications Monographs, 1992; 59: 329–349. [Google Scholar]
- 64.Baker C, Loughren EA, Crone D, et al. Patients’ perceptions of a NHS Health Check in the primary care setting. Qual Prim Care 2015; 22: 232–237. [PubMed] [Google Scholar]
- 65.Riley R, Coghill N, Montgomery A, et al. Experiences of patients and healthcare professionals of NHS cardiovascular health checks: A qualitative study. J Public Health (Oxf). 2016; 38: 543–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Norman P. Predicting the uptake of health checks in general practice: Invitation methods and patients’ health beliefs. Soc Sci Med 1993; 37: 53–59. [DOI] [PubMed] [Google Scholar]
- 67.Harkins C, Shaw R, Gillies M, et al. Overcoming barriers to engaging socio-economically disadvantaged populations in CHD primary prevention: A qualitative study. BMC Public Health. 2010; 10: 391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhong X, Potemans B, Zhang L, et al. Getting a grip on NCDs in China: An evaluation of the implementation of the Dutch-China Cardiovascular Prevention Program. Int J Behav Med. 2015; 22: 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Eborall H, Stone M, Aujla N, et al. Influences on the uptake of diabetes screening: A qualitative study in primary care. Br J Gen Pract. 2012; 62: e204–e211. DOI: 10.3399/bjgp12X630106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hardy S, Deane K, Gray R. The Northampton Physical Health and Wellbeing Project: The views of patients with severe mental illness about their physical health check. Ment Health Fam Med 2012; 9: 233–240. [PMC free article] [PubMed] [Google Scholar]
- 71.Hart JT. The inverse care law. Lancet 1971; 1: 405–412. [DOI] [PubMed] [Google Scholar]
- 72.Delpech R, Ringa V, Falcoff H, et al. Primary prevention of cardiovascular disease: More patient gender-based differences in risk evaluation among male general practitioners. Eur J Prev Cardiol. 2016; 23: 1831–1838. [DOI] [PubMed] [Google Scholar]
- 73.Lorant V, Boland B, Humblet P, et al. Equity in prevention and health care. J Epidemiol Community Health 2002; 56: 510–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Artac M, Dalton ARH, Majeed A, et al. Effectiveness of a national cardiovascular disease risk assessment program (NHS Health Check): Results after one year. Prev Med 2013; 57: 129–134. [DOI] [PubMed] [Google Scholar]
- 75.Kringos D, Boerma W, Bourgueil Y, et al. The strength of primary care in Europe: An international comparative study. Br J Gen Pract, 63: e742–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material for Barriers and facilitators to participation in a health check for cardiometabolic diseases in primary care: A systematic review by Anne-Karien M de Waard, Per E Wändell, Martin J Holzmann, Joke C Korevaar, Monika Hollander, Carl Gornitzki, Niek J de Wit, François G Schellevis, Christos Lionis, Jens Søndergaard, Bohumil Seifert, Axel C Carlsson and on behalf of the SPIMEU Research Group in European Journal of Preventive Cardiology