Abstract
Objectives
Compare cigarette and smokeless tobacco (ST) perceptions within a youth population where ST use is common.
Methods
Male baseball players (N = 594) at 36 rural high schools in California rated separately 20 potential risks or benefits associated with cigarettes or ST, along with global harm ratings. Informed by principal components analysis, 3 composite categories were created: oral/rule-breaking risks (eg, mouth cancer, getting in trouble), systemic risks (eg, heart attack), and benefits (eg, relaxation). Standardized composite scores and harm ratings were compared by product and by tobacco use status.
Results
Cigarettes were perceived as likely to impart oral/rule-breaking risks and systemic risks, unlikely to cause benefits, and as very harmful overall. ST was perceived similarly as cigarettes regarding oral/rule-breaking risks, but less likely to cause systemic risks, and more beneficial. Most participants rated cigarettes as more harmful than ST. Similar patterns existed in all tobacco use groups, including non-users and dual-users.
Conclusions
In this population, cigarettes were perceived as very harmful. ST was perceived similarly to cigarettes only for some risks and as less harmful overall. Communication for rural adolescents should consider multifaceted aspects of ST risk.
Keywords: adolescents, rural health, smokeless tobacco, perceptions
INTRODUCTION
Smokeless tobacco encompasses a range of tobacco products that are used orally and without combustion. In the United States, the most common types of smokeless tobacco (ST) are conventional moist snuff (excluding snus), a form of finely ground tobacco that is held in the mouth, and loose leaf chewing tobacco, which is coarsely shredded and chewed. Together, these 2 types comprised >95% of ST sales in 2014.1 ST use among US youth has remained relatively steady, despite a long-term decline in cigarette smoking; in 2015, past 30-day ST use among male high school students (11.9%) approximately equaled cigarette use (11.8%).2
ST use carries important health consequences, including increased risk of oral and pancreatic cancer and dental diseases, such as periodontal disease and tooth loss.3,4 These risks are serious; however, academic and medical communities generally agree that, taken in total, ST use is not as harmful as smoking combustible cigarettes.5,6
In population based-surveys, many individuals report ST to be equally or more harmful than cigarettes. In a systematic review,7 only in 18% of the reviewed studies did a majority of respondents classify ST as less harmful than cigarettes. More often, study populations had no majority opinion (27%) or insufficient data were reported (32%); although, tobacco users tended to have more accurate relative risk perceptions than non-users.7 In nationally representative studies of US youth, respondents were more likely to perceive ST and cigarettes as similar in harm than to perceive ST as less harmful.8–10 Perceiving any difference in harm between cigarettes and ST was associated with cigarette use.10
There have been calls for public communication to clarify the differential risks between combustible and non-combustible tobacco products, as a misperception that these products are equally harmful could conceivably prevent a combustible tobacco smoker from switching to less harmful ST.11,12 In contrast, concern exists that public health messages aiming to convey the greater harm of combustible tobacco could be misconstrued as endorsing the “safer” product or could erode motivation to quit use of all tobacco.13
Existing studies typically consider harm as a unidimensional concept. However, study participants may interpret harm to include multiple risk types, including non-health related, and potentially variable by tobacco product.14–16 Adolescents’ decisions to use tobacco or engage in other risky behaviors may be based on factors beyond health, including social norms and perceived benefits.14,17 Additionally, most studies that compare ST and combustible tobacco risk perceptions have featured largely urban samples, in which ST familiarity and social acceptability may be low. Misperceptions in ST/cigarette relative harm observed in urban and national samples may not reflect views held in rural populations, for which any potential health communication regarding ST would be more relevant.
In this study, we compared the perceived risks and benefits of cigarettes and ST (non-snus moist snuff and chewing tobacco) using a multidimensional conditional risk assessment instrument14–16 among male high school baseball players in rural California, a population with elevated levels of ST use.18 Studies in this population are important because adolescent athletes may hold specific beliefs and face environmental influences that affect their risk of using tobacco,19 particularly for baseball athletes and ST.20
Our objectives were to: 1) Compare perceived ST risks and benefits by ST use; and 2) Compare the perceived risks and benefits of ST and cigarettes, in the total sample and in subgroups defined by tobacco use.
METHODS
Design and Participants
The present study is a cross sectional analysis of the baseline wave of a cohort study of male interscholastic baseball players, taking place during 3 consecutive spring seasons (2014–2016) at 36 rural California high schools. The study enrolled schools with interscholastic varsity baseball programs and located in municipalities of <50,000 residents and county population density <1000 persons/square-mile.21 Initially, administrators and athletic coaches were contacted at potentially eligible schools based on prior participation in a study of rural adolescents.18 To expand recruitment, schools in the same interscholastic baseball league or recommended by school coaches or administrators were also contacted. Approximately 80 schools were contacted. Of 53 schools that met with the study team, 36 agreed to participate (68%), representing 21 counties in Northern and Central California and with a median municipality size of 8,000 residents. Individual members of the schools’ boys’ baseball team were eligible if providing self-consent (age 18) or signed parental consent and participant assent (age 14–17). Consent forms were distributed to approximately 1060 individuals, and 762 forms were returned (72%). Of returned forms, 642 (84%) indicated positive, active consent, and 594 of these students (93%) completed the in-person confidential computer survey.
Variables
Socio-demographic variables included age, grade in school, race/ethnicity (Hispanic/Latino, non-Hispanic White, other), and parental education (≥1 parent with at least a college degree). Participants were shown representative images and brief descriptions of 7 tobacco products in separate question blocks: cigarettes, cigars (including premium cigars, little cigars, and cigarillos), electronic cigarettes (e-cigarettes, including cigarette-like disposable, rechargeable, and larger refillable devices), hookah/waterpipe, snus, dissolvable tobacco, and conventional ST (listed in surveys as dip or chew). For each product, participants were asked if they had ever used it, the number of times used in their life (later dichotomized <20 or ≥20 to approximate one cigarette pack), and the number of days used in the past 30 days. Questions regarding snus and dissolvable tobacco were excluded from analysis due to lack of familiarity among non-users, low use prevalence, and, for dissolvable tobacco, discontinued product availability.
Tobacco Behavior Groups
Participants were categorized into 4 mutually exclusive tobacco use groups based on past 30-day behaviors: past 30-day tobacco non-users (n = 418); past 30-day non-ST users (n = 72); past 30-day ST users (n = 62); and past 30-day dual non-ST/ST users (n = 42). Non-ST products included cigarettes, cigars, e-cigarettes, and hookah. Past 30-day use is an important metric in youth tobacco evaluation but may include both frequent and infrequent tobacco users. Therefore, as a sensitivity analysis, we also re-categorized participants into 7 mutually exclusive tobacco use groups based on past 30-day use, total lifetime consumption, and number of days used in the past 30 days.
Perception Measures
Separately for cigarettes and ST, participants were asked to estimate the probability (0–100) that 20 specific health-related or social outcomes would happen to them, presented in individually randomized order. Developed for measuring cigarette related-perceptions,14 these items have been adapted for other tobacco products, demonstrating consistent associations with non-cigarette tobacco use,15,16 and had previously been shown to predict cigarette smoking prospectively.22 Outcomes were asked conditionally on the hypothetical scenario: “Imagine that you just began using [cigarettes/dip or chew]. You use [cigarettes/dip or chew] 2 to 3 times per day. Sometimes you use alone, and sometimes you use with friends.” Participants indicated their perceived probability on visual scales with horizontal sliding bars.16 Outcomes included 15 possible risks: bad cough, bad breath, become addicted, brown teeth, get in trouble, harm someone nearby, heart attack, lung cancer, mouth cancer, mouth sores, start smoking cigarettes (for cigarettes: start using dip), trouble catching breath, upset family, upset friends, and worse athletic performance; and 5 possible benefits: better athletic performance, feel more alert, feel relaxed, fit in more, and look cool.
Principal Components and Psychometric Properties
Multidimensionality was likely, given 20 different items. Overall goodness-of-fit tests of the graded response model23,24 and generalized partial credit model25 for ordinal responses (10-levels) to the ST perception data did not provide evidence of good fit (p ≤ 0.01), suggestive of multidimensionality, contingent on no other model assumption violations. Instead of using one total score across all 20 items, we sought to create subsection composite scores for analyses.
We performed principal components analysis (Varimax rotation), following previous methodology.16,22 In analyzing ST items, 3 components with Eigenvalues >1 cumulatively accounted for 60% of the variation in the data (Supplemental Table 1) and were used to develop composite scores, corresponding to the mean response within each of the 3 components. The first component, which we termed “oral and rule-breaking risks,” consisted of 7 risk items related to oral/dental health (eg, mouth cancer and bad breath) and potential consequences from authority figures (ie, get in trouble and upset family). The second component, “systemic health risks,” included 5 risk items related to non-oral health (eg, heart attack and lung cancer) and 3 risk items related to peers and behaviors (ie, upset friends, harm someone nearby, and start smoking cigarettes). The final component, “benefits,” included the 5 benefit items. Each component featured positive inter-item correlation. Correlation was generally weaker between components, particularly between the benefits component items and the items related to risks, but correlations between all risk-related items were statistically significant (Benjamini-Hochberg procedure for multiple tests26).
Each component demonstrated strong internal consistency: oral and rule-breaking risks (Chronbach’s alpha: 0.882), systemic health risks (0.905), and benefits (0.769). Each item was well correlated with the remainder of its component (corrected item-total correlation). Chronbach’s alpha did not increase by any amount after removing any single item, indicating that removing any one item did not make the construct more reliable. While components were derived based on ST ratings, the same item groupings for cigarettes were also internally consistent.
There was a separate global measure of overall harm. For cigarettes and ST, participants were asked, “In your opinion, how harmful is using [cigarettes/dip or chew] to general health?” and moved a horizontal bar from 0 (not at all harmful) to 100 (extremely harmful).
Study Size
For the present analysis, there were 565 individuals who provided ratings of perceived overall harm for cigarettes and ST. The anticipated minimally detectable difference between products (cigarettes and ST) in perceived overall harm depended on the number of individuals in each tobacco use group. Under the following assumptions: power 80%, 2-tailed alpha 5%, variance explained by other model variables 40%, standard deviation 18, and design effect for intra-school clustering 1.25, the expected minimally detectable differences in perceived harm between products would be 3.1 (past 30-day non-users), 7.4 (past 30-day non-ST users), 9.8 (past 30-day dual-users), 8.0 (past 30-day ST users), and 2.6 (total sample). Units are on the rating scale from 0 to 100.
Statistical Analyses
In descriptive analyses, participants’ demographic and tobacco use variables were summarized as mean ±standard deviation or frequency and percent. We calculated the mean perception ratings (0–100 scale) for each of the 20 individual cigarette and ST risk or benefit items. We tested differences between cigarette and ST ratings (Wilcoxon signed-rank test for nonparametric distributions and within-participant pairing) and calculated the percent of participants who rated each consequence as more likely to occur with use of cigarettes than use of ST. In an exploratory analysis, we examined how many participants provided a “maximum” (ie, 100) or “minimum” (ie, 0) rating for each product.
In the main analyses, we compared tobacco-related perceptions in 3 ways. First, to examine differences in how ST ever and never users perceive specific ST risks and benefits, we compared the mean standardized scores of each of the 20 individual ST risk or benefit items between ST ever users and ST never users. Next, we examined potential perceived differences between cigarettes and ST by comparing the standardized global harm score and the 3 adjusted mean composite scores and between cigarettes and ST in each of the 4 tobacco use groups. Finally, to examine potential perceived differences between types of risks for each product, we compared adjusted scores for the 2 composite risk types (ie, oral/rule-breaking risks vs. systemic health risks) for cigarettes and for ST in each of the tobacco use groups.
To standardize perception ratings for socio-demographic variables, we fitted separate mixed effects linear regression models for each of the 20 individual ST and cigarette risk or benefit items (dependent variable), including fixed effect terms for product ever-use, socio-demographic variables, year the survey was taken, and a random intercept term for school. Visual inspection of residual-vs.-fitted plots revealed no major violations of model fit. As in earlier work,16 to improve interpretability of adjusted estimates (ie, to return to the original 0–100 scale), we calculated marginal adjusted mean scores for each risk and benefit.27 We followed the same approach in calculating marginal standardized mean composite scores for cigarettes and ST on oral/rule-breaking risks, systemic health risks, benefits, and the global measure of harm.
In all analyses, multiple imputation (chained equations, 25 imputations) was used to replace missing covariate values: grade in school (n missing: 1) and parental education (n missing: 41). Perception measures were the main outcome variable and were not imputed, except in the case of computing composite scores. For composite scores, participants missing responses for fewer than 10 of the 20 individual items had perceived probabilities multiply imputed for the missing items (0.2% of all perception data). Individual missing ≥10 individual items for cigarettes or ST or missing the overall harm item were excluded from analyses. A sensitivity analysis based on complete cases (no imputation) was conducted. Non-parametric 95% confidence intervals were obtained via empirical quantiles of bootstrap estimates (5000 iterations) with case resampling at 2 levels: schools, then participants to account for clustering by school in variance estimates. The Benjamini-Hochberg procedure was used to determine statistical significance with multiple testing.26 Analyses were completed using Stata 14.2 (College Station, TX) and R 3.3.2 (Vienna, Austria).
RESULTS
Participants
In this study sample (Table 1), 57% of respondents had ever used a tobacco product and 30% had used at least one product within the past 30 days. ST (dip/chew) was the most commonly used product: 37% ever use, 18% past 30-day use (Table 1).
Table 1.
Characteristics and tobacco use status of study population
| Characteristics | totala (N = 594) | Tobacco Use Groups | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Past 30-day non-user (n = 418) | Past 30-day non-ST user (n = 72) | Past 30-day dual-user (n = 42) | Past 30-day ST user (n = 62) | |||
| Age in years, mean (SD) | 15.8 (1.2) | 15.7 (1.1) | 16.0 (1.3) | 16.3 (1.1) | 16.5 (1.2) | * |
| Grade in school, n (%) | * | |||||
| 9 | 174 (29) | 138 (33) | 21 (29) | 8 (19) | 7 (11) | |
| 10 | 163 (27) | 123 (29) | 19 (26) | 6 (14) | 15 (24) | |
| 11 | 140 (24) | 97 (23) | 13 (18) | 15 (36) | 15 (24) | |
| 12 | 116 (20) | 59 (14) | 19 (26) | 13 (31) | 25 (40) | |
| Race/ethnicity, n (%) | ||||||
| Hispanic/Latino | 237 (40) | 194 (46) | 29 (40) | 27 (64) | 37 (60) | |
| White (not Hispanic/Latino) | 287 (48) | 172 (41) | 32 (44) | 12 (29) | 21 (34) | |
| Other | 70 (12) | 52 (12) | 11 (15) | 3 (7) | 4 (6) | |
| Parental education, n (%) | ||||||
| ≥ 1 parent with college degree | 327 (59) | 236 (60) | 35 (52) | 26 (67) | 30 (56) | |
| Tobacco ever use, n (%) | ||||||
| Any product | 341 (57) | 165 (39) | 72 (100) | 42 (100) | 62 (100) | * |
| Non-ST tobaccob | 311 (52) | 140 (33) | 72 (100) | 42 (100) | 57 (92) | * |
| Smokeless tobacco | 219 (37) | 77 (18) | 38 (53) | 42 (100) | 62 (100) | * |
| Tobacco past 30-day use, n (%) | ||||||
| Any product | 176 (30) | 0 (0) | 72 (100) | 42 (100) | 62 (100) | * |
| Non-ST tobacco | 114 (19) | 0 (0) | 72 (100) | 42 (100) | 0 (0) | * |
| Smokeless tobacco | 104 (18) | 0 (0) | 0 (0) | 42 (100) | 62 (100) | * |
| Tobacco use ≥ 20 times, n (%) | ||||||
| Any product | 142 (24) | 26 (6) | 40 (56) | 36 (86) | 40 (65) | * |
| Non-ST tobacco | 113 (19) | 24 (6) | 38 (53) | 28 (67) | 23 (37) | * |
| Smokeless tobacco | 73 (12) | 4 (1) | 4 (6) | 29 (69) | 36 (58) | * |
Cell counts may not sum to column totals due to missing values for some variables
Non-ST tobacco products include: cigarettes, cigars, e-cigarettes, and hookah
p < 0.05 for difference over the 4 tobacco use groups: ANOVA (age) or chi-square
Abbreviations: SD = standard deviation; ST = smokeless tobacco
Perceptions of ST Ever and Never Users
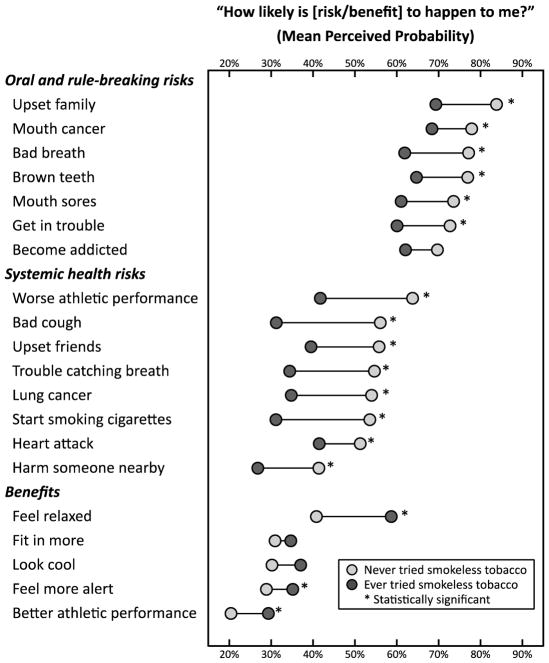
Across all risk items, ST ever users perceived ST as less likely to cause health or social consequences and more likely to offer benefits than did ST never users (Figure 1). Differences between ST ever and never users were statistically significant for 17 of the 20 individual risk or benefit items after correction for multiple tests. Differences for the 3 items that did not reach statistical significance (addiction, fit in more, and look cool) were consistent in direction with other items in the same category.
Figure 1.
Standardized perceived risks and benefits of using smokeless tobacco, among smokeless tobacco ever-users and never-users.
The figure shows standardized mean perceived probabilities for each of 20 possible outcomes. Probabilities indicate the reported likelihood with which respondents believed each outcome would happen to them if they were to use smokeless tobacco. Values adjusted for age, race/ethnicity, parental education, and year survey was taken. Individual risk/benefit items were sorted into categories based on principal components analysis. Statistical significance based on Benjamini-Hochberg correction for multiple testing to maintain false discovery rate ≤ 0.05.
Visually examining Figure 1, for both ST ever and never users, the first category, which included oral health risks, such as mouth cancer and brown teeth, and rule-breaking risks, such as getting into trouble or upsetting family members, was viewed as the set of consequences most likely to occur with ST use. The category of systemic health risks, such as heart attack and lung cancer (that also included harming others and starting to smoke cigarettes), was largely viewed as less likely to occur than oral/rule-breaking risks, particularly among ST ever users (Figure 1). ST never users viewed benefits of ST use as unlikely; however, among ever users, perceived probabilities of benefits were higher (Figure 1).
Cigarette and ST Individual Perception Items
Among the 20 individual items, the outcome “upset family” was perceived as the most likely to occur, both for cigarettes and ST (Table 2). “Better athletic performance” was the outcome perceived as least likely to occur. For the 7 items grouped as oral and rule-breaking risks, mean perceived likelihood was greater for cigarettes on 3 items, greater for ST on 3 items, and not statistically significantly different for another (“become addicted”). Across these items, 28–51% of participants gave cigarettes a higher rating than ST (Table 2). For items grouped as systemic health risks, cigarettes were consistently perceived as more likely than ST to confer these outcomes, with at least a majority (54–72%) assigning a greater rating to cigarettes (Table 2). In contrast, for the 5 items grouped as benefits, ST was perceived as more likely than cigarettes to lead to these outcomes, with only 22–43% of participants rating cigarettes higher (Table 2).
Table 2.
Individual item perception ratings for cigarettes and smokeless tobacco
| Cigarettes | Smokeless Tobacco | differencec | cigarettes higherd (%) | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Mean (SD) | rhoa | alphab | Mean (SD) | rhoa | alphab | |||
| Oral and rule-breaking risks | 0.88 | 0.88 | ||||||
| Upset family | 83.3 (29) | 0.65 | 0.87 | 78.3 (29) | 0.64 | 0.87 | 5.0 | 45.7 |
| Mouth cancer | 63.9 (31) | 0.70 | 0.87 | 74.2 (27) | 0.77 | 0.85 | −10.4 | 28.4 |
| Bad breath | 77.0 (29) | 0.58 | 0.88 | 71.3 (30) | 0.72 | 0.86 | 5.7 | 51.2 |
| Brown teeth | 68.4 (30) | 0.71 | 0.86 | 72.3 (29) | 0.75 | 0.85 | −3.9 | 38.7 |
| Mouth sores | 58.6 (30) | 0.67 | 0.87 | 68.6 (30) | 0.72 | 0.86 | −10.0 | 29.8 |
| Get in trouble | 71.6 (33) | 0.72 | 0.86 | 68.0 (33) | 0.55 | 0.88 | 3.7 | 44.7 |
| Become addicted | 66.8 (34) | 0.70 | 0.86 | 66.7 (30) | 0.57 | 0.88 | 0.0 | 47.6 |
| Systemic health risks | 0.86 | 0.91 | ||||||
| Worse at athletics | 72.4 (32) | 0.58 | 0.85 | 55.4 (36) | 0.64 | 0.90 | 17.0 | 62.0 |
| Bad cough | 71.2 (29) | 0.74 | 0.83 | 46.4 (34) | 0.80 | 0.88 | 24.6 | 71.5 |
| Upset friends | 60.2 (34) | 0.68 | 0.84 | 49.3 (34) | 0.60 | 0.90 | 11.0 | 57.8 |
| Trouble catching breath | 70.8 (28) | 0.72 | 0.83 | 46.8 (33) | 0.80 | 0.88 | 24.1 | 72.0 |
| Lung cancer | 70.5 (30) | 0.51 | 0.85 | 46.7 (34) | 0.74 | 0.89 | 23.9 | 69.6 |
| Start smoking/using dipe | 57.9 (33) | 0.43 | 0.83 | 44.8 (35) | 0.64 | 0.90 | 13.1 | 55.3 |
| Heart attack | 56.5 (31) | 0.67 | 0.84 | 47.4 (31) | 0.74 | 0.89 | 9.1 | 54.4 |
| Harm someone nearby | 56.4 (35) | 0.57 | 0.85 | 35.4 (33) | 0.65 | 0.90 | 21.1 | 62.9 |
| Benefits | 0.68 | 0.77 | ||||||
| Feel relaxed | 44.3 (32) | 0.44 | 0.64 | 47.2 (32) | 0.50 | 0.74 | −2.7 | 43.1 |
| Fit in more | 24.8 (27) | 0.53 | 0.59 | 32.4 (29) | 0.59 | 0.71 | −7.7 | 32.3 |
| Look cool | 21.6 (28) | 0.39 | 0.65 | 32.6 (30) | 0.61 | 0.70 | −10.9 | 24.8 |
| Feel more alert | 25.0 (26) | 0.52 | 0.59 | 30.9 (27) | 0.50 | 0.74 | −5.8 | 33.0 |
| Better at athletics | 16.1 (27) | 0.32 | 0.68 | 23.2 (27) | 0.50 | 0.74 | −7.1 | 22.1 |
Item correlation with remaining items in the composite score
Chronbach’s alpha for composite score (title rows) or Chronbach’s alpha recalculated with each individual item removed
Mean differences in rating between cigarettes and smokeless tobacco (all differences p < 0.05 except “become addicted” by Wilcoxon signed-rank test)
Percent of participants with higher rating for cigarettes than for ST
Worded as start smoking cigarettes in smokeless survey questions and as start using dip/chew on cigarette questions
Abbreviation: SD = standard deviation; N = 563 to 567 (depending on missing values per item)
On the global measure of overall harm, 65% of participants assigned a higher rating to cigarettes than to ST, but only 15% rated ST as more harmful than cigarettes (Supplemental Table 2). In exploratory analysis, many of the individuals who did not assign a higher rating to one product over the other had provided the minimum or maximum rating, in that both products were assigned a score of 0 or 100 (Supplemental Table 2). For instance, of the 20% of participants to rate cigarettes and ST as equally harmful, 92% of these assigned the maximum score of 100.
Composite Scores
For the composite items, adolescents perceived cigarettes and ST similarly in terms of oral health and rule-breaking risks (Table 3). In the total sample, composite scores for oral/rule-breaking risks were high and not statistically significantly different between products (cigarettes: 69.9; ST: 71.4; p = 0.13). There were no statistically significant differences in composite scores between cigarettes and ST in any of the use groups, with the exception of past 30-day tobacco non-users, who perceived ST as slightly more likely to convey oral or rule-breaking risks (cigarettes: 72.5; ST: 75.3; p = 0.01).
Table 3.
Cigarette and smokeless tobacco perceived risk and benefit standardized composite scores, according to tobacco use group
| n | Cigarette Score | ST Score | Difference (95% CI) | p-valuea | cigarettes higherb (%) | |
|---|---|---|---|---|---|---|
|
|
||||||
| Oral and rule-breaking risks | ||||||
| Total sample | 567 | 69.9 | 71.4 | −1.4 (−3.3, 0.4) | 0.13 | 41.6 |
| Past 30-day non-user | 401 | 72.5 | 75.3 | −2.8 (−4.8, −0.8) | 0.01* | 36.3 |
| Past 30-day non-ST user | 66 | 67.7 | 70.0 | −2.3 (−8.0, 2.3) | 0.32 | 41.8 |
| Past 30-day dual-user | 39 | 54.9 | 49.9 | 5.0 (−3.8, 15.0) | 0.24 | 31.5 |
| Past 30-day ST user | 61 | 64.8 | 60.7 | 4.1 (−2.1, 12.4) | 0.20 | 48.5 |
| Systemic health risks | ||||||
| Total sample | 567 | 64.5 | 46.5 | 18.0 (14.5, 21.8) | <0.001* | 76.5 |
| Past 30-day non-user | 401 | 66.5 | 51.3 | 15.2 (11.7, 19.4) | <0.001* | 66.9 |
| Past 30-day non-ST user | 66 | 59.0 | 44.0 | 15.0 (8.8, 21.5) | <0.001* | 82.8 |
| Past 30-day dual-user | 39 | 54.3 | 22.1 | 32.3 (21.3, 43.6) | <0.001* | 79.2 |
| Past 30-day ST user | 61 | 63.6 | 33.6 | 30.0 (20.1, 38.8) | <0.001* | 82.5 |
| Benefits | ||||||
| Total sample | 567 | 26.4 | 33.2 | −6.8 (−9.5, −4.3) | <0.001* | 28.7 |
| Past 30-day non-user | 401 | 25.6 | 30.5 | −4.9 (−7.8, −2.2) | <0.001* | 38.0 |
| Past 30-day non-ST user | 66 | 25.8 | 34.1 | −8.3 (−15.3, −2.3) | 0.01* | 26.1 |
| Past 30-day dual-user | 39 | 33.0 | 44.5 | −11.4 (−20.7, −2.4) | 0.02* | 25.2 |
| Past 30-day ST user | 61 | 27.7 | 43.4 | −15.6 (−21.9, −7.6) | <0.001* | 15.5 |
| Overall harm | ||||||
| Total sample | 565 | 89.6 | 74.2 | 15.3 (12.2, 18.6) | <0.001* | 65.1 |
| Past 30-day non-user | 397 | 91.2 | 79.7 | 11.4 (8.4, 14.8) | <0.001* | 56.0 |
| Past 30-day non-ST user | 69 | 88.7 | 75.3 | 13.4 (7.2, 19.8) | <0.001* | 65.2 |
| Past 30-day dual-user | 40 | 77.6 | 42.0 | 35.7 (22.8, 49.4) | <0.001* | 54.2 |
| Past 30-day ST user | 59 | 87.9 | 58.1 | 29.8 (20.7, 37.2) | <0.001* | 75.0 |
Composite scores determined within categories of risks or benefits, as identified by principal components analysis. Higher values indicate greater perceived likelihood of the outcome. Overall harm was from a single global item. Values adjusted for age, race/ethnicity, parental education, and year survey was taken.
Comparing mean cigarette score to mean ST score
Percent of participants with higher score for cigarettes than for ST
Statistically significant after Benjamini-Hochberg correction for multiple testing
Abbreviations: CI = confidence interval; ST = smokeless tobacco
In all use groups, cigarettes were viewed as substantially more likely than ST to lead to systemic health consequences or other non-oral risks (Table 3). All groups perceived ST as more likely than cigarettes to confer benefits, including the sample overall (cigarettes: 26.4; ST: 33.2; p < 0.001) (Table 3). Cigarettes were near-universally rated as causing great harm to health, with a mean rating in the total sample of 89.6 (Table 3). In all use groups, cigarettes were rated as more harmful than ST, including non-ST tobacco users and dual-users (Table 3). Findings were qualitatively unchanged under alternative behavior classifications featuring 7 tobacco use categories, although not all associations were statistically significant, potentially due to having relatively few participants in some categories (Supplemental Table 3). Findings were also not meaningfully different under a complete case analysis (Supplemental Table 4).
The difference in composite scores between oral/rule-breaking risk and systemic health risks was much larger for ST than for cigarettes (Supplemental Table 5). Whereas for cigarettes both oral/rule-breaking risk and systemic health risks were viewed as likely, for ST, there were larger perceived differences between these risk types in all tobacco use groups.
DISCUSSION
In this population of rural male adolescents, those who had used smokeless tobacco perceived it to be less harmful and more beneficial than those who had not, consistent with previous work on perceptions of ST8,9,28 and other tobacco products.8,14,15,22,29 Notably, while both ST ever and never users rated ST as highly likely to lead to oral health and rule-breaking consequences, those who had used ST viewed other types of risks, such as lung cancer or harming others, as much less likely and similar in probability to ST-related benefits. This suggests that perceived social risks and benefits stand alongside perceived health risks as discriminating correlates of ST behavior and that adolescents differentiate between various risks types in conceptualizing the potential harms of smokeless tobacco.
Adolescents in this sample perceived the harm of ST and cigarettes differently, including among tobacco never users, ST users, non-ST users, and dual users. This reflects an understanding of the properties of these tobacco products that largely aligns with experts: ST use is much less likely to induce pulmonary disease and harmful second-hand exposures than smoking cigarettes, but the prospects of oral health problems and, for many youth, friction with family or school authority figures persist with both products. Interestingly, oral health and social risks were found to comprise a single component, perhaps reflecting that those outcomes were all viewed as similarly credible and closely tied to ST use.
While the majority of rural male students in this sample rated cigarettes as more harmful than ST, in nationally representative surveys, in contrast, it is not uncommon for a majority of respondents to fail to rate ST as less harmful than cigarettes.7–10 Questionnaire items that emphasize “harm” may overlook subtleties in beliefs not captured as a single concept. We speculate that youth may conceptualize harm as encompassing a range of health and social consequences, including but not limited to getting into trouble and non-fatal health risks. For many, these short-term effects could be viewed as probable, immediate, and unacceptable, even while understanding that more severe long-term consequences, such as lung cancer or heart attacks, are not equally likely across tobacco products.
In prior qualitative studies, both adolescents and adults reported complicated beliefs regarding the relative safety of cigarettes and ST.30–32 While generally recognizing that smoking and ST convey different types of risks, some respondents, particularly smokers, viewed these different risks as equally unappealing.32 For others, beliefs that damage to the mouth and jaw caused by ST is not as consequential as the effects of cigarettes on the lungs was frequently reported as a motivating factor in ST use.30,31 Compatible with the present study, but in a largely urban sample with a low prevalence of ST use, adolescents consistently rated ST as less likely than cigarettes to lead to long-term chronic disease, with the notable exception of oral cancer.15
Other non-cigarette tobacco products, such as e-cigarettes, cigars, and tobacco waterpipe have increased in popularity among adolescents and young adults2,33 and are frequently viewed as less dangerous relative to cigarettes.9,15 In interviews, young people have reported social benefits associated with cigar and waterpipe use, while also tending to underestimate and discount long-term risks.34 In the present study, potential benefits of tobacco use were viewed, on average, as less likely than potential risks. However, those who used ST or cigarettes perceived benefits to be more likely than did non-users, and ST was perceived as more likely than cigarettes to convey those benefits, potentially reflecting the social context of the rural baseball athletes who participated.
It has been argued that the public has a right to be informed of the comprehensive risks across combustible and non-combustible tobacco products,11 but limited evidence exists that stressing differences in relative harm between cigarettes and ST is effective in preventing youth smoking. Competing messages not to initiate ST use but espousing ST as a potential smoking alternative could engender confusion,35 particularly given a tendency for the public to underestimate absolute risk when presented in reference to a higher risk alternative.36 In the present study, male adolescents largely recognized cigarettes as more harmful than ST. It is possible that messages encouraging current adult cigarette smokers to switch to a less harmful tobacco product could provide a benefit to those smokers. Care must be taken that explicit efforts to emphasize the relative risks between cigarettes and ST do not erode currently held beliefs among youth regarding ST harm or divert resources from existing and effective tobacco control efforts.37
The present study calculated perceived differences between cigarette and ST-related risks using indirect measures, in which participants were presented items for each product separately rather than asked to compare one to another directly.38 For categorical survey items, some evidence suggests that indirect measures are more likely than direct measures to detect a difference in tobacco product perceptions.9 Indirect measures may better capture actual product perceptions, because respondents would be less inclined to select a “socially appropriate” choice that all tobacco is equally harmful.38 However, direct measures may be stronger correlates of youth tobacco behaviors.9 Further methodology research, including for non-categorical and risk-specific perception measures is warranted.
In addition, while the measures used in this study asked participants to estimate the “probability” that an event would happen to them, their perceived ratings would not necessarily be realistic on a probabilistic scale for many of the outcomes, such as cancer. This is consistent with prior work showing that adolescents often overestimate the actual risks of mortality events.39 In expressing tobacco-related risks, it may be challenging for participants to convey probabilities accurately.7 The use of visual response scales in the present study reduced ambiguity and potentially aided them in accurately expressing perceived rank among different outcomes. Even in the case that absolute probabilities are inaccurate, differences in perceptions between tobacco products and between tobacco use groups maintain relevance.
Among study limitations, this population of high school baseball players in rural California may not generalize to more diverse, national or statewide populations. Schools were enrolled from a non-random list of candidate schools. Recruitment intentionally focused on a target population in which ST use is a familiar, even normative, to provide information relevant to athletes and rural youth who have been targeted in ST marketing,40,41 are more likely to use ST,42,43 and may be insufficiently represented in national or statewide surveys. Advantageously, including multiple types of risks and benefits revealed associations that may have been obscured under a single perceived harm measure. Multiple imputation reduced information loss, and numeric findings were adjusted for socio-demographic factors.
IMPLICATIONS FOR TOBACCO REGULATION
Policies, including regulation, that are able to shift tobacco use from more harmful to less harmful products at the population level are under consideration.6 The US Food and Drug Administration comprehensive plan for tobacco and nicotine regulation embraces this approach.44 Whether conventional ST products have a role in achieving the goal of population harm reduction without increasing tobacco and/or nicotine use among youth is a contentious topic. Existing cohort studies demonstrate that youth who use ST are at elevated risk of progression to cigarette smoking.45,46
Harm is therefore a key consideration in both tobacco regulation and youth tobacco decision-making. For the public, “harm” may be multidimensional, comprising different risk types. In this study, rural male adolescents did not perceive ST and cigarettes as equivalent tobacco products. Cigarettes were widely perceived as conveying high probability of short-term social risks, short-term and long-term health risks, and unlikely to offer benefits. ST was viewed as less risky on a variety of measures, particularly for non-oral chronic diseases. For ST users, smokeless tobacco was widely seen as more likely than cigarettes to offer benefits. Official information campaigns from the FDA or other government entities should be cautious of emphasizing risk differences between ST and cigarettes if such communications would result in greater acceptance of ST among rural male adolescents already at elevated risk of ST and unlikely to smoke. Targeting of any such campaigns to adult cigarette smokers most likely to benefit from switching to ST would be essential; assuming targeting feasibility challenges could be surmounted. At a minimum, existing public information campaigns should continue to focus on credible ST health risks and aim to reduce perceived product benefits among adolescents.
Supplementary Material
Acknowledgments
Thank you to Elizabeth T. Couch and Janelle Urata of the University of California San Francisco for contributions to data collection and helpful comments on the manuscript. This project received support from US National Institutes of Health and Food and Drug Administration under grant NCI/FDA P50 CA180890 and from the NIH under grant NCATS KL2 TR000143. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Footnotes
Human Subjects Statement
The University of California San Francisco Internal Review Board approved all study procedures. Those procedures meet the ethical standards outlined in the Helsinki Declaration. Participating adolescents provided signed parental consent and participant assent (age 14–17) or self-consent (age 18). Participating schools received $150 to $300, based on the percent of signed consent forms returned (regardless of affirming or declining participation). Individual respondents received $10 credit to an online retailer.
Conflicts of Interest Statement
The authors declare that they have no competing interests. Funding agencies played no role in the conduct of the research, preparation of the manuscript, or the decision to submit for publication.
Contributor Information
Benjamin W. Chaffee, Assistant Professor, University of California San Francisco School of Dentistry, Center for Tobacco Control Research and Education, San Francisco, CA.
Jing Cheng, Professor, University of California San Francisco School of Dentistry, Center for Tobacco Control Research and Education, San Francisco, CA.
References
- 1.Federal Trade Commission Smokeless Tobacco Report for 2014. Federal Trade Commission; Washington, DC: 2016. [Google Scholar]
- 2.Kann L, McManus T, Harris WA, et al. Youth Risk Behavior Surveillance - United States, 2015. MMWR Surveill Summ. 2016;65(6):1–174. doi: 10.15585/mmwr.ss6506a1. [DOI] [PubMed] [Google Scholar]
- 3.Smokeless Tobacco and Public Health: A Global Perspective. 2014 National Cancer Institute and Centers for Disease Control and Prevention. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention, National Institutes of Health; NIH Publication No. 14–7983. [Google Scholar]
- 4.Warnakulasuriya S, Dietrich T, Bornstein MM, et al. Oral health risks of tobacco use and effects of cessation. Int Dent J. 2010;60(1):7–30. [PubMed] [Google Scholar]
- 5.Fiore MC, Schroeder SA, Baker TB. Smoke, the chief killer - strategies for targeting combustible tobacco use. N Engl J Med. 2014;370(4):297–299. doi: 10.1056/NEJMp1314942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zeller M, Hatsukami D. The strategic dialogue on tobacco harm reduction: a vision and blueprint for action in the US. Tob Control. 2009;18(4):324–332. doi: 10.1136/tc.2008.027318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Czoli CD, Fong GT, Mays D, Hammond D. How do consumers perceive differences in risk across nicotine products? A review of relative risk perceptions across smokeless tobacco, e-cigarettes, nicotine replacement therapy and combustible cigarettes. Tob Control. 2017;26(e1):e49–e58. doi: 10.1136/tobaccocontrol-2016-053060. [DOI] [PubMed] [Google Scholar]
- 8.Amrock SM, Lee L, Weitzman M. Perceptions of e-cigarettes and noncigarette tobacco products among US youth. Pediatrics. 2016;138(5):e20154306. doi: 10.1542/peds.2015-4306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Persoskie A, O’Brien EK, Nguyen AB, Tworek C. Measuring youth beliefs about the harms of e-cigarettes and smokeless tobacco compared to cigarettes. Addict Behav. 2017;70:7–13. doi: 10.1016/j.addbeh.2017.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tomar SL, Hatsukami DK. Perceived risk of harm from cigarettes or smokeless tobacco among U.S. high school seniors. Nicotine Tob Res. 2007;9(11):1191–1196. doi: 10.1080/14622200701648417. [DOI] [PubMed] [Google Scholar]
- 11.Kozlowski LT, Edwards BQ. “Not safe” is not enough: smokers have a right to know more than there is no safe tobacco product. Tob Control. 2005;14(Suppl 2):ii3–7. doi: 10.1136/tc.2004.008334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Phillips CV, Wang C, Guenzel B. You might as well smoke; the misleading and harmful public message about smokeless tobacco. BMC Public Health. 2005;5:31. doi: 10.1186/1471-2458-5-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robins R. The seduction of harm reduction: proceedings from the September 2004 Summit. Sacramento, CA: Department of Health Services; 2005. pp. 1–120. [Google Scholar]
- 14.Halpern-Felsher BL, Biehl M, Kropp RY, Rubinstein ML. Perceived risks and benefits of smoking: differences among adolescents with different smoking experiences and intentions. Prev Med. 2004;39(3):559–567. doi: 10.1016/j.ypmed.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 15.Roditis M, Delucchi K, Cash D, Halpern-Felsher B. adolescents’ perceptions of health risks, social risks, and benefits differ across tobacco products. J Adolesc Health. 2016;58(5):558–566. doi: 10.1016/j.jadohealth.2016.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chaffee BW, Gansky SA, Halpern-Felsher B, et al. Conditional risk assessment of adolescents’ electronic cigarette perceptions. Am J Health Behav. 2015;39(3):421–432. doi: 10.5993/AJHB.39.3.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parsons JT, Siegel AW, Cousins JH. Late adolescent risk-taking: effects of perceived benefits and perceived risks on behavioral intentions and behavioral change. J Adolesc. 1997;20(4):381–392. doi: 10.1006/jado.1997.0094. [DOI] [PubMed] [Google Scholar]
- 18.Gansky SA, Ellison JA, Kavanagh C, et al. Patterns and correlates of spit tobacco use among high school males in rural California. J Public Health Dent. 2009;69(2):116–124. doi: 10.1111/j.1752-7325.2008.00109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agaku IT, Singh T, Jones SE, et al. Combustible and smokeless tobacco use among high school athletes - United States, 2001–2013. MMWR Morb Mortal Wkly Rep. 2015;64(34):935–939. doi: 10.15585/mmwr.mm6434a2. [DOI] [PubMed] [Google Scholar]
- 20.Cooper J, Ellison JA, Walsh MM. Spit (smokeless)-tobacco use by baseball players entering the professional ranks. J Athl Train. 2003;38(2):126–132. [PMC free article] [PubMed] [Google Scholar]
- 21.Hewitt M. Health Program Office of Technology Assessment. Washington, DC: Superintendent of Documents, US Government Printing Office; 1989. Defining “rural” areas: Impact on health care policy and research. [Google Scholar]
- 22.Song AV, Morrell HE, Cornell JL, et al. Perceptions of smoking-related risks and benefits as predictors of adolescent smoking initiation. Am J Public Health. 2009;99(3):487–492. doi: 10.2105/AJPH.2008.137679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Samejima F. Estimation of latent ability using a response pattern of graded scores. ETS Research Report Series. 1968;1968(1) [Google Scholar]
- 24.Samejima F. A general model for free-response data. Psychometrika Monograph Supplement. 1972 [Google Scholar]
- 25.Muraki E. A generalized partial credit model: Application of an EM algorithm. ETS Research Report Series. 1992;1992(1) [Google Scholar]
- 26.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995:289–300. [Google Scholar]
- 27.Snowden JM, Rose S, Mortimer KM. Implementation of G-computation on a simulated data set: demonstration of a causal inference technique. Am J Epidemiol. 2011;173(7):731–738. doi: 10.1093/aje/kwq472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Overland S, Hetland J, Aaro LE. Relative harm of snus and cigarettes: what do Norwegian adolescents say? Tob Control. 2008;17(6):422–425. doi: 10.1136/tc.2008.026997. [DOI] [PubMed] [Google Scholar]
- 29.Brose LS, Brown J, Hitchman SC, McNeill A. Perceived relative harm of electronic cigarettes over time and impact on subsequent use. A survey with 1-year and 2-year follow-ups. Drug Alcohol Depend. 2015;157:106–111. doi: 10.1016/j.drugalcdep.2015.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu ST, Nemeth JM, Klein EG, et al. Risk perceptions of smokeless tobacco among adolescent and adult users and nonusers. J Health Commun. 2015;20(5):599–606. doi: 10.1080/10810730.2015.1012237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Couch ET, Darius E, Walsh MM, Chaffee BW. Smokeless tobacco decision-making among rural adolescent males in California. J Community Health. 2017;42(3):544–550. doi: 10.1007/s10900-016-0286-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wray RJ, Jupka K, Berman S, et al. Young adults’ perceptions about established and emerging tobacco products: results from eight focus groups. Nicotine Tob Res. 2012;14(2):184–190. doi: 10.1093/ntr/ntr168. [DOI] [PubMed] [Google Scholar]
- 33.Jamal A, Gentzke A, Hu SS, et al. Tobacco use among middle and high school students - United States, 2011–2016. MMWR Morb Mortal Wkly Rep. 2017;66(23):597–603. doi: 10.15585/mmwr.mm6623a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cornacchione J, Wagoner KG, Wiseman KD, et al. Adolescent and young adult perceptions of hookah and little cigars/cigarillos: implications for risk messages. J Health Commun. 2016;21(7):818–825. doi: 10.1080/10810730.2016.1177141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tomar SL, Fox BJ, Severson HH. Is smokeless tobacco use an appropriate public health strategy for reducing societal harm from cigarette smoking? Int J Environ Res Public Health. 2009;6(1):10–24. doi: 10.3390/ijerph6010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rothman AJ, Kiviniemi MT. Treating people with information: an analysis and review of approaches to communicating health risk information. J Natl Cancer Inst Monogr. 1999;(25):44–51. doi: 10.1093/oxfordjournals.jncimonographs.a024207. [DOI] [PubMed] [Google Scholar]
- 37.Gartner CE, Hall WD, Chapman S, Freeman B. Should the health community promote smokeless tobacco (snus) as a harm reduction measure? PLoS Med. 2007;4(7):e185. doi: 10.1371/journal.pmed.0040185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Popova L, Ling PM. Perceptions of relative risk of snus and cigarettes among US smokers. Am J Public Health. 2013;103(11):e21–23. doi: 10.2105/AJPH.2013.301547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fischhoff B, Parker AM, de Bruin WB, et al. Teen expectations for significant life events. The Public Opinion Quarterly. 2000;64(2):189–205. doi: 10.1086/317762. [DOI] [PubMed] [Google Scholar]
- 40.Miller Lo EJ, Giovenco DP, Wackowski OA, et al. The cigarette and smokeless tobacco markets in Texas relative to the United States. Tob Regul Sci. 2017;3(2):183–191. doi: 10.18001/TRS.3.2.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ling PM, Haber LA, Wedl S. Branding the rodeo: a case study of tobacco sports sponsorship. Am J Public Health. 2010;100(1):32–41. doi: 10.2105/AJPH.2008.144097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nelson DE, Mowery P, Tomar S, et al. Trends in smokeless tobacco use among adults and adolescents in the United States. Am J Public Health. 2006;96(5):897–905. doi: 10.2105/AJPH.2004.061580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pesko MF, Robarts AM. Adolescent tobacco use in urban versus rural areas of the United States: The influence of tobacco control policy environments. J Adolesc Health. 2017;61(1):70–76. doi: 10.1016/j.jadohealth.2017.01.019. [DOI] [PubMed] [Google Scholar]
- 44.FDA News Release. [Accessed November 1, 2017];FDA announces comprehensive regulatory plan to shift trajectory of tobacco-related disease, death. 2017 Available at: https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm568923.
- 45.Severson HH, Forrester KK, Biglan A. Use of smokeless tobacco is a risk factor for cigarette smoking. Nicotine Tob Res. 2007;9(12):1331–1337. doi: 10.1080/14622200701705209. [DOI] [PubMed] [Google Scholar]
- 46.Walsh MM, Langer TJ, Kavanagh N, et al. Smokeless tobacco cessation cluster randomized trial with rural high school males: intervention interaction with baseline smoking. Nicotine Tob Res. 2010;12(6):543–550. doi: 10.1093/ntr/ntq022. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.