Abstract
Background
Poor maternal mental health during the postpartum period can have significant effects on the health of mothers, infants, and families. The findings from cross-sectional studies suggest that stress and social support are related to maternal mental health. This study contributes to the literature through the use of longitudinal data and examining moderation and mediation among these factors.
Methods
In 2012–2013, mothers completed surveys assessing stress, social support, and depressive and anxiety symptoms following birth (n=125), and three (n=110) and six months (n=99) after birth. We examined temporal associations, moderation, and mediation of social support on the relationship between stress and postpartum depressive and anxiety symptoms using modified Poisson regression models and the counterfactual approach to mediation.
Results
Current levels of stress and social support were associated with depressive and anxiety symptoms, both independently and when considered together at multiple time points. Social support did not strongly moderate or mediate the relationships between stress and maternal mental health.
Conclusions
Interventions to reduce current perceptions of stress and increase social support for mothers during the postpartum period may help improve maternal mental health symptoms. Efforts are needed to assess the current needs of mothers continuously.
Keywords: Postpartum depression, Postpartum anxiety, Stress, Social Support, Motherhood
INTRODUCTION
During the postpartum period, many mothers oscillate between times of happiness and satisfaction and times of challenge, due to the physical and emotional stressors of labor and delivery, and adjustment to a new maternal role (Britton 2008). The Centers for Disease Control and Prevention (CDC) estimated that about 10–15% of women experience postpartum depressive symptoms, including feelings of hopelessness, lack of interest, or dysphoria, with onset during the first year after delivery (Centers for Disease Control and Prevention 2008). Postpartum anxiety symptoms, including increased autonomic arousal (racing heart, dry mouth, or perspiration) and subjective experiences of anxious feelings, also often occur among new mothers, with an estimated 18% of women experiencing anxiety symptoms during the first three months postpartum (Farr et al. 2014). Depressive and anxiety symptoms during the postpartum period may have substantial short and long-term implications for maternal health, above and beyond the clinical symptoms of the mental health condition Farr et al. 2014, Meltzer-Brody and Stuebe 2014), including physical health symptoms (Farr et al. 2014, O'Hara and McCabe 2013).
Depressive and anxiety symptoms during the postpartum period also have significant implications for the health and development of children and the well-being of families, in part due to the negative influence of the symptoms on maternal parenting behaviors (O'Hara and McCabe 2013). In addition, partners of mothers who experience postpartum depressive or anxiety symptoms are at an increased risk for depression, anxiety, and frequently report feelings of stress, frustration, and hopelessness (Davey, Dziurawiec, and O'Brien-Malone 2006, Tsang et al. 2003). In light of the negative effects for mothers and their families, understanding modifiable factors that may reduce maternal depressive and anxiety symptoms is a public health priority.
Contributing Factors to Postpartum Mental Health
Stress
Exposure to stressors and stress often increase during the postpartum period due to infant care demands and changing social role expectations (Razurel et al. 2011). Exposure to stressful events (stressors) and the individual responses to these challenging situations (stress), may contribute to poor maternal mental health during the postpartum period (Manuel et al. 2012, Thomason et al. 2014). The relationship between stress and mental health may be especially pertinent during the postpartum period as 30% of mothers report experiencing psychological and physiological distress due to their postpartum stress (Rallis et al. 2014).
Stressors are often considered as risk factors for postpartum depression or depressive symptoms, however, a recent review found mixed evidence (Yim et al. 2015). Individual stress responses to stressors vary for many reasons Hankin et al. 2015); therefore, mothers’ levels of perceived stress may be a better predictor of postpartum depressive symptoms (Yim et al. 2015). Prior studies have shown that perceived stress during the prenatal and postpartum periods is associated with high levels of postpartum depressive or anxiety symptoms (Thomason et al. 2014, Britton 2008). For example, mothers experiencing specific types of stress, such as low perceived competence as a parent, had elevated risk for postpartum depressive or anxiety symptoms (Thomason et al. 2014).
Social support
Perceived social support is defined as the belief that members of one's social network will provide resources, such as emotional, informational, and tangible support, when needed (Cohen 1992). Perceived social support is strongly associated with enhanced life satisfaction and improved affect across the life span (Siedlecki et al. 2014). New mothers have reported an increased need for social support during the postpartum period to adjust to the demands of motherhood, such as physical strain, caring for the infant, and balancing work and child care demands (Negron et al. 2013). Although interpersonal interactions within the social network may act as a stressor if too much or too little support is received, social support may be key to maternal mental well-being and recovery during the postpartum period (Negron et al. 2013). For women in the postpartum period, perceptions of sufficient social support from their partners have been associated with decreased maternal and infant distress (Stapleton et al. 2012). Low levels of social support, especially from the mothers’ parents and romantic partners, and high levels of dissatisfaction with the quality of social support during the postpartum period have been associated with an increased risk of postpartum depressive symptoms ( Howell, Mora, and Leventhal 2006, Hildingsson, Tingvall, and Rubertsson 2008). However, it is less clear if low levels of social support directly contribute to an increased risk of depressive or anxiety symptoms or if the effects are a combination of multiple processes. One study found increased levels of social support directly reduced depressive symptoms and also increased mothers’ perceived competence, which further reduced depressive symptoms (Ponomartchouk and Bouchard, 2015).
Social support as a mediator or moderator of stress
It is clear perceived stress and social support are independently strongly associated with postpartum depressive or anxiety symptoms (Jesse, Kim, and Herndon 2014, Manuel et al. 2012, ). However, very few studies have examined the effects of social support on the relationship of stress and postpartum depressive or anxiety symptoms (Razurel et al. 2013). Previous studies also have limited investigation to specific stressful events, such as family conflict, and natural disasters (Lau, Wong, and Fu 2008, Manuel et al. 2012), rather than overall maternal perceptions of stress. The dearth of evidence regarding social support as a moderator or mediator of the relationship between stress and maternal mental health is a significant impediment to intervention development for mothers and their families (Razurel et al. 2013). Understanding if social support is a moderator, a mediator, or both can guide the development of such interventions. Determining if social support is a moderator of the association between stress and postpartum depressive or anxiety symptoms would help clarify which women tend to be negatively affected by stress and assist in tailoring and targeting the intervention to those who are most likely to respond to specific intervention efforts (Chmura Kraemer et al. 2008). In contrast, determining if social support is a mediator between stress and maternal postpartum depressive or anxiety symptoms would help clarify whether stress affects these mental health outcomes and assist in determining what components to include in an intervention (Chmura Kraemer et al. 2008).
Given the significant relationships between poor maternal postpartum mental health and the negative health consequences for mothers, children, and families, it is important to understand potentially modifiable factors that may moderate or mediate the association between stress and maternal depressive or anxiety symptoms so that interventions can be developed to improve maternal mental health outcomes. The purpose of this research was to explore the relation of perceived stress and social support to postpartum depressive and anxiety symptoms and to examine the relation of social support to the association between stress and maternal postpartum depressive and anxiety symptoms.
METHODS
Conceptual Framework
The stress-buffering hypothesis proposed by Cohen and Wills (1985) has been used extensively to examine whether social support is associated with reductions in the potentially adverse effects of stressful events (Biaggi et al. 2016). Cohen and Wills (1985) posited that social support directly contributed to well-being through enhancing positive affect and perceived self-worth (main effect). However, social support may also indirectly improve well-being by mitigating potentially stressful situations or by attenuating the impacts of stressful situations (buffering effect) (Cohen and Wills 1985).
In our application of the stress-buffering hypothesis for postpartum depressive and anxiety symptoms, we expected that mothers with high levels of perceived stress would have increased risk of above normal depressive or anxiety symptoms. Conversely, we expected that mothers with high perceived social support would have reduced risk of above normal depressive or anxiety symptoms. We also hypothesized that high levels of social support would mediate and moderate the effects of high levels of stress on depressive or anxiety symptoms.
Study population
After receiving approval from the local Institutional Review Board, women were recruited from a large hospital in Iowa within 48 hours of having live birth. To be eligible for the study, women had to: be at least 18 years old and able to speak and read English. Women with multiple births and/or birth complications were not excluded from participation.
Research assistants visited the mother/baby unit three times per week between October and December 2012. They approached mothers who met the eligibility criteria (live birth in past 48 hours; age 18 years or greater; English proficiency), explained the study, and asked if they were interested in participating. Door markers were used to identify mothers who were not currently available (sleeping, provider visiting, etc.) to meet with researchers. Each recruiting session ended when all eligible, available mothers were invited to participate.
Following the provision of written and signed informed consent, all participants completed the first survey using self-administered paper-and-pencil or online methods (Harris et al. 2009). A tablet computer was available to participants who wished to complete the survey online. Participants completed follow-up surveys three and six months after birth via the method chosen at enrollment. Participants were contacted to complete a follow-up survey only if they had completed a survey at the preceding time point. Given that nurses initially identified potentially eligible individuals, it is unclear how many women were eligible for this study during the enrollment period. Although the protocol was to record the number of women approached during each recruiting session and the number of women enrolled, research assistants did not consistently record this information. Based on the available reports, 70% of women who were invited enrolled in the study. A total of 125 mothers enrolled in the study and completed the first survey. Approximately 10% were lost to follow-up at each subsequent survey (three month: 15 lost to follow-up, n=110; six month: 11 lost to follow-up, n=99). Based on the power calculations for the primary research question for this study, we aimed to recruit 104 mothers, which, after accounting for loss to follow-up, had 80% power to detect modest beta estimates of at least 0.30 with a two-sided alpha equal to 0.05.
Measures
Depressive and Anxiety Symptoms
Mothers reported their depressive and anxiety symptoms using the short form Depression, Anxiety, and Stress Scales (DASS–21) (Lovibond and Lovibond 1995). In the first survey following birth, participants reported their experiences during pregnancy. In the three- and six-month follow-up surveys, participants reported their experiences in the past three months.
The depressive and anxiety subscales of the DASS-21 included seven questions focused on each type of negative emotional symptom. Participants reported the frequency of experiencing each symptom on a scale from 0 (“never”) to 3 (“almost always”), with summed scores across the seven subscale items ranging from 0 to 21. In the current sample, Cronbach’s alpha for the three time points ranged from 0.76 to 0.88 for depressive symptoms and 0.52 to 0.64 for anxiety symptoms. Scores were not normally distributed, thus, for the purposes of this study, each depressive and anxiety symptom score was dichotomized as a normal experience of negative emotions or as a higher than normal experience of negative emotions using the cut-off scores (5 for depressive symptoms, 4 for anxiety symptoms) suggested by the scale developers (Lovibond and Lovibond 1995).
The DASS-21 has been successfully used to assess increased negative emotional symptoms among postpartum women (Cunningham et al. 2013). In prior validation studies, the depressive and anxiety symptom subscales were highly correlated with the Beck Depression Inventory and the Beck Anxiety Inventory (Lovibond and Lovibond 1995).
Stress
Maternal perception of stress, or the extent to which a participant felt mental or emotional strain, irritability, or a tendency to respond disproportionately to stressful situations (Antony et al. 1998) was assessed during the initial survey and at three and six months postpartum using the stress subscale of the DASS-21 (Lovibond and Lovibond 1995). Participants reported their experiences of seven situations, such as feeling touchy, intolerant of distractions, and agitated on a scale from 0 (“never”) to 3 (“almost always”), with summed scores across the seven items ranging from 0 to 21. In this sample, Cronbach’s alpha scores for the stress subscale ranged from 0.81 to 0.84 at the three time points. Stress was modeled as a continuous variable, with higher scores indicating a greater experience of stress. The DASS-21 has been successfully used to assess increased negative stress symptoms with postpartum women ( Cunningham et al. 2013). Prior research indicated that the three subscales of the DASS measured three distinct categories of negative emotional symptoms (Sinclair et al. 2012) and should be considered separately to understand the nature of psychological well-being (Shea, Tennant, and Pallant 2009). Multiple authors have hypothesized a relationship of high stress levels and heightened depressive and anxiety symptoms during the postpartum period, which may explain the correlation between the subscales (Thomason et al. 2014, Groer and Morgan 2007, Britton 2008)
Social Support
The RAND Medical Outcomes Study Social Support Survey (MOS-SSS) is a 19-item scale that measures different types of support. Participants rated their perceptions of support availability on a scale from 1 (“none of the time”) to 5 (“all of the time”). This study included the emotional/informational support, affectionate support, and positive social interaction subscales. Social support was modeled as the average score across the 19-items. The Cronbach’s alpha scores suggested a high degree of internal consistency on the overall scale at each of the three time points (range: 0.97–0.98). The MOS-SSS has been successfully used with a wide range of populations, including postpartum women (Da Costa et al. 2010).
Statistical Analysis
Univariate analyses were used to describe the demographic composition and psychological well-being of the sample. Bivariate analyses of depressive and anxiety symptoms by time were used to graph the changes in maternal psychological well-being during the first six months of the postpartum period to examine the heterogeneity of experiences across time.
Next, modified Poisson regression models proposed by Zou (Zou 2004) were used to calculate the crude relative risk for experiencing depressive or anxiety symptoms at three or six months postpartum for a one-unit increase in the average score on the MOS-SSS (social support) and total stress score in each of the previous time points. These analyses were followed by a series of multivariable modified Poisson regression models (Zou 2004) to examine further the key relationship. To control for the association of prior social support with current social support, the relative risks were adjusted for social support in all prior time points (e.g., the relative risk for depressive symptoms at 6 months after delivery was adjusted for social support reported at birth and 3 months). Similar relative risk estimates were calculated for stress, adjusted for perceived stress at prior time points. Adjusting for the score at prior time points also clarified the temporal relationship between support or stress and maternal mental health. The next model was adjusted for both social support and stress during the same time period and maternal age, education, and mental health symptoms reported after delivery.
Moderation, the extent to which the relationship between stress and maternal mental health was altered by social support, was assessed by adding an interaction between stress and social support to the models. Moderations models were calculated with stress and social support as continuous variables, which were consistent with earlier results, and also with stress as a continuous variable and social support as a dichotomous variable split at the mean score. The direction and significance of the results of the two models were the same, and the Akaike Information Criterion (Akaike, 1974) of the two models were also similar; thus, we present the simplified analysis with social support as a dichotomous variable.
Mediation, the extent to which social support is part of the causal pathway between stress and maternal mental health, was assessed using the counterfactual approach to mediation through the SAS macro developed by Valeri and VenderWeele (VanderWeele 2015). The counterfactual approach extends the product method approach to mediation developed by Baron and Kenny (1986) to allow for the calculation of total effects as the sum of the direct and indirect effects in the presence of nonlinearities (Valeri and VanderWeele 2013). The log-linear mediation models failed to converge; thus, we used logistic regression for modeling these relationships and reported the odds ratios (OR) and 95% confidence intervals (CI) produced by these models.
Based on the literature review and a directed acyclic graph (DAG), a visual method of selecting potential confounders to avoid introduction of conditional bias (Shrier and Platt 2008), we included prenatal depressive or anxiety symptoms, education, and age as covariates. All analyses were conducted using SAS version 9.4.
RESULTS
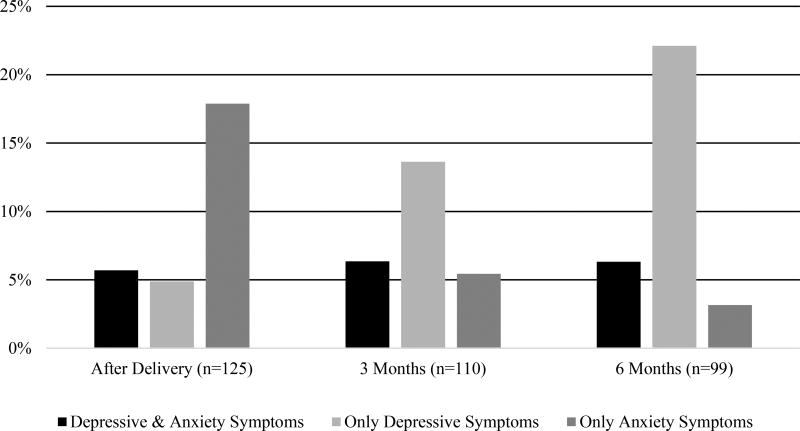
On average, mothers were 30 years old (mean=29.7 years; SD=5.6 years), and the majority (62%) had multiple children (Table 1). As was consistent with the demographic characteristics of the surrounding community, the majority of mothers were white (76%), non-Hispanic (94%), and had earned some college credit (86%). The proportion of mothers who experienced only above-normal depressive symptoms (i.e., normal anxiety levels, heightened depressive symptoms) increased over time (Figure 1). In contrast, the proportion of mothers who experienced only above-normal anxiety symptoms (i.e., normal depressive symptoms, heightened anxiety symptoms) decreased over time. Approximately 5% of mothers reported above-normal symptoms of depressive and anxiety at each of the data collection points. The scores for perceptions of social support ranged from 1 to 5, with 5 indicating higher perception of social support. The mean social support scores after delivery (mean=4.57, sd=0.63), at three-months postpartum (mean=4.27, sd=0.81), and at six-months postpartum (mean=4.40, sd=0.78) were high (Table 2). Stress scores ranged from 0 to 21, with a higher score indicating higher perceptions of stress. The mean stress scores ranged from 4.59 to 4.86 across the three time points, indicating modest levels of stress over the three time periods.
Table 1.
Demographic characteristics of the sample (n=125)
| Demographic Characteristics | Mean (sd) or Numbera (%) |
|---|---|
| Age (in years) | 29.7 (sd=5.6) |
| Race | |
| Non-White | 30 (24.00) |
| White | 95 (76.00) |
| Ethnicity | |
| Hispanic | 7 (5.60) |
| Non-Hispanic | 118 (94.40) |
| Relationship Status after Delivery | |
| Single | 9 (7.44) |
| In a Relationship | 112 (92.56) |
| Parity | |
| First Child | 47 (37.90) |
| Multiple Children | 77 (62.10) |
| Education | |
| High School Diploma or Less | 17 (13.60) |
| At Least Some College Credit | 108 (86.40) |
| Initiated Breastfeeding | |
| Yes | 97 (88.18) |
| No | 13 (11.82) |
Range from 110 to 125 due to missing data
Figure 1.
Proportion of Mothers Reporting Above Normal Depressive and Anxiety Symptoms
Table 2.
Exposure, mediator/moderator, and outcome characterstics
| Mental Health Symptomsa | Mean (sd) |
|---|---|
| Scores after Delivery | |
| Depressive Symptom Subscale | 2.05 (2.08) |
| Anxiety Symptom Subscale | 2.12 (2.06) |
| Three-month Scores | |
| Depressive Symptom Subscale | 2.46 (2.29) |
| Anxiety Symptom Subscale | 1.45 (1.62) |
| Six-month Scores | |
| Depressive Symptom Subscale | 2.89 (3.07) |
| Anxiety Symptom Subscale | 1.38 (1.76) |
|
| |
| Social Support Experiencesb | |
|
| |
| After Delivery Social Support | 4.57 (0.63) |
| Three-month Social Support | 4.27 (0.81) |
| Six-month Social Support | 4.40 (0.78) |
|
| |
| Stress Experiencesc | |
|
| |
| Scores after Delivery | 4.85 (2.95) |
| Three-month Scores | 4.59 (2.89) |
| Six-month Scores | 4.86 (3.23) |
Possible scores range from 0 to 21;
Possible scores range from 1 to 5;
Possible scores range from 0 to 21
In unadjusted analyses, higher levels of social support reported after delivery and at three months postpartum were associated with a decreased risk of experiencing above-normal depressive symptoms at three-months postpartum (Table 3). For above-normal depressive symptoms at six-months postpartum, only higher social support reported after delivery was associated with reduced risk. Social support was not strongly associated with anxiety symptoms at three or six months postpartum; however, higher social support reported at three months postpartum was significantly associated with reduced risk of above-normal three-month anxiety symptoms.
Table 3.
Temporal relative risks (RR) and 95% confidence intervals (CI) for stress and social support in relation to maternal depressive or anxiety symptoms
| Depressive Symptoms RR (95% CI) |
Anxiety Symptoms RR(95% CI) |
|||
|---|---|---|---|---|
| 3 Months After Delivery |
6 Months After Delivery |
3 Months After Delivery |
6 Months After Delivery |
|
| Unadjusted Relative Risk | ||||
|
| ||||
| Social Supporta | ||||
| After Delivery | 0.62 (0.49–0.80) | 0.73 (0.87–0.92) | 0.85 (0.47–1.54) | 0.87 (0.36–2.12) |
| 3 Months | 0.56 (0.44–0.71) | 0.81 (0.61–1.07) | 0.61 (0.41–0.89) | 0.67 (0.35–1.27) |
| 6 Months | -- | 0.77 (0.56–1.04) | -- | 0.62 (0.36–1.07) |
| Stressb | ||||
| After Delivery | 1.22 (1.10–1.34) | 1.15 (1.04–1.26) | 1.20 (1.05–1.37) | 1.26 (1.05–1.51) |
| 3 Months | 1.38 (1.27–1.50) | 1.19 (1.09–1.30) | 1.20 (0.99–1.47) | 1.21 (1.04–1.41) |
| 6 Months | -- | 1.19 (1.10–1.28) | -- | 1.22 (1.15–1.29) |
|
| ||||
| Relative Risk adjusted for Prior Experiencesc | ||||
|
| ||||
| Social Supporta | ||||
| After Delivery | 1.02 (0.72–1.45) | 0.88 (0.61–1.27) | 1.36 (0.69–2.69) | 1.24 (0.42–3.72) |
| 3 Months | 0.52 (0.38–0.71) | 0.97 (0.61–1.53) | 0.52 (0.33–0.82) | 0.71 (0.26–2.00) |
| 6 Months | -- | 0.79 (0.48–1.31) | -- | 0.77 (0.34–1.75) |
| Stressb | ||||
| After Delivery | 1.07 (0.72–1.25) | 0.84 (0.74–0.96) | 1.13 (0.94–1.36) | 0.78 (0.57–1.05) |
| 3 Months | 1.35 (1.21–1.50) | 1.15 (1.06–1.25) | 1.13 (0.87–1.47) | 1.21 (1.00–1.44) |
| 6 Months | -- | 1.27 (1.17–1.39) | -- | 1.39 (1.16–1.67) |
|
| ||||
| Model 1d | ||||
|
| ||||
| Social Supporta | 0.53 (0.40–0.72) | 0.86 (0.65–1.15) | 0.65 (0.40–1.00) | 0.59 (0.31–1.11) |
| Stressb | 1.39 (1.26–1.54) | 1.16 (1.06–1.26) | 1.19 (0.96–1.49) | 1.08 (0.96–1.22) |
One Point Increase in Average Social Support Score,
One Point Increase in Stress Score;
Social support variables adjusted for prior time period(s) social support, stress variables adjusted for prior time period(s) stress;
Adjusted for maternal age, maternal education, maternal after delivery mental health symptoms, and stress and social support during the same time period
Overall, in unadjusted analyses, higher perceived levels of stress were associated with an increased risk of above normal depressive and anxiety symptoms (Table 3). However, three-month stress scores were not significantly associated with above-normal anxiety symptoms at three-months postpartum. In contrast to the social support relationship, stress at prior time points was significantly associated with future reports of depressive and anxiety symptoms.
Table 4.
Moderation of the relative risks (RR) (with 95% confidence intervals (CI)) of stress in relation to depressive or anxiety symptoms by social supporta
| High Social Support RR (95% CI) |
Low Social Support RR (95% CI) |
RR (95% CI) by social support within strata of stress |
|
|---|---|---|---|
| Three Month Depressive Symptomsb | |||
|
| |||
| 3rd Quartile Stress Score | 0.83 (0.35–1.96) | 1.62 (1.33–1.97) | 0.52 (0.22–1.19) |
| Median Stress Score | 0.34 (0.11–1.09) | Ref | 0.34 (0.11–1.09) |
| 1st Quartile Stress Score | 0.14 (0.03–0.68) | 0.62 (0.51–0.76) | 0.23 (0.05–1.11) |
|
| |||
| Six Month Depressive Symptomsc | |||
|
| |||
| 3rd Quartile Stress Score | 0.92 (0.49–1.71) | 1.26 (1.07–1.48) | 0.73 (0.40–1.33) |
| Median Stress Score | 0.46 (0.22–0.97) | Ref | 0.46 (0.22–0.97) |
| 1st Quartile Stress Score | 0.23 (0.09–0.59) | 0.80 (0.67–0.94) | 0.29 (0.10–0.78) |
|
| |||
| Three Month Anxiety Symptomsb | |||
|
| |||
| 3rd Quartile Stress Score | 0.46 (0.09–2.33) | 1.59 (103–2.44) | 0.29 (0.06–1.39) |
| Median Stress Score | 0.35 (0.9–41.29) | Ref | 0.35 (0.10–1.29) |
| 1st Quartile Stress Score | 0.26 (0.06–1.18) | 0.63 (0.41–0.97) | 0.41 (0.07–2.34) |
|
| |||
| Six Month Anxiety Symptomsb | |||
|
| |||
| 3rd Quartile Stress Score | 0.40 (0.06–2.69) | 1.49 (1.26–1.76) | 0.27 (0.04–1.82) |
| Median Stress Score | 0.20 (0.02–2.26) | Ref | 0.20 (0.02–2.26) |
| 1st Quartile Stress Score | 0.10 (0.01–1.93) | 0.67 (0.57–0.79) | 0.15 (0.01–2.84) |
Adjusted for maternal age, depressive or anxiety symptoms at birth, and maternal education;
Interaction term not significant at p<0.05;
Interaction term significant at p<0.01
Adjusting for prior reports of social support at three months postpartum, higher current perceptions of social support were associated with significantly reduced risk of above-normal depressive and anxiety symptoms (Table 3). Social support was not significantly associated with six-month depressive or anxiety symptoms after controlling for past reported social support. At three months postpartum, higher current stress was associated with above-normal depressive symptoms but was not associated with above-normal anxiety symptoms, controlling for current and past reported stress. High stress reported at each time point was significantly associated with six-month above-normal depressive symptoms. Contrary to the rest of the findings, increased stress reported after delivery was associated with lower risk of above-normal depressive symptoms after controlling for stress reported at each time-point. Increased stress at three and six months postpartum was associated with significantly increased risk of above-normal depressive symptoms at six months postpartum. Increased stress at six months postpartum was associated with increased risk of above-normal anxiety symptoms at six-months postpartum.
Adjusting for stress and social support reported during the same time period and for the covariates of maternal age, maternal education, and maternal reported depressive or anxiety symptoms after delivery, at three months postpartum, higher perceptions of stress and lower perceptions of social support were significantly associated with above-normal postpartum depressive symptoms (Table 3, Model 1 ). At six months postpartum, only increased stress was significantly associated with above-normal depressive symptoms. At three months postpartum, only increased social support was associated with reduced risk of above-normal anxiety symptoms. Neither stress, nor social support was significantly associated with six-month postpartum anxiety symptoms.
Moderation analysis
Overall, evidence to support moderation of the relationship between stress and depressive or anxiety symptoms by social support was limited after controlling for maternal age, education, and depressive or anxiety symptoms reported at birth (Table 4), except for depressive symptoms at six -months (p<0.01). The adjusted relative risk (aRR) of experiencing depressive symptoms at six months was significantly lower (aRR: 0.29; 95% CI: 0.10–.78) among mothers with high social support in the first quartile of stress score, compared with mothers with low social support in the first quartile of the stress scores. In contrast, social support was not significantly protective against depressive symptoms among mothers in the third quartile of stress scores (aRR:0.73; 95% CI: 0.40–1.33). For three-month depressive and anxiety symptoms and six-month anxiety symptoms, the relations of stress to symptoms did not significantly differ by level of social support.
Mediation analysis
For the mediation models (Table 5), the direct effect, which was significant across depressive or anxiety symptoms, was interpreted as the odds of above normal depressive or anxiety symptoms for a change from the 25th percentile to the 75th percentile of the stress scale scores, assuming social support was constant and controlling for maternal age, maternal education, and depressive or anxiety symptoms report following birth. The direct effect measured the relation of stress to depressive or anxiety symptoms if we disabled the pathway from stress to social support. The indirect effect, the association of stress with depressive or anxiety symptoms by changing social support, was also significant for three-month depressive symptoms, and three- and six-month anxiety symptoms. Finally, the total association, which was also significant across depressive and anxiety symptoms, was the overall change in depressive or anxiety symptoms based on changing stress score from the 25th percentile to the 75th percentile. Overall, the direct relations of stress to depressive and anxiety symptoms explained a much higher proportion of the total than the indirect effects, which suggested that mediation by social support was minimal.
Table 5.
Mediation of odds ratios (OR) with 95% confidence intervals (CI) for the association of stress with depressive or anxiety symptoms by social supporta
| Depressive Symptoms | Anxiety Symptoms | |||
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | |||
| 3 Months After Delivery |
6 Months After Delivery |
3 Months After Delivery |
6 Months After Delivery |
|
| Mediation | ||||
|
| ||||
| Direct Effect | 5.85 (2.67–12.83) | 147.63 (73.57–296.21) | 1.84 (1.45–2.34) | 22.92 (9.49–55.37) |
| Indirect Effect | 1.11 (1.03–1.21) | 1.00 (0.95–1.05) | 1.04 (1.01–1.06) | 1.12 (1.04–1.21) |
| Total Effect | 6.51 (2.95–14.37) | 147.93 (73.7–296.89) | 1.91 (1.50–2.43) | 25.67 (10.41–63.33) |
Adjusted for maternal age, depressive or anxiety symptoms at birth, and maternal education
DISCUSSION
The purpose of this research was to explore the relations of perceived stress and social support to postpartum depressive and anxiety symptoms and to examine the associations of social support with the relationship between stress and maternal postpartum depressive and anxiety symptoms. Although much research has supported the relationship of stress and social support to maternal mental health, limited research has examined the temporal relationships and the combined effects of stress and social support on maternal mental health.
Stress
In this study, increased levels of stress were associated with increased risk of above-normal depressive and anxiety symptoms during the postpartum period. Overall, the current stress level measured at the same time was significantly associated with anxiety and depressive symptoms, adjusting for prior stress. This finding was consistent with prior research showing that maternal stress was associated with increased depressive symptoms related to the novel stressors related to caring for an infant (Mott et al. 2011) and may suggest that stress has an important relation to depressive and anxiety symptoms. Thus, ongoing stress reduction interventions during the postpartum period may be an effective way to improve maternal mental health. Because our data showed that the associations of stress with depressive and anxiety symptoms may change over time, it may be necessary to tailor the intervention to maternal stress throughout the postpartum period.
Social Support
In this sample of mothers, positive social support was associated with reduced risk of depressive and anxiety symptoms at three-months postpartum. These associations persisted after adjusting for social support, perceived stress, and depressive or anxiety symptoms at earlier time points, maternal age, and maternal education. Prior cross-sectional research suggested social support improves maternal mental health outcomes during the postpartum period (Boury, Larkin, and Krummel 2004, Howell, Mora, and Leventhal 2006, ), which was consistent with our findings. Our results showed that current perceptions of social support were associated with depressive and anxiety symptoms at three-months postpartum, but social support was not protective against depressive or anxiety symptoms at six-months postpartum. The significant relationships between current perceptions of social support and maternal mental health in the early postpartum period highlight the relative importance of current social support needs compared with previous support received, which may suggest maternal experience of and need for social support changes over time (Asselmann et al. 2016). Given the importance of social support in our findings and the prior literature, interventions using social support to reduce depressive and anxiety symptoms during the postpartum period may be most effective if they are provided at multiple points during the period and are flexible to meet the specific needs of the mothers across time. Additional research may further clarify the characteristics of social support desired by mothers across the postpartum period, such as what type of social support is needed, who best provides the support, and when support is most helpful (House 1981).
Moderation and Mediation of Stress and Social Support
Our findings do not support social support as a moderator or mediator of the relationship between stress and depressive and anxiety symptoms. Both stress and social support were associated with maternal mental health during the early postpartum period; so, it may be necessary to address both issues in interventions among new mothers. At six-months postpartum, social support did significantly moderate the association between stress and depressive symptoms, which may suggest social support should continue to be the focus on interventions to reduce depressive symptoms. Social support may be addressed through interventions, such as the Mothers’ Advocates in the Community, a promising intervention that pairs a new mothers with a non-professional mentor during the postpartum period (Taft et al. 2011). Mindfulness-based interventions also show promise in improving mental health during the postpartum period through reducing the effects of stressors (Vieten and Astin 2008). Despite the independent pathways of effect of social support and stress on maternal mental health, it may be possible to tailor an intervention to mothers to address both perceptions of social support and stress. For example, a novel intervention could combine the mentoring from Mothers’ Advocates in the Community with teaching mindfulness-based interventions.
Limitations
This study sample was relatively homogeneous (i.e., predominately white race with above average education), reflecting the community in which this study was conducted, but potentially reducing the generalizability of results. While mothers were followed for six months after birth of the infant, it is possible that the relationships between stress, social support, and postpartum depressive and anxiety symptoms changed during the remainder of the postpartum period that was not included in the study. However, this study captured one of the most stressful periods, immediately after birth, when mothers are adjusting to the care of new infants (Mulsow et al. 2002).
Although previous studies reported good internal consistency of the DASS anxiety subscale in postpartum samples (Cunningham et al. 2013), it was lower than expected in this sample and thus could have resulted in misclassification or inaccuracy of results. The low alpha score may indicate that the anxiety measure captured multiple facets of emotional distress rather than a single indicator of anxiety, or that the DASS-21 is not an appropriate measure of post-partum anxiety. Future research using the DASS-21 may consider including another measure of anxiety to gain additional information. Finally, the study may have been insufficiently powered to detect moderation and mediation effects. Future research with a larger, more diverse sample and longer follow-up period may be necessary to examine these complex relationships further.
Implications
This study is among the first to examine the relationships of social support and stress with maternal depressive and anxiety symptoms across multiple time points during the early postpartum period, examining the potential combined impacts of social support and stress (Razurel et al. 2013). Our findings highlight the importance of interventions during the early postpartum periods to reduce stress and increase social support to improve mothers’ mental health. Considering that stressors and support needs change over time, future research should identify the types of stressors and support relevant to each time point, including what type of social support is needed and who should provide the support to have the greatest effect on maternal mental health.
Acknowledgments
This project was funded, in part, by the University of Iowa Heartland Center for Occupational Health and Safety. The Institute for Clinical and Translational Science at the University of Iowa is supported by the National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) program, grant U54TR001356. The CTSA program is led by the NIH’s National Center for Advancing Translational Sciences (NCATS). This publication's contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
References
- Akaike Hirotugu. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19(6):716–23. [Google Scholar]
- Antony Martin M, Bieling Peter J, Cox Brian J, Enns Murray W, Swinson Richard P. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment. 1998;10(2):176–181. [Google Scholar]
- Asselmann E, Wittchen H-U, Erler L, Martini J. Peripartum changes in social support among women with and without anxiety and depressive symptoms prior to pregnancy: a prospective-longitudinal study. Archieves of Women's Mental Health. 2016 doi: 10.1007/s00737-016-0608-6. [DOI] [PubMed] [Google Scholar]
- Baron Reuben M, Kenny David A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Biaggi Alessandra, Conroy Susan, Pawlby Susan, Pariante Carmine M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. Journal of Affective Disorders. 2016;191:62–77. doi: 10.1016/j.jad.2015.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton John R. Maternal anxiety: course and antecedents during the early postpartum period. Depression and Anxiety. 2008;25(9):793–800. doi: 10.1002/da.20325. [DOI] [PubMed] [Google Scholar]
- Chmura Kraemer Helena, Kiernan Michaela, Essex Marilyn, Kupfer David J. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychology. 2008;27(2S):S101–8. doi: 10.1037/0278-6133.27.2(Suppl.).S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen Sheldon. Stress, social support, and disorder. In: Veiel HOF, Baumann U, editors. The Meaning and Measurement of Social Support. New York: Hemisphere Press; 1992. pp. 109–124. [Google Scholar]
- Cohen Sheldon, Wills Thomas A. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98(2):310–57. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Prevalence of self-reported postpartum depressive symptoms--17 states, 2004–2005. MMWR. Morbidity and Mortality Weekly Report. 2008;57(14):361–6. [PubMed] [Google Scholar]
- Cunningham Nadia K, Brown Philippa M, Brooks Janette, Page Andrew C. The structure of emotional symptoms in the postpartum period: Is it unique? Journal of Affective Disorders. 2013;151(2):686–694. doi: 10.1016/j.jad.2013.08.002. [DOI] [PubMed] [Google Scholar]
- Da Costa Deborah, Dritsa Maria, Verreault Nancy, Balaa Caline, Kudzman Jennifer, Khalifé Samir. Sleep problems and depressed mood negatively impact health-related quality of life during pregnancy. Archives of Women's Mental Health. 2010;13(3):249–257. doi: 10.1007/s00737-009-0104-3. [DOI] [PubMed] [Google Scholar]
- Davey SJ, Dziurawiec S, O'Brien-Malone A. Men's voices: postnatal depression from the perspective of male partners. Qualitative Health Research. 2006;16(2):206–20. doi: 10.1177/1049732305281950. [DOI] [PubMed] [Google Scholar]
- Farr Sherry L, Dietz Patricia M, O'Hara Michael W, Burley Kim, Ko Jean Y. Postpartum anxiety and comorbid depression in a population-based sample of women. Journal of Women's Health. 2014;23(2):120–128. doi: 10.1089/jwh.2013.4438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groer MW, Morgan K. Immune, health and endocrine characteristics of depressed postpartum mothers. Psychoneuroendocrinology. 2007;32(2):133–9. doi: 10.1016/j.psyneuen.2006.11.007. [DOI] [PubMed] [Google Scholar]
- Hankin Benjamin L, Badanes Lisa S, Smolen Andrew, Young Jami F. Cortisol reactivity to stress among youth: Stability over time and genetic variants for stress sensitivity. Journal of Abnormal Psychology. 2015;124(1):54–67. doi: 10.1037/abn0000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris Paul A, Taylor Robert, Thielke Robert, Payne Jonathon, Gonzalez Nathaniel, Conde Jose G. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildingsson Ingegerd, Tingvall Maria, Rubertsson Christine. Partner support in the childbearing period—A follow up study. Women and Birth. 2008;21(4):141–148. doi: 10.1016/j.wombi.2008.07.003. [DOI] [PubMed] [Google Scholar]
- House JS. Work Stress and Social Support. Reading, MA: Addision-Wesley Publishing; 1981. [Google Scholar]
- Howell EA, Mora P, Leventhal H. Correlates of early postpartum depressive symptoms. Maternal and Child Health Journal. 2006;10(2):149–57. doi: 10.1007/s10995-006-0116-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jesse D Elizabeth, Kim Heejung, Herndon Cynthia. Social Support and Self-Esteem as Mediators Between Stress and Antepartum Depressive Symptoms in Rural Pregnant Women. Research in Nursing & Health. 2014;37(3):241–252. doi: 10.1002/nur.21600. [DOI] [PubMed] [Google Scholar]
- Lau Ying, Wong Keung, Daniel Fu. The role of social support in helping Chinese women with perinatal depressive symptoms cope with family conflict. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2008;37(5):556–571. doi: 10.1111/j.1552-6909.2008.00273.x. [DOI] [PubMed] [Google Scholar]
- Lovibond Peter F, Lovibond Sydney H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Manuel Jennifer I, Martinson Melissa L, Bledsoe-Mansori Sarah E, Bellamy Jennifer L. The influence of stress and social support on depressive symptoms in mothers with young children. Social Science & Medicine. 2012;75(11):2013–2020. doi: 10.1016/j.socscimed.2012.07.034. [DOI] [PubMed] [Google Scholar]
- Meltzer-Brody Samantha, Stuebe Alison. The long-term psychiatric and medical prognosis of perinatal mental illness. Best Practice & Research Clinical Obstetrics & Gynaecology. 2014;28(1):49–60. doi: 10.1016/j.bpobgyn.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mott Sarah L, Schiller Crystal Edler, Richards Jenny Gringer, O’Hara Michael W, Stuart Scott. Depression and anxiety among postpartum and adoptive mothers. Archives of Women's Mental Health. 2011;14(4):335–343. doi: 10.1007/s00737-011-0227-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulsow Miriam, Caldera Yvonne M, Pursley Marta, Reifman Alan, Huston Aletha C. Multilevel factors influencing maternal stress during the first three years. Journal of Marriage and Family. 2002;64(4):944–956. [Google Scholar]
- Negron R, Martin A, Almog M, Balbierz A, Howell EA. Social support during the postpartum period: mothers' views on needs, expectations, and mobilization of support. Maternal and Child Health Journal. 2013;17(4):616–23. doi: 10.1007/s10995-012-1037-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annual Review of Clinical Psychology. 2013;9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612. [DOI] [PubMed] [Google Scholar]
- Ponomartchouk Daria, Bouchard Geneviève. New mothers' sense of competences: predictors and outcomes. Journal of Child and Family Studies. 2015;24(7):1977–86. [Google Scholar]
- Rallis Sofia, Skouteris Helen, McCabe Marita, Milgrom Jeannette. The transition to motherhood: towards a broader understanding of perinatal distress. Women and Birth. 2014;27(1):68–71. doi: 10.1016/j.wombi.2013.12.004. [DOI] [PubMed] [Google Scholar]
- Razurel C, Bruchon-Schweitzer M, Dupanloup A, Irion O, Epiney M. Stressful events, social support and coping strategies of primiparous women during the postpartum period: a qualitative study. Midwifery. 2011;27(2):237–242. doi: 10.1016/j.midw.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Razurel C, Kaiser B, Sellenet C, Epiney M. Relation between perceived stress, social support, and coping strategies and maternal well-being: a review of the literature. Women & Health. 2013;53(1):74–99. doi: 10.1080/03630242.2012.732681. [DOI] [PubMed] [Google Scholar]
- Shea Tracey L, Tennant Alan, Pallant Julie F. Rasch model analysis of the Depression, Anxiety and Stress Scales (DASS) BMC Psychiatry. 2009;9(1):21–31. doi: 10.1186/1471-244X-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrier Ian, Platt Robert W. Reducing bias through directed acyclic graphs. BMC Medical Research Methodology. 2008;8(1):70–85. doi: 10.1186/1471-2288-8-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siedlecki Karen L, Salthouse Timothy A, Oishi Shigehiro, Jeswani Sheena. The relationship between social support and subjective well-being across age. Social Indicators Research. 2014;117(2):561–576. doi: 10.1007/s11205-013-0361-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair Samuel Justin, Siefert Caleb J, Slavin-Mulford Jenelle M, Stein Michelle B, Renna Megan, Blais Mark A. Psychometric evaluation and normative data for the depression, anxiety, and stress scales-21 (DASS-21) in a nonclinical sample of US adults. Evaluation & the Health Professions. 2012;35(3):259–279. doi: 10.1177/0163278711424282. [DOI] [PubMed] [Google Scholar]
- Stapleton LR, Schetter CD, Westling E, Rini C, Glynn LM, Hobel CJ, Sandman CA. Perceived partner support in pregnancy predicts lower maternal and infant distress. Journal of Family Psychology. 2012;26(3):453–63. doi: 10.1037/a0028332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taft Angela J, Small Rhonda, Hegarty Kelsey L, Watson Lyndsey F, Gold Lisa, Lumley Judith A. Mothers' AdvocateS In the Community (MOSAIC)-non-professional mentor support to reduce intimate partner violence and depression in mothers: a cluster randomised trial in primary care. BMC Public Health. 2011;11(1):178–88. doi: 10.1186/1471-2458-11-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomason Elizabeth, Volling Brenda L, Flynn Heather A, McDonough Susan C, Marcus Sheila M, Lopez Juan F, Vazquez Delia M. Parenting stress and depressive symptoms in postpartum mothers: Bidirectional or unidirectional effects? Infant Behavior and Development. 2014;37(3):406–415. doi: 10.1016/j.infbeh.2014.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsang HW, Tam PK, Chan F, Cheung WM. Sources of burdens on families of individuals with mental illness. International Journal of Rehabilitation Research. 2003;26(2):123–30. doi: 10.1097/00004356-200306000-00007. [DOI] [PubMed] [Google Scholar]
- Valeri Linda, VanderWeele Tyler J. Mediation analysis allowing for exposure–mediator interactions and causal interpretation: Theoretical assumptions and implementation with SAS and SPSS macros. Psychological Methods. 2013;18(2):137–50. doi: 10.1037/a0031034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vieten C, Astin J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Archives of Women's Mental Health. 2008;11(1):67–74. doi: 10.1007/s00737-008-0214-3. [DOI] [PubMed] [Google Scholar]
- Yim Ilona S, Tanner Stapleton Lynlee R, Guardino Christine M, Hahn-Holbrook Jennifer, Dunkel Schetter Christine. Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Clinical Psychology. 2015;11(1):99–137. doi: 10.1146/annurev-clinpsy-101414-020426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou Guangyong. A modified poisson regression approach to prospective studies with binary data. American Journal of Epidemiology. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]