Abstract
The stigma of drug addiction is associated with negative perceptions and can be a barrier to treatment. With the rise in opioid overdose deaths, understanding stigmatizing attitudes towards individuals who use opioids is a crucial matter. There is a lack of opioid use research on stigma and, therefore, we aimed to discern stigmatizing attitudes towards people with opioid addiction. A randomized, between-subjects case vignette study (n = 2,605) was conducted with a nation-wide online survey. Participants rated a hypothetical individual addicted to opioids on different dimensions of stigma after seeing one version of a vignette that varied by three conditions: 1) a male versus a female, 2) an individual labeled as being a “drug addict” versus having an “opioid use disorder” and 3) an individual whose use started by taking prescription opioids from a friend versus receiving a prescription from a doctor. Our results indicated that there were higher stigmatizing attitudes overall towards a male, an individual labeled as a “drug addict” and an individual who took prescription opioids from a friend. Interaction effects also showed that a female labeled with an “opioid use disorder” and male labeled as a “drug addict” was rated with higher stigma. The findings from our study are the first to show that information about gender, precipitating events and language matter when assessing stigma and opioid use and may affect the delivery of patient care.
Keywords: Opioids, Stigma, Opioid Use Disorder, Nonmedical Prescriptions, Gender, Language
1. Introduction
The opioid epidemic in the United States is a growing public health concern. Since 1999, the sales of prescription opioids have nearly quadrupled (Frenk et al., 2015), as has the number of overdose deaths from prescription opioids (CDC, 2016). In 2015, 91 individuals a day died from an opioid overdose (including prescription opioids and heroin), totaling to more than 33,000 deaths (Rudd et al., 2016).
The increase in prescriptions for opioids has been attributed to a number of factors such as new standards for appropriate pain control management, liberalizing laws for opioid prescriptions to treat non-cancer chronic pain from state medical boards in the 1990’s (Kenan et al., 2012; Kuehn, 2007; Manchikanti et al., 2010) and, the marketing and promotion of opioids from pharmaceutical companies to doctors, minimizing the risk of addiction to opioids (Van Zee, 2009). In addition, pain management clinics are inappropriately prescribing/distributing drugs, labeled as, “pill mills”, may in part have contributed to the proliferation of overprescribed opioids (Rigg et al., 2010). Despite the minimization of the addictive properties of opioids, both research and clinical practice have shown that repeated use of opioids can affect brain connectivity and function that lead to severe consequences such as physical dependence and chronic addiction (Volkow and McLellan, 2016).
In spite of the prevalence of nonmedical opioid use, however, there remain barriers to receiving treatment (e.g., lack of health coverage, costs of treatment) after developing an opioid addiction. In 2016, more than 2 million Americans had an opioid use disorder, but a little more than 20% of individuals had received treatment for opioid addiction (SAMHSA, 2017b). The lack of individuals receiving treatment for opioid use points to the importance of understanding such barriers, one of which is the stigmatization of individuals with an opioid use disorder. Stigma is a multidimensional construct that can be in the form of an attitude, an attribute or characteristic, or a shared belief about a behavior (Crocker et al., 1998; Goffman, 1963; Stafford and Scott, 1986) and can manifest in different ways. Self-stigma is an internalized negative belief that individuals hold about themselves, while public stigma refers to the negative beliefs of the public toward a person or group (Corrigan and Watson, 2002). Perceived stigma is an internalized negative belief that others have a commonly held stereotype about a stigmatized group. Perceived stigma is associated with higher internalized shame and can be a barrier for individuals to enter treatment (Luoma et al., 2010). Stigma can lead to fear and social isolation and may deter individuals from seeking treatment and/or help and can impact the way treatment providers interact with someone with a substance use disorder (Botticelli and Koh, 2016). For example, it has been demonstrated that healthcare professionals commonly have negative attitudes towards individuals with a substance use disorder, which can contribute to lower quality of care that these individuals receive (Van Boekel et al., 2013). Furthermore, the effect of language on stigmatizing attitudes in two studies showed that when an individual is referred to as a “substance abuser” compared to having a “substance use disorder”, healthcare providers judged the substance abuser as less deserving of treatment (Kelly, 2004) and more culpable and deserving of punitive action (Kelly and Westerhoff, 2010).
Stigmatizing individuals with an opioid use disorder or other substance use disorders can lead to stereotyping, labeling, prejudice, and discrimination. For instance, previous research has shown that public attitudes towards drug addictions are more stigmatized than mental illnesses (Barry et al., 2014) and individuals with a substance use disorder may be perceived as having control over their illness and, therefore, being more responsible for their behaviors (Corrigan et al., 2009). Moreover, prescription opioids can be obtained legally from a medical doctor, and in some cases, addiction can develop from repeated opioid use (Kolodny et al., 2015). Individuals who obtain an opioid prescription from a doctor may have “less control” over the development of an addiction and may be held less responsible for their behaviors. Therefore, individuals who use opioids compared to other substances may be stigmatized differently, and improving public policies through the use of communication strategies (e.g., highlighting individual stories with contextual information) should be considered (McGinty et al., 2017). It has recently been shown that higher stigma towards individuals with an opioid use disorder was associated with greater public support for punitive policies and lower support for health-oriented policies such as increasing government spending (Kennedy-Hendricks et al., 2017). While their results provide evidence for policy implications, whether these results can be attributed to individual factors (e.g., taking opioids from someone) or system factors (e.g., prescribing practices) is unknown. Therefore, we aimed to understand public stigma towards an opioid addiction by comparing individual and system factors.
Although it has been previously reported that rates of nonmedical prescription opioid use are greater among men, there are no differences in the occurrences of opioid use disorder among men and women (Saha et al., 2016). In the past year, it has been estimated that 11% of men and 6% of women received treatment for illicit drug use (SAMHSA, 2017a). The role that gender plays in stigmatizing attitudes towards opioid use has not been thoroughly explored, and only a few studies have investigated gender and drug addiction in the context of stigma. Studies have shown that respondents rated a male with a drug addiction higher for variables such as blame, fear, and anger compared to a female (Sattler et al., 2017) and women were rated with higher negative attributions who used cannabis and methamphetamine compared to men (Sorsdahl et al., 2012). Another recent study investigating implicit and explicit beliefs about persons who inject drugs found that there were no differences between genders, but a higher implicit belief about warranting punishment was found for a person framed as a Latino(a) versus a person framed as White (Kulesza et al., 2016).
The stigmatization of individuals with an addiction can be influenced by many complex factors (Sattler et al., 2017); therefore, we aimed to encompass different characteristics and dimensions involved with stigma (i.e., responsibility, positive and negative effect and dangerousness). Previously, there has been a focus on stigma research investigating attitudes towards alcohol use (Keyes et al., 2010; Schomerus et al., 2010) and substance use (Corrigan et al., 2009; Luoma et al., 2007; Sattler et al., 2017). A recent study investigated social stigma and social distance (e.g., experience with prescription opioid use disorders) towards individuals with an opioid use disorder (Kennedy-Hendricks et al., 2017). They found that there were higher levels of stigma towards individuals framed as “having an addiction to prescription painkillers” and there was no difference in regards to social distance. These findings provide evidence that there is stigma towards individuals with an opioid use disorder, but how the information contributes to public stigma and opioid use needs further exploration. We, therefore, focused on the effect that language, target gender and precipitating events (i.e., how the drug was initially obtained) have on the stigmatization of opioid use. In light of previous research on the role of language in stigmatization, we first looked at stigmatizing attitudes when an individual is labeled as a “drug addict” versus an individual with an “opioid use disorder”. Given the role that gender may play in stigmatizing attitudes and the prevalence of opioid use disorder, we investigated how the gender of an individual with an opioid use disorder affects stigma. Lastly, we wanted to discern whether stigma is affected by information provided about the precipitating events that may contribute or lead to excessive opioid use. We examined an individual who was prescribed opioids from a doctor and an individual who took opioids from a friend. To our knowledge, the role of precipitance has never been studied in the context of opioid use, and in light of the role that overprescribing may have played in exacerbating the opioid epidemic, we sought to uncover the pertinence of precipitance. We used case vignettes to investigate the influence of language, precipitance of obtaining the opioids and gender on stigmatizing attitudes. We hypothesized that there would be greater stigmatizing attitudes (higher responsibility, dangerousness and negative affect and lower positive affect) towards 1) a male versus a female, 2) an individual labeled as a “drug addict” versus having an “opioid use disorder” and 3) an individual who took prescription opioids from a friend versus receiving a prescription from a doctor.
2. Methods
2.1. Participants
Participants were recruited and paid through Amazon’s Mechanical Turk (MTurk; http://www.mTurk.com), a crowdsourcing website. MTurk, which has become a popular tool to conduct survey-based research, connects suppliers of basic labor tasks (known as “requesters”) with people who are willing to complete them (known as “workers”) in an online labor market. MTurk workers provide samples that are more representative (Berinsky et al., 2012; Buhrmester et al., 2011; Mason and Suri, 2012) and more diverse geographically and demographically (Strickland and Stoops, 2015) than convenience samples used in traditional academic studies. Further, MTurk has become more prevalent among researchers as a means to investigate variables with clinical relevance (Chandler and Shapiro, 2016) and it has repeatedly been shown that research conducted on MTurk replicates published experimental findings (Berinsky et al., 2012).
To be eligible to participate, participants had to live in the United States and be at least eighteen years old. After accepting the assignment on MTurk, participants were taken to Qualtrics (https://www.qualtrics.com), a widely used online management software that is used for collection and analysis of data, where they provided informed consent and were notified that there would be questions mixed in to ensure that they were paying attention. All participants were then randomly assigned to one of eight possible scenarios. After being shown the vignette, they were asked two comprehension questions. All participants who missed either or both of these questions (228 out of 2,833) were eliminated from the analysis, leaving us with a sample of 2,605 participants (92% completed the survey). This study was approved by Connecticut College’s Institutional Review Board (IRB).
2.2. Case Vignettes
Each vignette described a hypothetical individual who became addicted to opioids. The vignettes varied based on three conditions: 1) Target Gender: male or female, 2) Language: “drug addict” or “opioid use disorder”, 3) Precipitance: doctor or individual. Table 1 shows an example of a vignette with target gender as female, language-using opioid use disorder and precipitance as a doctor. The descriptions in the vignettes were all the same, except the wording was changed based on the different conditions (see Table S1 for full descriptions)1. After reading the vignette, participants were asked to rate the individual on an interval scale (e.g., 1– 6, where 1 is low, and 6 is extremely) based on four variables: responsibility, dangerousness, positive affect (concern, sympathy) and negative affect (anger, disappointment). The variables were selected based on earlier work that showed that variables such as affect, responsibility (Skinner et al., 2007) and dangerousness (Sattler et al., 2017) might contribute to the stigmatization of others.
Table 1.
Example case vignette scenario with female, opioid use disorder and doctor
| Jane currently has an opioid use disorder. |
| Her situation started one year ago, when she twisted her ankle while jogging. To make her mild pain go away, she was given a prescription for a bottle of painkillers from a medical doctor. The bottle included a one-month supply of pills even though injuries like this typically take a couple of days to heal. |
| Although Jane’s pain went away in two days, she finished the entire bottle over the next month. After that, she was unable to resist her cravings for more painkillers. Excessive drug use caused her to lose her job and she now spends much of her time obtaining and using more painkillers. |
2.3. Measures
After responding to the vignette, participants completed demographic measures, substance use history and the Perceived Stigma of Addiction Scale (PSAS) (Luoma et al., 2010), a measure that assesses perceptions of public stigma towards substance users (see Table 2 for descriptive statistics). The PSAS was completed last so it would not influence participant perceptions during the experimental task. Lastly, participants were asked if they knew someone with opioid addiction (i.e., familiarity).
Table 2.
Descriptive Statistics on Demographic Measures.
| Measure | aM ± bSD & Frequencies |
|---|---|
| Age | 36.9 ± 12.32 |
| Gender | |
| Male | 1395 |
| Female | 1197 |
| Other | 13 |
| Race | |
| American Indian/Native American | 11 |
| Asian | 203 |
| Black/African American | 181 |
| Hispanic/Latino | 120 |
| White/Caucasian | 1948 |
| Pacific Islander | 5 |
| Other | 18 |
| Mixed race | 119 |
| Income ($) | |
| Less than 12,000 | 386 |
| 12,000–29,000 | 586 |
| 30,000–47,999 | 601 |
| 48,000–66,000 | 473 |
| More than 66,000 | 559 |
| Education | |
| Eighth grade or lower | 2 |
| Some high school | 12 |
| High school graduate | 223 |
| Some college | 725 |
| Professional training/license | 92 |
| College graduate | 1130 |
| Graduate degree | 421 |
| Familiarity | |
| Yes | 935 |
| No | 1670 |
| Current/past opioid use | |
| Yes | 235 |
| No | 2370 |
| Total cPSAS Score | 28.4 ± 5.243 |
M = mean
SD = standard deviation
PSAS = Perceived Stigma of Addiction Scale
2.4. Statistical Analysis
Data analysis was conducted with the Statistical Package for Social Sciences 24.0 (SPSS 24.0, IBM Corp.) with alpha set to p < .05. A one-way analysis of variance (ANOVA) for the PSAS scores and chi-square (χ2) analyses were conducted for all other measures to assess any differences across scenarios (Table 3). A 2 (Target Gender: male versus. female) × 2 (Language: addict versus. disorder) × 2 (Precipitance: doctor versus. individual) multivariate analysis of covariance (MANCOVA) was implemented to investigate stigma attitudes based on positive and negative affect, responsibility and dangerousness. A principal component factor analysis with varimax rotation for the four affect scales (concern, sympathy, anger, and disappointment) was conducted similarly to previous work on stigma (Skinner et al., 2007). Participant’s past and current nonmedical prescription opioid use (yes, no) were included as a covariate based on previous findings that showed one’s use could influence stigma towards individuals with drug addiction (Sattler et al., 2017). Participants significantly differed on the PSAS score and familiarity (yes, no), and therefore, these measures were entered as additional covariates. Previous studies have demonstrated that normalization procedures are not necessary for large sample sizes (Ghasemi and Zahediasl, 2012; Lumley et al., 2002). Nevertheless, Mann-Whitney U tests were conducted for each factor to reinforce the robustness of our results.
Table 3.
Inferential statistics for measures based on scenario.
| Measure | Statistic | p-value |
|---|---|---|
| Age | F(7, 2597) = 0.632 | 0.730 |
| Gender | χ2 (14) = 12.73 | 0.548 |
| Race | χ2 (49) = 58.33 | 0.170 |
| Income | χ2 (28) = 23.92 | 0.686 |
| Education | χ2 (42) = 41.46 | 0.494 |
| Familiarity | χ2 (7) = 15.06 | 0.035 |
| Current/past opioid use | χ2 (7) = 2.35 | 0.938 |
| Total aPSAS score | F(7, 2597) = 2.312 | 0.024 |
PSAS = Perceived Stigma of Addiction Scale
3. Results
3.1. Stigma Attitudes
3.1.1. Responsibility.
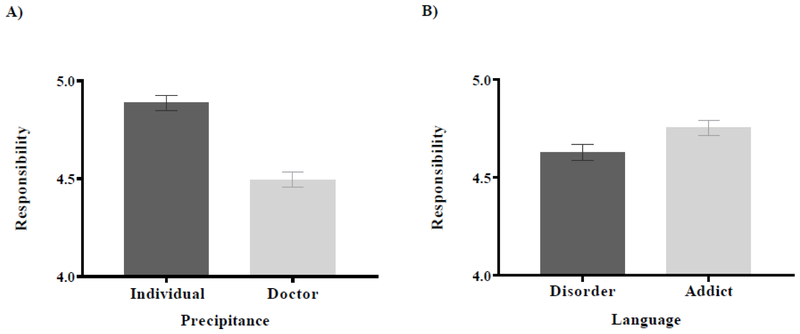
There were significant main effects of Language (F (1, 2594) = 5.11, p = .024) and Precipitance (F (1, 2594) = 49.59, p < .0001), but no significant main effect of Target Gender (F (1, 2594) = 0.31, p = .577). For Language, the addict was rated with higher responsibility compared to disorder (Figure 1A), and for precipitance, the individual was rated with higher responsibility than the doctor (Figure 1B). No interaction or covariate effects were found for responsibility (all p’s > .05).
Figure 1. Responsibility.
A) For the main effect of Language, addict was rated with higher responsibility compared to disorder (p < .0001). B) For the main effect Precipitance, individual was rated with higher responsibility compared to doctor (p = .024).
Planned follow-up Mann-Whitney U tests showed a significant difference for Language between addict and disorder (U = 808762.50, p = .036) and Precipitance between individual and doctor (U = 679590.50, p < .0001), but not for Target Gender (U = 840816.00, p = .687), which are consistent with the MANOVA results.
3.1.2. Dangerousness.
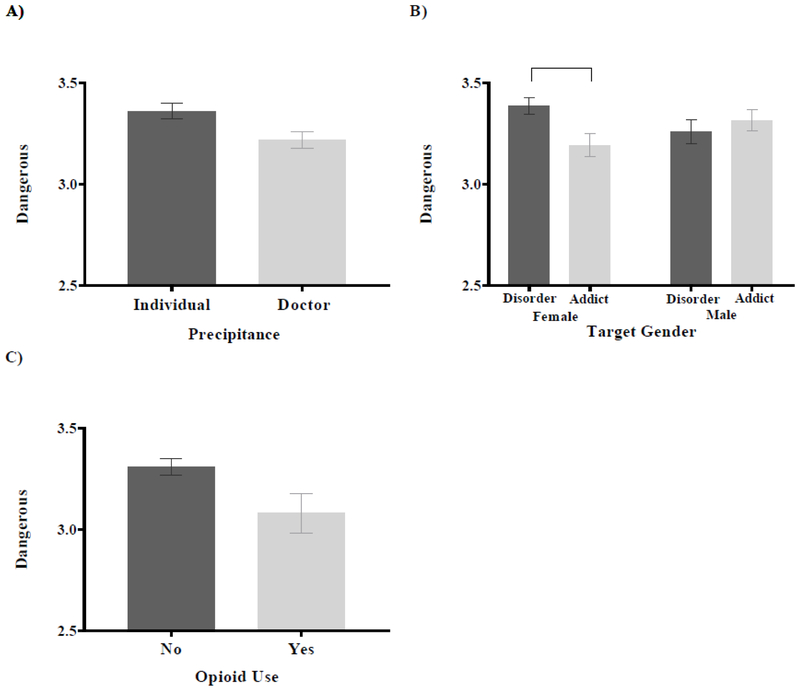
There was significant main effect of Precipitance (F (1, 2594) = 6.41, p = .011) and no main effects of Language (F (1, 2594) = 1.46, p = .227) or Target Gender (F (1, 2594) = 0.01, p = .942). For Precipitance, individual was rated as more dangerous than doctor (Figure 2A). An interaction effect of Target Gender x Language was found (F (1, 2594) = 4.96, p = .026). Post hoc analysis showed that disorder was rated as more dangerous than addict within the female condition (t (1304) = −2.43, p = .015) (Figure 2B). Lastly, there was a significant covariate effect of opioid use (F (1, 2594) = 4.97, p = .026), indicating that individuals with past/current use of opioids had lower dangerous ratings (Figure 2C). No other interaction or covariate effects were found (all p’s > .05).
Figure 2. Dangerousness.
A) For the main effect of Precipitance, individual was rated with higher dangerousness than doctor (p = .011). B) The Target Gender x Language interaction effect showed that within the female condition, disorder was rated with higher dangerousness than addict (p = .015). C) Participants who had used nonmedical prescription opioids had overall lower dangerous ratings compared to participants who had not used nonmedical prescription opioids (p = .026).
Planned follow-up Mann-Whitney U tests showed a significant difference for Precipitance between individual and doctor (U = 801962.00, p = .015), which is consistent with the MANCOVA findings. Target Gender (U = 845215.50, p = .872) and Language (U = 824666.50, p = .230) were not significant.
3.1.3. Positive Affect.
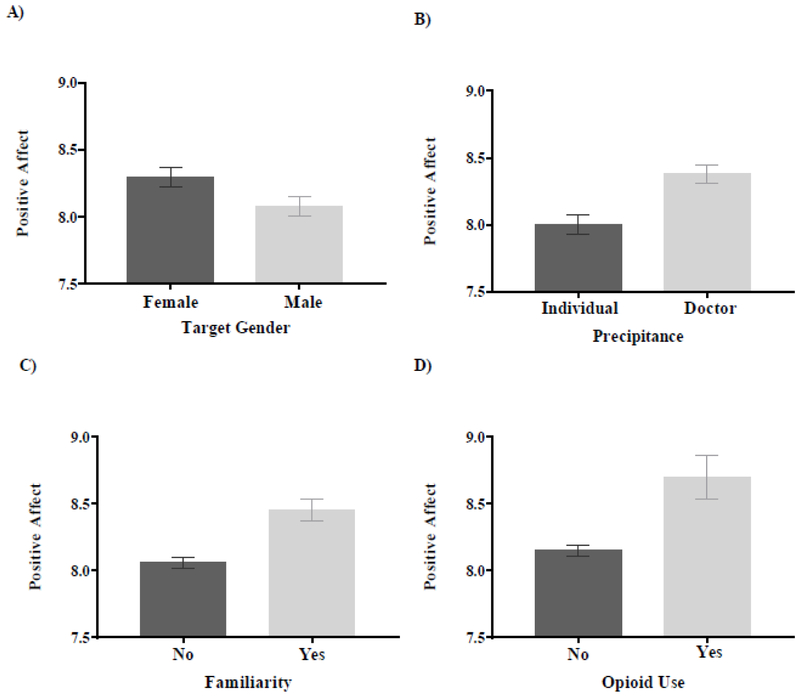
There were significant main effects of Target Gender (F (1, 2594) = 4.85, p = .028) and Precipitance (F (1, 2594) = 14.71, p < .0001) and no significant main effect of Language (F (1, 2594) = 0.90, p = .764). For Target Gender, female was rated with higher positive affect compared to male (Figure 3A) and for Precipitance, doctor was rated with higher positive affect compared to individual (Figure 3B). There were significant covariate effects for familiarity (F (1, 2594) = 15.36, p < .0001), opioid use (F (1, 2594) = 7.17, p = .007) and total PSAS score (F (1, 2594) = 22.70, p < .0001). Familiarity and past/current opioid use were associated with higher positive affect ratings (Figure 3C and3D). A bivariate Spearman’s rho correlation was conducted for the PSAS score and positive affect and the results showed that individuals with a higher PSAS score (higher perceptions of public stigma) had lower positive affect ratings r(2603) = −.06, p = .001). No interaction effects were found for positive affect (all p’s > .05).
Figure 3. Positive Affect.
A) For the main effect of Target Gender, female was rated with higher positive affect than male (p = .028). B) For the main effect of Precipitance, doctor was rated with higher positive affect compared to individual (p < .0001). C) Participants who knew someone with an opioid addiction had higher overall positive affect ratings compared to participants who did not know someone with an opioid addiction (p < .0001). D) Participants who had used nonmedical prescription opioids had higher overall positive affect ratings compared to participants who had not used nonmedical prescription opioids (p = .007).
Planned follow-up Mann-Whitney U tests showed a significant difference for Target Gender between male and female (U = 808531.50, p = .037) and Precipitance between individual and doctor (U = 775245.50, p < .0001), but not for Language (U = 832203.00, p = .429), which is consistent with the MANCOVA results.
3.1.4. Negative Affect.
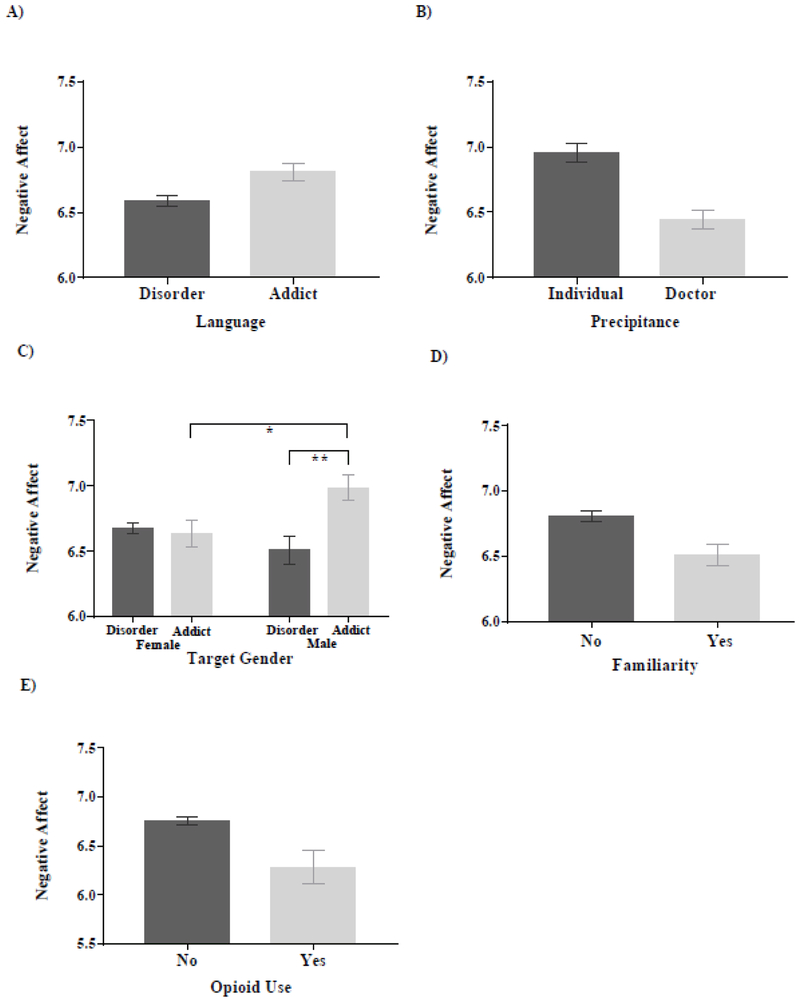
There were significant main effects of Language (F (1, 2594) = 4.63, p = .031) and Precipitance (F (1, 2594) = 25.68, p < .0001), but no main effect of Target Gender (F (1, 2594) = 0.84, p = .359). For Language, addict was rated with higher negative affect compared to disorder (Figure 4A) and for Precipitance, individual was rated with higher negative affect compared to doctor (Figure 4B). An interaction effect of Target Gender x Language was revealed (F (1, 2594) = 6.68, p = .010). Post hoc analyses showed that addict was rated with higher negative affect compared to disorder within the male condition (t (1297) = −3.34, p = .001) and male was rated with higher negative affect than female in the addict condition (t (1345) = −2.52, p = .012) (Figure 4C). There were significant covariate effects for familiarity (F (1, 2594) = 6.87, p = .009) and opioid use (F (1, 2594) = 5.81, p = .016). Familiarity and past/current opioid use were associated with higher positive affect ratings (Figure 4D and4E). No other covariate or interaction effects were found (all p’s > .05).
Figure 4. Negative Affect.
A) For the main effect of Language, addict was rated with higher negative affect compared to disorder (p = .031). B) For the main effect of Precipitance, individual was rated with higher negative affect compared to doctor (p < .0001). C) For the interaction effect of Target Gender by Language, male was rated with higher negative affect compared to female in the addict condition (*p = .031) and in the male condition, addict was rated with higher negative affect compared to disorder (**p = .001). D) Participants who knew someone with an opioid addiction had lower overall negative affect ratings compared to participants who did not know someone with an opioid addiction (p = .009). E) Participants who had used nonmedical prescription opioids had lower negative affect compared to participants who had not used nonmedical prescription opioids (p = .016).
Planned follow-up Mann-Whitney U tests showed a significant difference for Language between male and female (U = 806502.50, p = .033) and for Precipitance between individual and doctor (U = 754958.50, p < .0001), but not for Target Gender (U = 830725.00, p = .358), which is consistent with the MANCOVA results.
3.2. Principal Component Factor Analysis
The four affect scales (concern, sympathy, disappointment, and anger) were analyzed with a principal component factor analysis with varimax rotation. Similar to the findings of Skinner et al. (2007), two components with an eigenvalue greater than 1 were found. Anger and disappointment had factors loadings of .85 and .87 and these items were loaded on the first component. Concern and sympathy had factor loadings of .82 and .91 and these items were loaded on the second component. Scores for anger and disappointment were combined for a measure of negative affect and concern and sympathy were combined for a measure of positive effect.
4. Discussion
In this study, we aimed to discern the variables involved with stigmatization of an individual with the opioid addiction. When assessing the role of precipitance, our results illustrate that there were higher stigmatizing attitudes (i.e., responsibility, dangerousness, positive affect and negative affect) towards an individual who took opioids from a friend (individual factor), compared to an individual who received an opioid prescription from a doctor (system factor), despite the fact that each scenario ended identically. Our findings on precipitance can be explained in terms of the attributional theory of stigma, where the cause of an event or behavior can be inferred as external (situational factors), internal (dispositional or personal characteristics), controllable (e.g., onset of an addiction) and stable (e.g., reversibility of the addiction) (Corrigan, 2000; Sattler et al., 2017; Weiner et al., 1988). When applied to drug addictions, the attributional framework is of particular relevance because the degree of controllability that someone has over their addiction may affect a stigmatizing response to that person (Hegarty and Golden, 2008). A chasm between academics exists on how to define addiction. There are strong proponents of the belief that addiction is a “choice” or a “voluntary behavior” (Levy, 2013), while others argue that addiction is a “brain disease” characterized by a loss of control and compulsive behaviors (Henden et al., 2013; Volkow et al., 2016). In our study, we theorize that participants may have assigned more “controllability” to the individual who took the opioids from a friend compared to the individual who received a prescription from a doctor and therefore, was rated with higher stigma. With the role that overprescribing may have played in the opioid epidemic, this finding provides a better understanding of how information about precipitating events can contribute to stigmatization.
In addition to precipitance, our results indicated that language and gender also play a part in stigmatizing attitudes. We found that an individual labeled as a drug addict had a higher responsibility and negative affect ratings compared to someone with an opioid use disorder, while a male had lower positive affect ratings compared to a female. Our findings are in line with previous studies on substance use that show that males (Sattler et al., 2017) and being labeled as a “substance abuser” (Kelly and Westerhoff, 2010) have higher stigma ratings compared to females and “substance disorder”. We also found an interaction effect that showed that opioid use disorder was rated with higher dangerousness than drug addict within the female condition. In 2013, the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) was released with the goal of newer scientific findings on psychiatric disorders becoming more compatible with the newest version of the International Classification of Diseases (ICD-11) (Regier et al., 2013). Hundreds of experts from different disciplines contributed to the DSM-5 and newer classifications such as “opioid use disorder” and “substance use disorder” were added into the manual. However, with the changes in clinical nomenclature, the effect on public perceptions about psychiatric disorders may not have been fully understood. In light of our findings, clinical terminology such as “disorder” needs to be taken into consideration when assessing women with opioid addictions. This interaction result can be looked at in terms of the attribution theory of stigma relating to stability (e.g., reversibility of the addiction). An individual labeled with a disorder potentially could be seen as having a “condition” that may be less reversible than someone labeled as an addict. Furthermore, research has shown that women tend to abuse substances less than men and women may be stigmatized more when using substances because of a violation of gender norms (Hecksher and Hesse, 2009). A woman’s suitability as a “mother or carer” may be in question if she has a drug problem (Toner et al., 2008), which may explain the differences in the dangerousness ratings. In addition, we showed that there were interaction effects of language and gender on negative affect ratings. When comparing male to female in the drug addict condition, the male was rated with higher negative affect ratings. Within the male condition, drug addict was rated higher with higher negative affect ratings than disorder. A male labeled as a “drug addict” might align with gender expectations of what may be common perceptions of male behavior. Overall, our interaction effects suggest that language matters for both males and females and labeling criteria needs to be further scrutinized.
Lastly, our results indicated that familiarity, participants’ past/current opioid use and PSAS scores might be involved with stigmatization of an individual who uses opioids. Previous research suggests that familiarity of drug addictions (e.g., contact/knowing someone with an addiction or personal experience with drug) can influence stigmatizing attitudes towards someone with a drug addiction (Addison and Thorpe, 2004; Corrigan et al., 2009; Sattler et al., 2017) and our study showed similar results. In addition, we found a negative correlation between the PSAS score and positive affect ratings. Participants with a higher PSAS score (higher perceived perceptions of public stigma) had lower positive affect ratings. Higher perceptions of public stigma may reflect higher internalized stigma or shame (Luoma et al., 2010), which could explain the lower positive affect ratings. However, our PSAS result should be taken speculatively because the phrases in the measure pertain to “substance use” and may reflect general beliefs, rather than specificity towards opioids. Lastly, while our study was open to the public, it was conducted with MTurk and, therefore, our findings may reflect the viewpoints representative of individuals who use MTurk. Our sample was predominantly White, and since opioid use disorder has historically affected White individuals, our results may have been influenced by racial aspects. Nonetheless, our inferential statistics showed that race was not different across each scenario. Future studies should address the role that race has on public attitudes towards individuals who use opioids.
Our study strengths include a nation-wide survey that allowed us to gather information from a large sample size. Also, the survey allowed responders to maintain their anonymity, which ensured private communication, lack of judgment from an interviewer and, therefore, maximized truthful responses. Our study also has a few limitations. First, the PSAS and other measures were given at the end of the study to avoid influencing participants’ perceptions about the experimental task. Second, our addict condition chosen for the task was based on a commonly used lay term to create high external validity. Future studies could vary the language and investigate other commonly used lay terms. Lastly, we aimed to understand the multidimensionality of stigma; however, our factors may not have entirely encompassed this complex construct. Other studies could include more factors to assess any differences in attitudes towards opioid use.
The goal of this study was to have a greater understanding of the stigmatizing attitudes towards opioid use. Our findings add to the existing literature on stigma and drug addiction, while also providing a better foundation for comprehending the influence of factors such as precipitance, gender, and language on the stigmatization of opioid use. These findings are especially salient given the rise in opioid use and opioid overdose deaths. A better discernment of the factors involved with the inception of opioid use and how stigma can negatively impact individuals can potentially shift perspectives on multiple levels (e.g., healthcare level and community level) to facilitate policy changes. How healthcare providers and scientists label individuals addicted to opioids create an arena that translates to the community and the media. Therefore, implementing changes on the healthcare and research level can be the first step to changing public attitudes. For instance, knowledge and competency about opioid use disorder, as well as familiarity with addictions, can be increased by providing educational platforms and training to healthcare professionals and researchers. Further, the use of pejorative language should be eliminated (e.g., “addict”), and the recovery process should be promoted (Broyles et al., 2014). In turn, the community and the media can be informed through communication strategies, which could include sympathetic narratives (e.g. humanizing individual experiences and struggles), messages without blame (e.g. emphasizing the role of factors outside of an individual’s control) and messages highlighting structural barriers (e.g. pointing to a lack of insurance coverage for treatment) (McGinty et al., 2017). Increasing public support for policies and raising awareness by providing information to promote change can help to facilitate legislative policy advocacy. While the current study did not directly measure policy implementation, it would be beneficial for future studies to investigate the intersection of policy and stigma.
Supplementary Material
Highlights.
Gender, language and precipitation matter for stigma and opioid use
Greater scrutiny is needed for addiction labeling criteria for both genders
Familiarity with opioid use lowers stigmatizing attitudes
Acknowledgements
This study was funded by Connecticut College, faculty support account 152–10000–202380 (PI: Dr. Chavanne). Dr. Goodyear is supported by the 5T32AA007459 training grant. Dr. Haass-Koffler’s work is currently supported by the NIAAA K01AA023867 and previously by the 5T32AA007459 training grant.
Role of Funding Source
Nothing Declared
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Authors Disclosures
Conflict of Interest
No conflict declared
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi: ...
References
- Addison SJ, Thorpe SJ, 2004. Factors involved in the formation of attitudes towards those who are mentally ill. Soc. Psychiatry Psychiatric Epidemiol. 39, 228–234. [DOI] [PubMed] [Google Scholar]
- Barry CL, McGinty EE, Pescosolido BA, Goldman HH, 2014. Stigma, discrimination, treatment effectiveness, and policy: Public views about drug addiction and mental illness. Psychiatr. Serv 65, 1269–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berinsky AJ, Huber GA, Lenz GS, 2012. Evaluating online labor markets for experimental research: Amazon. com’s Mechanical Turk. Polit. Anal. 20, 351–368. [Google Scholar]
- Botticelli MP, Koh HK, 2016. Changing the language of addiction. Jama, 316, 1361–1362. [DOI] [PubMed] [Google Scholar]
- Broyles LM, Binswanger IA, Jenkins JA, Finnell DS, Faseru B, Cavaiola A, Pugatch M, Gordon AJ, 2014. Confronting inadvertent stigma and pejorative language in addiction scholarship: A recognition and response. Subst. Abuse, 35, 217–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, Gosling SD, 2011. Amazon’s Mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspect. Psychol. Sci. 6, 3–5. [DOI] [PubMed] [Google Scholar]
- CDC, 2016. Wide-ranging online data for epidemiologic research (WONDER). http://wonder.cdc.gov.
- Chandler J, Shapiro D, 2016. Conducting clinical research using crowdsourced convenience samples. An. Rev. Clin. Psychol. 12, 53–81. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, 2000. Mental health stigma as social attribution: Implications for research methods and attitude change. Clin. Psychol. 7, 48–67. [Google Scholar]
- Corrigan PW, Kuwabara SA, O’Shaughnessy J, 2009. The public stigma of mental illness and drug addiction. J. Soc. Work, 9, 139–147. [Google Scholar]
- Corrigan PW, Watson AC, 2002. Understanding the impact of stigma on people with mental illness. World Psychiatry, 1, 16–20. [PMC free article] [PubMed] [Google Scholar]
- Crocker J, Major B, Steele C, 1998. Social stigma, in: Gilbert D, Fiske ST, Lindzey G (Eds.), The handbook of social psychology. McGraw-Hill, Boston, MA., pp. 504–553. [Google Scholar]
- Frenk SM, Porter KS, Paulozzi LJ, 2015. Prescription opioid analgesic use among adults: United States, 1999–2012. NCHS Data Brief, 1–8. [PubMed] [Google Scholar]
- Ghasemi A, Zahediasl S, 2012. Normality tests for statistical analysis: a guide for non-statisticians. Int. J. Endocrinol. Metab. 10, 486–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman E, 1963. Stigma: Notes on the management of spoiled identity. Englewood Cliffs.
- Hecksher D, Hesse M, 2009. Women and substance use disorders. Mens Sana Monogr. 7, 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hegarty P, Golden AM, 2008. Attributional beliefs about the controllability of stigmatized traits: Antecedents or justifications of prejudice? J. Appl. Soc. Psychol. 38, 1023–1044. [Google Scholar]
- Henden E, Melberg HO, Røgeberg OJ, 2013. Addiction: choice or compulsion? Front. Psychiatry, 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, 2004. Toward an addictionary: A proposal for more precise terminology. Alcohol. Treat. Q. 22, 79–87. [Google Scholar]
- Kelly JF, Westerhoff CM, 2010. Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. Int. J. Drug Policy, 21, 202–207. [DOI] [PubMed] [Google Scholar]
- Kenan K, Mack K, Paulozzi L, 2012. Trends in prescriptions for oxycodone and other commonly used opioids in the United States, 2000–2010. Open Med. 6, e41–e47. [PMC free article] [PubMed] [Google Scholar]
- Kennedy-Hendricks A, Barry CL, Gollust SE, Ensminger ME, Chisolm MS, McGinty EE, 2017. Social stigma toward persons with prescription opioid use disorder: Associations with public support for punitive and public health-oriented policies. Psychiatr. Serv (Washington, D.C.) 68, 462–469. [DOI] [PubMed] [Google Scholar]
- Keyes K, Hatzenbuehler M, McLaughlin K, Link B, Olfson M, Grant B, Hasin D, 2010. Stigma and treatment for alcohol disorders in the United States. Am. J. Epidemiol. 172, 1364–1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolodny A, Courtwright DT, Hwang CS, Kreiner P, Eadie JL, Clark TW, Alexander GC, 2015. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Ann. Rev. Public Health 36, 559–574. [DOI] [PubMed] [Google Scholar]
- Kuehn BM, 2007. Opioid prescriptions soar: Increase in legitimate use as well as abuse. Jama, 297, 249–251. [DOI] [PubMed] [Google Scholar]
- Kulesza M, Matsuda M, Ramirez JJ, Werntz AJ, Teachman BA, Lindgren KP, 2016. Towards greater understanding of addiction stigma: Intersectionality with race/ethnicity and gender. Drug Alcohol Depend. 169, 85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy N, 2013. Addiction is not a brain disease (and it matters). Front. Psychiatry, 4, 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley T, Diehr P, Emerson S, Chen L, 2002. The importance of the normality assumption in large public health data sets. Ann. Rev. Public Health, 23, 151–169. [DOI] [PubMed] [Google Scholar]
- Luoma JB, O’Hair AK, Kohlenberg BS, Hayes SC, Fletcher L, 2010. The development and psychometric properties of a new measure of perceived stigma toward substance users. Subst. Use Misuse, 45, 47–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luoma JB, Twohig MP, Waltz T, Hayes SC, Roget N, Padilla M, Fisher G, 2007. An investigation of stigma in individuals receiving treatment for substance abuse. Addict Behav. 32, 1331–1346. [DOI] [PubMed] [Google Scholar]
- Manchikanti L, Fellows B, Ailinani H, Pampati V, 2010. Therapeutic use, abuse, and nonmedical use of opioids: a ten-year perspective. Pain Physician, 13, 401–435. [PubMed] [Google Scholar]
- Mason W, Suri S, 2012. Conducting behavioral research on Amazon’s Mechanical Turk. Behav. Res. Methods, 44, 1–23. [DOI] [PubMed] [Google Scholar]
- McGinty E, Pescosolido B, Kennedy-Hendricks A, Barry CL, 2017. Communication strategies to counter stigma and improve mental illness and substance use disorder policy. Psychiatr. Serv., appi. ps. 201700076. [DOI] [PMC free article] [PubMed]
- Regier DA, Kuhl EA, Kupfer DJ, 2013. The DSM‐5: Classification and criteria changes. World Psychiatry, 12, 92–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigg KK, March SJ, Inciardi JA, 2010. Prescription drug abuse & diversion: Role of the pain clinic. J. Drug Issues, 40, 681–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA, Seth P, David F, Scholl L, 2016. Increases in drug and opioid-involved overdose deaths - United States, 2010–2015. MMWR. 65, 1445–1452. [DOI] [PubMed] [Google Scholar]
- Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, Jung J, Pickering RP, Ruan WJ, Smith SM, Huang B, Hasin DS, Grant BF, 2016. Nonmedical prescription opioid use and DSM-5 nonmedical prescription opioid use disorder in the United States. J. Clin. Psychiatry, 77, 772–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA S.A.a.M.H.S.A., 2017a. https://www.samhsa.gov/data/sites/default/files/NSDUHDetTabs-2016/NSDUH-DetTabs-2016.htm.
- SAMHSA S.A.a.M.H.S.A., 2017b. https://www.samhsa.gov/data/sites/default/files/NSDUHDetTabs-2016/NSDUH-DetTabs-2016.htm.
- Sattler S, Escande A, Racine E, Göritz AS, 2017. Public stigma toward people with drug addiction: A factorial survey. J. Stud. Alcohol Drugs, 78, 415–425. [DOI] [PubMed] [Google Scholar]
- Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC, 2010. The stigma of alcohol dependence compared with other mental disorders: A review of population studies. Alcohol Alcohol, 46, 105–112. [DOI] [PubMed] [Google Scholar]
- Skinner N, Feather NT, Freeman T, Roche A, 2007. Stigma and discrimination in health‐care provision to drug users: The role of values, affect, and deservingness judgments. J. Appl. Soc. Psychol. 37, 163–186. [Google Scholar]
- Sorsdahl K, Stein DJ, Myers B, 2012. Negative attributions towards people with substance use disorders in South Africa: Variation across substances and by gender. BMC Psychiatry, 12, 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafford MC, Scott RR, 1986. Stigma, deviance, and social control, in: Ainlay SC, Becker G, Coleman LM (eds.) The dilemma of difference. Perspectives in social psychology (A series of texts and monographs). Springer, Boston, MA, pp. 77–91. [Google Scholar]
- Strickland JC, Stoops WW, 2015. Perceptions of research risk and undue influence: Implications for ethics of research conducted with cocaine users. Drug Alcohol Depend. 156, 304–310. [DOI] [PubMed] [Google Scholar]
- Toner P, Hardy E, Mistral W, 2008. A specialized maternity drug service: Examples of good practice. Drugs: education, prevention and policy, 15, 93–105. [Google Scholar]
- Van Boekel LC, Brouwers EP, Van Weeghel J, Garretsen HF, 2013. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: A systematic review. Drug Alcohol Depend. 131, 23–35. [DOI] [PubMed] [Google Scholar]
- Van Zee A, 2009. The promotion and marketing of oxycontin: Commercial Triumph, public health tragedy. Am. J. Public Health, 99, 221–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Koob GF, McLellan AT, 2016. Neurobiologic advances from the brain disease model of addiction. N. Engl. J. Med. 374, 363–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, McLellan AT, 2016. Opioid abuse in chronic pain — Misconceptions and mitigation strategies. N. Engl. J. Med. 74, 1253–1263. [DOI] [PubMed] [Google Scholar]
- Weiner B, Perry RP, Magnusson J, 1988. An attributional analysis of reactions to stigmas. J. Pers. Soc. Psychol. 55, 738. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.