Abstract
Ménière’s disease (MD) represents a heterogeneous group of relatively rare disorders with three core symptoms: episodic vertigo, tinnitus, and sensorineural hearing loss involving 125 to 2,000 Hz frequencies. The majority of cases are considered sporadic, although familial aggregation has been recognized in European and Korean populations, and the search for familial MD genes has been elusive until the last few years. Detailed phenotyping and cluster analyses have found several clinical predictors for different subgroups of patients, which may indicate different mechanisms, including genetic and immune factors. The genes associated with familial MD are COCH, FAM136A, DTNA, PRKCB, SEMA3D, and DPT. At least two mechanisms have been involved in MD: (a) a pro-inflammatory immune response mediated by interleukin-1 beta (IL-1β), tumor necrosis factor alpha (TNFα), and IL-6, and (b) a nuclear factor-kappa B (NF-κB)-mediated inflammation in the carriers of the single-nucleotide variant rs4947296. It is conceivable that microbial antigens trigger inflammation with release of pro-inflammatory cytokines at different sites within the cochlea, such as the endolymphatic sac, the stria vascularis, or the spiral ligament, leading to fluid imbalance with an accumulation of endolymph. Computational integration of clinical and “omics” data eventually should transform the management of MD from “one pill fits all” to precise patient stratification and a personalized approach. This article lays out a proposal for an algorithm for the genetic diagnosis of MD. This approach will facilitate the identification of new molecular targets for individualized treatment, including immunosuppressant and gene therapy, in the near future.
Keywords: precision medicine, Meniere disease, vertigo, tinnitus, sensorineural hearing loss, molecular genetics, genomics
Introduction
Computational biomedicine integrating clinical and “omics” data is leading to molecular, individualized patient-oriented treatments, replacing the traditional approach based on clinical symptoms and few laboratory or imaging markers. Ménière’s disease (MD) is a set of rare inner ear disorders defined by a core phenotype: (a) episodes of vertigo associated with ipsilateral cochlear symptoms, such as tinnitus or aural fullness, and (b) sensorineural hearing loss (SNHL), which initially fluctuates and involves low and medium frequencies 1, 2. However, the condition exhibits a great clinical heterogeneity and large differences in response to therapy. The disorder is commonly explained by the accumulation of endolymph with increased pressure in the cochlear duct (endolymphatic hydrops [EH]), which damages the organ of Corti, the hearing organ; this overpressure leads to the rupture of the inner ear membranes, resulting in a loss of endocochlear potential in humans. The damage involves the scala media of the cochlea and the vestibular end organs (saccule and utricle) and eventually the semicircular canals 3. However, the clinical heterogeneity of MD is born in the pathophysiology itself and EH cannot explain the episodes of vertigo. Some patients with demonstrated EH do not develop all MD symptoms, whereas in some patients with definite MD an EH cannot be demonstrated 4. For this reason, EH is considered to be a marker of some underlying pathological process that is related to MD, such as a disorder of endolymphatic fluid homeostasis 5.
Repeated exposure of hair cells to toxic levels of a K +-enriched perilymph, the overpressure itself, and the sudden rupture of distended membranes explain the long-term vestibular and auditory damage in MD 6, 7.
The treatment of MD is based on empirical clinical practice. There is some evidence of therapies reducing the number of attacks, including trans-tympanic steroids 8, but so far none has been able to prevent progressive damage to the inner ear.
The prevalence of MD is variable, ranging from 3.5 per 100,000 inhabitants in Japan to 513 per 100,000 in Finland 9– 15. The condition shows differences in its prevalence according to ethnic background, it is more commonly observed in European than in Asian or American populations 16, 17, and it is rarely found in sub-Saharan populations, suggesting an ethnic-mediated genetic contribution. These differences in prevalence could also be explained by differences in availability of health care, but the finding of familial aggregation and multiple families in European and Korean populations supports the genetic background in MD 18, 19.
Furthermore, deep phenotyping and cluster analyses have found few clinical predictors for several subgroups of patients with MD, which may indicate different mechanisms of disease, including genetic and autoimmune factors 20, 21.
We describe the evidence supporting the possibility that MD is a heterogeneous disorder with several clinical variants, such as familial, autoimmune, and auto-inflammatory MD. We show the preliminary data that support the genetic contribution to MD and present a tentative algorithm for the genetic diagnosis of MD. This approach will facilitate the identification of new molecular targets for an individualized treatment.
Diagnosis of Ménière’s disease
The diagnostic criteria for MD were revised in 2015 by a Joint Consensus agreed on by five international scientific societies: the Barany Society, the Korean Balance Society, the Japan Society for Equilibrium Research, the European Academy of Otology and Neurotology, and the Equilibrium Committee of the American Academy of Otolaryngology-Head and Neck Surgery 1. Two diagnostic categories were accepted: definite MD and probable MD ( Table 1). These criteria are based on clinical symptoms and do not consider different subgroups of patients, laboratory markers (except pure tone audiograms), or imaging data. Although the aim of the revised diagnostic criteria is to gain precision in the diagnosis by improving the phenotyping, no “omics” data were available in 2015 and patient stratification was limited to bilateral involvement and familial MD.
Personalized medicine will combine hearing profile and high-resolution magnetic resonance imaging to improve the characterization of the MD phenotype and, together with genomic datasets, will open the door to targeted therapeutic strategies.
Table 1. Diagnostic criteria for definite and probable Ménière’s disease (MD) 1.
| Definite MD |
|---|
| A. Two or more spontaneous episodes of vertigo, each lasting 20 minutes to 12 hours |
| B. Audiometrically documented low- to medium-frequency sensorineural hearing loss
in one ear, defining the affected ear on at least one occasion before, during, or after one of the episodes of vertigo |
| C. Fluctuating aural symptoms (hearing, tinnitus, or fullness) in the affected ear |
| D. Not better accounted for by another vestibular diagnosis |
| Probable MD |
| A. Two or more episodes of vertigo or dizziness, each lasting 20 minutes to 24 hours |
| B. Fluctuating aural symptoms (hearing, tinnitus, or fullness) in the affected ear |
| C. Not better accounted for by another vestibular diagnosis |
Clinical research studies should include only patients with definite MD. Probable MD must be considered when no reliable hearing test has confirmed the temporal relationship between the episode of vertigo and the hearing loss.
From clinical variants toward personalized Ménière’s disease
Molecular and clinical heterogeneity among patients is very common in multifactorial inflammatory disorders. The immune response to the same antigenic exposure or to immune treatments commonly shows wide inter-individual variations. The transition from symptom-based to molecular-based personalized treatments first requires a deep knowledge of the genetic epidemiology of MD. Therefore, large-scale analyses of the genomic and molecular datasets of individuals experiencing defined disease conditions are required to identify reliable patient-specific biomarkers linking genotypes and single-cell gene expression profiles with endophenotypes. MD could involve one ear (unilateral) or both ears (bilateral MD). There is little clinical evidence supporting the possibility that they have different mechanisms 22. In patients with unilateral MD, hearing loss usually involves low and middle frequencies more than high frequencies, even in patients with a long follow-up (>20 years); on the other hand, patients with bilateral MD have an involvement of all frequencies in the audiogram 22. So the cochlear damage will be limited to the apical and middle turn in individuals with MD limited to a single ear, but it will affect the entire cochlea in patients with bilateral involvement. However, the major finding of clinical research in MD has been the identification of different clinical subgroups of patients with potentially different etiological factors.
The Ménière’s Disease Consortium (a European multicenter initiative to collect clinical and biological data) has identified five clinical variants among patients with MD ( Table 2). So hierarchical cluster analyses using few categorical variables as predictors can identify subgroups of patients in clinical practice 20, 21. Initially, 398 patients with bilateral MD were investigated since they showed a lower variation in the phenotype according to hearing profile. Group or MD type 1, which included 46% of patients, was defined by SNHL starting in one ear and involving the second ear in the following months or years but without migraine and autoimmune comorbidities. Group 2, 17% of patients, was characterized by simultaneous onset of hearing loss in both ears without migraine or autoimmunity. MD type 3 (13% of patients) clustered in families with MD, and group 4 (12% of patients) was associated with migraine in all cases. MD type 5 represented 11% of patients with MD and additionally autoimmune disease.
Table 2. Clinical subgroups of patients with unilateral and bilateral Ménière’s disease.
| Unilateral Ménière’s disease (MD) | |
|---|---|
| Type 1 | Sporadic MD (if concurrent migraine, autoimmune disease, or familial MD is observed, patients are out of this subgroup) |
| Type 2 | Delayed MD (hearing loss precedes vertigo attacks in months or years) |
| Type 3 | Familial MD (at least two patients in the first or second degree) |
| Type 4 | Sporadic MD with migraine (temporal relationship not required) |
| Type 5 | Sporadic MD plus an autoimmune disease |
| Bilateral MD | |
| Type 1 | Unilateral hearing loss becomes bilateral |
| Type 2 | Sporadic, simultaneous hearing loss (usually symmetric) |
| Type 3 | Familial MD (most families have bilateral hearing loss, but unilateral and bilateral cases may coexist in the same family) |
| Type 4 | Sporadic MD with migraine |
| Type 5 | Sporadic MD with an autoimmune disease |
In a subsequent study, Frejo et al. analyzed clinical data from 1,073 patients with unilateral MD with at least 5 years of follow-up since disease onset 21. Of note, some of the predictors described in patients with bilateral MD were also confirmed in patients with unilateral involvement. In unilateral MD, group 1 was the clinical variant most frequently observed (53%), and it included patients without a familial history of MD, migraine, or autoimmune comorbidity; MD type 2 was termed delayed MD and was a rare condition (8%) characterized by SNHL which antedated the vertigo episodes; familial MD or type 3 (13%) included all familial cases of MD, although some patients in these families may show unilateral SNHL; MD type 4 (15%) was associated with migraine with or without aura; and MD type 5 (11%) was defined by a concurrent autoimmune disorder.
However, the cluster analysis using the aggregated data of the unilateral and bilateral patients was not able to reproduce the same groups. This is probably due to an increase of heterogeneity pointing to unilateral and bilateral MD being different disorders.
Evidence for a genetic contribution to Ménière’s disease
Several lines of epidemiological evidence support a genetic contribution in MD, including (a) the higher prevalence observed in the European population over other ethnicities 16 and (b) a strong familial aggregation found in Europeans and South Koreans ranging from 6% to 10% of cases with a high sibling recurrence risk ratio (λs = 24–45) 18, 19, 23– 25.
The genes that have been related to the initiation and progression of MD can be classified into four main categories: (a) cell surface channels, (b) extracellular matrix proteins, (c) immune-associated, and (d) proliferation and cell survival genes.
Small case control studies suggested an association with HLA class II genes in different populations 26, 27, but these findings were not further replicated 28. However, two genes of the immune response have been associated with hearing loss progression in MD in larger cohorts: MICA and TLR10. So the carriers of the allelic variant MICA*A.4 showed a slower hearing loss progression, but the significance of this finding remains unknown 29. In a separate study, the common variant rs11096955 in the TLR10 gene also influenced the progression of SNHL in patients with bilateral MD 30. The MIF gene, encoding macrophage migration inhibitory factor, is a multifunctional cytokine which mediates the production of pro-inflammatory cytokines and enhances autoimmune-mediated neuroinflammation 31. Moreover, MIF seems to increase blood–brain barrier permeability 32 and may have a role in macrophage activation in MD 33, 34. Altogether, these findings support a role for the innate immune response in patients with MD.
More recently, Li et al. used a molecular network-based method using a random walk with restart algorithm to predict genes potentially involved in MD 35. A total of 43 genes were prioritized, and 11 of them were genes involved with immune-associated biological processes, such as CD4, IL6, IL-1R1, and TLR2 35. A genome association study using a high-density genotyping array containing 196,524 single-nucleotide variants identified two common allelic variants in the NFKB1 gene (rs3774937 and rs4648011) that seem to modify the hearing progression in patients with MD 36. Nuclear factor-kappa B (NF-κB) is a complex of transcription factors, which regulate the inflammatory response, and its activation by cytokine receptors in lymphoid cells seems to exacerbate the inflammatory response in MD 37.
Additional evidence for a genetic contribution is also supported by the exome sequencing studies conducted in four families with MD and an autoimmune background. These rare families showed an autosomal dominant pattern of inheritance and segregated rare variants with potential pathogenic effects in the FAM136A, DTNA, PRKCB, and DPT genes 38– 40. Although these genes for familial MD should be confirmed in sporadic cases and more families with MD are needed to accept them as causal genes in MD, these findings point to a genetic heterogeneity in familial cases.
Allelic heterogeneity has been found in Korean families with mutations in the COCH gene (DFNA9) as well. So, according to the location of the mutation on the gene, distinct vestibular phenotypes have been described; these range from progressive bilateral vestibular loss without episodic vertigo (p.G38D variant) to an MD-like phenotype with severe episodes of vertigo (p.C162Y variant) 41.
Evidence for an autoimmune variant of Ménière’s disease
Different studies have estimated that a third of patients with MD cases may have an immune dysfunction, but the mechanisms involved have not been established 42. Several hypotheses have been proposed to explain the development of autoimmune responses in the inner ear: (a) a cross-reaction due to shared epitopes between inner ear proteins and microbial proteins, such as cochlin; (b) collateral damage, as persistent levels of cytokines and chemokines may provoke delayed immune reactions, possibly explaining the relapsing/remitting course of MD; (c) self-intolerance to inner ear antigens; and (d) immunogenetic factors leading to a persistent inflammatory response 42.
Autoimmune EH has been induced experimentally by injection of antigens or monoclonal antibodies in murine models 43. Several inner ear proteins with molecular weights of 28, 42, 58, and 68 kDa could be the main components inducing autoimmune MD in the guinea pig model 44. Additionally, antibodies against type II collagen have been found in the serum of patients with MD 44.
Riente et al. observed the presence of autoantibodies to inner ear antigens in the serum of patients with MD, but the authors were not able to determine whether the presence of the antibodies occurs before the beginning of symptoms of MD or it is the result of the inner ear inflammation and tissue destruction 45.
The cytokine tumor necrosis factor (TNF)-like weak inducer of apoptosis (TWEAK), a member of the TNF superfamily, and the TWEAK/Fn14 pathway have been involved in several autoimmune diseases, including multiple sclerosis, systemic lupus erythematosus, rheumatoid arthritis, or ulcerative colitis 46. However, this pathway has only started to be investigated in MD. So the allelic variant rs4947296 is associated with bilateral MD in the Spanish population and has been found in 18% of patients with a comorbid autoimmune disorder 37. This region on chromosome 6 is a trans-expression quantitative trait locus and regulates the expression of multiple genes in the TWEAK/Fn14 pathway in peripheral mononuclear cells, leading to an NF-κB-mediated inflammatory response in MD 37.
Evidence for an auto-inflammatory variant of Ménière’s disease
Auto-inflammatory disorders include a spectrum of rare genetic disorders with an innate immune-mediated inflammatory background 47. This condition is usually characterized by high levels of the pro-inflammatory cytokine interleukin-1 beta (IL-1β) and the absence of autoantibodies in the sera of patients. This spectrum ranges from familial Mediterranean fever, the first monogenic auto-inflammatory disease described, associated with mutations in the MEFV gene 48, 49, or cryopyrin-associated periodic fever syndromes, caused by mutations in the NLRP3 gene 50, to complex polygenic auto-inflammatory diseases such as adult-onset Still’s disease, Crohn’s disease, ulcerative colitis, or sarcoidosis 47. Several mechanisms have been demonstrated in auto-inflammatory diseases, including (a) IL-1β-mediated auto-inflammation which may involve the NLRP3 inflammasome and its responses to IL-1β blockade 51, (b) IL-18-mediated auto-inflammation with mutations in the NLRC4 gene and macrophage activation syndrome 52, and (c) A20 haploinsufficiency with mutations in the TNFAIP3 gene associated with an increase of pro-inflammatory cytokines such as IL-1β, TNFα, IL-6, IL-18, and IL-17 and NF-κB-mediated inflammation 53. Although the evidence to support an auto-inflammatory process is still limited in MD, a case control study has shown that pro-inflammatory cytokines such as IL-1β, IL-1RA, TNFα, and IL-6 were elevated in 21% of MD patients in the supernatant from patient-derived peripheral blood mononuclear cells 54. Since these patients did not show any comorbid autoimmune condition, they could be considered within the spectrum of auto-inflammatory disorders. Moreover, extracts from Aspergillus and Penicillium molds triggered a release of TNFα in these patients with high basal levels, which was not observed in the control experiments, suggesting that these molds may contribute to the exacerbation of innate-mediated inflammation in MD 54.
Genetic diagnosis of Ménière’s disease
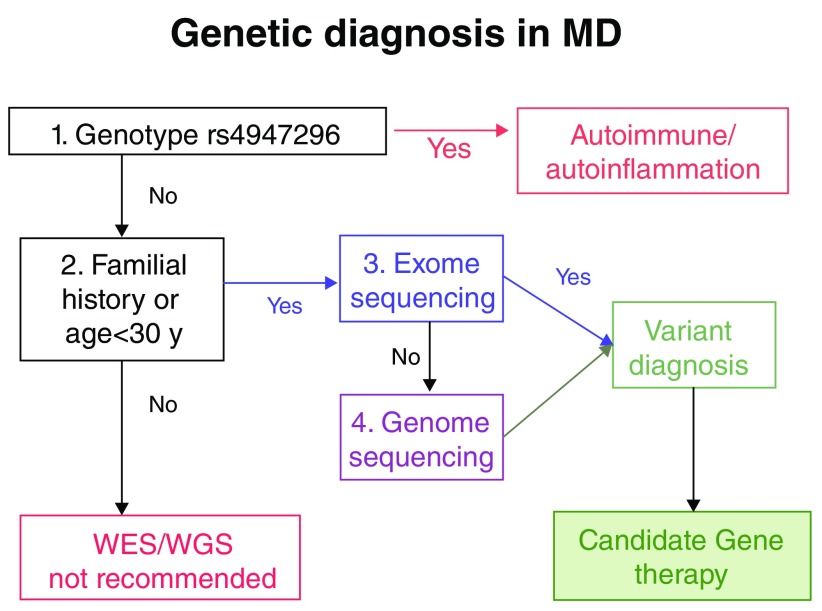
Figure 1 lays out a proposal for an algorithm for the genetic diagnosis of MD. Initially, all individuals with a MD phenotype should be tested for rs4947296 to assess whether they have an NF-κB-mediated inflammatory response that is potentially treatable. If a given patient does not carry the risk genotype but presents a familial history of MD or the onset of the disease occurred before the age of 30 years, we recommend performing exome sequencing. Although there are few exome datasets of patients with MD, initially the genetic diagnosis is expected to be possible in 20% to 30% of cases. This diagnosis rate will probably improve with whole genome sequencing, as has occurred with SNHL.
Figure 1. Potential algorithm for the genetic diagnosis of Ménière’s disease (MD).
WES, whole exome sequencing; WGS, whole genome sequencing.
However, if there is no familial history or the onset of the condition occurs over the age of 30 years, we consider the yield of exome or genome sequencing to be very low. Several initiatives such as Genome England ( www.genomicsengland.co.uk) or the Ménière’s Disease Consortium have designed and tested different gene panels for familial and sporadic MD, and the algorithm for the genetic diagnosis of MD will include some of these genes in the near future.
Conclusions
-
1.
MD should be considered a set of different rare disorders with a core phenotype: episodic vertigo, SNHL, and tinnitus
-
2.
Familial clustering and autosomal dominant MD show a genetic heterogeneity involving several genes such as COCH, DTNA, FAM136A, PRKCB, SEMA3D, and DPT, but the diagnostic value of genetic testing in patients with sporadic MD remains to be established
-
3.
A personalized treatment should consider the investigation of pro-inflammatory cytokines and rs4947296 as markers of NF-κB-mediated inflammation
-
4.
Genetic diagnosis of MD will pave the way for personalized medicine in vestibular disorders
Editorial Note on the Review Process
F1000 Faculty Reviews are commissioned from members of the prestigious F1000 Faculty and are edited as a service to readers. In order to make these reviews as comprehensive and accessible as possible, the referees provide input before publication and only the final, revised version is published. The referees who approved the final version are listed with their names and affiliations but without their reports on earlier versions (any comments will already have been addressed in the published version).
The referees who approved this article are:
Sung Huhn Kim, Department of Otorhinolaryngology, Yonsei University College of Medicine, Seoul, South Korea
Peter Paul van Benthem, Department of Otorhinolaryngology and Head and Neck Surgery, Leiden University Medical Center, Leiden, Netherlands
Issam Saliba, Division of Otolaryngology-Head and Neck Surgery, Montreal University Hospital Center (CHUM), University of Montreal, Montreal, Quebec, Canada
Funding Statement
Jose A. Lopez-Escamez is supported by the Luxembourg National Research Fund (grant INTER/Mobility/17/11772209), Ménière’s Society (UK), Instituto de Salud Carlos III (grant PI17/01644), and FEDER Funds and H2020 Marie Skłodowska-Curie Actions (ITN-2016–722046) from the EU.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 1; referees: 3 approved]
References
- 1. Lopez-Escamez JA, Carey J, Chung WH, et al. : Diagnostic criteria for Menière’s disease. J Vestib Res. 2015;25(1):1–7. 10.3233/VES-150549 [DOI] [PubMed] [Google Scholar]
- 2. Espinosa-Sanchez JM, Lopez-Escamez JA: Menière’s disease. Handb Clin Neurol. 2016;137:257–77. 10.1016/B978-0-444-63437-5.00019-4 [DOI] [PubMed] [Google Scholar]
- 3. HALLPIKE CS: Ménière’s disease. Postgrad Med J. 1955;31(357):330–40. 10.1136/pgmj.31.357.330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Agrawal Y, Minor LLB: Ménière’s Disease and other causes of episodic vertigo.In: Bronstein AM. Vertigo and imbalance Oxford University press.2013;242 10.1093/med/9780199608997.003.0022 [DOI] [Google Scholar]
- 5. Merchant SN, Adams JC, Nadol JB: Pathophysiology of Meniere's syndrome: are symptoms caused by endolymphatic hydrops? Otol Neurotol. 2005;26(1):74–81. 10.1097/00129492-200501000-00013 [DOI] [PubMed] [Google Scholar]
- 6. SCHUKNECHT HF: Meniere's disease. Arch Otolaryngol. 1963;78:110. [DOI] [PubMed] [Google Scholar]
- 7. Thompsen J, Bretlau P: General conclusions.In Pfaltz CR (Ed). Controversial aspects of Ménière’s disease; New York: Georg Thieme Verlag Stuttgart1986:120–136. [Google Scholar]
- 8. Patel M, Agarwal K, Arshad Q, et al. : Intratympanic methylprednisolone versus gentamicin in patients with unilateral Ménière’s disease: A randomised, double-blind, comparative effectiveness trial. Lancet. 2016;388(10061):2753–62. 10.1016/S0140-6736(16)31461-1 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 9. Alexander TH, Harris JP: Current epidemiology of Meniere's syndrome. Otolaryngol Clin North Am. 2010;43(5):965–70. 10.1016/j.otc.2010.05.001 [DOI] [PubMed] [Google Scholar]
- 10. Havia M, Kentala E, Pyykkö I: Prevalence of Menière’s disease in general population of Southern Finland. Otolaryngol Head Neck Surg. 2005;133(5):762–8. 10.1016/j.otohns.2005.06.015 [DOI] [PubMed] [Google Scholar]
- 11. Kotimäki J, Sorri M, Aantaa E, et al. : Prevalence of Meniere disease in Finland. Laryngoscope. 1999;109(5):748–53. 10.1097/00005537-199905000-00013 [DOI] [PubMed] [Google Scholar]
- 12. Watanabe Y, Mizukoshi K, Shojaku H, et al. : Epidemiological and clinical characteristics of Menière's disease in Japan. Acta Otolaryngol Suppl. 1995;115(sup519):206–10. 10.3109/00016489509121906 [DOI] [PubMed] [Google Scholar]
- 13. Wladislavosky-Waserman P, Facer GW, MokrI B, et al. : Meniere's disease: a 30-year epidemiologic and clinical study in Rochester, Mn, 1951–1980. Laryngoscope. 1984;94(8):1098–1102. 10.1288/00005537-198408000-00020 [DOI] [PubMed] [Google Scholar]
- 14. Okafor BC: Incidence of Menière’s Disease. J Laryngol Otol. 1984;98(8):775–9. 10.1017/S0022215100147449 [DOI] [PubMed] [Google Scholar]
- 15. Tyrrell JS, Whinney DJ, Ukoumunne OC, et al. : Prevalence, associated factors, and comorbid conditions for Ménière’s disease. Ear Hear. 2014;35(4):e162–9. 10.1097/AUD.0000000000000041 [DOI] [PubMed] [Google Scholar]
- 16. Ohmen JD, White CH, Li X, et al. : Genetic evidence for an ethnic diversity in the susceptibility to Ménière’s disease. Otol Neurotol. 2013;34(7):1336–41. [DOI] [PubMed] [Google Scholar]
- 17. Wiet RJ: Patterns of ear disease in the southwestern American Indian. Arch Otolaryngol. 1979;105(7):381–5. [DOI] [PubMed] [Google Scholar]
- 18. Requena T, Espinosa-Sanchez JM, Cabrera S, et al. : Familial clustering and genetic heterogeneity in Meniere's disease. Clin Genet. 2014;85(3):245–52. 10.1111/cge.12150 [DOI] [PubMed] [Google Scholar]
- 19. Lee JM, Kim MJ, Jung J, et al. : Genetic aspects and clinical characteristics of familial Meniere's disease in a South Korean population. Laryngoscope. 2015;125(9):2175–80. 10.1002/lary.25207 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 20. Frejo L, Soto-Varela A, Santos-Perez S, et al. : Clinical Subgroups in Bilateral Meniere Disease. Front Neurol. 2016;7:182. 10.3389/fneur.2016.00182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Frejo L, Martin-Sanz E, Teggi R, et al. : Extended phenotype and clinical subgroups in unilateral Meniere disease: A cross-sectional study with cluster analysis. Clin Otolaryngol. 2017;42(6):1172–80. 10.1111/coa.12844 [DOI] [PubMed] [Google Scholar]
- 22. Belinchon A, Perez-Garrigues H, Tenias JM, et al. : Hearing assessment in Menière’s disease. Laryngoscope. 2011;121(3):622–6. 10.1002/lary.21335 [DOI] [PubMed] [Google Scholar]
- 23. Flook M, Lopez Escamez JA: Meniere’s Disease: Genetics and the Immune System. Curr Otorhinolaryngol Rep. 2018;6(1):24–31. 10.1007/s40136-018-0182-8 [DOI] [Google Scholar]
- 24. Morrison AW, Bailey ME, Morrison GA: Familial Ménière’s disease: Clinical and genetic aspects. J Laryngol Otol. 2009;123(1):29–37. 10.1017/S0022215108002788 [DOI] [PubMed] [Google Scholar]
- 25. Hietikko E, Kotimäki J, Sorri M, et al. : High incidence of Meniere-like symptoms in relatives of Meniere patients in the areas of Oulu University Hospital and Kainuu Central Hospital in Finland. Eur J Med Genet. 2013;56(6):279–85. 10.1016/j.ejmg.2013.03.010 [DOI] [PubMed] [Google Scholar]
- 26. Xenellis J, Morrison AW, McClowskey D, et al. : HLA antigens in the pathogenesis of Menière’s disease. J Laryngol Otol. 1986;100(1):21–4. 10.1017/S0022215100098698 [DOI] [PubMed] [Google Scholar]
- 27. Lopez-Escamez JA, Vilchez JR, Soto-Varela A, et al. : HLA-DRB1*1101 allele may be associated with bilateral Méniére’s disease in southern European population. Otol Neurotol. 2007;28(7):891–5. [DOI] [PubMed] [Google Scholar]
- 28. Hietikko E, Kotimäki J, Okuloff A, et al. : A replication study on proposed candidate genes in Ménière’s disease, and a review of the current status of genetic studies. Int J Audiol. 2012;51(11):841–5. 10.3109/14992027.2012.705900 [DOI] [PubMed] [Google Scholar]
- 29. Gazquez I, Moreno A, Aran I, et al. : MICA-STR A.4 is associated with slower hearing loss progression in patients with Ménière’s disease. Otol Neurotol. 2012;33(2):223–9. 10.1097/MAO.0b013e31824296c8 [DOI] [PubMed] [Google Scholar]
- 30. Requena T, Gazquez I, Moreno A, et al. : Allelic variants in TLR10 gene may influence bilateral affectation and clinical course of Meniere's disease. Immunogenetics. 2013;65(5):345–55. 10.1007/s00251-013-0683-z [DOI] [PubMed] [Google Scholar]
- 31. Cox GM, Kithcart AP, Pitt D, et al. : Macrophage migration inhibitory factor potentiates autoimmune-mediated neuroinflammation. J Immunol. 2013;191(3):1043–54. 10.4049/jimmunol.1200485 [DOI] [PubMed] [Google Scholar]
- 32. Liu YC, Tsai YH, Tang SC, et al. : Cytokine MIF Enhances Blood-Brain Barrier Permeability: Impact for Therapy in Ischemic Stroke. Sci Rep. 2018;8(1): 743. 10.1038/s41598-017-16927-9 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 33. Gázquez I, Moreno A, Requena T, et al. : Functional variants of MIF, INFG and TFNA genes are not associated with disease susceptibility or hearing loss progression in patients with Ménière's disease. Eur Arch Otorhinolaryngol. 2013;270(4):1521–9. 10.1007/s00405-012-2268-0 [DOI] [PubMed] [Google Scholar]
- 34. Yazdani N, Khorsandi Ashtiani MT, et al. : Association between MIF gene variation and Meniere's disease. Int J Immunogenet. 2013;40(6):488–91. 10.1111/iji.12058 [DOI] [PubMed] [Google Scholar]
- 35. Li L, Wang Y, An L, et al. : A network-based method using a random walk with restart algorithm and screening tests to identify novel genes associated with Menière’s disease. PLoS One. 2017;12(8):e0182592. 10.1371/journal.pone.0182592 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 36. Cabrera S, Sanchez E, Requena T, et al. : Intronic variants in the NFKB1 gene may influence hearing forecast in patients with unilateral sensorineural hearing loss in Meniere's disease. PLoS One. 2014;9(11):e112171. 10.1371/journal.pone.0112171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Frejo L, Requena T, Okawa S, et al. : Regulation of Fn14 Receptor and NF-κB Underlies Inflammation in Meniere's Disease. Front Immunol. 2017;8:1739. 10.3389/fimmu.2017.01739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Requena T, Cabrera S, Martín-Sierra C, et al. : Identification of two novel mutations in FAM136A and DTNA genes in autosomal-dominant familial Meniere's disease. Hum Mol Genet. 2015;24(4):1119–26. 10.1093/hmg/ddu524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Martín-Sierra C, Requena T, Frejo L, et al. : A novel missense variant in PRKCB segregates low-frequency hearing loss in an autosomal dominant family with Meniere's disease. Hum Mol Genet. 2016;25(16):3407–15. 10.1093/hmg/ddw183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Martín-Sierra C, Gallego-Martinez A, Requena T, et al. : Variable expressivity and genetic heterogeneity involving DPT and SEMA3D genes in autosomal dominant familial Meniere's disease. Eur J Hum Genet. 2017;25(2):200–7. 10.1038/ejhg.2016.154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kim BJ, Kim AR, Han KH, et al. : Distinct vestibular phenotypes in DFNA9 families with COCH variants. Eur Arch Otorhinolaryngol. 2016;273(10):2993–3002. 10.1007/s00405-015-3885-1 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 42. Greco A, Gallo A, Fusconi M, et al. : Meniere's disease might be an autoimmune condition? Autoimmun Rev. 2012;11(10):731–8. 10.1016/j.autrev.2012.01.004 [DOI] [PubMed] [Google Scholar]
- 43. Yoo TJ, Yazawa Y, Tomoda K, et al. : Type II collagen-induced autoimmune endolymphatic hydrops in guinea pig. Science. 1983;222(4619):65–7. 10.1126/science.6623056 [DOI] [PubMed] [Google Scholar]
- 44. Yoo TJ, Kwon SS, Shea J, et al. : Presence of autoantibodies in the sera of Ménière’s disease. International Congress Series. 2003;1240:1195–9. 10.1016/S0531-5131(03)00813-6 [DOI] [Google Scholar]
- 45. Riente L, Bongiorni F, Nacci A, et al. : Antibodies to inner ear antigens in Meniere's disease. Clin Exp Immunol. 2004;135(1):159–63. 10.1111/j.1365-2249.2004.02317.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Xu WD, Zhao Y, Liu Y: Role of the TWEAK/Fn14 pathway in autoimmune diseases. Immunol Res. 2016;64(1):44–50. 10.1007/s12026-015-8761-y [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 47. Pathak S, McDermott MF, Savic S: Autoinflammatory diseases: update on classification diagnosis and management. J Clin Pathol. 2017;70(1):1–8. 10.1136/jclinpath-2016-203810 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 48. Ancient missense mutations in a new member of the RoRet gene family are likely to cause familial Mediterranean fever. The International FMF Consortium. Cell. 1997;90(4):797–807. 10.1016/S0092-8674(00)80539-5 [DOI] [PubMed] [Google Scholar]
- 49. French FMF Consortium: A candidate gene for familial Mediterranean fever. Nat Genet. 1997;17(1):25–31. 10.1038/ng0997-25 [DOI] [PubMed] [Google Scholar]
- 50. Hoffman HM, Mueller JL, Broide DH, et al. : Mutation of a new gene encoding a putative pyrin-like protein causes familial cold autoinflammatory syndrome and Muckle-Wells syndrome. Nat Genet. 2001;29(3):301–5. 10.1038/ng756 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 51. Jesus AA, Goldbach-Mansky R: IL-1 blockade in autoinflammatory syndromes. Annu Rev Med. 2014;65:223–44. 10.1146/annurev-med-061512-150641 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 52. Canna SW, de Jesus AA, Gouni S, et al. : An activating NLRC4 inflammasome mutation causes autoinflammation with recurrent macrophage activation syndrome. Nat Genet. 2014;46(10):1140–6. 10.1038/ng.3089 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 53. Zhou Q, Wang H, Schwartz DM, et al. : Loss-of-function mutations in TNFAIP3 leading to A20 haploinsufficiency cause an early-onset autoinflammatory disease. Nat Genet. 2016;48(1):67–73. 10.1038/ng.3459 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 54. Frejo L, Gallego-Martinez A, Requena T, et al. : Proinflammatory cytokines and response to molds in mononuclear cells of patients with Meniere disease. Sci Rep. 2018;8(1): 5974. 10.1038/s41598-018-23911-4 [DOI] [PMC free article] [PubMed] [Google Scholar]