ABSTRACT
In low-resource settings, inpatient case fatality for severe acute malnutrition (SAM) remains high despite evidenced-based protocols and resources to treat SAM. Key reasons include a combination of insufficiently trained staff, poor teamwork and inadequate compliance to WHO treatment guidelines which are proven to reduce mortality. Checklists have been used in surgery and obstetrics to ameliorate similarly complicated yet repetitive work processes and may be a key strategy to improving inpatient SAM protocol adherence and reducing unnecessary death. Here, we share our experience developing and piloting an inpatient malnutrition checklist (MLNC) for children 6 to 59 months and associated scoring system to coordinate care delivery, improve team documentation, strengthen WHO malnutrition protocol adherence and facilitate quality improvement in a district hospital in rural Rwanda. MLNC was developed after careful review of the 2009 Rwandan National Nutrition Protocol and 2013 WHO malnutrition guidelines. Critical steps were harmonized, extracted and designed into an initial MLNC with input from pediatric ward nurses, doctors, a locally based pediatrician and a registered dietitian. A scoring system was developed to facilitate quality improvement. Using the standard Plan-Do-Study-Act cycle, MLNC was modified and progress assessed on a monthly to bimonthly basis. Significant modifications occurred in the first 6 months of piloting including incorporation of treatment reminders and formatting improvements, as well as initiation of the MLNC from the emergency department. The MLNC is the first checklist to be developed that unifies WHO 10 steps of treatment of inpatient SAM with local standards. Anecdotally, MLNC was observed to identify gaps in key malnutrition care, promote protocol adherence and facilitate quality improvement. Data gathering on the MLNC local facility impact is underway. Collaborative international efforts are needed to create an inpatient malnutrition checklist for wider use to improve quality and reduce unnecessary, facility-based child mortality.
KEYWORDS: Malnutrition, checklists, quality improvement, low-resource setting, under-5 mortality
Background
Globally, approximately 13 million children are diagnosed with severe acute malnutrition (SAM) annually, with 1–2 million preventable child deaths associated with SAM [1]. Evidence shows that WHO guidelines have led to improved survival and mortality of children admitted to inpatient facilities for SAM [2] and that case fatality may be reduced with strict compliance to treatment recommendations [3,4].
In low-resource settings, inpatient case fatality for inpatient malnutrition remains high despite availability of evidenced-based treatment protocols and resources [1,5]. Key reasons include insufficiently trained staff, poor teamwork and inadequate compliance to WHO treatment recommendations proven to reduce mortality [6–10]. WHO Checklists have been developed in surgery [11] and obstetrics [12] to ameliorate similarly complicated, yet repetitive work processes. The WHO Surgical Safety Checklist was created and implemented to decrease adverse events and increase teamwork amongst groups that can be hierarchical and disempowering to healthcare workers [13,14]. Since implementation, the Surgical Checklist has led to reductions in morbidity and mortality [15], as well as improved adherence to processes of care, teamwork and communication [14,15]. In anesthesia, checklists were able to improve process adherence and capture performance of critical safety elements [16].
In Rwanda, a national Performance-Based Financing (PBF) scheme was previously implemented to provide financial incentives to health providers for improvements in key national health priority output indicators related to maternal and child-care [17]. One of the indicators – ‘Number of malnourished children referred to district hospital for treatment during preventive care visit’ – is tied to improvement in higher-level referral for malnutrition. While this scheme may help to increase access to services via referrals, it’s limited in its ability to affect quality of inpatient malnutrition care.
We propose, that the development of a checklist to guide the inpatient management of malnutrition (encompassing severe and moderate complicated malnutrition as well as severe uncomplicated malnutrition) in low-resource settings is a key strategy to adherence improvement to the inpatient WHO malnutrition protocol and reduction of unnecessary deaths from malnutrition at the facility level. The inpatient management of acute malnutrition is particularly amenable to a checklist format, given 10 clear steps outlined by WHO. Progression of treatment steps is largely the same from patient to patient with most deviations during acute stabilization. Similar to surgery, malnutrition requires effective communication, timely action and collaborative team effort to ensure high quality, efficient patient care and reduce deaths. A malnutrition checklist could improve communication, streamline documentation and improve delivery of evidence-based malnutrition care to patients from the time of admission through rehabilitation and discharge to improve adherence to WHO protocols and reduce mortality.
Here, we describe development and pilot testing of an inpatient malnutrition checklist (MLNC) and scoring system for children 6–59 months. MLNC was developed to coordinate care delivery, team documentation, communication, improve inpatient WHO malnutrition protocol adherence and facilitate QI work on the wards of a district hospital in rural Rwanda. We hope that this shared experience and protocol to date can be used as a starting point for others to modify and utilize in their own settings. Additionally, we hope to raise awareness and call for an international collaborative to undertake the development of a global malnutrition checklist to be used as a resource in reducing child mortality.
Objective
MLNC aimed to create a single, streamlined document that unified WHO and national Rwandan guidelines for inpatient malnutrition care that could be used by frontline healthcare workers as a guidance of critical steps in malnutrition management. MLNC was designed to coordinate an entire teams’ documentation of malnutrition care which can span weeks in duration. Thus, while initially filled out by a physician in the emergency department, the MLNC also includes documentation fields for nurses and/or nutritionists depending on workflow of the hospital. Lastly, a scoring system based on the MLNC was developed to enable hospitals to more easily implement quality improvement (QI) projects that identify and address gaps in key process indicators. In order to not disrupt regional requirements in medical record documentation, this checklist was implemented as additional rather than a replacement of routine documentation practices.
Methods
A draft MLNC was developed in November 2015 after critical review of the Rwandan National Nutrition Protocol [18] and the WHO 2013 malnutrition guidelines [19]. There are 10 critical steps of inpatient acute malnutrition management from diagnosis in the emergency room through the completion of inpatient care [20]. These steps were extracted, harmonized, and designed into the initial MLNC with collaborative end-user feedback by local nurses and physicians, as well as a consultant pediatrician and registered dietitian-supporting treatment on the unit. Local staff, including the hospital’s general practitioners, pediatric and emergency room nurses, and nutritionist, were formally trained on MLNC theory and use to promote smooth adoption into routine clinical care.
Checklists were printed on colored paper to increase visibility in the patient chart and clean copies were kept in the emergency and pediatric departments. The emergency department doctor and nurse initiated the checklist, registered the child as having acute malnutrition, documented height and weight, and completed the initial medical management documentation. After transfer to the pediatric department, checklist documentation was reviewed and daily treatment iterated by the pediatric department staff (nurse, doctor, nutritionist). Generally, the nutritionist updated height, weight and calculated WHO z-scores; doctors prescribed feeding regimens and medications; and nurses documented care implementation and adverse reactions to feeding, such as vomiting. Pediatric team disagreements regarding care were addressed during ward rounds.
Over the next 6 months, experience with MLNC was discussed during weekly QI pediatric team meetings and revisions made based on user feedback. Last, a simplified scoring system was developed to assess malnutrition protocol adherence based on MLNC documentation (Supplemental Material Figure A: Malnutrition Checklist March 2017). Figure 1 describes the components of inpatient malnutrition management that were assessed for in the QI project and the associated scoring of the different components.
Figure 1.
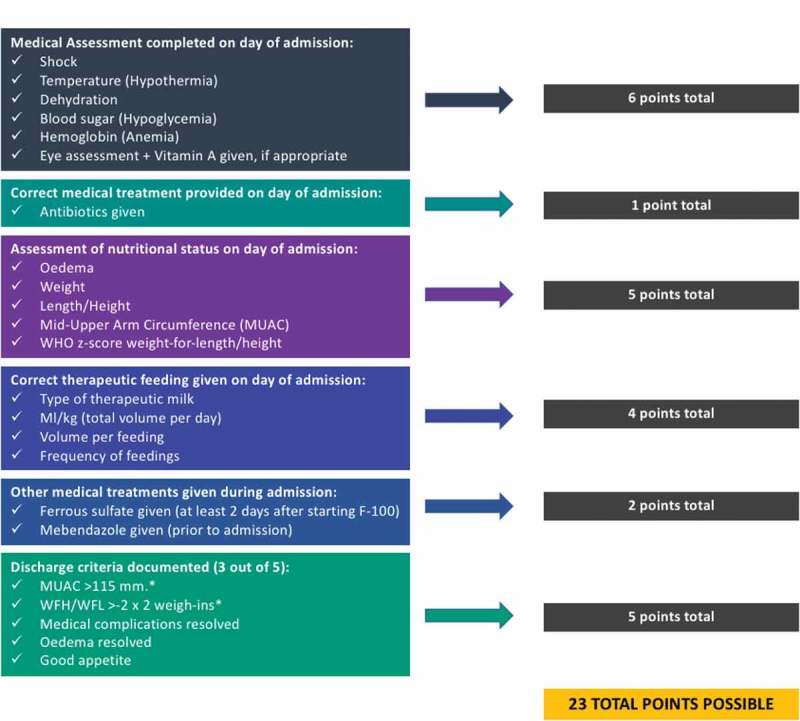
Scoring system for assessment of adherence to an inpatient malnutrition checklist (MLNC).
The pediatric QI team at Rwinkwavu District Hospital in Rwinkwavu, Rwanda began its first QI project using the MLNC in September 2015 focusing initially on documentation adherence. The subsequent QI project narrowed its scope to address specific documentation gaps, such as identification of shock in the emergency department for children with a diagnosis of SAM. The Plan-Do-Study-Act (PSDA) cycle of QI was used to plan the QI project, establish baseline indicators, implement use of the checklist, and make modifications as time went on.
Results
MLNC was modified and progress of protocol adherence to the area of focus chosen assessed on a monthly to bimonthly basis. Run charts were displayed on the pediatric unit to track the progress of the QI project and to encourage staff
Modifications to MLNC during the first 6 months of use included clarifying criteria for advancing therapeutic milk feedings, prompts for medication provision on the appropriate day of treatment, medication dosage references, and guidance on discharge criteria and education. The nutritionist reported positive feedback related to the tool, particularly its ease in being able to monitor the daily progress of the patient, while the doctors felt that clearly outlining and prompting treatment for the 10 critical treatment steps was useful for proper treatment of malnutrition.
Now that MLNC has been in use for over two years, efforts are underway to document the QI project outcomes and its effects on inpatient malnutrition treatment processes. The QI teams continue to meet regularly and have begun identifying more granular components of the MLNCs to focus on, such as hypoglycemia.
Conclusions
Preliminary experience with a locally developed MLNC suggests it is helpful in simplifying the complex treatment of inpatient malnutrition. Anecdotally, the MLNC was successfully implemented to address gaps in key malnutrition care processes as well as facilitate QI which promoted coordinated delivery of inpatient malnutrition services with improved adherence to protocols.
We experienced a number of challenges which will likely be common experiences to others using this tool or developing their own. First, the MLNC requires supportive implementation and leadership by respected mentors to facilitate the acceptance of the checklist and lead to improved team work. In our districts, we were fortunate that in addition to engaged hospital staff and regular support by a pediatrician and registered dietitian, hospitals are supported by routine QI mentorship through previously described MESH mentors [21–23] who provide enhanced supervision of staff on clinical and systems improvement initiatives. Second, the MLNC is ideally initiated in the emergency room setting requiring coordination between pediatric and emergency room staff. Poor early identification of malnutrition limits MLNC utility in the early, emergency management of acute malnutrition. Last, implementing MLNC as additional rather than replacement of current documentation puts a higher documentation burden on healthcare workers. However, as in our experience, once hospitals see the utility of MLNC they may choose to replace old documentation practices with the MLNC thus reducing redundancy in documentation and increasing visibility of malnutrition management.
In Rwanda, use of the MLNC has already expanded to a second District Hospital and we hope to share these experiences with other Rwandan facilities to improve the quality of care of inpatient acute malnutrition management regionally.
More broadly, we hope that this work will be the first step in calling for a MLNC which has input from international stakeholders and might be used and adapted to local country settings to improve adherence to evidence based protocols for inpatient malnutrition treatment, ultimately resulting in decreased mortality related to malnutrition for children under five.
Responsible Editor Stig Wall, Umeå University, Sweden
Funding Statement
This work was carried out through support from the Global Pediatrics Program of the Department of Pediatrics at Boston Children's Hospital, Partners In Health/Inshuti Mu Buzima (PIH/IMB), Rwinkwavu District Hospital, Ministry of Health Rwanda, and Boston Children’s Hospital Global Health Program.
Acknowledgements
We would like to acknowledge all the Rwandan healthcare workers who participated for their leadership, involvement and perseverance which make this work possible. Your resilience, grit and hope continually inspire us. Thank you to the Rwandan Ministry of Health for their visionary leadership and partnership with PIH/IMB to improve the lives of women and children. Thank you to the PIH/IMB mentorship and QI team, for their guidance in QI activities and training. Thank you to Judith Palfrey, Director of the Global Pediatrics Program at Boston Children's Hospital, and the Global Pediatrics Program of the Department of Pediatrics at Boston Children's Hospital for their technical support.
Disclosure statement
Authors AM, SB, RN, AD, and SN were employees of Rwinkwavu District Hospital at the time of the study but did not receive additional financial benefits as a result of participation in this study.
Ethics and consent
Not required.
Paper context
Severe acute malnutrition remains a significant cause of preventable child death, despite clear protocols and resources to treat it. The World Health Organization has developed clinical checklists which have reduced facility based mortality. We developed and implemented an inpatient malnutrition checklist with a scoring system for documenting quality improvement. We hope this work will inspire international dialogue to create a global malnutrition checklist to promote quality care, World Health Organization protocol adherence and child survival.
Supplemental data
Supplemental data for this article can be accessed here.
References
- [1]. Collins S. Treating severe acute malnutrition seriously. Arc Dis Child. 2007;92:453–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2]. Maitland K, Berkley JA, Shebbe M, et al. Children with severe malnutrition: can those at highest risk of death be identified with the WHO protocol? PLoS Med. 2006;3:e500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Collins S, Sadler K. Outpatient care for severely malnourished children in emergency relief programmes: a retrospective cohort study. Lancet. 2002;360:1824–1830. [DOI] [PubMed] [Google Scholar]
- [4]. Ahmed T, Ali M, Ullah MM, et al. Mortality in severely malnourished children with diarrhoea and use of a standardised management protocol. Lancet. 1999;353:1919–1922. [DOI] [PubMed] [Google Scholar]
- [5]. de Onis M, Weise Prinzo Z. Managing children with severe acute malnutrition–what’s new? A health policy perspective. Indian Pediatr. 2014;51:17–18. [DOI] [PubMed] [Google Scholar]
- [6]. Ashworth A, Chopra M, McCoy D, et al. WHO guidelines for management of severe malnutrition in rural South African hospitals: effect on case fatality and the influence of operational factors. Lancet. 2004;363:1110–1115. [DOI] [PubMed] [Google Scholar]
- [7]. Deen JL, Funk M, Guevara VC, et al. Implementation of WHO guidelines on management of severe malnutrition in hospitals in Africa. Bull World Health Organ. 2003;81:237–245. [PMC free article] [PubMed] [Google Scholar]
- [8]. Karaolis N, Jackson D, Ashworth A, et al. WHO guidelines for severe malnutrition: are they feasible in rural African hospitals? Arch Dis Child. 2007;92:198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. Nathoo KJ, Bannerman CH, Pirie DJ. Pattern of admissions to the paediatric medical wards (1995 to 1996) at Harare Hospital, Zimbabwe. Cent Afr J Med. 1999;45:258–263. [DOI] [PubMed] [Google Scholar]
- [10]. Puoane T, Sanders D, Chopra M, et al. Evaluating the clinical management of severely malnourished children–a study of two rural district hospitals. South Afr Med J. 2001;91:137–141. [PubMed] [Google Scholar]
- [11]. Jackson J. Managing perioperative care In: Bullock I, Macleod Clark J, Rycroft-Malone J, editors. Adult nursing practice: using evidence in care. Oxford: Oxford University Press; 2012. p. 446. [Google Scholar]
- [12]. Spector JM, Lashoher A, Agrawal P, et al. Designing the WHO safe childbirth checklist program to improve quality of care at childbirth. Int J Gynaecol Obstet. 2013;122:164–168. [DOI] [PubMed] [Google Scholar]
- [13]. Russ S, Rout S, Sevdalis N, et al. Do safety checklists improve teamwork and communication in the operating room? A systematic review. Ann Surg. 2013;258:856–871. [DOI] [PubMed] [Google Scholar]
- [14]. Leape LL. The checklist conundrum. N Engl J Med. 2014;370:1063–1064. [DOI] [PubMed] [Google Scholar]
- [15]. Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–499. [DOI] [PubMed] [Google Scholar]
- [16]. Kahlenberg L, Harsey L, Patterson M, et al. Implementation of a modified WHO pediatric procedural sedation safety checklist and its impact on risk reduction. Hosp Pediatr. 2017;7:225–231. [DOI] [PubMed] [Google Scholar]
- [17]. Basinga P, Gertler PJ, Binagwaho A, et al. Effect on maternal and child health services in Rwanda of payment to primary health-care providers for performance: an impact evaluation. Lancet. 2011;377:1421–1428. [DOI] [PubMed] [Google Scholar]
- [18]. Ministry of Health Rwanda national nutrition protocol. Kigali: Government of Rwanda; 2009. [Google Scholar]
- [19]. World Health Organization Guideline: updates on the management of severe acute malnutrition in infants and children. Geneva: World Health Organization; 2013. [PubMed] [Google Scholar]
- [20]. World Health Organization Pocket book of hospital care for children: guidelines for the management of common childhood illnesses. 2nd ed. Geneva: World Health Organization; 2013. [PubMed] [Google Scholar]
- [21]. Anatole M, Magge H, Redditt V, et al. Nurse mentorship to improve the quality of health care delivery in rural Rwanda. Nurs Outlook. 2013;61:137–144. [DOI] [PubMed] [Google Scholar]
- [22]. Manzi A, Magge M, Hedt-Gauthier BL, et al. Clinical mentorship to improve pediatric quality of care at the health centers in rural Rwanda: a qualitative study of perceptions and acceptability of health care workers. BMC Health Serv Res. 2014;275–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23]. Magge M, Anatole M, Rwabukwisi FC, et al. Mentoring and quality improvement strengthen integrated management of childhood illness implementation in rural Rwanda. Arch Dis Child. 2015;100:565–570. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


