Abstract
The purpose of this study was to assess occupational injury characteristics and predictors among career firefighters. A total of 249 firefighters from central Texas and northern California participated in this internet-based survey. Approximately 27% of firefighters had reported an occupational injury within the previous 12 months. The majority of injuries occurred on the scene of a non-fire call while performing an activity that required lifting, pushing, or pulling. Firefighters’ backs were most frequently injured. Of the reported injuries, approximately 18% returned to work on modified duty, but 46% were not allowed to work due to their occupational injuries. Firefighters who reported occupational injuries were more likely to be older and experiencing occupational stress compared to their co-workers who did not report occupational injuries. Injured firefighters were also more likely to report fewer job rewards (money/salary), over-commitment, less esteem (respect and support), and fewer promotional prospects. These injury factors should be incorporated into interventions to reduce or prevent workplace injuries.
Every 8 minutes a firefighter is injured (Haynes & Molis, 2015b). Firefighters respond to various emergencies during each work shift that place them in harm’s way. These emergencies include medical calls, fire suppression, and hazardous material exposures. According to the National Fire Protection Association (NFPA), in 2015, approximately 1.16 million firefighters were working in the United States (U.S.); 30% were career firefighters and 70% were volunteer firefighters (Hylton & Stein, 2017). In 2015, the NFPA reported 68,085 firefighter injuries sustained in the line of duty (Hylton & Molis, 2016). In addition to occupational injuries, 8,350 infectious disease and 27,250 hazardous condition exposures occurred (Hylton & Molis, 2016). An estimated 43% of the firefighter injuries occurred at the scene of a fire (on the fireground), with the leading injury causes including falls, slips, and jumps (27.2%) followed by overexertion and strain (27.2%) (Hylton & Molis, 2016).
Injuries incurred by firefighters range from first aid to fatal injuries. Sixty-eight on-duty firefighters died in 2015 including: 32 volunteer firefighters, 24 career firefighters, 6 federal land agency firefighters, 3 federal contractor firefighters, 1 civilian employee of the military, and 1 state prison inmate (Fahy, LeBlanc, & Molis, 2016). Approximately 51% of these firefighter deaths were attributed to sudden cardiac death (Fahy et al., 2016). Workers’ compensation claims can be costly (anywhere from US $5,168 to US $34,000 per claim) and as much as US $2.8 billion to US $7.8 billion is spent annually to prevent and address firefighter injuries at a national level (National Institute of Standards and Technology [NIST], 2005; Walton, Conrad, Furner, & Samo, 2003). In addition to workers’ compensation costs, Los Angeles fire officials reported spending US $51,000 per day, or US $19 million annually on overtime to cover shifts left vacant by firefighters absent due to injury (Dolan, 2015). In an effort to reduce firefighter occupational injuries, the National Occupational Research Agenda (NORA) has set goals to reduce injuries and fatalities associated with structural firefighting by 10% and vehicle-related traumatic injuries by 20% (National Institute for Occupational Safety and Health (NIOSH), 2013).
This review of the literature has identified several risk factors for occupational injury among firefighters including demographics (i.e. years of service, age, rank, ethnicity), personal factors (i.e., depression, stress, sleep disorders, smoking status), and organizational factors. However, the literature findings conflicted. For instance, Moore-Merrell, Zhou, McDonald-Valentine, Goldstein, and Slocum (2008) and Szubert and Sobala (2002) reported that firefighters with fewer years of service/tenure were at increased risk for injury, whereas Liao, Arvey, Butler, and Nutting (2001) found tenure to only be significant in regard to length of recovery from injury. Meanwhile, Hong, Chin, Phelps, Feld, and Vogel (2012) reported firefighters with more than 17 years of fire service were more likely to report an injury. In addition, Seabury and McLaren (2010a) found the frequency and severity of firefighter injuries, particularly musculoskeletal injuries, to be worse among older firefighters. According to Jahnke, Poston, Haddock, and Jitnarin (2013), none of the demographic variables (e.g., ethnicity, age, marital status, education, rank, or years of service/tenure) were associated with occupational injuries. However, former smokers (compared to never smokers), and firefighters with depressive symptoms were at higher risk for injury. Research has also shown that firefighters with strong organizational commitments were less likely to report occupational injuries (Hong et al., 2012). Moore-Merrell et al. (2008) performed a frequency analysis and found that the leading contributors to on duty injury were lack of situational awareness (37.4%), lack of wellness/fitness (28.6%), and human error (10.7%).
Strains, sprains, and/or muscular pain are the most common types of occupational injuries to occur among firefighters (55.3%) in every type of duty (i.e., fire scene, non-fire emergency, and training), followed by wound, cut, bleeding, and bruises (15.3%; Haynes & Molis, 2015b). The leading causes of fire scene injuries were falls/slips/jumps (28.7%), overexertion/strain (25.9%), contact with an object (10.9%), and exposure to fire products (9.5%; Haynes & Molis, 2015b). Other studies confirmed these findings, indicating that strains and sprains were the leading source of injury, and overexertion was one of the primary causes of injury among firefighters (Poplin, Harris, Pollack, Peate, & Burgess, 2011; Reichard & Jackson, 2010; Szubert & Sobala, 2002; Walton et al., 2003).
As an occupational health professional, the key to implementing an effective workplace health and safety program, aimed at reducing occupational injuries, is to be cognizant of which factors increase firefighters’ risk of occupational injury. The purpose of this study was to assess occupational injury characteristics (i.e. injury location, activity being performed, cause of injury, body part injured, treatment sought, and return to work outcome) and injury predictors among career firefighters.
Methods
A cross-sectional survey was conducted with career firefighters from central Texas and northern California. Convenience sampling was used to recruit from fire departments that were accessible and in close proximity to the researchers. Recruitment of firefighters used various strategies. First, staff at two occupational health clinics approached firefighters during their annual physical examinations. Second, research staff distributed study flyers with contact information at fire stations and at fire training educational programs. Third, fire administrators disseminated study information to their fire department members via email. Depending on recruitment channels, the response rate varied significantly, ranging from 39% to 3%. When firefighters were recruited by health care staff with whom they had rapport, their participation was relatively high (195/493 = 39.2% response rate), compared to those firefighters recruited by a researcher they did not know (45/1,549 = 2.9% response rate). Nine participants did not indicate their departments; therefore the recruitment method for them is unknown. A total of 301 firefighters from six fire departments (department size varied from 71 members to 1,129 members) were screened between March 2015 and March 2016. Of those screened, 253 attempted the online questionnaire. Of those who attempted the online questionnaire, four responses were removed (two completed the consent only, one did not meet the inclusion criteria, and one did not answer the dependent variable question regarding occupational injury). Thus, the final sample size was 249. The Committee of Human Research of the University of California, San Francisco, approved all study procedures. Participation was voluntary. Informed consent was documented from firefighter participants before they completed the online survey.
Measures
Demographic Characteristics.
Demographic and work-related characteristics included age, gender, race/ethnicity, years of fire service, position (rank), and number of hours worked in a shift (24 hours vs. 48 hours). Race/ethnicity was categorized as White non-Hispanic, Hispanic, Black or African American, Asian, or Other.
Occupational Stress.
The short version of the Effort-Reward Imbalance Questionnaire (ERI-S) was used to measure occupational stress. The effort reward imbalance model hypothesizes that perceived high effort spent and low reward received adversely affects individual health by eliciting negative emotions and causing stressful responses (Siegrist, 2012). The ERI-S is commonly used in occupational health research (Leineweber et al., 2010; Siegrist, 1996; Siegrist, Wege, Puhlhofer, & Wahrendorf, 2009). Leineweber et al. (2010) reported excellent internal consistency, with Cronbach alpha coefficients ≥ 0.80 for all three ERI-S scales. In this study, all Cronbach’s alpha values indicated high internal consistency (α > 0.70) with α=0.71 on the “effort” scale, α=0.80 on the “reward” scale, and α=0.79 on the “over-commitment” scale. The instrument consisted of 16 five-point Likert-scaled (1 = strongly disagree to 5 = strongly agree) items and contains three psychometric scales: effort, reward, and over-commitment. In addition, three subscales of the reward scale have been derived: esteem, promotion, and security. The higher the effort scale score, the more demands and/or obligations the firefighter is experiencing at work (i.e. pressure to work overtime). The lower the reward scale score, the fewer occupational rewards, such as salary, esteem, job security, and promotions, are received by the firefighter. Overcommitment is measured in the last scale; a higher score indicates a firefighter’s overcommitted work style.
Work-related injury.
Work-related injury was assessed by asking, “Within the past 12 months, have you experienced any work-related injuries?” using yes/no response categories. This question was prefaced by, “The following questions are about work-related injuries you have incurred in the past 12 months while working as a firefighter.” A work-related injury was defined according to the Occupational Safety and Health Administration (2001) standards (1904.5a) in the questionnaire as, “An injury is considered work-related if an event or exposure in the work environment caused or contributed to the condition or significantly aggravated a pre-existing condition.” Firefighters who reported a work-related injury were then asked about the injury location, activity being performed when injured, primary cause and type of injury, and the body part injured. These injury questions were adapted from the National Fire Protection Association (Hylton & Molis, 2015) injury survey of fire departments. Additionally, firefighters were asked if they sought health care, filed a workers’ compensation claim, or changed their duty status.
Location of Injury Occurrence.
Injury location was categorized as on the scene of a non-fire call, fire/rescue activities on the fireground, during training, responding to or returning from a call, or other/on-duty time (please specify). An additional category entitled “at the station” was created from “Other” free-typed responses that included activities that occurred at the station (i.e. checking the apparatus at the start of the shift, working out, station work). Responses under “Other” that were not included in “At the station” were: lifting/walking/climbing, chronic exposure, pneumonia, and unknown.
Activity Being Performed when Injured.
Firefighters were asked to select which primary activity they were performing when the injury occurred. If the injury occurred on the scene of a non-fire call, the following activities were listed: lifting/pushing/pulling or entering/exiting apparatus. If the injury occurred on the fire scene, the following activities were listed: advancing/directing hose, overhaul, forcible entry, ventilation, using ground ladders, rescue, salvage, working on aerial ladders, entering/exiting apparatus, loading/unloading/transporting equipment, and investigating. If the injury occurred during training, the following activities were listed: physical training, lifting individuals, advancing/directing hose, using ground ladders, rescue, entering/exiting apparatus, and loading/unloading/transporting equipment. Options listed under “other/on-duty time” included: strength training/weight lifting, aerobic exercise/other fitness activities, equipment apparatus checks, station maintenance, and “Other, please specify” free-type response. An additional category entitled, “roviding medical care” was created for “On the scene of a non-fire call” from free-typed responses such as “medical care kneeling before a patient” and “working on a full arrest.”
Primary Cause and Type of Injury, and Body Part Injured.
The following response options were provided for the primary cause of the work-related injury: fall/jump/slip/trip, overexertion or strain, contact with an object or struck by an object, exposure to fire products (products of combustion), exposure to chemicals, extreme weather, and other. Type of injury was categorized as: burn, dislocation or broken (fractured) bones, exposure to bloodborne pathogens (needlestick), hazardous chemical exposure, head injury, heat stroke, smoke or gas inhalation, sprain/strain/muscular pain, wound/cut/bleeding/bruise, and other. Injured body part locations included: head, neck, nose, eye(s), ear(s), hand, wrist, elbow, shoulder, back, hip, groin, knee, ankle, foot, and other. The terms calf and shin were incorporated into “knee” to accompany free text responses such as: “below knee on back of the leg”, “calf”, and “left shin.”
Health Care, Workers’ Compensation Claims, and Duty Status.
Firefighters were asked if they received health care (yes/no) and if a workers’ compensation claim was filed (yes/no). Duty status was assessed by three questions using a yes/no response for each: Were you subsequently placed on modified duty? Were you subsequently prohibited from working? Did you transfer jobs? All firefighter participants were asked if they had ever used personal sick leave, vacation, or traded time/shifts due to a work-related injury (yes/no).
Data Analyses
Data were analyzed using SPSS 23. Descriptive statistics were used for all study variables. Values for continuous variables were presented as means and standard deviations and categorical variables were summarized by frequencies and percentages. Chi-square analyses were used to compare demographic and work characteristics between firefighters who reported a work-related injury within the past 12 months and those who did not report an injury. A p-value of 0.05 or less was considered statistically significant. Analyses were based on the actual sample size, and no imputations were made for missing data.
Results
The majority of career firefighter participants were middle-aged (M = 41.8 years), White non-Hispanic (73.1%), and male (92%). They had worked many years in the fire service (M = 15.1 years) and the majority (78.3%) reported they worked 48-hour shifts at the fire department. Over one third (34.1%) identified their primary role as firefighter paramedic. Table 1 displays more details regarding demographic and work-related characteristics of career firefighter participants.
Table 1.
Demographic Characteristics of Firefighter Participants (N = 249)
| Characteristics | Mean | SD |
|---|---|---|
| Age (years) | 41.8 | 8.3 |
| Years worked in the fire service |
15.1 |
8.8 |
|
N |
% |
|
| Gender | ||
| Male | 229 | 92.0 |
| Female | 18 | 7.2 |
| Missing | 2 | 0.8 |
| Race/Ethnicity | ||
| White, non-Hispanic | 182 | 73.1 |
| Hispanic | 28 | 11.7 |
| Black or African American | 13 | 5.2 |
| Asian | 11 | 4.4 |
| Othera | 6 | 2.4 |
| Missing | 9 | 3.6 |
| Primary Role | ||
| Firefighter | 32 | 12.9 |
| Firefighter paramedic | 85 | 34.1 |
| Apparatus operator/engineer/driver | 48 | 19.3 |
| Company officer (Lt, Cpt) | 79 | 31.7 |
| Battalion chief | 3 | 1.2 |
| Missing |
2 |
0.8 |
| Type of Shift | ||
| 24 hours | 47 | 18.9 |
| 48 hours | 195 | 78.3 |
| Otherb | 5 | 2.0 |
| Missing | 2 | 0.8 |
Other: American Indian, Alaska Native, Native Hawaiian, and Other Pacific Islander, and Other
Other: 24 hour & 48 hour shifts (varies), 72 hours off & 48 hours on, 72 hours on, 96 hours on
Work-related Injuries
Approximately, 27% (67/249) of the career firefighter participants reported experiencing at least one work-related injury within the past 12 months. Of those injured, 82.1% (55/67) reported one injury, 11.9 % (8/67) reported two injuries, and 4.5% (3/67) reported three or more injuries within the past 12 months. One participant reported a work-related injury, but did not disclose any details about the injury or how many injuries incurred over the past 12 months. A total of 80 injuries were reported from 66 participants. Among those who reported injuries, 70% (56/80) filed a workers’ compensation claim and 70% received health care for their work-related injury. Due to their injuries, 46.3% (37/80) were prohibited from working, and 17.5% (14/80) were placed on modified duty. Of the 249 participants, 39 (15.7%) reported using sick leave, vacation, or traded time/shifts due to work-related injuries within the past 12 months. Table 2 provides more information on work-related injury characteristics.
Table 2.
Work-Related Injury Characteristics of Firefighter Participants (N = 249)
| Characteristics | N | % |
|---|---|---|
| Work-related injury within the past 12 months (yes)* | 67 | 26.9 |
| Reported 1 work-related injury within the past 12 months | 55 | 22.1 |
| Reported 2 work-related injuries within the past 12 months | 8 | 3.2 |
| Reported 3+ work-related injuries within the past 12 months |
3 |
1.2 |
| Injury reporting and duty status (n = 80 total injuries reported) | ||
| Filed a worker’s compensation claim (yes) | 56 | 70.0 |
| Received medical care due to work-related injury (yes) | 56 | 70.0 |
| Placed on modified duty due to work-related injury (yes) | 14 | 17.5 |
| Missing | 2 | 2.5 |
| Taken off duty due to a work-related injury (yes) | 37 | 46.3 |
| Missing |
1 |
1.3 |
| Used personal sick leave, vacation, or traded time/shifts due to a work-related injury within the past 12 months (yes) | 39 | 15.6 |
Of those who reported an injury (n = 67), one participant did not provide any further details, therefore, injury details are only known for 66 participants.
Injuries most commonly occurred at the scene of a non-fire call (31.3%), followed by on fire scene during fire/rescue activities (26.3%), and during training activities (20%). Lifting, pushing, and pulling (22.5%) activities at a non-fire call scene were the most common activities resulting in a work-related injury, followed by advancing/directing a hose (8.8%) on the fireground. The primary cause of injury reported was overexertion (64%), followed by falls, jumps, slips, and trips (12%). Approximately 79% of the injuries were classified as sprain, strain, and muscular pain, with the back (31.3%, 25/80) being the body part most frequently injured, followed by the knee/calf/shin (26.3%, 21/80). More information on the location, activity being performed, and type of injury can be found in Table 3. Figure 1 depicts the primary cause of injury, and Figure 2 shows the distribution of body parts injured.
Table 3.
Work-related Injury Characteristics (n = 80 total number of injuries reported)
| Place of Injury Occurrence and Activity Being Performed | N | % of 80 |
|---|---|---|
| On the scene of a non-fire call | 25 | 31.3 |
| Lifting, pushing, pulling | 18 | 22.5 |
| Providing medical care | 4 | 5.0 |
| Entering/exiting apparatus | 2 | 2.5 |
| Othera | 1 | 1.3 |
| On the fireground performing fire/rescue activities | 21 | 26.3 |
| Advancing/directing hose | 7 | 8.8 |
| Loading, unloading, and transporting equipment | 3 | 3.8 |
| Rescue | 3 | 3.8 |
| Otherb | 8 | 10.2 |
| During training | 16 | 20.0 |
| Physical training | 5 | 6.3 |
| Advancing/directing hose | 2 | 2.5 |
| Loading, unloading, and transporting equipment | 2 | 2.5 |
| Otherc | 7 | 8.9 |
| At the station | 10 | 12.5 |
| Strength training/weight lifting | 2 | 2.5 |
| Equipment/apparatus checks | 3 | 3.8 |
| Otherd | 4 | 5.0 |
| Unspecified | 1 | 1.3 |
| Responding to or returning from a call | 4 | 5.0 |
| Entering/exiting apparatus | 1 | 1.3 |
| Lifting, pushing, pulling | 1 | 1.3 |
| Unspecified | 2 | 2.5 |
|
Other/on-duty timee |
4 |
5.0 |
|
Type of Injury |
N |
% |
| Sprain, strain, muscular pain | 63 | 78.8 |
| Dislocation or broken (fractured) bones | 7 | 8.8 |
| Contagious disease exposure | 3 | 3.8 |
| Otherf | 7 | 8.8 |
Other: going down concrete steps (1)
Other: entering/exiting apparatus (1), overhaul (1), ventilation (1), working on aerial ladder (1), lifting (1), many of the answers could be used (1), all of the above (1), cumulative (1)
Other: lifting people (1), using ground ladders (1), entering/exiting apparatus (1), boat operations (1), swimming in river (1), forcible entry (1), building training props (1)
Other: station maintenance (1), cooking (1), squatting down (1), lifting hose (1)
Other: lifting/walking/climbing (1), chronic exposure (1), pneumonia (1), unknown (1)
Other: burn (1), smoke or gas inhalation (1), wound/cut/bleeding/bruise (1), cancer (1), herniated disc (2), piece of metal in eye (1)
Figure 1.
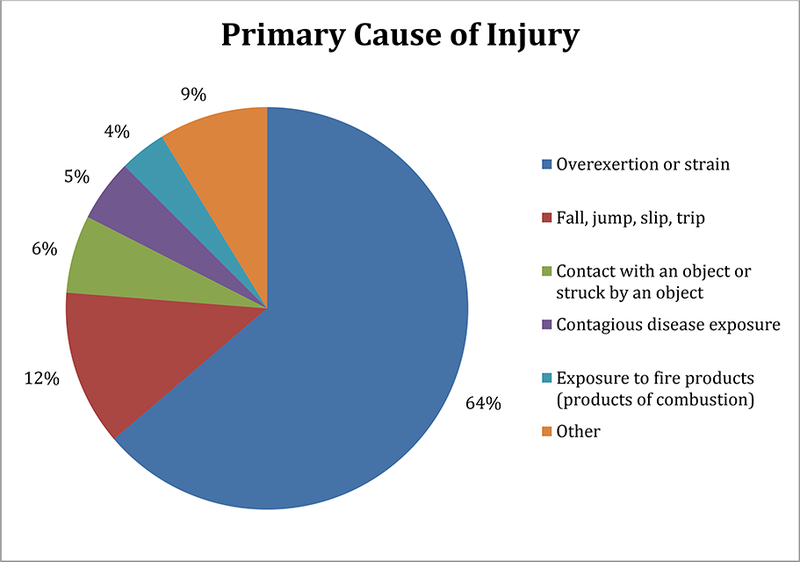
Primary Cause of Injury (n = 80 total injuries reported)
Figure 2.
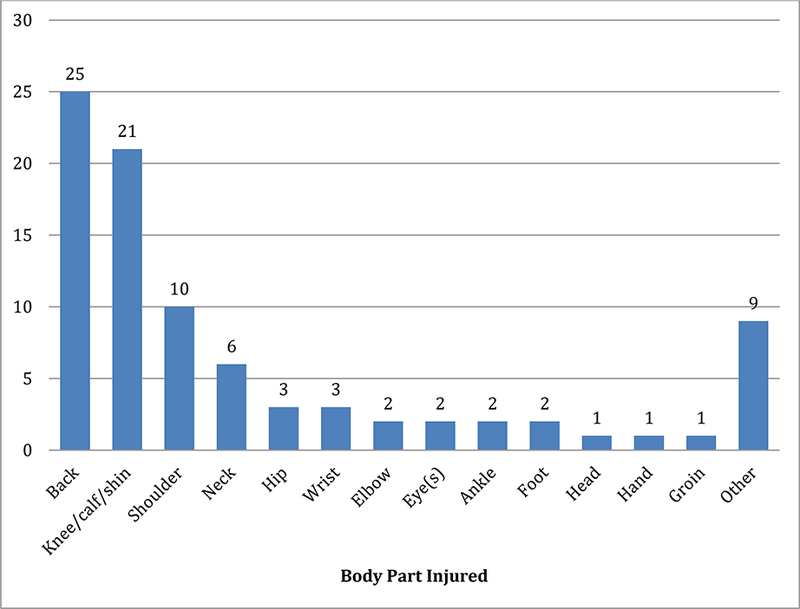
Body Part Injured (n = 80 total injuries reported)
* Total of number of body parts injured add up to 88 because participants could select more than one body part injured per an injury.
Other: airborne/respiratory/lungs, chest/intercostal muscles, arm, forearm, gastrointestinal upset
Comparison of Demographic and Work-Related Characteristics between Firefighters with and without Work-related Injury
Table 4 compares demographic and work-related characteristics between career firefighters who reported a work-related injury within the past 12 months and those career firefighters who did not report a work-related injury. Older career firefighters were more likely to report a work-related injury within the past 12 months (p = .031). In addition, career firefighters who reported more occupational stress as measured by the ERI ratio (p = .003), over-commitment (p = .030), fewer job rewards (p = .001), less esteem (p = .001), and fewer promotional prospects (p = .014) were also more likely to report a work-related injury compared to their co-workers who did not report an occupational injury within the past 12 months. Other characteristics such as gender, race/ethnicity, primary position, and type of shift were not significantly associated with work-related injury.
Table 4.
Comparison of Demographic and Work-Related Characteristics between Firefighters with and without Work-related Injury (N = 247)
|
Characteristics |
Work-related Injury (Yes) |
χ2 (p-value) |
|
|
N |
% |
||
| Gender | 1.58 (.264) | ||
| Male (n = 229) | 58 | 25.3 | |
| Female (n = 18) | 7 | 38.9 | |
| Race/Etdnicity | 3.25 (.517) | ||
| White, non-Hispanic (n = 182) | 45 | 24.7 | |
| Hispanic (n = 28) | 8 | 28.6 | |
| Black or African American (n = 13) | 6 | 46.2 | |
| Asian (n = 11) | 3 | 27.3 | |
| Otdera (n = 6) | 1 | 16.7 | |
| Primary Role | 6.31 (.177) | ||
| Firefighter (n = 32) | 8 | 25.0 | |
| Firefighter paramedic (n = 85) | 20 | 23.5 | |
| Apparatus operator/driver/engineer (n = 48) | 19 | 39.6 | |
| Company Officer (Lt, Cpt) (n = 79) | 18 | 22.8 | |
| Battalion chief (n = 3) | 0 | 0 | |
| Type of Shift | 2.18 (.336) | ||
| 24 hours (n = 47) | 11 | 23.4 | |
| 48 hours (n = 195) | 54 | 27.7 | |
| Otderb (n = 5) |
0 |
0 |
|
|
Work-related Injury |
|||||
|
Yes (n=67) |
No (n=182) |
t (p-value) |
|||
|
Mean |
SD |
Mean |
SD |
||
| Age | 43.7 | 7.6 | 41.1 | 8.5 | 2.17 (.031) |
| Years worked in tde fire service | 16.5 | 9.4 | 14.6 | 8.6 | 1.39 (.165) |
| Occupational Stress | |||||
| Effort Reward Ratio | 1.0 | 0.3 | 0.9 | 0.2 | 2.96 (.003) |
| Effort | 8.8 | 1.7 | 8.5 | 1.8 | 1.37 (.172) |
| Overcommitment | 13.6 | 2.9 | 12.6 | 3.0 | 2.19 (.030) |
| Reward | 21.1 | 3.1 | 22.5 | 3.0 | 3.22 (.001) |
| Esteem | 5.8 | 1.2 | 6.3 | 1.1 | 3.44 (.001) |
| Promotion | 8.8 | 1.4 | 9.4 | 1.5 | 2.48 (.014) |
| Security | 6.5 | 1.1 | 6.8 | 1.1 | 1.85 (.065) |
Otders: American Indian, Alaska Native, Native Hawaiian, Pacific Islander, and Otder
Otder: work botd 24 hour & 48 hour shifts (varies), 72 hours off & 48 hours on, 72 hours on, 96 hours on
Discussion
This study explored characteristics of career firefighters’ reported occupational injuries (i.e. injury location, activity being performed, cause of injury, body part injured, treatment sought, and return-to-work outcome). In addition, this study also examined the association between occupational injuries and demographics, work-related characteristics, and occupational stress.
Work-related Injury
Within the past 12 months, 26.9% of career firefighter participants experienced a work-related illness or injury. Among all career firefighter participants, 22.1% reported one injury, 3.2% reported two, and 1.2% reported three or more injuries. These findings are similar to those reported by Jahnke et al. (2013) who also measured work-related injuries among career firefighters within the past 12 months (20.1% reported one injury, 3.0% reported two, 1.7% reported three or more). It is worth noting that our study included more firefighter paramedic participants, whereas Jahnke et al. (2013) included more participants who solely identified as firefighters (categorical response options were similar for both studies). Approximately 46% of career firefighters who reported an injury were prohibited from working due to their injuries, and 17.5% were placed on modified duty. These findings are considerably higher than those reported by the 2015 NFPA U.S. firefighter injuries report (Haynes & Molis, 2015a), which estimated that 16.9% of all firefighter injuries resulted in lost work time. However, according to the National Fire Incident Reporting System (NFIRS), 42% of firefighters reported lost work time due to fire-related injuries in 2010–2012 (Federal Emergency Management Agency, 2014). These differences in lost work time may be due to the fact that NFPA and NFIRS data are estimates of injury rates. Firefighters may underreport their injuries. For instance, although 15.6% of firefighter participants reported using personal sick leave, vacation, or trading time/shifts within the past 12 months due to a work-related injury, these injuries may have not been captured by NFPA or NFIRS, thereby resulting in artificially low injury responses and lower lost time rates.
Firefighting is a dangerous profession. Compared to private-sector employees, firefighters are almost four times more likely to experience a work-related injury and musculoskeletal disorder (MSD; Seabury & McLaren, 2010b). In this study, the most common location of injury occurrence was on the scene of a non-fire call (31.3%), followed by fire/rescue activities on the fireground (26.3%). This finding is consistent with the literature which reports a 58.5% decrease in the number of fires since 1980 (National Fire Protection Association, 2014). The NFPA reported that 43% of all firefighter injuries occurred on the fireground in 2014 and only 23% occurred during non-fire emergencies. This finding may be due to the fact that the NFPA reports include both volunteer and career firefighters. Volunteer firefighters are more likely to be injured on the scene of a fire because volunteer fire departments are typically smaller and generally do not provide emergency medical services, so non-fire emergencies comprise less of their call volume. Contrary to this study’s findings and the NFPA literature, Jahnke et al. (2013) reported injuries among their study’s career firefighter cohort primarily occurred during training (33.3%), followed by fire scene or during rescue operations combined (27.9%), and only 17.1% of the injuries occurred at the scene of non-fire calls. The reason for this discrepancy is unknown.
In regard to activity being performed when injured, lifting/pushing/pulling on the scene of a non-fire call were most common (22.5%). On the fireground, firefighters were more likely to be injured by advancing/directing a hose than other activities, which is consistent with other study findings (Jahnke et al., 2013). In this study, the primary cause and type of injury was overexertion/strain and sprain/strain/muscular pain, which is well supported in the literature (Frost, Beach, Crosby, & McGill, 2015; Karter, 2011; Poplin et al., 2011; Reichard & Jackson, 2010; Szubert & Sobala, 2002; Walton et al., 2003). The most common body part injured was the back, which concurs with Frost et al. (2015) findings, where 32% of reported firefighter injuries affected the back.
Factors Related to Work-related Injuries
Increasing firefighter age was associated with a greater likelihood of work-related injury within the past 12 months (p = .031). Seabury and McLaren (2010a) found the frequency and severity of work-related injuries, particularly musculoskeletal injuries, to be worse among older firefighters. This study did not measure severity; however, older firefighters were more likely to report a work-related injury. Contrary to earlier findings, Liao et al. (2001) and Jahnke et al. (2013) reported age was not significantly related to injury frequency among career firefighters. Years worked in the fire service/tenure were not associated with injury in this study, which was contrary to the findings of other studies (Jahnke et al., 2013; Liao et al., 2001). Nevertheless, studies from Moore-Merrell et al. (2008), and Szubert and Sobala (2002) both reported that career firefighters with fewer years of service/tenure were at increased risk for injury. Meanwhile, Hong et al. (2012) reported career firefighters with more than 17 years of fire service were more likely to report an injury. None of the following variables were significantly related to work-related injury in this study: gender, race/ethnicity, primary role/rank, or type of shift. These results are similar to those findings in another study (Jahnke et al., 2013). Conversely, Hong et al. (2012) reported that career Hispanic/Latino firefighters were 34% less likely to report an occupational injury (p < .01) compared to their White co-workers. This contrary finding may be due to different methods used to measure work-related injury. Hong et al. (2012) assessed injury by asking, “While working as a firefighter, have you experienced any work-related accidents or injuries?” whereas, this study inquired only about work-related injuries within the past 12 months.
Finally, firefighters who reported work-related injuries were more likely to report elevated levels of occupational stress (p = .003) and overcommitment (p = .030) on the ERI-S that was used to measure occupational stress. Overcommitment includes feeling overwhelmed by work, sacrificing too much for the job, and being unable to relax and “switch off” work. Siegrist (2001) defined overcommitment as a “set of attitudes, behaviors and emotions that reflect excessive striving in combination with a strong desire of being approved and esteemed.” A high level of overcommitment has been shown to increase an individual’s risk for injury (Lee, You, Gillen, & Blanc, 2015). In addition, firefighter participants who reported injuries also reported lower levels of esteem (p = .001) in the form of respect and support from superiors and colleagues, fewer job rewards such as salary/income (p = .001), and fewer promotional prospects (p = .014) compared to those who reported no work-related injury. Along the same premise, Hong et al. (2012) found that firefighters who felt that their fire service organization was committed to improving their health and well being were 54% less likely to report a work-related injury (p < .01).
Limitations
Limitations to the current study include the use of convenience sampling, which introduces selection bias. Self-reported work-related injury were not validated by record review so the rates reported in this study may be either over- or underestimated compared to actual rates. However, in regard to self-reported injury validity, Gabbe, Finch, Bennell, and Wajswelner (2003) found that almost 80% of their participants accurately recalled the number of sports injuries and body regions injured. This study sample only included career firefighters from six fire departments in two states, and each fire department used different terminology for their primary role/rank; therefore, the primary role results should be interpreted with caution and findings cannot be generalized to volunteer firefighters. Female firefighters only comprised 7.2% of the study sample; firefighters from racial/ethnic groups other than White, non-Hispanic constituted less than 30% of the sample. These results were expected because the fire service is a predominately white male-dominated profession. Finally, other possible injury predictors such as fire station call volume, rural/urban environment, safety climate at the department, organizational commitment, and personnel factors (e.g., obesity, physical fitness level, smoking and alcohol status, and depression screening) were not considered in this study.
Despite the above limitations, this study has the following strengths. First, six fire departments from two geographically different states (California and Texas) participated in the study, increasing generalizability. Second, the use of technology via the internet-based survey enabled firefighters to complete the survey at their convenience either on their smartphone or computer. Lastly, study staff collaborated with a multi-disciplinary team which included: fire departments, union leaders, occupational health professionals, occupational health clinics, and academic researchers.
Implications for Practice
Awareness of current risk factors for occupational injuries among firefighters provides occupational health professionals with valuable information that they can apply to their employer’s injury and illness prevention program (IIPP). According to the Occupational Safety and Health Administration (OSHA, n.d.), the first step to reduce occupational injuries is to collect and evaluate existing information about workplace hazards. This step includes reviewing past injury and illness records, such as the OSHA 300 and 301 logs, incident investigation reports, and workers’ compensation records. This study revealed that injuries occurred most commonly at the scene of non-fire calls while performing activities that required lifting, pushing, and pulling. Injuries that occurred on the scene of a fire frequently involved advancing or directing hoses. The primary cause and type of injury was overexertion/strain and sprain/strain/muscular pain, with the back being the most common body part injured. Armed with this information, the OSHA IIPP recommends a workplace walk-through inspection for hazards (OSHA, n.d.). Occupational health professionals should encourage workers to participate in the inspection team and have an open dialogue about workplace hazards they observe. For instance, among firefighters, team members should inquire about specific lifting, pushing, and pulling activities that could result in back injuries. Are injuries due to ineffective body mechanics, equipment malfunctions, combative patients, or building design and layout? Hazard assessment checklists, such as the California Department of Industrial Relations (n.d.) checklist, located at http://www.dir.ca.gov/dosh/etools/09-031/hazassesscheck.pdf may also assist the occupational health professional identify and evaluate workplace hazards. Once the IIPP for hazards is developed, the occupational health professional should continue to review program outcomes, revise the program based on feedback and in response to accidents and near misses, and continue to educate firefighters on safety measures and new practices. Through introduction to educational content, firefighters may change their workplace practices, thereby reducing their risk for injuries. For instance, Mayer et al. (2015) assessed the impact of an on duty back and core muscular endurance exercise program in firefighters; after 24 weeks, the exercise group exhibited 12% greater back muscle endurance (p = .02) and 21% greater core muscle endurance (p < .001). The cost savings in terms of reduction in days lost to injury can be significant. Kim, Hayden, and Mior (2004) developed a cost-effective back education program for firefighters that reduced lost work days by 72.4% over a two-year period.
In this study, firefighters who reported a work-related injury were more likely to report elevated levels of occupational stress (p = .003) and overcommitment (p = .030). Implementing a stress prevention program in which firefighters and their leadership are aware of the early warning signs of occupational stress (e.g., headache, sleep disturbances, difficulty concentrating, short temper, upset stomach, job dissatisfaction, and low morale; National Institute for Occupational Safety and Health [NIOSH], 1999) may reduce occupational injuries. In addition, firefighters who reported occupational injuries also reported lower levels of respect and support from superiors and colleagues (p = .001), fewer job rewards such as salary/income (p = .001), and fewer promotional prospects (p = .014) compared to those who reported no work-related injury.These findings highlight the importance of creating a healthy organization that recognizes employees for their job performance, provides career development opportunities, promotes a culture that values individual workers, and management actions consistent with organization values (NIOSH, 1999). Healthy organizations strive to advance worker well-being through total worker health policies, programs, and practices (NIOSH, 2015). Total worker health interventions that target both injuries and chronic disease can improve workforce health (Anger et al., 2015). Numerous fire departments have Employee Assistance Programs (EAP), which assist firefighters in coping with personal issues, such as occupational stress, that may negatively impact their job performance, health, and well-being. In addition, some fire departments have an on-call “Crisis Counselor” who serves as a sounding board for firefighters and provides firefighters with resources, such as referrals to mental health care providers who commonly care for first responders. The International Association of Fire Fighters (2008) offers an online behavioral wellness manual that can also be found in the 3rd Edition of the Fire Service Joint Labor Management Wellness-Fitness Initiative. Lastly, fire departments should also examine their organizational culture and cultivate a work environment where firefighters of every rank feel respected and receive recognition for their work so they do not feel forgotten, unappreciated, or disrespected. To assess employees’ work organization issues, NIOSH (2010) has published a “Quality of Worklife Questionnaire” that is available at https://www.cdc.gov/niosh/topics/stress/pdfs/qwl2010.pdf.
Conclusion
Findings from this study indicate that age, occupational stress, overcommitment, job rewards (salary), esteem (respect and support from superiors and colleagues), and promotional prospects have a significant effect on work-related injuries among U.S. career firefighters. Firefighters in this study who were older, reported higher levels of occupational stress, overcommitment, fewer rewards (money/salary), lower levels of esteem (respect and support), and fewer promotional prospects were significantly more likely to have experienced a work-related injury within the past 12 months compared to their co-workers who did not report a work-related injury. These results emphasize the importance of understanding demographic and work-related characteristics to develop and implement an effective workplace health and safety program aimed at reducing work-related injuries among firefighters.
Contributor Information
S. Phelps, School of Nursing, University of California, San Francisco Occupational and Environmental Health program, and is working on firefighter health and safety research..
D. Drew-Nord, Occupational and Environmental Health Nursing Graduate Program, School of Nursing, University of California, San Francisco..
R. Neitzel, Environmental Health Sciences, School of Public Health, University of Michigan..
M. Wallhagen, Department of Physiological Nursing, School of Nursing, University of California, San Francisco..
B. Michael, Department of Epidemiology, School of Public Health, University of California, Berkley and director of the Targeted Research Training program..
H. OiSaeng, Occupational and Environmental Health Nursing Graduate Program, School of Nursing, University of California, San Francisco..
References
- Anger WK, Elliot DL, Bodner T, Olson R, Rohlman DS, Truxillo DM, … Montgomery D (2015). Effectiveness of total worker health interventions. Journal of Occupational Health Psychology, 20(2), 226–247. doi: 10.1037/a0038340 [DOI] [PubMed] [Google Scholar]
- California Department of Industrial Relations. (n.d.). Hazard Assessment Checklist. from http://www.dir.ca.gov/dosh/etools/09-031/hazassesscheck.pdf
- Dolan J (2015). L.A. audits: Costly police, firefighter workers’ comp claims avoidable. Los Angeles Times. Retrieved from http://www.latimes.com/local/cityhall/la-me-injured-on-duty-20150327-story.html [Google Scholar]
- Fahy RF, LeBlanc PR, & Molis JL (2016). Firefighter Fatalities in the United States - 2015.
- Federal Emergency Management Agency. (2014). Fire-Related Firefighter Injuries Reported to the National Fire Incident Reporting System (2010–2012).; <j>Frost DM, Beach TA, Crosby I, & McGill SM (2015). Firefighter injuries are not just a fireground problem. Work, 52(4), 835–842. doi: 10.3233/WOR-152111 [DOI] [PubMed] [Google Scholar]
- Gabbe BJ, Finch CF, Bennell KL, & Wajswelner H (2003). How valid is a self reported 12 month sports injury history? British Journal of Sports Medicine, 37(6), 545–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynes HJG, & Molis JL (2015a). Firefighter Injuries in the United States: National Fire Protection Association. [Google Scholar]
- Haynes HJG, & Molis JL (2015b). U.S. Firefighter Injuries - 2014: National Fire Protection Association. [Google Scholar]
- Hong O, Chin DL, Phelps S, Feld J, & Vogel S (2012). Occupational injuries, duty status, and factors associated with injuries among firefighters. Workplace Health & Safety, 60(12), 517–523. doi: 10.3928/21650799-20121116-08 [DOI] [PubMed] [Google Scholar]
- Hylton JG, & Molis JL (2015). Firefighter Injuries in the United States - 2014: National Fire Protection Association [NFPA]. [Google Scholar]
- Hylton JG, & Molis JL (2016). Firefighter injuries in the United States: National Fire Protection Association. [Google Scholar]
- Hylton JG, & Stein GP (2017). U.S. Fire Department Profile - 2015: National Fire Protection Association. [Google Scholar]
- International Association of Fire Fighters. (2008). IAFF Wellness Fitness Initiative Resource: Behavioral Health. from https://www.iaff.org/HS/wfiresource/BehavioralHealth/behavioralhealth.html
- Jahnke SA, Poston WS, Haddock CK, & Jitnarin N (2013). Injury among a population based sample of career firefighters in the central USA. Injury Prevention, 19, 393–398. [DOI] [PubMed] [Google Scholar]
- Karter MJ, & Molis JL,. (2011). U.S. Firefighter Injuries-2010 (pp. 3): National Fire Protection Association Fire Analysis and Research Division. [Google Scholar]
- Kim P, Hayden JA, & Mior SA (2004). The cost-effectiveness of a back education program for firefighters: a case study. J Can Chiropr Assoc, 48(1), 13–19. [PMC free article] [PubMed] [Google Scholar]
- Lee SJ, You D, Gillen M, & Blanc PD (2015). Psychosocial work factors in new or recurrent injuries among hospital workers: a prospective study. International Archives of Occupational and Environmental Health, 88(8), 1141–1148. doi: 10.1007/s00420-015-1038-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leineweber C, Wege N, Westerlund H, Theorell T, Wahrendorf M, & Siegrist J (2010). How valid is a short measure of effort-reward imbalance at work? A replication study from Sweden. Occupational and Environmental Medicine, 67(8), 526–531. doi: 10.1136/oem.2009.050930 [DOI] [PubMed] [Google Scholar]
- Liao H, Arvey RD, Butler RJ, & Nutting SM (2001). Correlates of work injury frequency and duration among firefighters. Journal of Occupational Health Psychology, 6(3), 229–242. [PubMed] [Google Scholar]
- Mayer JM, Quillen WS, Verna JL, Chen R, Lunseth P, & Dagenais S (2015). Impact of a supervised worksite exercise program on back and core muscular endurance in firefighters. American Journal of Health Promotion, 29(3), 165–172. doi: 10.4278/ajhp.130228-QUAN-89 [DOI] [PubMed] [Google Scholar]
- Moore-Merrell L, Zhou A, McDonald-Valentine S, Goldstein R, & Slocum C (2008). Contributing Factors to Firefighter Line-of-duty Injury in Metropolitan Fire Departments in the United States: International Association of Firefighters. [Google Scholar]
- National Fire Protection Association [NFPA]. (2014). Number of Fires by Type of Fire: National Fire Protection Association.
- National Institute for Occupational Safety and Health [NIOSH]. (1999). Stress at Work. DHHS (NIOSH) Publication No. 99–101. from https://www.cdc.gov/niosh/docs/99-101/pdfs/99-101.pdf
- National Institute for Occupational Safety and Health [NIOSH]. (2010). Quality of Worklife Module from https://www.cdc.gov/niosh/topics/stress/pdfs/qwl2010.pdf National Institute for Occupational Safety and Health [NIOSH]. (2013). National Public Safety Agenda. [Google Scholar]
- National Institute for Occupational Safety and Health [NIOSH]. (2015). Total Worker Health. from https://www.cdc.gov/niosh/twh/totalhealth.html
- National Institute of Standards and Technology [NIST]. (2005). The Economic Consequences of Firefighter Injuries and Their Prevention. Final report (NIST GCR 05–874): U.S. Department of Commerce and National Institute of Standards and Technology. [Google Scholar]
- Occupational Safetyand Health Administration [OSHA]. (2001). 1904.5 (a) Recording and Reporting Occupational Injuries and Illness. from https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=9636
- Occupational Safety and Health Administration [OSHA]. (n.d.). Recommended Practices for Safety and Health Programs. from https://www.osha.gov/shpguidelines/hazard-Identification.html
- Poplin GS, Harris RB, Pollack KM, Peate WF, & Burgess JL (2011). Beyond the fireground: injuries in the fire service. Injury prevention : journal of the International Society for Child and Adolescent Injury Prevention. doi: 10.1136/injuryprev-2011-040149 [DOI] [PubMed] [Google Scholar]
- Reichard AA, & Jackson LL (2010). Occupational injuries among emergency responders. American Journal of Industrial Medicine, 53(1), 1–11. doi: 10.1002/ajim.20772 [DOI] [PubMed] [Google Scholar]
- Seabury SA, & McLaren CF (2010a). The frequency, severirt, and economic consequences of musculoskeletal injuries to firefighters in California: RAND Center for Health and Safety in the Workplace. [PMC free article] [PubMed] [Google Scholar]
- Seabury SA, & McLaren CF (2010b). The frequency, severity, and economic consequences of musculoskeletal injuries to firefighters in California Santa Monica, CA: RAND Center for Health and Safety in the Workplace. [PMC free article] [PubMed] [Google Scholar]
- Siegrist J (1996). Adverse health effects of high-effort/low-reward conditions. Journal of Occupational Health Psychology, 1(1), 27–41. [DOI] [PubMed] [Google Scholar]
- Siegrist J (2001). A theory of occupational stress In Dunham J (Ed.), Stress in the workplace: Past, present and future. (pp. pp. 52–66). Philadelphia, PA: Whurr Publishers. [Google Scholar]
- Siegrist J (2012). Effort-reward imbalance at work - theory, measurement and evidence. from http://www.uniklinik-duesseldorf.de/fileadmin/...fuer.../ERI-Website.pdf
- Siegrist J, Wege N, Puhlhofer F, & Wahrendorf M (2009). A short generic measure of work stress in the era of globalization: effort-reward imbalance. Int Arch Occup Environ Health, 82(8), 1005–1013. doi: 10.1007/s00420-008-0384-3 [DOI] [PubMed] [Google Scholar]
- Szubert Z, & Sobala W (2002). Work-related injuries among firefighters: sites and circumstances of their occurrence. International Journal of Occupational Medicine and Environmental Health, 15(1), 49–55. [PubMed] [Google Scholar]
- Walton SM, Conrad KM, Furner SE, & Samo DG (2003). Cause, type, and workers’ compensation costs of injury to fire fighters. American Journal of Industrial Medicine, 43(4), 454–458. doi: 10.1002/ajim.10200 [DOI] [PubMed] [Google Scholar]


