Abstract
Background
Patients with advanced cancer have high rates of psychological distress, including depression, anxiety and spiritual despair. We examined the effectiveness of Individual Meaning Centered Psychotherapy (IMCP) compared to supportive psychotherapy (SP) and enhanced usual care (EUC) in improving spiritual well-being and quality-of-life and reducing psychological distress in patients with advanced cancer.
Methods
321 Patients were randomly assigned to IMCP (N=109), SP (N=108), or EUC (N=104). Assessments were conducted at 4 time points: pre-intervention, mid-treatment (4 weeks), post-treatment (8 weeks), and post-treatment (16 weeks).
Results
Significant treatment effects (small to medium in magnitude) were observed for IMCP, compared to EUC, for five of seven outcome variables (quality-of-life, sense of meaning, spiritual well-being, anxiety and desire for hastened death), with Cohen’s d ranging from .1 to .34; no significant improvement was observed for patients receiving supportive therapy (SP) (d < .15, p > .05 for all variables). The effect of IMCP was significantly greater than SP for quality-of-life and sense of meaning (d=.19), but not for the remaining study variables.
Conclusions
This study provides further support for the efficacy of IMCP as a treatment for psychological and existential/spiritual distress in patients with advanced cancer. Significant treatment effects (small to moderate effect sizes) were observed when compared to usual care, and somewhat more modest differences in improvement (small effect sizes) were observed when compared to supportive psychotherapy. Thus, the benefits of MCP appear to be unique to the intervention, and highlight the importance of addressing existential issues with patients approaching the end of life.
Keywords: Psychotherapy, spiritual well-being, Meaning Centered Psychotherapy, distress, depression
The past decade has witnessed growing interest in the development of psychotherapeutic interventions that incorporate aspects of spirituality, and in particular, a sense of meaning. This approach is particularly appealing to patients with advanced cancer, where concerns about death and dying may engender spiritual and existential distress. 1–3 A number of interventions focused on spiritual well-being were developed in the 1980’s and 1990’s, but these studies have rarely targeted patients with advanced or terminal illness.4–6 More recently, interest in spiritual well-being has prompted a new wave of interventions that directly target this population. For example, Managing Cancer and Living Meaningfully (CALM) is a 3 to 8 session intervention grounded in “relational, attachment and existential theory” (p. 236).7 A pilot study of CALM provided some support for this intervention, but only 24 of 50 patients completed the treatment and only 16 patients completed a follow-up assessment. Thus, while further research may demonstrate the effectiveness of this intervention, there is currently little evidence to support its utility. Similarly, Chochinov and colleagues developed Dignity Therapy, which helps end-stage cancer patients create a “Legacy” document for their loved ones.8 Their randomized clinical trial of Dignity Therapy demonstrated little evidence of significant improvement between pre- and post-intervention levels of distress, spiritual well-being or quality-of-life.9 Ando and colleagues also utilized a short-term life review intervention to enhance spiritual well-being in terminally ill cancer patients.10 Their study of 68 palliative care patients demonstrated significantly greater improvement (compared to patients assigned to a control group) on a measure of spiritual well-being, as well as several items drawn from a measure of psychological distress. Despite these advances, none of these interventions have demonstrated strong treatment effects in large, systematic clinical trials.
In response to the need for an intervention with demonstrated effectiveness in alleviating the existential distress (i.e., spiritual despair, loss of meaning) that often arises in patients with advanced disease, we developed Meaning-Centered Psychotherapy (MCP). This intervention differs from other end-of-life interventions by focusing squarely on identifying sources of meaning in the patient’s life, whereas other interventions focus on meaning indirectly, such as by reviewing the patient’s personal history (e.g., legacy). This intervention is based on the underlying belief that existential distress is grounded in the belief that one’s life is meaningless11; MCP addresses existential distress by helping patients sustain or enhance their sense of meaning through re-experiencing and recreating meaning through utilizing the sources of meaning described by Frankl’s seminal book, Man’s Search for Meaning.12 Originally designed as a group-based intervention, two randomized controlled trials (RCTs) demonstrated significantly greater improvement for MCP in a range of outcomes when compared to a supportive group psychotherapy.13–14 Since that time, researchers around the globe have adopted MCP, with pilot studies and culturally-sensitive adaptations arising in multiple countries and settings.15–19 However, a group-based intervention can be problematic when applied to patients with advanced disease (e.g., worsening illness and medical appointments often interfere with scheduled group sessions), highlighting the need for an individualized approach.
We developed and tested an individualized version of Meaning-Centered Psychotherapy (IMCP), which showed strong, albeit preliminary results in a small pilot study. 20 Significant improvements were observed for most outcome variables when compared to patients receiving an attention-control condition (therapeutic massage). However, this control condition prevented an analysis of whether IMCP provides unique benefits compared to other psychotherapeutic approaches commonly used in the medical settings, such as supportive psychotherapy. Indeed, multiple studies have demonstrated improvement in patient outcomes following supportive psychotherapy, and this intervention is widely used in oncology settings.21 The current study provides a rigorous test of IMCP in a large sample of patients with advanced cancer. We hypothesized that IMCP would result in significantly greater improvement in our primary outcomes: spiritual well-being, sense of meaning and quality-of-life, when compared to supportive psychotherapy (SP) and enhanced usual care (EUC).
Method
Participants
Patients with advanced cancer were recruited from outpatient clinics at Memorial Sloan Kettering Cancer Center (MSK) between March of 2011 and March of 2016. Power calculations indicated that a sample size of 104 participants per treatment arm (N=312) was required to generate power of .80 for detecting a time x treatment interaction effect of d=.20. Prospective participants were identified through flyers posted in the ambulatory care clinics, solicitation by research assistants, and referrals from treating physicians. Eligibility requirements were: age 18 years old, English speaking, stage IV solid tumor cancer, and at least moderate distress (a Distress Thermometer22 score of 4 or greater). Patients with significant cognitive impairment or severe psychiatric disturbance (e.g., psychosis, suicidal ideation) based on clinician assessment were excluded. All participants provided written informed consent. The study was approved by the Institutional Review Boards of MSK and Fordham University.
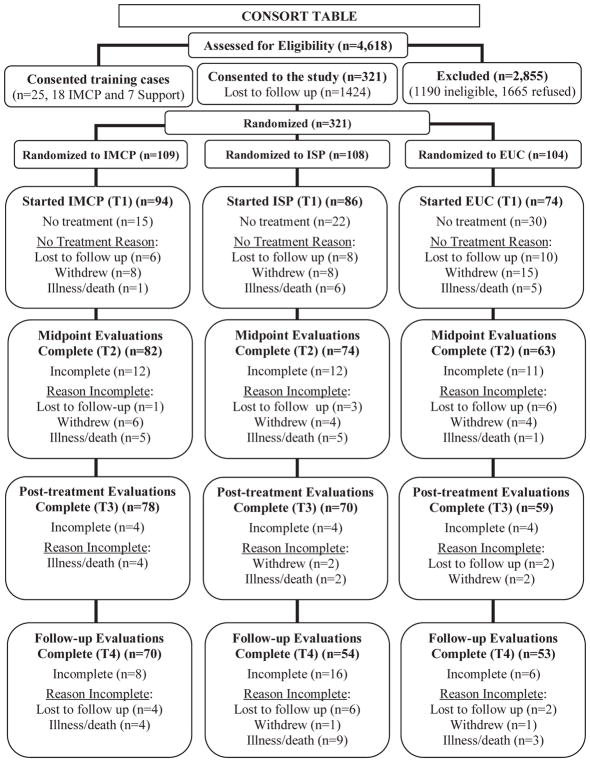
A total of 4618 patients were assessed for eligibility, and 346 were deemed eligible and provided informed consent (see Figure 1). Of these 346 participants, 25 were used as “training cases” to train staff in the provision of IMCP or supportive psychotherapy (SP). The remaining 321 individuals were randomized to one of the three treatment arms (IMCP: n=109, SP: n=108, EUC: n=104). Randomization was stratified based on pretreatment level of distress (Distress Thermometer score of 4–6 versus 7–10) and physical functioning (Karnofsky Performance Rating Scale23 of 60–79 versus 80–100). Because the study was a psychotherapy intervention, neither patients nor therapists were blind to treatment arm. The final sample, described in Table 1, included 230 women (71.7%), ranging in age from 25 to 85 (M=58.0, SD=11.0). The sample was predominantly white/non-Hispanic (n=242, 75.7%), and the most common cancer diagnoses were lung (n=55, 17.4%), pancreatic (n=54, 16.8%), and ovarian (n=48, 15.0%). There were no significant differences between the three treatment arms on any demographic or medical variables.
Figure 1.
CONSORT Diagram
Table 1.
Sample characteristics
| MCP (n=109) | SP (n=108) | EUC (n=104) | F / χ2 | p | |
|---|---|---|---|---|---|
|
| |||||
| Gender | |||||
| Male | 28 (25.7%) | 37 (34.3%) | 26 (25.0%) | χ2 = 2.81 | p = .25 |
| Female | 81 (74.3%) | 71 (65.7%) | 78 (75.0%) | d.f.=2 | |
|
| |||||
| Age (Mean/SD) | 58.1 (10.2) | 58.8 (12.0) | 57.1 (10.9) | F = 0.56 | p = .57 |
|
| |||||
| Years of Education (Mean/SD) | 16.7 (2.7) | 16.4 (2.5) | 16.5 (2.5) | F = 0.51 | p = .60 |
|
| |||||
| Race/Ethnicity | |||||
| Caucasian/Non-Hispanic | 83 (76.1%) | 82 (75.9%) | 78 (75.0%) | χ2 = 6.39 | p = .38 |
| African-American | 14 (12.8%) | 10 (9.3%) | 7 (6.7%) | d.f.=6 | |
| Hispanic | 8 (7.3%) | 8 (7.4%) | 14 (13.5%) | ||
| Other | 4 (3.7%) | 8 (7.4%) | 5 (4.8%) | ||
|
| |||||
| Religion | |||||
| Catholic | 32 (29.6%) | 36 (33.3%) | 35 (33.7%) | χ2 = 2.96 | p = .94 |
| Other Christian | 22(20.4%) | 23 (21.3%) | 18 (17.3%) | d.f.=8 | |
| Jewish | 28 (25.9%) | 28 (25.9%) | 26 (25.0%) | ||
| Other | 9 (8.3%) | 6 (5.6%) | 5 (4.8%) | ||
| None | 17 (15.7%) | 15 (13.9%) | 20 (19.2%) | ||
|
| |||||
| Primary Cancer Diagnosis | |||||
| Breast | 13 (14.1%) | 9 (10.3%) | 12 (16.2%) | χ2=10.83 | p = .37 |
| Colon/Rectal | 14 (15.2%) | 8 (9.2%) | 11 (14.9%) | d.f.=10 | |
| Lung | 11 (12.0%) | 21 (24.1%) | 11 (14.9%) | ||
| Ovarian | 17 (18.5%) | 10 (11.5%) | 11 (14.9%) | ||
| Pancreas | 18 (19.6%) | 18 (20.7%) | 9 (12.2%) | ||
| Other | 19 (20.7%) | 21 (24.1%) | 10 (27.0%) | ||
|
| |||||
| Karnofsky Performance score (Mean/SD) | 80.9 (8.2) | 80.5 (8.5) | 80.3 (7.9) | F = 0.17 | p = .85 |
|
| |||||
| Distress Thermometer (Mean/SD) | 6.3 (1.7) | 6.2 (1.8) | 6.2 (1.8) | F = 0.24 | p = .79 |
Of the 217 individuals randomized to one of the two active intervention arms (IMCP and SP), 44 participants (20.3%) never attended treatment and 28 (12.9%) attended less than seven sessions; 145 patients (66.8%) attended all seven sessions (see Figure 1). There was no significant difference between IMCP and SP in average number of sessions attended (5.3 versus 4.9; t=0.97, p=.33) or the proportion that completed all seven sessions (70.6% v. 63.0%, chi-square=1.23, p=.27). Of the 321 participants, 220 completed the mid-treatment assessment (IMCP=82, SP=73, EUC=65), 208 completed the post-treatment assessment (IMCP=78, SP=69, EUC=61), and 175 completed the follow-up assessment (IMCP=68, SP=54, EUC=53).
Procedures
Participants were administered a battery of questionnaires prior to the first session. There were three primary outcome variables used to measure existential distress and overall quality-of-life: FACIT Spiritual Well-Being Scale (SWB),24 the Personal Meaning Index of the Life Attitude Profile-Revised (LAP-R),25 and the McGill Quality of Life Questionnaire (MQOL).26 Secondary outcome variables, measuring psychological distress more generally, were the Hopelessness Assessment in Illness questionnaire (HAI),27 the Schedule of Attitudes toward Hastened Death (SAHD),28 and the Hospital Anxiety and Depression Scale Anxiety (HADS-A) and Depression HADS-D) scales.29 Participants also completed a pre-treatment questionnaire (prior to randomization) eliciting preferences for psychotherapy content and awareness of their prognosis. Outcome variables were re-administered, along with a measure of therapeutic alliance (the Working Alliance Inventory-Short Form, WAI-SF30) for patients randomized to MCP or SP, prior to the fourth treatment session (one month after randomization, for EUC condition). Outcome measures were re-administered, along with a post-treatment questionnaire eliciting perceptions of the treatment, after the 7-session intervention (or two months after randomization, for those assigned to EUC), and again two months after completing the study intervention (four months after randomization to EUC). This study was approved by the Institutional Review Boards of MSK and Fordham University, and was registered with clinicaltrials.gov (number NCT01323309).
Study interventions
Meaning Centered Psychotherapy, a manualized psychotherapy grounded in the work of Viktor Frankl,12,31 was originally developed as an 8-session group intervention and subsequently adapted to an individualized format.13,33 The intervention has focuses on helping patients with advanced cancer develop or increase a sense of meaning in their lives, and has demonstrated effectiveness in a pilot study contrasting IMCP.14 We utilized two control conditions, supportive psychotherapy (SP) and enhanced usual care (EUC). Supportive therapy sessions also followed an established treatment manual,34 and focused on coping with advanced cancer by encouraging patients to share concerns related to their diagnosis and treatment, describe their experiences and emotions, and identify challenges. Both “active” treatments (IMCP and SP) were by a mental health clinician (psychiatrist, clinical psychologist, social worker or doctoral student in clinical psychology) with experience treating advanced cancer patients. Study therapists were trained using both didactic and observational methods, and completed a minimum of two supervised training cases prior to being assigned study cases. We weekly supervision was provided by experienced clinical psychologists or psychiatrists, and all sessions were audio-recorded to assess treatment adherence. In order to prevent “bleed” across conditions, therapists conducted sessions in only one intervention. Although the two treatment arms were designed as weekly sessions, participants were given up to 14 weeks to complete the intervention (e.g., if medical treatment needs impacted their availability).
Patients assigned to EUC were provided with a list of resources for mental health treatment, as well as targeted referrals specific to problem areas identified on the Distress Thermometer (e.g., social work, chaplaincy, pain management). In addition, EUC patients were provided with a packet of resources for coping with cancer, along with a signed copy of The Human Side of Cancer,35 a book designed to help patients cope with stressors associated with cancer and its treatment.
Adherence to Treatment Format
A random sample of sessions (n=108) were reviewed by a research assistant (blind to treatment arm) to monitor treatment adherence. Ratings indicated close adherence to the treatment manual, with mean ratings for IMCP content of 0.96 (on a scale of 0–1) for IMCP sessions versus 0.02 for SP sessions. Conversely, mean ratings for SP content was 0.08 (on a scale of 0–1) for IMCP sessions versus 0.97 for SP sessions. Mean ratings of therapist IMCP “process” behaviors was 1.71 (on a scale of 0–2) for IMCP sessions versus 0.04 for SP sessions, and 0.30 for therapist SP “process” behaviors within IMCP sessions versus 1.81 for SP sessions (all p’s < .001). There was no significant difference in patient ratings of the therapeutic alliance, as measured by the WAI-SF, between IMCP (M=69.9, SD=12.6) and SP (M=67.2, SD=11.4), t=1.40, p=.16.
Statistical Analysis
Treatment effects were analyzed with a series of mixed models. In each model, treatment arm and assessment time point were entered as fixed effects and subject as a random effect. The time by treatment interaction served as the omnibus test of whether improvement differed for the three study groups, with independent contrasts comparing each intervention (IMCP and SP) against EUC, and planned comparisons contrasting the two active treatments against one another and a combined active treatment condition (including both IMCP and SP) against EUC. We analyzed these data twice, first including all participants that began treatment (i.e., an intent-to-treat analysis) and a second time including only participants who attended three or more sessions. To control for inflated type I error due to multiple outcome variables, we adjusted critical alpha values (based on two-tailed tests) using the False Discovery Method.36
Results
Group Differences in Demographic Characteristics, Attendance and Attrition
Preliminary analyses sought to identify any group differences that might necessitate consideration as potential covariates. There were no group differences observed on any of the demographic variables. Although attrition prior to treatment differed significantly across the three conditions (IMCP: 14.7%, SP: 20.4%. EUC: 28.8%), chi-square=6.46, df=2, p=.04, phi=.14, the magnitude of this difference was modest, and largely due to greater attrition in the EUC arm. As noted above, there was no difference in attrition rates when the MCP and SP arms were compared to one another, nor any difference in the mean number of sessions attended by IMCP and SP participants.
Efficacy of Individual Meaning Centered PsychotherapyIntent-to-treat analyses
Analyses that included all participants who began the study (i.e., provided data at the baseline assessment; N=321) generated a significant group x treatment interaction effect for each of the three primary outcome variables: SWB, F(2,589)=3.92, p=.02, LAP-R, F(2,598)=9.37, p<.0001, and MQOL, F(2,596)=4.53, p=.01. The impact of treatment on the secondary outcome variables (HAI, SAHD, HADS-A, HADS-D) was not significant, but approached significance for the HADS-A, F(2,596)=2.87, p=.06. In addition, a significant main effect was observed for time (indicating improvement across the entire sample) for four dependent variables: SWB, HAI, HADS-A and HADS-D. Analysis of the individual treatment arms (see Tables 2 and 3) revealed significantly greater improvement for IMCP patients compared to EUC on each of the three primary outcome variables (SWB, LAP-R, and MQOL), as well as for two of the four secondary outcomes (SAHD, and HADS-A); and a third (HADS-D) approached significance (p=.07). Many of these effects remained significant even after controlling for type I error using the False Discovery Method (see Table 2). There was no significant effect for SP compared to EUC on any of the outcome variables. However, planned contrast analyses comparing IMCP to SP indicated significant differences in the rate of improvement for two variables LAP-R, t=3.43, p=.014, and MQOL, t=2.38, p=.018; SWB also approached significance, t=1.88, p=.06.
Table 2.
Mixed models analyzing treatment outcome (N=160)
| Main Effect | Time x Treatment Arm Effects | ||||
|---|---|---|---|---|---|
| Dependent Variable | Time B [95% CI] |
IMCP v. EUC B [95% CI] |
SP v. EUC B [95% CI] |
IMCP/SP v. EUC B [95%CI] |
IMCP v. SP B [95%CI] |
| SWB | .05 [−.00, .11] | .16 [.08, .23]* | .07 [−.01, .15] | .14 [.00, .28] | .07 [−.00, .15] |
| LAP-R | .05 [−.00, .11] | .16 [.09, .23]* | .07 [−.01, .15] | .23 [.10, .36]* | .09 [.02, .16] |
| MQOL | .04 [−.04, .12] | .14 [.04, .24]* | .02 [−.09, .13] | .16 [−.02, .34] | .12 [.02, .22] |
| HAI | −.09 [−.15, −.03]* | −.05 [−.14, .03] | −.04 [−.13, .05] | −.10 [−.25, .05] | −.01 [−.09, .07] |
| SAHD | −.02 [−.08, .04] | −.09 [−.17, −.01] | −.04 [−.12, .04] | −.13 [−.27, .02] | −.05 [−.12, .03] |
| HADS-A | −.07 [−.13, −.00] | −.10 [−.18, −.02] | −.07 [−.16, .01] | −.17 [−.32, .02] | −.02 [−.10, .06] |
| HADS-D | −.08 [−.14, −.02] | −.07 [−.16, .01] | −.07 [−.16, .02] | −.14 [−.29, .01] | −.01 [−.09, .08] |
Note: Data reflect intent-to-treat analyses; bolded/italicized coefficients represent significant effects (p < .05);
indicates significant coefficients based on False Discovery Method.
SWB: FACIT Spiritual Well-Being Scale; LAP-R: Life Attitude Profile, Revised; MQOL: McGill Quality of Life Scale; HAI: Hopelessness Assessment in Illness scale; SAHD: Schedule of Attitudes towards Hastened Death; HADS-A: Hospital Anxiety and Depression Scale, Anxiety subscale; HADS-D: Hospital Anxiety and Depression Scale, Depression subscale
Table 3.
Changes in Spiritual Well-being and Psychological Functioning Following IMCP and SP
| SWB | LAP-R | MQOL | HAI | SAHD | HADS-A | HADS-D | ||
|---|---|---|---|---|---|---|---|---|
| Time Point | na | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) |
| Individual Meaning Centered Psychotherapy (IMCP) | ||||||||
| Pre-treatment | 94 | 28.48 (10.4) | 74.74 (18.0) | 6.29 (1.5) | 4.62 (1.5) | 2.89 (3.1) | 7.83 (4.3) | 5.53 (3.8) |
| Mid-treatment | 82 | 31.26 (10.6) | 79.39 (18.4) | 6.87 (1.7) | 4.20 (3.7) | 2.45 (2.5) | 7.35 (3.8) | 4.88 (3.4) |
| Post-treatment | 78 | 34.59 (9.4) | 85.82 (16.8) | 7.33 (1.7) | 3.12 (3.3) | 1.97 (2.3) | 5.74 (4.0) | 3.92 (3.8) |
| Follow-up | 70 | 33.29 (9.3) | 83.41 (16.9) | 7.06 (1.5) | 3.47 (3.1) | 2.06 (2.0) | 6.14 (3.7) | 4.11 (3.5) |
| d (pre-post) [95% CI] |
0.86 [0.64, 1.09] |
1.03 [0.80, 1.26] |
0.78 [0.56, 1.01] |
0.56 [0.34, 0.79] |
0.42 [0.19, 0.65] |
0.58 [0.35, 0.80] |
0.51 [0.29, 0.74] |
|
| d (pre-f/u) [95% CI] |
0.86 [0.62, 1.09] |
0.82 [0.58, 1.06] |
0.49 [0.25, 0.73] |
0.46 [0.22, 0.69] |
0.31 [0.07, 0.55] |
0.50 [0.26, 0.74] |
0.46 [0.27, 0.70] |
|
| Supportive Psychotherapy (SP) | ||||||||
| Pre-treatment | 86 | 28.18 (9.3) | 77.01 (16.0) | 6.19 (1.6) | 5.49 (3.3) | 2.95 (3.1) | 8.83 (4.1) | 5.99 (3.2) |
| Mid-treatment | 73 | 31.27 (8.2) | 80.30 (14.9) | 6.47 (1.2) | 4.56 (2.9) | 2.55 (2.7) | 8.12 (3.9) | 5.15 (3.3) |
| Post-treatment | 69 | 32.86 (8.9) | 82.48 (14.7) | 6.55 (1.6) | 4.14 (3.1) | 2.62 (2.9) | 7.86 (4.2) | 4.46 (3.1) |
| Follow-up | 54 | 32.28 (8.3) | 82.96 (13.9) | 6.65 (1.6) | 3.70 (2.8) | 2.24 (2.9) | 6.92 (3.5) | 4.11 (2.5) |
| d (pre-post) [95% CI] |
0.57 [0.33, 0.82] |
0.59 [0.35, 0.83] |
0.12 [−0.12, 0.36] |
0.33 [0.10, 0.58] |
0.12 [−0.13, 0.36] |
0.37 [0.13, 0.61] |
0.48 [0.24, 0.72] |
|
| d (pre-f/u) [95% CI] |
0.48 [0.20, 0.76] |
0.54 [0.27, 0.82] |
0.13 [−0.14, 0.31] |
0.41 [0.13, 0.68] |
0.21 [−0.06, 0.48] |
0.57 [0.29, 0.84] |
0.58 [0.30, 0.86] |
|
| Enhanced Usual Care (EUC) | ||||||||
| Pre-treatment | 74 | 29.53 (8.0) | 75.49 (16.3) | 6.24 (1.6) | 4.85 (3.2) | 2.19 (3.2) | 8.57 (3.6) | 5.62 (3.7) |
| Mid-treatment | 62 | 31.19 (8.4) | 75.60 (15.9) | 6.48 (1.6) | 4.56 (3.5) | 2.05 (3.5) | 7.82 (3.9) | 5.48 (3.4) |
| Post-treatment | 60 | 31.88 (8.3) | 77.95 (15.0) | 6.49 (1.5) | 3.91 (3.4) | 2.05 (3.1) | 7.77 (3.8) | 5.10 (3.5) |
| Follow-up | 53 | 33.25 (8.2) | 78.55 (17.4) | 6.44 (1.5) | 4.04 (3.5) | 1.91 (3.0) | 7.70 (3.7) | 4.83 (3.5) |
| d (pre-post) [95% CI] |
0.31 [0.05, 0.57] |
0.24 [−0.02, 0.50] |
0.23 [−0.03, 0.49] |
0.48 [0.22, 0.75] |
0.02 [−0.23, 0.29] |
0.25 [−0.01, 0.51] |
0.22 [−0.04, 0.48] |
|
| d (pre-f/u) [95% CI] |
0.49 [0.21, 0.77] |
0.29 [0.01, 0.56] |
0.09 [−0.19, 0.36] |
0.28 [0.00, 0.56] |
.05 [−0.22, 0.33] |
0.29 [0.02, 0.57] |
0.26 [−0.02, 0.53] |
|
| Between Group Effect Sizes for Slopes | ||||||||
| IMCP v. EUC | 0.21 | 0.34 | 0.21 | 0.10 | 0.17 | 0.18 | 0.14 | |
| SP v. EUC | 0.06 | 0.14 | 0.03 | 0.07 | 0.07 | 0.14 | 0.12 | |
| IMCP/SP v. EUC | 0.16 | 0.27 | 0.14 | 0.10 | 0.14 | 0.18 | 0.14 | |
| IMCP v. SP | 0.15 | 0.19 | 0.19 | 0.02 | 0.09 | 0.04 | 0.01 | |
Note: Data reflect intent-to-treat analyses;
p < .05,
p < .01,
p < .001
n for individual cells may vary slightly based on missing data
SWB: FACIT Spiritual Well-Being Scale (Range: 0–48), LAP-R: Life Attitude Profile, Existential Transcendence scale (Range: −33–182), MQOL: McGill Quality of Life Scale (Range: 0–10), HAI: Hopelessness Assessment in Illness scale (Range: 0–16); SAHD: Schedule of Attitudes towards Hastened Death (Range: 0–20); HADS-A: Hospital Anxiety and Depression Scale, Anxiety subscale (Range: 0–21); HADS-D: Hospital Anxiety and Depression Scale, Depression subscale (Range: 0–21);
d corresponds to the within group change (or difference) score, where D=X1–X2 and d= MeanD/SDD, Cohen categorized d scores of .2 as small,.5 moderate, and.8 as large.34
Analysis of participants who attended 3 or more sessions
Analysis of participants that attended three or more treatment sessions (n=264; all EUC participants were included) generated somewhat stronger treatment effects, with a significant group by treatment interaction on all three primary outcome variables: SWB, F(2,583)=4.09, p=.02; LAP-R, F(2,592)=10.00, p < .0001; MQOL, F(2,590)=5.05, p=.007. Of the four secondary outcome variables, only HADS-A, F(2,590)=3.06, p=.05, generated a significant treatment effect while a fifth variable (SAHD) approached significance, F(2,589)=2.55, p=.08. When compared directly to EUC, IMCP demonstrated significantly greater improvement on five of the seven dependent variables (SWB, LAP-R, MQOL, SAHD, and HADS-A), with a sixth (HADS-D) approaching significance (p=.07). Once again, no significant difference in improvement was observed between SP and EUC for any of the dependent variables. Post-hoc contrasts demonstrated an even greater discrepancy in improvement between IMCP and SP, as improvement was greater for IMCP on each of the three primary outcome variables (SWB, LAP-R, and MQOL). Of note supplemental analyses that included gender as a possible covariate resulted in comparable findings (data available upon request).
Discussion
These findings add to a growing literature that supports the efficacy of Meaning Centered Psychotherapy, and provides several unique contributions. Unlike prior research, this study included a “no treatment” comparison arm (enhanced usual care), since distress might improve (or worsen) over time even without intervention. In addition, we included only patients who had a moderate to high level of distress at baseline (based on a widely-used screening tool, the Distress Thermometer). The results of these analyses were consistent with our prior research, demonstrating treatment effects for IMCP (small to moderate in magnitude) and little to no significant benefit from supportive psychotherapy.
As in our previous studies, the strongest treatment effects for IMCP were observed for measures of overall quality of life, sense of meaning and spiritual well-being. These treatment effects were somewhat stronger than those observed for supportive psychotherapy, an “active” mental health intervention, but the effect size for these differences in treatment effects were small and most comparisons of IMCP to supportive psychotherapy were not significant. Even more modest treatment effects were observed for IMCP on desire for hastened death, anxiety, hopelessness, and depression. These results indicate that while IMCP generated somewhat better treatment outcomes, the difference between these two interventions (IMCP and supportive psychotherapy) is modest. Not surprisingly, slightly stronger results were observed when we analyzed data from only those patients that attended at least three sessions. This analysis provides a less conservative estimate of treatment effects, and indicates that improvement is bolstered by more frequent attendance.
Of the outcome variables studied, only depression and hopelessness failed to demonstrate significantly greater improvement compared to EUC, as these variables improved comparably across all three treatment arms. This finding may be due to the relative effectiveness of other interventions for improving severe psychiatric symptoms such as depression and hopelessness, including outside sources of support or treatment (which was encouraged as part of the “enhanced” usual care). Indeed, many patients were receiving concurrent mental health interventions, further highlighting the potential benefits of MCP as an adjuvant intervention for alleviating existential distress and improving spiritual well-being.
Although this study utilized a rigorous, 3-arm randomized, controlled design, several methodological considerations limit the conclusiveness of these results. First, we did not control for concurrent mental health or palliative care interventions. In fact, the EUC condition explicitly facilitated identifying outside sources of support. Some participants (in all three arms) were also on concomitant psychotropic medications (whether prescribed for psychiatric symptoms or other reasons – e.g., sedation, neuropathic pain, etc.). Controlling for the countless variations in psychotropic medications (including type of medication, reason prescribed, and dose) was simply not feasible, and may have hindered our assessment of the relative effectiveness of IMCP. Similarly, while we opted to set a minimum threshold of distress for entry into the study, it is not clear whether this helped or hindered our analyses, as it likely reduced the range of distress observed in the sample. This decision was made in order to more accurately assess the utility of IMCP in alleviating distress (since improvement is harder to establish in patients with low levels of distress), but the extent to which this methodological decision impacted our findings is unknown. Disappointment in being assigned to EUC may have impacted our study findings (and let to the slightly higher attrition rate among EUC participants). Finally, the generalizability of these results is limited by the over-representation of women in our sample. Although post-hoc analyses indicated no difference in treatment effects between men and women, further research examining this possible source of bias is warranted.
Despite these study limitations, our results provide further evidence that MCP is an effective intervention for improving quality-of-life and spiritual well-being and reducing psychological distress. This intervention targets the challenging domains of existential and spiritual despair, which many clinicians feel ill prepared to address. Given the importance of spiritual well-being and sense of meaning among patients confronting a terminal illness, the availability of a manualized, empirically supported intervention such as IMCP has tremendous potential for improving patient quality of life during the final months of life. Moreover, although this intervention was designed for patients with advanced cancer, the focus on (and utility for) enhancing meaning and quality of life may have broad applicability across a range of illnesses and conditions in which physical and psychological functioning is adversely impacted.
Acknowledgments
The authors express their appreciation to the following research assistants and study interventionists: Marta Checci, Denise Gelfand, Michael Hoyt, Jordana Jacobs, Kate DuHamel, Elissa Kolva, Stephanie Lacey, and Emma Stein, along with Dr. Kate DuHamel, for supervising the supportive psychotherapy treatment arm.
Funding/Support: This study was supported by a grant from the National Cancer Institute (Grant number R01 CA128134; W. Breitbart, Principle Investigator).
Funding Source: NIH R01 CA164350
Footnotes
Conflict of Interest disclosures: none
Role of the Funder/Sponsor: The funding agency had no role in the design, implementation or analysis of this study.
Author Contributions: Brieitbart: conceptualization, funding acquisition, design, data analysis, writing; Pessin: conceptualization, funding acquisition, design, data analysis, writing; Rosenfeld: conceptualization, funding acquisition, design, data analysis, writing; Applebaum: subject recruitment, interventionist, writing; Lichtenthal: subject recruitment, interventionist, writing; Li: design, data analysis; James: subject recruitment, interventionist, writing; Marziliano: subject recruitment, interventionist, writing; Masterson: subject recruitment, interventionist, writing; Tobias: subject recruitment, interventionist, writing; Fenn: subject recruitment, data management, writing;
References
- 1.Breitbart W. Spirituality and meaning in supportive care: spirituality and meaning-centered group psychotherapy intervention in advanced cancer. Sup Care Cancer. 2002;10:272–8. doi: 10.1007/s005200100289. [DOI] [PubMed] [Google Scholar]
- 2.Greenstein M, Breitbart W. Cancer and the experience of meaning: A group psychotherapy program for people with cancer. Am J Psychotherapy. 2000;54:486–500. doi: 10.1176/appi.psychotherapy.2000.54.4.486. [DOI] [PubMed] [Google Scholar]
- 3.Breitbart W, Heller KS. Reframing hope: Meaning-centered care for patients near the end of life. J Pall Med. 2003;6:979–88. doi: 10.1089/109662103322654901. [DOI] [PubMed] [Google Scholar]
- 4.Spiegel D, Bloom JR, Yalom I. Group support for patients with metastatic cancer. A randomized outcome study. Arch Gen Psychiatry. 1981;38:527–533. doi: 10.1001/archpsyc.1980.01780300039004. [DOI] [PubMed] [Google Scholar]
- 5.Yalom ID, Greaves C. Group therapy with the terminally ill. Am J Psychiatry. 1977;134:396–400. doi: 10.1176/ajp.134.4.396. [DOI] [PubMed] [Google Scholar]
- 6.Kissane DW, Bloch S, Smith GC, et al. Cognitive-existential group psychotherapy for women with primary breast cancer: a randomised controlled trial. Psycho-Onc. 2003;12:532–546. doi: 10.1002/pon.683. [DOI] [PubMed] [Google Scholar]
- 7.Lo C, Hales S, Jung JD, et al. Managing Cancer And Living Meaningfully (CALM): Phase 2 trial of a brief individual psychotherapy for patients with advanced cancer. Palliat Med. 2014;28:234–42. doi: 10.1177/0269216313507757. [DOI] [PubMed] [Google Scholar]
- 8.Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Dignity therapy: a novel psychotherapeutic intervention for patients near the end of life. J Clin Oncol. 2005;23:5520–5525. doi: 10.1200/JCO.2005.08.391. [DOI] [PubMed] [Google Scholar]
- 9.Ando M, Morita T, Akechi T, Okamoto T. Efficacy of short-term life-review interviews on the spiritual well-being of terminally ill cancer patients. J Pain Symptom Manage. 2010;39:993–1002. doi: 10.1016/j.jpainsymman.2009.11.32020538183. [DOI] [PubMed] [Google Scholar]
- 10.Ando M, Morita T, Akechi T, Okamoto T Japanese Task Force for Spiritual Care. Efficacy of short-term life-review interviews on the spiritual well-being of terminally ill cancer patients. J Pain Symptom Manage. 2010;39:993–1002. doi: 10.1016/j.jpainsymman.2009.11.320. [DOI] [PubMed] [Google Scholar]
- 11.Yalom ID. Existential Psychotherapy. New York: Basic Books; 1980. [Google Scholar]
- 12.Frankl VF. Man’s Search for Meaning. 4. Massachusetts: Beacon Press; 1959/1992. [Google Scholar]
- 13.Breitbart W, Rosenfeld B, Gibson C, et al. Meaning-Centered Group Psychotherapy for patients with advanced cancer: A pilot randomized controlled trial. Psycho-Onc. 2010;19:21–8. doi: 10.1002/pon.1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Breitbart W, Rosenfeld B, Pessin H, Applebaum A, Kulikowski J, Lichtenthal WG. Meaning-centered group psychotherapy: an effective intervention for improving psychological well-being in patients with advanced cancer. J Clin Onc. 2015;33:749–54. doi: 10.1200/JCO.2014.57.2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Applebaum AJ, Kulikowski JR, Breitbart W. Meaning-centered psychotherapy for cancer caregivers (MCP-C): rationale and overview. Pall Support Care. 2015;13:1631–41. doi: 10.1017/S1478951515000450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van der Speck N, Vos J, van Uden-Kraan CF, et al. Effectiveness and cost-effectiveness of meaning-centered group psychotherapy in cancer survivors: protocol of a randomized controlled trial. BMC Psychiatry. 2014;14:22. doi: 10.1186/1471-244X-14-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leng J, Lue F, Chen A, et al. Cultural and linguistic adaptation of meaning-centered psychotherapy for Chinese cancer patients. In: Breitbart W, editor. Meaning-Centered Psychotherapy in the Cancer Setting. New York: Oxford Press; pp. 122–133. [Google Scholar]
- 18.Goldzweig G, Hasson-Ohayon I, Elinger G, et al. Adaptation of meaning-centered group psychotherapy in the Israeli context: The process of importing an intervention and preliminary results. In: Breitbart W, editor. Meaning-Centered Psychotherapy in the Cancer Setting. New York: Oxford Press; pp. 145–156. [Google Scholar]
- 19.Gil F, Fraguell C, Limonero JT. Replication study of meaning-centered group psychotherapy in Spain: Cultural and linguistic challenges. In: Breitbart W, editor. Meaning-Centered Psychotherapy in the Cancer Setting. New York: Oxford Press; pp. 157–167. [Google Scholar]
- 20.Breitbart W, Poppito S, Rosenfeld B, et al. Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. J Clin Onc. 2012;30:1304–19. doi: 10.1200/JCO.2011.36.2517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lederberg MS, Holland JC. Supportive psychotherapy in cancer care: an essential ingredient of all therapy. In: Watson M, Kissane D, editors. Handbook of Psychotherapy in Cancer Care. 2011. pp. 3–14. [Google Scholar]
- 22.Roth AJ, Kornblith AB, Batel-Copel L, Peabody E, Scher HI, Holland JC. Rapid screening for psychologic distress in men with prostate carcinoma. Cancer. 1998;82:1904–8. doi: 10.1002/(sici)1097-0142(19980515)82:10<1904::aid-cncr13>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 23.Karnofsky DA, Burchenal JH. The clinical evaluation of chemotherapeutic agents in cancer. In: MacLeod CM, editor. Evaluation of Chemotherapeutic Agents. New York: Columbia University Press; 1949. pp. 191–205. [Google Scholar]
- 24.Brady MJ, Peterman AH, Fitchett G, Mo M, Cella D. A case of including spirituality in quality of life measurement in oncology. Psycho-oncology. 1999;8:417–28. doi: 10.1002/(sici)1099-1611(199909/10)8:5<417::aid-pon398>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 25.Reker GT. Manual of the Life Attitude Profile-Revised (LAP-R) Peterborough, ON: Student Psychologists Press; 1992. [Google Scholar]
- 26.Cohen SR, Mount BM, Strobel MG, et al. The McGill Quality of Life Questionnaire: a measure of quality of life appropriate for people with advanced disease. A preliminary study of validity and acceptability. Palliat Med. 1995;9:207–19. doi: 10.1177/026921639500900306. [DOI] [PubMed] [Google Scholar]
- 27.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 28.Rosenfeld B, Pessin H, Lewis C, et al. Assessing hopelessness in terminally ill cancer patients: Development of the Hopelessness Assessment in Illness Questionnaire. Psych Assess. 2011;23:325–36. doi: 10.1037/a0021767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosenfeld B, Breitbart W, Stein K, et al. Measuring desire for death among patients with HIV/AIDS: The Schedule of Attitudes toward Hastened Death. Am J Psychiatry. 1999;156:94–100. doi: 10.1176/ajp.156.1.94. [DOI] [PubMed] [Google Scholar]
- 30.Hatcher RL, Gillaspy JA. Development and validation of a revised short version of the Working Alliance Inventory. Psychotherapy Res. 2006;16:12–25. [Google Scholar]
- 31.Frankl VF. The will to meaning: Foundations and applications of logotherapy, expanded edition. New York: Penguin Books; 1969/1988. [Google Scholar]
- 32.Breitbart WS, Poppito SR. Meaning-Centered Group Psychotherapy for Patients with Advanced Cancer: A Treatment Manual. New York: Oxford Press; 2014. [Google Scholar]
- 33.Breitbart WS, Poppito SR. Individual Meaning-Centered Psychotherapy for Patients with Advanced Cancer: A Treatment Manual. New York: Oxford Press; 2014. [Google Scholar]
- 34.Payne DK, Lundberg JC, Brennan MF, Holland JC. A psychosocial intervention for patients with soft tissue sarcoma. Psycho-oncology. 1997;6:65–71. doi: 10.1002/(SICI)1099-1611(199703)6:1<65::AID-PON236>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 35.Holland JC, Lewis S. The Human Side of Cancer: Living with Hope, Coping with Uncertainty. New York: Harper Perennial; [Google Scholar]
- 36.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Royal Stat Soc Series B (Methodological) 1995:289–300. [Google Scholar]