Abstract
Background
Children suffering non-accidental trauma (NAT) are at high risk of death. It is unclear whether markers of injury severity for trauma center/system benchmarking such as injury severity score (ISS) adequately characterize this. Our objective was to evaluate mortality prediction of ISS in children with NAT compared to accidental trauma (AT).
Methods
Pediatric patients age<16years from the Pennsylvania state trauma registry 2000–2013 were included. Logistic regression predicted mortality from ISS for NAT and AT patients. Multilevel logistic regression determined the association between mortality and ISS while adjusting for age, vital signs, and injury pattern in NAT and AT patients. Similar models were performed for head AIS. Sensitivity analysis examined impaired functional independence at discharge as an alternate outcome.
Results
50,579 patients were included with 1,866 (3.7%) NAT patients. NAT patients had a similar rate of mortality at an ISS of 13 as an ISS of 25 for AT patients. NAT patients also have higher mortality for a given head AIS level (range 1.2–5.9-fold higher). ISS was a significantly greater predictor of mortality in AT patients (AOR 1.14; 95%CI 1.13—1.15, p<0.01) than NAT patients (AOR 1.09; 95%CI 1.07—1.12, p<0.01) per 1-point ISS increase, while head injury was a significantly greater predictor of mortality in NAT patients (AOR 3.48; 95%CI 1.54—8.32, p<0.01) than AT patients (AOR 1.21; 95%CI 0.95—1.45, p=0.12). NAT patients had a higher rate of impaired functional independence at any given ISS or head AIS level than AT patients.
Conclusions
NAT patients have higher mortality and impaired function at a given ISS/head AIS than AT patients. Conventional ISS thresholds may under-estimate risk and head injury is a more important predictor of mortality in the NAT population. These findings should be considered in system performance improvement and benchmarking efforts that rely on ISS for injury characterization.
Level of Evidence
III, epidemiologic
Keywords: pediatric, ISS, mortality, non-accidental trauma, head injury
BACKGROUND
Children who are victims of non-accidental trauma (NAT) suffer high rates of mortality and morbidity compared to other injured children.1 In 2006, the estimated hospitalization costs alone for NAT patients was $78.3million.2 Given the potential years of productive life lost combined with total societal costs estimated at $103billion, NAT is a serious public health problem.2
Organized trauma systems with the inclusion of specialized pediatric trauma centers have improved outcomes for these patients.3–5 Recent focus on research, quality improvement, and trauma center benchmarking have driven performance.6 Risk adjustment using injury scoring systems have significant impact across these domains. The most ubiquitous scoring system is the Injury Severity Score (ISS), based on the Abbreviated Injury Scale (AIS).7 This remains true for injured children evaluated at trauma centers, despite the availability of several pediatric specific trauma scoring systems.8–10
It is critical to ensure that benchmarking and quality improvement efforts based on ISS characterization of injury in pediatric trauma patients perform well. Our group and others previously demonstrated the traditional ISS threshold of 15 to define severe injury in pediatric patients over-estimated risk, and an ISS threshold of 25 may be a better definition in children.11 Poor performance of characterization of risk in injured children can result in imprecise benchmarking, poor quality improvement targets, and wasted resources with unnecessary performance review of low risk cases with potentially missing high-risk patients.
Given the significant mortality risk of NAT patients, it is possible that ISS under-estimates the risk of poor outcome in these children. Thus, it remains unclear whether markers of injury severity for trauma center/system benchmarking such as injury severity score (ISS) adequately characterize risk in this population. Further, head injury appears to be a significant driver of poor outcome in NAT patients and may more important than global ISS.12
Therefore, our objective was to evaluate ISS and head AIS for the ability to predict mortality in pediatric trauma patients with NAT compared to those with accidental trauma (AT). We hypothesized that ISS would under-estimate the risk of mortality for patient with NAT compared to AT, and that head injury would be a more important predictor of mortality in NAT patients.
METHODS
Study Population
All pediatric patients aged 16 years or less in the Pennsylvania state trauma registry between January 1st, 2000 and June 30th, 2013 were eligible for inclusion. Patients missing age data were excluded. Patients missing complete AIS score data to permit calculation of ISS were also excluded. Finally, patients with any AIS score of 6 that was also coded as surviving to discharge were excluded as AIS misclassification.
Demographics, injury characteristics, vital signs, International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes, and hospital disposition were collected for each subject. All vital signs for children were age-adjusted and binary variables created to indicate whether each vital sign was abnormal or not for the child’s age. As there are likely differences across age groups within the pediatric population, patients were categorized into infant/toddler (age <2years), children (age 2–12 years), and adolescents (age >12) age subgroups based on established standards.
Missing Data
Missing data were assessed for variables to be utilized in analysis, including gender, mechanism of injury, non-accidental trauma, and admission systolic blood pressure (SBP), heart rate (HR), and respiratory rate (RR). After application of exclusion criteria, missing data were 1% or less for all analysis variables except for admission SBP at 4.8%. All patients had complete data for age, AIS, and ISS. Thus, given missing data <5%, patients were excluded from analyses for which they were missing observed variables.
Injury Characterization
Injuries were primarily characterized using AIS scores and body region. The Pennsylvania trauma registry allows coding of multiple AIS scores for each patient in eight body regions, including head, face, neck, chest, abdomen, spine, upper extremities, and lower extremities. The maximum AIS score for each of these body regions was identified for each patient. The ISS used for purposes of this study was then calculated as the sum of the squared value for the three highest AIS scores in different body regions.
NAT patients were identified through a specific variable in the registry that indicated the patient was evaluated and report made concerning child abuse. Additionally, patients with an e-code of 967 were identified as NAT patients.
Statistical Analysis
A logistic regression model was used to obtain the predicted mortality based on ISS separately for NAT and AT patients, and predicted mortality was plotted against the ISS. A sub-group analysis was performed repeating this model stratified across pediatric age groups to evaluate further differences in ISS performance between NAT and AT in infants and toddlers, children, and adolescents.
A multi-level logistic regression was used to evaluate the association between mortality and ISS in pediatric patients after adjusting for age, abnormal admission SBP, HR, and RR, presence of multi-system injury defined as more than one AIS body system injured, and presence of severe head injury, defined as head AIS>2. A random effect was included for facilities to account for clustering at the center level. The interaction between NAT and ISS was tested with pre-planned stratification of the model across NAT and AT patients if the interaction was significant. This allowed estimation of the effect on mortality per point change in ISS in NAT and AT patients separately.
Since head injury is a strong driver of mortality in NAT,13 a similar multi-level logistic regression model was constructed to evaluate the association between mortality and head AIS. Predicted mortality was estimated at each level of head AIS and compared between NAT and AT patients, as was the effect on mortality per point change in head AIS. The multi-level logistic model was also performed to evaluate the interaction between NAT status and presence of any head injury, defined as head AIS≥1, as well as severe head injury. Models were then again stratified if the interaction was positive across NAT status to determine the differential effect of head injury on mortality in NAT and AT patients.
Continuous data are presented as median (interquartile range [IQR]). Continuous variables were compared using Wilcoxon rank-sum tests, and categorical variables were compared using Chi-squared tests. Adjusted odds rations (AOR) with 95%CI were obtained from regression models. A two-sided p value ≤0.05 was considered significant. Data analysis was conducted using Stata v13MP (StataCorp; College Station, TX).
Sensitivity Analysis
Given the potential morbidity and years of productive life lost in the pediatric trauma population, a sensitivity analysis was performed using functional status as discharge (FSD) as an alternative outcome. The Pennsylvania trauma registry assesses FSD using a modified Functional Independence Measure score to measure the level of independent functioning in patients 2 years and older across five domains including feeding, locomotion, expression, transfer mobility, and social interaction. Categorical scores include 1 (complete dependence), 2 (modified dependence), 3 (independent with device), or 4 (completely independent) for each domain, giving a total FSD score from 5 to 20. The FSD was dichotomized at 15 to reflect patients that are at least independent with a device across all domains (FSD≥15) compared to patients with impaired functional independence in at least one domain (FSD<15). The models described above were repeated using impaired functional independence (FSD<15) as the outcome to determine the association with ISS and head AIS.
RESULTS
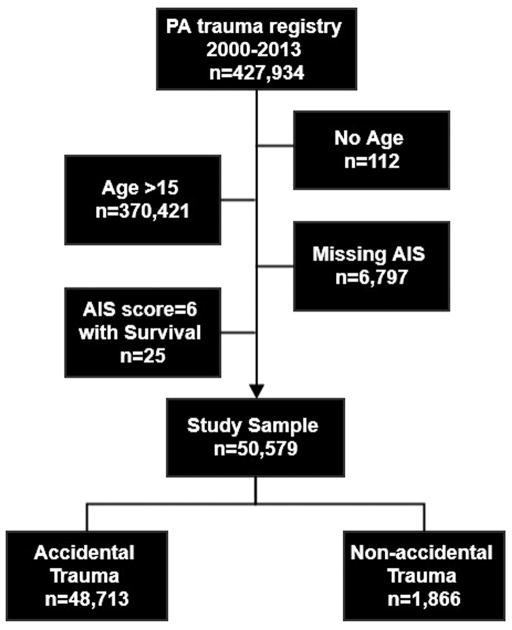
From 57,401 pediatric patients in the Pennsylvania trauma state trauma registry, 50,579 met inclusion criteria (Fig. 1). Of these, 1,866 (3.7%) were identified as NAT patients. Overall, NAT patients were younger and more severely injured with higher unadjusted mortality and impaired functional independence compared with AT patients (Table 1). More NAT patients were seen at pediatric trauma centers, with an overall NAT rate of 4.9% at pediatric only trauma centers, 3.8% at combined pediatric and adult trauma centers, and 1.3% at adult only trauma centers (p<0.001).
Figure 1.
Study participant selection of pediatric trauma patients from the Pennsylvania trauma registry 2000—2013.
Table 1.
Comparison of accidental and non-accidental trauma pediatric patients
| Accidental Trauma N=48,713 |
Non-accidental Trauma N=1,866 |
p value | |
|---|---|---|---|
| Age [years, med (IQR)] | 8 (4, 13) | 1 (1, 2) | <0.001 |
| Age group [n (%)] | <0.001 | ||
| Infant/toddler age group | 8,760 (18) | 1,644 (88) | |
| Child age group | 27,448 (56) | 201 (11) | |
| Adolescent age group | 12,505 (26) | 21 (1) | |
| Sex [n (% male)] | 32,297 (66) | 1,099 (59) | <0.001 |
| Mechanism [n (% blunt)] | 45,421 (94) | 1,773 (99) | <0.001 |
| Hypotension [n (%)] | 18,045 (37) | 64 (3) | <0.001 |
| Abnormal heart rate [n (%)] | 8,674 (18) | 167 (9) | <0.001 |
| Abnormal respiratory rate [n (%)] | 20,060 (41) | 720 (39) | 0.025 |
| ISS [med (IQR)] | 9 (4, 11) | 11 (4, 21) | <0.001 |
| Max head AIS [med (IQR)] | 2 (2, 4) | 4 (3, 5) | <0.001 |
| Multisystem injury [n (%)] | 19,808 (41) | 1,233 (66) | <0.001 |
| Trauma center type [n (%)] | <0.001 | ||
| Pediatric only | 25,267 (52) | 1,289 (69) | |
| Combined Pediatric/Adult | 9,910 (20) | 393 (21) | |
| Adult only | 13,536 (28) | 184 (10) | |
| Mortality [n (%)] | 702 (1) | 141 (8) | <0.001 |
| Impaired functional independence [n (%)]* | 2,223 (9) | 41 (22) | <0.001 |
N for accidental trauma patients = 23,876; N for non-accidental trauma patients = 188
IQR, interquartile range; ISS, injury severity score; Max, maximum; AIS, abbreviated injury scale
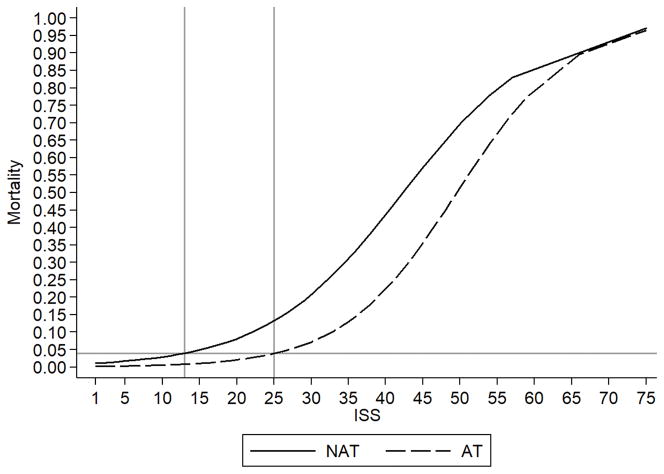
Predicted mortality plotted against ISS in NAT patients and AT patients demonstrates a similar rate of mortality at an ISS of 25 for AT patients as an ISS of 13 for NAT patients (Fig. 2). When stratified by pediatric age group, NAT patients in the child age group had the highest mortality at the lowest ISS, followed by NAT patients in the infant and toddler age group (eFig. 1). Patients in the child age group had the greatest disparity in mortality over ISS across NAT and AT patients. A significant interaction was seen between NAT status and ISS (p<0.001). Multi-level logistic regression demonstrated that for every 1-point increase in ISS, the odds of mortality increased 9% among NAT patients (AOR 1.09; 95%CI 1.07—1.12, p<0.001) compared 14% among AT patients (AOR 1.14; 95%CI 1.13—1.15, p<0.001).
Figure 2.
Predicted mortality across ISS in pediatric trauma patients with non-accidental trauma (NAT) and accidental trauma (AT). NAT patients have a similar predicted mortality rate at an ISS of 13 as AT patients at an ISS of 25.
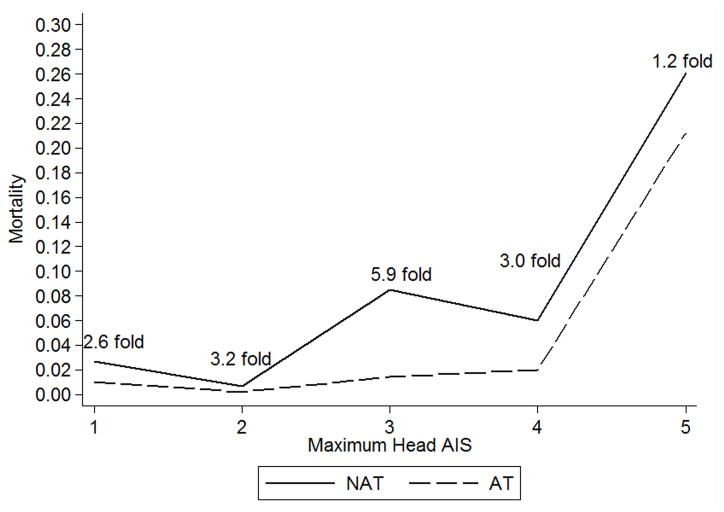
Regression modeling also demonstrated mortality was consistently higher among NAT patients compared to AT patients across head AIS, ranging from 1.2-fold higher for a head AIS of 5 to 5.9-fold high for a head AIS of 3 (Fig. 3). For every 1-point increase in head AIS, the odds of mortality increased 78% among NAT patients (AOR 1.78; 95%CI 1.25—2.50, p=0.001) compared 54% among AT patients (AOR 1.54; 95%CI 1.37—1.74, p<0.001).
Figure 3.
Risk-adjusted mortality across Head AIS in pediatric trauma patients with non-accidental trauma (NAT) and accidental trauma (AT).
A significant interaction between NAT status and presence of any head injury (p<0.001) as well as severe head injury (p<0.001) was present. When stratifying regression models, no association between mortality and the presence of any head injury was seen among AT patients (AOR 1.21; 95%CI 0.95–1.45, p=0.12), while presence of any head injury was associated with a nearly 3.5-fold increase in odds of mortality among NAT patients (AOR 3.48; 95%CI 1.54–8.32, p<0.001). Severe head injury was associated with a 2.2-fold increase in odds of mortality among AT patients (AOR 2.23; 95%CI 1.80–2.87, p<0.001) compared with a more than 4.4-fold increase among NAT patients (AOR 4.41; 95%CI 2.02–9.66, p<0.01).
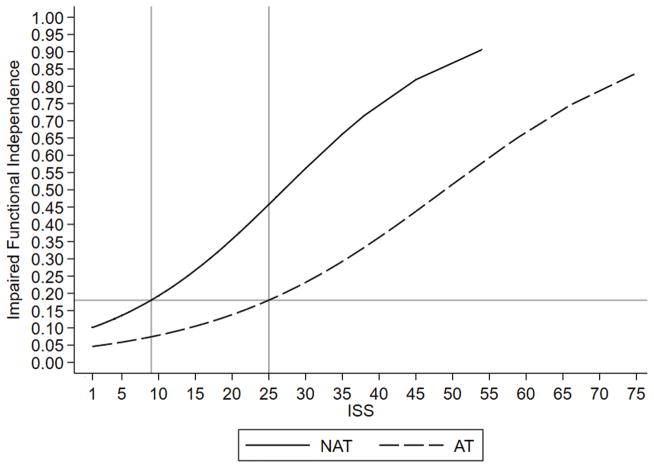
In sensitivity analysis, 26,140 patients had a FSD recorded. Predicted impaired functional independence plotted against ISS in NAT patients and AT patients demonstrates a similar rate of impaired functional independence at an ISS of 25 for AT patients as an ISS of 9 for NAT patients (Fig. 4). Similarly, the rate of impaired functional independence was consistently higher among NAT patients compared to AT patients across head AIS, ranging from 1.8-fold higher for a head AIS of 4 to 2.1-fold high for a head AIS of 1 (eFig. 2).
Figure 4.
Predicted rate of impaired functional independence (FSD<15) across ISS in pediatric trauma patients with non-accidental trauma (NAT) and accidental trauma (AT) stratified by pediatric age group.
DISCUSSION
This study demonstrates that ISS under-estimates the risk of mortality among NAT children, with consistently higher risk of mortality for a given ISS level compared to children with AT. The associated risk of mortality per point increase in ISS is significantly greater for AT patients than NAT patients, suggesting ISS level may play a less important role in mortality risk adjustment for NAT compared to AT patients.
Similarly, mortality across head AIS was consistently higher among NAT compared to AT patient; however, the per point increase in head AIS was associated with a larger increase in the risk of mortality in NAT compared with AT patients. The presence of any level of head injury was a predictor of mortality in NAT patients, but not AT patients. Severe head injury was associated with double the risk of mortality in NAT compared as in AT patients. Finally, the NAT rate was highest at pediatric trauma centers. This may likely be due at least in part to greater case detection and awareness by providers in these centers. It may also represent an educational opportunity for adult trauma centers that see significant numbers of injured children.
When looking at impaired functional independence at discharge, NAT patients again had a significantly higher risk for any given ISS level. NAT patients also had a 2-fold higher risk of impaired functional independence across the levels of head AIS.
Thus, these results suggest that traditional injury severity scoring such as the ISS and AIS under-estimate the risk of mortality and impaired functional outcome in NAT compared to AT patients. Head injury does appear to be a better predictor of poor outcome than ISS in NAT patients.
Others have similarly demonstrated NAT patients have worse outcomes compared to AT patients, with longer hospital and intensive care unit stays, higher rates of craniotomy and laparotomy, as well as higher mortality and nearly double ISS as a group.1, 14 However, a number of studies have documented conventional ISS definitions of severe injury (ISS>15) perform poorly in predicting outcomes in the pediatric population.
Several authors have evaluated ISS thresholds that maximize sensitivity and specificity for predicting outcomes among injured children, finding thresholds of ISS≥20, ISS>25, and even ISS≥28 performed best.10, 11, 15, 16 These studies suggest ISS over-estimates the risk of poor outcome in the general pediatric trauma population compared to a conventional ISS threshold of 15 defining severe injury in the adult. This may be due to the resilience of pediatric physiology and low risk of death in single system injuries among children. The results of the current study demonstrate just the opposite in the NAT population.
There may be several reasons for these findings. First, ISS is driven by AIS. The various body regions of AIS are not weighted, with each given the same significance. However, the risk of death between a severe head injury and extremity injury are not similar. Our results here and others suggest mortality is often driven by head injury in the NAT population.12 Johnson et al demonstrated NAT head injuries were often associated with apnea leading to cerebral hypoxia and ischemia independent of type of brain injury,17 and may account for the poor outcome in NAT compared to AT patients at a given severity of head injury seen here. This issue may be further exacerbated in some cases, as a delay in seeking medical attention or failing to disclose the true mechanism of injury by caregivers is common and may lead to increasing secondary brain injury and worse outcomes in the NAT patient with head injury.
Differences in age groups for outcome were also seen. The child age group had the greatest mortality differential. This may be influenced by the developmental neurobiology during this period of life, with head injury leading to more severe derangements and higher risk of death and disability. Children also tend to have more focal brain lesions after NAT than infants, which may impact outcome and requirement for neurosurgical intervention.18 The differences in outcome across pediatric age groups seen here deserve further exploration in future studies.
Under-recognition of NAT may also play a role in worse outcome for a given level of injury severity. Particularly in younger children, where NAT is most common, the lack of history and reliable exam can make diagnosis of NAT difficult. One study documented that 20% of NAT deaths had a delayed recognition of abuse.14 Jenny and colleagues evaluated abusive head injury, finding nearly a third were not recognized as NAT, with a delay in diagnosis on average of 7 days.19 They also found that 40% of unrecognized injuries had complications related to the missed diagnosis, and estimated 4 of 5 deaths were potentially preventable with earlier recognition.
This study has several potential implications. The ISS is commonly used in pediatric injury research to stratify and risk-adjust injury severity of patients, and is applied uniformly across NAT and AT patients. Thus, NAT status must be accounted for or poor risk-adjustment may result from under-estimation of risk in NAT patients. Further, studies that use ISS as inclusion criteria or sub-group analyses must take these findings into account when including NAT patients.
Performance improvement programs frequently use ISS to classify injury severity among injured children. Monitoring of under-triage and over-triage rates for trauma team activation is often based on stratifying patients using an ISS>15 to denote severely injured patients.20 This may again under-estimate risk in NAT patients, leading to unrecognized under-triage among this population. Performance improvement and case review triggers may need to be modified to capture all relevant cases.
These results may also have implications for risk-adjustment methods used in trauma center benchmarking efforts, such as the Pediatric Trauma Quality Improvement Program.6 Risk-adjustment benchmarking methods should consider NAT status, as well as weighing head injury more heavily than global ISS in these patients. Specific benchmarking in the NAT population may also be beneficial feedback to individual centers, and may allow development of best practices for care in this population.
This study has several limitations for consideration. First are those inherent to the retrospective observational design. Further, this is a registry based study. The data was not specifically collected for this analysis. The outcomes we could examine were limited by this. It is possible that NAT was under-reported both in the registry specific variable and utilizing e-codes; however, our prevalence was similar to recently published data.21 The ISS is mathematically complex with only certain specific values possible as a result of squaring AIS values. Missing data was minimal after application of exclusion criteria and was unlikely to alter our results given the study sample size.
The registry only collects data from trauma centers and children not brought to a trauma center in Pennsylvania are not evaluated, potentially leading to under-reporting of NAT. Further, it appears that NAT case detection may be lower at adult trauma centers. This could lead to additional potential under-reporting of NAT patients in the database; however most patients were seen at pediatric or combined pediatric/adult trauma center.
Longer term outcomes and quality of life measures were not available in the registry. We did evaluate FSD as an alternate outcome, also demonstrating under-estimation of poor outcome in NAT patients based on ISS. Only 52% of patients had a valid FSD documented; however, this is similar to that in other registry studies of functional outcomes after injury.22 Further, the FSD is only valid in age 2 or older, and thus many younger children with high incidence of NAT were not assessed. Other functional outcomes over longer time horizons are important to measure in pediatric trauma, given the potential disability over a lifetime following injury. Finally, this study focuses on ISS given its wide spread adoption and use for pediatric trauma patients; however, other scoring systems may better capture injury severity across accidental and non-accidental trauma.
CONCLUSION
NAT patients have higher mortality and impaired function at a given ISS and head AIS than AT patients. Conventional ISS thresholds may underestimate risk of death, and head injury is a more important predictor of mortality in the NAT population. These findings should be considered in research applications, as well as system performance improvement and benchmarking efforts that rely on ISS for injury characterization of pediatric trauma patients.
Supplementary Material
Acknowledgments
No funding or support was directly received to perform the current study.
Footnotes
There are no conflicts of interest for the current study
This paper was presented as an oral podium presentation at the 4th annual meeting of the Pediatric Trauma Society in Charleston, SC, November 2–4, 2017.
AUTHOR CONTRIBUTIONS: J.B.B. and B.A.G designed the study and performed the literature search. J.B.B. and M.L.G. performed the data collection. J.B.B performed the data analysis. J.B.B., M.L.G., C.M.L. and B.A.G. participated in initial manuscript preparation. All authors contributed to data interpretation and critical revision of the manuscript.
References
- 1.Roaten JB, Partrick DA, Nydam TL, Bensard DD, Hendrickson RJ, Sirotnak AP, Karrer FM. Nonaccidental trauma is a major cause of morbidity and mortality among patients at a regional level 1 pediatric trauma center. Journal of Pediatric Surgery. 2006;41:2013–2015. doi: 10.1016/j.jpedsurg.2006.08.028. [DOI] [PubMed] [Google Scholar]
- 2.Leventhal JM, Martin KD, Gaither JR. Using US data to estimate the incidence of serious physical abuse in children. Pediatrics. 2012;129:458–464. doi: 10.1542/peds.2011-1277. [DOI] [PubMed] [Google Scholar]
- 3.Hall JR, Reyes HM, Meller JL, Loeff DS, Dembek R. The outcome for children with blunt trauma is best at a pediatric trauma center. Journal of Pediatric Surgery. 1996;31:72–77. doi: 10.1016/s0022-3468(96)90322-x. [DOI] [PubMed] [Google Scholar]
- 4.Potoka DA, Schall LC, Ford HR. Improved Functional Outcome for Severely Injured Children Treated at Pediatric Trauma Centers. Journal of Trauma and Acute Care Surgery. 2001;51:824–834. doi: 10.1097/00005373-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Potoka DA, Schall LC, Gardner MJ, Stafford PW, Peitzman AB, Ford HR. Impact of Pediatric Trauma Centers on Mortality in a Statewide System. Journal of Trauma and Acute Care Surgery. 2000;49:237–245. doi: 10.1097/00005373-200008000-00009. [DOI] [PubMed] [Google Scholar]
- 6.American College of Surgeons Committee on Trauma. [Accessed: Sept 4, 2016];Pediatric Trauma Quality Improvement Program. Available at: https://www.facs.org/quality-programs/trauma/tqip/pediatric-tqip.
- 7.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 8.Marcin JP, Pollack MM. Triage scoring systems, severity of illness measures, and mortality prediction models in pediatric trauma. Crit Care Med. 2002;30:S457–467. doi: 10.1097/00003246-200211001-00011. [DOI] [PubMed] [Google Scholar]
- 9.Mayer T, Matlak ME, Johnson DG, Walker ML. The modified injury severity scale in pediatric multiple trauma patients. J Pediatr Surg. 1980;15:719–726. doi: 10.1016/s0022-3468(80)80271-5. [DOI] [PubMed] [Google Scholar]
- 10.Palmer C. Major Trauma and the Injury Severity Score - Where Should We Set the Bar? Annu Proc Assoc Adv Automot Med. 2007;51:13–29. [PMC free article] [PubMed] [Google Scholar]
- 11.Brown JB, Gestring ML, Leeper CM, Sperry JL, Peitzman AB, Billiar TR, Gaines BA. The value of the injury severity score in pediatric trauma: Time for a new definition of severe injury? J Trauma Acute Care Surg. 2017;82:995–1001. doi: 10.1097/TA.0000000000001440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deans KJ, Minneci PC, Lowell W, Groner JI. Increased morbidity and mortality of traumatic brain injury in victims of nonaccidental trauma. Journal of Trauma and Acute Care Surgery. 2013;75:157–160. doi: 10.1097/ta.0b013e3182984acb. [DOI] [PubMed] [Google Scholar]
- 13.Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten DF, Sinal SH. A population-based study of inflicted traumatic brain injury in young children. Jama. 2003;290:621–626. doi: 10.1001/jama.290.5.621. [DOI] [PubMed] [Google Scholar]
- 14.Estroff JM, Foglia RP, Fuchs JR. A comparison of accidental and nonaccidental trauma: it is worse than you think. J Emerg Med. 2015;48:274–279. doi: 10.1016/j.jemermed.2014.07.030. [DOI] [PubMed] [Google Scholar]
- 15.Ducrocq SC, Meyer PG, Orliaguet GA, Blanot S, Laurent-Vannier A, Renier D, Carli PA. Epidemiology and early predictive factors of mortality and outcome in children with traumatic severe brain injury: experience of a French pediatric trauma center. Pediatr Crit Care Med. 2006;7:461–467. doi: 10.1097/01.PCC.0000235245.49129.27. [DOI] [PubMed] [Google Scholar]
- 16.Orliaguet GA, Meyer PG, Blanot S, Jarreau MM, Charron B, Buisson C, Carli PA. Predictive factors of outcome in severely traumatized children. Anesth Analg. 1998;87:537–542. doi: 10.1097/00000539-199809000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Johnson DL, Boal D, Baule R. Role of Apneain Nonaccidental Head Injury. Pediatric Neurosurgery. 1995;23:305–310. doi: 10.1159/000120976. [DOI] [PubMed] [Google Scholar]
- 18.Kannan N, Ramaiah R, Vavilala MS. Pediatric Neurotrauma. Int J Crit Illn Inj Sci. 2014;4:131–137. doi: 10.4103/2229-5151.134152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jenny C, Hymel KP, Ritzen A, Reinert SE, Hay TC. Analysis of missed cases of abusive head trauma. JAMA. 1999;281:621–626. doi: 10.1001/jama.281.7.621. [DOI] [PubMed] [Google Scholar]
- 20.Escobar MA, Jr, Morris CJ. Using a multidisciplinary and evidence-based approach to decrease undertriage and overtriage of pediatric trauma patients. J Pediatr Surg. 2016;51:1518–1525. doi: 10.1016/j.jpedsurg.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 21.Bogumil DDA, Demeter NE, Kay Imagawa K, Upperman JS, Burke RV. Prevalence of nonaccidental trauma among children at American College of Surgeons–verified pediatric trauma centers. Journal of Trauma and Acute Care Surgery. 2017;83:862–866. doi: 10.1097/TA.0000000000001629. [DOI] [PubMed] [Google Scholar]
- 22.Brown JB, Stassen NA, Cheng JD, Sangosanya AT, Bankey PE, Gestring ML. Trauma center designation correlates with functional independence after severe but not moderate traumatic brain injury. J Trauma. 2010;69:263–269. doi: 10.1097/TA.0b013e3181e5d72e. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.