Abstract
Subjective stressors are critical to the caregiver stress process, yet little work has examined resources that contribute to longitudinal changes in subjective stressors. The present study examines a variety of factors that contribute to changes in subjective stressors across time. Dementia caregivers (N=153) completed an in-person interview and 8 daily telephone interviews at baseline, and follow up interviews at 6 and 12-months. Growth curve analyses examine how care- and non-care stressors, respite, dyadic relationship quality, family support/conflict and care transitions (e.g., nursing home placement) are associated with changes in role overload and role captivity across 12 months. Caregivers who transitioned out of their role had higher overload and captivity at baseline. Among caregivers who transitioned out of caregiving, higher captivity at baseline was associated with declines in captivity and overload; more non-care stressors at baseline was linked to increased captivity and greater overload across time. Adult day service use and family support were associated with lesser captivity over time; taking more breaks from caregiving was linked to lower overload. Higher dyadic relationship quality was associated with lower captivity and overload. Findings contribute to caregiver intervention efforts by highlighting important resources associated with subjective stressors across time.
Keywords: dementia caregiving, care transitions, subjective stressors
The impairments of a person with dementia (PWD) impose significant demands on family caregivers. Unlike the assessment of objective care stressors, which are directly associated with care tasks, subjective stress taps directly into caregivers’ appraisal of their care tasks as being more than they can manage (role overload) or appraising the caregiving role as unwanted and confining (role captivity; Pearlin, Menaghan, Lieberman, & Mullan, 1981). Consistent with the Transactional Model of Stress and Coping, subjective stressors are more important in contributing to caregiver outcomes than an objective measure of primary stressors; impact of objective/subjective stressors is mediated by one’s appraisal of the stressor and on the social and cultural resources at his or her disposal (Lazarus & Folkman, 1984; Pearlin et al., 1981). Compared to the objective demands of care, subjective stressors may be more amenable to change and therefore hold implications for caregiver intervention research. Thus, it is critical that research identify resources and factors that contribute to subjective stressors.
Most research on caregivers’ subjective stress has been cross-sectional in nature, providing a snapshot of characteristics associated with role overload and captivity at a particular point in time. This design limits our understanding of subjective stressors across time as well as factors that may lead to adaptation or further stress proliferation across time. One exception comes from Aneshensel and colleagues (Aneshensel, Pearlin, Mullen, Zarit, & Whitlatch, 1995) who examined subjective care stressors across a one-year period. Findings from this longitudinal work showed that subjective stressors among caregivers (N = 555 at baseline, and N = 352 at 1-year follow-up) had moderate stability over a one-year period. The study also found that characteristics of the caregiver/PWD dyad may contribute to subjective stress, specifically, the loss of intimate exchange between the caregiver and PWD intensified caregivers’ feelings of role overload across the study duration. Moreover, subjective stressors perpetuate other subjective stressors, such that greater role overload at baseline contributed to greater role captivity across a 1-year period. Likewise, objective stressors and the ADL needs of the PWD were found to intensify caregivers’ subjective stressors.
Care transitions and caregiving stress
A factor directly associated with objective caregiving stressor exposures, caregiving characteristics, and caregiver health is the transition whereby caregivers relinquish the caregiving role to another relative, or more often to a care facility. Care transitions tend to be related to decreased care-related stressor exposures, and lower assistance and support from other family members (Gaugler et al., 2000; Gaugler, Kane, Kane, Clay, & Newcomer, 2003). Further, there may be a selection effect at play where relatively healthy caregivers tend to continue caregiving longer than the ones who are less fit and physically capable. For example, caregivers who experience a transition are more likely to experience increasing functional limitations over time (Liu, Kim, & Zarit, 2015), yet little work examines the association between care transitions and subjective stressors.
Subjective stressors may precipitate care transitions, and no longer providing daily caregiving may relieve subjective stress. Caregivers may also experience subjective stressors amidst such transitions, because of concerns about the quality of institutional care. In this situation, the lingering subjective stressors related to caregiving could still interfere with caregiver well-being. Another type of transition involves the death of the PWD, and the subsequent period of grief and bereavement, which are unique stressors in themselves.
Aneshensel and colleagues (1995) highlighted the important association between subjective stressors and transitioning out of the caregiving role. Caregivers who continued to provide in-home care to the PWD throughout the duration of the study had lower levels of overload and captivity at baseline than those caregivers who transitioned out of the caregiving role. However, caregivers who institutionalized the PWD experienced decreasing role overload and captivity compared to the ones who continued with in-home care over time (Aneshensel et al., 1995). Further study is needed to assess how subjective stressors are related to caregiving transitions that occur either through institutionalization of the PWD or relinquishing care to another family member (Alspaugh, Stephens, Townsend, Zarit, & Greene, 1999). Based on prior research, care transition was examined for its impact on the longitudinal subjective stress in the current study.
Care and non-care stressors
Care-related stressors are often anchored within the needs, symptoms, and decline of the PWD. Perhaps most obvious in the context of dementia is the memory loss experienced by the PWD. Managing memory problems and consistently reorienting a confused PWD may become quickly overwhelming for caregivers, particularly when combined with other care tasks. A PWDs inability to partake independently in activities of daily living (ADL) is another source of stress for caregivers (Giebel, Challis, & Montaldi, 2014). Likewise, PWDs resistance to care has been linked to overload while caregivers’ appraisal of resistance to care is predictive of overload and captivity (Fauth, Femia, & Zarit, 2016). Similar to resistance to care are disruptive behavior problems and symptoms of dementia (BPSD). Deimling and Bass (1986) found that cognitive incapacity of the PWD had a less important direct effect on caregiving stress than BPSD. Caregivers experience other non-care stressors throughout daily life that are critical to well-being. A study on spouses of persons with mild cognitive impairment (MCI) indicates that non-care related stressors are significantly related to higher daily negative affect (Savla, Roberto, Blieszner, Cox, & Gwazdauskas, 2011), however limited research has sought to link non-care stressors to overload and captivity.
Caregiver Resources
Caregivers maintain a variety of resources to assist with managing stress. Caregivers consistently cite the need to take a break from care duties and responsibilities. Thus, the ability to utilize respite is a major person-level resource for caregivers. This need for respite is often met by adult day services (ADS), which provides out-of-home care for older adults with a variety of impairments. ADS significantly decreases the number of hours that caregivers spend providing care, and is linked to decreases in overload, worry, and strain (Gaugler et al., 2003). Caregivers find alternative forms of respite, and benefit from time to take breaks from caregiving. The degree to which caregivers feel that they can take a break from care is an important, yet understudied resource.
The caregiver-care-recipient relationship dyad is an important resource for caregivers. Caregivers are often spouses or adult children who had a pre-existing relationship prior to becoming a caregiver for the PWD. The nature of these relationships inevitably shifts within the context of dementia. Thus, the loss of intimate exchange, past and current quality of relationship are linked to caregiver burden and mental health outcomes (Adams, McClendon, & Smyth, 2008; Davis, Gilliss, Deshefy-Longhi, Chestnutt, & Molloy, 2011; Quinn, Clare, & Woods, 2009; Steadman, Tremont, & Davis, 2007). Less research has linked relationship quality to subjective care stress; one study found that for caregivers with higher relationship quality, increased care-recipient disability was related to higher levels of overload (Lawrence, Tennstedt, & Assmann, 1998). However, it is likely that caregivers with higher relationship quality may view this relationship as a positive resource, and therefore exhibit lower levels of captivity and overload across time. A better understanding of such associations is critical for the development of dyadic interventions.
Caregivers provide care within the larger context of other social and family relationships. Caregivers report greater role overload when they perceive that they have lower levels of social support (Mitchell & Knowlton, 2012). Likewise, family support has moderating effects on the association between caregivers’ role overload and depression (Choi et al., 2016). Caregivers experiencing family conflict have significantly higher perceived burden and poorer mental health than caregivers without family conflict (Strawbridge & Wallhagen, 1991). Grown children caring for aging parents are likely to experience sibling tension (Suitor, Gilligan, Johnson, & Pillemer, 2014), and family tension may increase during care transitions, particularly at the end of life (Christ, Behar, Messner, & Behar, 2015). Little is known about how resources at the family level have longitudinal associations with subjective care stress. Such an exploration would allow for researchers to understand the long-term association of family-level resources, and assist in the development of family-based caregiver interventions.
The Present Study
The first aim of this study is to confirm longitudinal trajectories of role overload and role captivity over 12 months based on prior work (Aneshensel et al., 1995). The second aim is to understand what aspects of caregiving are predictive of longitudinal changes in subjective stress. Given the major changes in caregiver health associated with caregiving transitions (e.g., Liu, Kim, & Zarit, 2015), transitions were first taken into account as main effects and then moderators of the time variable, objective stressors, and caregiving resources. Under the guidance of the stress process model, objective stressors at baseline were modeled as predictors of subjective stress over time. We then considered resources at the personal, dyadic, and family level at baseline and their effect on subjective stress over time.
Hypothesis 1: Fewer care-related and non-care stressors at baseline are associated with overall lower levels and steeper declines in role overload and captivity across time.
Hypothesis 2: Caregivers with more person-level resources specifically, more time away from caregiving and caregivers who report greater positive daily events will show lower overall role overload and captivity, and greater declines in role overload and captivity across time.
Hypothesis 3: At the dyadic level, higher caregiver-care recipient relationship quality at baseline will be associated with lower levels, and greater declines in role overload and captivity across time.
Hypothesis 4: At the family-level, less family conflict and greater family support will be associated with lower levels, and greater declines in role overload and captivity across time.
Methods
Participants and procedures
Participants were 184 caregivers providing primary care to a person clinically diagnosed with a type of dementia from the Daily Stress and Health (DaSH) Study (Zarit, Kim, Femia, Almeida, & Klein, 2014). Caregivers had to be living in the same household as the PWD. As an initial step, in-person interviews were conducted at the caregivers’ home, where caregivers signed consent forms, provided socio-demographic information, and baseline data on caregiving situations, resources, and well-being. Caregivers completed a daily phone interview over 8 consecutive days, providing data on daily stressors, mood, health and well-being. Follow-up phone interviews were conducted at 6 months, and 12 months to obtain repeated measures on caregiving situations and subjective stressors. Caregivers were paid a small honorarium for their participation.
We accounted for transitions that may occur for caregivers across time; we defined caregiving transition as turning care over to someone else or nursing home/ institutional placement. Caregivers who experienced bereavement (n = 31) at either 6 or 12 months were not included in the study. The final working sample included N = 153 caregivers a) whose relatives were living between baseline and at one year follow-up and b) who continued to be primary caregivers or experienced one of the aforementioned types of caregiving transition.
Measures
Subjective Stress.
Role captivity and role overload, were assessed at baseline, 6 and 12 months. Role captivity (e.g., “I feel trapped by my relative’s illness”) was measured by a 3-item scale that measured caregivers’ feelings that their involvement exceeded what they were willing to provide (α = .83; 4-point response scale ranging from 1 = none of the time to 4 = all of the time). Higher scores indicated the caregiving role was unwanted (Aneshensel, Pearlin, Mullan, Zarit, & Whitlatch, 1995; Pearlin, Mullan, Semple, & Skaff, 1990). Role overload (e.g., “I have more things to do than I can handle” was measured by a 3-item scale that assessed caregivers’ subjective appraisal of the time and effort they made in providing care (α = .63; 4-point response scale ranging from 1 = none of the time to 4 = all of the time).
Time.
Time in the study was coded in numeric months to represent length of participation and the corresponding time of data collection in the study. The baseline interview was coded as 0, the 6-month interview was coded as 6, and the 12-month interview was coded as 12.
Caregiving transition.
We took into account whether or not caregivers transitioned out of the caregiving role at any point in the study. This transition was coded to indicate any types of transition reported at either 6- or 12-month interview (1 = had a transition and 0 = did not have a transition), such that the caregiver was no longer providing primary care to their living PWD. Among caregivers who indicated a transition out of the caregiving role (n = 31), PWDs were then cared for either informally by another family member (n = 2) or formally in institutional settings such as nursing homes (n = 29).
Adult Day Service.
Caregivers reported the total number of days per week at baseline that they used ADS for the PWD (M = 3.89 days, SD = 1.15 days).
Care-related stressors.
Care-related stressors including memory problems, ADL needs, and behavior and psychological symptoms of dementia (BPSD) were evaluated at baseline. Memory problems (e.g., “In the past week, did your relative have difficulty concentrating on a task?”) were assessed using 7 items (on a 5-point response scale ranging from 1 = No, did not occur to 5 = Often, every day, α = .70) from the Revised Memory and Behavior Problems Checklist (Teri et al., 1992). Caregivers reported how often each item had occurred in the past week. The frequency of memory problems correlated well with findings from cognitive screening tests such as the MMSE (Aneshensel, et al., 1995). ADL needs assessed the PWD’s ability to eat, dress, groom themselves, bathe and shower, use the toilet, and get in and out of bed (13 items; 4-point response scale ranging from 1 = does not need help to 4 = cannot do without help; coded so that higher scores indicated greater ADL needs and dependency; α = .83; Katz, Ford, Moskowitz, Jackson, & Jaffe, 1963; Lawton & Brody, 1969). BPSD were assessed daily using Daily Record of Behavior (DRB) on 19 behavior items (e.g., “Did your relative struggle, resist or refuse to wash, bathe or shower?”) over a 24-hour time frame (Fauth, et al., 2006; Femia, Zarit, Stephens, & Greene, 2007). The average level of daily BPSD over 8 days was calculated across the daily interview period at baseline.
Non-care stressors.
Non-care stressors were assessed using the Daily Inventory of Stressful Events (DISE; Almeida, Wethington, & Kessler, 2002). Caregivers reported occurrences (1 = yes; 0 = no) of eight events (e.g., “Did you experience anything else that was stressful last night or today?”) over the previous 24-hour period. Caregivers were specifically instructed to report events they found stressful other than those encountered when assisting their relative. The average level of daily non-care stressors was calculated across the daily interview period at baseline.
Positive events.
Positive events were assessed using 5 items (e.g., “Did you share a good laugh with someone last night or today?”) drawn from the DISE (Almeida et al., 2002). Caregivers reported occurrences of five positive experiences during the past 24 hours. The average level of daily positive events was calculated across the daily interview period at baseline.
Time to take a break.
Caregivers responded on a 4-point scale (1 = None of the time to 4 = Often) on the typical time away from care responsibilities in a typical week. The measure was administered repeatedly at baseline, 6- and 12-month.
Dyadic relationship quality at baseline.
Caregivers reported relational closeness (e.g., “Taking everything into consideration, how close do you feel in the relationship between you and your relative?) on a 4-point Likert scale (1 = Not at all to 4 = Very) at baseline. A mean score was calculated with higher scores indicated better dyadic relationship quality.
Family conflict and lack of support at baseline.
A family conflict scale used 6 items to assess disagreement from family members on the nature of the PWDs illness and how care should be provided (e.g., “How much disagreement have you had with anyone in your family concerning the cause of your relative’s symptoms and behaviors?”). The lack of support scale used 3 items to assess other family members’ lack of assistance on caregiving (e.g., “how much disagreement have you had with anyone in your family because they don’t give you enough help?”). Caregivers responded to a 4-point response scale ranging from 1 = None to 4 = A lot to all items at baseline. Mean item scores were calculated for each scale.
Data Analysis Strategy
The data analysis for this paper was generated using SAS software, Version 8 of the SAS System for Unix. Analyses were conducted in a series of steps to explore role captivity and overload trajectories and associations over time. First, the unconditional growth curve models with time as the only predictor were fit to explore the nature of captivity and overload trajectories. In the level-1 within-person model, caregiver’s subjective stressor was specified as:
| (1) |
where subjective stressor for caregiver i at time t was a function of an intercept (, baseline subjective stressor), linear time (,within-person association between time and subjective stressor), and the within-person residual, , whose variance was and assumed to be homogeneous across persons. In the level-2 model, the individual specific intercepts and slopes were specified as:
| (2) |
where βs are population-level parameters, representing the mean intercept () and mean slope () of the subjective stressor trajectory pooling over all caregivers in the sample. are unexplained between-person differences in the intercept with a variance, , representing the degree of individual variability around the mean intercept.
Second, the effect of caregiving transition on the outcomes was explored by modeling it as a level-2 predictor in equations (2). If caregiving transition had significant main effect and/or interaction effects with the time variable on the outcomes, these effects were kept in the base model for hypothesis testing in all ensuing analyses. The level-1 model remained the same. The level-2 model was specified as:
| (3) |
Third, models were fit by adding memory problems, ADL needs, BPSD, and non-care stressors at baseline into the level-2 model (3), while fitting the same level-1 model. Hypothesis 1 was tested by fully evaluating the main effect of stressors and their interactions with the time variable, the main effect of transition, and its interaction with time. Nonsignificant interactions were trimmed. The level-2 model was specified as:
| (4) |
Finally, person-level, dyadic-level, and family-level resources were added to the stressor model sequentially. Hypothesis 2–4 were tested by estimating the main effects of person-, dyadic-, and family-level resources and their interactions with time, transition, and time*transition. Nonsignificant main effects and interactions were trimmed before each subsequent step of hypothesis testing. The level-1 equation remained the same. The level-2 equations in the full model were specified as:
| (5) |
where βs are population-level parameters; the person-specific intercept, , from equation (5) is now modeled as functions of objective caregiving stressors and resources, while controlling for caregiving transitions; the person-specific linear time slope, , is also modeled as functions of objective caregiving stressors and resources, while controlling for caregiving transitions. is between-person differences in the intercept with a variance, .
Results
Descriptive statistics are presented in Table 1. Participants were mostly female caregivers (mean age= 60) providing care to a spouse or parent with dementia. Unconditional growth curve models show that role captivity (β = −0.01, p = .01) and overload (β = −0.007, p = .05) decreased over time among all caregivers. After caregiving transition status was added, the model showed that caregivers who experienced a transition over the course of the study had higher levels of captivity at baseline (β = 0.37, p = .04) and had decreasing captivity across time (β = −0.04, p < .0001). Caregivers who transitioned declined in overload over time (β = −0.06, p < .0001). Significant effects of caregiving transitions were thus kept in the base model for hypothesis testing. Parameter estimates for the caregiving transition models are presented in Table 2; parameter estimates from the full models for hypotheses testing are presented in Table 3.
Table 1.
Caregiver Characteristics at Baseline and Caregiving Transition over time (N = 153)
| M or Freq | SD or % | Range | |
|---|---|---|---|
| Age | 60.65 | 10.84 | 39 – 89 |
| Female | 133 | 86.93 | |
| Spouse | 50 | 32.68 | |
| Child | 94 | 61.44 | |
| Educationa | 4.38 | 1.18 | 1 – 6 |
| Married with a partner | 99 | 64.71 | |
| Duration of careb | 62.67 | 46.27 | 2 – 216 |
| Number of ADS days per week | 3.89 | 1.15 | 2 – 5 |
| Memory problemsc | 3.14 | 0.89 | 1 – 5 |
| ADL dependency of IWDsd | 3.00 | 0.50 | 2 – 4 |
| BPSD stressorse | 7.40 | 7.79 | 0 – 32 |
| Non-care stressorsf | 2.00 | 1.57 | 0 – 6 |
| Positive eventsg | 3.10 | 1.36 | 0 – 6 |
| Time to take a breakh | 2.10 | 0.78 | 1 – 4 |
| Relationship qualityi | 3.59 | 0.66 | 1 – 4 |
| Family conflictj | 3.39 | 0.65 | 1 – 4 |
| Family supportk | 3.25 | 0.97 | 1 – 4 |
| Caregiving transition at 6 months | 37 | 0 – 1 | |
| Caregiving transition at 12 months | 25 | 0 – 1 |
Note. ADS = adult day services; IWD = individual with dementia; ADL = activities of daily living.
Measured on a 6-point scale: 1 (less than high school) to 6 (post college degree).
Measured in months.
Measured as the mean of 7 items on a 5-point scale: 1 (no, did not occur) to 5 (often, everyday).
Measured as the mean of 13 ADL items on a 4-point scale: 1 (does not need help) to 4 (cannot do without help).
Measured as the count of 19 BPSD stressors.
Measured as the count of 8 non-care related stressful events.
Measured as the count of 5 positive events.
Measured on 1 item on a 4-point scale: 1 (never) to 4 (often).
Measured as the mean of 2 items on a 4-point scale: 1 (not at all) to 4 (very).
Measured as the mean of 6 items on a 4-point scale: 1 (a lot) to 4 (none).
Measured as the mean of 3 items on a 4-point scale: 1 (a lot) to 4 (none).
Table 2.
Effects of Caregiving Transition on Trajectories of Role Captivity and Overload
| Role Captivity |
Role Overload |
|
|---|---|---|
| Effect | Estimate (s.e.) | Estimate (s.e.) |
| Intercept | 2.03 (0.07)*** | 2.78 (0.06)*** |
| Time | 0.00 (0.00) | 0.00 (0.00) |
| Transition | 0.37 (0.17)* | 0.27 (0.15) |
| Time × Transition | −0.04 (0.01)*** | −0.06 (0.01)*** |
Notes. Transition was coded as 1 = had a caregiving transition over 12 months, and 0 = did not have transitions over 12 months.
Time was coded as 0 = baseline, 6 = 6 months, and 12 = 12 months, representing the actually months in the study.
p ≤ .05
p ≤ .01
p ≤ .001
Table 3.
Full Models of Role Captivity and Overload over 12 Months
| Role Captivity |
Role Overload |
|
|---|---|---|
| Effect | Estimate (s.e.) | Estimate (s.e.) |
| Intercept | 3.99 (0.59)*** | 2.84 (0.44)*** |
| Timea | −0.01 (0.00) | 0.00 (0.00) |
| Time to take breaksb | n/a | −0.12 (0.03)*** |
| Transition | 0.09 (0.18) | −1.05 (0.69) |
| Time × Transition | −0.09 (0.02)*** | −0.02 (0.03) |
| Time × Transition × Non-care stressorsc | 0.02 (0.01)*** | n/a |
| Memory problemsc | 0.03 (0.07) | 0.08 (0.06) |
| ADL dependency of PWDsc | 0.00 (0.12) | 0.14 (0.10) |
| BPSD stressorsc | 0.01 (0.01) | 0.01 (0.01) |
| Non-care stressors | 0.04 (0.04) | 0.08 (0.03)* |
| Total # of ADS daysc | −0.13 (0.05)* | n/a |
| Relationship qualityc | −0.28 (0.09)** | −0.17 (0.08)* |
| Family supportc | −0.21 (0.06)** | n/a |
| Transition × Relationship quality | n/a | 0.37 (0.20)† |
Notes. Non-significant 2-way and 3-way interactions were trimmed; ADL= Activities of Daily Living; PWD=Person with dementia; BPSD= Behavior problems and symptoms of dementia; ADS= Adult Day Services.
Coded as 0, 6, 12 to reflect months between interviews over time.
This was a time-varying variable.
These were time invariant variables measured only at baseline.
p ≤ .1
p ≤ .05
p ≤ .01
p ≤ .001
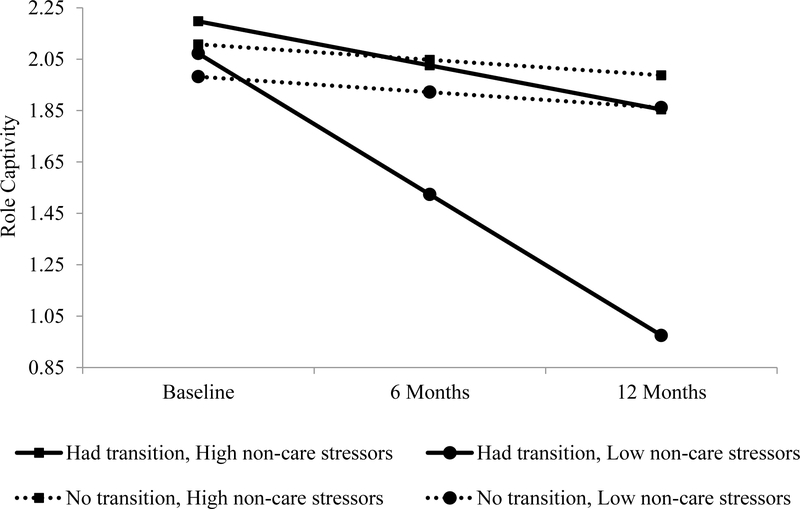
Hypothesis 1 was tested by adding caregiving stressors (memory problems, ADL needs, and BPSD) and non-care stressors to the model. Hypothesis 1 was partially supported. No significant effects were found for care-related stressors on role overload and role captivity. High non-care related stressors at baseline were associated with greater levels of overload across 12 months (β = 0.08, p = .01), but did not have a main effect on captivity (β = 0.04, p > .05). We found a significant 3-way interaction between non-care stressors, care transition, and time (β = 0.02, p = .0002). Figure 2 shows that among caregivers who experienced a transition, those who had low non-care stressors at baseline experienced the greatest decrease in captivity over time.
Figure 2.
Model predicted effects of non-care stressors at baseline and caregiving transitions on role captivity trajectory among caregivers over 12 months. Among caregivers who experienced a transition, those who had high non-care stressors at baseline experienced the greatest decrease in captivity over time.
Hypothesis 2 was tested by adding predictors of person-level resources (i.e., positive events at baseline and ADS use at baseline, and time to take breaks over time) into the caregiving stressor model. Hypothesis 2 was supported in that ADS use had a significant main effect on captivity (β = −0.13, p = .01) such that using more ADS days at baseline was associated with lower levels of captivity over 12 months. Moreover, having time to take breaks from care was significantly associated with lower levels of overload across 12 months among all caregivers (β = −0.12, p = .0001).
Hypothesis 3 was tested by adding dyadic-level resources (i.e., relationship quality at baseline) into the person-level resource model. Hypothesis 3 was supported in that higher relationship quality at baseline was associated with lower levels of captivity (β = −0.28, p = .002) and lower role overload (β = −0.17, p = .03) over time.
Hypothesis 4 was tested by adding family conflict and family support at baseline to the dyadic-level resource model. Hypothesis 4 was partially supported in that family support was associated with lower levels of captivity across time (β = −0.21, p = .001), but not overload.
Discussion
We found associations between subjective stressors and resources at the person-, dyad-, and family-level. A particularly novel finding was the association between non-care stressors and subjective stressors, specifically, when caregivers reported higher non-care stressors at baseline, they reported higher levels of overload at 12 months. Stressors unrelated to caregiving contribute to subjective stressors (Austrom et al., 2014). Our study suggests that non-care stressors have a longitudinal association with role-overload, but not role captivity. Amidst more non-care stressors, caregivers may be more inclined to feel overwhelmed and thus present greater levels of role overload across time. These findings indicate the interdependence of the caregiving role and non-caregiving roles, the notion that experiences in one role essentially “spill over” to affect experiences of the other roles In line with Stephens & Franks, (1995), results suggest that negative spillover may occur from non-care stressors that spill directly into the caregiving role. These findings support the notion that experiences within and outside of the caregiving role have associations with subjective stressors. The impact of non-care stressors on caregiving has been overlooked in comparison to care-related stressors.
Among caregivers who experienced a transition, those who had high non-care stressors at baseline experienced the greatest decrease in captivity over time. Caregivers who transitioned out of the care role experienced greater declines in captivity when they had high non-care stressors as opposed to low non-care stressors. Higher non-care stressors allow for caregivers to experience declines in captivity amidst their transition out of caregiving. Caregivers who transition out of their role, but have low non-care stressors, did not exhibit as steep of a decline in captivity. The finding suggests that encroaching life events that are non-care related may have a greater detrimental impact than the stressors from caregiving itself.
Our study indicates the importance of person-level resources that allow caregivers some time away from caregiving, specifically ADS use and time to take breaks from care. Both of these resources fall under the broader theme of caregiver respite, which has been widely cited as beneficial for caregiver health and well-being (Gaugler, Jarrott, et al., 2003). Our study indicates the value of two different types of respite, ADS use, which is a formal service, and time to take breaks from caregiving, which was based on caregivers’ appraisal of their ability to step away from caregiving. ADS use, which was measured as the objective use of ADS at baseline, was associated with lower overall levels of captivity. Respite care has been described by caregivers as offering both normality and freedom (Ashworth & Baker, 2000), thus, the consistent availability of a formal service, such as ADS, may offer a reliable form of respite that allows caregivers to feel less captivated by their role. In light of a recent review (Maayan, Soares-Weiser, & Lee, 2014) which indicates the need for well-designed trials and high-quality research to assess the benefits of respite care, our findings indicate that subjective stressors are an important consideration, and potential outcome to examine in future studies.
In contrast to ADS use, having time to take breaks from care was measured more subjectively, and was associated with lower levels of overload. These findings warrant further investigation into what factors allow caregivers to take restorative breaks from care, independent of formal respite services (Watts & Teitelman, 2005). These efforts may be particularly useful for caregivers living in rural areas, where formal respite services are not readily available, or caregivers with limited financial means. Likewise, utilization rates of formal respite services are relatively low (Chappell, Reid, & Dow, 2001) which may justify further attention be paid to alternative or informal mechanisms by which caregivers may take a break from care, or feel as though they are able to take a break from care.
Hypothesis 3 sought to examine the association between subjective stressors and dyadic-level resources. At the dyadic level, higher relationship quality between the caregiver and PWD was associated with lower levels of captivity and overload across time. Findings indicate that the relational context in which caregiving takes place has important implications for caregiver well-being (Quinn et al., 2009). While some work has pointed to poor relationship quality as a risk factor for institutionalization (Winter, Gitlin, & Dennis, 2011), we found that positive relationship quality is an important resource for caregivers. It is essential, therefore, to understand what factors influence caregivers’ perceptions of relationship quality with the PWD. This inquiry could be useful in building dyadic intervention efforts that preserve relationship quality between caregivers and PWDs.
Finally, we sought to test family-level resources associated with subjective stressors. Specifically, greater family support was related to lower levels of role captivity across time; caregivers who feel they have greater support from family members feel less obligated to their caregiving role. Findings build on previous work by (Mitrani, Feaster, McCabe, Czaja, & Szapocznik, 2005) (2006) which argues that family functioning significantly contributes to caregiver distress. These results warrant the use of a family system’s perspective to understand and advance knowledge regarding the role that other family members play in the caregiver stress process (Mitrani, et al., 2006). Moreover, facilitating family support is a logical focus for clinicians, and intervention efforts.
The findings of this study must be considered within several limitations. First, we only assessed caregivers across 12 months, a longer period of assessment would allow for us to assess more instances of change in role captivity and role overload. Next, we recruited participants from ADS programs. The results of our study therefore cannot be generalized to caregivers who do not utilize ADS. Further, caregivers who utilize ADS may hold inherent biases that are different from caregivers who do not use such services. Nonetheless, this study contributes important information about what resources are associated with changes in subjective stressors across time. Specifically, results reveal important associations between care transitions and subjective stressors which may be useful in identifying caregivers who are likely to relinquish care. Moreover, findings may guide intervention efforts which seek to address caregiver well-being. Ultimately, this work contributes to the goal of allowing caregivers to provide sufficient, sustainable care that does not come at the cost of their own well-being.
Figure 1.
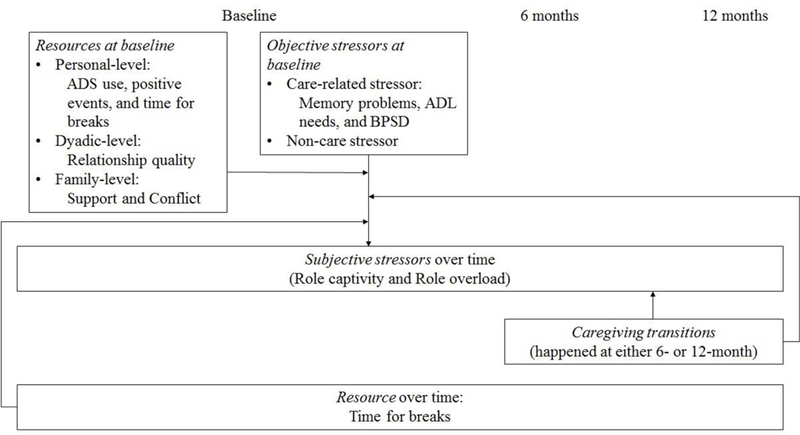
Conceptual model
Acknowledgments
Funding
This work was supported by the National Institute of Aging at the National Institute of Health (R01 AG031758).
References
- Adams KB, McClendon MJ, & Smyth KA (2008). Personal losses and relationship quality in dementia caregiving. Dementia, 7(3), 301–319. 10.1177/1471301208093286 [DOI] [Google Scholar]
- Alspaugh MEL, Stephens MAP, Townsend AL, Zarit SH, & Greene R (1999). Longitudinal patterns of risk for depression in dementia caregivers: Objective and subjective primary stress as predictors. Psychology and Aging, 14(1), 34–43. [DOI] [PubMed] [Google Scholar]
- Aneshensel CS, Pearlin LI, Mullan JT, Zarit SH, & Whitlatch CJ (1995). Profiles in Caregiving: The Unexpected Career. Academic Press. [Google Scholar]
- Ashworth M, & Baker AH (2000). ‘Time and space’: carers’ views about respite care. Health & Social Care in the Community, 8(1), 50–56. 10.1046/j.1365-2524.2000.00221.x [DOI] [PubMed] [Google Scholar]
- Austrom MG, Lu YY-F, Perkins AJ, Boustani M, Callahan CM, & Hendrie HC (2014). Impact of Non-caregiving Related Stressors on Informal Caregiver Outcomes. American Journal of Alzheimer’s Disease and Other Dementias, 29(5), 426–432. 10.1177/1533317513518652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chappell NL, Reid RC, & Dow E (2001). Respite reconsidered: A typology of meanings based on the caregiver’s point of view. Journal of Aging Studies, 15(2), 201–216. 10.1016/S0890-4065(00)00026-8 [DOI] [Google Scholar]
- Choi K, Choi DR, Zang DY, Park YS, Kang SY, Yoon H, … Lee HJ(2016). Moderating Effects of Optimism and Family Support on the Depression of Family Caregivers of Cancer Patients. Korean Journal of Health Promotion, 16(3), 192–202. 10.15384/kjhp.2016.16.3.192 [DOI] [Google Scholar]
- Christ GH, Behar LC, Messner C, & Behar L (2015). Handbook of Oncology Social Work: Psychosocial Care for People with Cancer. Oxford University Press, Incorporated. [Google Scholar]
- Davis LL, Gilliss CL, Deshefy-Longhi T, Chestnutt DH, & Molloy M (2011). The nature and scope of stressful spousal caregiving relationships. Journal of Family Nursing, 17(2), 224–240. 10.1177/1074840711405666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deimling GT, & Bass DM (1986). Symptoms of Mental Impairment Among Elderly Adults and Their Effects on Family Caregivers. Journal of Gerontology, 41(6), 778–784. 10.1093/geronj/41.6.778 [DOI] [PubMed] [Google Scholar]
- Fauth EB, Femia EE, & Zarit SH (2016). Resistiveness to care during assistance with activities of daily living in non-institutionalized persons with dementia: associations with informal caregivers’ stress and well-being. Aging & Mental Health, 20(9), 888–898. 10.1080/13607863.2015.1049114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler JE, Edwards AB, Femia EE, Zarit SH, Stephens M-AP, Townsend A, & Greene R (2000). Predictors of Institutionalization of Cognitively Impaired Elders: Family Help and the Timing of Placement. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 55(4), P247–P255. 10.1093/geronb/55.4.P247 [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Jarrott SE, Zarit SH, Stephens MAP, Townsend A, & Greene R (2003). Respite for dementia caregivers: The effects of adult day service use on caregiving hours and care demands. INTERNATIONAL PSYCHOGERIATRICS, 15(1), 37–58. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Jarrott SE, Zarit SH, Stephens M-AP, Townsend A, & Greene R (2003). Adult day service use and reductions in caregiving hours: effects on stress and psychological well-being for dementia caregivers. International Journal of Geriatric Psychiatry, 18(1), 55–62. 10.1002/gps.772 [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Kane RL, Kane RA, Clay T, & Newcomer R (2003). Caregiving and Institutionalization of Cognitively Impaired Older People: Utilizing Dynamic Predictors of Change. The Gerontologist, 43(2), 219–229. 10.1093/geront/43.2.219 [DOI] [PubMed] [Google Scholar]
- Giebel CM, Challis DJ, & Montaldi D (2014). A revised interview for deterioration in daily living activities in dementia reveals the relationship between social activities and well-being. Dementia, 1471301214553614. 10.1177/1471301214553614 [DOI] [PubMed] [Google Scholar]
- Lawrence RH, Tennstedt SL, & Assmann SF (1998). Quality of the caregiver–care recipient relationship: Does it offset negative consequences of caregiving for family caregivers? Psychology and Aging, 13(1), 150–158. 10.1037/0882-7974.13.1.150 [DOI] [PubMed] [Google Scholar]
- Lazarus RSL, & Folkman S (1984). Stress, Appraisal, and Coping. Springer Publishing Company. [Google Scholar]
- Maayan N, Soares-Weiser K, & Lee H (2014). Respite care for people with dementia and their carers In Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd. Retrieved from http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD004396.pub3/abstract [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell MM, & Knowlton A (2012). Caregiver Role Overload and Network Support in a Sample of Predominantly Low-Income, African-American Caregivers of Persons Living with HIV/AIDS: A Structural Equation Modeling Analysis. AIDS and Behavior, 16(2), 278–287. 10.1007/s10461-011-9886-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitrani VB, Feaster DJ, McCabe BE, Czaja SJ, & Szapocznik J (2005). Adapting the Structural Family Systems Rating to Assess the Patterns of Interaction in Families of Dementia Caregivers. The Gerontologist, 45(4), 445–455. 10.1093/geront/45.4.445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Menaghan EG, Lieberman MA, & Mullan JT (1981). The Stress Process. Journal of Health and Social Behavior, 22(4), 337–356. 10.2307/2136676 [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, & Skaff MM (1990). Caregiving and the Stress Process: An Overview of Concepts and Their Measures. The Gerontologist, 30(5), 583–594. 10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Quinn C, Clare L, & Woods B (2009). The impact of the quality of relationship on the experiences and wellbeing of caregivers of people with dementia: A systematic review. Aging & Mental Health, 13(2), 143–154. 10.1080/13607860802459799 [DOI] [PubMed] [Google Scholar]
- Savla J, Roberto KA, Blieszner R, Cox M, & Gwazdauskas F (2011). Effects of Daily Stressors on the Psychological and Biological Well-being of Spouses of Persons With Mild Cognitive Impairment. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 66B(6), 653–664. 10.1093/geronb/gbr041 [DOI] [PubMed] [Google Scholar]
- Steadman PL, Tremont G, & Davis JD (2007). Premorbid Relationship Satisfaction and Caregiver Burden in Dementia Caregivers. Journal of Geriatric Psychiatry and Neurology, 20(2), 115–119. 10.1177/0891988706298624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens MA, & Franks MM (1995). Spillover between daughters’ roles as caregiver and wife: interference or enhancement? The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 50(1), P9–P17. [DOI] [PubMed] [Google Scholar]
- Strawbridge WJ, & Wallhagen MI (1991). Impact of Family Conflict on Adult Child Caregivers. The Gerontologist, 31(6), 770–777. 10.1093/geront/31.6.770 [DOI] [PubMed] [Google Scholar]
- Suitor JJ, Gilligan M, Johnson K, & Pillemer K (2014). Caregiving, Perceptions of Maternal Favoritism, and Tension Among Siblings. The Gerontologist, 54(4), 580–588. 10.1093/geront/gnt065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts JH, & Teitelman J (2005). Achieving a restorative mental break for family caregivers of persons with Alzheimer’s disease. Australian Occupational Therapy Journal, 52(4), 282–292. 10.1111/j.1440-1630.2005.00524.x [DOI] [Google Scholar]
- Winter L, Gitlin LN, & Dennis M (2011). Desire to Institutionalize a Relative With Dementia: Quality of Premorbid Relationship and Caregiver Gender. Family Relations, 60(2), 221–230. 10.1111/j.1741-3729.2010.00644.x [DOI] [Google Scholar]
- Zarit SH, Kim K, Femia EE, Almeida DM, & Klein LC (2014). The Effects of Adult Day Services on Family Caregivers’ Daily Stress, Affect, and Health: Outcomes From the Daily Stress and Health (DaSH) Study. The Gerontologist, 54(4), 570–579. 10.1093/geront/gnt045 [DOI] [PMC free article] [PubMed] [Google Scholar]