Abstract
Many people living with Chronic Obstructive Pulmonary Disease (COPD) have low general health literacy; however, there is little information available on these patients’ eHealth literacy, or their ability to seek, find, understand, and appraise online health information and apply this knowledge to address or solve disease-related health concerns. A nationally representative sample of patients registered in the COPD Foundation’s National Research Registry (N=1,270) were invited to complete a web-based survey to assess socio-demographic (age, gender, marital status, education), health status (generic and lung-specific health-related quality of life), and socio-cognitive (social support, self-efficacy, COPD knowledge) predictors of eHealth literacy, measured using the 8-item eHealth literacy scale (eHEALS). Over 50% of respondents (n=176) were female (n=89), with a mean age of 66.19 (SD = 9.47). Overall, participants reported moderate levels of eHealth literacy, with more than 70% feeling confident in their ability to find helpful health resources on the Internet. However, respondents were much less confident in their ability to distinguish between high- and low-quality sources of web-based health information. Very severe versus less severe COPD (β=4.15), lower lung-specific health-related quality of life (β=−0.19), and greater COPD knowledge (β=0.62) were significantly associated with higher eHealth literacy. Higher COPD knowledge was also significantly associated with greater knowledge (ρ=0.24, p=.001) and use (ρ=0.24, p=.001) of web-based health resources. Findings emphasize the importance of integrating skill-building activities into comprehensive patient education programs that enable patients with severe cases of COPD to identify high-quality sources of web-based health information. Additional research is needed to understand how new social technologies can be used to help medically underserved COPD patients benefit from web-based self-management support resources.
Keywords: eHealth literacy, chronic obstructive pulmonary disease (COPD)
Chronic Obstructive Pulmonary Disease (COPD) is the 3rd leading cause of death in the United States (U.S.; American Lung Association [ALA], 2014) and stands as a leading cause of mortality worldwide (Pauwels et al., 2015). This progressive chronic lung condition is characterized by a unique mixture of small airway disease (chronic bronchitis) and parenchyma destruction (emphysema) which leads to narrowing airways and permanent, irreversible lung damage (ALA, 2014). Symptoms of COPD include prolonged coughing, excessive mucus production, and dyspnea (i.e., shortness of breath) exacerbations (National Institutes of Health [NIH], 2013b), which are defined as sustained (≥ 48 hours) bouts of coughing or sputum production that leads to increased medication use. Patients who regularly experience dyspnea exacerbations are more likely to disengage from activities of daily living due to fear of breathlessness, which can cause greater deconditioning that can aggravate dyspnea even further (Harris, Hayter, & Allender, 2008; Thorpe, Kumar, & Johnston, 2014). Mismanaged COPD exacerbations often also routinely lead to unplanned emergency room and hospital visits (Ambrosino & Vaghegginin, 2006; Guarscio et al., 2013; Menn et al., 2012).
In 2011, 12.7 million U.S. adults were diagnosed with COPD, and an additional 12 million were likely living with the disease without a formal diagnosis (NIH, 2013a). Exposure to tobacco smoke is the primary risk factor for COPD (NIH, 2013b), with nearly 50% of smokers developing COPD at some point in their lives (Mannino, Watt, & Hole, 2006; Rennard & Vestbo, 2006). Smoking cessation is the single most cost-effective intervention to stop the progression of COPD (Anthonisen et al., 1994; Ebrahim & Smith, 1997; Faulkner, Lenz, & Stading, 2006), yet patients living with COPD often continue to smoke due to peer pressure and lack of personal agency to autonomously quit (Eklund, Nilsson, Hedman, & Lindberg, 2012). Even if smoking cessation is realized, patients with COPD usually only experience marginal improvements in lung functioning one year after quitting (Pride, 2001). Today, patients admitted for COPD complications are now younger than they were at the turn of the century, and they are more likely to be female living with significant comorbidity (Dajczman et al., 2012) and low socioeconomic status (Gershon, Dolmage, Stephenson, & Jackson, 2012). Disadvantages such as living in lower-income housing has been noted as an independent risk factor for COPD-related hospitalizations (Kartaloğlu, 2013).
As COPD progresses, symptoms become more complex and often spiral into a challenging mix of interrelated physical, emotional, and psychosocial problems that are difficult to manage (Disler et al., 2012), often due to related co-morbidities (Sin, Anthonisen, Soriano & Agusti 2006; Fabbri, Luppi, Beghe & Rabe, 2008). Accordingly, COPD patients report high levels of depression, anxiety, and social isolation (Williams, Bruton, Ellis-Hill, & McPherson, 2007) as well as impaired disease-specific health-related quality of life (HRQoL) (Ghobadi, Ahari, Kameli & Lari, 2012; Jones et al., 2011). Unfortunately, adults living with COPD often face challenges when attempting to access healthcare services for treating their symptoms due to advanced age (Emery, 1994), limited mobility (Koster et al., 2004; Butcher, Meshke & Sheppard, 2004), and residing in geographically remote or medically underserved areas (Abrams, Vaughan-Sarrazin, Fan & Kaboli, 2011). Moreover, healthcare providers have limited opportunities to teach important self-management skills to patients, such as purse lipped and diaphragmatic breathing, stress management, and dyspnea prevention (Cicutto & Brooks, 2006; Hernandez, Balter, Bourbeau, & Hodder, 2009). Medical costs attributed to COPD-related complications could be reduced by up to 50% if patients were more actively involved in these types of self-management activities (Dalal, et al., 2010; National Business Coalition on Health, 2012).
Many COPD patients also have low health literacy (Roberts et al., 2008; Kale et al., 2015), in that, they possess a limited ability to obtain, process, and understand basic health information needed to make informed health decisions (Institute of Medicine, 2004). Low health literacy in COPD is associated with concerns about medication side-effects and the belief that COPD is not a chronic condition (Kale et al., 2015). Up to 15% of patients living with COPD are unable to understand and act on print-based patient education materials (Taylor et al. 2005), and only about 50% fully comply with prescribed pharmaceutical regimens (Restrepo et al., 2008). Many patients living with COPD experience challenges reading medication labels and interpreting medical test results (Disler, Gallagher, & Davidson, 2012), have difficulty remembering medical appointment times, and are unable to understand risk communication (Roberts et al., 2008). Omachi and colleagues (2013) found that COPD patients who score lowest on health literacy are 5 times more likely to report visiting an emergency room and 7 times more likely to be hospitalized, even after controlling for differences in socioeconomic status (SES). Furthermore, low health literacy in COPD isolates patients from the very support systems that help them control disease progression (Kiser et al., 2011). However, relatively little is known about health literacy in COPD. Most of the COPD literature examines medication use and effects of formal pulmonary rehabilitation on health outcomes, with fewer studies examining associations between patient health literacy and important process and functional outcomes (Roberts et al., 2008; Effing et al., 2012).
The importance of COPD knowledge to patient well-being is recognized by both patients and providers (Sadeghi, Brooks, & Goldstein, 2013). Global Initiative for Chronic Obstructive Lung Disease (GOLD) standards suggest that the intensity and content of educational messages for patients living with COPD should vary depending on individual disease severity (Pauwels et al., 2015). Research demonstrates that patients with COPD who develop shared treatment plans with their healthcare provider show higher self-efficacy and better adherence to self-management regimens (Bourbeau, Nault, & Dang-Tan, 2004; Heisler et al., 2003; Worth & Dhein, 2004). However, patients and their primary care providers often have conflicting views on the key messages that should be taken away following a consultation (Parkin & Skinner, 2003). Patients report numerous challenges communicating with healthcare providers due to the use of complex medical jargon, language barriers, limited time, and conflicting cultural perspectives (Roberts et al., 2008; Sadeghi et al., 2013; Taylor et al, 2007). Although these barriers exist, few literacy-sensitive patient education resources are available to support patients in learning more about the social and behavioral dimensions of COPD self-management (Clark et al., 2009; Kessler et al., 2006).
New technologies provide great opportunities to support patients who are living with COPD. Rapid advancements in mobile electronic devices (e.g., smartphones) and consumer shifts toward more interactive online tools (e.g., social media) have caused a spike in the availability of health communication technologies (El-Gayar, Timsina, Nawar, & Eid, 2013; Nguyen, Gill, Wolpin, Steele & Benditt, 2009). Interactive health communication technologies available on the Internet may provide older patients more opportunities to access and engage personalized self-management resources in the comfort and convenience of their own homes (Hall, Stellefson, & Bernhardt, 2012; Stellefson et al., 2013). Evidence suggests that effects of social media use on health outcomes are largely positive in chronic disease management, with few adverse consequences (Merolli, Gray, & Martin-Sanchez, 2013). Use of new technologies such as social media can change illness perceptions and influence how patients and informal caregivers approach disease management (Pousti, Urquhart, & Linger, 2014). Despite these promising benefits, older adults living with chronic conditions such as COPD experience progressive cognitive declines that contribute to difficulty when using technology (Hung, Wisnivesky, Siu & Ross, 2009). Small, observational pilot and usability studies indicate that patients living with COPD encounter some barriers when using eHealth tools for behavioral self-management (Nguyen et al., 2008), including challenges creating social media accounts and posting messages on interactive discussion forums (Stellefson et al., 2015). However, other studies in COPD note few technical issues experienced by patients when participating in internet-mediated walking programs (Moy et al., 2015) or when using mobile health (mHealth) tools to support self-management (Williams, Price, Hardinge, Tarassenko & Farmer, 2014). These conflicting results highlight the need to better understand specific needs and barriers to technology access, use, and engagement among people living with COPD (McCabe, McCann, & Brady, 2014).
Social media may help patients and caregivers make more informed decisions through more proactive patient engagement (Patel, Change, Greysen, & Chopra, 2015; Stellefson et al., 2013). However, existing cognitive and affective barriers, such as poor confidence and negative attitudes toward technology, can preclude patients from successfully using the Internet to learn about available treatments and adaptive coping skills. Also, there is potential for patient-provider interactions on social media to be incongruent with recommended health communication guidelines (Chretien & Kind, 2013). These findings highlight the importance of assessing how confident COPD patients are in terms of using the Internet and social media to make informed health decisions. eHealth literacy is defined as a patient’s capacity to seek, locate, understand, and evaluate health information from the Internet and apply such knowledge when addressing or solving a disease-related health concern (Norman & Skinner, 2006a). This multi-faceted, dynamic construct extends beyond traditional domains of health literacy and numeracy, and tends to vary based on an individual’s previous/current technology use, demographic and cognitive status, and health-related quality of life (HRQoL; Neter & Brainin, 2012; Norman & Skinner, 2006a). Because screening for eHealth literacy in clinical settings is usually impractical (Collins, Currie, Bakken, Vawdrey & Stone, 2012), it is very difficult for healthcare providers to determine the extent to which patients may experience challenges when using health information and communication technologies.
While some studies have tested the use of Internet-based self-management interventions among COPD patients (Nguyen, Carrieri-Kohlman, Rankin, Slaughter, & Stulbarg, 2005; Nguyen et al., 2013), we are not aware of any studies assessing eHealth literacy in patients living with COPD. Martinez and colleagues (2014) analyzed national survey data on Internet access and frequency of use among a convenience sample of patients living with COPD. Findings suggested that lack of Internet access was a marker of SES disparity and limited physical mobility, with more frequent Internet use associated with less somatic disease, greater numbers of COPD-related exacerbations, and less satisfaction with care. One additional finding was that patients who regularly accessed the Internet for information on COPD treatments reported more difficulty communicating with their healthcare providers, noting that providers often lacked empathy for their condition. While this study described correlates of Internet access and use among COPD patients, it did not measure eHealth literacy, nor was it designed to evaluate the type of Internet-based tools, such as social media, that COPD patients may use to access health information. Therefore, a fundamental gap exists with regard to understanding how confident COPD patients feel when using the Internet and social media to seek, find, appraise, and use health information to make informed health decisions. Exploring factors associated with eHealth literacy among COPD patients is important because patients can be hard-to-reach and medically underserved, which makes them ideal candidates for receiving Internet-based patient education and self-management support resources. However, there is a lack of attention given to factors that affect eHealth literacy in COPD, which may perpetuate inequities in health information accessibility that can contribute to negative health outcomes in this vulnerable patient population.
Considering these gaps in knowledge, the purpose of this non-experimental, cross-sectional survey was to explore the extent to which socio-demographic, health status, and socio-cognitive variables predicted eHealth literacy in a national sample of patients living with COPD. Building on the work of Martinez and colleagues (2014), Wilson’s models of information behavior (Wilson, 1999) and other models of information-seeking behavior (Nelson et al., 2004) were adapted to provide a theoretical basis for this investigation. These models describe how health information needs become activated by basic health stressors caused by a particular disease status. In this study, we sought to describe how basic health stressors were associated with COPD patients’ confidence in online health information seeking behaviors. Additionally, we examined the extent to which intervening variables, such as socio-demographic characteristics, were associated with eHealth literacy. Other mechanisms related to perceived health-related needs, such as knowledge, self-efficacy, and social support, were also thought to have some influence on patient eHealth literacy using various Internet-enabled devices. Figure 1 illustrates this conceptual model, which describes how patients living with COPD have a perceived need to seek health-related information about their condition based on its severity and their own general and disease-specific HRQoL. This perceived need is either reinforced or hindered by intervening variables (i.e., socio-demographic characteristics) and activating mechanisms (i.e., COPD-related knowledge, self-efficacy, social support). Using this conceptual framework of online health information seeking behavior, the following four research questions were explored:
Research Question #1 (RQ #1): To what extent do COPD patients use electronic devices, the Internet, and social media to locate and share health information?
Research Question #2 (RQ #2): What is the relationship between age and use (or non-use) of electronic devices and social media for health information among patients living with COPD?
Research Question #3 (RQ #3): What is the self-reported level of eHealth literacy among patients living with COPD?
Research Question #4 (RQ #4): What are the intervening variables (i.e., socio-demographic characteristics, Internet use) and activating mechanisms (i.e., COPD-related knowledge, self-efficacy, social support) associated with eHealth literacy among patients living with COPD?
Figure 1.
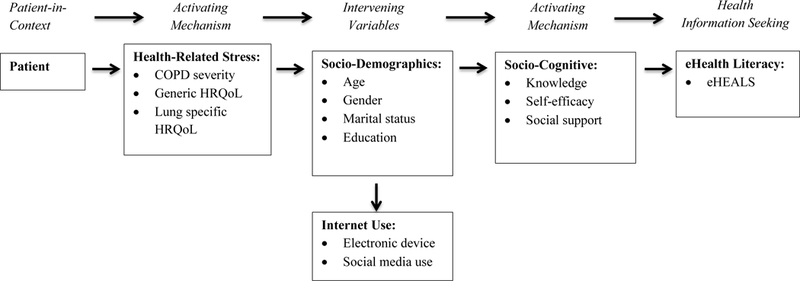
Conceptual model of health information seeking among patients living with COPD.
Method
Sample
Individuals diagnosed with COPD were recruited from the COPD Foundation (http://www.copdfoundation.org/)’s National Research Registry (CRR). Established in 2007 to facilitate COPD research, CRR is a confidential database of individuals, self-reporting physician or specialist diagnosed COPD. The CRR operates under the direction of the COPD Foundation’s Board of Directors, and is guided by an Oversight Committee comprised of leaders in the medical, ethical, scientific, and COPD communities. Individuals enrolled in the CRR have the opportunity to participate in research after completing a 6-page baseline survey document, along with consent documents stating that they agree to be contacted about potential research opportunities that include patients diagnosed with COPD. All individuals registered in the CRR over the age of 40 with a valid email address were eligible to participate (n=1,270). While COPD develops most often in adults over 40 (NIH, 2013c), the majority of eligible patients were over the age of 60 (n=981, 77.24%) and female (n=703, 55.35%). Most eligible patients in the CRR were white (n=1,184, 93.23%), with less than 3% representation from African Americans (n=31, 2.44%). Patients living in all 50 US states were eligible to participate; however, patients who did not report speaking English were excluded (n=10), because the reliability of the administered scales when translated into different languages was unknown.
Procedures
All eligible participants were sent an email invitation to participate in a web-based survey administered using Qualtrics© (2014) online survey software. CRR enrollees were asked to provide electronic informed consent prior to completing the survey. The current project was approved by a hospital-based Institutional Review Board (IRB) overseeing the CRR and a university-based IRB where the data was stored. Upon completion of the survey, participants were thanked for their participation and notified that their email address would be entered into a random drawing to receive one $45 supermarket/gasoline gift card. The total number of completed online surveys was 199 (response rate=15.7%). Sending follow-up email invitations to non-responders was not possible due to CRR policies that limited each member of the registry from being contacted more than once regarding a research opportunity. Listwise deletion was used to omit cases with missing data (n=23). Complete data were analyzed from 176 patients enrolled in the CRR who responded to the entire survey.
Independent variables
Demographic variables.
Demographic items assessed socio-demographic variables including age, gender, race (White, Black or African American, Asian or Pacific Islander, American Indian or Alaska Native, Mixed Race, or Other), ethnicity (Hispanic/Non-Hispanic), marital status (now married, now widowed, never married, divorced or separated), and education level (less 8th grade, 8th to 11th grade, completed high school, some college, college graduate, post graduate).
Technology and social media use for health information.
Two items from the 2012 Health Information National Trends Survey (HINTS) were adapted to collect data on use of the Internet for health information seeking. Respondents were asked, “In the past 12 months, have you used any of the following devices to look for health or medical information for yourself regarding COPD?” The following electronic devices were considered: desktop computer, laptop computer, mobile phone or smartphone, or other mobile wireless device. To evaluate the use of social media for finding health information, respondents were asked, “In the last 12 months, have you used any of the following types of social media to locate or share health information?” Respondents could select from the following types of social media: participation in an online support group; using popular social networking sites like Facebook, Twitter, or LinkedIn.com; or writing in an online diary or blog.
Health status.
Participants were asked to report all comorbid conditions, disease severity, and both lung-specific and generic HRQoL. Lung-specific HRQoL was assessed using the COPD Assessment Test (CAT), which is an 8-item self-reported questionnaire (Jones et al., 2009) that quantifies the impact of COPD symptoms on a scale from 0 (mild) to 40 (very severe) to indicate the impact of disease (Dodd et al., 2010). The minimum important clinically significant difference on the CAT is ± 2 points (Kon et al., 2014). Among clinically stable COPD patients, scores on CAT are highly correlated with scores on the St. George’s Respiratory Questionnaire (Jones et al., 2009), which is a commonly used, yet lengthy (50-item) instrument that measures disease-specific HRQoL in patients with obstructive airway disease. Generic HRQoL was evaluated using the EuroQol (EQ)-5D (EuroQol Group, 1990), an instrument that describes and evaluates general HRQoL. The five domains of HRQoL assessed by the EQ-5D are: (1) mobility, (2) self-care, (3) usual activity, (4) pain, and (5) anxiety/depression. For each domain, participants are asked to choose from three response boxes ranging from ‘no problems’ (level 1) to ‘some problems’ (level 2) to ‘inability or extreme difficulty’ (level 3). Responses are used to characterize an individual’s unique health state by using a 5-digit descriptor ranging from 11111 for perfect health to 33333 for worst possible health (35 = 243 possible health states). Weights are applied to score responses on each of the five domains and then converted to a single index value ranging from 0 to 1, where a score of 1 represents a perfect health state. This index value is based on a value set derived from a Time Trade Off valuation study reflecting data collected in the U.S. population (Shaw, Johnson, & Coons, 2005). EQ-5D validation studies have supported its construct validity (Hurst, Kind, Ruta, Hunter & Stubbings, 1997), test-retest reliability (EuroQol Group, 1990), internal consistency (Kind, Dolan, Gudex & Williams, 1998), responsiveness to change (Hurst et al., 1997), and generalizability (Van Agt, Essink-Bot, Krabbe, & Bonsel, 1994). The EQ-5D is self-administered, written at a seventh grade level, and can be completed in five to ten minutes (Paz, 2009). Data collected with the EQ-5D in this study showed satisfactory internal consistency (α = 0.74).
Socio-cognitive mechanisms.
COPD knowledge was evaluated using the Chronic Obstructive Pulmonary Disease Knowledge Questionnaire (COPD-Q; Maples, Franks, Ray, Steven & Wallace, 2010). The COPD-Q is a valid, readable, and reliable 13-item self-administered true/false questionnaire assessing COPD knowledge in patients with low health literacy skills. COPD self-efficacy was measured using the Self-Efficacy for Managing Chronic Disease (SEMCD)-6 scale (Lorig et al., 2001), which contains 6 items that assess a patient’s ability to control symptoms, physically and emotionally function, and communicate with their physician on a scale from 1 (not at all confident) to 10 (totally confident). Reliability of SEMCD-6 scores have been high (α = 0.91; Lorig et al., 2001). Data collected using the SEMCD-6 in this study showed evidence of satisfactory internal consistency (α = 0.91). Perceived social support was evaluated using the Oslo 3-item Social Support Scale (OSS-3), a brief measure of social functioning (Dalgard et al., 2006; Abiola, Udofia & Zakari, 2013). Item 1 of the OSS assesses the number of people the respondent can count on during difficult times. Item 2 assesses how much concern other people show to the respondent on a scale from 1 (none) to 5 (a lot). Item 3 gauges how easy it is for respondents to get practical help from others in times of need on a scale from 1 (very difficult) to 5 (very easy). OSS-3 scores can range from 2–14, with a score of 2–8 indicating ‘poor’ support, 9–11 indicating ‘moderate’ support, and 12–14 indicating ‘strong’ social support.
Outcome Variable: eHealth literacy
eHealth literacy.
eHealth literacy was evaluated using the eHealth Literacy Scale (eHEALS; Norman & Skinner, 2006b), which is a brief 8-item rating scale designed to assess one’s perceived ability to locate, comprehend and evaluate health information from online sources and apply newly gained knowledge to make health decisions. A systematic literature review of health literacy screening tools found that the eHEALS is a reliable computer-based measure of patients’ perceived skills at finding and using electronic health information (Collins et al., 2012). eHEALS is the only computer-based health literacy-screening instrument that is available to measure self-reported knowledge and self-efficacy for obtaining and evaluating online health resources. Responders are asked to indicate their level of agreement with eight statements regarding online health information seeking on a Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). Scores on each of the 8-items are summed to obtain a total eHealth literacy score (range = 8 to 40). Data collected using the eHEALS shows high internal consistency (α = 0.88; Norman & Skinner, 2006b; Neter & Brainin, 2012; Van der Vaart et al., 2011). In this study, data collected using the eHEALS also demonstrated high internal consistency (α = 0.90).
Data Analysis
SAS version 9.4 computer software (SAS Institute, Inc., 2013) was used to compute frequency and descriptive statistics related to demographics, socio-cognitive variables, health status, types of electronic devices used (i.e., desktop computers, laptop computers, cell phones, mobile devices) to access Internet-based health information, and use of social media for health information (RQ#1). A series of two sample, two-sided t-tests with the Satterthwaite correction compared the age of users and non-users of electronic devices and social media for health information seeking (RQ#2). The Satterthwaite method accounts for the unequal target population variances of the groups being compared. Frequency and descriptive mean (±SD) statistics were computed to analyze eHEALS responses (RQ#3). To preserve the logical order of categorical response options, eHEALS scores were collapsed into agree (‘strongly agree’ and ‘agree’), undecided, or disagree (‘strongly disagree’ and ‘disagree’) categories. Associations between predictors such as demographics (age, gender, marital status, education), health status (generic HRQoL, lung-specific HRQoL), and socio-cognitive mechanisms (social support, self-efficacy, COPD knowledge) were examined using multiple linear and forward stepwise multiple regressions (RQ#4). Marital status, self-reported COPD severity, and education level were recoded using Helmert coding (Wendorf, 2004) to contrast each categorical level with the means of subsequent levels. Each predictor was then entered into a simple linear regression to obtain unadjusted estimates of each independent variable’s association with the dependent variable, eHealth literacy. If independent variables were significantly (p<.05) correlated with eHealth literacy in univariate analysis, or if variables had potential to be a confounder in the multiple regression model (i.e., age, gender, marital status), they were entered into stepwise multiple linear regression analyses with forward entry. The Mann-Whitney-Wilcoxon test and Spearman rank correlation procedures were used to examine associations between ordinal eHEALS items and each statistically significant (p<.05) predictor emerging from the stepwise regression model.
Results
Sample Characteristics
Table 1 presents demographic characteristics of patients (N=176, Response Rate=13.9%) who responded to the online survey. The mean age of participants was 66.19 years (SD = 9.47 years), which was very similar to the CRR sampling frame. Respondents were about equally divided on gender (n=89 were female, 50.6%), although the proportion of female respondents was less than expected based on the total number of females in the CRR sampling frame (n=703, 55.4%). Respondents were overwhelmingly White (n=169, 96.0%), which was expected based on the very large proportion of white patients in the sampling frame (n=1,184, 93.2%). Respondents were also highly educated, with only 2.80% (n=4) not reporting a high school diploma. Over 60% of participants were married (n=108), while almost one-quarter reported being divorced or separated (n=42).
Table 1.
Socio-Demographic Characteristics of Patients with COPD
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 89 (50.6) |
| Male | 86 (48.9) |
| Race | |
| White | 169 (96) |
| Black | 2 (1.1) |
| Asian or Pacific Islander | 1 (0.6) |
| American Indian or Alaska Native | 1 (0.6) |
| Mixed race | 1 (0.6) |
| Other | 1 (0.6) |
| Education level | |
| 8th to 11th grade | 5 (2.8) |
| High school graduate | 22 (12.5) |
| Some college | 83 (47.2) |
| College graduate | 37 (21) |
| Post graduate degree | 29 (16.5) |
| Marital status | |
| Married | 108 (61.4) |
| Widowed | 16 (9.1) |
| Never married | 10 (5.7) |
| Divorced or separated | 42 (23.9) |
| Perceived COPD status | |
| Mild | 17 (9.7) |
| Moderate | 53 (30.1) |
| Severe | 78 (44.3) |
| Very Severe | 28 (15.9) |
| Self-reported co-morbidities | |
| Diabetes | 23 (13.1) |
| Hypertension | 75 (42.6) |
| Cardiovascular Disease | 33 (18.8) |
| Cancer | 8 (4.5) |
| Arthritis or Joint Problems |
78 (44.3) |
Note. N=176.
Socio-cognitive mechanisms.
The mean COPD-Q score was 9.82±1.63, indicating that participants possessed reasonably high knowledge of COPD. The mean score on the SEMCD-6 was 6.09±2.14 on the 10-point scale, which suggested that respondents were only moderately confident in their ability to manage their condition. The mean total OSS-3 score was 9.39±2.62. Sixty-four respondents (36.36%) reported “poor” levels of perceived social support, while 69 participants (39.2%) reported “moderate” levels of social support. Less than one-quarter of respondents (n=43, 24.4%) reported feeling a “strong” sense of social support.
Health status.
Most respondents reported living with moderate (n=53, 30.1%), severe (n=28, 15.9%), or very severe (n=28, 15.9%) cases of COPD. As expected, most respondents experienced at least one co-morbid condition (n=144, 81.8%), with arthritis/joint problems (n=78, 44.3%) and hypertension (n=75, 42.6%) being most commonly reported.
Main Findings
RQ#1.
The majority of participants reported accessing the Internet for health information using their desktop computer (n=116; 65.9%), while almost half reported use of a laptop (n=87; 49.3%). Almost one-quarter of patients reported using mobile wireless devices (n=43, 24.4%) and mobile phones (n=38, 21.7%) to access online health information. Over one-third (n=59, 33.5%) reported accessing popular social media websites such as Facebook, Twitter, and YouTube for health information, while slightly more than 30% (n=53) reported use of Internet-based discussion boards or support groups to locate and share health/medical information. Very few respondents (n=10, 5.7%) reported keeping an online diary or posting regularly to a health-related blog.
RQ#2.
Interestingly, there were no statistically significant differences in age among users and non-users of all electronic devices evaluated by participants (p values =.07 to .50); however, there was a statistically significant difference in age among users (M= 61.39 years, SD = 9.10 years) and non-users (M=68.61 years, SD=8.72 years) of social media for health information, t(112.13)= 5.03, p<.001. Younger patients were more likely to use social media to access and share health and medical information related to COPD. Weak, yet statistically significant, associations were observed between use of social for health information and use of wireless laptop computers (rs=0.16, p=0.03), cell phones (rs=0.27, p<0.001), and mobile tablet computers (rs =0.18, p=0.01).
RQ#3.
Figure 1 illustrates the response frequencies for each eHEALS item. The statements, “I know how to use the Internet to answer my health questions” (n=142; 80.68%), “I know how to find helpful health resources on the Internet” (n=126; 71.59%), and “I know how to use the health information I find on the Internet to help me” (n=124; 70.45%) showed the highest levels of agreement (i.e., “agree” and “strongly agree”). Two statements that respondents had the greatest level of disagreement with were related to confidence using online health information to make health decisions (n=38; 21.59%) and ability to distinguish between high- and low-quality health resources on the Internet (n=33; 18.75%). The mean total score on the eHEALS in the sample was 29.11 (SD = 5.72). Table 2 lists the mean scores and standard deviations for all 8 eHEALS items.
Table 2.
Mean (±SD) responses on 8-item eHEALS
| eHealth Literacy Scale (eHEALS) itemsa | M (SD) |
|---|---|
| (1) I know what health resources are available on the Internet. |
3.47 (1.02) |
| (2) I know where to find helpful health resources on the Internet. |
3.63 (0.99) |
| (3) I know how to find helpful health resources on the Internet. |
3.80 (0.93) |
| (4) I know how to use the Internet to answer my health questions. |
3.95 (0.85) |
| (5) I know how to use the health information I find on the Internet to help me. |
3.78 (0.79) |
| (6) I have the skills I need to evaluate the health resources I find on the Internet. |
3.88 (0.90) |
| (7) I can tell high-quality from low-quality health resources on the Internet. |
3.38 (1.07) |
| (8) I feel confident in using information from the Internet to make health decisions. |
3.21 (0.93) |
Note. N=176.
eHEALS items were rated on a 5-point Likert scales: 1 = Strongly Disagree; 2 = Disagree; 3 = Undecided; 4 = Agree; 5 = Strongly Agree
RQ#4.
In simple regression, all independent variables except for age, gender, and marital status were significantly associated (p<0.05) with eHealth literacy (Table 3). Table 4 describes results of the multiple linear regression including all demographic, health status, and socio-cognitive mechanisms as predictors. Overall, the full model explained approximately 25% (R2 = 0.250, R2adj=0.179) of the variance in eHealth literacy scores, F(15,174)=3.54, p<0.001. Four predictor variables – (1) very severe COPD vs. mild-severe COPD, (2) COPD knowledge, (3) COPD self-efficacy, and (4) lung-specific HRQoL – entered into the stepwise model and accounted for 16% of the variance in eHealth literacy (Table 5). Final model estimates indicated that very severe COPD versus less severe COPD (β=4.15), lower lung-specific HRQoL (β=−0.19), and greater COPD knowledge (β=0.62) were all associated with higher eHealth literacy scores. After adjusting for the predictor variables in the stepwise model, the association between COPD self-efficacy and eHealth literacy became non-significant (p=0.18), indicating that multicollinearity likely affected relationships between these variables. An examination of variance inflation factors and tolerance statistics confirmed the presence of multicollinearity for each predictor entered into the stepwise model.
Table 3.
Simple Linear Regression Predicting Total eHEALS Scores
| Independent variable | β | SE β | t | p-value |
|---|---|---|---|---|
| Age (years) | -0.02 | 0.05 | -0.40 | 0.69 |
| Female | -1.22 | 0.86 | -1.42 | 0.16 |
| Marital status | ||||
| Married | 1.29 | 1.04 | 1.24 | 0.22 |
| Widowed | 0.55 | 1.68 | 0.33 | 0.74 |
| Never married | 3.42 | 2.01 | 1.70 | 0.09 |
| Education | ||||
| 8th-11th grade | -4.70 | 2.70 | -1.74 | 0.08 |
| High school | -4.67 | 1.58 | -2.96** | 0.01 |
| Some college | -2.56 | 1.20 | -2.13* | 0.04 |
| College graduate | -4.10 | 1.39 | -2.96** | 0.01 |
| COPD status | ||||
| Mild | 0.001 | 1.70 | 0.00 | 0.99 |
| Moderate | -4.19 | 1.29 | -3.24** | 0.001 |
| Severe | -3.27 | 1.22 | -2.69** | 0.01 |
| COPD assessment Test |
-0.18 | 0.06 | -2.84** | 0.005 |
| EuroQol index | 5.26 | 2.39 | 2.20* | 0.03 |
| COPD knowledge Scorea |
0.66 | 0.26 | 2.55* | 0.01 |
| Self-efficacy | 0.60 | 0.20 | 3.07** | 0.003 |
| Social support | 0.33 | 0.16 | 2.05* | 0.04 |
Note. N=176. Betas (β) reflect the estimate of expected change in the dependent variable per unit change in the independent variable
p<.05.
p<.01.
Table 4.
Multiple Linear Regression Analysis Predicting eHealth Literacy
| Independent variable | βa | SE β | t | p-value | |
|---|---|---|---|---|---|
| Constant | 25.71 | 5.83 | 4.41 | 0.0001 | |
| Age | -0.070 | 0.047 | -1.48 | 0.14 | |
| Gender | 1.644 | 0.860 | 1.91 | 0.06 | |
| Marital Status | |||||
| Divorced/separated vs. all other levels |
-1.318 | 1.007 | -1.31 | 0.19 | |
| COPD Status (self-reported) | |||||
| Mild vs. all other Levels |
-1.818 | 1.679 | -1.08 | 0.28 | |
| Mild-moderate vs. severe-very severe |
1.550 | 0.963 | 1.61 | 0.11 | |
| Mild-severe vs. very Severe |
2.757* | 1.201 | 2.29 | 0.02 | |
| Education | |||||
| Less than 8th grade – some high school vs higher |
-0.795 | 2.697 | -0.29 | 0.77 | |
| Less than 8th grade – high school grad vs higher |
1.758 | 1.354 | 1.30 | 0.20 | |
| Less than 8th grade – some college vs higher |
-1.850 | 1.054 | -1.76 | 0.08 | |
| Less than 8th grade – college grad vs higher |
3.227* | 1.343 | 2.40 | 0.02 | |
| COPD Assessment Test | -.0196* | 0.094 | -2.08 | 0.04 | |
| EuroQol Index | 2.065 | 3.012 | 0.69 | 0.49 | |
| COPD Knowledge | 0.761** | 0.256 | 2.97 | 0.003 | |
| Self-Efficacy | 0.048 | 0.275 | 0.17 | 0.86 | |
| Social Support | 0.106 | 0.168 | 0.63 | 0.53 | |
| R2 | 0.250 | ||||
| Adjusted R2 | 0.179 | ||||
| F(15, 174) | 3.54*** | ||||
Note. N=176.
Betas (β) reflect the estimate of expected change in the dependent variable per unit change in the independent variable.
p<.05.
p<.01.
p<.001
Table 5.
Final Stepwise Multiple Linear Regression Predicting eHealth Literacy
| Step | Variable | βa | SE β | F | p-value |
|---|---|---|---|---|---|
| 1 | COPD self-efficacy | 0.330 | 0.243 | 1.84 | 0.18 |
| 2 | Mild-severe vs. very Severe COPD status |
4.146*** | 1.140 | 13.22 | 0.0004 |
| 3 | COPD knowledge | 0.622* | 0.248 | 6.29 | 0.01 |
| 4 | Disease-specific HRQoL | -.190* | 0.094 | -2.08 | 0.02 |
| R2 | 0.164 | ||||
| C(p) | 12.248 | ||||
| F(4, 174) | 8.34*** | ||||
Note. N=176. Betas (β) reflect the estimate of expected change in the dependent variable per unit change in the independent variable
p<.05.
p<.001
Table 6 reports all correlations between eHEALS item scores and the four predictor variables entered into the stepwise linear regression model. Each predictor variable from the stepwise model was significantly (p<.05) associated with at least two eHEALS item scores (Table 6). Most notably, individuals with ‘very severe’ as compared to ‘less severe’ COPD reported greater scores on the following eHEALS items: Item 1) Knowledge of what health resources were available on the Internet (U=0.26, p<.001); Item 2) Where to find health resources on the Internet (U=0.21, p=.005); Item 4) How to use the Internet to answer health-related questions (U=0.21, p=.006); Item 5) How to use health information from the Internet to help solve health-related problems (U=0.16, p=.029); and Item 7) How to decipher high-quality from low-quality health information on the Internet (U=0.19, p=.014). The only eHEALS item without at least one statistically significant correlation with a stepwise predictor variable was one item (#8) assessing confidence using information from the Internet to make health decisions.
Table 6.
Spearman Rank Correlations between eHEALS Items and Predictors remaining in the Stepwise Linear Regression Model Predicting eHealth Literacy
| eHealth Literacy Scale (eHEALS) items | Very severe vs. mild to severe perceived COPDa |
COPD knowledge |
COPD self-efficacy |
Lung-specific HRQoL |
|---|---|---|---|---|
| (1) I know what health resources are available on the Internet. |
0.262** (.001) |
0.239** (.001) |
0.126 (.010) |
-0.136 (.073) |
| (2) I know where to find helpful health resources on the Internet. |
0.209** (.005) |
0.118 (.119) |
0.158* (.037) |
-0.125 (.098) |
| (3) I know how to find helpful health resources on the Internet. |
0.146 (.053) |
0.065 (.391) |
0.194** (.001) |
-0.151* (.045) |
| (4) I know how to use the Internet to answer my health questions. |
0.208** (.006) |
0.144 (.057) |
0.124 (.102) |
-0.116 (.126) |
| (5) I know how to use the health information I find on the Internet to help me. |
0.164* (.029) |
0.238** (.001) |
0.241** (.001) |
-0.242** (.001) |
| (6) I have the skills I need to evaluate the health resources I find on the Internet. |
0.100 (.185) |
0.145 (.055) |
0.254** (.001) |
-0.241** (.001) |
| (7) I can tell high-quality from low- quality health resources on the Internet. |
0.185* (.014) |
0.133 (.078) |
0.251** (.001) |
-0.195** (.001) |
| (8) I feel confident in using information from the Internet to make health decisions. |
0.140 (.064) |
0.147 (.052) |
0.141 (.062) |
-0.114 (.131) |
Note. ( ) Actual p values in parentheses
Results of Mann-Whitney-Wilcoxon Test
p<.05.
p<.01
More general knowledge of COPD was significantly associated with greater knowledge of health resources available on the Internet (ρ=0.239, p=.001), as well as greater knowledge of how to use online health information to find self-care information (ρ=0.238, p=.001). Greater COPD self-efficacy was significantly associated with knowing where to find helpful resources on the Internet (ρ=0.158, p=.037), how to use health information from the Internet to make health decisions (ρ=0.241, p=.001), and how to evaluate online health resources (ρ=0.254, p<.001). In addition, COPD self-efficacy was positively associated with feeling able to decipher between high- and low-quality online resources (ρ=0.251, p<.001). Greater lung-specific HRQoL was associated with less knowledge regarding how to find (ρ=−0.151, p=.045) and use (ρ=−0.242, p=.001) health-related resources on the Internet, and less confidence evaluating (ρ=−0.241, p=.001) and determining the quality of (ρ=−0.195, p=.001) health-related resources found online.
Discussion
This study used a conceptual model of health information seeking to help identify salient activating mechanisms and intervening variables associated with eHealth literacy among a nationally representative sample of patients with COPD. Previous research had identified predictors of Internet access and use in COPD (Martinez et al. 2014); however, our cross-sectional study was the first, to our knowledge, to explore how patients living with COPD perceived their ability to find, understand, and use web-based health information (i.e., eHealth literacy). Information on relevant factors affecting eHealth literacy in COPD is essential for determining the extent to which patients are confident in their ability to benefit from Internet- and social media-based patient education and self-management support materials and programs.
Digital Device and Social Media Use
Among this highly educated sample of predominantly white older adults living with COPD, most used a desktop or laptop computer to access online health information. Over 20% of patients surveyed also used mobile wireless devices or mobile phones, which was quite similar to health-related digital device use in the general older adult population (Tennant et al., 2015). Interestingly, results from this study showed no age-related differences in patient use of laptops or wireless devices for health-related purposes. As the digital health divide shrinks and the “graying” of social media continues (Boulos, 2012), mobile device ownership will likely transform healthcare for aging patients living with chronic disease (Hamine, Gerth-Guyette, Faulx, Green, & Ginsburg, 2015).
A growing body of literature in COPD is exploring the use of mHealth application (apps) for disease self-management. The rise in mobile Internet and smartphone-based apps across many demographic lines and age groups (Smith, 2015) are providing new opportunities to communicate with patients using strategies such as short message service (SMS) text messaging and biofeedback during pulmonary rehabilitation (Marshall, Medvedev & Antonov, 2008). The future of COPD self-management is likely to benefit from enhanced use of mobile smartphones and tablets (Borycki, 2012), yet studies testing use of mobile phones for health in older adult populations are generally limited to feasibility studies with low sample sizes that lack generalizability (Joe & Demiris, 2013). Small, cross-sectional studies report that COPD patients may be more interested in communicating with healthcare providers using SMS text messaging, as compared to using email or communicating on social media (Ojeda et al., 2014; Sanchez et al., 2014). Ongoing systematic reviews are evaluating the comparative effectiveness of mobile technology interventions versus variations of face-to-face and digital delivered interventions to determine how effective mHealth interventions are in sustaining self-management in COPD (McCabe et al., 2014). To develop more patient-centered, web-based approaches to patient education in COPD, it will be important to identify patient preferred mobile communication tools that optimize engagement and improve clinical outcomes in diverse patient populations (Nguyen et al., 2009).
Findings from the current study revealed a small association between social media use and use of wireless technology (i.e., laptops, mobile phones, and tablet computer) for health information seeking. Over one-third of respondents reported use of various types of health-related social media (e.g., virtual discussion boards, online support groups). Unlike electronic device use, where no differences in age were observed, younger patients with COPD were more likely to report using social media for health-related purposes. Research suggests that social media use among baby boomers with chronic disease is increasing and will likely continue to grow with the rise in mobile device use (Fox & Purcell, 2010). However, understanding disease-specific barriers to social media use in COPD will be important for determining how to best leverage the potential of these available interactive health communication tools (e.g., social networks, bookmarking sites, media sharing, micro-blogging). Research testing the effects of social media on health generally only cover a limited range of social media platforms (e.g., online support groups, discussion forums, message boards; Merolli et al., 2013). For social media to become a more meaningful part of chronic disease management, adaptable and flexible social technologies need to be tailored to the individual needs of patients who may be geographically dispersed and psychologically diverse (Merolli et al., 2013). Capitalizing on the personalization potential of social media, such as customized profile alerts, reminder systems, and storytelling, can provide unique benefits to patients with COPD who often struggle with psychosocial health issues such as anxiety and depression. Testing effects of select mobile engagement strategies on symptom awareness, medication adherence, and physical activity may help inform the development of more evidence-based practices for integrating social media into COPD management.
eHealth Literacy in COPD
Overall, patients with COPD in this study self-reported moderate levels of eHealth literacy, with eHEALS scores comparable to other studies in the general older adult population (Choi & Dinitto, 2013; Tennant et al., 2015). Over two-thirds of respondents felt confident in their ability to find useful health resources on the Internet and apply the information learned to answer their own health-related questions. However, respondents were much less confident in their ability to distinguish between low- and high-quality sources of online health information. Difficulty delineating between low- and high-quality sources of web-based health information has been reported in several studies examining eHealth literacy in older adults (Manafo & Wong, 2012; Tennant et al., 2015). Identifying patients with COPD who are able to discern the quality of web-based sources of health information is important, because skilled online information seekers are generally more willing to engage in clinical decision-making and formal disease self-management programs (Clarke et al., 2015). Future patient-centered research in COPD should examine the type of websites used for health information among patients living with COPD, including the frequency with which they access different types of Internet resources. Increased frequency of use may be correlated with disease-related knowledge, attitudes, self-efficacy, and perceived social support.
Activating Mechanisms and Intervening Variables Influencing eHealth Literacy in COPD
Health-related stress.
Most patients in this cross-sectional study experienced moderate to very severe COPD, with the majority living with the co-morbidities of arthritis and hypertension. Respondents with more severe COPD demonstrated greater overall eHealth literacy. Specifically, individuals with very severe as compared to less severe COPD, reported greater knowledge of where to find high-quality health-related resources on the Internet. Patients with more severe disease also reported a greater understanding of how to use web-based health information to answer their health-related questions. These results support findings from Martinez and colleagues (2014), who suggested that COPD patients experiencing more breathing exacerbations might access the Internet more frequently to find information on self-managing breathlessness. Patients living with more advanced stages of COPD are prime candidates to receive patient support resources on the Internet to help them manage unexpected breathing exacerbations occurring at home. The progressive nature of COPD makes the Internet and social media especially valuable for supporting sustained patient empowerment. Even patients living with mild to moderate COPD need more knowledge related to their condition and its sequelae. Newly diagnosed patients may be able to access early intervention through online referrals or “web prescriptions” that direct them to evidence-based online resources and trainings that can introduce patients to their new life living with COPD and how to manage the condition effectively.
Demographic factors.
Age, gender, and marital status were not significantly associated with eHealth literacy in this national sample of patients living with COPD. Although age has been identified as one of the most important contributors to operational eHealth-related Internet skills (van Deursen & van Dijk, 2011), the impact of advanced age on web-based health information seeking among people living with chronic disease may be condition specific. Martinez and colleagues (2014) noted that older patients with COPD were more likely to live without Internet access and less likely to use the Internet even if they had access. While declines in cognitive ability and low technological readiness negatively affect online health information seeking (Miller & Bell, 2012) and general health literacy (Serper et al., 2014) among older adults, it is possible that advanced age may not negatively affect eHealth literacy among those living with COPD. In this patient population, the dynamic construct of eHealth literacy may be affected more so by technological advancements and individual motivational levels.
Similar to research conducted in the general older adult population (Tennant et al., 2015), a positive relationship was observed between education level and eHealth literacy among people living with COPD. A recent systematic review explored the effect of education level on a proxy of eHealth literacy, the ability to evaluate the perceived quality and trustworthiness of online health information (Diviani et al., 2015). While results from this review were inconsistent, the majority of studies suggested that lower education levels were associated with lack of trust in online health information and poorer skills evaluating information that was located. Research suggests that older adults who trust the Internet will use it for a variety of health-related purposes such as seeking new health information, communicating with their healthcare provider(s), and ordering prescriptions (Zulman, Kirch, Zheng, & An, 2011). To better meet the needs of COPD patients who may lack trust in Internet-based health information, data management should be transparent and based on the best available science (Kayser, Kushnirul, Osborne, Norgaard, & Turner, 2015) and always cite sources for passive consumers (or voyeurs) of online health information (Montague & Asan, 2012).
Socio-cognitive factors.
Survey respondents in this study possessed reasonably good knowledge of COPD, with respondents scoring slightly higher on the COPD-Q than what has been reported in previous studies (Ray, Helmer, Steven, Franks, & Wallace, 2013). Prior research suggests that COPD patients have poor knowledge of disease-specific educational domains such as causes of COPD, consequences of inadequate therapy, and exacerbation management (Hernandez et al., 2009), yet they possess more knowledge on the pathophysiology of the disease and available COPD treatments (Scott, Baltzan, Dajczman, & Wolkoye, 2010). In this study, greater COPD knowledge was associated with more knowledge of existing health-related resources on the Internet and more confidence using online health information to make health decisions. Both the Internet and social media present enumerable opportunities for lung health education targeted at people living with COPD. Patients who are more eHealth literate have the potential to become more knowledgeable about their condition as it progresses over time. However, the extent to which eHealth literacy predicts COPD knowledge in discrete COPD self-management domains (e.g., physical activity, medication adherences, diet, oxygen use) is unclear, and should be investigated further to inform future educational programs.
Self-efficacy.
Findings from this study showed a positive association between COPD self-efficacy and eHealth literacy, which is consistent with prior research (Bodie & Dutta, 2008). Patients who reported greater COPD self-efficacy in this study also reported greater knowledge of how to find helpful resources on the Internet and how to evaluate these resources to make informed health decisions. In addition to the positive effects of high COPD self-efficacy on mood, dyspnea, and mental health (Simpson & Jones, 2013), this study suggest that patients with high self-efficacy may also perceive themselves to be more adept at locating health and medical information online. Chronic disease patients who participate in interactive health communication interventions often feel greater self-efficacy for managing their condition (Stellefson et al., 2013, Lorig, Ritter & Lauren, 2010; Lorig et al., 2008). While these significant associations are promising, it should be noted that multicollinearity between predictor variables attenuated the relationship between COPD self-efficacy and eHealth literacy in this study. Because of this, future research measuring eHealth literacy in COPD should include more items that assess efficacy beliefs related to seeking, understanding, evaluating, and applying health information from both the Internet and social media.
Social support.
Lack of strong social support networks was reported by a substantial number of COPD patients in this study. Social support is essential to maintaining good health and a favorable COPD prognosis (Marino, Sirey, Raue, & Alexopoulus, 2008); however, patients living with COPD often report social isolation and insufficient support from peers, family members, and healthcare providers (Williams et al., 2007). Martinez et al. (2014) noted that COPD patients accessed the Internet more frequently if they reported poor interactions with their provider. Greater Internet use by patients reporting non-productive interactions with the healthcare system could indicate that patients use the Internet to fill knowledge gaps caused by poor provider communication. Social media that incorporates more visual patient education materials, family-centered self-management (Ryan & Sawin, 2009), and peer support may help to fill this gap and lead to more trusting and empathetic patient-provider relationships (Lorig et al., 2010; Nguyen et al, 2005; Sadeghi et al., 2013; Stellefson et al., 2013). As recommended by Martinez et al. (2014), future research should examine if greater online health information seeking is associated with improvements in patient satisfaction and less uncertainty and anxiety related to potential for breathing exacerbations.
Limitations
As with all cross-sectional studies, causality is often unclear; therefore, significant associations in this study cannot be used to establish cause-and-effect relationships. For example, it is likely that eHealth literacy predicts COPD-related knowledge, which was not explicitly tested in this study. The current analysis also uses survey data with a relatively low overall response rate (~14%) for Internet surveys (Nulty, 2008), which leaves the potential for bias related to selective participation. Survey respondents chose to participate in the CRR, and may have been more eHealth literate than patients not enrolled in the Registry. As part of CRR enrollment, patients routinely engage in online communication through reading and responding to online posts about current and forthcoming research opportunities. Also, minority populations with COPD and patients with low SES were underrepresented in the sample. The majority of participants identified as being white and highly educated, which is not reflective of the socio-demographics of COPD (Blanchette, Dalal, & Mapel, 2012; Kartaloğlu, 2013). Future studies assessing eHealth literacy and use of the Internet and social media for health information in COPD should aim to recruit a larger number of participants with more diverse racial/ethnic and educational backgrounds. Attempts should also be made to recruit patients from clinical and community-based healthcare settings rather than only using email recruitment via disease registries.
The current study also did not measure frequency of Internet use for health information, and it did not ask specific questions related to the use of search engines or popular consumer health websites (e.g., Mayo Clinic, COPDfoundation.org, WebMD). This prevented the authors from understanding how often and where patients with COPD go to search for online health information. In addition, the construct of eHealth literacy was measured with the eHEALS, which has been questioned in the age of new media due to its inclusion of very general statements assessing confidence using the Internet for health information and lack of items asking about social media use (Norman, 2011; van der Vaart et al., 2011). However, items asking about online health information seeking were restricted to COPD (e.g., “In the past 12 months, have you used the Internet on any of the following devices to look for health or medical information for yourself regarding COPD?”), which may have impacted responses among over 80% of patients reporting at least one other co-morbid condition. Future studies should investigate COPD patient engagement with popular social media (e.g., Facebook, Twitter, Pinterest, YouTube) to determine which websites may be used for different self-management purposes (e.g., inhaler use education, exacerbation management, lifestyle support).
Finally, use of stepwise multiple regression to identify the most important predictors of the outcome of interest (i.e., eHealth literacy) has been challenged by researchers who argue that the analysis (a) results in inaccurate predictor subset size that does not optimize effects; (b) capitalizes on sampling error which yields results that may not be replicable; and (c) uses methods that fail to input the correct degrees of freedom to conduct the analysis (Thompson, 2001). Some researchers disagree with the extent to which these issues adversely impact stepwise analyses conducted in behavioral and social science research (Knapp & Sawilowsky, 2001). As health information processing variables and constructs continue to be evaluated in COPD, the use of hierarchical predictor variable entry may provide advantages when attempting to identify relationships between eHealth literacy, information seeking, and health outcomes.
Conclusion
Results of the current study contribute to the literature in two primary ways. First, we found that greater COPD severity is significantly associated with higher eHealth literacy. Second, we found that greater educational attainment and higher COPD-related knowledge predicts higher eHealth literacy. We also observed that over one-third of COPD patients are using social media to obtain online health information. Online health information seeking and sharing has the potential to help improve health care for severely impaired COPD patients who have difficulty accessing hospital-based pulmonary rehabilitation. These findings emphasize the importance of integrating skill-building activities into comprehensive patient education programs that enable COPD patients, especially those with low education levels and limited COPD-related knowledge, to identify high-quality sources of web-based health information related to their disease. If public health researchers in pulmonary medicine and lung health education are to play a greater role in preventing breathing complications and associated mortality in COPD, there is need to reduce the “digital divide” in COPD even further by identifying new ways to satisfy patient information needs through more participatory, Internet-mediated self-management support programs. Additional research is needed to understand how new technologies should be used to help patients cope with and manage COPD-related morbidity. Patient-centered approaches to eHealth self-management support, based on individual cognitive and clinical characteristics, are more likely to provide educational experiences that lead to better process and functional health outcomes in COPD.
Figure 2.
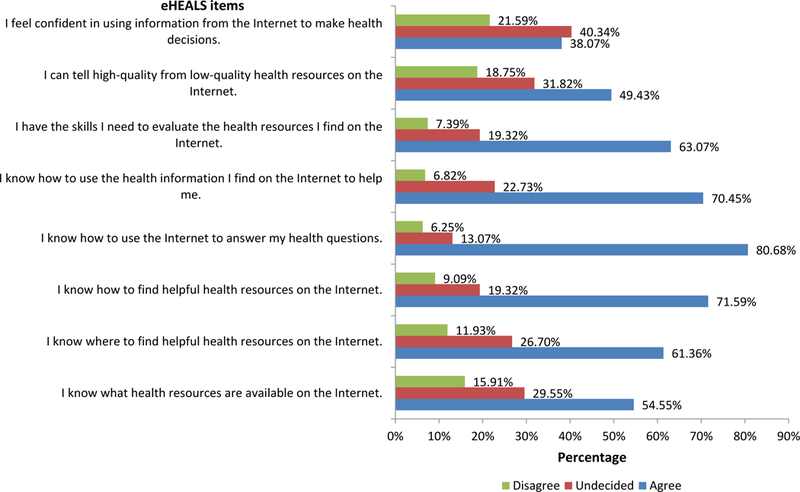
Participant responses to eHEALS items (N=176). Response categories were grouped into agree (including ‘strongly agree’ and ‘agree’), undecided, or disagree (including ‘strongly disagree’ and ‘disagree’). All missing values (n=2) were coded as ‘undecided’.
Contributor Information
Michael L. Stellefson, Associate Professor, Department of Health Education and Promotion, East Carolina University.
Jonathan J. Shuster, Professor Emeritus, Department of Health Outcomes and Policy, University of Florida
Beth H. Chaney, Associate Professor, Department of Health Education and Promotion, East Carolina University.
Samantha R. Paige, Predoctoral Fellow, Department of Health Education and Behavior, University of Florida.
Julia M. Alber, Assistant Professor, Kinesiology Department, California Polytechnic State University.
J. Don Chaney, Associate Professor and Chair, Department of Health Education and Promotion, East Carolina University.
P.S. Sriram, Professor and Chief, Division of Pulmonary and Critical Care Medicine, College of Medicine, University of Florida.
References
- Abiola T, Udofia O, & Zakari M (2013). Psychometric properties of the 3-item Oslo social support scale among clinical students of Bayero University Kano, Nigeria. Malaysian Journal of Psychiatry, 22(2), 32–41. Retrieved from http://www.mjpsychiatry.org/index.php/mjp/article/view/264/0 [Google Scholar]
- Abrams TE, Vaughan-Sarrazin M, Fan VS, & Kaboli PJ (2011). Geographic isolation and the risk for chronic obstructive pulmonary disease–related mortality: A cohort study. Annals of Internal Medicine, 155(2), 80–86. doi: 10.7326/0003-4819-155-2-201107190-00003 [DOI] [PubMed] [Google Scholar]
- Ambrosino N, & Vagheggini G (2006). Is there any treatment other than drugs to alleviate dyspnea in COPD patients? International Journal of Chronic Obstructive Pulmonary Disease, 1(4), 355–361. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2707811/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Lung Association. (2014). Chronic obstructive pulmonary disease (COPD) fact sheet Retrieved from http://www.lung.org/lung-disease/copd/resources/facts-figures/COPD-Fact-Sheet.html. [Google Scholar]
- Anthonisen NR, Connett JE, Kiley JP, Altose MD, Bailey WC, Buist AS, O’Hara P (1994). Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1: The lung health study. Journal of the American Medical Association, 272(19), 1497–1505. doi: 10.1001/jama.1994.03520190043033 [DOI] [PubMed] [Google Scholar]
- Blanchette CM, Dalal AA, & Mapel D (2012). Changes in COPD demographics and costs over 20 years. Journal of Medical Economics, 15(6), 1176–1182. doi: 10.3111/13696998.2012.713880 [DOI] [PubMed] [Google Scholar]
- Bodie GD, & Jyoti Dutta M (2008). Understanding health literacy for strategic health marketing: eHealth literacy, health disparities and the digital divide. Health Marketing Quarterly, 252(1–2), 175–203. doi: 10.1080/07359680802126301 [DOI] [PubMed] [Google Scholar]
- Borycki E (2012). M-health: Can chronic obstructive pulmonary disease patients use mobile phones and associated software to self-manage their disease? In Quintana Y, Van Kirk Villalobos A, & May D (Volume 172), Advancing Cancer Education and Healthy Living in Communities (pp. 79–84). doi: 10.3233/978-1-61499-088-8-79 [DOI] [PubMed] [Google Scholar]
- Boulos MNK (2012). Social media and mobile health. In Kickbusch I, Pelikan JM, Apfel F, & Tsouros AD, The solid facts – Health literacy: Enabling healthier decisions in the 21st century (pp. 1–86). Retrieved from http://www.euro.who.int/__data/assets/pdf_file/0008/190655/e96854.pdf [Google Scholar]
- Bourbeau J, Nault D, & Dang-Tan T (2004). Self-management and behaviour modification in COPD. Patient Education and Counseling, 52(3), 271–277. doi: 10.1016/S0738-3991(03)00102-2 [DOI] [PubMed] [Google Scholar]
- Butcher SJ, Meshke JM, & Sheppard MS (2004). Reductions in functional balance, coordination, and mobility measures among patients with stable chronic obstructive pulmonary disease. Journal of Cardiopulmonary Rehabilitation and Prevention, 24(4), 274–280.Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15286536 [DOI] [PubMed] [Google Scholar]
- Choi NG, & Dinitto DM (2013). The digital divide among low-income homebound older adults: Internet use patterns, eHealth literacy and attitudes toward computer/Internet use. Journal of Medical Internet Research, 15(5), 93. doi: 10.2196/jmir.2645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chretien KC & Kind T (2013). Social media as a tool in medicine. Circulation, 127, 1413–1421. doi: 10.1161/CIRCULATIONAHA.112.128017 [DOI] [PubMed] [Google Scholar]
- Cicutto LC & Brooks D (2006). Self-care approaches to managing chronic obstructive pulmonary disease: A provincial survey. Respiratory Medicine, 100(9), 1540–1546. doi: 10.1016/j.rmed.2006.01.005 [DOI] [PubMed] [Google Scholar]
- Clarke MA, Moore JL, Steege LM, Koopman RJ, Belden JL, Canfield SM, … & Kim MS (2015). Health information needs, sources, and barriers of primary care patients to achieve patient-centered care: A literature review. Health Informatics Journal, 1–25. doi: 10.1177/1460458215602939 [DOI] [PubMed] [Google Scholar]
- Collins SA, Currie LM, Bakken S, Vawdrey DK, & Stone PW (2012). Health literacy screening instruments for eHealth applications: A systematic review. Journal of Biomedical Informatics, 45(3), 598–607. doi: 10.1016/j.jbi.2012.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dajczman E, Fiter R, Cohen L, Baltzan M, Wolkove N, & Prefontaine D (2012). Changing demographics of patients with COPD admitted to a sub-acute pulmonary rehabilitation unit. American Journal of Respiratory and Critical Care Medicine, 185, A5237. doi: 10.1164/ajrccm-conference.2012.185.1_MeetingAbstracts.A523710.1164/ajrccm-conference.2012.185.1_MeetingAbstracts.A5237 [DOI] [Google Scholar]
- Dalal A, Christensen L, Liu F, & Riedel AA (2010). Direct costs of chronic obstructive pulmonary disease among managed care patients. International Journal of Chronic Obstructive Pulmonary Disease, 5, 341–349. doi: 10.2147/COPD.S13771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalgard OS, Dorwick C, Lehtinen V, Vazquez-Barquero JL, Casey P, Wilkinson G, Dunn G (2006). Negative life events, social support and gender difference in depressions: A multinational community survey with data from the ODIN study. Social Psychiatry and Psychiatric Epidemiology, 41(6), 444–451. doi: 10.1007/s00127-006-0051-5 [DOI] [PubMed] [Google Scholar]
- Disler RT, Gallagher RD, & Davidson PM (2012). Factors influencing self-management in chronic obstructive pulmonary disease: An integrative review. International Journal of Nursing Studies, 49(2), 230–242. doi: 10.1016/j.ijnurstu.2011.11.005 [DOI] [PubMed] [Google Scholar]
- Diviani N, van den Putte B, Giani S, & van Weert J (2015). Low health literacy and evaluation of online health information: A systematic review of the literature. Journal of Medical Internet Research, 17(5), 112. doi: 10.2196/jmir.4018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodd JW, Hogg L, Nolan J, Jefford H, Grant A, Lord VM, Hopkinson NS (2011). The COPD assessment test (CAT): Response to pulmonary rehabilitation. A multicentre prospective study. Thorax, 66(5), 425–429. doi: 10.1136/thx.2010.156372 [DOI] [PubMed] [Google Scholar]
- Ebrahim S, & Smith GD (1997). Systematic review of randomised controlled trials of multiple risk factor interventions for preventing coronary heart disease. British Medical Journal, 314, 1666–1674. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9193292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effing TW, Bourbeau J, Vercoulen J, Apter AJ, Coultas D, Meek P, van der Palen J (2012). Self-management programmes for COPD: Moving forward. Chronic Respiratory Diseases, 9(1), 27–35. doi: 10.1177/1479972311433574 [DOI] [PubMed] [Google Scholar]
- Eklund B, Nilsson S, Hedman L, & Lindberg I (2012). Why do smokers diagnosed with COPD not quit smoking? - A qualitative study. Tobacco Induced Diseases, 10(1), 17. doi: 10.1186/1617-9625-10-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Gayar O, Timsina P, Nawar N, & Eid W (2013). Mobile applications for diabetes self-management: Status and potential. Journal of Diabetes Science and Technology, 7(1), 247–262. doi: 10.1177/193229681300700130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emery CF (1994). Effects of age on physiological and psychological functioning among COPD patients in an exercise program. Journal of Aging and Health, 6(1), 3–16. doi: 10.1177/089826439400600101 [DOI] [PubMed] [Google Scholar]
- EuroQol Group. (1990). EuroQol-A new facility for the measurement of health-related quality of life. Health Policy, 16, 199–208. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10109801 [DOI] [PubMed] [Google Scholar]
- Fabbri LM, Luppi F, Beghe B, & Rabe KF (2008). Complex chronic comorbidities of COPD. European Respiratory Journal, 31(1), 204. doi: 10.1183/09031936.00114307 [DOI] [PubMed] [Google Scholar]
- Faulkner MA, Lenz TL, & Stading JA (2006). Cost-effectiveness of smoking cessation and the implications for COPD. International Journal of Chronic Obstructive Pulmonary Disease, 1(3), 279–287. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2707159/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox S & Purcell K (2010, March 24). Social media and health Retrieved from http://www.pewinternet.org/2010/03/24/social-media-and-health/ [Google Scholar]
- Gershon AS, Dolmage TE, Stephenson A, & Jackson B (2012). Chronic obstructive pulmonary disease and socioeconomic status: A systematic review. COPD: Journal of Chronic Obstructive Pulmonary Disease, 9(3), 216–226. doi: 10.3109/15412555.2011.648030 [DOI] [PubMed] [Google Scholar]
- Ghobadi H, Ahari SS, Kameli A, & Lari SM (2012). The relationship between COPD assessment test (CAT) scores and severity of airflow obstruction in stable COPD patients. Tanaffos, 11(2), 22–26. [PMC free article] [PubMed] [Google Scholar]
- Guarascio AJ, Ray SM, Finch CK, & Self TH (2013). The clinical and economic burden of chronic obstructive pulmonary disease in the USA. ClinicoEconomics and Outcomes Research, 5, 235–245. doi: 10.2147/CEOR.S34321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall AK, Stellefson M, & Bernhardt JM (2012). Healthy aging 2.0: The potential of new media and technology. Preventing Chronic Disease, 9, E67. doi: 10.5888/pcd9.110241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamine S, Gerth-Guyette E, Faulx D, Green BB, & Ginsburg AS (2015). Impact of mHealth chronic disease management on treatment adherence and patient outcomes: A systematic review. Journal of Medical Internet Research, 17(2), e52. doi: 10.2196/jmir.3951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris D, Hayter M, & Allender S (2008). Improving the uptake of pulmonary rehabilitation in patients with COPD: Qualitative study of experiences and attitudes. British Journal of General Practice, 58(555), 703–710. doi: 10.3399/bjgp08X342363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heisler M, Vijan S, Anderson RM, Ubel PA, Bernstein SJ, & Hofer TP (2003). When do patients and their physicians agree on diabetes treatment goals and strategies, and what difference does it make? Journal of General Internal Medicine, 18(11). doi: 10.1046/j.1525-1497.2003.21132.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez P, Balter M, Bourbeau J, & Hodder R (2009). Living with chronic obstructive pulmonary disease: a survey of patients’ knowledge and attitudes. Respiratory Medicine, 103(7), 1004–1012. doi: 10.1016/j.rmed.2009.01.018 [DOI] [PubMed] [Google Scholar]
- Hung WW, Wisnivesky JP, Siu AL, & Ross JS (2009). Cognitive decline among patients with chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine, 180(2), 134–137. doi: 10.1164/rccm.200902-0276OC [DOI] [PubMed] [Google Scholar]
- Hurst NP, Kind P, Ruta D, Hunter M, & Stubbings A (1997). Measuring health-related quality of life in rheumatoid arthritis: Validity, responsiveness and reliability of EUROQOL (EQ-5D). British Journal of Rheumatology, 36, 551–559. doi: 10.1093/rheumatology/36.5.551 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2004, April 8). Health literacy: A prescription to end confusion Retrieved from http://www.iom.edu/Reports/2004/Health-Literacy-A-Prescription-to-End-Confusion.aspx. [Google Scholar]
- Joe J & Demiris G (2013). Older adults and mobile phones for health: A review. Journal of Biomedical Informatics, 46(5), 947–954. doi: 10.1016/j.jbi.2013.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones PW, Brusselle G, Dal Negro RW, Ferrer M, Kardos P, Levy ML, & Banik N (2011). Health-related quality of life in patients by COPD severity within primary care in Europe. Respiratory Medicine, 105(1), 57–66. doi: 10.1016/j.rmed.2010.09.004 [DOI] [PubMed] [Google Scholar]
- Jones PW, Harding G, Berry P, Wiklund I, Chen WH, & Leidy NK (2009). Development and first validation of the COPD assessment test. European Respiratory Journal, 34(3), 648–654. doi: 10.1183/09031936.00102509 [DOI] [PubMed] [Google Scholar]
- Kale MS, Federman AD, Krauskopf K, Wolf M, O’Conor R, Martynenko M, Wisnivesky JP (2015). The association of health literacy with illness and medication beliefs among patients with chronic obstructive pulmonary disease. Plos One, 10(4), 123937. doi: 10.1371/journal.pone.0123937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kartaloğlu Z (2013). Socioeconomic Status and Chronic Obstructive Pulmonary Disease. TAF Preventive Medicine Bulletin, 12(1), 87–96. doi: 10.5455/pmb.1-13311198324 [DOI] [Google Scholar]
- Kayser L, Kushniruk A, Osborne RH, Norgaard O, & Turner P (2015). Enhancing the effectiveness of consumer-focused health information technology systems through eHealth literacy: A framework for understanding users’ needs. JMIR Human Factors, 2(1), e9. doi: 10.2196/humanfactors.3696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R, Stahl E, Vogelmeier C, Haughney J, Trudeau E, Lofdahl CG, & Partridge MR (2006). Patient understanding, detection, and experience of COPD exacerbations: An observational, interview-based study. Chest, 130(1), 133–142. doi: 10.1378/chest.130.1.133 [DOI] [PubMed] [Google Scholar]
- Kind P, Dolan P, Gudex C, & Williams A (1998). Variations in population health status: Results from a United Kingdom national questionnaire survey. BMJ, 316(7133), 736–741. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC28477/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiser K, Jonas D, Warner Z, Scanlon K, Bryant SB, & Dewalt DA (2011). A randomized controlled trial of a literacy sensitive self-management interventions for chronic obstructive disease patients. Journal of General Internal Medicine, 27(2), 190–195. doi: 10.1007/s11606-011-1867-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knapp TR, & Sawilowsky SS (2001). Constructive criticisms of methodological and editorial practices. The Journal of Experimental Education, 70(1), 65–79. doi: 10.1080/00220970109599498 [DOI] [Google Scholar]
- Kon SS, Clark AL, Dilaver D, Canavan JL, Patel MS, Polkey MI, & Man WDC (2013). Response of the COPD assessment test to pulmonary rehabilitation in unselected chronic respiratory disease. Respirology, 18(6), 974–977. doi: 10.1111/resp.12084 [DOI] [PubMed] [Google Scholar]
- Koster A, Bosma H, Kempen GI, Van Lenthe FJ, van Eijk JTM, & Mackenbach JP (2004). Socioeconomic inequalities in mobility decline in chronic disease groups (asthma/COPD, heart disease, diabetes mellitus, low back pain): Only a minor role for disease severity and comorbidity. Journal of Epidemiology and Community Health, 58(10), 862–869. 10.1136/jech.2003.018317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig KR, Ritter PL, Dost A, Plant K, Laurent DD, & Mcneil I (2008). The expert patients programme online, a 1-year study of an internet-based self-management programme for people with long-term conditions. Chronic Illness, 4(4), 247–256. doi: 10.1177/1742395308098886 [DOI] [PubMed] [Google Scholar]
- Lorig KR, Ritter PL, & Laurent DD (2010). Online diabetes self-management program: A randomized study. Diabetes Care, 33(6), 1275–1281. doi: 10.2337/dc09-2153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW Jr, Bandura A, & Holman HR (2001). Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care, 39(11), 1217–1223. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11606875 [DOI] [PubMed] [Google Scholar]
- Manafo E & Wong S (2012). Assessing the eHealth literacy skills of older adults: A preliminary study. Journal of Consumer Health on the Internet, 16(4), 369–381. doi: 10.1080/15398285.2012.701163 [DOI] [Google Scholar]
- Mannino DM, Watt G, & Hole D (2006). The natural history of chronic obstructive pulmonary disease. European Respiratory Journal, 27, 627–643. doi: 10.1183/09031936.06.00024605 [DOI] [PubMed] [Google Scholar]
- Maples P, Franks A, Ray S, Stevens AB, & Wallace LS (2010). Development and validation of a low-literacy chronic obstructive pulmonary disease knowledge questionnaire (COPD-Q). Patient Education and Counseling, 81(1), 19–22. doi: 10.1016/j.pec.2009.11.020 [DOI] [PubMed] [Google Scholar]
- Marino P, Sirey JA, Raue PJ, & Alexopoulous GS (2008). Impact of social support and self-efficacy on functioning in depressed older adults with chronic obstructive pulmonary disease. International Journal of Chronic Obstructive Pulmonary Disease, 3(4), 713–718. doi: 10.2147/COPD.S2840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall A, Medvedev O, & Antonov A (2008). Use of smartphone for improved self-management of pulmonary rehabilitation. International Journal of Telemedicine and Applications, 1–5. doi: 10.1155/2008/753064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez CH, St Jean BL, Plauschinat CA, Rogers B, Beresford J, Martinez FJ, Han MK (2014). Internet access and use by COPD patients in the national Emphysema/COPD association survey. BMC Pulmonary Medicine, 14(1), 66. doi: 10.1186/1471-2466-14-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe C, McCann M, & Brady AM (2014). Computer and mobile technology interventions for self management in chronic obstructive pulmonary disease. The Cochrane Library, 12, 1–11. doi: 10.1002/14651858.CD011425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menn P, Heinrich J, Huber R, Jörres RA, John J, Karrasch S, Holle R (2012). Direct medical costs of COPD – an excess cost approach based on two population-based studies. Respiratory Medicine, 106(4), 540–548. doi: 10.1016/j.rmed.2011.10.013 [DOI] [PubMed] [Google Scholar]
- Merolli M, Gray K, & Martin-Sanchez F (2013). Health outcomes and related effects of using social media in chronic disease management: A literature review and analysis of affordances. Journal of Biomedical Informatics, 46, 957–969. doi: 10.1016/j.jbi.2013.04.010 [DOI] [PubMed] [Google Scholar]
- Miller LM, & Bell RA (2012). Online health information seeking: The influence of age, information trustworthiness, and search challenges. Journal of Aging Health, 24(3), 525–541. doi: 10.1177/0898254311428167 [DOI] [PubMed] [Google Scholar]
- Montague E, & Asan O (2012). Trust in technology-mediated collaborative health encounters: Constructing trust in passive user interactions with technologies. Ergonomics, 55(7), 752–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moy ML, Collins R, Martinez CH, Kadri R, Holleman RG, Richardson CR (2014). An internet-mediated walking program for veterans with COPD. Annals of Behavioral Medicine,47(5), 485–496 [Google Scholar]
- National Business Coalition on Health. (2012, September). COPD: A major driver of avoidable health care costs Retrieved from http://www.nbch.org/nbch/files/cclibraryfiles/filename/000000002422/nbch_ab_copd_f.pdf. [Google Scholar]
- National Cancer Institute. (2012). HINTS 4, cycle 2. Health information national trends survey Retrieved from http://hints.cancer.gov/ [Google Scholar]
- National Institutes of Health. (2013a, March 29) Chronic Obstructive Pulmonary Disease (COPD) Retrieved from https://report.nih.gov/nihfactsheets/ViewFactSheet.aspx?csid=77 [Google Scholar]
- National Institutes of Health. (2013b, July 31). What causes COPD? Retrieved from http://www.nhlbi.nih.gov/health/health-topics/topics/copd/causes [Google Scholar]
- National Institutes of Health. (2013c). COPD: The more you know, the better for you and your loved ones Retrieved from http://www.nhlbi.nih.gov/health/educational/copd/campaign-materials/pub/copd-atrisk.pdf [Google Scholar]
- Nelson DE, Kreps GL, Hesse BW, Croyle RT, Willis G, Arora NK, Alden S (2004). The Health Information National Trends Survey (HINTS): Development, design, and dissemination. Journal of Health Communication, 9(5), 443–460. [DOI] [PubMed] [Google Scholar]
- Neter E, & Brainin E (2012). eHealth literacy: Extending the digital divide to the realm of health information. Journal of Medical Internet Research, 14(1), e19. doi: 10.2196/jmir.1619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen H, Carrieri-Kohlman V, Rankin S, Slaughter R, & Stulbarg M (2005). Is internet-based support for dyspnea self-management in patients with chronic obstructive pulmonary disease possible? Results of a pilot study. Heart & Lung: The Journal of Acute and Critical Care, 34(1), 51–62. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15647734 [DOI] [PubMed] [Google Scholar]
- Nguyen HQ, Donesky D, Reinke LF, Wolpin S, Chyall L, Benditt JO, Carrieri-Kohlman B (2013). Internet-based dyspnea self-management support for patients with chronic obstructive pulmonary disease. Journal of Pain and Symptom Management, 46(1), 43–55. doi: 10.1016/j.jpainsymman.2012.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen HQ, Donesky-Cuenco S, Wolpin LF, Reinke JO, Benditt SM, Paul SM, & Carrieri-Kohlman V (2008). Randomized controlled trial of an internet-based versus face-to-face dyspnea self-management program for patients with chronic obstructive pulmonary disease: Pilot study. Journal of Medical Internet Research, 10(9). doi: 10.2196/jmir.990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen HQ, Gill D, Wolpin S, Steele B, & Benditt J (2009). Pilot study of a cell phone-based exercise persistence intervention post-rehabilitation in COPD. International Journal of Chronic Obstructive Pulmonary Disease, 4, 301–313. doi: 10.2147/COPD.S6643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman CD (2011). eHealth literacy 2.0: Problems and opportunities with an evolving concept. Journal of Medical Internet Research, 13(4), 125. doi: 10.2196/jmir.2035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman CD, & Skinner HA (2006a). eHEALS: The eHealth literacy scale. Journal of Medical Internet Research, 8(4), 27. doi: 10.2196/jmir.8.4.e27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman CD, & Skinner HA (2006b). eHealth literacy: Essential skills for consumer health in a networked world. Journal of Medical Internet Research, 8(2), 9. doi: 10.2196/jmir.8.2.e9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nulty DD (2008). The adequacy of response rates to online and paper surveys: What can be done? Assessment & Evaluation in Higher Education, 33(3), 301–314. doi: 10.1080/02602930701293231 [DOI] [Google Scholar]
- Ojeda IC, Sanchez G, Calderon J, Hoyos R, Guerreros AG, Canelos B, Cherrez A (2014). Preferences of using social media (SoMe) for health care in COPD. American Journal of Respiratory and Critical Care Medicine, 189, A3025 Retrieved from http://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2014.189.1_MeetingAbstracts.A3025 [Google Scholar]
- Omachi TA, Sarkar U, Yelin EH, Blanc PD, & Katz PP (2013). Lower health literacy is associated with poorer health status and outcomes in chronic obstructive pulmonary disease. Journal of General Internal Medicine, 28(1), 74–81. doi: 10.1007/s11606-012-2177-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkin T & Skinner TC (2003). Discrepancies between patient and professionals recall and perception of an outpatient consultation. Diabetic Medicine, 20(11), 909–914. doi: 10.1046/j.1464-5491.2003.01056.x [DOI] [PubMed] [Google Scholar]
- Patel R, Change T, Greysen SR, & Chopra V (2015). Social media use in chronic disease: A systematic review and novel taxonomy. The American Journal of Medicine doi: 10.1016/j.amjmed.2015.06.015 [DOI] [PubMed] [Google Scholar]
- Pauwels RA, Buist AS, Calverley PM, Jenkins CR, & Hurd S S….& Zielinski J (2007). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine, 176(6), 532–555. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11316667 [DOI] [PubMed] [Google Scholar]
- Paz SH, Liu H, Fongwa MN, Morales LS, & Hays RD (2009). Readability estimates for commonly used health-related quality of life surveys. Quality of Life Research, 18(7), 889–900. doi: 10.1007/s11136-009-9506-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pousti H, Urquhart C, & Linger H (2014). Exploring the role of social media in chronic care management: A sociomaterial approach. In Doolin B, Lamprou E, Mitev N, McLeod L, Information Systems and Global Assemblages (pp. 163–185). Retrieved from http://link.springer.com/chapter/10.1007%2F978-3-662-45708-5_11#page-1 [Google Scholar]
- Pride NB (2001). Smoking cessation: Effects on symptoms, spirometry and future trends in COPD. Thorax, 56(2), ii7–ii10. Retrieved from http://thorax.bmj.com/content/56/suppl_2/ii7.full.pdf [PMC free article] [PubMed] [Google Scholar]
- Qualtrics©. (2014). Survey Research Suite Retrieved from http://www.qualtrics.com. [Google Scholar]
- Ray SM, Helmer RS, Stevens AB, Franks AS, & Wallace LS (2013). Clinical utility of the chronic obstructive pulmonary disease knowledge questionnaire. Family medicine, 45(3), 197–200. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23463434 [PubMed] [Google Scholar]
- Rennard SI, & Vestbo J (2006). COPD: The dangerous underestimate of 15%. Lancet, 367, 1216–1219. doi: 10.1016/S0140-6736(06)68516-4 [DOI] [PubMed] [Google Scholar]
- Restrepo RD, Alvarez MT, Wittnebel LD, Sorenson H, Wettstein R, Vines DL, Wilkins RL (2008). Medication adherence issues in patients treated for COPD. International Journal of Chronic Obstructive Pulmonary Disease, 3(3), 371–384. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2629978/pdf/copd-3-371.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts NJ, Ghiassi R, & Partridge MR (2008). Health literacy in COPD. International Journal of Chronic Obstructive Pulmonary Disease, 3(4), 499 Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2650589/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan P, & Sawin KJ (2009). The individual and family self-management theory: Background and perspectives on context, process, and outcomes. Nursing Outlook, 57(4), 217–225. doi: 10.1016/j.outlook.2008.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeghi S, Brooks D, & Goldstein RS (2013). Patients’ and providers’ perceptions of the impact of health literacy on communication in pulmonary rehabilitation. Chronic Respiratory Disease, 10(2), 65–76. doi: 10.1177/1479972312471548 [DOI] [PubMed] [Google Scholar]
- Sanchez G, Calderon J, Hoyos R, Guerreros AG, Canelos B, Castro E, & Ojeda IC (2014). Preferences Of Using Social Media (some) For Health Care In COPD. American Journal of Respiratory and Critical Care Medicine, 189, A3025 Retrieved from http://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2014.189.1_MeetingAbstracts.A3025 [Google Scholar]
- Scott AS, Baltzan MA, Dajczman E, & Wolkove N (2010). Patient knowledge and information needs in chronic obstructive pulmonary disease: Back to basics. CHEST Journal, 138(4_MeetingAbstracts), 476A–476A. doi: 10.3109/15412555.2011.605402 [DOI] [PubMed] [Google Scholar]
- SAS Institute, Version 9.4. (2013). http://www.sas.com/en_us/software/sas9.html. [Google Scholar]
- Serper M, Patzer RE, Curtis LM, Smith SG, O’Conor R, Baker DW, & Wolf MS (2014). Health literacy, cognitive ability, and functional health status among older adults. Health Services Research, 49(4), 1249–1267. doi: 10.1111/1475-6773.12154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw JW, Johnson JA, & Coons SJ (2005). US valuation of the EQ-5D health states: Development and testing of the D1 valuation model. Medical Care, 43(3), 203–220. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15725977 [DOI] [PubMed] [Google Scholar]
- Simpson E & Jones MC (2013). An exploration of self-efficacy and self-management in COPD patients. British Journal of Nursing, 22(19), 1105–1109. doi: 10.12968/bjon.2013.22.19.1105 [DOI] [PubMed] [Google Scholar]
- Sin DD, Anthonisen NR, Soriano JB, & Agusti AG (2006). Mortality in COPD: Role of comorbidities. European Respiratory Journal, 28(6), 1245–1257. doi: 10.1183/09031936.00133805 [DOI] [PubMed] [Google Scholar]
- Smith A (2015, April 1). U.S. smartphone use in 2015 Retrieved from http://www.pewinternet.org/files/2015/03/PI_Smartphones_0401151.pdf [Google Scholar]
- Stellefson M, Chaney B, Barry AE, Chavarria E, Tennant B, Walsh-Childers K, Zagora J (2013). Web 2.0 chronic disease self-management for older adults: A systematic review. Journal of Medical Internet Research, 15(2), 35. doi: 10.2196/jmir.2439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stellefson M, Chaney BH, Chaney JD, Paige S, Payne-Purvis C, Tennant B, Alber J (2015). Engaging community stakeholders to evaluate the design, usability, and acceptability of a chronic obstructive pulmonary disease social media resource center. JMIR Research Protocols, 4(1), 17. doi: 10.2196/resprot.3959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor J, Dawson S, Sridhar M, et al. (2005). Functional illiteracy amongst those with Chronic Obstructive Pulmonary Disease (COPD). European Respiratory Journal, 26, 57s. [Google Scholar]
- Taylor R, Dawson S, Roberts N, Sridhar M, & Partridge MR (2007). Why do patients decline to take part in a research project involving pulmonary rehabilitation? Respiratory Medicine, 101(9), 1942–1946. doi: 10.1016/j.rmed.2007.04.012 [DOI] [PubMed] [Google Scholar]
- Tennant B, Stellefson M, Dodd V, Chaney BH, Chaney JD, Paige S, & Alber J (2015). eHealth literacy and web 2.0 health information seeking behaviors among baby boomers and older adults. Journal of Medical Internet Research, 17(3), 70. doi: 10.2196/jmir.3992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson B (2001). Significance, effect sizes, stepwise methods, and other issues: Strong arguments move the field. The Journal of Experimental Education, 70(1), 80–93. Retrieved from http://www.jstor.org/stable/20152666 [Google Scholar]
- Thorpe O, Kumar S, & Johnston K (2014). Barriers to and enablers of physical activity in patients with COPD following a hospital admission: A qualitative study. International Journal of Chronic Obstructive Pulmonary Disease, 9, 115–128. doi: 10.2147/COPD.S54457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Agt HME, Essink-Bot ML, Krabbe PFM, & Bonsel GJ (1994). Test-retest reliability of health state valuations collected with the EuroQol questionnaire. Social Science Medicine, 39, 1537–1544. doi: 10.1016/0277-9536(94)90004-1 [DOI] [PubMed] [Google Scholar]
- van der Vaart R, van Deursen AJ, Drossaert CH, Taal E, van Dijk JA, & van de Laar MA (2011). Does the eHealth literacy scale (eHEALS) measure what it intends to measure? Validation of a Dutch version of the eHEALS in two adult populations. Journal of Medical Internet Research, 13(4), 86. doi: 10.2196/jmir.1840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Deursen AJAM & van Dijk JAGM (2011). Internet skills performance tests: Are people ready for eHealth? Journal of Medical Internet Research, 13(2), e35. doi: 10.2196/jmir.1581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wendorf CA (2004). Primer on multiple regression coding: Common forms and the additional case of repeated contrasts. Understanding Statistics, 3(1), 47–57. doi: 10.1207/s15328031us0301_3 [DOI] [Google Scholar]
- Wiliams V, Bruton A, Ellis-Hill C, & McPherson K (2007). What really matters to patients living with chronic obstructive pulmonary disease? An exploratory study. Chronic Respiratory Disease, 4(2), 77–85. doi: 10.1177/1479972307078482 [DOI] [PubMed] [Google Scholar]
- Williams V, Price J, Hardinge M, Tarassenko L, & Farmer A (2014). Using a mobile health application to support self-management in COPD: A qualitative study. British Journal of General Practice, 64(264), 392–400. doi: 10.3399/bjgp14X680473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson TD (1999). Models in information behaviour research. Journal of Documentation, 55(3), 249–270. Retrieved from http://www.emeraldinsight.com/doi/abs/10.1108/EUM0000000007145 [Google Scholar]
- Worth H & Dhein Y (2004). Does patient education modify behaviour in the management of COPD? Patient Education and Counseling, 52(3), 264–270. doi: 10.1016/S0738-3991(03)00101-0 [DOI] [PubMed] [Google Scholar]
- Zulman DM, Kirch M, Zheng K, & An LC (2011). Trust in the Internet as a health resource among older adults: Analysis of data from a nationally representative survey. Journal of Medical Internet Research, 13(1), e19. doi: 10.2196/jmir.1552 [DOI] [PMC free article] [PubMed] [Google Scholar]


