Highlights
-
•
Acute dacryocystitis presents as a pre-septal cellulitis, responds to systemic antibiotic and drainage without permanent visual loss.
-
•
We describe a healthy man presenting with complete visual loss following orbital cellulitis and abscess formation due to acute dacryocystitis.
-
•
The clinical, radiological, intraoperative and postoperative findings are discussed with review of all similar reported cases.
-
•
Our aim is to stress on prompt recognition of these cases for appropriate treatment to avoid catastrophic visual loss.
Keywords: Dacryocystitis, Orbital, Cellulitis, Case report
Abstract
Introduction
Acute dacryocystitis usually presents as a pre-septal cellulitis since the lacrimal sac lies anterior to the orbital septum. Orbital cellulitis secondary to acute dacryocystitis is very rare due to a variety of anatomic barriers to the orbit but can occur and result in abscess formation with risk of visual compromise.
Presentation of case
We describe a case of otherwise healthy adult who presented with complete visual loss following orbital cellulitis and abscess formation secondary to acute dacryocystitis. The clinical, radiological, intraoperative and postoperative findings are discussed.
Discussion
Typically, orbital cellulitis responds well to systemic antibiotic and surgical drainage without permanent visual loss. There are 7 cases reported in the literature of acute dacryocystitis complicated by permanent visual loss.
Conclusion
Patients with acute dacryocystitis need to be carefully monitored for signs of orbital cellulitis. Prompt recognition and appropriate treatment of this condition are essential.
1. Introduction
Acute dacryocystitis commonly causes pre-septal cellulitis as the lacrimal sac lies anterior to the orbital septum. Due to natural anatomic barriers to the orbit, orbital cellulitis secondary to acute dacryocystitis is very rare but has been reported resulting in abscess formation with risk of visual loss. Typically, orbital cellulitis responds well to systemic antibiotic therapy and surgical drainage without permanent loss of vision [1]. We describe a case of otherwise healthy adult who presented to our academic institution with complete visual loss following orbital cellulitis and abscess formation secondary to acute dacryocystitis. Our case has been prepared and reported in line with the SCARE criteria in: “The SCARE Statement: Consensus-based surgical case report guidelines”. International Journal of Surgery 2016; 34:180–186. The authors further stress that they have no financial disclosures related to their recommendations [1].
2. The case
A 35-year old male presented with pain, redness and eyelid swelling of the right eye for 3 days. His condition was rapidly progressing with proptosis, restricted eye movement and decreased vision in the right eye over the following day. He had no associated history of fever. He was otherwise healthy and had no history of trauma. Prior to his presentation, the right eye was completely normal with normal vision and eye movement. He had visited another hospital 2-days prior to his presentation to us but did not have any symptoms suggestive of cellulitis at that time. He was diagnosed with acute dacryocystitis and pre-septal cellulitis on the right side, was given oral antibiotics and discharged home with a follow up appointment in 3 weeks. Despite compliance with the oral antibiotics, his symptoms continued to worsen until he lost the vision in his right eye, which brought him to our emergency room seeking urgent medical advice.
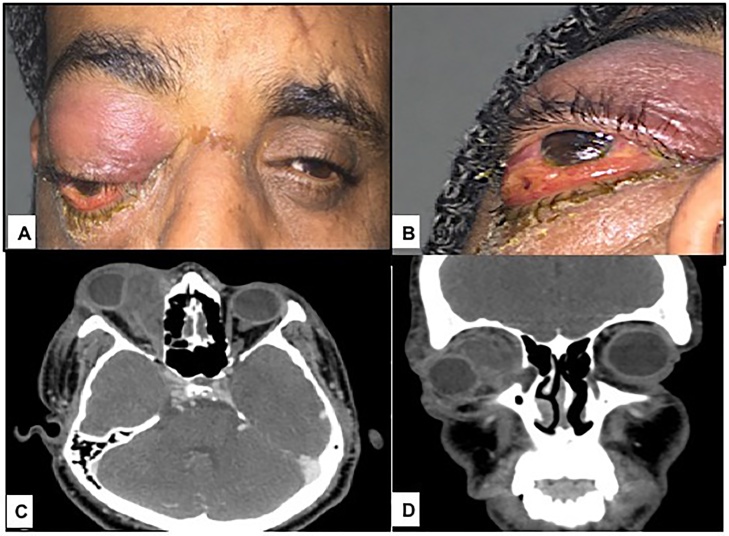
On evaluation, his vital signs were stable. The clinical examination showed right upper and lower eyelid erythema and edema, which was tense on attempted retropulsion, and right eye proptosis with complete ophthalmoplegia (Fig. 1A & B). The visual acuity of the right eye was no light perception and of the left eye was 20/20. The intraocular pressure of the right eye was 50 mmHg while it was 16 mmHg in the left eye. The right pupil was fixed, mid-dilated, and nonreactive to light. The slit lamp examination of the right eye showed conjunctival chemosis and signs of exposure keratopathy. Fundus examination of the right eye showed hyperemic disc and choroidal folds. The slit lamp examination and fundus examination of the left eye were unremarkable.
Fig. 1.
A & B: External photograph showing right eye dystopia and proptosis, right upper and lower eyelid edema and erythema and conjunctival chemosis. C & D: Axial and coronal CT of the orbit with contrast showing dilatation of the right lacrimal sac, a large extraconal non-enhancing fluid collection seen adjacent to the right medial rectus muscle and causing mass effect on the globe.
A computed tomography (CT) of the right orbit with contrast showed dilatation of the right lacrimal sac as well as the ipsilateral nasolacrimal duct. The lacrimal sac was showing rim enhancement extending into the extra-orbital post septal region. There was a large extraconal non-enhancing collection measuring 4.7 cm (anteroposterior) × 2.0 cm (transverse) × 2.1 cm (cranio-caudal) seen adjacent to the right medial rectus muscle and causing mass effect on the globe (Fig. 1C & D). The findings were in favor of right-sided dacryocystitis associated with orbital cellulitis and extraconal orbital abscess.
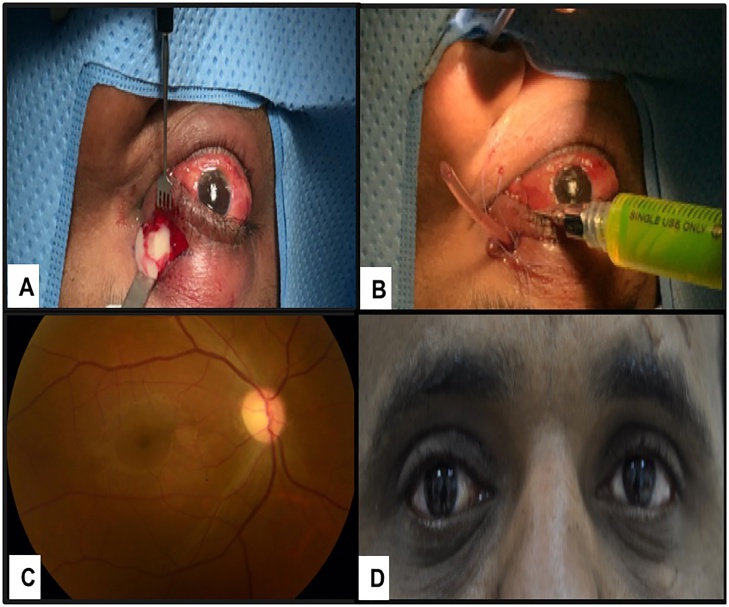
He was immediately started on intravenous ceftriaxone and clindamycin and underwent urgent surgical drainage of the abscess. Intraoperatively the abscess was drained from the lacrimal sac and medial part of the orbit (Fig. 2A) and a swab was taken from the purulent material for microbiology. Posterior rupture of the lacrimal sac into the orbit was expected. Irrigation was done using normal saline and cefazolin. Irrigation of the lacrimal drainage system showed the reflux coming through the drain which confirmed the nasolacrimal duct obstruction (Fig. 2B).
Fig. 2.
A: Significant purulent material was drained from the lacrimal sac and medial part of the orbit. B: Irrigation of the lacrimal drainage system showed the reflux coming through the wound drain which confirmed the nasolacrimal duct obstruction. C: Color fundus photo of the right eye showing temporal optic disc pallor. D: External photograph of the patient which was taken in the last follow up visit.
Postoperatively, proptosis had markedly reduced as well as the eyelid edema and erythema. Improvement in motility was also noted and conjunctival chemosis became much less. His visual acuity remained at no light perception. Culture results were positive for staphylococcus epidermidis which was sensitive to ceftriaxone and clindamycin. Intravenous dexamethasone was administered on the third postoperative day with marked improvement in the extraocular motility and periocular swelling. He was discharged on the seventh postoperative day on oral amoxicillin/clavulanic acid and was followed up as an outpatient. Three months later, he underwent right external dacryocystorhinostomy and intubation without complications. He was followed up regularly with a plan for stent removal 4 months after the surgery. He did not regain vision and developed right optic nerve atrophy (Fig. 2C & D).
3. Discussion
Dacryocystitis is an infection of the lacrimal sac due to nasolacrimal duct obstruction. Acute dacryocystitis can present as a pre-septal cellulitis, which generally involves soft tissue in the pre-septal area. Orbital cellulitis is a vision-threatening infectious process involving the ocular adnexal structures posterior to the orbital septum. Orbital cellulitis can rarely occur secondary to acute dacryocystitis and typically responds well to systemic antibiotic and surgical drainage without permanent visual loss [2]. The attachment of orbital septum to the lacrimal crest prevents the spread of infection to the posterior orbit. In addition, other anatomical structures such as the lacrimal fascia, the posterior limb of the medial canthal ligament, and deep heads of the pre-tarsal and pre-septal orbicularis muscles also act as a barrier to posterior extension. Orbital abscess secondary to dacryocystitis generally occurs in the medial and inferior aspects of the globe because of the anteroinferior location of the lacrimal sac. The anterior and inferior location of the lacrimal sac in relation to the globe can result in a channel of communication between the medial and inferior rectus muscles directly to the intraconal space, which can result in rapid loss of vision necessitating urgent surgical intervention [3].
There are 7 cases of visual loss following orbital cellulitis secondary to acute dacryocystitis reported in the literature. Summary of the cases (including ours) is shown in Table 1. Kikkawa et al. found that a prior episode of dacryocystitis is a risk factor for orbital extension by distension of the lacrimal sac and disruption of its posterior barriers. These barriers weaken from distension increasing the likelihood of posterior rupture and spread [3]. Although our patient had no history of dacryocystitis, chronic distention of the lacrimal sac may had led to posterior rupture and orbital extension. Other theories included spread of infection to ethmoid sinus via lamina papyracea, with subsequent extension from the sinus to the orbit [4]. Other causes include hematogenous spread from other systemic causes and, in some cases a primary orbital cellulitis that can extend into the lacrimal sac before the presence of dacryocystitis. Immunosuppression can also be a contributing factor [5].
Table 1.
Summary of all 8 cases of acute dacryocystitis complicated by orbital cellulitis and loss of vision including our present case.
| Author/year | Patient age/gender | VA on presentation/final VA | Location of orbital abscess /side |
Previous dacryocystitis | Mechanism of vision loss | Organisms |
|---|---|---|---|---|---|---|
| Kikkawa/2002, [3] | 38 years/ F 64 years/ F |
NLP/NLP LP/LP |
Extraconal/ left Intraconal / right |
Yes No |
Optic nerve compromise Optic nerve compromise |
Staphylococcus aureus. Nonenterococcal group D streptococci, streptococcus viridans, streptococcus intermedius. |
| Maheshwari/2009, [2] | 50 years/ F 65 years/ F |
NLP/NLP NLP/NLP |
Intraconal / right Extraconal / left |
Yes Yes |
Optic nerve compromise Optic nerve compromise |
Gram-positive diplococci. NS. |
| Coşkun/2011, [5] | 45 years/ F | LP/NLP | Extraconal / left |
No | Central retinal artery occlusion | Coagulase-negative staphylococcus. |
| Wladis/2016, [7] | 66 years/ F | NLP/NLP | NS | NS | Ophthalmic artery occlusion. | Streptococcus pyogenes. |
| Pfeiffe/2016, [14] | 50 years/ F | NLP/NLP | Extraconal / left |
No | Optic nerve compromise | Staphylococcus epidermidis. |
| Alsalamah */ 2018 | 35 years/ M | NLP/NLP | Extraconal / right |
No | Optic nerve compromise | Staphylococcus epidermidis. |
VA = visual acuity, F = female, M = male, NLP = no light perception, LP = light perception, NS = not specified.
present case.
The microorganisms found in dacryocystitis-induced orbital cellulitis are similar to the microorganisms found in uncomplicated dacryocystitis [6]. Intraoperative cultures revealed that Gram-positive bacteria are the most common pathogens [7]. The most frequently isolated microorganisms are Staphylococcus species (Staphylococcus aureus and coagulase-negative Staphylococcus) and Streptococcus species [8,9]. These microorganisms are also found in paranasal sinus infections [10]. The mechanism of vision loss is thought to be due to optic nerve compression and ischemia as in our patient or secondary to the elevation of intraocular pressure by the mass effect of the abscess, which results in central retinal artery obstruction or ophthalmic artery obstruction [5,7]. Thrombophlebitis in the valve-less orbital veins and optic neuritis caused by invasion of organism may also be an explanation [10,11]. Prompt diagnosis and emergency treatment is very essential in orbital infections. A delay in treatment can result in serious complications like vision loss, cavernous sinus thrombosis, meningitis, frontal abscess, and even death [9,12,13]. If an abscess is present, incision and drainage to prevent rupture of the lacrimal sac and posterior extension into the orbit is highly recommended, with dacryocystorhinostomy being the definitive treatment [14].
In conclusion, acute dacryocystitis should be considered as one of the causes of orbital cellulitis and abscess formation. Patients with orbital cellulitis and or orbital abscess should be questioned about symptoms of lacrimal drainage obstruction. We recommend that patients with acute dacryocystitis should be carefully monitored with very close follow up and should be warned about symptoms and signs of pre-septal and orbital cellulitis, which can rapidly progress and cause severe visual sequelae. Prompt recognition and appropriate treatment are essential to prevent visual loss.
Conflicts of interest
The authors have no conflict of interest related to this case report.
Funding
The Case report has been supported by King Saud University Medical City, however there were no funds involved.
Ethical Approval
Case reports do not require ethical approval at our institution.
Consent
General informed written consent has been obtained from the patient. The General informed written consent includes patient’s approval for anonymous use of relevant clinical and surgical information in an anonymous way.
Author contribution
Abrar K. Alsalamah: Review of chart, literature review and drafting of the case report
Hind M. Alkatan: Critical review and correction of the manuscript and the corresponding author.
Yasser H. Al-Faky: Surgical care of the patient and manuscript review
Registration of Research Studies
No Registration is needed for Case reports.
Guarantor
Hind Manaa Alkatan, MD
Acknowledgement
This work was supported by the College of Medicine Research Center, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia.
References
- 1.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., the SCARE group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34(October):180–186. doi: 10.1016/j.ijsu.2016.08.014. https://www.ncbi.nlm.nih.gov/pubmed/27613565 [DOI] [PubMed] [Google Scholar]
- 2.Maheshwari R., Maheshwari S., Shah T. Acute dacryocystitis causing orbital cellulitis and abscess. Orbit. 2009;28(2–3):196–199. doi: 10.1080/01676830902925529. https://www.ncbi.nlm.nih.gov/pubmed/19839913 Available from: [DOI] [PubMed] [Google Scholar]
- 3.Kikkawa D.O., Heinz G.W., Martin R.T., Nunery W.N., Eiseman A.S. Orbital cellulitis and abscess secondary to dacryocystitis. Arch. Ophthalmol. 2002;120(8):1096–1099. Available from: https://www.ncbi.nlm.nih.gov/pubmed/?term=Kikkawa+D.+O.,+Heinz+G.+W.,+Martin+R.+T.,+Nunery+W.+N.,+Eiseman+A.+S.+Orbital+cellulitis+and+abscess+secondary+to+dacryocystitis. Archives+of+Ophthalmology. [PubMed] [Google Scholar]
- 4.Ahrens-Palumbo M.J., Ballen P.H. Primary dacryocystitis causing orbital cellulitis. Ann. Ophthalmol. 1982;14:600–601. https://www.ncbi.nlm.nih.gov/pubmed/7114699 Available from: [PubMed] [Google Scholar]
- 5.Coşkun M., Llhan Ö., Keskin U. Central retinal artery occlusion secondary to orbital cellulitis and abscess following dacryocystitis. Eur. J. Ophthalmol. 2011;21(5):649–652. doi: 10.5301/EJO.2011.6493. https://www.ncbi.nlm.nih.gov/pubmed/21462155 Available from: [DOI] [PubMed] [Google Scholar]
- 6.Martins M.C., Ricardo J.R.S., Akaishi P.M.S., Velasco e Cruz A.A. Orbital abscess secondary to acute dacryocystitis: case report. Arquivos Brasileiros de Oftalmologia. 2008;71(4):576–578. doi: 10.1590/s0004-27492008000400020. https://www.ncbi.nlm.nih.gov/pubmed/18797671 Available from: [DOI] [PubMed] [Google Scholar]
- 7.Wladis E.J., Shinder R., LeFebvre D., Sokol J., Boyce M. Clinical and microbiologic features of dacryocystitis-related orbital cellulitis. Orbit. 2016;35(5):258–261. doi: 10.1080/01676830.2016.1176214. https://www.ncbi.nlm.nih.gov/pubmed/27399840 Available from: [DOI] [PubMed] [Google Scholar]
- 8.Liu I.T., Kao S.C., Wang A.G., Tsai C.C., Liang C.K., Hsu W.M. Pre-septal and orbital cellulitis: a 10-year review of hospitalized patients. J. Chin. Med. Assoc. 2006;69:415–422. doi: 10.1016/S1726-4901(09)70284-9. https://www.ncbi.nlm.nih.gov/pubmed/?term=Liu+IT,+Kao+SC,+Wang+AG,+Tsai+CC,+Liang+CK,+Hsu+WM.+Pre-+septal+and+orbital+cellulitis%3A+a+10-year+review+of+hospitalized+patients Available from: [DOI] [PubMed] [Google Scholar]
- 9.Chaudhry I.A., Shamsi F.A., Elzaridi E. Outcome of treated orbital cellulitis in a tertiary eye care center in the Middle East. Ophthalmology. 2007;114:345–354. doi: 10.1016/j.ophtha.2006.07.059. https://www.ncbi.nlm.nih.gov/pubmed/?term=Chaudhry+IA,+Shamsi+FA,+Elzaridi+E,+et+al.+Outcome+of+treated+orbital+cellulitis+in+a+tertiary+eye+care+center+in+the+Middle+East.+Ophthalmology+2007 Available from: [DOI] [PubMed] [Google Scholar]
- 10.Vairaktaris E., Moschos M.M., Vassiliou S. Orbital cellulitis, orbital subperiosteal and intraorbital abscess: report of three cases and review of the literature. J. Craniomaxillofac. Surg. 2009;37:132–136. doi: 10.1016/j.jcms.2008.10.007. https://www.ncbi.nlm.nih.gov/pubmed/?term=Vairaktaris+E,+Moschos+MM,+Vassiliou+S,+et+al.+Orbital+cellulitis,+orbital+subperiosteal+and+intraorbital+abscess%3A+report+of+three+cases+and+review+of+the+literature Available from: [DOI] [PubMed] [Google Scholar]
- 11.Schmitt N.J., Beatty R.L., Kennerdell J.S. Superior ophthalmic vein thrombosis in a patient with dacryocystitis- induced orbital cellulitis. Ophthal. Plast. Reconstr. Surg. 2005;21(5):387–389. doi: 10.1097/01.iop.0000176269.84949.96. https://www.ncbi.nlm.nih.gov/pubmed/16234708 Available from: [DOI] [PubMed] [Google Scholar]
- 12.Mauriello J.A., Jr., Wasserman B.A. Acute dacryocystitis: an unusual cause of life-threatening orbital intraconal abscess with frozen globe. Ophthal. Plast. Reconstr. Surg. 1996;12(4):294–295. https://www.ncbi.nlm.nih.gov/pubmed/8944391 Available from: [PubMed] [Google Scholar]
- 13.Ataullah S., Sloan B. Acute dacryocystitis presenting as an orbital abscess. Clin. Exp. Ophthalmol. 2002;30(1):44–46. doi: 10.1046/j.1442-9071.2002.00476.x. https://www.ncbi.nlm.nih.gov/pubmed/11885795 Available from: [DOI] [PubMed] [Google Scholar]
- 14.Pfeiffer M., Hacopian A., Merritt H., Phillips M., Richani K. Complete vision loss following orbital cellulitis secondary to acute dacryocystitis. Case Rep. Ophthalmol. Med. 2016:1–3. doi: 10.1155/2016/9630698. https://www.ncbi.nlm.nih.gov/pubmed/?term=Pfeiffer,+M.,+Hacopian,+A.,+Merritt,+H.,+Phillips,+M.+and+Richani,+K.+Complete+Vision+Loss+following+Orbital+Cellulitis+Secondary+to+Acute+Dacryocystitis Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]