Abstract
The prevalence of hypertension is highest among Black women, but treatment adherence is reportedly low. Stress unique to the experiences of Black Americans may be associated with low adherence and poor blood pressure control, but few studies have examined the relationships between stress, adherence, and blood pressure control among hypertensive Black women. This study seeks to fill gaps in research by examining the association between stress, adherence, and blood pressure control. The baseline sample (n = 571) of at-risk or hypertensive Black women from the SisterTalk II RCT (Northeastern USA, 2004–2006) to improve adherence to recommendations for hypertension was analyzed. Participants self-reported stress, pharmacological adherence, non-pharmacological adherence (i.e. lifestyle management such as diet and exercise), and demographics. Blood pressure and anthropometrics (BMI and waist circumference) were measured. Statistical analysis included ANOVA, t-tests, linear regression. Tests of mediation examined if adherence mediated the relationship between stress and blood pressure control. This study found that stress was associated with lower age (p < .001) and being a single parent (p < .001). Stress was also associated with higher systolic blood pressure (p = .029), and poor blood pressure control (p = .043). Participants who reported higher stress also reported lower non-pharmacological adherence (p = .042). Non-pharmacological adherence was found to mediate the association between stress and blood pressure control. Hence, results document a relationship between stress with non-pharmacological adherence and blood pressure control among Black American women. More research is necessary to examine the relationship between stress and treatment adherence.
Keywords: Stress, Pharmacological adherence, Non-pharmacological adherence, Hypertension, Blood pressure control, Black American women
Highlights
-
•
84% of Black women with hypertension were non-adherent to their anti-hypertensive medication.
-
•
59% of Black women with hypertension were non-adherent to lifestyle management for hypertension control (e.g. diet & PA).
-
•
Women who were non-adherent to lifestyle management reported greater stress and blood pressure compared to those adherent.
-
•
Adherence to lifestyle management strategies may be key to addressing the relationship between stress and blood pressure.
1. Introduction
The prevalence of hypertension in the United States has remained largely unchanged within the last decade, with age-adjusted overall prevalence among adults at 30.8% in 2013–2014 (CDC, 2016). Prevalence of hypertension was reported to be highest among Black Americans (43.3%), compared to White (29.1%), Hispanic (28.2%) and Asian Americans (26.5%) (CDC, 2016), with Black women having higher prevalence of hypertension compared to Black men (Abel and Efird, 2013; CDC, 2016). Hypertensive individuals are at an increased risk of cardiovascular diseases including coronary heart disease, stroke, congestive heart failure and peripheral arterial disease (Kotchen, 2012).
Despite the risk of other co-morbid conditions and complications, 52.8% of adults with hypertension have uncontrolled hypertension (Fryar et al., 2017). Uncontrolled hypertension is defined as having an average systolic blood pressure (BP) of 130 mm Hg or above or an average diastolic BP of 80 mm Hg or above that is either untreated or remains in this range despite antihypertensive medication prescription (Whelton et al., 2017).
Treatment adherence, including pharmacological and non-pharmacological adherence, has been found to be the main factor underlying uncontrolled hypertension (Kronish and Ye, 2013; Machado et al., 2016). Pharmacological adherence refers to the degree to which patients consume clinician-prescribed medications, such as diuretics, beta blockers, ACE inhibitors (defined as 80% or more of the medications that are consumed), while non-pharmacological adherence refers to lifestyle management (e.g. diet, including sodium and alcohol restrictions, and exercise) recommendations provided by healthcare providers (Haynes et al., 1980; Houston et al., 2011; Kronish and Ye, 2013). Adherence to pharmacological and non-pharmacological treatment guidelines is highly important for protecting cardiovascular health, but it is estimated that between 43% and 65% of hypertensive adults are treatment non-adherent (De Geest et al., 2014; Jankowska-Polanska et al., 2016; Jung et al., 2013). This is concerning because sustained non-adherence may increase the risk for future cardiovascular disease events, negatively impact quality of life, and increase health-related costs (Gosmanova et al., 2014).
Studies have documented the association between low treatment adherence, low BP control, and the adverse health impact of hypertension among Black Americans (Chobanian et al., 2003; Ephraim et al., 2014; Hong et al., 2016). Psychosocial determinants of health may influence treatment adherence among Black Americans. Numerous risk factors have been proposed for non-adherence to hypertensive guidelines among Black Americans. For example, lower rates of health insurance coverage and reduced access to health care for Black Americans have been associated with lower rates of BP control (Ephraim et al., 2014). A lack of understanding of what constitutes good hypertension treatment approaches, and self-management skills have also been suggested as possible factors (Ayotte et al., 2009; Boutin-Foster et al., 2007). In addition, lack of knowledge necessary to surmount barriers related to hypertension self-management (e.g. solving dietary problems that affect BP) may further contribute to the problem (Lesley, 2007). Medical mistrust may also be a factor in non-adherence to healthcare providers' advice (Abel and Efird, 2013; Abel and Greer, 2017). Pharmacologically, the higher frequency of side effects among Black hypertensive patients (as much as 2 to 4 times compared to other racial groups) may explain lower rates of pharmacological adherence (Chobanian et al., 2003). Though many potential causes have been suggested for non-adherence to hypertension treatment, the underlying factors specific to Black women for treatment non-adherence remain poorly understood (Abel and Efird, 2013). Thus, further research is warranted to better identify/understand the barriers to treatment adherence among Black women.
A potential and underexplored factor is the experience of stress, which has been suggested as a key driver of poor blood pressure control by the International Society on Hypertension in Blacks (Flack et al., 2010). Stress often forces individuals to readjust their attitudes, behavior, and cognition, which may adversely impact their mental and physical health (Thoits, 1995). Furthermore, chronic stress may contribute to the biological wear and tear leading to physiologic alterations and earlier health deterioration, or the “weathering”, of individuals (Geronimus et al., 1991). Long-term stress may contribute to allostatic load, which is the chronic over-activity or under-activity of allostatic systems (McEwen, 1998). Repeated activation of these systems may alter blood lipids, BP and result in the prolonged circulation of stress hormones and inflammatory cytokines that increase cardiovascular disease risk (Warren-Findlow, 2006).
Black Americans may be exposed to unique psychosocial stressors and report negative life events (e.g. discrimination) that directly affect cortisol and catecholamine that in turn, contribute to hypertension and arterial dysfunction (Charkoudian and Rabbitts, 2009; Hatch and Dohrenwend, 2007). In addition to the effects of stress on physical health, stress has also been posited to be a potential determinant of poor hypertensive treatment adherence (Darviri et al., 2016; Forsyth et al., 2014; Sparrenberger et al., 2009). For example, one study reported an association between the experience of discrimination and eating for reasons other than hunger among African American1 women (Johnson et al., 2012). However, despite the potential relationship between stress, adherence and BP outcomes for Black Americans, few studies examine these relationships among Black women. The aim of the current paper is to examine the potential associations between life stress, adherence (pharmacological and non-pharmacological) and BP control among Black women. Based on the Lazarus' cognitive model of stress and social cognitive theory, where a health behavior (e.g. treatment adherence) is affected by an individual's appraisal and experience of external stressors, (Bandura, 2001; Lazarus and Folkman, 1984) we hypothesize that: (1) life stress is associated with low treatment adherence and poor BP control, and (2) pharmacological and non-pharmacological adherence mediates the relationship between life stress and poor BP control.
2. Methods
2.1. Design and setting
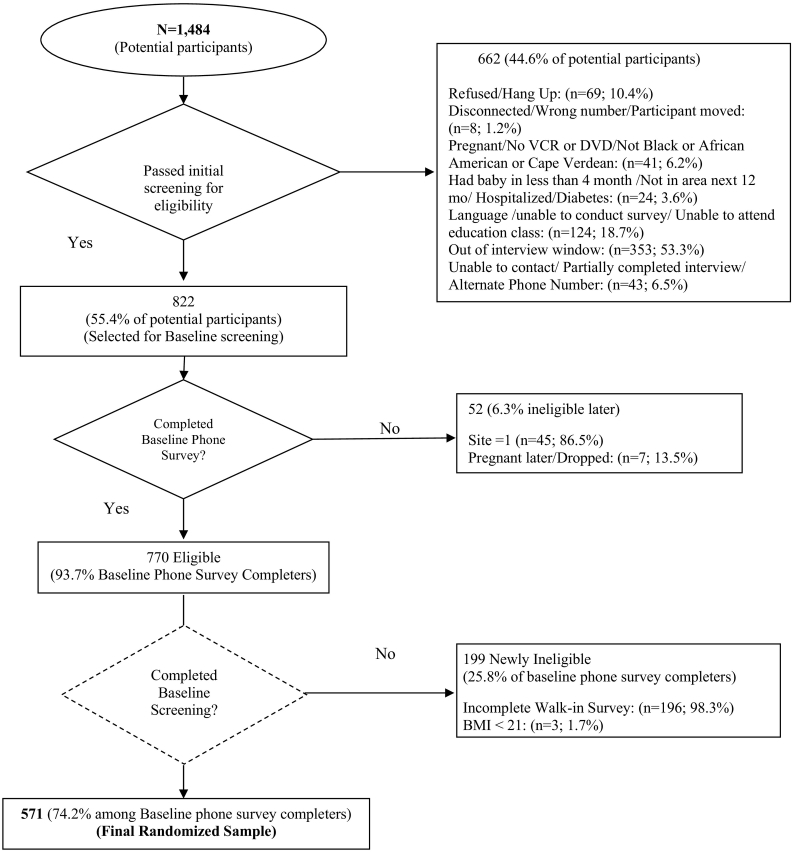
The present study examines baseline data from SisterTalk II, a clinical trial examining adherence to recommended changes in dietary and physical activity behaviors among Black women who were already hypertensive or at-risk (in the high-normal category) for hypertension (Risica and Kang, 2018) (See Fig. 1). The following definitions (based on the American College of Cardiology and American Heart Association) were used: “elevated” refers to blood pressure between 120 and 129 mm Hg systolic and less that 80 mm Hg diastolic; “hypertension” refers to blood pressure above 130 mm Hg systolic and 80 mm Hg diastolic; “controlled” blood pressure refers to measurements below 130 mm Hg systolic and 80 mm Hg diastolic for all participants (Whelton et al., 2017). Women were eligible to participate if they were over the age of 18 years, self-identified as Black, were hypertensive or high-normal, could speak and read basic English and had a BMI of at least 22 kg/m2. Exclusion criteria includes: pregnancy, having delivered a baby <4 months ago, is hospitalized, and diabetic. Participants were recruited from the Providence, Rhode Island and Boston, Massachusetts's metropolitan areas, between 2004 and 2006.
Fig. 1.
Recruitment of participants (Northeastern US, 2004–2006).
The following variables were measured as part of the broader SisterTalk II study: physical measures (height, weight, waist circumference, blood pressure), diet, physical activity, psychosocial measures (e.g. goal setting, motivation, self-efficacy, social support, knowledge, stress, adherence) were collected. Variables of interest of the present paper are further described below. A baseline survey was administered via telephone (where participants provided verbal consent). Participants provided a signed informed consent at recruitment clinics. The study received approval from the Brown University Institutional Review Board. The final sample was 571 participants.
2.2. Measures
2.2.1. Life stress
Life stress was measured using a single item question that was adapted for the SisterTalk study, “On a scale of 1 to 10, how stressful is your life? A 1 means your life is not stressful at all and a 10 means it is extremely stressful”. The response options ranged from 1 = not stressful at all to 10 = extremely stressful. This single-item question was validated against the Cohen perceived stress scale (rho 0.41 and p < .001).
2.2.2. Adherence
Adherence was assessed using two questions for adherence to pharmacological and non-pharmacological recommendations respectively. For pharmacological adherence, participants reported the number of days per week for the past 4 weeks that they took their medication(s) exactly as instructed. We used the cut-off point of 80% (i.e. 22 days) as recommended by Kronish and Ye (2013) as the definition of adherence to medication.
For non-pharmacological adherence, participants self-reported the frequency for the past 4 weeks that they followed their physician's treatment plan that includes: (1) following a low fat or weight loss diet, (2) limiting salt intake; (3) limiting alcohol consumption, and; (4) exercise. Response options are: 1 (none of the time), 2 (some of the time), 3 (most of the time), and 4 (all of the time). These four items were combined and averaged to create a composite score (Cronbach's α = 0.72). Thereafter, a binary variable (adherent vs. non-adherent) was created for all participants with using a cutoff score of 3 (i.e. on average, none of the items fall below “most of the time”).
2.2.3. Blood pressure control
BP measurements were obtained using a Welch/Allyn ‘Vital Signs’ (manufacturer) digital BP automated cuff. This device was previously validated against a mercury sphygmomanometer and met the criteria of the American Association for the Advancement of Medical Instrumentation (Jones et al., 2001). Prior to obtaining BP measurements, participants were seated at rest for 15 min with their feet flat on the floor. Appropriate cuff sizes based on the arm circumference of the participant were used to obtain BP readings. BP control was defined as <130/80 mm Hg according to the revised 2017 guidelines by the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (Whelton et al., 2017).
2.2.4. Covariates
Covariates included diabetic status, BMI (kg/m2), and waist circumference (cm). Using CDC guidelines, the classifications for BMI are: (1) Normal, 18.5 to 24.9 kg/m2, (2) Overweight, 25.0 to 29.9 kg/m2, (3) Obese. >29.9 kg/m2; for waist circumference, (4) women with waist circumference of 88 cm and over have increased disease risk for any given BMI category compared to women with waist circumference of <88 cm. (National Institutes of Health, 1998). Diabetic status was self-reported. Height was measured in centimeters with the use of a stadiometer (without shoes and headwear). Weight was measured in kg using balance beam scales with the participant in light clothing with their shoes removed. To assess waist circumference, we used a protocol for identifying the waist using a hip bone landmark as described by Chumlea and Kuczmarski (1995). Participants' height, weight, and waist circumference were measured by trained project staff.
Participants self-reported demographics including age, ethnicity, birthplace, education attainment, employment status, income, household composition (i.e. “lives alone”, “lives with children”, “lives with both adults and children”, “lives with other adults”), and number of people in the household. Ethnicity, birthplace, education attainment, employment, income, and household composition were categorical variables while age and number of people in the household while the demographic variables were continuous.
2.3. Statistical analysis
Descriptive statistics included means and standard deviations for continuous variables and frequencies and percentages for categorical variables. One-way analysis of variance (ANOVA) (for 3 or more levels of IV) or between-subjects t-test (for 2 levels of IV) was used to assess the association between categorical variables (i.e. income, ethnicity, education, household composition, BP control status, and adherence status) and continuous variables (i.e. stress). Linear regression analysis was used to assess the association between two continuous variables. The respective analytic methods are annotated in the results table. Significant univariate associations and covariates (diabetic status, BMI, waist circumference) were adjusted for accordingly. Mediation analysis was performed to test the direct/indirect pathways of life stress on BP as mediated by medication adherence, based on the mediation analyses method as described by Baron and Kenny (1986). Mediation effects were tested with the use of a macro provided by Preacher and Hayes (2008). The X-Y relationship is mediated by M if: (1) there is a significant association between X and Y, (2) there is a significant association between X and M, (3) there is a significant association between M and Y, and (4) the effect of X on Y after controlling for M is zero. If X is still significant after controlling for M, then the results support partial mediation. Covariates (diabetic status, BMI, waist circumference, and significant demographic variables) will be included in the model in addition to X, M, and Y (producing unadjusted and adjusted effects sizes for comparison), All analyses were conducted using SPSS version 24 (IBM Corp., 2015). Significance criterion was set at α < 0.05.
3. Results
The present study sample features a diverse demographic sample of Black women in terms of ethnicity, income, education, and household composition. The mean age of the sample was about 48 years old. About 67% of the participants were ethnically African American, 19% were ethnically Caribbean, 8% were ethnically Cape Verdean, and 6% ethnically Native American (Table 1).
Table 1.
Demographics, clinical variables and statistical analyses with stress (Northeastern US, 2004–2006).
| All (n = 571) |
Stress score |
Systolic BP |
Diastolic BP |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD n (%) |
Mean ± SD | Coefficient (SE)1 | p | Mean ± SD | Coefficient (SE)1 | p | Mean ± SD | Coefficient (SE)1 | p | |
| Age | 47.6 ± 11.7 | −0.701 (0.177) | <.001⁎ | 0.602 (0.062) | <.001⁎ | 0.123 (0.034) | <.001⁎ | |||
| 18 to 29 years | 42 (7) | 6.4 ± 2.4 | 114.9 ± 11.5 | 72.7 ± 9.0 | ||||||
| 30 to 39 years | 112 (20) | 6.7 ± 2.4 | 119.1 ± 16.0 | 76.8 ± 10.7 | ||||||
| 40 to 49 years | 146 (26) | 6.8 ± 2.7 | 125.3 ± 15.8 | 79.3 ± 8.5 | ||||||
| 50 to 59 years | 187 (33) | 5.8 ± 2.9 | 128.1 ± 17.2 | 78.7 ± 9.2 | ||||||
| Above 60 years | 84 (14) | 5.3 ± 2.7 | 140.2 ± 23.5 | 79.4 ± 9.8 | ||||||
| All (n = 571) |
Stress score |
Systolic BP |
Diastolic BP |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | F-statistic2 | p | Mean ± SD | F-statistic2 | p | Mean ± SD | F-statistic2 | p | ||
| Household income | 0.935 | .479 | 1.978 | .080 | 0.923 | .466 | ||||
| <10K | 106 (20) | 6.6 ± 3.1 | 126.9 ± 19.8 | 78.2 ± 8.1 | ||||||
| 10–20K | 78 (15) | 6.1 ± 2.6 | 126.2 ± 17.5 | 78.1 ± 9.9 | ||||||
| 21–30K | 108 (20) | 6.4 ± 2.7 | 129.5 ± 21.7 | 79.3 ± 10.2 | ||||||
| 31–40K | 81 (15) | 6.3 ± 2.7 | 124.8 ± 17.1 | 76.9 ± 9.3 | ||||||
| 41–70K | 103 (19) | 6.1 ± 2.3 | 122.7 ± 17.2 | 77.1 ± 10.0 | ||||||
| >70K | 54 (11) | 5.7 ± 2.6 | 122.1 ± 15.9 | 76.9 ± 9.4 | ||||||
| Education | 0.983 | .448 | 3.110 | .026⁎ | 2.089 | .101 | ||||
| Less than high school | 74 (13) | 6.2 ± 2.3 | 130.3 ± 22.4 | 79.3 ± 10.4 | ||||||
| High school graduate/GED | 160 (28) | 5.9 ± 2.9 | 127.4 ± 19.6 | 77.9 ± 9.3 | ||||||
| Some college | 181 (32) | 6.5 ± 2.5 | 126.7 ± 17.9 | 78.9 ± 9.3 | ||||||
| College and above | 150 (27) | 6.1 ± 2.4 | 122.8 ± 16.4 | 76.6 ± 9.7 | ||||||
| Ethnicity | 1.128 | .342 | 0.287 | .835 | 0.078 | .972 | ||||
| African | 380 (67) | 6.1 ± 2.7 | 126.4 ± 19.1 | 78.1 ± 10.1 | ||||||
| Caribbean | 108 (19) | 6.4 ± 2.3 | 125.7 ± 17.9 | 78.4 ± 8.8 | ||||||
| Cape Verdean | 44 (8) | 6.3 ± 2.3 | 126.2 ± 16.8 | 77.7 ± 7.6 | ||||||
| Native American | 33 (6) | 6.8 ± 2.8 | 129.2 ± 20.8 | 78.5 ± 7.7 | ||||||
| Household composition/lives with | 2.363 | .004⁎ | 4.859 | .002⁎ | 1.971 | .117 | ||||
| Children only | 127 (22) | 7.1 ± 2.7 | 124.6 ± 16.7 | 77.7 ± 8.9 | ||||||
| Other adults | 129 (23) | 5.6 ± 2.7 | 130.4 ± 20.03 | 79.7 ± 10.7 | ||||||
| Both adults and children | 190 (33) | 6.2 ± 2.6 | 123.2 ± 16.6 | 77.1 ± 9.3 | ||||||
| Alone | 125 (22) | 5.7 ± 2.7 | 128.7 ± 21.3 | 78.4 ± 9.3 | ||||||
| All (n = 571) | Stress | |||||||||
| All (n = 571) |
Stress score |
Systolic BP |
Diastolic BP |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Coefficient (SE)1, 3 | p | Mean ± SD | Coefficient (SE)1, 4 | p | Mean ± SD | Coefficient (SE)1, 5 | p | ||
| Systolic BP | 126.4 ± 18.7 | NA | 0.630 (0.288) | .029⁎ | NA | NA | NA | NA | NA | NA |
| Diastolic BP | 78.1 ± 9.6 | NA | 0.138 (0.148) | .058 | NA | NA | NA | NA | NA | NA |
| BMI | 36.4 ± 7.5 | NA | 0.019 (0.015) | .201 | NA | 0.178 (0.104) | .089 | 0.148 (0.053) | .005⁎ | |
| Normal | 12 (2) | 6.5 ± 3.1 | 119.1 ± 18.9 | 73.5 ± 9.2 | ||||||
| Overweight | 101 (18) | 5.9 ± 2.4 | 124.3 ± 20.2 | 76.7 ± 10.9 | ||||||
| Obese | 163 (29) | 6.1 ± 2.8 | 126.2 ± 17.5 | 77.7 ± 8.7 | ||||||
| Morbidly obese | 283 (51) | 6.3 ± 2.8 | 127.4 ± 18.9 | 78.9 ± 9.6 | ||||||
| Waist circumference | 106.8 ± 15.9 | NA | 0.004 (0.007) | .451 | NA | 0.096 (0.048) | .046⁎ | 0.072 (0.025) | .005⁎ | |
| <88 cm | 48 (8) | 6.2 ± 2.9 | 119.8 ± 17.8 | 74.3 ± 11.4 | ||||||
| ≥88 cm | 512 (92) | 6.1 ± 2.8 | 126.7 ± 18.1 | 78.5 ± 9.3 | ||||||
| All (n = 571) |
Stress score |
Systolic BP |
Diastolic BP |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | t-statistic2, 3 | p | Mean ± SD | t-statistic2, 4 | p | Mean ± SD | t-statistic2, 5 | p | ||
| Diabetic status | 0.684 | .409 | 3.177 | .075 | 0.827 | .363 | ||||
| Yes | 103 (18) | 6.0 ± 2.9 | 129.3 ± 19.9 | 77.3 ± 9.1 | ||||||
| No | 466 (82) | 6.2 ± 2.7 | 125.7 ± 18.4 | 78.3 ± 9.7 | ||||||
| BP control | 3.767 | .043⁎ | NA | NA | NA | NA | NA | NA | ||
| Yes | 370 (65) | 5.9 ± 2.8 | ||||||||
| No | 201 (35) | 6.3 ± 2.7 | ||||||||
Note.
Simple Linear Regression.
One-way ANOVA/t-test.
Adjusted for age and household composition.
Adjusted for age, education and household composition.
Adjusted for age only.
The average systolic/diastolic BP of the sample was 126/78 ± 18.7/9.6 mm/Hg (within the “elevated blood pressure” range of US national guidelines) (Whelton et al., 2017). The average BMI of the study sample was 36.4 ± 7.5 kg/m2 (CDC classification for “obese” is ≥30 kg/m2), and the average waist circumference was 106.8 ± 15.9 cm (CDC classification for “high risk” is >88 cm) (CDC, 2015). Sixty five percent (65%) of the sample achieved blood pressure control (Table 1), which is higher than the national average (about 54%) (Merai et al., 2016). Only 16% of participants were adherent to pharmacological treatment. Forty one percent (41%) of participants were adherent to non-pharmacological treatment.
Higher age was inversely associated with life stress (p < .001). Life stress scores were significantly different by household composition groups (p = .004). Participants who lived with only children (i.e. single mothers) reported significantly higher life stress scores compared to all other subgroups (with “other adults”, p < .001; with “both adults and children”, p < .001; “alone”, p = .011). Stress levels did not differ by any other demographic characteristic.
Stress was associated with higher systolic BP (p = .029). Stress scores were significantly higher among participants who did not have BP control than participants who had BP control (p = .043). No association was reported between BMI, waist circumference, and stress.
Age was significantly associated with systolic and diastolic BP (both p < .001). There were group differences in education on systolic BP, and participants with “less than high school” education had significantly higher systolic BP (p = .026). There were group differences in household composition on systolic BP. Participants who lived with other adults and who lived alone had higher systolic BP compared to those who lived with children only and with both adults and children (p = .002).
3.1. Adherence outcomes
No differences in stress scores were observed between participants who were pharmacologically adherent or non-adherent. However, stress scores were higher among participants who did not adhere to non-pharmacological recommendations compared to participants who were adherent (p = .042). (Table 2).
Table 2.
Adherence outcome and statistical analyses with stress (adjusted) (Northeastern US, 2004–2006).
| AllA |
Stress score |
Systolic BP |
Diastolic BP |
BP control |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | Mean ± SD | t-statistic1 | p | Mean ± SD | t-statistic1 | p | Mean ± SD | t-statistic1 | p | Yes | No | χ2/p | |
| Pharmacological adherence | 0.822 | .532 | 0.250 | .617 | 3.009 | .084 | .101/.750 | ||||||
| Adherent | 44 (16) | 6.6 ± 2.7 | 131.7 ± 15.3 | 82.8 ± 9.9 | 24 (17) | 20 (15) | |||||||
| Non-adherent | 233 (84) | 6.9 ± 2.6 | 133.3 ± 20.2 | 80.1 ± 9.5 | 121 (83) | 112 (85) | |||||||
| Non-pharmacological adherence | 2.551 | .042⁎ | 5.115 | <.001⁎ | 1.805 | .126 | 25.03/<.001⁎ | ||||||
| Adherent | 232 (41) | 6.0 ± 2.5 | 126.0 ± 19.0 | 78.2 ± 9.8 | 176 (44) | 86 (41) | |||||||
| Non-adherent | 335 (59) | 7.0 ± 2.6 | 127.0 ± 18.4 | 78.1 ± 9.8 | 220 (56) | 115 (59) | |||||||
Note. Data expressed as [M ± SD] or [n (%)].
Bolded texts denote which statistical test was used.
Between-subjects t-test.
Total participants on hypertensive medication prescription was n = 277; total participants prescribed a non-pharmacological regimen by clinicians was n = 567.
Participants who were non-pharmacologically adherent had lower SBP compared to participants who were non-adherence (p < .001), and there were more participants who were achieved BP control who were non-pharmacologically adherent.
3.2. Mediation analyses
Mediation analysis was not performed for pharmacological adherence as pharmacological adherence was not associated with stress, which is a criterion for mediation. Fig. 2 displays the mediation model of non-pharmacological adherence as a mediator of the relationship between stress and poor BP control. The criteria for mediation was met, with stress (X) reported to be negatively associated with non-pharmacological adherence (M) (a-path) (r = −0.31, p = .031) and BP control (Y) (c-path) (r = −0.29, p = .041). Non-pharmacological adherence was negatively associated with BP control (b-path) (r = −0.31, p = .045). The total effect (c′-path) of life stress on BP control was significant (r = −0.28, p = .044). Hence, non-pharmacological adherence partially mediated the relationship between stress and BP control.
Fig. 2.
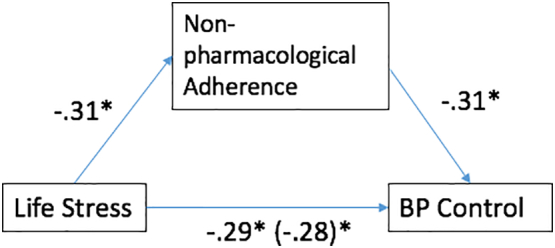
Mediation model for stress (X), non-pharmacological adherence (M), and BP control (Y), adjusted. (Northeastern US, 2005–2006).
4. Discussion
Using a cross-sectional sample obtained from the baseline results of the SisterTalk II study, this paper examines the relationship between stress, treatment adherence and BP control. Overall, our results generally supported the hypothesis that stress is associated with adherence and BP control. To our knowledge, no other studies have reported that non-pharmacological adherence mediates the relationship between stress and BP control.
Higher stress was found to be associated with higher systolic BP. In addition, higher stress was also reported among participants who did not achieve BP control. These findings are congruent with what has been reported in other studies with larger samples sizes (Bosworth et al., 2008; Hicken et al., 2014; Strogatz et al., 1997). Stress (especially long-term stress) is hypothesized to lead to changes in vascular structure and permanent increases in BP due to repeated activations in the sympathetic nervous system (Zimmerman and Frohlich, 1990).
Current literature has yet to conclusively define the causes of stress among hypertensive Black women. Some factors may include findings that hypertensive Black Americans perceive their health condition as more serious than Whites (Bosworth et al., 2006), which may increase their stress levels. In addition, a recent systematic review concluded that the experience of racial discrimination, which is posited to serve as a potent psychosocial stressor, is frequently associated with hypertensive status among Black adults (Dolezsar et al., 2014). However, more evidence is needed to conclusively address the relationship between stress and BP (Frommer et al., 1986; Mann, 2012). While the present paper did not assess perceived severity and discrimination, these potential constructs are relevant to a topic that is lacking research and future studies should examine these constructs.
Higher stress was reported among participants who were non-pharmacologically non-adherent. To the authors' knowledge, no studies have examined the relationship between stress and non-pharmacological adherence among Black hypertensive women. While the literature has established that the ability to manage stress is associated with health behaviors (e.g. consumption of a healthy diet and regular exercise) (Ogden, 2012), more research should be done to specifically examine how stress influences adherence among hypertensive Black women. Stress has been found to lead to the adoption of unhealthy behaviors as a coping mechanism, including the adoption of poor dietary practices, such as consuming fatty, sugary and calorie-dense foods as a form of short-term relief for stress (Park and Iacocca, 2014). Our study's results also support findings in the literature examining stress and physical activity. A literature review reported that stress impairs one's ability to engage in physical activity, though the exact mechanisms underlying this relationship remain largely unknown (Stults-Kolehmainen and Sinha, 2014).
While the relationship between stress and adherence among Black Americans is poorly understood, future studies should examine factors such as the patient-provider relationships, which may influence stress and adherence-related health outcomes. Black patients have an increased likelihood of experiencing negative outcomes when receiving clinical care from race-discordant (e.g. White) physicians (Martin and Cooper, 2013), with lower levels of trust in physicians being suggested to be one such negative outcome (Schoenthaler et al., 2014). Physician mistrust has been associated with racism-related stress (Harrell, 2000). These findings are important, as physician trust has also been shown to be a predictor of adherence to treatment recommendations (Cooper et al., 2003). Future studies should seek to further elucidate the relationship between trust, stress, and adherence.
No differences in stress levels were found between pharmacologically adherent and non-adherent groups. The relationship between stress and hypertensive medication adherence has not been thoroughly examined in the literature, though a recent study documented that stress (together with depression) accounted for significant variance in the association between perceived discrimination and medication adherence among hypertensive Black patients (Forsyth et al., 2014). No studies have directly examined the relationship between stress and pharmacological adherence among the hypertensive population, though qualitative research has reported that Black hypertensive patients mention stress as an impediment to medication adherence (Lewis et al., 2010). Hence, further research should attempt to explore this relationship, and in particular explore how different types of stressors (e.g. discrimination, SES, chronic vs. acute stressors, etc.) affect adherence.
Results of the present study should be interpreted with consideration for several limitations. Firstly, adherence measures were adapted for the current study and did not include previously validated measures such as the Morisky scale (Morisky et al., 1986) or objective indicators such as pill counts or pharmacy refill data. In using the 2017 ACC/AHA revised guidelines for hypertension, this study includes participants who may not have otherwise been prescribed pharmacological guidelines during the time of data collection, and hence there is a need to obtain new data. Additionally, the study did not distinguish the types of physician advice for non-pharmacological adherence such as diet or physical activity, and did not identify intentional or unintentional adherence related to medical therapies. The single-item measure used to assess stress did not separate out types of stress such as occupational stress, financial stress, socioeconomic or racial discrimination stressors that are known to differentially affect BP (Spruill et al., 2009), and also has yet to be validated. Future studies may also consider obtaining biological indicators of stress (e.g. salivary cortisol) to enhance the validity of stress measurement, although such approaches should consider, as we did, how medical mistrust may present as a barrier to participation. Furthermore, longitudinal studies directly examining the relationship between stress, adherence and blood pressure control across different geographical regions in the United States (e.g. extending beyond the Northeast to the South, Midwest, and West) are needed to enhance the reliability and generalizability of evidence.
The present study contributes significantly to the literature by filling gaps in research and documenting a relationship between stress, adherence and BP in an ethnically and socioeconomically diverse sample of Black American women. In addition, considering the comorbidity of hypertension and obesity (and that Black women have the highest prevalence of obesity compared to other racial groups), improving non-pharmacological adherence would be key to improving this health disparity (Nguyen et al., 2008; Ogden et al., 2014). In summary, findings indicate that women with higher systolic BP, with poor BP control and who were non-pharmacologically non-adherent reported higher stress. Non-pharmacological adherence mediated the relationship between stress and BP control, suggesting that following a healthy diet and active life style are important health behaviors in the management of hypertension, especially among Black women who experience higher stress.
Acknowledgments
National Heart, Lung, and Blood Institute, USA, 7R01HL069379.
Footnotes
This paper distinguishes between “African American” as an ethnicity and “Black” as a race.
References
- Abel W.M., Efird J.T. The association between trust in health care providers and medication adherence among Black women with hypertension. Front. Public Health. 2013;1:66. doi: 10.3389/fpubh.2013.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abel W.M., Greer D.B. Spiritual/religious beliefs & medication adherence in Black women with hypertension. J. Christ. Nurs. 2017;34(3):164–169. doi: 10.1097/CNJ.0000000000000333. [DOI] [PubMed] [Google Scholar]
- Ayotte B.J., Trivedi R., Bosworth H.B. Racial differences in hypertension knowledge: effects of differential item functioning. Ethn. Dis. 2009;19(1):23–27. [PubMed] [Google Scholar]
- Bandura A. Social cognitive theory: an agentic perspective. Annu. Rev. Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- Baron R.M., Kenny D.A. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bosworth H.B., Dudley T., Olsen M.K. Racial differences in blood pressure control: potential explanatory factors. Am. J. Med. 2006;119(1):70.e79-15. doi: 10.1016/j.amjmed.2005.08.019. [DOI] [PubMed] [Google Scholar]
- Bosworth H.B., Powers B., Grubber J.M. Racial differences in blood pressure control: potential explanatory factors. J. Gen. Intern. Med. 2008;23(5):692–698. doi: 10.1007/s11606-008-0547-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutin-Foster C., Ogedegbe G., Ravenell J.E., Robbins L., Charlson M.E. Ascribing meaning to hypertension: a qualitative study among African Americans with uncontrolled hypertension. Ethn. Dis. 2007;17(1):29–34. [PubMed] [Google Scholar]
- CDC . 2015. Healthy weight - Assessing your weight.https://www.cdc.gov/healthyweight/assessing/index.html (Retrieved from) [Google Scholar]
- CDC . 2016. Health, United States.http://www.cdc.gov/nchs/hus.htm (Retrieved from) [Google Scholar]
- Charkoudian N., Rabbitts J.A. Sympathetic neural mechanisms in human cardiovascular health and disease. Mayo Clin. Proc. 2009;84(9):822–830. doi: 10.4065/84.9.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chobanian A.V., Bakris G.L., Black H.R. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- Chumlea N.C., Kuczmarski R.J. Using a bony landmark to measure waist circumference. J. Am. Diet. Assoc. 1995;95(1):12. doi: 10.1016/s0002-8223(95)00003-8. [DOI] [PubMed] [Google Scholar]
- Cooper L.A., Roter D.L., Johnson R.L., Ford D.E., Steinwachs D.M., Powe N.R. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann. Intern. Med. 2003;139(11):907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- IBM Corp. IBM Corp; Armonk, NY: 2015. IBM SPSS Statistics for Windows, Version 24.0. [Google Scholar]
- Darviri C., Artemiadis A.K., Protogerou A. A HEALth Promotion and STRESS Management Program (HEAL-STRESS study) for prehypertensive and hypertensive patients: a quasi-experimental study in Greece. J. Hum. Hypertens. 2016;30(6):397–403. doi: 10.1038/jhh.2015.99. [DOI] [PubMed] [Google Scholar]
- De Geest S., Ruppar T., Berben L., Schonfeld S., Hill M.N. Medication non-adherence as a critical factor in the management of presumed resistant hypertension: a narrative review. EuroIntervention. 2014;9(9):102–109. doi: 10.4244/EIJV9I9A185. [DOI] [PubMed] [Google Scholar]
- Dolezsar C.M., McGrath J.J., Herzig A.J., Miller S.B. Perceived racial discrimination and hypertension: a comprehensive systematic review. Health Psychol. 2014;33(1):20–34. doi: 10.1037/a0033718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ephraim P.L., Hill-Briggs F., Roter D.L. Improving urban African Americans' blood pressure control through multi-level interventions in the Achieving Blood Pressure Control Together (ACT) study: a randomized clinical trial. Contemp. Clin. Trials. 2014;38(2):370–382. doi: 10.1016/j.cct.2014.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flack J.M., Sica D.A., Bakris G. Management of high blood pressure in Blacks: an update of the International Society on Hypertension in Blacks consensus statement. Hypertension. 2010;56(5):780–800. doi: 10.1161/HYPERTENSIONAHA.110.152892. [DOI] [PubMed] [Google Scholar]
- Forsyth J., Schoenthaler A., Chaplin W.F., Ogedegbe G., Ravenell J. Perceived discrimination and medication adherence in black hypertensive patients: the role of stress and depression. Psychosom. Med. 2014;76(3):229–236. doi: 10.1097/PSY.0000000000000043. [DOI] [PubMed] [Google Scholar]
- Frommer M.S., Edye B.V., Mandryk J.A., Grammeno G.L., Berry G., Ferguson D.A. Systolic blood pressure in relation to occupation and perceived work stress. Scand. J. Work Environ. Health. 1986;12(5):476–485. doi: 10.5271/sjweh.2115. [DOI] [PubMed] [Google Scholar]
- Fryar C.D., Ostchega Y., Hales C.M., Zhang G., Kruszon-Moran D. Vol. 289. 2017. Hypertension Prevalence and Control Among Adults: United States, 2015–2016; pp. 1–8. (NCHS data brief) [PubMed] [Google Scholar]
- Geronimus A.T., Andersen H.F., Bound J. Differences in hypertension prevalence among U.S. black and white women of childbearing age. Public Health Rep. 1991;106(4):393–399. [PMC free article] [PubMed] [Google Scholar]
- Gosmanova E.O., Lu J.L., Streja E., Cushman W.C., Kalantar-Zadeh K., Kovesdy C.P. Association of medical treatment nonadherence with all-cause mortality in newly treated hypertensive US veterans. Hypertension. 2014;64(5):951–957. doi: 10.1161/HYPERTENSIONAHA.114.03805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell S.P. A multidimensional conceptualization of racism-related stress: implications for the well-being of people of color. Am. J. Orthop. 2000;70(1):42–57. doi: 10.1037/h0087722. [DOI] [PubMed] [Google Scholar]
- Hatch S.L., Dohrenwend B.P. Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: a review of the research. Am. J. Community Psychol. 2007;40(3–4):313–332. doi: 10.1007/s10464-007-9134-z. [DOI] [PubMed] [Google Scholar]
- Haynes R.B., Taylor D.W., Sackett D.L., Gibson E.S., Bernholz C.D., Mukherjee J. Can simple clinical measurements detect patient noncompliance? Hypertension. 1980;2(6):757–764. doi: 10.1161/01.hyp.2.6.757. [DOI] [PubMed] [Google Scholar]
- Hicken M.T., Lee H., Morenoff J., House J.S., Williams D.R. Racial/ethnic disparities in hypertension prevalence: reconsidering the role of chronic stress. Am. J. Public Health. 2014;104(1):117–123. doi: 10.2105/AJPH.2013.301395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong K., Muntner P., Kronish I., Shilane D., Chang T.I. Medication adherence and visit-to-visit variability of systolic blood pressure in African Americans with chronic kidney disease in the AASK trial. J. Hum. Hypertens. 2016;30(1):73–78. doi: 10.1038/jhh.2015.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houston T.K., Allison J.J., Sussman M. Culturally appropriate storytelling to improve blood pressure: a randomized trial. Ann. Intern. Med. 2011;154(2):77–84. doi: 10.7326/0003-4819-154-2-201101180-00004. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health . 1998. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report.http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf Retrieved from. doi:98-4083. [PubMed] [Google Scholar]
- Jankowska-Polanska B., Blicharska K., Uchmanowicz I., Morisky D.E. The influence of illness acceptance on the adherence to pharmacological and non-pharmacological therapy in patients with hypertension. Eur. J. Cardiovasc. Nurs. 2016;15(7):559–568. doi: 10.1177/1474515115626878. [DOI] [PubMed] [Google Scholar]
- Johnson P., Risica P.M., Gans K.M., Kirtania U., Kumanyika S.K. Association of perceived racial discrimination with eating behaviors and obesity among participants of the SisterTalk study. J. Natl. Black Nurses Assoc. 2012;23(1):34–40. [PMC free article] [PubMed] [Google Scholar]
- Jones C.R., Taylor K., Poston L., Shennan A.H. Validation of the Welch Allyn ‘Vital Signs’ oscillometric blood pressure monitor. J. Hum. Hypertens. 2001;15(3):191–195. doi: 10.1038/sj.jhh.1001141. [DOI] [PubMed] [Google Scholar]
- Jung O., Gechter J.L., Wunder C. Resistant hypertension? Assessment of adherence by toxicological urine analysis. J. Hypertens. 2013;31(4):766–774. doi: 10.1097/HJH.0b013e32835e2286. [DOI] [PubMed] [Google Scholar]
- Kotchen T.A. Hypertensive Vascular Disease. 18 ed. McGraw-Hill; 2012. Chapter 247. [Google Scholar]
- Kronish I.M., Ye S. Adherence to cardiovascular medications: lessons learned and future directions. Prog. Cardiovasc. Dis. 2013;55(6):590–600. doi: 10.1016/j.pcad.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus, & Folkman . 1984. Coping and Adaptation. [Google Scholar]
- Lesley M.L. Social problem solving training for African Americans: effects on dietary problem solving skill and DASH diet-related behavior change. Patient Educ. Couns. 2007;65(1):137–146. doi: 10.1016/j.pec.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Lewis L.M., Askie P., Randleman S., Shelton-Dunston B. Medication adherence beliefs of community-dwelling hypertensive African Americans. J. Cardiovasc. Nurs. 2010;25(3):199–206. doi: 10.1097/JCN.0b013e3181c7ccde. [DOI] [PubMed] [Google Scholar]
- Machado J.C., Cotta R.M.M., Moreira T.R., da Silva L.S. Adherence to non-pharmacological treatment: analysis of the impact of three health educational and nutritional strategies in hypertensive patients. Rev. Nutr. 2016;29(1):11–22. [Google Scholar]
- Mann S.J. Psychosomatic research in hypertension: the lack of impact of decades of research and new directions to consider. J. Clin. Hypertens. (Greenwich) 2012;14(10):657–664. doi: 10.1111/j.1751-7176.2012.00686.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin K.D., Cooper L.A. Maximizing the benefits of “we” in race-discordant patient-physician relationships: novel insights raise intriguing questions. J. Gen. Intern. Med. 2013;28(9):1119–1121. doi: 10.1007/s11606-013-2448-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen B.S. Stress, adaptation, and disease. Allostasis and allostatic load. Ann. N. Y. Acad. Sci. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- Merai R., Siegel C., Rakotz M. CDC grand rounds: a public health approach to detect and control hypertension. MMWR Morb. Mortal. Wkly Rep. 2016;65(45):1261–1264. doi: 10.15585/mmwr.mm6545a3. [DOI] [PubMed] [Google Scholar]
- Morisky D.E., Green L.W., Levine D.M. Concurrent and predictive validity of a self-reported measure of medication adherence. Med. Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- Nguyen N.T., Magno C.P., Lane K.T., Hinojosa M.W., Lane J.S. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J. Am. Coll. Surg. 2008;207(6):928–934. doi: 10.1016/j.jamcollsurg.2008.08.022. [DOI] [PubMed] [Google Scholar]
- Ogden . 5 ed. McGraw Hill; 2012. Stress and Illness. [Google Scholar]
- Ogden C.L., Carroll M.D., Kit B.K., Flegal K.M. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park C.L., Iacocca M.O. A stress and coping perspective on health behaviors: theoretical and methodological considerations. Anxiety Stress Coping. 2014;27(2):123–137. doi: 10.1080/10615806.2013.860969. [DOI] [PubMed] [Google Scholar]
- Preacher K.J., Hayes A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods. 2008;30(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Risica P.M., Kang A.W. SisterTalk II: A Randomized Controlled Trial to Improve Adherence to Weight Loss for Hypertension Control among Black Women. Ann. Behav. Med. 2018;52(S1):S1–838. [Google Scholar]
- Schoenthaler A., Montague E., Baier Manwell L., Brown R., Schwartz M.D., Linzer M. Patient-physician racial/ethnic concordance and blood pressure control: the role of trust and medication adherence. Ethn. Health. 2014;19(5):565–578. doi: 10.1080/13557858.2013.857764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrenberger F., Cichelero F.T., Ascoli A.M. Does psychosocial stress cause hypertension? A systematic review of observational studies. J. Hum. Hypertens. 2009;23(1):12–19. doi: 10.1038/jhh.2008.74. [DOI] [PubMed] [Google Scholar]
- Spruill T.M., Gerin W., Ogedegbe G., Burg M., Schwartz J.E., Pickering T.G. Socioeconomic and psychosocial factors mediate race differences in nocturnal blood pressure dipping. Am. J. Hypertens. 2009;22(6):637–642. doi: 10.1038/ajh.2009.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strogatz D.S., Croft J.B., James S.A. Social support, stress, and blood pressure in black adults. Epidemiology. 1997;8(5):482–487. doi: 10.1097/00001648-199709000-00002. [DOI] [PubMed] [Google Scholar]
- Stults-Kolehmainen M.A., Sinha R. The effects of stress on physical activity and exercise. Sports Med. 2014;44(1):81–121. doi: 10.1007/s40279-013-0090-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoits P.A. Stress, coping, and social support processes: where are we? What next? J. Health Soc. Behav. 1995;Spec No, 53–79 [PubMed] [Google Scholar]
- Warren-Findlow J. Weathering: stress and heart disease in African American women living in Chicago. Qual. Health Res. 2006;16(2):221–237. doi: 10.1177/1049732305278651. [DOI] [PubMed] [Google Scholar]
- Whelton P., Carey R., Aronow W. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. Hypertension. 2017 [Google Scholar]
- Zimmerman R.S., Frohlich E.D. Stress and hypertension. J. Hypertens. 1990;Supplement, 8(4):S103–S107. [PubMed] [Google Scholar]