Highlights
-
•
This is an extremely rare case and quite challenging both to diagnose and to treat.
-
•
Immunostaining is sometimes needed to confirm the diagnosis.
-
•
Contrary to most similar reported case, the tumor recurred after surgery.
-
•
Although rarely needed, chemotherapy may successfully prevent tumor progression.
Keywords: Mediastinal liposarcoma, Mediastinal tumor, Rare, Surgery, Chemotherapy
Abstract
Introduction
Primary mediastinal dedifferentiated liposarcoma is an extremely rare malignant mesenchymal neoplasm composed of lipogenic tissue. It can be huge enough to compress heart and surrounding organs leading to clinical symptoms.
Presentation of case
We present a case of huge primary mediastinal dedifferentiated liposarcoma in a 54-year-old man, confirmed by immunohistochemistry staining, who received surgical removal. However, six months later, the tumor recurred, and the patient underwent chemotherapy for 6 cycles resulting in stable disease. Six months after the last visit, the tumor showed no sign of recurrence anymore.
Discussion
Among the various subtypes, the dedifferentiated mediastinal liposarcoma is the least found type of liposarcoma and often leads to misdiagnosis. Challenges occurred not only in diagnosis but also in treatment since it frequently grows back and chemotherapy may be needed after surgery.
Conclusion
This is a highly rare case of huge mediastinal liposarcoma that recurred after surgery and gave a satisfying outcome after chemotherapy.
1. Introduction
Liposarcomas are malignant mesenchymal tumors with varying degrees of atypia. It mostly found in lower limbs and retroperitoneum. Mediastinal liposarcoma (ML) is an extremely rare entity, accounting for about 1% of all mediastinal tumors, predominantly in posterior part, and less than 2% of all liposarcomas [1]. Dedifferentiated liposarcoma is the least common subtype of liposarcoma, particularly found in male over the fourth decades [2] and appear to be challenging to diagnose.
Due to its slow progression, around 15% of patient may be asymptomatic. The symptoms are related to tumor size and its invasion to adjacent organs. Most patients present with dyspnea, chest discomfort or cough. Patients may also present with superior vena cava syndrome [2] Most similar reported cases were successfully treated by complete surgical excision alone [1,2], but in this case, after removal of the giant tumor, it recurred 6 months later and leading for a need of chemotherapy.
All the works reported in this article were in line with the Surgical Case Report (SCARE) guideline [3].
2. Case report
A 54-year-old male presented with shortness of breath for 4 months, gradually worsened so severely that upon admission, he could no longer lying down, along with cough and swallowing difficulty. He was light smoker. Physical findings showed diminished breath sound in the left hemithorax.
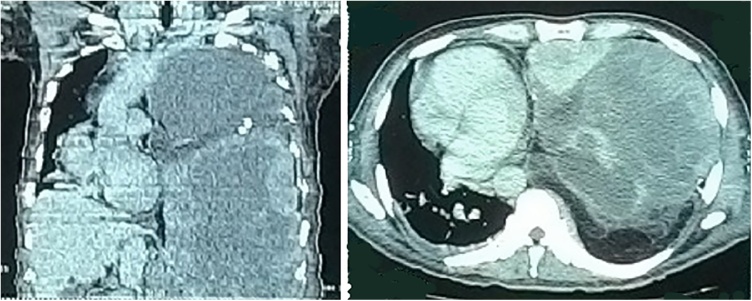
Complete blood count and serum tumor markers (AFP, Beta-HCG, LDH and CEA) were all within normal limit. Chest X-ray showed consolidation in almost the whole left hemithorax, shifting the trachea and mediastinum to the right. Thoracic CT-scan revealed a fat-containing mass with heterogenous density extending into the anterior mediastinum, enhanced with contrast, causing left lung atelectasis, suggestive for mediastinal teratoma with right minimal pleural effusion (Fig. 1).
Fig. 1.
The coronal and axial view of chest CT Scan revealed an inhomogeneous fatty mass in the left hemithorax, shifting heart and trachea to the right.
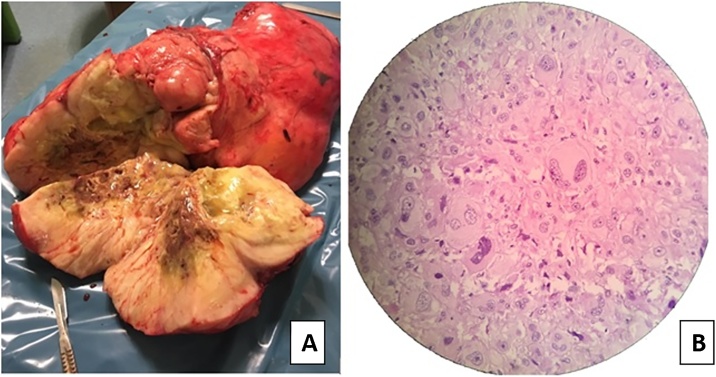
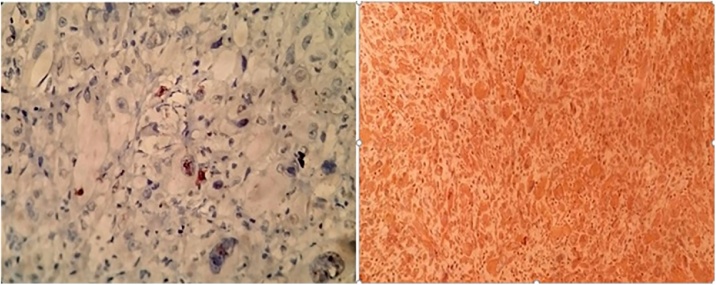
Cytology of transthoracic lung biopsy were inconclusive. Patient was then scheduled for median sternotomy, open biopsy and surgical removal. Upon surgery, a giant capsulated mass measuring 50 × 30 cm was removed (Fig. 2A). However, due to its invasion to the great blood vessels, it was not possible to remove all the tumor tissues, and we leave about 3 × 5 cm mass around innominate vein. Histopathologic findings revealed solid mass, composed of spindle-like cells forming herring-bone appearance, with enlarged nuclei and mitotic activity. In some spots, lipoblast cells were found (Fig. 2B). Immunohistochemistry staining of Pancytokeratin and CD-30 were both negative but turned out to be positive with Vimentin and S-100, confirming the diagnosis of primary dedifferentiated liposarcoma (Fig. 3). Post-operative chest X-ray showed the lung had fully re-expanded and symptoms resolved.
Fig. 2.
(A) Macroscopic view of the tumor, measured 50 × 30 cm.(B) Microscopic view shows spindle-like cells and lipoblast cells.
Fig. 3.
Immunohistochemistry of S100 (left) and Vimentin (right).
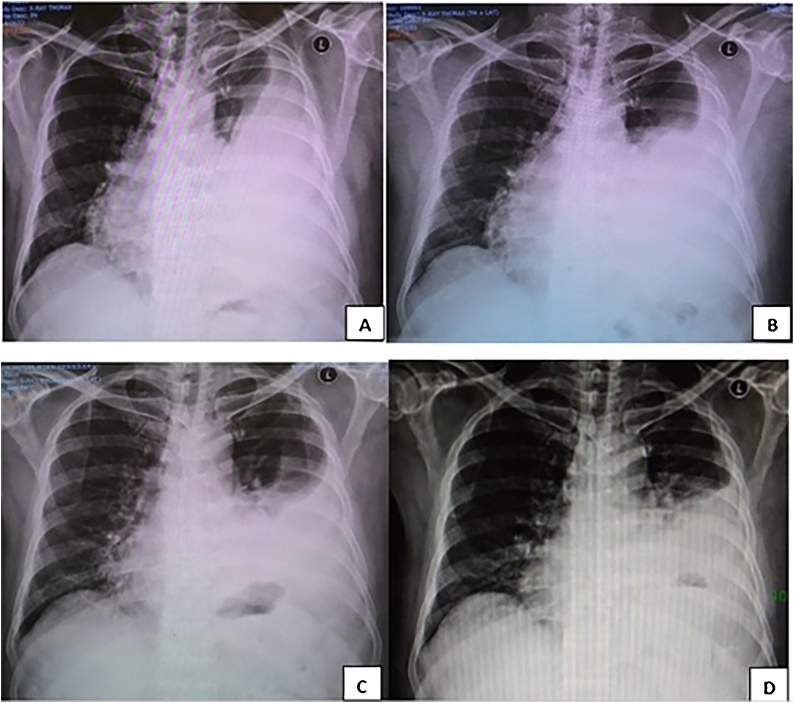
Because some little malignant tissues were still left in the mediastinum, the liposarcoma had high tendency for recurrence. Hence, we recommended the patient to undergo chemotherapy. Unfortunately, he never showed up until six months later, he came back with shortness of breath again. Chest x-ray and Thoracic CT scan revealed soft tissue mass and pleural effusion again in the left hemithorax. Patient was decided to undergo chemotherapy with Ifosfamide-Doxorubicin for 6 cycles. Serial follow up and response evaluation criteria in solid tumor (RECIST) concluded that he was in stable disease (Fig. 4) with minimal toxicity found (grade 0–1). He didn’t complain any respiratory symptoms and the laboratory findings after chemotherapy were all within normal limit. Patient was back to his daily activities and scheduled for routine follow up. Six months after the last chemotherapy cycle, no signs or symptoms of recurrence observed.
Fig. 4.
Serial chest X-ray. (A) Six months after surgical resection. (B) After 3 cycles chemotherapy. (C) After 6 cycles chemotherapy. (D) 4 months after chemotherapy.
3. Discussion
Primary mediastinal liposarcoma was firstly described in 1939, and due to its extremely low prevalence, there were only less than 200 cases reported to date [4]. There were many hypotheses regarding the origin of this tumor. Some authors stated that it arises within the adipose tissue of the adult thymus because from the hematoxylin-eosin staining, an attenuated rim of thymic tissue around the tumor mass was frequently found. However, this is quite controversial because most mediastinal liposarcomas were found in the posterior part. Therefore, some authors stated that it originated from primitive mesenchymal cells which still have lipogenesis property anywhere in mediastinum [4].
Based on histological findings, liposarcoma was initially classified into four subtypes: the well-differentiated, myxoid, round cell, and pleomorphic types. In 1979 a new subtype called dedifferentiated liposarcoma was introduced as the fifth subtype. The feature of dedifferentiated liposarcoma is the histological coexistence of a well to poorly differentiated liposarcoma and non-lipomatous differentiated areas. Molecular genetic alterations amplified sequences of chromosome region 12q13-15, including genes such as MDM2, CDK4 and CPM were supposed to be its origin [4,5].
The suspicion arises from CT images which usually showed varied-size mass which combines fat densities with attenuations similar to other soft tissues [1]. To confirm the diagnosis, clinicians should rule out the dedifferentiated liposarcoma by adequate sampling, cytogenetics, along with immunostaining for MDM2, CDK4, Vimentin or PPAR gamma [5].
Complete surgical resection of the tumor is in the only treatment of choice, and this is also the most important factors predicting postoperative survival time [6]. However, in some cases where tumor size is too big or causing adhesion with great vessels making it not possible to undergo complete removal and leave positive margin, re-resections should be considered. The rate of complete removal is 50% on average (15–78%) [7]. In this case, we left about 3 × 5 cm mass due to infiltration to innominate vein. Hence, he was planned for adjuvant chemotherapy, but unfortunately the patient never showed up until 6 months later when the tumor recurred.
Although dedifferentiated liposarcoma appears to have low sensitivity to radiation and chemotherapy, adjuvant therapy is still recommended [8], particularly to those with margins <10 mm after resection [8]. We decided the patient to undergo chemotherapy with six cycles regimen for sarcoma containing Ifosfamide-Doxorubicin. Upon completion of the regimen, serial CT images and RECIST revealed no more progression of tumor size and the patient was concluded stable disease and has reached 6 months progression-free survival.
4. Conclusion
Primary mediastinal dedifferentiated liposarcoma is extremely rare and appears to be challenging not only to diagnose but also to treat, due to its huge size extending to great vessels making complete surgical resection frequently not possible and hence, leading to high tendency for recurrence. Adjunctive chemotherapy may be prescribed particularly for tumors not fully resected and appears to be effective to prevent recurrence.
Conflict of interest
Authors of this manuscript have no financial or personal relationships with other people or organizations that could inappropriately influence or bias our work.
Funding
There was no financial funding or sponsors involved in the collection, analysis and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Ethical approval
Ethical approval has been exempted by the institution in which this manuscript was written and submitted from.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request. There is no ethical issue in this paper and all identifying names or identities have been omitted from the manuscript.
Authors contribution
The author Ken Min Chin has made substantial contribution in terms of acquisition of data, analysis and interpretation of data and drafting the article and writing the final paper. The authors Chung Yip Chan and Ser Yee Lee are in charge of the clinical care of the patient and have made substantial contribution in terms of analysis and interpretation of data, drafting the article, writing the final paper and revising the final manuscript for critically important intellectual content. All authors have approved the final version of the manuscript to be submitted.
Registration of research studies
This article is a case report. No trials or new experiment was conducted in this study.
Guarantor
Noni Novisari Soeroso.
References
- 1.Fernández-Tena A., López-González F.J. Mediastinal liposarcoma in a 30-year-old woman with dyspnea and chest pain. Respir. Med. Case Rep. 2017;21:86–88. doi: 10.1016/j.rmcr.2017.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barbetakis N., Samanidis G., Samanidou E. Primary mediastinal liposarcoma: a case report. J. Med. Case Rep. 2007;1:161. doi: 10.1186/1752-1947-1-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agha R.A., Fowler A.J., Saeta A. The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Chen G., Qiu X., Liu Y. Primary mediastinal pleomorphic liposarcoma involving the superior vena cava. Thorac. Cancer. 2014;5(3):265–270. doi: 10.1111/1759-7714.12084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wei S., Henderson-Jackson E., Qian X., Bui M.M. Soft tissue tumor immunohistochemistry update illustrative examples of diagnostic pearls to avoid pitfalls. Arch. Pathol. Lab. Med. 2017;141(8):1072–1091. doi: 10.5858/arpa.2016-0417-RA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhao X., Li P., Huang X., Chen L., Liu N., She Y. Prognostic factors predicting the postoperative survival period following treatment for primary retroperitoneal liposarcoma. Chin. Med. J. (Engl.) 2015;128(1):85–90. doi: 10.4103/0366-6999.147822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim E.-S., Jang S.-H., Park H.-C., Jung E.-H., Moon G.-B. Dedifferentiated liposarcoma of the retroperitoneum. Cancer Res. Treat. 2010;42(1):57–60. doi: 10.4143/crt.2010.42.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao C., Zhang F., Zhang X. Recurrent primary mediastinal liposarcoma: a case report. Oncol. Lett. 2016;11(6):3782–3784. doi: 10.3892/ol.2016.4453. [DOI] [PMC free article] [PubMed] [Google Scholar]