A Dieulafoy lesion is a rare vascular anomaly in the GI tract at risk for clinically significant bleeding. Here we present a case of clinically significant upper-GI bleeding secondary to a Dieulafoy lesion that was successfully treated with the help of a novel duodenoscope-friendly endoscopic clip.
A 71-year-old woman with a history of colonic diverticular bleeding treated with angiographic coil embolization of a branch of the left colic artery presented with painless hematochezia. She initially had stable hemodynamics and had acute on chronic anemia, with a hemoglobin level of 6.8 g/dL and hematocrit of 22%. The patient received a polyethylene glycol lavage in preparation for a colonoscopy; however, she continued to have hematochezia and became hypotensive.
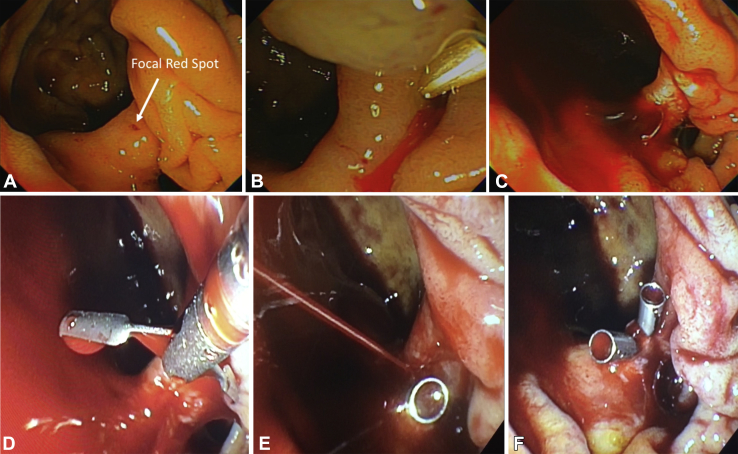
An upper endoscopy was urgently performed, and bright red blood was noted in the duodenum, but despite meticulous examination, no source of bleeding was identified. Examination with a duodenoscope noted a focal red spot along the rim of a periampullary diverticulum (Fig. 1A). We treated it with a bipolar cautery probe, during which the lesion initially oozed (Fig. 1B) and later led to brisk pulsatile bleeding. An attempt at combination therapy with epinephrine and bipolar cautery was unsuccessful (Fig. 1C).
Figure 1.
A, Focal red spot along the rim of the periampullary diverticulum. B, Treatment with bipolar cautery probe leading to oozing. C, Brisk pulsatile bleed not amenable to epinephrine and cautery. D, Duodenoscope view of Dieulafoy lesion with endoclip before deployment. E, Persistent pulsatile bleeding despite first endoclip placement. F, Hemostasis achieved after second endoclip.
The decision was made to apply mechanical therapy with a novel endoclip (DuraClip Repositional Hemostasis Clip; CONMED Corporation, Utica, NY) specifically designed for more effective use with a duodenoscope (Video 1, available online at www.VideoGIE.org). The endoclip features a small jaw-opening size that allows for easy maneuverability, greater field visibility, and a mechanism of deployment compatible with the elevator mechanism of the duodenoscope. Despite placement of the first clip (Fig. 1D), there was still brisk and actively spurting arterial bleeding (Fig. 1E). A second endoclip was placed, and complete hemostasis was achieved (Fig. 1F). The patient did well and was discharged after a few days of close monitoring.
Dieulafoy lesions account for 1% to 2% of acute GI bleeding, which has the potential to be life threatening.
Our case features the use of a duodenoscope for optimal evaluation of a bleeding lesion in a difficult location in combination with a novel endoclip that enabled precise and effective deployment and hemostasis, obviating the need for angiographic or surgical intervention.
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Treatment of a massive upper-GI bleed secondary to a duodenal Dieulafoy lesion with a novel duodenoscope-friendly endoclip.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Treatment of a massive upper-GI bleed secondary to a duodenal Dieulafoy lesion with a novel duodenoscope-friendly endoclip.