Abstract
Background
There is a national opioid misuse and overdose crisis. Consensus guidelines seek to inform practice and reduce risk; however, effect on clinician attitudes and knowledge remains unclear.
Methods
We surveyed 228 medical students and physicians in Wisconsin to assess their knowledge regarding at-risk patients, alternatives to opioids, and best treatment practices for opioid addiction. We also assessed attitudes about prescribing naloxone, relapse likelihood, and responsibility for the crisis.
Results
Knowledge and attitudes were similar, including that overprescribing by health care professionals is a driving factor. Attitudes on relapse likelihood were different, but both groups believed sustained recovery from addiction was possible.
Discussion
Enhancement of opioid-related education is both necessary to address knowledge gaps and desired by students and physicians.
INTRODUCTION
There is a crisis of opioid misuse, addiction, and overdose in the United States and in Wisconsin. 1 Prescription opioids caused 45% of overdose deaths in Wisconsin in 2013; heroin contributed an additional 27%.2 Among addiction treatment admissions in Wisconsin, opioids now rank second (17.4%) after alcohol (62.6%) as the primary substances of misuse among treatment seekers.3
Prescribers are a major source of illicitly used opioids. Users most commonly obtain them from a prescriber, family member, or friend. Additionally, many heroin-addicted individuals began their opioid use with an opioid prescription.4 The education of prescribers and trainees regarding opioid-related issues and risk management is crucial to alleviating the current crisis.
Previous studies indicate that clinician education on substance use disorders needs enhancement.5 Specifically, medical students and physicians at all levels receive inadequate education about the assessment and management of substance use disorders. This may result in a lack of confidence and ability to identify and address substance use disorders.5
Multiple recent practice guidelines and state legislative efforts have sought to reduce opioid-related harms as related to opioid prescribing.6 The development of consensus guidelines is intended to reduce variability in prescribing habits, which may be worsened by pharmaceutical marketing practices, differences in training, and variable state policies for handling opioid abuse. The extent to which attitudes and practices have been modified in this evolving policy environment remains unclear, and recent studies have indicated persistent, wide variation in attitudes, knowledge, and behavior.7
This study aimed to characterize knowledge and attitudes pertinent to opioid prescribing and related risks along the spectrum of physician training and practice in Wisconsin. A brief survey was administered to medical students and practicing physicians affiliated with the University of Wisconsin (UW) School of Medicine and Public Health to compare knowledge and attitudes at various stages in training to inform educational interventions.
METHODS
Study Recruitment
We recruited UW School of Medicine and Public Health medical students and physicians from 2 institutional email listservs. One listserv included all medical students (n=770) and the other included all physicians associated with the Department of Family Medicine (n=167). We focused on the Department of Family Medicine list because these physicians are on the front lines of managing chronic pain and thus serve as a good representation of primary care knowledge and attitudes. Participation was voluntary and no remuneration was offered. Due to the voluntary, limited nature of the survey and its anonymity, the study was deemed exempt from formal review by the University of Wisconsin’s Health Sciences Institutional Review Board. Prior approval from the school administration was obtained to utilize the listservs.
Survey
We created a 1-time, anonymous, web-based 10-question survey to assess facets of medical student and physician knowledge and attitudes regarding opioid addiction and related issues.
(See Appendix available at https://www.wisconsinmedicalsociety.org/_WMS/publications/wmj/pdf/117/1/Appendix%201_Supplementary%20Material%20Chouinard%20et%20al%20-%20Survey.pdf.) Questions were written with input from medical students, an addiction education organization (Wisconsin Voices for Recovery), and 2 primary care clinicians including an addiction medicine specialist. We utilized the Qualtrics software to allow ease of distribution and data analysis. An email containing a brief explanation and survey link was distributed to the listservs. Participants had 10 days to complete the survey, and a reminder was provided on day 8. The “Prevent Ballot Box Stuffing” setting within Qualtrics was selected to ensure only 1 submission per link. In addition to identifying their training level and department (the only demographic questions asked), participants were asked questions assessing their attitudes and knowledge related to opioid prescribing, opioid addiction, and the current opioid crisis. Questions assessing knowledge included identifying the type of patient at highest risk for opioid-related overdose, availability of naloxone, best treatment practices for opioid use disorder, and effective alternatives to opioid analgesics. Attitudes on prescribing naloxone, relapse likelihood, responsibility for the current opioid crisis, and chronic pain management practices also were queried. Finally, participants were asked an open-ended question on which related topics they would like to learn more about.
Data Analysis
We used Microsoft Excel 2016 to perform data analysis. Responses were compared between students and physicians using the chi-square test, with statistical significance defined as a P-value less than 0.05.
RESULTS
Of the 770 medical students who received the link, 170 surveys were completed (22% response rate, Figure 1). Fifty-eight percent (n = 98) of medical student respondents were in the preclinical years (M1 and M2), and 42% (n = 72) were in the clinical years (M3 and M4). Of the 167 physicians who received the link, 58 surveys were completed (35% response rate). All were currently practicing, and 53 were in family medicine, 2 were in internal medicine, 1 was in psychiatry, and 2 were in urgent care. Twenty-six percent (n = 15) of physician respondents were in practice less than 10 years, and 74% (n = 43) were in practice for more than 10 years.
Figure 1.
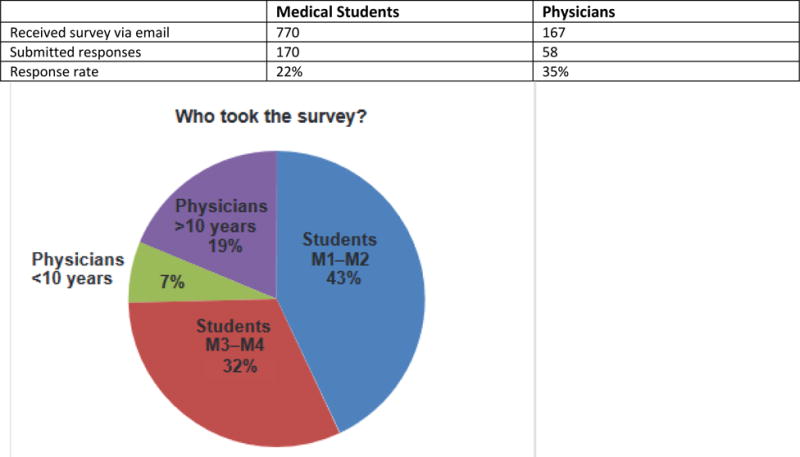
Data Showing Survey Response Rate and Level of Training Among All Respondents
We found many similarities in the responses between groups, but also several key differences (Figure 2), which we address in turn.
Figure 2.
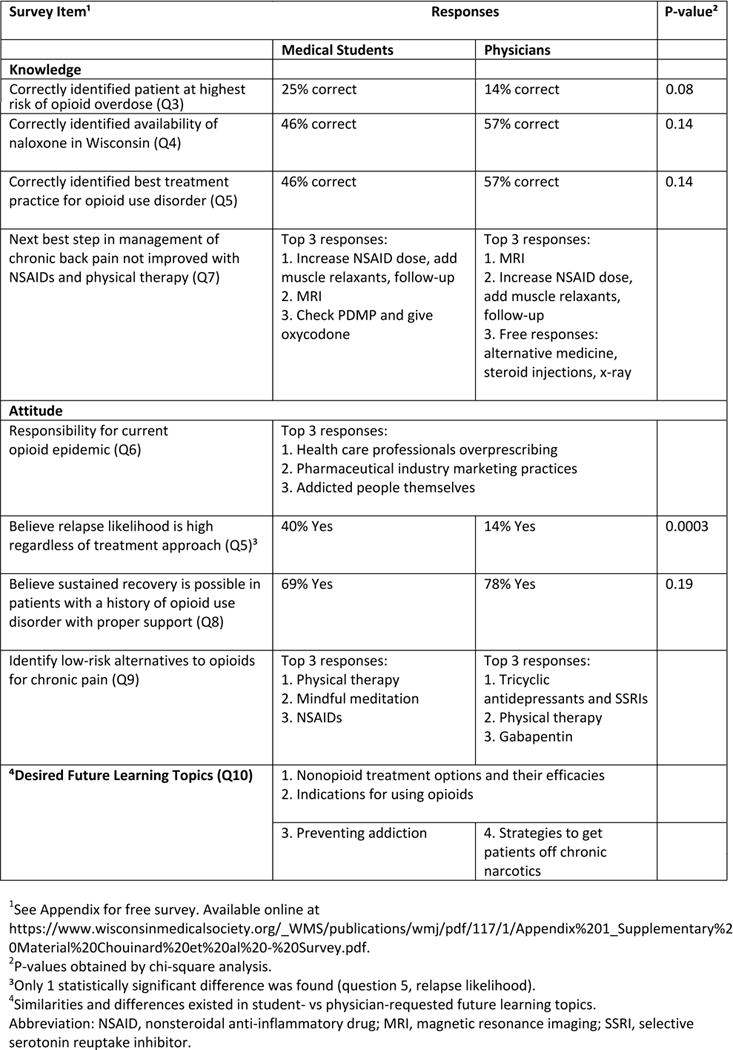
Responses for Knowledge and Attitude Questions
Similarities—Knowledge
Regarding the “knowledge” questions, only 25% of students and 14% of physicians correctly identified the highest risk patient for opioid-related overdose, with both choosing a young white man rather than a middle-aged white woman. Most physicians correctly identified the legal availability of naloxone in Wisconsin and the best treatment practice for opioid use disorder. In contrast, less than half of students selected these choices, although this difference was not statistically significant. To manage a patient with recalcitrant chronic back pain, the top 2 choices for both groups were to obtain magnetic resonance imaging and to utilize a higher NSAID dose with addition of a muscle relaxant.
Similarities—Attitudes
Regarding the “attitude” questions, both physicians and students supported harm reduction strategies through increased access to naloxone. (See survey question 4 in Appendix available at https://www.wisconsinmedicalsociety.org/_WMS/publications/wmj/pdf/117/1/Appendix%201_Supplementary%20Material%20Chouinard%20et%20al%20-%20Survey.pdf) and lower risk alternatives to chronic pain management, such as physical therapy. Both groups also believed sustained recovery is possible with proper support. Both groups ranked health care professionals as most responsible for the current opioid crisis, followed by pharmaceutical companies, and then the addicted people themselves. Both groups desired to learn more about nonopioid treatment options and their efficacies, as well as when opioids are indicated.
Differences
A few key differences existed between groups (Figure 2). Students were more likely than physicians to believe that relapse is likely regardless of treatment approach (P = 0.0003). In addition, medical students requested more information on strategies to prevent addiction, while physicians requested more information about how to wean patients off chronic opioids.
DISCUSSION
This study assessed student and physician attitudes and knowledge about opioid misuse and addiction in a large Midwest academic hospital. This setting is particularly relevant because Wisconsin and the Midwest are among the regions hardest hit by the escalating opioid crisis.1
Primary findings included that both groups acknowledged the key role of physician prescribing as the major source of opioids fueling the crisis. Students were more likely to believe that addicted patients have an elevated risk of relapse, regardless of treatment approach. This may suggest an early pessimism in trainees toward evidence-based therapies for use disorders. Given that relapse rates are as high as 91%,8 future opioid-related education should emphasize that relapse is a normal part of recovery. Similar knowledge deficits existed in physicians and students. Strikingly, both physicians and students failed to identify the highest-risk patient. Both groups expressed a desire for additional education on opioid addiction and alternatives for managing chronic pain.
Overall, our data demonstrate the need for meaningful changes to medical school curricula and for physician continuing educational opportunities. Medical education remains focused on the scientific aspect of disease and less on the human toll of chronic illnesses like opioid addiction. Efforts to change ingrained opioid prescribing habits may be enhanced by increasing learner exposure to this human toll.
Several studies have investigated attitudes and knowledge about opioid issues in students and clinicians, but only one included medical students.9,10 In this way, the current work expands on these previous studies by assessing both knowledge and attitudes, as well as suggesting possible areas to improve teaching.
There were several limitations that may affect the generalizability of our results. First, response rates were modest for both students and physicians. In addition, we chose to pool data from students in the M1-M2 “preclinical” and M3-M4 “clinical” years, which may blur differences by training stage. Second, although survey items were reviewed for content by multiple experts in opioid addiction, they were not rigorously validated. Third, in an effort to limit survey length and enhance response rates, we did not collect demographic information such as sex. This limits the ability to understand potential confounding or moderating factors. Finally, physician responses came primarily from family physicians. Different specialties may have different attitudes and knowledge about opioids. Future studies should investigate attitudes and knowledge in a larger pool of participants and should include other specialties, such as dentists, pharmacists, and nurses.
In conclusion, this work represents a step toward understanding educational needs of current and future clinicians. Such findings may guide curriculum and policy changes that could have a meaningful impact on the opioid abuse crisis, for which physicians play a central role as part of the current problem and must also be part of the solution.
Supplementary Material
Contributor Information
Skyler Chouinard, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin.
Aman Prasad, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin. Medical Scientist Training Program (MSTP).
Randall Brown, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin. Department of Family Medicine and Community Health.
References
- 1.Alcohol and other drug use statistics. Wisconsin Department of Health Services. 2015 https://www.dhs.wisconsin.gov/stats/aoda.htm. Accessed March 8, 2018.
- 2.Wisconsin special emphasis report: drug overdose deaths, 1999-2013. Wisconsin Department of Health Services. https://www.dhs.wisconsin.gov/publications/p01077.pdf. Accessed March 8, 2018.
- 3.TEDS Substance Abuse Treatment Admissions by Primary Substance of Abuse, According to Sex, Age Group, Race, and Ethnicity. Center for Behavioral Health Statistics and Quality. 2013 https://www.samhsa.gov/data/sites/default/files/2015%20TEDS_State%20Admissions.pdf. Updated 2016 Accessed March 8, 2018.
- 4.Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71(7):821–826. doi: 10.1001/jamapsychiatry.2014.366. [DOI] [PubMed] [Google Scholar]
- 5.Survey Research Laboratory, University of Illinois at Chicago. Missed opportunity: CASA National Survey of Primary Care Physicians and Patients on Substance Abuse. New York, NY: National Center on Addiction and Substance Abuse, Columbia University; 2000. [Google Scholar]
- 6.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. JAMA. 2016;315(15):1624–1645. doi: 10.1001/jama.2016.1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hwang CS, Kang EM, Kornegay CJ, Staffa JA, Jones CM, McAninch JK. Trends in the concomitant prescribing of opioids and benzodiazepines, 2002−2014. Am J Prev Med. 2016;51(2):151–160. doi: 10.1016/j.amepre.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 8.Smyth BP, Barry J, Keenan E, Ducray K. Lapse and relapse following inpatient treatment of opiate dependence. Ir Med J. 2010;103(6):176–179. [PubMed] [Google Scholar]
- 9.Weinstein SM, Laux LF, Thornby JI, et al. Medical students’ attitudes toward pain and the use of opioid analgesics: implications for changing medical school curriculum. South Med J. 2000;93(5):472–478. [PubMed] [Google Scholar]
- 10.Wolfert MZ, Gilson AM, Dahl JL, Cleary JF. Opioid analgesics for pain control: Wisconsin physicians’ knowledge, beliefs, attitudes, and prescribing practices. Pain Med. 2010;11(3):425–434. doi: 10.1111/j.1526-4637.2009.00761.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


