EUS-directed transgastric ERCP (EDGE) is a relatively new technique that has been made possible by the introduction of the lumen-apposing metal stent (LAMS). This procedure allows access to the biliary tract in patients with Roux-en-Y gastric bypass (RYGB) anatomy without the need of surgical intervention or balloon-assisted endoscopic procedures. In an EDGE procedure, a LAMS creates a temporary connection between the gastric pouch and the excluded stomach, allowing a direct pathway for the performance of ERCP. In this video we demonstrate EDGE in a step-by-step fashion (Video 1, available online at www.VideoGIE.org).
A 66-year-old woman with a history of RYGB was admitted because of right-upper-quadrant pain for 3 days. On admission, her vital signs were stable, and CT of the abdomen with intravenous contrast material revealed choledocholithiasis with a common bile duct measuring 10 mm. Her laboratory results were as follows: white blood cell count, 16.22/μL; hemoglobin, 10.7 g/dL; platelet count, 345,000/mL; bilirubin, 3.1 mg/dL; aspartate aminotransferase, 97 U/L; alanine aminotransferase, 62 U/L; and alkaline phosphatase, 366 U/L.
Given her postsurgical anatomy, the options of a laparoscopy-assisted procedure versus EDGE were presented and discussed with her. After detailed explanation of the risks and benefits of both procedures, she opted for EDGE in an attempt to avoid surgery.
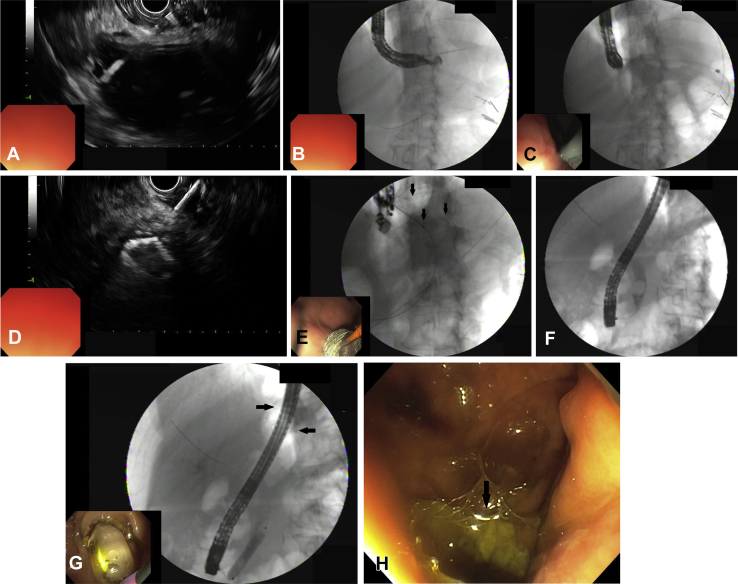
Using sonographic guidance, the excluded stomach was punctured with a 19-gauge FNA needle, and a 0.035-inch wire was passed into it using fluoroscopy (Figs. 1A and B). The hot Axios LAMS delivery system (Boston Scientific, Natick, Mass) was loaded over the wire and 2 attempts were made to access the excluded stomach; both were unsuccessful. The puncture tract was then dilated with an 8.5F Soehendra dilator (Wilson-Cook Medical, Winston-Salem, NC) (Fig. 1C). The gastro-gastric fistula was created by deploying the LAMS under sonographic and fluoroscopic guidance (Figs. 1D and E). After dilating the lumen of the LAMS, the duodenoscope was advanced to the major papilla to perform ERCP. The major papilla was small. Initial cholangiogram revealed a large stone in the distal CBD (Fig. 1F). Sphincterotomy and sphincteroplasty were performed prior to stone extraction (Fig. 1G). After completion of the procedure, the LAMS was intact and in an adequate position.
Figure 1.
A, Excluded stomach puncture. B, Wire in excluded stomach. C, Tract dilation. D, Distal flange of lumen-apposing metal stent (LAMS) in the excluded stomach. E, Fully deployed LAMS connecting gastric pouch and excluded stomach. F, Duodenoscope through the lumen of the LAMS. G, Impacted stone in the lower common bile duct. H, LAMS in place at the end of the procedure.
The 2 parts of the procedure (stent placement and ERCP) were performed the same day because of an imminent risk of ascending cholangitis. The day after the procedure, her vital signs were normal, her right-upper-quadrant pain had resolved, and her white blood cell count and liver enzymes started to normalize. She was discharged 2 days after the procedure with a follow-up appointment in our GI clinic in 2 weeks. At her follow-up visit, she had no complaints, and her liver enzymes had completely normalized. She had not noticed any weight gain.
Stent removal and closure of the gastrogastric fistula was performed 4 weeks after the initial procedure. Both were done successfully by use of the technique previously described in this journal by Crismale et al with a combination of cauterization of the fistula borders and endoscopic suturing.
EDGE is an effective technique to access the biliary tract in patients with Roux-en-Y anatomy. We recommend using general anesthesia during this procedure to avoid aspiration of fluid that may come from the excluded stomach. Surgical backup in case of adverse events is paramount when this procedure is performed.
Disclosure
The author disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
EUS-directed transgastric ERCP.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
EUS-directed transgastric ERCP.