Abstract
Background:
The accelerating accumulation of greenhouse gases in the Earth’s atmosphere is changing global environmental conditions in unprecedented and potentially irreversible ways. Climate change poses a host of challenges to the health of populations through complex direct and indirect mechanisms. The direct effects include an increased frequency of heat waves, rising sea levels that threaten low-lying communities, anticipated extremes in the global hydrologic cycle (droughts, floods, and intense storms), and adverse effects on agricultural production and fisheries due to environmental stressors and changes in land use. Indirectly, climate change is anticipated to threaten health by worsening urban air pollution and increasing rates of infectious (particularly waterborne and vector-borne) disease transmission.
Objective:
To provide a state-of-the-science review on the health consequences of a changing climate.
Findings:
Environmental public health researchers have concluded that, on balance, adverse health outcomes will dominate under these changed climatic conditions. The number of pathways through which climate change can affect the health of populations makes this environmental health threat one of the largest and most formidable of the new century. Geographic location plays an influential role the potential for adverse health effects caused by climate change, and certain regions and populations are more vulnerable than others to expected health effects. Two kinds of strategies are available for responding to climate change: mitigation policies (which aim to reduce greenhouse gas emissions) and adaptation measures (relating to preparedness for anticipated impacts).
Conclusions:
To better understand and address the complex nature of health risks posed by climate change, interdisciplinary collaboration is critical. Efforts to move beyond our current reliance on fossil fuels to cleaner, more sustainable energy sources may offer some of the greatest health opportunities in more than a century and cobenefits beyond the health sector. Because the nations least responsible for climate change are most vulnerable to its effects, the challenge to reduce greenhouse gas emissions is not merely technical, but also moral.
Keywords: extreme weather events, global climate change, greenhouse gas emissions, health, vulnerable populations
INTRODUCTION TO CLIMATE AND CLIMATE CHANGE
The overall energy budget of the planet, the balance between incoming shortwave radiation and outgoing longwave radiation, whether resulting from natural variability or from human activity, drive climatic change. This balance is mediated by the Earth’s atmosphere, in much the same way that the glass of a greenhouse allows sunlight to enter and then traps heat energy inside. An atmosphere with higher levels of greenhouse gases will retain more of this heat and result in higher average surface temperatures than will an atmosphere with lower levels of these gases.
Greenhouse Gases
Since the mid-1800s, the composition of the Earth’s atmosphere has changed dramatically from what it was in the preindustrial period. These changes include increases in atmospheric levels of carbon dioxide (CO2), methane (CH4), and nitrous oxide (N2O) that now exceed the highest concentrations recorded over the past 800,000 years, with mean rates of increase over the past century being unprecedented (with very high confidence) in the past 22,000 years.1 The concentration of CO2, the most significant of the greenhouse gases, has risen by approximately 35%, from about 280 parts per million by volume (ppmv) in the late 1800s to about 400 ppmv at present. This growth has accelerated over the past decade, as 2011 emissions were 43% higher than in 2005.1 Higher greenhouse gas concentrations have contributed to warming of the Earth by absorbing and reemitting infrared radiation toward the lower atmosphere and the Earth’s surface. From 1880 to 2012, the global average temperature rose by 0.85°C according to multiple independently produced datasets. By the end of this century, the average global temperature is projected to rise between 1.5°C and 4°C.2 The rate of change in global temperatures is faster now than during any period over the past thousand years.
Earth System Changes
Despite greenhouse warming being itself a dramatic effect across the Earth’s surface, changing temperatures are only part of the story. Higher temperatures evaporate soil moisture more quickly (potentially leading to severe droughts); yet, warm air can hold more moisture than cool air and can trigger heavy precipitation events; such hydrologic extremes (e.g., floods and droughts), which are of substantial concern to public health professionals. Additionally, the Arctic and Antarctic ice caps are melting, releasing vast amounts of water into the oceans, raising ocean levels, and potentially altering the flow of ocean currents.
Increasing global temperatures are associated with corresponding Earth system changes. Between 1971 and 2010, sea levels rose on average by approximately 2 mm per year. Arctic perennial sea ice extent declined by about 11.5% per decade over this period, and snow cover and glaciers have diminished in both hemispheres.3 According to the Intergovernmental Panel on Climate Change (IPCC), sea level will rise between 26 and 98 cm by 2100.
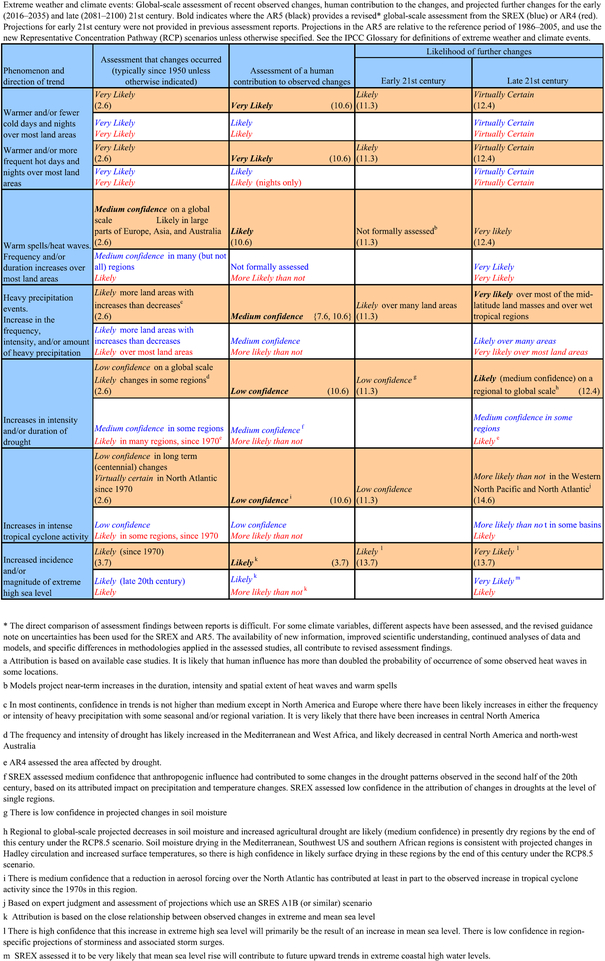
The potential exists for large-scale and potentially irreversible changes in Earth systems, such as slowing of the ocean circulation that transports warm water to the North Atlantic, large-scale melting of the Greenland and west Antarctic ice sheets, and accelerated warming due to positive feedbacks in the carbon cycle (such as the release of methane from thawing Arctic tundra). The probability of these events is unknown, but it is likely to be affected by how rapidly climate change evolves and its duration. Figure 1 shows the likelihood of these and other extreme events as determined by the IPCC’s most recent report.4
Figure 1.
Extreme weather and climate events: global scale assessment of recent observed changes.4
CLIMATE CHANGE CONSEQUENCES ON HEALTH
Particularly Vulnerable Regions
Geographic location plays an influential role in the potential for adverse health effect linked to climate change.5 Thus, certain regions and populations are more vulnerable than others to the health effects of climate change.6 These vulnerable areas include:
-
1.
Populations within or bordering regions with a high endemicity of climate-sensitive diseases (e.g., malaria).
-
2.
Areas with an observed association between epidemic disease and weather extremes (e.g., El Niño—linked epidemics).
-
3.
Areas at risk from combined climate effects relevant to health (e.g., stress on food and water supplies).
-
4.
Areas at risk from concurrent environmental or socioeconomic stresses and with little capacity to adapt.
Earth system changes have direct and indirect implications for human health. The sections that follow address major categories of anticipated health effects of climate change. These include risks from weather extremes, natural disasters, air pollution, and infectious diseases, particularly those that are water-, food-, or vector-borne.
Direct Consequences on Human Health
Weather extremes
Heat waves.
Extremes of both hot and cold temperatures are associated with rates of morbidity and mortality higher than rates in the intermediate, or comfortable, temperature range.7 The relationship between temperature and morbidity and mortality is J-shaped, with a steeper slope at higher temperatures.8 In the United States, extreme heat events cause more deaths each year than all other extreme weather events combined, and frequency of daily temperatures over 100°F is expected to increase substantially. Temperatures now occurring once in 20 years could happen every 2 to 4 years.9 The previous decade was the warmest on record in the United States.10
In the United States, an average of 658 deaths are classified as directly attributable to heat-related causes annually.11 The total population health effect of heat stress, however, is likely due more to the fact that heat-related deaths are routinely classified under other proximate causes.12 An estimated 20,000 people were killed in the United States from 1936 through 1975 by the effects of heat and solar radiation (National Safety Council, Environmental Health Center, 2001), with more than 3,400 deaths occurring between 1999 and 2003. The 1995 Chicago heat wave took approximately 600 lives over 5 days.13 The 2003 European heat wave is estimated to have killed more than 40,000 people in just 2 weeks, with more than 70,000 overall, while a Russian heat wave caused more than 15,000 deaths in 2010.14 Researchers estimate that the probability of mega-heat waves (those that break centuries-long seasonal temperature records) will increase by a factor of 5 to 10 within the next 40 years.15
Reduced extreme cold.
As an increase in summer temperature-related mortality is consistently anticipated in studies of climate change, so are at least partially compensating decreases in winter cold-related deaths. However, relatively milder winters attributable to climate change are unlikely to offset the more severe health effects of summertime extremes.16 Modeling of future summer and winter climate scenarios for New York City and Europe indicates that the net effect of future warming will be an increase in the number of annual deaths.17,18
Natural disasters.
Extreme storms, floods, tropical cyclones, wildfires, windstorms, landslides, and droughts have claimed millions of lives during the past several decades and have adversely affected the lives of many more millions of people while causing extensive property damage. From 1970 to 2012, 1.94 million deaths and US $2.4 trillion of economic losses were reported globally as a result of 8335 disasters directly linked to meteorologic and hydrologic conditions.19 In less developed regions, disasters can trigger large-scale dislocation of populations, often to places ill-prepared to welcome and care for the refugee populations deluged with undernutrition and communicable diseases. Displaced groups are also commonly subjected to risks for violence, sexual abuse, and mental illness. Overall, crude mortality rates in such displaced populations may reach as high as 30 times baseline, with much of the mortality occurring in children under the age of 5.20
Storms and floods.
Under most scenarios of climate change, the IPCC expects an increase in the frequency, intensity, and/or amount of heavy precipitation events.21 Globally, the IPCC projects that the area affected by monsoon systems will increase over the 21st century, with monsoon precipitation likely to intensify.22 These heavy downpours can cause or amplify flooding events. Floods are the most frequently occurring natural disaster, and globally the frequency of river flood events has been increasing.23 Conservative estimates report that around 2.8 billion people were affected by floods between 1980 and 2009, causing an estimated 500,000 deaths.24 Flooding also can elevate risks for drowning, injuries, hypothermia, and infectious diseases, such as cryptosporidium, giardia, leptospirosis, cholera, diarrheal disease, and vector-borne disease.25 High population densities in high-risk areas such as floodplains and coastal zones increase vulnerability. Degradation of the local environment also contributes significantly to vulnerability. For example, Hurricane Mitch, the most deadly hurricane to strike the Western Hemisphere in the past 2 centuries, caused 11,000 deaths in Central America, many due to mudslides in deforested areas, with thousands more people still recorded as missing.26
Wildfires.
The incidence of extensive wildfires in the western United States rose 4-fold between the 1970 to 1986 and 1987 to 2003 periods.27 Several climate-related factors may have played a role in this increase in wildfires: droughts that desiccate forests, higher springtime temperatures that hastened spring snowmelt and thereby lowered soil moisture, and rising numbers of tree pest species that caused tree death.27
The health effects of wildfires are wide ranging, threatening health directly through human fatalities and burns and through reduced air quality. Fire smoke carries large amounts of fine particulate matter that exacerbates cardiac and respiratory problems such as asthma and chronic obstructive pulmonary disease for those within the immediate vicinity of fires as well as in areas downwind. Numerous studies have shown that human health can be severely affected by wildfires, with certain populations being particularly vulnerable, such as young children, those with asthma, or those with other respiratory illnesses.28
Ocean temperatures and hurricanes.
Records indicate that sea surface temperatures have steadily increased over the past century, and more sharply over the past 40 years. Ocean warming is the largest near the surface, where the upper 75 m warmed by 0.11°C in the decade between 1971 and 2010. The IPCC confirms that it is very likely that the globally averaged ocean temperatures will increase in the near future.21
These ocean temperature trends in turn have implications for hurricane activity (also known as tropical cyclones). Hurricanes form only in regions where sea surface temperatures are above 26°C.29 During the late 1990s, overall hurricane activity in the North Atlantic doubled and the Caribbean experienced a 5-fold increase.30 Hurricane intensity also may be associated with warmer temperatures.31,32 As Hurricane Katrina demonstrated in 2005, such events have enormous public health significance. Despite this evidence surrounding warmer sea temperatures and hurricanes, current IPCC projections under 21st-century warming indicate that it is likely that the global frequency of hurricanes will either decrease or remain essentially unchanged; however, there is potential for an increase in both the global mean hurricane maximum wind speed and rainfall rates.22
Sea-level rise.
Sea surface warming also causes a rise in sea level due to thermal expansion of salt water; the melting of small glaciers also causes sea levels to rise. One expected effect is an increase in flooding and coastal erosion in low-lying coastal areas. This will endanger large numbers of people, with 14 of the world’s 19 current megacities (those exceeding 10 million in population) situated at sea level. The health consequences of sea-level rise include population displacement, lost livelihood, and exposure to coastal storm surges and floods.18
Global sea levels rose 17 cm throughout the 20th century, and are likely to rise more rapidly throughout the 21st century.33 Midrange IPCC estimates project a 26- to 98-cm sea-level rise by the 2080s, which could cause the loss of up to 22% of the world’s coastal wetlands.34 Current global estimates suggest that more than 200 million people are vulnerable to flooding during temporary extreme sea-level events produced by storms, putting them at risk for a range of health problems including displacement, salt water intrusion into fresh water aquifers, and disruption of storm water drainage and sewage disposal systems.33
Effect on food production.
Climate change is likely to have major effects on global crop and livestock production and on the viability of fisheries.35 Some changes will be positive and others negative, and the net effect on food production will likely vary from place to place. Changes in food production will depend on several key factors. First are the direct effects of temperature, precipitation, CO2 levels (e.g., relating to the CO2 fertilization effect), extreme climate variability, and sea-level rise.36
Drought is also projected to be an increasing problem with climate change for certain areas of the world. Approximately 1.7 billion people (one-third of the world’s population) currently live in water-stressed countries, and that number is projected to increase to 5 billion people by the year 2025.37 Drought will exacerbate undernutrition, still one of the world’s greatest health challenges, with 800 million people currently undernourished.38 Poorer countries already struggle with large and growing food-insecure populations and are particularly vulnerable to changes in food production. Climate change projections suggest that the number of undernourished children under the age of 5 may increase by 20 to 25 million (17%–22%), with an increase in the global malnourished by 49 million (11%).39
Decreases in average annual stream flow are anticipated in central Asia and southern Africa, where the food supply may be especially affected. Melting of many of the glacial systems that supply dry season river flow to more than a billion people is already occurring. Current projections suggest that glaciers of the Tibetan plateau are likely to melt entirely by year 2035.40 Additionally, diarrhea and diseases such as scabies, conjunctivitis, and trachoma are associated with poor hygiene and can result from a breakdown in sanitation when water resources become depleted.41 The Organisation for Economic Cooperation and Development (OECD) projects that about 1.4 billion people will be without access to basic sanitation in 2015 under a “business as usual” scenario with mid-range population growth within communities.42
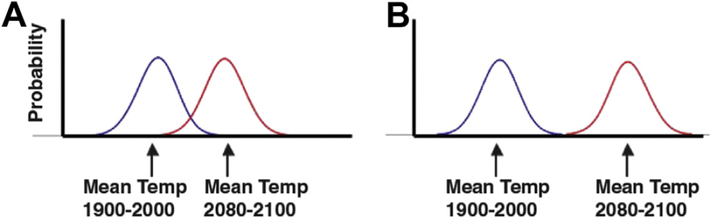
Despite technological advances such as improved crop varieties and irrigation systems, food production depends on weather conditions.43 A recent study shows a high probability that by the end of this century, the average growing season temperatures will exceed the hottest temperatures on record from 1900 to 2006 (Fig. 2).44 Reduced yields are expected to occur throughout the tropics due to heat stress, and crops may be damaged from flooding, erosion, and wildfires. Climate change effects on global agricultural productivity will vary regionally, with reductions especially likely in sub-Saharan Africa and South Asia.45 Reductions in regional productivity could destabilize food security on a global scale.44
Figure 2.
Hypothetical distributions of summer season temperatures from 1900 to 2000 and 2080 to 2100. The x axis indicates seasonal temperature; the y axis, probability of occurrence (number of years in the century). (A) The highest growing-season temperature of the 20th century represents the median seasonal temperature by the end of the 21st century. (B) Future temperatures are out-of-bounds hot: that is, it is certain that the growing season temperature at the end of the 21st century will exceed the hottest growing season ever observed.44
Climate change also may threaten the health of fisheries. The recent slowing of the North Atlantic Gulf Stream may reduce the abundance of plankton, a major source of food for many fish larvae.46 Declining larval fish populations will affect the capacity of over-exploited fish stocks to recover. Threats to global fisheries in turn threaten coastal and island populations that rely on fish as their main source of protein. Fish represent 16% of the animal protein consumed by people worldwide. Climate change, together with other pressures such as overfishing, may seriously threaten this nutrition source.
INDIRECT ECOSYSTEM-MEDIATED EFFECTS OF CLIMATE CHANGE ON HEALTH OUTCOMES
Air Pollution
Rising levels of air pollution due to climate change rank high among future health concerns, according to international assessments.47 Global epidemiological analyses estimate that ambient urban air pollution in the form of fine particulate matter (PM2.5, solid particles, and condensed liquid droplets of diameter 2.5 microns or smaller) and ozone (O3) caused 3.2 million premature deaths in 2010, rendering this exposure the dominant environmental threat to health.48
Accelerating climate change is anticipated to affect air pollution levels by altering atmospheric chemical reaction rates, boundary layer conditions affecting the vertical mixing of pollutants, and changes in airflow affecting the transport of pollution.49
Ozone.
Ozone is a secondary pollutant formed in the presence of sunlight as a result of chemical reactions between nitrogen oxide gases (NOx) and volatile organic compounds (VOCs). Natural emissions of VOCs comprise a significant fraction of total hydrocarbon levels, and in some areas exceed emissions from anthropogenic sources.50 Warm weather accelerates both the formation and destruction of O3 in the atmosphere, and so the net effect of climate change on O3 concentrations is unclear.51
For 15 cities in the eastern United States, the average number of days exceeding the health-based 8-hour O3 standard is projected to increase by 60% (from 12 to almost 20 days each summer) by the 2050s because of warmer temperatures.52 In California, higher temperatures are projected to increase the frequency, intensity, and duration of conditions conducive to air pollution formation—potentially by up to 85% for high-ozone days in Los Angeles and the San Joaquin Valley.53
Particulate matter.
Particulate matter is consistently implicated as the most damaging air pollutant to human health.54 These particles are both directly emitted by natural sources (wind-blown dust and smoke) and human activities (primarily the combustion of fossil fuels for transportation and energy), and formed secondarily in the atmosphere through chemical reactions of NOx, sulfates, and hydrocarbons with sunlight and water vapor.
Because of the complex chemical composition of PM2.5 and its weak correlation with meteorologic variables, the effects of climate change on PM2.5 levels are uncertain.47,49 Global climate modeling suggests that changes in surface cyclone circulation patterns are expected to reduce precipitation rates and increase the frequency of stagnant air masses and the accumulation of particulate concentrations at mid-latitudes worldwide.55
Aeroallergens.
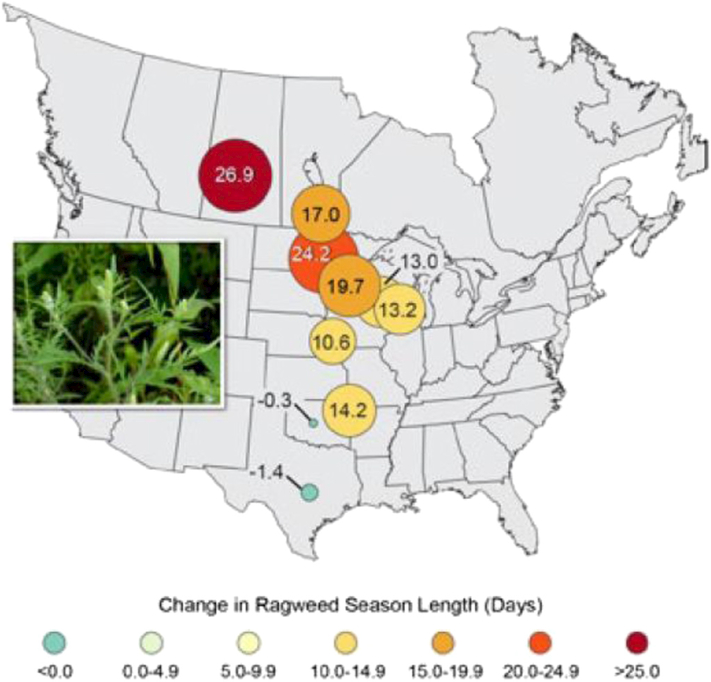
Pollen is another air contaminant that may increase with climate change. Higher levels of CO2 promote growth and reproduction by some plants, including many that produce allergens. For example, ragweed plants experimentally exposed to high levels of CO2 can increase their pollen production several-fold, perhaps part of the reason for rising ragweed pollen levels in recent decades (Fig. 3).56,57 Ragweed season has been lengthening since the mid-1990s along a 1600-mile north-south transect through mid-North America, particularly at higher latitudes.58
Figure 3.
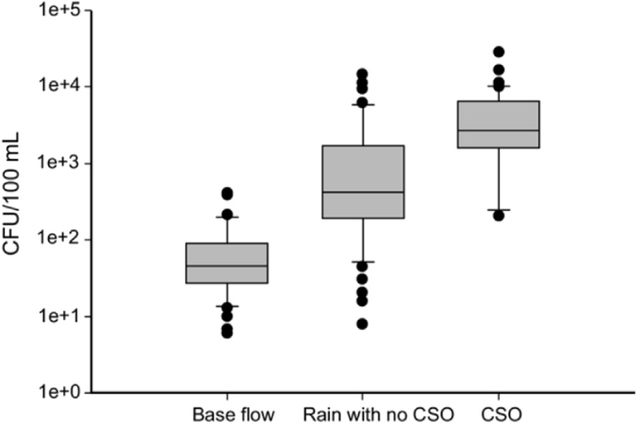
Levels of Escherichia coli in the Milwaukee estuary, which discharges to Lake Michigan, 2001–2007, during base flow (n46); following rain events with no CSO (n70); and following CSO events (n54). Boxes indicate 75% of values, with median values drawn in each. Whiskers are 95% of value and outliers are shown as closed circles. There were significant differences in E coli levels following rainfall and CSOs compared with base flow (P ≤ .05).5 Abbreviations: CFU, colony-forming units; CSO, combined sewer overflow.
Infectious Disease
A range of infectious diseases can be influenced by climatic conditions. The diseases most sensitive to influence by ambient climate conditions are those spread not by person-to-person pathways but directly from the source: the water- and foodborne diseases as well as vector-borne diseases (which involve insects or rodents within the pathogen’s life cycle).
Water- and foodborne diseases.
Water- and foodborne diseases are likely to become a greater public health problem as climate change accelerates, due to elevated temperatures, increases in extreme rainfall and flooding frequency, and an anticipated deterioration in water quality following wider drought events.
Freshwater ecosystems.
Waterborne diseases are particularly sensitive to changes in the global hydrologic cycle, as both water quantity and water quality play a role in the transmission of these diseases. Outbreaks of waterborne diseases are not random events, and disease outbreaks from most waterborne pathogens are distinctly seasonal and cluster in key watersheds.8 There is strong evidence that links incidence of waterborne outbreaks from pathogens such as Cryptosporidium,59 Escherichia coli 0157:H7,60 and Campylobacter jejuni60 following heavy rainfall events. Storm events of more than 3 inches of rainfall within 24 hours can overwhelm combined sewer systems and lead to an overflow that contaminates recreational and drinking water sources.61 Climate change is anticipated to increase the frequency of these events. Regional climate models for the Great Lakes area of the United States, suggests a 50% to 120% increase in sewage overflow events by the end of this century (Fig. 4).61
Figure 4.
Ragweed pollen season lengthens. Ragweed pollen season length increased in central North America between 1995 and 2011 by as much as 11 to 27 days in parts of the United States and Canada in response to rising temperatures. Increases in the length of this allergenic pollen season are correlated with increases in the number of days before the first frost. As shown in the figure, the largest increases have been observed in northern cities. (Data updated from Ziska et al. 2011;58 Photo credit: Lewis Ziska, USDA).102
Marine ecosystems.
Warm water and increased nitrogen levels favor marine algae blooms, including 2 groups, dinoflagellates and diatoms that can release toxins into the marine environment. These harmful algal blooms (HABs)—previously called red tides—can cause acute paralytic, diarrheic, and amnesic poisoning in humans, as well as extensive deterioration of near-shore ecosystems. Modeling in the Netherlands predicts that by the year 2100, a 4°C increase in summer temperatures in combination with nutrient fluctuations would double growth rates of several species of HABs in the North Sea.62 As ocean acidification continues due to increased CO2 absorption, the toxicity of the HABs will likely be exacerbated.63
Some bacteria, especially the Vibrio spp., also proliferate in warm marine waters, transmitting disease through drinking water or by environmental exposure in seawater and seafood. Increased cholera outbreaks in the Baltic have been linked to heat waves and low salinity.64
Overall, there is growing evidence that climate-driven changes in air and water temperatures, rainfall, humidity, and coastal salinity can contribute to the risk for waterborne diseases in both marine and freshwater ecosystems. In fact, a recent meta-analysis of 87 water-borne outbreaks occurring globally from 1910 to 2010 showed an association with heavy rainfall and flooding, with Vibrio and Leptospira spp. being the most often cited etiologic agents.65
Foodborne diseases.
An increased frequency of warm days and greater humidity can heighten the incidence of foodborne infectious diseases. Data from Great Britain show a strong association between instances of food poisoning and warmer temperatures during the preceding 2 to 5 weeks.66 Additionally, warm temperatures contributed to an estimated 30% of cases of salmonellosis in much of continental Europe, especially when they exceed a threshold of 6°C above average.67 Other foodborne agents, such as campylobacter, are also seasonal but are not as strongly linked to temperature fluctuations. Food spoilage is temperature-dependent, as pest species, especially flies, rodents, and cockroaches, have increased contact with food at higher temperatures.68
Vector-borne diseases.
Vector-borne diseases, as a class, are one of the most-studied health effects of climate change due to their widespread occurrence and sensitivity to climatic factors. These are infectious diseases, caused by protozoa, bacteria, and viruses that are spread by arthropod vectors such as mosquitoes and ticks. Prevailing scientific evidence suggests that there are 3 primary mechanisms through which climate change can affect vector-borne and zoonotic diseases:
-
1.
Geographic range shifts of vectors or reservoirs.
-
2.
Changes in rates of development, survival, and reproduction of vectors, reservoirs, and the pathogens that they carry.
-
3.
Changes in biting rates of infected vectors or the prevalence of infection in reservoir or vector populations, which affects the likelihood of transmission resulting from contact with humans.69,70
Mosquito-borne diseases.
Malaria and arboviruses are transmitted to humans by mosquitoes. Because insects are cold-blooded, climate change can shift the distribution of mosquito populations, affect mosquito biting rates and survival, and shorten or lengthen pathogen development time inside the mosquito, which ultimately determines infectivity.
Malaria is a temperature-sensitive disease and with its incidence of malaria in highly endemic areas varying seasonally and in various regions, malaria has been shown to alter in response to weather perturbations. For example, malaria transmission has been associated with temperature anomalies in some African highland areas, and more recently warmer ambient temperatures have been found to increase malaria incidence in densely populated highlands in Ethiopia and Colombia.71,72
Arboviruses include the causative agents of dengue fever, West Nile virus, chikungunya, and Rift Valley fever—each of which may be affected by climate. Rift Valley fever is usually transmitted through contact with the blood or organs of infected animals; however, Aedes mosquitoes also can transmit this disease. All known Rift Valley fever virus outbreaks in East Africa from at least 1950 to 1998, followed periods of abnormally high rainfall.73 Modeling shows that Chikungunya virus may spread into northern and central Europe due to warmer, wetter weather.74
Tick-borne disease.
Lyme disease is a prevalent tick-borne infectious disease caused by the spirochaete bacteria Borrelia burgdorferi in North America and Europe, and recent studies have reported an association between climate and tick-borne diseases, including temperature75,76 and precipitation.77 Temperature and vapor pressure contribute to maintaining populations of the tick, Ixodes scapularis, which is the microorganism’s secondary host in the United States. Because tick survival requires a monthly average minimum temperature above −7°C, temperature limits the northern boundary of Lyme disease.78 Climate models project a northward expansion of this tick into Canada due to warming temperatures.76
HEALTH EFFECTS MEDIATED THROUGH HUMAN INSTITUTIONS
Nutrition
As the global climate changes, indirect effects will manifest in reduced soil quality, incidence of plant diseases, and weed and insect populations, which will effect human health. Greater heat and humidity also will increase food spoilage (discussed in the section on infectious diseases).
For some foods, nutritional quality will diminish with climate change. With exposure to higher levels of CO2, some crops reduce their incorporation of nitrogen, resulting in lower protein levels. Studies of barley, wheat, rice, potatoes, and soybeans show reduced protein content when crops are grown under high CO2 conditions, an effect that varies with soil conditions, air quality, and other factors.79 For populations that depend on crops for their protein, this effect could further threaten nutritional status. Finally, global economic systems will play a large role in determining population vulnerability. Change-related price shocks, could more than double by mid-century, placing populations in developing countries at further risk.80
Sea-Level Rise, Violence, and Conflict
Rising sea levels may affect human health and well-being indirectly, in addition to directly through inundation or heightened storm surges. Rising seas, in concert with withdrawal of fresh water from coastal aquifers, could result in salt water intruding into those aquifers and disrupting drinking water systems, storm water drainage, and sewage disposal. These phenomena, with or without flooding, could force coastal communities to migrate; as a consequence, refugees suffer substantial health burdens, overcrowding, lack of shelter, and competition for resources. Conflict may be one of the worst results emerging from such forced population migrations.81 There is increasing but inconclusive evidence of a link between climate change and violence ranging from self-inflicted and interpersonal harm to armed conflict.82 After examining 50 quantitative studies finding associations between climatologic changes and various conflict outcomes, one meta-analysis found that for each SD of increased rainfall or warmer temperatures, the likelihood of intergroup conflict increased 14% on average.83 Thus, as climatic changes are expected to affect variability of rainfall and increase annual mean temperatures globally, assuming future populations behave similarly to historical populations, available evidence suggests an increase in risk for violent conflict.
Mental Health
Mental health disorders such as post-traumatic stress disorder (PTSD) may substantially affect population well-being after natural disasters and/or displacement due to climate change, depending on the unexpectedness of the impact, the intensity of the experience, the degree of personal and community disruption, and long-term exposure to the visual signs of the disaster.84 Symptoms of PTSD have been found in as many as 75% of refugee children and adolescents.85 Human health effects of disasters in the United States are generally projected to be less severe than in poorer countries where the public health infrastructure is less developed.
RESPONSE TO CLIMATE CHANGE
Mitigation and Adaptation
Two kinds of strategies are available for responding to climate change. The first, known as mitigation, corresponds to primary prevention, and the second, known as adaptation, corresponds to secondary prevention (or preparedness).
Mitigation refers to efforts to stabilize or reduce the production of greenhouse gases. This goal can be achieved through policies and technologies that take advantage of cleaner energy production (such as solar and wind power, and bioenergy) and reduced energy demand. Similarly, transportation policies that promote walking, bicycling, mass transit, and fuel-efficient automobiles result in fewer greenhouse gas emissions (GHGs) compared with the current US reliance on large, fuel-inefficient automobiles. Gains in energy efficiency also play a role in reducing GHGs. A final aspect of mitigation aims to accelerate the removal of greenhouse gases from the Earth’s atmosphere. Carbon dioxide sinks such as forests are effective in this regard, so land-use policies that preserve and expand forests are an important tool in mitigating global climate change.
Adaptation refers to efforts to reduce the public health effects of climate change. For example, if we anticipate severe weather events such as hurricanes, then preparation by emergency management authorities and medical facilities can minimize morbidity and mortality. This presupposes rigorous efforts at vulnerability assessment, to identify likely events, at-risk populations, and opportunities to reduce harm.86,87 Public health surveillance systems can detect outbreaks of infectious diseases in vulnerable areas, a prerequisite to early control. Many current public health challenges, such as deaths from heat waves, floods, and air pollution, will be amplified by climate change. Much of preparedness thus can build on analyses of the strengths and weaknesses of current prevention efforts and a rethinking of potential thresholds that may change in the future (e.g., expected change in the volume of storm water runoff, or the frequency of heat waves).
Health Cobenefits of Climate Change Mitigation
An important theme in both climate change mitigation and adaptation is cobenefits, or the multiple benefits that a single activity or policy can generate across different sectors or fields of study. Although the steps needed to address climate change may appear formidable, some of them, such as reducing GHGs, developing and deploying sustainable energy technologies, shifting transportation patterns, designing resiliency into cities, yield multiple benefits making them especially attractive, cost-effective, and politically feasible.88
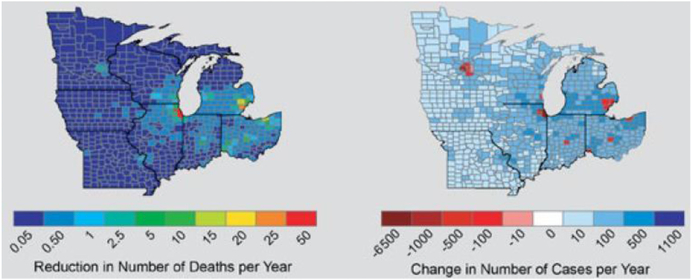
One example is reducing fossil fuel use in power plants—a principal means of reducing GHGs yet, also a strategy to reduce air pollution.89 Another example is promoting active means of transportation through sustainable community design. In communities designed to facilitate active transportation (walking and bicycling) and transit use, vehicular travel is reduced thereby reducing transportation contributions to climate change and yields other benefits as well: increased physical activity, less air pollution, and reduced health care costs from improvement in human health.90–92 One study found that the replacement of all short auto trips with active transport and public transportation during the warmer half of the year would yield major economic and health benefits for the 11 largest cities in the upper Midwest by reducing 1300 premature deaths per year (Fig. 5).90
Figure 5.
Reducing emissions, improving health. Annual reduction in the number of premature deaths (left) and annual change in the number of cases with acute respiratory symptoms (right) due to reductions in particulate matter and ozone caused by reducing automobile exhaust. The maps project health benefits if automobile trips shorter than 5 miles (round trip) were eliminated for the 11 largest metropolitan areas in the Midwest. Making 50% of these trips by bicycle just during 4 summer months would save 1295 lives and yield savings of more than $8 billion per year from improved air quality, avoided mortality, and reduced health care costs for the upper Midwest alone.90
Thus, action on climate change provides an opportunity not only to protect the environment, but also to improve and protect human health. One group of researchers found that emission reduction measures to reduce global mean warming by about 0.5°C could simultaneously prevent up to 4.7 million premature deaths annually, and improve crop yields from reduced ozone damage. These benefits have substantially greater economic value than marginal abatement costs.93 Economic analysis has shown that climate change mitigation could largely be compensated by health gains from reduced air pollution alone, and the benefits could be even wider.94
Unintended Consequences
Steps taken to address climate change can have unintended consequences. A leading example is biofuel production, a rapidly growing industry resulting from economic incentives and public policies. Today, biofuels provide around 2% of the total transport fuel; yet, by 2050 biofuels could provide 27% of all global transport fuel, contributing to the replacement of diesel, kerosene, and jet fuel production.95 This demand for biofuels may accelerate the conversion of forests to cropland, which could paradoxically increase CO2 levels.96
A full life-cycle analysis for biofuels revealed slightly higher PM generation from use of corn-based ethanol compared with use of gasoline and cellulosic ethanol. Moreover, growing corn for ethanol involves more fertilizer and farm machinery and may simply shift air pollution to rural from urban locations.97
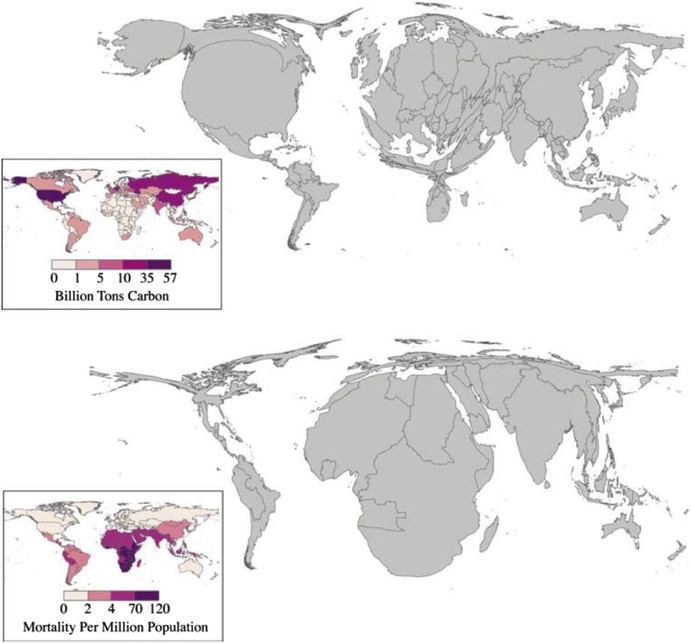
Ethical Considerations
Climate change raises numerous ethical concerns. On a global scale, the nations that are responsible for the bulk of GHGs to date (and are more resilient to the effects of climate change) account for a small proportion of the world’s population. In contrast, the large population of the global south—the poor countries—account for a relatively small share of cumulative GHGs, and a very low per capita emission rate (although total emissions from developing nations are growing rapidly, with China surpassing the United States in 2006). The United States, with 5% of the global population, produces 25% of total annual GHGs. This discrepancy exemplifies the ethical implications posed by climate change on a global scale, shown graphically in Figure 6.98
Figure 6.
Cartograms: CO2 emissions and health. Cartogram comparison of undepleted cumulative carbon dioxide (CO2) emissions (by country) for 1950 to 2000 (upper map) versus the regional distribution of 4 climate-sensitive health effects (malaria, malnutrition, diarrhea, and inland flood-related fatalities) (lower map). This is only a partial list of potential health outcomes, and there are significant uncertainties in all the underlying models. These estimates should therefore be considered a conservative, approximate estimate of the health burden of climate change. Note: CO2 emissions data from Marland, Boden, and Andres,103 adjusted for changing boundaries between 1950 and 2000, Health impacts from McMichael et al.98,104
On a more local scale, climate change poses an environmental justice concern as minorities are exposed to different types of stresses and risks. Ethical concerns arise among certain disadvantaged populations, including those social groups that are politically and socially marginalized, the poor, and certain races and ethnicities, such as poor blacks, who may be at a higher risk for experiencing the negative effects of climate change. For example, black Americans are reportedly more susceptible to extreme heat-related mortality than other racial groups in the United States because they often live in densely urbanized areas that tend to experience higher temperatures than surrounding areas (also known as the urban heat island effect). With higher temperatures come greater risk to the poor, as they are less likely to have access to air conditioning, insulation, or other means to make housing improvements that assist in adaptation to extreme heat conditions.25,99
More broadly, ethical issue arises with respect to intergenerational justice. Climate change has enormous potential effects on the health and well-being of future generations;100 ethical and religious thinkers have argued that we, in the present, have a moral obligation to future generations to slow and ultimately reverse climate change. Economists have disputed the value we should place on the future costs of climate change. The key question lays in assigning the proper “discount rate” in the future.101
CONCLUSION
Climate change health risks are occurring today and pose serious and widespread challenges for global health. Mitigation strategies to reduce emissions from fossil fuel combustion are essential to reduce these effects but can simultaneously offer substantial human health and environmental benefits. Given atmospheric residence time of greenhouse gases, adaptation is also necessary. Therefore, the best global health approach to climate change must incorporate both mitigation and adaptation strategies, as well as draw from sectors ranging from energy, transportation, agriculture, and more.
Footnotes
The authors have no conflicts of interest and all authors had access to the data and a role in writing the manuscript.
References
- 1.Masson-Delmotte V, Schulz M, Abe-Ouchi A, et al. Information for Paleoclimate Archives In: Stocker TF, Qin D, Plattner GK, et al. , eds. Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK and New York, NY: Cambridge University Press; 2013. [Google Scholar]
- 2.Collins M, Knutti R, Arblaster J, et al. Long-term climate change: projections, commitments and irreversibility In: Stocker T, QIn D, Plattner GK, et al. , eds. Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK and New York, NY: Cambridge University Press; 2013. [Google Scholar]
- 3.Rhein M, Rintoul S, Aoki S, et al. Observations: ocean In: Stocker T, QIn D, Plattner GK, et al. , eds. Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK and New York, NY: Cambridge University Press; 2013. [Google Scholar]
- 4.IPCC. 2013: Summary for policymakers In: Stocker T, QIn D, Plattner GK, et al. , eds. Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK and New York, NY: Cambridge University Press; 2013. [Google Scholar]
- 5.Samson J, Berteaux D, McGill B, Humphries M. Geographic disparities and moral hazards in the predicted impacts of climate change on human populations. Glob Ecol Biogeogr 2011;20:532–44. [Google Scholar]
- 6.Hess JJ, Malilay JN, Parkinson AJ. Climate change: the importance of place. Am J Prev Med 2008;35:468–78. [DOI] [PubMed] [Google Scholar]
- 7.Kovats RS, Hajat S. Heat stress and public health: a critical review. Annu Rev Public Health 2008;29:41–55. [DOI] [PubMed] [Google Scholar]
- 8.Curriero FC, Patz JA, Rose JB, Lele S. The association between extreme precipitation and waterborne disease outbreaks in the United States, 1948–1994. Am J Public Health 2001;91:1194–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karl TR. Global Climate Change Impacts in the United States: A State of Knowledge Report from the U.S Global Change Research Program. Cambridge, UK: Cambridge University Press; 2009. [Google Scholar]
- 10.Walsh J, Wuebbles D, Hayhoe K, et al. Our changing climate In: Melillo JM, Richmond TC, Yohe GW, eds. Climate Change Impacts in the United States: The Third National Climate Assessment. U.S. Global Change Research Program; 2014:19–67. [Google Scholar]
- 11.Centers for Disease Control and Prevention. Heat-related deaths after an extreme heat event—four states, 2012, and United States, 1999–2009. Available at: http://www.cdc.gov/mmwr/pdf/wk/mm6222.pdf. Accessed January 21, 2014.
- 12.Donoghue ER, Graham MA, Jentzen JM, et al. Criteria for the diagnosis of heat-related deaths: National Association of Medical Examiners: position paper. Am J Forensic Med Pathol 1997;18:11–4. [DOI] [PubMed] [Google Scholar]
- 13.Whitman S, Good G, Donoghue ER, Benbow N, Shou W, Mou S. Mortality in Chicago attributed to the July 1995 heat wave. Am J Public Health 1997;87:1515–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robine JM, Cheung SLK, Le Roy S, et al. Death toll exceeded 70,000 in Europe during the summer of 2003. C R Biol 2008;331:171–8. [DOI] [PubMed] [Google Scholar]
- 15.Barriopedro D, Fischer EM, Luterbacher J, Trigo RM, Garcia-Herrera R. The hot summer of 2010: redrawing the temperature record map of Europe. Science 2011;332:220–4. [DOI] [PubMed] [Google Scholar]
- 16.Medina-Ramón M, Schwartz J. Temperature, temperature extremes, and mortality: a study of acclimatisation and effect modification in 50 US cities. Occup Environ Med 2007;64:827–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li T, Horton RM, Kinney PL. Projections of seasonal patterns in temperature-related deaths for Manhattan, New York. Nat Clim Chang 2013;3:717–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McMichael AJ, Woodruff RE, Hales S. Climate change and human health: present and future risks. Lancet 2006;367:859–69. [DOI] [PubMed] [Google Scholar]
- 19.World Meteorological Organization, Etienne C, Williams M, et al. Atlas of mortality and economic losses from weather, climate, and water extremes (1970–2012). Available at: http://www.wmo.int/pages/prog/drr/transfer/2014.06.12-WMO1123_Atlas_120614.pdf. Accessed September 4, 2014.
- 20.Toole M, Waldman R. The public health aspects of complex emergencies and refugee situations. Annu Rev Public Health 1997;18:283. [DOI] [PubMed] [Google Scholar]
- 21.Kirtman B, Power SB, Adedoyin JA, et al. Near-term climate change: projections and predictability In: Stocker TF, Qin D, Plattner GK, et al. , eds. Climate Change: 2013: The Physical Science Basis, Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK and New York, NY: Cambridge University Press; 2013. [Google Scholar]
- 22.Christensen JH, Krishna Kumar K, Aldrian E, et al. Climate phenomena and their relevance for future regional climate change In: Stocker TF, Qin D, Plattner GK, et al. , eds. Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK and New York, NY: Cambridge University Press; 2013. [Google Scholar]
- 23.Guha-Sapir D, Vos F, Below R, Ponserre S. Annual Disaster Statistical Review 2010, Center for Research on the Epidemiology of Disasters. Brussels: Belgium; 2011. [Google Scholar]
- 24.Doocy S, Daniels A, Packer C, Dick A, Kirsch TD. The human impact of earthquakes: a historical review of events 1980–2009 and systematic literature review. PLoS Curr 2013;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith KR, Woodward A, Campbell-Lendrum D, et al. Human Health: Impacts, Adaptation, and Co-Benefits Cambridge, United KingdomUK and New York, NY: Cambridge University Press; 2014:1–69. [Google Scholar]
- 26.Lott N, McCown S, Graumann A, Ross T. Mitch: the deadliest Atlantic hurricane since 1780. Available at: http://www.ncdc.noaa.gov/oa/reports/mitch/mitch.html.
- 27.Westerling AL, Hidalgo HG, Cayan DR, Swetnam TW. Warming and earlier spring increase western US forest wildfire activity. Science 2006;313:940–3. [DOI] [PubMed] [Google Scholar]
- 28.Finlay SE, Moffat A, Gazzard R, Baker D, Murray V. Health impacts of wildfires. PLoS Curr 2012;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gray WM. Hurricanes: their formation, structure and likely role in the tropical circulation. Meteorol Trop Oceans 1979;77:155–218. [Google Scholar]
- 30.Goldenberg SB, Landsea CW, Mestas-Nuñez AM, Gray WM. The recent increase in Atlantic hurricane activity: causes and implications. Science 2001;293:474–9. [DOI] [PubMed] [Google Scholar]
- 31.Emanuel K, Sundararajan R, Williams J. Hurricanes and global warming: Results from downscaling IPCC AR4 simulations. Bull Am Meteorol Soc 2008;89:347–67. [Google Scholar]
- 32.Webster PJ, Holland GJ, Curry JA, Chang HR. Changes in tropical cyclone number, duration, and intensity in a warming environment. Science 2005;309:1844–6. [DOI] [PubMed] [Google Scholar]
- 33.Nicholls RJ. Planning for the impacts of sea level rise. Oceanogr-Oceanogr Soc 2011;24:144. [Google Scholar]
- 34.Nicholls RJ, Hoozemans FM, Marchand M. Increasing flood risk and wetland losses due to global sea-level rise: regional and global analyses. Glob Environ Change 1999;9:S69–87. [Google Scholar]
- 35.Brown ME, Funk CC. Food security under climate change. Science 2008;319:580–1. [DOI] [PubMed] [Google Scholar]
- 36.Reilly J, Baethgen W, Chege F, et al. Agriculture in a changing climate: impacts and adaptation In: Watson RT, Zinyowera MC, Moss RH, eds. Climate Change 1995—Impacts, Adaptations and Mitigation of Climate Change: Scientific-Technical Analyses. Cambridge, UK: IPCC, Cambridge University Press; 1996:429–67. [Google Scholar]
- 37.Frumkin H Environmental Health: From Global to Local. 2nd ed San Francisco, CA: Wiley; 2010. [Google Scholar]
- 38.World Health Organization; The World Health Report: 2002: Reducing the Risks, Promoting Healthy Life. Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 39.Nelson GC, Rosegrant MW, Koo J, et al. Climate Change: Impact on Agriculture and Costs of Adaptation. Washington DC: International Food Policy Research Institute; 2009. [Google Scholar]
- 40.Parry ML. Climate Change 2007: Impacts, Adaptation and Vulnerability. Cambridge, UK: IPCC, Cambridge University Press; 2007. [Google Scholar]
- 41.Patz JA. Public health risk assessment linked to climatic and ecological change. Hum Ecol Risk Assess Int J 2001;7:1317–27. [Google Scholar]
- 42.OECD; OECD Environmental Outlook to 2050. Paris: Organisation for Economic Co-operation and Development; 2012. Available at: http://www.oecd-ilibrary.org/content/book/9789264122246-en. [Google Scholar]
- 43.Reilly JM. Agriculture: The Potential Consequences of Climate Variability and Change for the United States. Cambridge, UK: Cambridge University Press; 2002. [Google Scholar]
- 44.Battisti DS, Naylor RL. Historical warnings of future food insecurity with unprecedented seasonal heat. Science 2009;323:240–4. [DOI] [PubMed] [Google Scholar]
- 45.Cline WR. Global Warming and Agriculture: Impact Estimates by Country. Washington DC: Peter G. Peterson Institute for International Economics; 2007. [Google Scholar]
- 46.Pauly D, Alder J, Bakun A, et al. Marine fisheries systems. Ecosyst Hum Well-Curr State Trends 2005;1:477–511. [Google Scholar]
- 47.Intergovernmental Panel on Climate Change, Working Group II. Climate change 2014: impacts, adaptation, and vulnerability. 2014. Available at: http://ipcc-wg2.gov/AR5/images/uploads/WGIIAR5-Chap11_FGDall.pdf. Accessed April 2, 2014.
- 48.Lim S, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ebi KL, McGregor G. Climate change, tropospheric ozone and particulate matter, and health impacts. Environ Health Perspect 2008;116:1449–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fuentes JD, Lerdau M, Atkinson R, et al. Biogenic hydrocarbons in the atmospheric boundary layer: a review. Bull Am Meteorol Soc 2000;81:1537–76. [Google Scholar]
- 51.Bernard SM, Samet JM, Grambsch A, Ebi KL, Romieu I. The potential impacts of climate variability and change on air pollution-related health effects in the United States. Environ Health Perspect 2001;109(Suppl 2):199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bell ML, McDermott A, Zeger SL, Samet JM, Dominici F. Ozone and short-term mortality in 95 US urban communities, 1987–2000. JAMA 2004;292:2372–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jacobson MZ. On the causal link between carbon dioxide and air pollution mortality. Geophys Res Lett 2008;35(3). Available at: http://onlinelibrary.wiley.com/store/10.1029/2007GL031101/asset/grl23620.pdf?v=1&t=i0s9aiuc&s=83cb2ad1f5f10572e0397a4e8b54e11896af2b75. Accessed October 2, 2014. [Google Scholar]
- 54.Brook RD, Rajagopalan S, Pope CA, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 2010;121:2331–78. [DOI] [PubMed] [Google Scholar]
- 55.Jacob DJ, Winner DA. Effect of climate change on air quality. Atmos Environ 2009;43:51–63. [Google Scholar]
- 56.Ziska LH, Caulfield F. The potential influence of rising atmospheric carbon dioxide (CO2) on public health: pollen production of common ragweed as a test case. World Resour Rev 2000;12:449–57. [Google Scholar]
- 57.Wayne P, Foster S, Connolly J, Bazzaz F, Epstein P. Production of allergenic pollen by ragweed (Ambrosia artemisiifolia L.) is increased in CO2-enriched atmospheres. Ann Allergy Asthma Immunol 2002;88:279–82. [DOI] [PubMed] [Google Scholar]
- 58.Ziska L, Knowlton K, Rogers C, et al. Recent warming by latitude associated with increased length of ragweed pollen season in central North America. Proc Natl Acad Sci 2011;108:4248–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mac Kenzie WR, Hoxie NJ, Proctor ME, et al. A massive outbreak in Milwaukee of Cryptosporidium infection transmitted through the public water supply. N Engl J Med 1994;331:161–7. [DOI] [PubMed] [Google Scholar]
- 60.Hrudey S, Payment P, Huck P, Gillham R, Hrudey E. A fatal water-borne disease epidemic in Walkerton, Ontario: comparison with other waterborne outbreaks in the developed world. Water Sci Technol 2003;47:7–14. [PubMed] [Google Scholar]
- 61.Patz JA, Vavrus SJ, Uejio CK, McLellan SL. Climate change and waterborne disease risk in the Great Lakes region of the US. Am J Prev Med 2008;35:451–8. [DOI] [PubMed] [Google Scholar]
- 62.Peperzak L Future increase in harmful algal blooms in the North Sea due to climate change. Water Sci Technol 2005;51:31–6. [PubMed] [Google Scholar]
- 63.Fu FX, Tatters AO, Hutchins DA. Global change and the future of harmful algal blooms in the ocean. Mar Ecol Prog Ser 2012;470:207–33. [Google Scholar]
- 64.Baker-Austin C, Trinanes JA, Taylor NG, Hartnell R, Siitonen A, Martinez-Urtaza J. Emerging Vibrio risk at high latitudes in response to ocean warming. Nat Clim Change 2013;3:73–7. [Google Scholar]
- 65.Cann K, Thomas DR, Salmon R, Wyn-Jones A, Kay D. Extreme water-related weather events and waterborne disease. Epidemiol Infect 2013;141:671–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bentham G, Langford IH. Climate change and the incidence of food poisoning in England and Wales. Int J Biometeorol 1995;39:81–6. [DOI] [PubMed] [Google Scholar]
- 67.Kovats R, Edwards S, Hajat S, Armstrong B, Ebi K, Menne B. The effect of temperature on food poisoning: a time-series analysis of salmonellosis in ten European countries. Epidemiol Infect 2004;132:443–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Goulson D, Derwent LC, Hanley ME, Dunn DW, Abolins SR. Predicting calyptrate fly populations from the weather, and probable consequences of climate change. J Appl Ecol 2005;42:795–804. [Google Scholar]
- 69.Kovats R, Campbell-Lendrum D, McMichel A, Woodward A, Cox JSH. Early effects of climate change: do they include changes in vector-borne disease? Philos Trans R Soc Lond B Biol Sci 2001;356:1057–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mills JN, Gage KL, Khan AS. Potential influence of climate change on vector-borne and zoonotic diseases: a review and proposed research plan. Environ Health Perspect 2010;118:1507–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Siraj A, Santos-Vega M, Bouma M, Yadeta D, Carrascal DR, Pascual M. Altitudinal changes in malaria incidence in highlands of Ethiopia and Colombia. Science 2014;343:1154–8. [DOI] [PubMed] [Google Scholar]
- 72.Githeko AK, Ndegwa W. Predicting malaria epidemics in the Kenyan highlands using climate data: a tool for decision makers. Glob Change Hum Health 2001;2:54–63. [Google Scholar]
- 73.Linthicum KJ, Anyamba A, Tucker CJ, Kelley PW, Myers MF, Peters CJ. Climate and satellite indicators to forecast Rift Valley fever epidemics in Kenya. Science 1999;285:397–400. [DOI] [PubMed] [Google Scholar]
- 74.Fischer D, Thomas SM, Suk JE, et al. Climate change effects on Chikungunya transmission in Europe: geospatial analysis of vector’s climatic suitability and virus’ temperature requirements. Int J Health Geogr 2013;12:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gray JS. Ixodes ricinus seasonal activity: Implications of global warming indicated by revisiting tick and weather data. Int J Med Microbiol 2008;298:19–24. [Google Scholar]
- 76.Ogden NH, Radojević M, Wu X, Duvvuri VR, Leighton PA, Wu J. Estimated effects of projected climate change on the basic reproductive number of the Lyme disease vector Ixodes scapularis. Env Health Perspect 2014;122:631–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.McCabe GJ, Bunnell JE. Precipitation and the occurrence of Lyme disease in the northeastern United States. Vector-Borne Zoonotic Dis 2004;4:143–8. [DOI] [PubMed] [Google Scholar]
- 78.Brownstein JS, Holford TR, Fish D. A climate-based model predicts the spatial distribution of the Lyme disease vector Ixodes scapularis in the United States. Environ Health Perspect 2003;111:1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Taub DR, Miller B, Allen H. Effects of elevated CO2 on the protein concentration of food crops: a meta-analysis. Glob Change Biol 2008;14:565–75. [Google Scholar]
- 80.Bailey R Growing a better future: food justice in a resource-constrained world. Oxfam Policy Pract Agric Food Land 2011;11:93–168. [Google Scholar]
- 81.Adger WN, Barnett J, Dabelko G, et al. Human Security. Cambridge, UK and New York, NY: Cambridge University Press; 2014. [Google Scholar]
- 82.Levy BS, Sidel VW. Collective violence caused by climate change and how it threatens health and human rights. Health Hum Rights Int J 2014;16:32–40. [PubMed] [Google Scholar]
- 83.Hsiang SM, Burke M. Climate, conflict, and social stability: what does the evidence say? Clim Change 2014;123:39–55. [Google Scholar]
- 84.Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiol Rev 2005;27:78–91. [DOI] [PubMed] [Google Scholar]
- 85.McCloskey LA, Southwick K. Psychosocial problems in refugee children exposed to war. Pediatrics 1996;97:394–7. [PubMed] [Google Scholar]
- 86.Menne B, Ebi KL. Climate Change and Adaptation Strategies for Human Health. New York, NY: Springer; 2006. [Google Scholar]
- 87.Schipper ELF, Burton I. The Earthscan Reader on Adaptation to Climate Change London, UK: Earthscan London; 2009. [Google Scholar]
- 88.Corfee-Morlot J, Agrawala S. The benefits of climate policy. Glob Environ Change 2004;14:197–9. [Google Scholar]
- 89.Cifuentes L, Borja-Aburto VH, Gouveia N, Thurston G, Davis DL. Assessing the health benefits of urban air pollution reductions associated with climate change mitigation (2000–2020): Santiago, Sao Paulo, Mexico City, and New York City. Environ Health Perspect 2001;109(Suppl 3):419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Grabow ML, Spak SN, Holloway T, Stone B Jr, Mednick AC, Patz JA. Air quality and exercise-related health benefits from reduced car travel in the midwestern United States. Environ Health Perspect 2012;120:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Maizlish N, Woodcock J, Co S, Ostro B, Fanai A, Fairley D. Health cobenefits and transportation-related reductions in greenhouse gas emissions in the San Francisco Bay area. Am J Public Health 2013;103:703–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Woodcock J, Givoni M, Morgan AS. Health impact modelling of active travel visions for England and Wales using an Integrated Transport and Health Impact Modelling tool (ITHIM). PLoS One 2013;8:e51462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Shindell D, Kuylenstierna JC, Vignati E, et al. Simultaneously mitigating near-term climate change and improving human health and food security. Science 2012;335:183–9. [DOI] [PubMed] [Google Scholar]
- 94.West JJ, Smith SJ, Silva RA, et al. Co-benefits of mitigating global greenhouse gas emissions for future air quality and human health. Nat Clim Change 2013;3:885–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.International Energy Agency; Technology roadmap: biofuels for transport. Paris, France: International Energy Agency; 2011. Available at: http://www.iea.org/publications/freepublications/publication/name-3976-en.html. Accessed October 2, 2014. [Google Scholar]
- 96.Gibbs HK, Johnston M, Foley JA, et al. Carbon payback times for crop-based biofuel expansion in the tropics: the effects of changing yield and technology. Environ Res Lett 2008;3:034001. [Google Scholar]
- 97.Hill J, Polasky S, Nelson E, et al. Climate change and health costs of air emissions from biofuels and gasoline. Proc Natl Acad Sci 2009;106:2077–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Patz JA, Gibbs HK, Foley JA, Rogers JV, Smith KR. Climate change and global health: quantifying a growing ethical crisis. EcoHealth 2007;4:397–405. [Google Scholar]
- 99.Wilson SM, Richard R, Joseph L, Williams E. Climate change, environmental justice, and vulnerability: an exploratory spatial analysis. Environ Justice 2010;3:13–9. [Google Scholar]
- 100.Page EA. Climate Change, Justice and Future Generations. Cheltenham, UK: Edward Elgar Publishing; 2007. [Google Scholar]
- 101.Stern NH. Britain G, ed. Review Stern: The Economics of Climate Change. London, UK: HM Treasury; 2006. [Google Scholar]
- 102.Luber G, Knowlton K, Balbus J, et al. Human health In: Melillo J, Richmond T, Yohe G, eds. Climate Change Impacts in the United States: The Third National Climate Assessment. Washington DC: U.S. Global Change Research Program; 2014:220–56. [Google Scholar]
- 103.Marland G, Boden TA, Andres RJ, Brenkert AL, Johnston CA. Global, regional, and national fossil fuel CO2 emissions In: Trends: A Compendium of Data on Global Change. Oak Ridge, TN: Oak Ridge National Laboratory, U.S. Department of Energy; 2007. Available at: http://cdiac.ornl.gov/trends/emis/overview. [Google Scholar]
- 104.McMichael AJ, Campbell-Lendrum D, Kovats S, et al. Global climate change In: Ezzati M, Lopez AD, Rodgers A, Murray CJL, eds. Comparative Quantification of Health Risks: Global and Regional Burden of Disease Due to Selected Major Risk Factors, Vol 2 Geneva: World Health Organization; 2004:1543–1649. [Google Scholar]