Cirrhosis is a morbid, multisystem disease associated with frequent hospitalizations and high mortality rates. The number of affected people is rising in the United States, reflected in a 59% increase in patients with cirrhosis seeking medical care in the past decade(1). Anticipating and preventing many of the complications of cirrhosis can be challenging. To aid gastroenterologists caring for this booming population, we propose the following “Dos and Don’ts” for management of cirrhosis in the inpatient and outpatient settings.
“Dos and Don’ts” in the Hospital (Table 1)
Table 1:
“Dos and Don’ts” In the Hospital.
| Do | Don’t | |
|---|---|---|
| Patient presents with ascites | Perform a diagnostic paracentesis on admission | Delay the procedure for coagulopathy or transfuse blood products prior to procedure |
| Spontaneous Bacterial Peritonitis | Start antibiotics quickly and give albumin on day 1 and day 3 | Forget to prescribe long term antibiotics for secondary prophylaxis |
| Suspected Variceal Bleeding | Perform endoscopy and start medical therapy (vasoactive agents and antibiotics) quickly | Forget secondary prophylaxis (NSBB and follow up EGD(s)) |
EGD = Esophagogastrodudodenoscopy, NSBB = Non-selective beta blocker
1. All patients with ascites admitted to the hospital should have a diagnostic paracentesis, regardless of coagulopathy.
Spontaneous bacterial peritonitis (SBP) is often asymptomatic and early treatment is associated with improved outcomes. Accordingly, patients with ascites who undergo a diagnostic paracentesis on admission have reduced in-hospital mortality. There is no evidence that patients with elevated International Normalized Ratios or thrombocytopenia benefit from periprocedural prophylactic blood product transfusions(2).
2. Treat SBP aggressively in the hospital and start secondary prophylaxis on discharge.
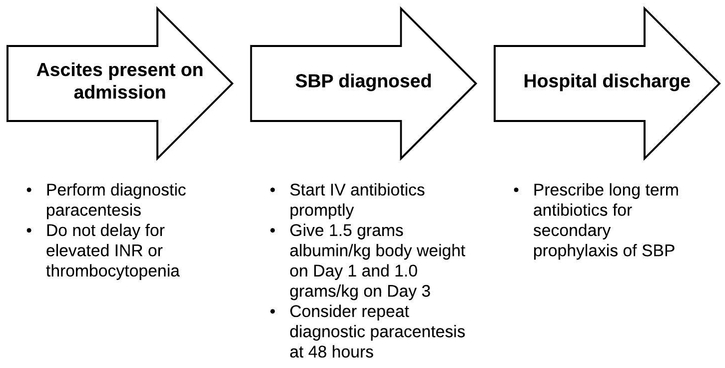
Following a diagnosis of SBP, patients should promptly receive antibiotics (Figure 1). SBP is associated with the development of hepatorenal syndrome, thus 25% albumin solution should be infused to maintain intravascular volume to protect the kidneys(3). Diuretics should be held until the infection has resolved. Empiric antibiotic therapy fails in up to 25% of cases; a repeat diagnostic paracentesis should be considered if there is no clinical improvement after 48 hours. Long-term antibiotic prophylaxis should be initiated on discharge. Of note, data from randomized trials of patients without SBP suggest benefit from quinolone-based primary prophylaxis, specifically those with Child-Turcotte Pugh (CTP) scores ≥9 and bilirubin ≥3 or impaired renal function (creatinine ≥ 1.2 or sodium ≤ 130 mmol/L) and an ascitic fluid total protein < 1.5 g/dL(4).
Figure 1:
Key points in diagnosis and management of Spontaneous Bacterial Peritonitis (SBP). INR = International Normalized Ratio, IV = Intravenous
3. Act quickly for suspected variceal bleeding and don’t forget secondary prophylaxis to prevent recurrent bleeding.
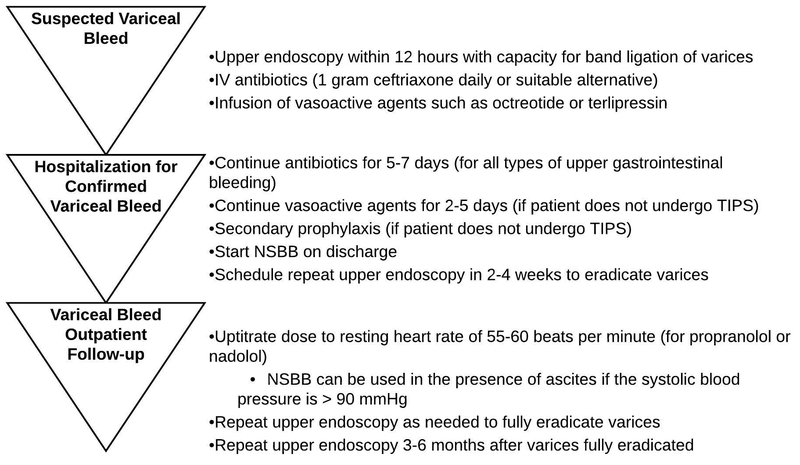
Patients with cirrhosis and upper gastrointestinal hemorrhage should undergo upper endoscopy within 12 hours of presentation (Figure 2). Prior to endoscopy, all patients should receive vasoactive agents and antibiotics. As patients with cirrhosis and gastrointestinal bleeding are at high risk for bacterial infections (not limited to SBP), antibiotics should be provided even if patients do not have ascites(5).
Figure 2:
Acute and Subacute management of Variceal Bleeding. IV = Intravenous, NSBB = Non-selective beta blocker, TIPS = Transjugular Intrahepatic Portosystemic Shunt
Patients who had a variceal bleed are at high risk for recurrent bleeding. Secondary prophylaxis includes starting nonselective beta-blockers (NSBB) on discharge and scheduling follow-up endoscopy to eradicate varices. Increasing data show that NSBB also improves all-cause mortality(6). Early Transjugular Intrahepatic Portosystemic Shunt placement should be considered in appropriate candidates (CTP B with endoscopically active bleeding despite medical therapy or CTP C with a score <14), even if they do not re-bleed after initial endoscopic therapy(4).
“Dos and Don’ts” in the Clinic (Table 2)
Table 2:
“Dos and Don’ts” in the Clinic.
| Do | Don’t | |
|---|---|---|
| Health Maintenance | Assess vaccination status and general health maintenance issues (cardiovascular disease and smoking cessation) | Leave all health maintenance up to patients’ primary care providers |
| Pain Management | Discuss the safety of limited (2 gram/day) acetaminophen use | Prescribe NSAIDs |
| Nutrition | Recognize malnutrition and refer to dieticians early | Restrict protein |
| Quality of Life | Discuss common disabling symptoms in cirrhosis | Wait for patients to bring these issues up |
| Alcohol Use | Screen for alcohol use disorders in all patients | Forget to reassess over time |
| Ascites Management | Instruct patients on self-management, salt restriction, weight recording, and red flags | Wait until ascites becomes unbearable necessitating emergency room or hospital admissions |
| Hepatocellular Carcinoma | Screen with ultrasound ± serum AFP every six months | Leave patients out of screening |
| Liver Transplant Referral | Refer early when a patient develops decompensated cirrhosis | Wait until the patient is hospitalized in life-threatening condition |
| Palliative Care | Address goals of care and refer to palliative care early | Wait until patient is in a critical state |
AFP = Alpha fetoprotein, NSAIDs = Non-steroidal anti-inflammatory drugs
1. Incorporate health maintenance into each visit, even if it is outside the scope of “typical gastroenterology” care.
Vaccination status including influenza and pneumococcal vaccines should be assessed at each visit. Vaccination against hepatitis A and B are recommended in cirrhosis, but only 1 in 3 patients with cirrhosis complete this vaccination series(7). Gastroenterology clinics should have the capacity to provide on-site vaccination.
Cardiovascular disease is prevalent in patients with cirrhosis, but owing to concerns of hepatotoxicity many providers are hesitant to prescribe statins. Statins are safe in patients with compensated cirrhosis, and current guidelines do not even recommend assessing liver enzymes after initiating statins(7). Further, there is mounting evidence that statin use is associated with decreased risk of decompensation and mortality(8). Gastroenterologists should educate patients and other medical providers that statins should be prescribed when indicated in patients with chronic liver disease.
2. Proactively discuss safe pain management in cirrhosis.
Over the counter and prescription analgesic use is common in cirrhosis. Acetaminophen is safe in cirrhosis if doses are limited to 2000 mg daily and should be used for first-line pain control. Non-steroidal anti-inflammatory drugs should be avoided in patients with ascites due to the risk of renal injury. Many patients with cirrhosis chronically use narcotics. Judicious narcotic use can be safe but may increase the risk of falls and Hepatic Encephalopathy (HE)(9). Non-pharmacologic modalities for pain including physical therapy, counseling, and yoga or meditation should be considered.
3. Refer early to dieticians and don’t restrict protein.
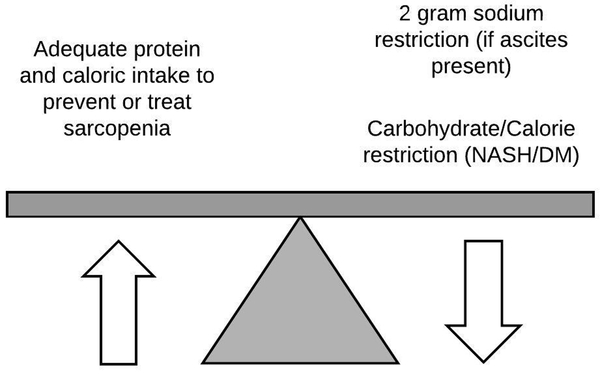
The majority of patients with decompensated cirrhosis are in catabolic states and are malnourished, contributing to a host of adverse events including HE, falls, and disability(10). Accordingly, protein intake should not be restricted. Cirrhosis patients should take in 1.2–1.5 g/kg/day of protein and 30–40 Kcal/kg/day(11). A nighttime snack should be recommended to help meet this goal. Providing specific dietary recommendations can be challenging given the need to balance sodium restriction for ascites (when present) and carbohydrate/calorie restriction for patients with non-alcoholic steatohepatitis or diabetes (Figure 3). Thus, early referral to a dietician is helpful.
Figure 3:
Dietary balance in cirrhosis. NASH = Non-alcoholic steatohepatitis, DM = Diabetes Mellitus
4. Inquire about and manage common quality of life symptoms in cirrhosis.
Cirrhosis patients can experience debilitating complications that affect quality of life (Table 3). These include muscle cramps, pruritus, sleep disturbances, and sexual dysfunction that can improve with symptomatic treatment(12). Patients may not disclose these concerns in a busy clinic visit, so they should be proactively assessed by providers.
Table 3:
Screening questions and treatment options for common disabling symptoms in cirrhosis.
| Symptom | Sample Questions | Therapeutic options |
|---|---|---|
| Muscle Cramps |
|
|
| Pruritus |
|
|
| Sleep disturbance |
|
|
| Sexual Dysfunction |
|
|
HE = Hepatic Encephalopathy
5. Screen for alcohol use in all patients with cirrhosis, and refer for treatment as needed.
Continued alcohol use can worsen liver disease even when alcohol is not the primary cause of the liver disease. Patients often underreport how much they drink(13). If there are concerns about recent use, alcohol screening tests can be used to detect alcohol consumption over the past week (e.g. urine ethyl glucuronide). Patients who screen positive for an alcohol use disorder should be referred for counselling and/or pharmacologic therapy. Alcohol use should also be reassessed during return visits, especially in the setting of worsening liver disease.
6. Educate patients on their role in managing their ascites, including easy access to outpatient paracentesis if needed.
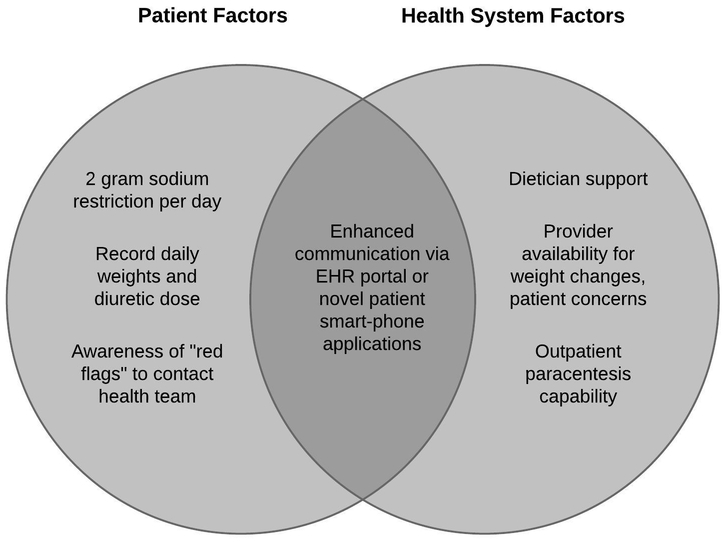
Patients with ascites need to follow a two-gram sodium diet. This is challenging, so patients and their caregivers should meet with a dietician to learn how to follow this. Providers should instruct patients to record their current diuretic dose along with daily weights, and to call the clinic for large (≥5 pound) fluctuations in weight. Ensuring availability of and easy access to outpatient therapeutic paracentesis is essential as this has been shown to significantly decrease healthcare costs and 30-day readmission rates (14) (Figure 4).
Figure 4:
Patients and health system factors associated with successful ascites management. EHR: Electronic Health Record
7. Screen patients with cirrhosis for hepatocellular carcinoma (HCC).
Patients with cirrhosis are at an increased risk for HCC, which has been rising in the United States. They should be screened for HCC with an ultrasound of the liver (± serum alpha fetoprotein testing) every six months. A recent systematic review of observational studies demonstrated that surveillance leads to earlier stage at diagnosis, higher rates of curative treatment, and improved survival(15). To promote adherence, patients should be educated regarding the benefits of surveillance and automated orders/reminders for clinic staff should be programmed in electronic health records.
8. Refer patients for liver transplant evaluation when they develop decompensated disease
A patient’s risk of death dramatically increases once they develop decompensations of their cirrhosis. Following such an event: variceal bleeding, ascites, or hepatic encephalopathy, referral for evaluation at a transplant center is indicated. While some patients may remain stable for months after the first decompensation, the clinical course is unpredictable and further decline can be precipitous; thus early referral is important.
9. Start addressing goals of care in non-urgent settings, and have a low threshold to refer patients for palliative care.
For all patients with decompensated cirrhosis, particularly when transplantation is not a part of their care, a focus on enhancing quality of life should be prioritized. Unfortunately, only 11% of patients with decompensated cirrhosis are referred for palliative care(16). Patients with decompensated cirrhosis should be given the opportunity to address goals of care and establish a healthcare proxy. Earlier involvement of palliative care can help focus care on patient wishes, avoid futile interventions, and could reduce unnecessary procedures and hospitalizations.
Acknowledgments
Financial Support: Mary Thomson receives funding from the NIH T32 Training Grant in Epidemiology and Health Services (DK062708). Elliot Tapper receives funding from the NIH through the Michigan Institute for Clinical and Health Research (KL2TR002241). No additional funding sources were used for this publication
Footnotes
Potential Competing Interests: No authors have conflicts of interest to disclose.
References
- 1.Beste LA, Leipertz SL, Green PK, et al. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US veterans, 2001–2013. Gastroenterology 2015;149:1471–1482. e5. [DOI] [PubMed] [Google Scholar]
- 2.Grabau CM, Crago SF, Hoff LK, et al. Performance standards for therapeutic abdominal paracentesis. Hepatology 2004;40:484–488. [DOI] [PubMed] [Google Scholar]
- 3.Sort P, Navasa M, Arroyo V, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med 1999;341:403–9. [DOI] [PubMed] [Google Scholar]
- 4.Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology 2013;57:1651–3. [DOI] [PubMed] [Google Scholar]
- 5.Garcia-Tsao G, Abraldes JG, Berzigotti A, et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology 2017;65:310–335. [DOI] [PubMed] [Google Scholar]
- 6.Puente A, Hernandez-Gea V, Graupera I, et al. Drugs plus ligation to prevent rebleeding in cirrhosis: an updated systematic review. Liver Int 2014;34:823–33. [DOI] [PubMed] [Google Scholar]
- 7.Tapper EB. Building Effective Quality Improvement Programs for Liver Disease: A Systematic Review of Quality Improvement Initiatives. Clin Gastroenterol Hepatol 2016;14:1256–1265 e3. [DOI] [PubMed] [Google Scholar]
- 8.Kamal S, Khan MA, Seth A, et al. Beneficial Effects of Statins on the Rates of Hepatic Fibrosis, Hepatic Decompensation, and Mortality in Chronic Liver Disease: A Systematic Review and Meta-Analysis. Am J Gastroenterol 2017;112:1495–1505. [DOI] [PubMed] [Google Scholar]
- 9.Tapper EB, Risech-Neyman Y, Sengupta N. Psychoactive Medications Increase the Risk of Falls and Fall-related Injuries in Hospitalized Patients With Cirrhosis. Clin Gastroenterol Hepatol 2015;13:1670–5. [DOI] [PubMed] [Google Scholar]
- 10.Cabre E, Gassull MA. Nutritional and metabolic issues in cirrhosis and liver transplantation. Curr Opin Clin Nutr Metab Care 2000;3:345–54. [DOI] [PubMed] [Google Scholar]
- 11.Plauth M, Cabre E, Riggio O, et al. ESPEN Guidelines on Enteral Nutrition: Liver disease. Clin Nutr 2006;25:285–94. [DOI] [PubMed] [Google Scholar]
- 12.Tapper EB, Kanwal F, Asrani SK, et al. Patient Reported Outcomes in Cirrhosis: A Scoping Review of the Literature. Hepatology 2017. [DOI] [PubMed] [Google Scholar]
- 13.Grant BF. Barriers to alcoholism treatment: reasons for not seeking treatment in a general population sample. Journal of studies on alcohol 1997;58:365–371. [DOI] [PubMed] [Google Scholar]
- 14.Hudson B, Round J, Georgeson B, et al. Cirrhosis with ascites in the last year of life: a nationwide analysis of factors shaping costs, health-care use, and place of death in England. The Lancet Gastroenterology & Hepatology 2017. [DOI] [PubMed] [Google Scholar]
- 15.Singal AG, Pillai A, Tiro J. Early detection, curative treatment, and survival rates for hepatocellular carcinoma surveillance in patients with cirrhosis: a meta-analysis. PLoS Med 2014;11:e1001624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Poonja Z, Brisebois A, van Zanten SV, et al. Patients with cirrhosis and denied liver transplants rarely receive adequate palliative care or appropriate management. Clinical Gastroenterology and Hepatology 2014;12:692–698. [DOI] [PubMed] [Google Scholar]