Abstract
Purpose of the Review:
Children with obesity experience disordered eating attitudes and behaviors at high rates, which increases their risk for adult obesity and eating disorder development. As such, it is imperative to screen for disordered eating symptoms and identify appropriate treatments.
Recent findings:
Family-based multicomponent behavioral weight loss treatment (FBT) is effective at treating childhood obesity and demonstrates positive outcomes on psychosocial outcomes, including disordered eating. FBT utilizes a socio-ecological treatment approach that focuses on the development of individual and family healthy energy balance behaviors as well as positive self- and body-esteem, supportive family relationships, richer social networks, and the creation of a broader environment and community that facilitates overall physical and mental health.
Summary:
Existing literature suggests FBT is an effective treatment option for disordered eating and obesity in children. Future work is needed to confirm this conclusion and to examine the progression and interaction of obesity and disordered eating across development to understand the time for optimal intervention.
Keywords: Childhood obesity, disordered eating, obesity treatment, psychological comorbidities, risk factors
Introduction
Childhood obesity is a serious public health concern. In the United States, 17% of children have obesity, and 5.8% meet criteria for extreme obesity (i.e., a body mass index [BMI] at or above 120% of the sex-specific 95th percentile on the CDC BMI-for-age growth charts) [1]. Rates of disordered eating attitudes and behaviors are higher in children with obesity than in children in the normal-weight range [2]. Childhood obesity and disordered eating attitudes and behaviors are each associated with numerous physical health issues that track into adulthood as well as increased psychological and social problems, including full-syndrome eating disorder (ED) development, such as binge eating disorder (BED) or bulimia nervosa (BN), internalizing symptoms, such as symptoms of depression or anxiety, and peer and family problems, including teasing and potentially harmful parent-child feeding practices [3–10]. Current research suggests that physical health issues and psychosocial problems may be exacerbated in children who experience both obesity and disordered eating attitudes and behaviors, making this group particularly vulnerable [7, 9, 8]. Treatments that address both issues in children may protect against both full-syndrome ED development and adult obesity. Family-based multicomponent behavioral weight loss treatment (FBT) is the gold standard for treating childhood obesity [11] and has demonstrated success in reducing disordered eating attitudes and behaviors [12–15]. The following paper reviews the association between obesity and disordered eating attitudes and behaviors in children, examines individual and environmental constructs associated with dysfunctional eating in children with obesity, and explores how the components of FBT may be beneficial both to obesity and disordered eating outcomes.
Association Between Overweight/Obesity and Disordered Eating Attitudes and Behaviors
The term disordered eating attitudes and behaviors comprises a number of different constructs, including negative attitudes towards weight and shape, unhealthy weight control behaviors, and binge eating [Table 1].
Table 1.
Disordered Eating and Psychological Comorbidities in Children with Obesity
| ED Related Disturbance | Definition | Rates in Children with Overweight/Obesity |
|---|---|---|
| Negative Attitudes Towards Shape and Weight | Body dissatisfaction: Negative appraisals of one’s shape and/or weight | 46.5% of girls with overweight/obesity report body dissatisfaction compared to 24.8% of normal-weight girls, while25.2% of boys with overweight/obesity report body dissatisfaction compared to 8.7% of normal-weight boys [16] |
| Shape and Weight Concerns: Worries or anxieties about shape and/or weight | ||
| Overvaluation of Shape and Weight: Self-esteem is highly contingent on shape and/or weight | ||
| Disordered Weight Control Behaviors | Inappropriate or hamrful behaviors designed to influence shape or weight or counteract the effects of overeating | 76% of girls with obesity and 55% of boys with obesity endorse unhealthy weight control behaviors compared to 50% of normal-weight girls and 24% of normal-weight boys |
| Unhealthy: Fasting, skipping meals, eating very little food, using food substitutes, and using cigarettes or diet pills to suppress appetite | 18% of girls with obesity and 6% of boys with obesity endorse extreme weight control behaviors compared to 10% and 3% in their normal-weight counterparts, respectively [20] | |
| Extreme: Self-induced vomiting, laxative or diuretic abuse | ||
| Binge Eating & Loss of Control Eating | Binge Eating: Consumption of an objectively large amount of food with simultaneous feelings of loss of control | 31.2% of youth with overweight/obesity report LOC eating alone and 22.2% report binge eating [7] and rates are higher in children with overweight/obesity than normal-weight peers [25] |
| Loss of Control Eating: Feeling of being unable to control what or how much one is eating | ||
Attitudes Towards Shape and Weight.
Body dissatisfaction refers to negative appraisals of one’s shape and/or weight while the related construct of shape and weight concerns is defined as worries or anxieties about shape and/or weight [2]. Research has indicated elevated rates of body dissatisfaction and shape and weight concerns in youth with overweight and obesity compared to their non-overweight peers [16], which can lead to weight gain over time [17]. Body dissatisfaction or shape and weight concerns, which may fluctuates based on factors such as recent eating behaviors and mood, often are linked with overvaluation of shape and weight—the degree to which one’s self-esteem is highly contingent on shape and/or weight, which is a more stable construct and is considered the core psychopathology of EDs [18]. Approximately 25% of adolescent girls with overweight/obesity overvalue shape and weight and it is a prospective risk factor for development of eating disorder behaviors [19].
Disordered Weight Control Behaviors.
Unhealthy or extreme weight control behaviors are defined as inappropriate or harmful behaviors designed to influence weight or shape or counteract the effects of overeating. Such behaviors exist on a continuum corresponding to the degree of harm presented to one’s health, ranging from unhealthy (e.g., fasting, skipping meals, eating very little food, using food substitutes, and using cigarettes or diet pills to suppress appetite) to extreme (e.g., self-induced vomiting, laxative or diuretic abuse). Studies have found that unhealthy weight control behaviors were endorsed by up to 76% of girls with obesity and 55% of boys with obesity and more extreme weight control behaviors were reported by 18% of girls with obesity and 6% of boys with obesity [20]. In comparison to their non-overweight peers, youth with overweight and obesity are more than twice as likely to endorse the use of unhealthy or extreme weight control behaviors [21], which merits clinical attention due to their association with a variety of adverse physical and psychosocial outcomes [22, 23], including future ED pathology [24].
Binge Eating and Loss of Control Eating.
Binge eating episodes are also significantly more likely to be reported by youth with overweight than their non-overweight peers [25]. Such episodes are defined as the consumption of an objectively large amount of food accompanied by loss of control (LOC) or a feeling that one is unable to control what or how much one is eating. In children, given that changing nutritional needs of pubertal development [26] may alter what might be considered to be an unambiguously large amount of food, LOC eating is often the focus of assessment [25]. A recent meta-analysis found that over one quarter of adolescents with overweight and obesity endorse binge eating episodes, with up to 30% reporting LOC eating [7]. Moreover, such episodes have been linked with future weight gain [27].
Correlates of Dysfunctional Eating in Children with Obesity
The following section briefly reviews correlates of disordered eating attitudes and behaviors and/or obesity in childhood [also see Figure 1]. Notably, relatively few studies have been completed in children with both obesity and disordered eating pathology and little is known about why some children develop both conditions while others may only experience one. Moreover, the developmental time course and the causal factors of the initiation of both obesity and disordered eating in children is complex; while theories exist, more research is necessary [2].
Figure 1.
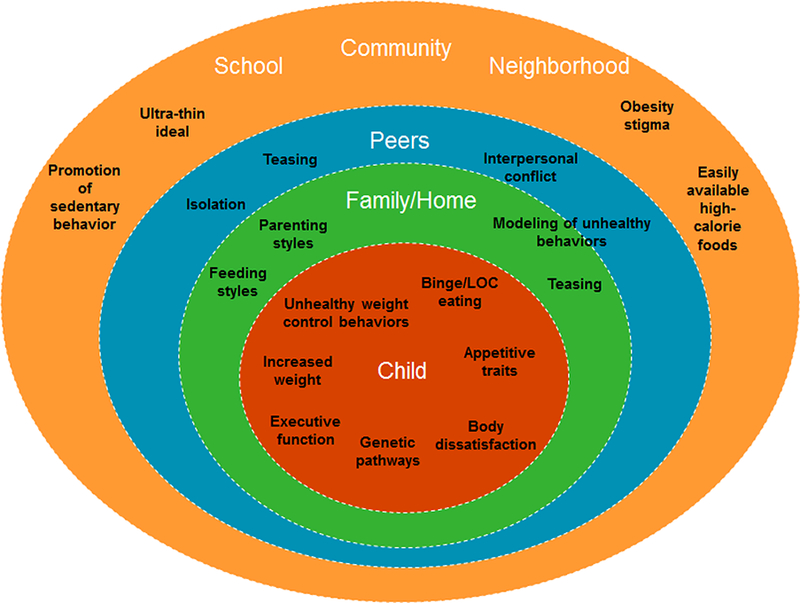
Individual and Environmental Correlates of Disordered Eating and Obesity
Individual-level Factors.
In addition to biological mechanisms and genotypes [28], emerging evidence suggests children with obesity who experience dysfunctional eating attitudes and behaviors have common underlying cognitive and behavioral characteristics. Evidence from cognitive tasks support deficits in executive functions (EFs), or a set of cognitive processes that support higher order cognitive abilities and goal attainment [29], in both children with obesity [30] and disordered eating [31]. Children with comorbid obesity and dysfunctional eating may have a cognitive profile that is distinct and more deficient then youth with obesity alone [32, 33]. Moreover, evidence by Goldschmidt and colleagues (2015) suggests a meditational model in which lower EF abilities are a precursor to binge eating, which in turn promotes excess calorie consumption and weight gain over time [34]. Another recent study found that adolescents with obesity who endorsed more cognitive dysregulation were more likely to endorse LOC eating [35].
As this research suggests, deficits in cognition may manifest in related dysfunctional behaviors. Food-seeking appetitive traits and poor self-regulation, including lack of satiety responsiveness, motivation to eat, impulsivity, and faster eating rates, have been observed in children with obesity at greater rates than normal-weight peers [36, 37]. Increasing endorsement of these traits may present a cumulative risk for excess calorie consumption and weight gain [36, 37]. The association between lack of satiety responsiveness and impulsivity with binge eating has also been highlighted [36] and other research suggests certain appetitive traits may be more severe in individuals with both obesity and BED [38].
Environmental-Level Factors.
Individual-level vulnerability factors may be exacerbated by obesogenic environments that promote easy access to food and sedentary activity. Palatable high-calorie foods are cheap, easily accessible, and are served in large portions, making it easy, affordable, and enjoyable to consume excess calories [39]. Furthermore, increases in sedentary jobs and reductions in recess and physical education in schools as well as advances in recreational technology (e.g., television, video games) mean children and families are spending more time seated and less time engaging in physical activity [40]. At the same time, individuals portrayed in the media have gotten thinner over the past 30 years, promoting the image of a ultra-thin body as ideal [41]. The combination of a thin ideal with an environment that promotes weight gain sends mixed messages that may lead to body dissatisfaction and development of unhealthy weight control behaviors [41]. Indeed, exposure to media promoting a thin ideal has been shown to predict disordered eating in adolescents with obesity [9].
In addition to societal characteristics, influences from family and peers may also interact with individual traits that predispose a child to weight gain and disordered eating. Authoritarian parenting, characterized by high demands and expectations but low responsiveness and support, is prospectively related to extreme weight control and binge eating behaviors compared to other parenting styles [42]. Conversely, authoritative parenting styles, characterized by high expectations and well as high responsiveness and support, are protective against obesity development [43]. Furthermore, family connectedness, such as feeling loved and having easy communication with a parent, is protective against disordered eating development in children with obesity [9]. Parental feeding practices, including restriction and pressure to eat, among others, have also been associated with various dysfunctional eating behaviors and excess food consumption [44, 45]. Additionally, children who are both underweight and overweight more commonly experience weight-related teasing by peers and family members than children of average weight, and appearance- and weight-related teasing has associations with ED behaviors [8, 46]. Moreover, teasing may be worse in individuals with both obesity and dysfunctional eating [47].
Using FBT for Childhood Obesity and Dysfunctional Eating
Due to the frequent comorbidity and similar underlying risk factors of childhood obesity and disordered eating, researchers have called to integrate the fields of obesity and EDs [48, 49] in order to promote shared knowledge and create preventative interventions that target the development of both issues. Initial work in this area has been conducted and appears promising [50, 51]. While this work continues, it is important to also consider treatment of the large number of children with obesity that currently experience dysfunctional eating attitudes and behaviors. Developing effective treatment methods that treat both obesity and subclinical disordered eating would not only reduce current psychological distress and potential health complications but may also serve to prevent the onset of diagnosable EDs as well as adult obesity, and their associated medical and psychological comorbidities.
FBT is the gold standard treatment for childhood obesity [52]. FBT follows a cognitive-behavioral therapy (CBT) approach to treatment and targets diet and physical activity using behavior change strategies. In FBT, parents are an integral part of treatment, as they control the home environment and can use positive parenting approaches and modeling to help children reach their weight loss goals. As such, they are included as participants in treatment programs, typically with one parent identified as the participating parent who attends each session and is a target for weight loss if they have overweight or obesity or desire to lose weight (and weight loss is an appropriate goal; i.e., not underweight). However, given changes are being made that affect the whole home and obesity runs in families [53], other family members are encouraged to join sessions whenever possible.
The positive outcomes of FBT are demonstrated by a large body of research indicating that children, as well as parents, are able to lose clinically-significant amounts of weight in FBT and children maintain a healthy weight into adulthood [11]. FBT has also been identified as being more cost-effective than treating the parent and child alone [54]. As such, the United States Preventive Services Task Force (USPSTF) and other professional organizations recommend clinicians screen children for obesity and refer them to comprehensive, intensive behavioral interventions such as FBT [52, 55]. Notably, dose of treatment is important, with 26 or more contact hours over 12 months identified as a minimal dose for efficacy [52].
FBT can be combined with a social facilitation maintenance (SFM) component, which utilizes a socioecological approach, emphasizing parental facilitation of children’s peer networks and improvement of children’s body image, as well as their responses to teasing, to promote maintenance of behaviors consistent with improved weight outcomes [56, 57]. When these approaches are integrated, they target development of healthy diet and activity behaviors, positive self- and body-esteem, supportive family relationships, and richer social networks as well as integration into a broader environment and community that facilitates overall physical and mental health [56, 57]. Two trials have tested FBT in combination with SFM, with results showing that participating in SFM following FBT, particularly when given at high dose, can lead to more successful weight loss maintenance than no follow-up treatment or a health education control treatment [56, 57]. Given the success of SFM, its components have subsequently been incorporated into current FBT protocols (e.g. NHLBI U01HL131552) and are discussed below as part of FBT.
Although a common concern regarding childhood obesity treatment is that the focus on modifying energy balance behaviors will increase the risk of the development of disordered eating or EDs, existing evidence suggests that this is not the case. Studies show a reduction in ED pathology following participation in an evidence-based weight loss program [12–15] as well as successful weight loss outcomes in children with ED pathology [12, 58, 15, 59, 13]. Notably, these studies provide insight into disordered eating pathology, but do not speak to the ability of FBT to treat clinical EDs. If a child presents with a full-syndrome ED, he/she should be referred to a specialist and given a treatment specifically designed for EDs. Goldschmidt and colleagues (2008) provide screening questions that may be used by healthcare providers to assess the presence and severity disordered eating attitudes and behaviors prior to referral to a weight management program [2]. The following section outlines the treatment components of FBT and discusses the mechanisms through which FBT may affect both excess weight and disordered eating [Table 2].
Table 2.
Treatment Components of FBT Weight loss and Maintenance Treatments and Relationship to Disordered Eating
| Specific Treatment Targets/Activities | Relationship to Disordered Eating | |
|---|---|---|
| Individual Behaviors | ||
| Diet Quality and Quantity |
- Children and parents shape to less than 15 servings of high-fat foods a week | - A flexible eating style within a generally healthy diet (e.g., not completely restricting access to high-calorie, palatable or “forbidden” foods) reduces disordered eating symptomology |
| - Children and parents eat 5 servings of fruits and vegetables a day | ||
| Physical/ Sedentary Activity |
- Children reduce screen time to less than 2 horns a day | - Physical activity for health and body esteem, not energy-balance, is emphasized |
| - Children increase physical activity to 90 min/day and parents to 60 min/day | - Physical activity promotes executive functioning, which may protect against dysregulation in disordered eating | |
| - Reduced screen time reduces time spent sedentary, overeating cues and exposure to body ideals | ||
| Healthy Routines | - Children and parents eat 3 meals and 1– 2 snacks per day | - Meal regularization is important to regulate hunger cues and prevents long periods without eating, which can be a trigger for disordered eating behaviors |
| - Children and parents keep a consistent and regular activity schedule | - Consistent routines and structure counter-act dysregulation | |
| - Children and parents keep consistent bedtimes and bedtime routines to ensure adequate sleep duration | ||
| Goal setting and Pre-planning | - Children and parents identify short and long-term weight and behavioral goals | - Prospective thinking and pre-planning help to build executive function skills and allow for planning around disordered eating behavior triggers |
| - Children and parents pre-plan meals, snacks, and physical activity each week | ||
| Self-Monitoring | - Children and parents track weight, food, and physical activity to monitor progress towards goals | - Regular weighing replaces too-frequent or avoidance of weighing that can perpetuate disordered eating thoughts and behaviors |
| - Monitoring of food and physical activity instances can help identify triggers contributing to disordered eating | ||
| Problem-Solving | - Children and parents problem solve around barriers to healthy eating and activity. | - Problem solving may be used for disordered eating behaviors, which could include improving decision making to avoid binge eating or finding alternatives to extreme weight control behaviors |
| Behavior Chains and Cognitive Restructuring | - Children identify antecedents and consequences to behaviors | - Behavior chains and cognitive restructuring may also be used for disordered eating attitudes and behaviors and are a key component of CBT for EDs |
| - Children identify negative automatic thoughts regarding the self and create a rational response | ||
| Building a Healthy Body Image | - Children participate in activities to reduce overvaluation of weight and shape and expand self-evaluation above and beyond appearance | - Overvaluation of weight and shape and body dissatisfaction are key features of eating disorders and activities included in FBT mimic evidence-based treatments for improving body image |
| Family and Home | ||
| Family Meetings and Contingency Management | - Children and parents identify a time each week to meet and discuss progress and barriers | - Family meetings promote interaction and cohesion among the child and parent, which may help to protect against disordered eating development |
| - Praise and external rewards are used to promote child buy-in to participation in FBT. | ||
| Communication and Parenting Skills | - Parents are taught communication skills and limit setting around energy-balance behaviors | - Parent behaviors (e.g., weight-based teasing of child, pressure to be thin) have been identified as risk factors for development of disordered eating. |
| Parental Modeling | - Parents are taught to model the behaviors they expect of their child to promote healthy child energy-balance behaviors | - Parental modeling of healthy energy-balance behaviors may replace unhealthy dieting behaviors, which have been identified as a risk factor for disordered eating. |
| - Parental modeling of healthy body image attitudes encourages development of healthy body image in the child | ||
| Healthy Home Environment |
- Parents are encouraged to create a home environment that easily supports healthy energy-balance behaviors, reducing temptations for sedentary behavior and high-fat foods. | - Creation of a healthy home environment reduces temptations that may “trigger” disordered eating attitudes and behaviors |
| Peers and Social Networks | ||
| Making New Friends and Active Get-Togethers | - Children are encouraged to build and form relationships with peers that support healthy eating and activity habits and can serve as an alternative rewarding experience to unhealthy eating and sedentary behavior | - Interpersonal conflict and isolation are related to disordered eating. Focusing on improving peer relationships helps reduce disordered eating. |
| Interpersonal Communication |
- Children learn about communication styles and build interpersonal communication skills | - Communication skill building serves to foster friendships and reduce conflict |
| Coping with Teasing |
- Children are taught to “tease the tease, not the teaser” (e.g., avoid insults) and to avoid emotional reactions that perpetuate the teasing cycle | - Weight-based teasing is related to disordered eating and adaptive coping strategies may prevent use of disordered eating behaviors |
| School, Work, Community, and Culture | ||
| Advocating for Healthy Social Environments and Navigating Barriers | - Children and parents identify and navigate environmental barriers that are weight-gain promoting and advocate within their community to promote healthy habits | - Creation of healthy environments and problem solving around unhealthy environments may reduce triggers for disordered eating |
| Understanding Stigma and Interpreting Media Messages | - Children are taught media literacy skills to interpret messages regarding ultra-thin ideals and obesity stigma in media | - Reduction in internalization of the thin ideal may work towards preventing and treating disordered eating attitudes and behaviors |
FBT Treatment Components
Individual Components
Diet Quality.
A key focus of FBT is to improve diet quality and maintain a reduced, but healthy, calorie range for weight loss. Children, and their participating parent, work to increase fruits and vegetables per day and to decrease high-fat foods to lose weight and promote long-term health [60]. An emphasis is placed on developing sustainable healthy eating habits and these changes are shaped over time, a process of reinforcing successive approximations of a target behavior that helps to slowly and steadily build new habits [61]. Moreover, by including high-fat foods in moderation each day, children are taught a flexible approach to eating in which no food is “forbidden”. This form of dietary change is associated with successful and sustainable weight management and reductions in disordered eating symptomology [62]. Healthy dietary change strategies stand in stark contrast to “driven dieting”, which is comprised of unhealthy psychological and behavioral experiences, such as maintaining rigid rules and fasting, which are frequently cited as a risk factor for ED development [62].
Physical/Sedentary Activity.
Physical activity is a critical component of weight management and long-term health [63]. As such, children in FBT work toward obtaining 90 minutes of activity at least five days a week. To do so, children are encouraged to choose activities they enjoy in order to develop healthy life-long physical activity habits [64]. When discussing physical activity, health benefits, not energy-balancing characteristics, are emphasized. Thus, children are taught that regular physical activity is part of a healthy and active lifestyle and not a compensatory behavior for eating. Additional benefits of increasing physical activity across treatment include benefits to EFs through exercise-induced physiological changes in the brain and practice of EF skills required for initiating complex motor movements and engaging in group play [65]. Reduction of sedentary activity, specifically recreational screen time (e.g., television-watching, video games) to two hours or fewer a day is another treatment target. Reducing screen time decreases time spent sedentary and encourages physical activity, which promotes positive mood as well as social interaction, and reduces exposure to media that may encourage unhealthy eating patterns as well as difficult to attain societal ideals (e.g., very thin body type) [66–68].
Healthy Routines.
The development of routines has been shown to be helpful in improving obesogenic behaviors and reducing weight [69]. FBT focuses on the establishment of routines for eating, physical activity, and sleep. Meal regularization is particularly important as eating regular meals and snacks helps to prevent feelings of extreme hunger, which can lead to poor food choices and overeating. Indeed, individuals who engage in unhealthy weight control behaviors or LOC/binge eating often go long periods of time between meals/snacks, and as a result, have dysregulated hunger signals [70]. More generally, routines help to ensure behaviors are achieved regularly (e.g., regular physical activity, 8–9 hours of sleep a night) and provide consistency and structure to counter-act dysregulation.
Goal-setting and Pre-planning.
In FBT, children and parents set short- and long-term goals around weight loss and energy-balance behaviors. Moreover, in session, families work to plan the following week (e.g., meals, physical activity). Planning is a complex EF [29] and may be one of the treatment activities that help children build their EF skills [65], which should aid in the general development of self-regulatory skills . Planning may also help to reduce impulsive decision-making and encourage goal-oriented behavior [71].
Self-monitoring.
In FBT, weights are taken weekly during session and children and parents weigh themselves once a week at home. Weighing regularly at established times provides participants with feedback about their weight loss progress and provides an opportunity to reflect on behaviors that have led to weight changes [72]. Structured weighing is also a hallmark of a CBT approach to EDs and is encouraged to replace either too-frequent weighing or avoidance of weighing that can perpetuate disordered eating thoughts and behaviors [70]. Additionally, participants in FBT monitor food intake and activity engagement. Self-monitoring of energy-balance behaviors can bring awareness to patterns of eating and activity, as well as psychological, social, or environmental factors that influence these patterns [73]. Self-monitoring combined with goal setting has been shown to mediate weight outcomes in FBT [56] and frequency of self-monitoring has been associated with better child weight outcomes in FBT [74]. Records also provide the interventionist insight into participant behaviors related to weight-loss or disordered eating behaviors that can then be addressed within session.
Problem-solving.
A cognitive behavioral approach to problem-solving is taught in FBT that asks participants to pause and think about all possible solutions before evaluating and choosing a course of action. Both children and parents are trained to use this strategy to approach problems relating to energy-balance behaviors, which could include improving decision making so as to help avoid binge eating or finding alternative and healthier solutions than extreme weight control behaviors.
Behavior Chains and Cognitive Restructuring.
Relatedly, behavior chains, which help to identify antecedents and consequences of behavior, can provide insight into issues to problem solve. Cognitive restructuring, or challenging negative automatic thoughts replacing them with more balanced, accurate thoughts, is also taught. These strategies are used to address negative thoughts and behavioral triggers that lead to emotional eating as well as to identify alternative coping strategies, but may also be used to address any unhealthy cognition or behavior that is a treatment barrier or is negatively affecting the child. Both parents and children are taught these skills and reinforced for their use across treatment. Behavior chains and cognitive restructuring are used in CBT for EDs to identify triggers for disordered eating behaviors and address thoughts related to body dissatisfaction, overvaluation of weight and shape, low self-esteem, and perfectionism [70].
Building a Healthy Body Image.
Given the number of children with obesity whom experience body dissatisfaction [16], this is a specific target of FBT. Treatment activities mirror those included in empirically-supported programs developed to improve body satisfaction [75]. Children complete activities that reduce overvaluation of weight and shape and expand their selfevaluation by integrating multiple characteristics above and beyond appearance, such as identifying physical activities their bodies help them to do and non-physical attributes that they like about themselves.
Family and Home Components
Family Meetings and Contingency Management.
Upon initiation of FBT, parent-child dyads identify a weekly meeting time to talk and reflect on their experiences, promoting a team-based approach to treatment. These meetings provide time for families to discuss successes and barriers in order to improve adherence with treatment recommendations as well as connectedness in the relationship, which help to both prevent and target disordered eating [9]. Furthermore, parents are able to monitor child behaviors and identify any concerning issues (e.g., LOC eating, skipping meals). Contingency management is a strategy utilized in FBT to help support child behavior change and family cohesion. Parents are encouraged to reinforce their child’s positive behaviors using verbal and non-verbal praise as well as external rewards. Frequent praise and positive reinforcement should also contribute to parent-child relationship and use of external rewards that are non-food items help to promote alternative reinforcers to food [76, 77].
Communication and Parenting Skills.
Communicating with a child regarding weight and energy-balance behaviors should be done carefully, as evidence has shown that pressure from parents to diet can promote disordered eating and weight gain [78]. Parental weight-based teasing is also common and can pre-date development of disordered eating [78]. Within FBT, parents are taught communication skills and are asked to focus on health, not weight, when discussing diet and physical activity with their children. Strategies are also taught for parenting around topics related to disordered eating attitudes and behaviors, such as encouraging discussion of media images, praising their child for non-appearance related characteristics, and avoiding discussions of their own or other’s bodies in front of their child. Improving communication, increasing support, and reducing conflict within the family through interpersonal psychotherapy has been shown to be helpful for children with overweight/obesity and LOC eating by reducing LOC eating episodes and disordered eating attitudes [79]. As such, FBT elements focusing on communication within the parent-child relationship may be one mechanism through which to reduce disordered eating.
Parental Modeling.
Children imitate and learn from parent energy-balance behaviors [80]. As such, parental modeling is a key component of FBT and has been theorized to contribute to the robust association between parent and child weight loss [81, 82]. Notably, unhealthy energy-balance behaviors that are modeled by parents also show an association with child behavior [78]. By providing parents with healthy weight management strategies, they may be less likely to engage in unhealthy weight management behaviors that would then be imitated by their children.
Healthy Home Environment.
Stimulus control, or management of the home environment to support goal-aligned behaviors, is a hallmark of FBT. By reducing temptations, children have less need to control impulses related to eating, which may reduce overconsumption of calories and disordered eating episodes [83]. Family and home environments that are set up to support the child have shown to be a mediator of weight outcomes in FBT [56].
Peers and Social Networks
Making New Friends and Active Get-Togethers.
Based on research suggesting children with obesity are more isolated than their normal weight peers [84], FBT encourages children to broaden their social networks and improve their social integration. Improving social ties may also be beneficial for improving disordered eating, which is associated with loneliness [85]. Relationships with others serve as alternate rewarding experiences to food and children are encouraged to seek out friends who will support healthy lifestyle changes, as obesity and obesogenic behaviors move through social networks [86]. Importantly, this includes friends who have a healthy view of self and appearance, as having friends who diet predicts development of unhealthy weight control behaviors and binge eating [87]. Within existing friendships, an emphasis is also placed on engaging in play dates that include healthy food and activity options. Playing with friends has been associated with greater physical activity in youth [88] and engaging in healthy behaviors with peers has been shown to mediate weight loss outcomes [56].
Interpersonal Communication.
To facilitate the establishment of social connections, and to allow for effective peer interaction, children are taught about different types of communication styles. Lower social competence has been linked with obesity development and treatment studies suggest social skills development and improved social interaction may be particularly helpful for children with adjustment and anxiety issues in weight management [89, 90]. Social connectedness and interpersonal communication skills should be effective for the prevention and treatment of disordered eating as well, as social stress has been identified as a trigger for binge eating [91] and therapies designed to improve interpersonal relationships with peers have been demonstrated as effective for reduction of disordered eating in adolescents [92].
Coping with Teasing.
Teasing from peers is related to both obesity and disordered eating behavior [8]. Interventionists work with children in FBT to identify adaptive ways to cope with teasing and utilize strategies to reduce teasing, including ignoring the teaser, reframing the tease into a less negative statement, or responding to the tease with a compliment [93].
School, Work, Community, and Culture
Advocating for Healthy Social Environments and Navigating Barriers.
The environment plays a large role in eating and activity behaviors [40]. In FBT, parents and children are asked to consider the environments outside the home in which they spend their time (e.g., school, work) and how these places influence the long-term goal of healthy weight management. Active problem solving is used to identify solutions for navigating environmental barriers (e.g., identify a route home from school that does not involve passing a favorite fast-food restaurant) and changing environments to support healthy behaviors (e.g., advocating for non-food birthday treats to be brought into classrooms). By creating a healthy environment, families may be less tempted to return to old habits [56]. Furthermore, in focusing on practicing newly learned behaviors across contexts, this promotes generalization of the new behaviors to a variety of life domains, encouraging mastery of the behaviors and habit formation [94, 95]. Indeed, it has been suggested that by including strategies that promote learning and memory in behavioral and psychological interventions, outcomes may improve [96].
Understanding Stigma and Interpreting Media Messages.
Engagement with media that promotes an idealized, thin body type is a risk factor for body dissatisfaction, disordered eating, and obesity, as well as other negative psychosocial outcomes in children [97]. Moreover, media for children contains stigmatizing messages of obesity that contribute to increased obesity bias in peers and reinforce stigmatization experienced by children with obesity [98]. Children in FBT are taught media literacy skills to practice interpreting media messages regarding weight and shape, reducing identification with the thin ideal as well as internalizing of stigmatizing messages regarding obesity [99].
Conclusions
Disordered eating attitudes and behaviors in children with obesity are common. Children who experience both obesity and disordered eating attitudes and behaviors are at risk for continued weight gain and adult obesity as well as the development of an ED. FBT is an effective treatment for childhood obesity and preventative intervention for adult obesity. Emerging research also suggests participation in FBT may be beneficial for improving disordered eating attitudes and behaviors in children with obesity while reducing weight, although additional empirical examination (e.g. a randomized controlled trial) is needed. Notably, there has been no evaluation to assess FBT as a treatment for diagnosable EDs in children and it is recommended children with EDs seek ED-specific treatment prior to consideration for participation in FBT.
FBT is likely an effective treatment for disordered eating in children with obesity given its focus on the development of healthy energy balance behaviors as well as positive self- and body-esteem, supportive family relationships, more meaningful social networks, and an environment and community that promotes overall physical and mental health. Future dismantling studies could be used to fully understand which treatment components of FBT may have the most potent effects on disordered eating. Moreover, a richer understanding of the development of both obesity and disordered eating in children, such as appetitive traits that may precede these conditions in early childhood, would be valuable in tailoring FBT to most effectively target a child’s individual needs and determine optimal time for intervention.
Acknowledgments
Denise E. Wilfley has received research funding through grants from the National Institute of Child Health and Human Development (Grant #R01HD036904), the National Institute of Mental Health (Grant #K24MH070446), and the St. Louis Children’s Hospital Foundation.
Footnotes
Compliance with Ethics Guidelines
Conflict of Interest
Jacqueline F. Hayes declares that she has no conflict of interest.
Ellen E. Fitzsimmons-Craft declares that she has no conflict of interest.
Anna M. Karam declares that she has no conflict of interest.
Jessica Jakubiak declares that she has no conflict of interest.
Mackenzie L. Brown declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Bibliography/References Cited
- *1.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the united states, 1988–1994 through 2013–2014. JAMA. 2016;315(21):2292–9. doi: 10.1001/jama.2016.6361.Analysis of obesity trends from 1988–1994 to 2013–2014 showing obesity rates of 17% and extreme obesity rates of 5.8% in children aged 2–19.
- 2.Goldschmidt AB, Aspen VP, Sinton MM, Tanofsky‐Kraff M, Wilfley DE. Disordered eating attitudes and behaviors in overweight youth. Obesity. 2008;16(2):257–64. [DOI] [PubMed] [Google Scholar]
- 3.Sheehan DV, Herman BK. The psychological and medical factors associated with untreated binge eating disorder. The primary care companion for CNS disorders. 2015; 17(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herpertz-Dahlmann B Adolescent eating disorders: update on definitions, symptomatology, epidemiology, and comorbidity. Child and Adolescent Psychiatric Clinics. 2015;24(1): 177–96. [DOI] [PubMed] [Google Scholar]
- 5.Pulgaron ER. Childhood obesity: a review of increased risk for physical and psychological comorbidities. Clinical therapeutics. 2013;35(1):A18–A32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cunningham SA, Kramer MR, Narayan KV. Incidence of childhood obesity in the United States. New England Journal of Medicine. 2014;370(5):403–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **7.He J, Cai Z, Fan X. Prevalence of binge and loss of control eating among children and adolescents with overweight and obesity: An exploratory meta‐analysis. International Journal of Eating Disorders. 2017;50(2):91–103.An exploratory meta-analysis showing more than a quarter of children and adolescents with overweight and obesity endorse binge/LOC eating.
- 8.Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan PJ, Mulert S. Weight-teasing among adolescents: correlations with weight status and disordered eating behaviors. International journal of obesity. 2002;26(1):123. [DOI] [PubMed] [Google Scholar]
- 9.Neumark‐Sztainer D, Wall M, Story M, Sherwood NE. Five‐year longitudinal predictive factors for disordered eating in a population‐based sample of overweight adolescents: Implications for prevention and treatment. International Journal of Eating Disorders. 2009;42(7):664–72. [DOI] [PubMed] [Google Scholar]
- 10.Pervanidou P, Bastaki D, Chouliaras G, Papanikolaou K, Laios E, Kanaka-Gantenbein C et al. Circadian cortisol profiles, anxiety and depressive symptomatology, and body mass index in a clinical population of obese children. Stress. 2013;16(l):34–43. [DOI] [PubMed] [Google Scholar]
- 11.Epstein LH, Paluch RA, Roemmich JN, Beecher MD. Family-based obesity treatment, then and now: twenty-five years of pediatric obesity treatment. Health Psychology. 2007;26(4):381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bishop-Gilyard CT, Berkowitz RI, Wadden TA, Gehrman CA, Cronquist JL, Moore RH. Weight reduction in obese adolescents with and without binge eating. Obesity. 2011;19(5):982–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **13.Balantekin KN, Hayes JF, Sheinbein DH, Kolko RP, Stein RI, Saelens BE et al. Patterns of eating disorder pathology are associated with weight change in family-based behavioral obesity treatment. Obesity. 2017;25(12):2115–22.An empirical study demonstrating varied patterns of eating disorder pathology in treatment-seeking children with obesity. Results also indicate family-based treatment for childhood obesity effectively reduces eating disorder pathology and weight in participating children, regardless of severity of eating disorder pathology.
- 14.Butryn ML, Wadden TA. Treatment of overweight in children and adolescents: Does dieting increase the risk of eating disorders? International Journal of Eating Disorders. 2005;37(4):285–93. [DOI] [PubMed] [Google Scholar]
- 15.Braet C Patient characteristics as predictors of weight loss after an obesity treatment for children. Obesity. 2006;14(1):148–55. [DOI] [PubMed] [Google Scholar]
- 16.Crow S, Eisenberg ME, Story M, Neumark-Sztainer D. Psychosocial and behavioral correlates of dieting among overweight and non-overweight adolescents. Journal of Adolescent Health. 2006;38(5):569–74. [DOI] [PubMed] [Google Scholar]
- 17.Loth KA, Watts AW, Van Den Berg P, Neumark-Sztainer D. Does body satisfaction help or harm overweight teens? A 10-year longitudinal study of the relationship between body satisfaction and body mass index. Journal of Adolescent Health. 2015;57(5):559–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cooper PJ, Fairburn CG. Confusion over the core psychopathology of bulimia nervosa. International Journal of Eating Disorders. 1993;13(4):385–9. [DOI] [PubMed] [Google Scholar]
- 19.Sonneville KR, Grilo CM, Richmond TK, Thurston IB, Jernigan M, Gianini L et al. Prospective association between overvaluation of weight and binge eating among overweight adolescent girls. Journal of Adolescent Health. 2015;56(1):25–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neumark-Sztainer D, Story M, Hannan PJ, Perry CL, Irving LM. Weight-related concerns and behaviors among overweight and nonoverweight adolescents: implications for preventing weight-related disorders. Archives of pediatrics & adolescent medicine. 2002;156(2):171–8. [DOI] [PubMed] [Google Scholar]
- *21.Lampard AM, Maclehose RF, Eisenberg ME, Larson NI, Davison KK, Neumark-Sztainer D. Adolescents who engage exclusively in healthy weight control behaviors: Who are they? International Journal of Behavioral Nutrition and Physical Activity. 2016;13(1):5.A study suggesting that healthy weight control strategies in adolescents are associated with lower body dissatisfaction, high self-esteem, and lower depressive symptoms.
- 22.Stephen EM, Rose JS, Kenney L, Rosselli-Navarra F, Weissman RS. Prevalence and correlates of unhealthy weight control behaviors: Findings from the national longitudinal study of adolescent health. Journal of eating disorders. 2014;2(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neumark-Sztainer D, Wall M, Story M, Standish AR. Dieting and unhealthy weight control behaviors during adolescence: Associations with 10-year changes in body mass index. Journal of Adolescent Health. 2012;50(l):80–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stice E, Gau JM, Rohde P, Shaw H. Risk factors that predict future onset of each DSM-5 eating disorder: Predictive specificity in high-risk adolescent females. Journal of abnormal psychology. 2017;126(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating-disordered behaviors, body fat, and psychopathology in overweight and normal-weight children. Journal of Consulting and Clinical Psychology. 2004;72(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cheng HL, Amatoury M, Steinbeck K. Energy expenditure and intake during puberty in healthy nonobese adolescents: A systematic review, 2. The American journal of clinical nutrition. 2016; 104(4): 1061–74. [DOI] [PubMed] [Google Scholar]
- 27.Tanofsky-Kraff M, Cohen ML, Yanovski SZ, Cox C, Theim KR, Keil M et al. A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics. 2006; 117(4): 1203–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bulik CM, Sullivan PF, Kendler KS. Genetic and environmental contributions to obesity and binge eating. International Journal of Eating Disorders. 2003;33(3):293–8. [DOI] [PubMed] [Google Scholar]
- 29.Diamond A Executive functions. Annual review of psychology. 2013;64:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reinert KR, Po’e EK, Barkin SL. The relationship between executive function and obesity in children and adolescents: A systematic literature review. Journal of obesity. 2013;2013:820956. doi: 10.1155/2013/820956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Darcy AM, Fitzpatrick KK, Manasse SM, Datta N, Klabunde M, Colborn D et al. Central coherence in adolescents with bulimia nervosa spectrum eating disorders. International Journal of Eating Disorders. 2015;48(5):487–93. [DOI] [PubMed] [Google Scholar]
- 32.Goldschmidt AB, O’Brien S, Lavender JM, Pearson CM, Le Grange D, Hunter SJ. Executive functioning in a racially diverse sample of children who are overweight and at risk for eating disorders. Appetite. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gowey MA, Lim CS, Dutton GR, Silverstein JH, Dumont-Driscoll MC, Janicke DM. Executive function and dysregulated eating behaviors in pediatric obesity. Journal of pediatric psychology. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goldschmidt AB, Hipwell AE, Stepp SD, McTigue KM, Keenan K. Weight gain, executive functioning, and eating behaviors among girls. Pediatrics. 2015;136(4):e856–e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gowey MA, Reiter-Purtill J, Becnel J, Peugh J, Mitchell JE, Zeller MH et al. Weight-related correlates of psychological dysregulation in adolescent and young adult (AYA) females with severe obesity. Appetite. 2016;99:211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wilfley DE, Vannucci A, White EK. Early intervention of eating-and weight-related problems. Journal of Clinical Psychology in Medical Settings. 2010;17(4):285–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kral TV, Moore RH, Chittams J, Jones E, O’Malley L, Fisher JO. Identifying behavioral phenotypes for childhood obesity. Appetite. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Giel KE, Teufel M, Junne F, Zipfel S, Schag K. Food-related impulsivity in obesity and binge eating disorder—A systematic update of the evidence. Nutrients. 2017;9(11): 1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML et al. The global obesity pandemic: shaped by global drivers and local environments. The Lancet. 2011;378(9793):804–14. [DOI] [PubMed] [Google Scholar]
- 40.Sallis JF, Glanz K. Physical activity and food environments: solutions to the obesity epidemic. The Milbank Quarterly. 2009;87(1): 123–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grabe S, Ward LM, Hyde JS. The role of the media in body image concerns among women: a meta-analysis of experimental and correlational studies. Psychological bulletin. 2008;134(3):460. [DOI] [PubMed] [Google Scholar]
- 42.Zubatsky M, Berge J, Neumark-Sztainer D. Longitudinal associations between parenting style and adolescent disordered eating behaviors. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2015;20(2): 187–94. [DOI] [PubMed] [Google Scholar]
- 43.Sokol RL, Qin B, Poti J. Parenting styles and body mass index: a systematic review of prospective studies among children. Obesity Reviews. 2017;18(3):281–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Loth KA, MacLehose RF, Fulkerson JA, Crow S, Neumark-Sztainer D. Are food restriction and pressure-to-eat parenting practices associated with adolescent disordered eating behaviors? International Journal of Eating Disorders. 2014;47(3):310–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rodgers RF, Paxton SJ, Massey R, Campbell KJ, Wertheim EH, Skouteris H et al. Maternal feeding practices predict weight gain and obesogenic eating behaviors in young children: a prospective study. International Journal of Behavioral Nutrition and Physical Activity. 2013;10(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Menzel JE, Schaefer LM, Burke NL, Mayhew LL, Brannick MT, Thompson JK. Appearance-related teasing, body dissatisfaction, and disordered eating: A meta-analysis. Body image. 2010;7(4):261–70. [DOI] [PubMed] [Google Scholar]
- 47.Jackson TD, Grilo CM, Masheb RM. Teasing history, onset of obesity, current eating disorder psychopathology, body dissatisfaction, and psychological functioning in binge eating disorder. Obesity. 2000;8(6):451–8. [DOI] [PubMed] [Google Scholar]
- 48.Neumark-Sztainer D The interface between the eating disorders and obesity fields: Moving toward a model of shared knowledge and collaboration. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2009;14(l):51–8. [DOI] [PubMed] [Google Scholar]
- 49.Sanchez-Carracedo D, Neumark-Sztainer D, Lopez-Guimera G. Integrated prevention of obesity and eating disorders: barriers, developments and opportunities. Public Health Nutrition. 2012;15(12):2295–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Neumark-Sztainer DR, Friend SE, Flattum CF, Hannan PJ, Story MT, Bauer KW et al. New moves—preventing weight-related problems in adolescent girls: a group-randomized study. American journal of preventive medicine. 2010;39(5):421–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stock S, Miranda C, Evans S, Plessis S, Ridley J, Yeh S et al. Healthy Buddies: a novel, peer-led health promotion program for the prevention of obesity and eating disorders in children in elementary school. Pediatrics. 2007;120(4):el059–e68. [DOI] [PubMed] [Google Scholar]
- *52.O’connor EA, Evans CV, Burda BU, Walsh ES, Eder M, Lozano P. Screening for obesity and intervention for weight management in children and adolescents: evidence report and systematic review for the US Preventive Services Task Force. Jama. 2017;317(23):2427–44.A systematic review and meta-analysis demonstrating that moderate intensity multicomponent lifestyle interventions for children are effective at reducing childhood obesity.
- 53.Whitaker KL, Jarvis MJ, Beeken RJ, Boniface D, Wardle J. Comparing maternal and paternal intergenerational transmission of obesity risk in a large population-based sample-. The American Journal of Clinical Nutrition. 2010;91(6): 1560–7. [DOI] [PubMed] [Google Scholar]
- 54.Epstein LH, Paluch RA, Wrotniak BH, Daniel TO, Kilanowski C, Wilfley D et al. Cost-Effectiveness of Family-Based Group Treatment for Child and Parental Obesity. Childhood Obesity. 2014; 10(2): 114–21. [DOI] [PubMed] [Google Scholar]
- 55.Spear BA, Barlow SE, Ervin C, Ludwig DS, Saelens BE, Schetzina KE et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics. 2007; 120(Supplement 4):S254–S88. [DOI] [PubMed] [Google Scholar]
- *56.Wilfley DE, Saelens BE, Stein RI, Best JR, Kolko RP, Schechtman KB et al. Dose, content, and mediators of family-based treatment for childhood obesity: A multisite randomized clinical trial. JAMA Pediatrics. 2017.A randomized-controlled trial suggested a high-dose of social facilitation maintenance treatment (SFM), a socioecological approach that emphasizes parental facilitation of children’s peer networks and improvement of children’s body image, as well as their responses to teasing, is effective for maintaining weight loss in children.
- 57.Wilfley DE, Stein RI, Saelens BE, Mockus DS, Matt GE, Hayden-Wade HA et al. Efficacy of maintenance treatment approaches for childhood overweight: a randomized controlled trial. JAMA. 2007;298(14): 1661–73. [DOI] [PubMed] [Google Scholar]
- 58.Giel KE, Zipfel S, Schweizer R, Braun R, Ranke MB, Binder G et al. Eating disorder pathology in adolescents participating in a lifestyle intervention for obesity: associations with weight change, general psychopathology and health-related quality of life. Obesity facts. 2013;6(4):307–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Goldschmidt AB, Best JR, Stein RI, Saelens BE, Epstein LH, Wilfley DE. Predictors of Child weight loss and maintenance among family-based treatment completers. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sotos-Prieto M, Bhupathiraju SN, Mattei J, Fung TT, Li Y, Pan A et al. Association of changes in diet quality with total and cause-specific mortality. New England Journal of Medicine. 2017;377(2):143–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cooper JO, Heron TE, Heward WL. Applied behavior analysis. 2007. [DOI] [PMC free article] [PubMed]
- **62.Haynos AF, Field AE, Wilfley DE, Tanofsky-Kraff M. A novel classification paradigm for understanding the positive and negative outcomes associated with dieting. The International Journal of Eating Disorders. 2015;48(4):362.A paper proposing a novel classification scheme for dieting that includes positive and negative psychological dimensions as well as high and low behavioral dimensions.
- 63.Reiner M, Niermann C, Jekauc D, Woll A. Long-term health benefits of physical activity-a systematic review of longitudinal studies. BMC public health. 2013; 13(1):813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tammelin R, Yang X, Leskinen E, Kankaanpaa A, Hirvensalo M, Tammelin T et al. Tracking of physical activity from early childhood through youth into adulthood. Med Sci Sports Exerc. 2014;46:955–62. [DOI] [PubMed] [Google Scholar]
- 65.Hayes JF, Eichen DM, Barch DM, Wilfley DE. Executive function in childhood obesity: Promising intervention strategies to optimize treatment outcomes. Appetite. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Harris JL, Bargh JA. Television viewing and unhealthy diet: implications for children and media interventions. Health communication. 2009;24(7):660–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Epstein LH, Paluch RA, Gordy CC, Dorn J. Decreasing sedentary behaviors in treating pediatric obesity. Archives of pediatrics & adolescent medicine. 2000;154(3):220–6. [DOI] [PubMed] [Google Scholar]
- 68.Tiggemann M, Slater A. NetTweens: The Internet and body image concerns in preteenage girls. The Journal of Early Adolescence. 2014;34(5):606–20. [Google Scholar]
- 69.Haines J, McDonald J, O’Brien A, Sherry B, Bottino CJ, Schmidt ME et al. Healthy habits, happy homes: randomized trial to improve household routines for obesity prevention among preschool-aged children. JAMA pediatrics. 2013; 167(11): 1072–9. [DOI] [PubMed] [Google Scholar]
- 70.Murphy R, Straebler S, Cooper Z, Fairburn CG. Cognitive behavioral therapy for eating disorders. Psychiatric Clinics. 2010;33(3):611–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gollwitzer PM. Weakness of the will: Is a quick fix possible? Motivation and Emotion. 2014;38(3):305–22. [Google Scholar]
- 72.Steinberg DM, Bennett GG, Askew S, Tate DF. Weighing every day matters: daily weighing improves weight loss and adoption of weight control behaviors. Journal of the Academy of Nutrition and Dietetics. 2015; 115(4):511–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Levy RL, Finch EA, Crowell MD, Talley NJ, Jeffery RW. Behavioral intervention for the treatment of obesity: strategies and effectiveness data. The American journal of gastroenterology. 2007;102(10):2314. [DOI] [PubMed] [Google Scholar]
- 74.Mockus DS, Macera CA, Wingard DL, Peddecord M, Thomas RG, Wilfley DE. Dietary self-monitoring and its impact on weight loss in overweight children. Pediatric Obesity. 2011;6(3 – 4): 197–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Stice E, Rohde P, Shaw H. The body project: A dissonance-based eating disorder prevention intervention. Oxford University Press; 2012. [Google Scholar]
- 76.Hawes DJ, Allen J. Evidence-based parenting interventions: Current perspectives and clinical strategies Positive Mental Health, Fighting Stigma and Promoting Resiliency for Children and Adolescents. Elsevier; 2016. p. 185–204. [Google Scholar]
- 77.Carr KA, Daniel TO, Lin H, Epstein LH. Reinforcement pathology and obesity. Current drug abuse reviews. 2011;4(3): 190–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Neumark-Sztainer D, Bauer KW, Friend S, Hannan PJ, Story M, Berge JM. Family weight talk and dieting: how much do they matter for body dissatisfaction and disordered eating behaviors in adolescent girls? Journal of Adolescent Health. 2010;47(3):270–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shomaker LB, Tanofsky-Kraff M, Matherne CE, Mehari RD, Olsen CH, Marwitz SE et al. A randomized, comparative pilot trial of family‐based interpersonal psychotherapy for reducing psychosocial symptoms, disordered‐eating, and excess weight gain in at‐risk preadolescents with loss - of - control - eating. International Journal of Eating Disorders. 2017;50(9):1084–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Blissett J, Fogel A. Intrinsic and extrinsic influences on children’s acceptance of new foods. Physiology & behavior. 2013;121:89–95. [DOI] [PubMed] [Google Scholar]
- 81.Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN. Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Archives of pediatrics & adolescent medicine. 2004;158(4):342–7. [DOI] [PubMed] [Google Scholar]
- 82.Wilfley DE, Tibbs TL, Van Buren D, Reach KP, Walker MS, Epstein LH. Lifestyle interventions in the treatment of childhood overweight: a meta-analytic review of randomized controlled trials. Health Psychology. 2007;26(5):521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ely AV, Cusack A, editors. The Binge and the Brain Cerebrum: the Dana forum on brain science; 2015: Dana Foundation. [PMC free article] [PubMed] [Google Scholar]
- 84.Strauss RS, Pollack HA. Social marginalization of overweight children. Archives of pediatrics & adolescent medicine. 2003;157(8):746–52. [DOI] [PubMed] [Google Scholar]
- 85.Levine MP. Loneliness and eating disorders. The Journal of psychology. 2012;146(l-2):243–57. [DOI] [PubMed] [Google Scholar]
- 86.Valente TW, Fujimoto K, Chou C-P, Spruijt-Metz D. Adolescent affiliations and adiposity: a social network analysis of friendships and obesity. Journal of Adolescent Health. 2009;45(2):202–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Eisenberg ME, Neumark-Sztainer D. Friends’ dieting and disordered eating behaviors among adolescents five years later: Findings from Project EAT. Journal of Adolescent Health. 2010;47(l):67–73. [DOI] [PubMed] [Google Scholar]
- 88.Salvy S- J, Roemmich JN, Bowker JC, Romero ND, Stadler PJ, Epstein LH. Effect of peers and friends on youth physical activity and motivation to be physically active. Journal of pediatric psychology. 2008;34(2):217–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tanofsky-Kraff M, Shomaker LB, Wilfley DE, Young JF, Sbrocco T, Stephens M et al. Excess weight gain prevention in adolescents: Three-year outcome following a randomized controlled trial. Journal of consulting and clinical psychology. 2017;85(3):218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jackson SL, Cunningham SA. Social competence and obesity in elementary school. American journal of public health. 2015;105(l):153–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Shank LM, Crosby RD, Grammer AC, Shomaker LB, Vannucci A, Burke NL et al. Examination of the interpersonal model of loss of control eating in the laboratory. Comprehensive psychiatry. 2017;76:36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Tanofsky-Kraff M, Shomaker LB, Wilfley DE, Young JF, Sbrocco T, Stephens M et al. Targeted prevention of excess weight gain and eating disorders in high-risk adolescent girls: a randomized controlled trial-. The American journal of clinical nutrition. 2014; 100(4): 1010–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Freedman JS. Easing the Teasing: How Parents Can Help Their Children. ERIC Digest. 1999. [Google Scholar]
- 94.Bouton ME, Winterbauer NE, Todd TP. Relapse processes after the extinction of instrumental learning: renewal, resurgence, and reacquisition. Behavioural processes. 2012;90(1):130–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Forman EM, Butryn ML, Manasse SM, Crosby RD, Goldstein SP, Wyckoff EP et al. Acceptance‐based versus standard behavioral treatment for obesity: Results from the mind your health randomized controlled trial. Obesity. 2016;24(10):2050–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Harvey AG, Lee J, Williams J, Hollon SD, Walker MP, Thompson MA et al. Improving outcome of psychosocial treatments by enhancing memory and learning. Perspectives on Psychological Science. 2014;9(2):161–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Rodgers RF, Damiano SR, Wertheim EH, Paxton SJ. Media exposure in very young girls: Prospective and cross-sectional relationships with BMIz, self-esteem and body size stereotypes. Developmental psychology. 2017;53(12):2356. [DOI] [PubMed] [Google Scholar]
- 98.Pont SJ, Puhl R, Cook SR, Slusser W. Stigma Experienced by Children and Adolescents With Obesity. Pediatrics. 2017:e20173034. [DOI] [PubMed] [Google Scholar]
- 99.Latner JD, Rosewall JK, Simmonds MB. Childhood obesity stigma: association with television, videogame, and magazine exposure. Body image. 2007;4(2): 147–55. [DOI] [PubMed] [Google Scholar]


