Abstract
Background & Aims
Fecal urgency is a common symptom among patients with gastrointestinal disorders, but can also occur in healthy individuals with normal bowel habits. There have been few studies of fecal urgency in the general population. We performed a cross-sectional analysis of data from the National Health and Nurition Examination Survey (NHANES) to analyze the prevalence of and risk factors for this symptom.
Methods
We analyzed data from 4,676 persons who completed the Bowel Health Questionnaire from the NHANES, from 2009 through 2010. The NHANES sampled a nationally representative group of adults in the United States and provides information on demographics, medical comorbidities, and dietary habits of survey participants. The Bowel Health Questionnaire provided additional information about bowel symptoms such as urgency, incontinence, constipation, and diarrhea. We identified individuals with fecal urgency and calculated differences in fecal urgency among subgroups using χ2 analysis. We used logistic regression to identify factors associated with urgency.
Results
In our study population, the prevalence of fecal urgency was 3.3%; 29.5% of individuals with fecal urgency had diarrhea. The prevalence of fecal urgency was significantly higher in individuals who had diarrhea (14.8%) than in individuals without diarrhea (3.1%). Older age, female sex, poverty, urinary urge incontinence, diarrhea, and increased stool frequency were all associated with fecal urgency on multivariable analysis. Decreased fiber intake and increased carbohydrate intake were associated with urgency among individuals with diarrhea.
Conclusions
In an analysis of data from 4676 individuals who completed a Bowel Health Questionnaire from the NHANES, we found a significantly higher proportion of individuals with diarrhea to have fecal urgency. However, most individuals with fecal urgency do not have diarrhea. Factors associated with fecal urgency vary among individuals with and without diarrhea.
Keywords: Irritable bowel syndrome, stool form, dietary factors, Unied States population
INTRODUCTION
Fecal urgency is a common and at times debilitating symptom of gastrointestinal conditions like Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease.1–3 It is also common among individuals with diabetes,4 pelvic floor dysfunction,5 and a history of pelvic or rectal radiotherapy.6 Fecal urgency is known to be one of the strongest factors associated with the development of fecal incontinence,7–11 and has been cited as one of the two most bothersome symptoms in patients with IBS (along with abdominal pain),1,12 and the most bothersome symptom in patients with diarrhea predominant IBS.13 Estimates of its prevalence vary based on the population studied, ranging from 11% – 18%14–16 in healthy individuals to 65% in patients with bowel dysfunction.16 However, there are no available nationally-representative, population-based estimates of this common symptom.
Although diarrhea is strongly associated with fecal urgency, many individuals with fecal urgency report no history of diarrhea or loose stools, and some even report constipation. Talley et al. reported that 11.6% of community individuals with normal bowel habits reported fecal urgency.14 Similarly, Heaton et al noted that IBS patients reported urgency with 35.1% of Bristol Stool Form Score (BSFS) type 4 stools.16 While specific estimates of urgency in constipated patients are lacking, Heaton et al did note urgency with 32.8% of BSFS type 2 stools among IBS patients.16
In this study, we performed a population-based study to better understand the prevalence, risk factors, and medical comorbidities associated with fecal urgency using a representative, national database. Our aims were to quantitatively describe the population of individuals with this understudied symptom, and to identify modifiable risk factors for this symptom in individuals with and without underlying diarrhea.
Methods
Study cohort
The National Health and Nutrition Examination Survey (NHANES) is a survey research program that is designed to analyze a nationally representative sample of non-institutionalized respondents in the United States. NHANES is conducted by the National Center for Health Statistics of the Centers for Disease Control (Atlanta, GA, USA). All participants provide written informed consent before completing the NHANES, and there are no patient identifiers in the publicly available NHANES database. Participants are selected using a stratified multistage probability design with oversampling of certain age and ethnic groups. Sample weights in NHANES allow inferences to the population of the United States, based on independent population estimates from the US Census Bureau. These sample weights are used to adjust the sample population based on race, Hispanic ethnicity, income, sex, and age, and are meant to compensate for differences in subject selection or response rates at various stages of the survey. Weighting was performed prior to univariable and multivariable analysis to adjust for sample frame.
Data from adult participants (age ≥20 years) in NHANES 2009–2010 who completed the specific bowel health question “During the past 12 months, how often have you had an urgent need to empty your bowels that makes you rush to the toilet?” were included in the study. Individuals answering “always” or “most of the time” were classified as having fecal urgency, while individuals answering “sometimes,” “rarely,” or “never” were classified as not having this symptom. Patients who had reported taking laxatives within the past 30 days were excluded from analysis (Supplemental Figure 1).
Bowel health questionnaire
As part of the bowel health questionnaire from the NHANES 2009–2010, individuals completed a series of questions in the Mobile Examination Center Interview Room using a Computer-Assisted Personal Interview System. Stool consistency was assessed using the BSFS (color picture card with pictures and written descriptors of the 7 stool types) and the following written question: “Please look at this card and tell me the number that corresponds to your usual or most common stool type.” Patients reporting BSFS type 6 or 7 stools were defined as having diarrhea. Fecal incontinence was assessed by asking: “How often during the past 30 days have you had any amount of accidental bowel leakage that consisted of mucus/liquid stool/solid stool?” Individuals answering “never” to all three questions were defined as not having fecal incontinence. Like Whitehead et al,8 we did not include accidental leakage of gas in the definition of fecal incontinence. The Bowel Health questionnaire was administered in 2005–2006 and 2007–2008 as well, but only the 2009–2010 iteration posed the above question regarding fecal urgency.
Co-variables
The following co-variables not included in the bowel health questionnaire were also included to evaluate factors potentially associated with fecal urgency: age, sex, race/ethnicity, education, poverty income ratio, self-rated health, self-reported medical comorbidities, body mass index (BMI), urinary urge incontinence, self-reported depression, and dietary intake. Race and ethnicity were recorded into the following classifications: Non-Hispanic White, Non-Hispanic Black, Hispanic (including Mexican American), and other race (including multi-racial). Education was divided into three levels: less than high school, high school, and more than high school levels. Poverty income ratio was categorized into two groups: ≤2 times the poverty threshold and >2 times the poverty threshold. Three BMI groups were assessed: normal weight (<25.0 kg/m2), overweight (25.0 to 29.9 kg/m2), and obese (≥30 kg/m2).
Patients who answered “Yes” to the question “During the past 12 months, have you leaked or lost control of even a small amount of urine with an urge or pressure to urinate and couldn’t get to the toilet fast enough?” were defined as having urinary urge incontinence. Dietary fiber, liquid, caffeine, milk total sugar, and carbohydrate intake were obtained from the first day of the 24-hour dietary recall from the NHANES 2009–2010. The distributions of all these dietary variables were divided into quartiles. Individuals who reported feeling “down, depressed or hopeless” more than half of the days over the prior 2 weeks were classified as being depressed.
Statistical analyses
We first identified individuals with fecal urgency, and summarized their background characteristics. Differences between proportions of fecal urgency in various subgroups were calculated and tested using chi-square analysis. We used logistic regression to identify factors associated with urgency. All of the variables of interest were then included in a single logistic model to provide mutually adjusted estimates of the prevalence odds ratio (POR) for urgency prevalence. Adjusted POR having a 95% confidence interval (CI) not including unity were considered statistically significant.
All estimates, standard errors, and association measures were calculated using sampling weights accounting for the complex survey design of NHANES. A Taylor linearization approach was used to calculate 95% CIs for the estimated occurrence. All statistical analyses were performed using STATA statistical software version 14.2 (College Station, TX, USA).
Results
Univariable Analysis of all individuals
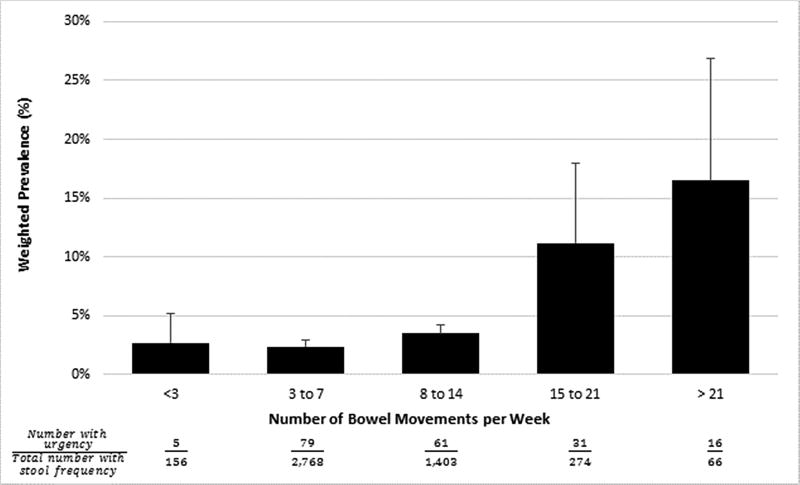
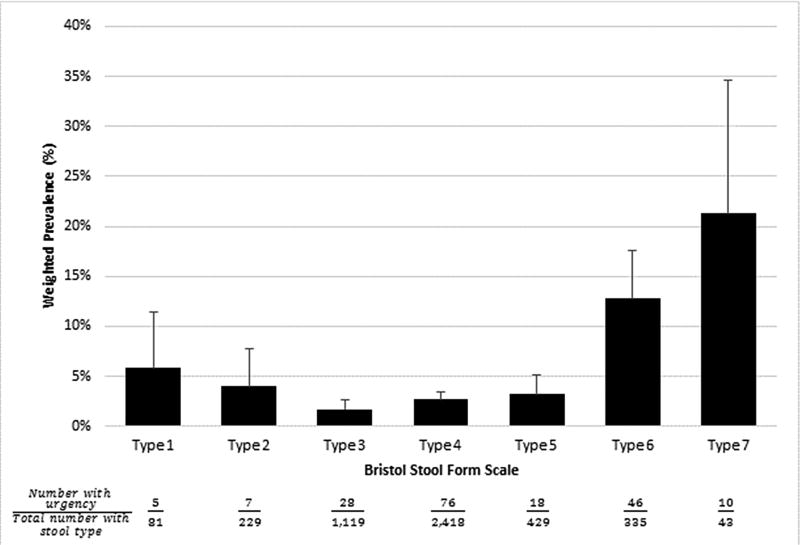
A total of 192 out of 4,676 individuals (3.3% adjusted) were classified as having fecal urgency. These individuals had a significantly higher prevalence of diarrhea (defined as BSFS stool type 6 or 7) compared to those without urgency (29.5% vs 7.2%, p < 0.001, Fisher’s exact test). On univariable analysis, the weighted prevalence of fecal urgency was over twice as high in women as compared to men (4.5% vs 2.1%, p = 0.001; Table 1). Increasing age was significantly associated with presence of fecal urgency, and there were significant differences in prevalence by race (Table 1). The weighted prevalence of fecal urgency increased in stepwise fashion with increase in stool frequency and form (Figure 1 and Figure 2). Stool frequency and BSFS stool type 6 or 7 were significant predictors of fecal urgency among both male and female patients (Supplemental tables 1 and 2). Patients reporting fecal incontinence were significantly more likely to report fecal urgency than those without this symptom (9.5% vs 2.7%, p < 0.0001).
Table 1.
Univariable Analysis of Demographic Factors Associated with Urgent Need to Empty the Bowel. NHANES 2009–2010.
| Sample | Weighted Sample | ||||
|---|---|---|---|---|---|
| N (%) | % | 95% CI | P-value | ||
| Overall Urgent Need Prevalence | 192 (4.1) | 3.3% | 2.9% – 3.7% | ||
| Gender (4,676) | 0.001 | ||||
| Male (2,374) | 65 (2.7) | 2.1% | 1.5% – 2.6% | ||
| Female (2,302) | 127 (5.5) | 4.5% | 3.5% – 5.5% | ||
| Age (years) (4,676) | |||||
| 20–29 (862) | 19 (2.2) | 1.8% | 0.8% – 2.7% | 0.0029 | |
| 30–39 (773) | 23 (3.0) | 2.8% | 1.3% – 4.4% | ||
| 40–49 (869) | 27 (3.1) | 2.7% | 1.2% – 4.3% | ||
| 50–59 (751) | 39 (5.2) | 3.0% | 2.1% – 3.9% | ||
| 60–69 (735) | 42 (5.7) | 5.5% | 3.6% – 7.5% | ||
| 70+ (686) | 41 (6.1) | 6.1% | 4.1% – 8.1% | ||
| Race/Ethnicity (4,676) | 0.0113 | ||||
| White (2,285) | 78 (3.4) | 2.9% | 2.1% – 3.7% | ||
| Black (807) | 44 (5.5) | 5.6% | 4.4% – 6.7% | ||
| Hispanics (1,345) | 59 (4.4) | 3.4% | 2.4% – 4.3% | ||
| Other-including multi-racial (239) | 11 (4.6) | 3.5% | 1.9% – 5.1% | ||
| Education (4,676) | 0.0013 | ||||
| < High school (1,276) | 74 (5.8) | 5.6% | 4.1% – 7.0% | ||
| High school or GED (1,093) | 40 (3.7) | 3.2% | 2.4% – 4.1% | ||
| > High school (2,307) | 78 (3.4) | 2.6% | 2.0% – 3.3% | ||
| Family Poverty Income Ratio (4,281) | 0.0008 | ||||
| <2 (2,090) | 107 (5.1) | 5.0% | 3.9% – 6.1% | ||
| ≥2 (2,191) | 67 (3.1) | 2.5% | 1.9% – 3.0% | ||
| Self-rated health (4,676) | 0.0001 | ||||
| Excellent/Very good/Good (3,549) | 112 (3.2) | 2.6% | 2.2% – 3.1% | ||
| Fair/Poor (1,127) | 80 (7.1) | 6.6% | 4.7% – 8.4% | ||
| Comorbidities | |||||
| Cancer (441) | 31 (7.0) | 6.4% | 3.6% – 9.1% | 0.0078 | |
| Thyroid problem (423) | 30 (7.1) | 4.6% | 3.3% – 6.0% | 0.0179 | |
| Anemia (194) | 14 (7.2) | 6.4% | 1.2% – 11.5% | 0.0807 | |
| Inflammatory bowel disease (48) | 6 (12.5) | 10.7% | 0.2% – 21.3% | 0.0081 | |
| Diabetes (521) | 40 (7.7) | 7.1% | 4.8% – 9.4% | 0.0009 | |
| Liver condition (69) | 6 (8.7) | 7.7% | −0.5% – 15.8% | 0.1146 | |
| BMI (4,647) | 0.0265 | ||||
| Normal (1,315) | 35 (2.7) | 2.1% | 1.1% – 3.1% | ||
| Overweight (1,555) | 62 (4.0) | 3.0% | 2.4% – 3.7% | ||
| Obese (1,777) | 91 (5.1) | 4.3% | 3.4% – 5.2% | ||
| Urinary urge incontinence (4,672) | <0.0001 | ||||
| Yes (1,008) | 87 (8.6) | 8.4% | 6.5% – 10.4% | ||
| No (3,664) | 104 (2.8) | 2.2% | 1.8% – 2.5% | ||
| Feeling down, depressed, hopeless (4,674) | <0.0001 | ||||
| Not at all/several days (4,307) | 150 (3.5) | 2.8% | 2.5% – 3.2% | ||
| More than half the days/Nearly everyday (367) | 40 (10.9) | 10.5% | 5.9% – 15.2% | ||
| Self-report Constipation (always/most of the time) (4,674) | 0.0562 | ||||
| Yes (166) | 13 (7.8) | 5.6% | 2.4% – 8.9% | ||
| No (4,508) | 178 (4.0) | 3.2% | 2.8% – 3.6% | ||
| Self-report diarrhea (always/most of the time) (4,674) | <0.0001 | ||||
| Yes (81) | 30 (37.0) | 33.6% | 16.8% – 50.4% | ||
| No (4,593) | 162 (3.5) | 2.9% | 2.6% – 3.2% | ||
| Fecal Incontinence (4,669) | <0.0001 | ||||
| Yes (434) | 61 (14.1) | 9.5% | 5.9% – 13.2% | ||
| No (4 23 5) | 131 (3 1) | 2.7% | 2.3% – 3.2% | ||
Figure 1.
Weighted prevalence of Urgent Need to Empty the Bowel According to Bowel Movements per week from NHANES 2009–2010.
Figure 2.
Weighted prevalence of Urgent Need to Empty the Bowel According to Bristol Stool Form Scale from NHANES 2009–2010.
Other factors associated with the presence of fecal urgency on univariable analysis were lower education levels, poverty, poor self-rated health, and higher BMI (Table 1). Patients reporting urinary urge incontinence were significantly more likely to report fecal urgency than those not reporting this symptom (8.4% vs 2.2%, p < 0.0001). Individuals who reported depression, hopelessness, or feeling down for more than half of the days were more likely to have fecal urgency than those with less frequent depression symptoms (10.5% vs 2.8%, p < 0.0001). Decreased alcohol intake was associated with increased prevalence of urgency, but no other dietary factors were associated on univariable analysis (Table 2).
Table 2.
Univariable Analysis of Dietary Factors Associated with Urgent Need to Empty the Bowel. NHANES 2009–2010.
| Sample | Weighted Sample | ||||
|---|---|---|---|---|---|
| N (%) | % | 95% CI | P-value | ||
| Overall Urgent Need Prevalence | 192 (4.1) | 3.3% | 2.9% – 3.7% | ||
| Alcohol intake (4,674) | 0.0294 | ||||
| Never drink (1,086) | 74 (6.8) | 5.6% | 3.9% – 7.3% | ||
| Former drinker (310) | 13 (4.2) | 3.1% | 0.9% – 5.4% | ||
| Rare drinker (1,552) | 57 (3.7) | 3.0% | 2.0% – 4.0% | ||
| Light drinker (989) | 29 (2.9) | 2.6% | 1.1% – 4.1% | ||
| Moderate drinker (360) | 10 (2.8) | 2.9% | 1.3% – 4.4% | ||
| Heavy drinker (377) | 9 (2.4) | 1.8% | 0.0% – 3.6% | ||
| Caffeine intake (4,621) | 0.9686 | ||||
| Lowest (<137 mg) (2,670) | 111 (4.2) | 3.3% | 2.5% – 4.1% | ||
| Mid (137–411 mg) (1,544) | 64 (4.2) | 3.3% | 2.3% – 4.3% | ||
| Highest (>411 mg) (407) | 15 (3.7) | 3.1% | 0.9% – 5.2% | ||
| Dietary Milk Intake (4,671) | 0.5179 | ||||
| Never (752) | 34 (4.5) | 3.8% | 2.3% – 5.3% | ||
| Rarely (less than once a week) (698) | 24 (3.4) | 2.5% | 1.1% – 4.0% | ||
| Sometimes (once a week or more, but less than once a week (1,331) | 51 (3.8) | 3.2% | 2.3% – 4.2% | ||
| Often (once a day or more) (1,890) | 83 (4.4) | 3.4% | 2.9% – 3.9% | ||
| Dietary Fiber Intake (4,621) | 0.0583 | ||||
| Lowest Quartile (<10.1 gm) (1,254) | 52 (4.1) | 3.1% | 2.3% – 3.9% | ||
| Middle Lower Quartile (10.1–14.5 gm) (1,022) | 51 (5.0) | 4.6% | 3.1% – 6.2% | ||
| Middle Upper Quartile (14.5–20.1 gm) (1,016) | 43 (4.2) | 3.3% | 2.0% – 4.6% | ||
| Highest Quartile (>20.1) (1,329) | 44 (3.3) | 2.4% | 1.8% – 3.1% | ||
| Dietary Liquid Intake (4,621) | 0.1816 | ||||
| Lowest Quartile (<1881.9 gm) (1,154) | 54 (4.7) | 4.7% | 2.5% – 6.9% | ||
| Middle Lower Quartile (1881.9–2498.5 gm) (934) | 48 (5.1) | 3.2% | 2.2% – 4.1% | ||
| Middle Upper Quartile (2498.5–3319.0 gm) (1,108) | 42 (3.8) | 3.2% | 1.7% – 4.6% | ||
| Highest Quartile (>3319.0 gm) (1,425) | 46 (3.2) | 2.6% | 2.0% – 3.2% | ||
| Dietary Total Sugar Intake (gm) (4,621) | 0.6037 | ||||
| Lowest Quartile (1,373) | 53 (3.9) | 3.1% | 2.1% – 4.2% | ||
| Middle Lower Quartile (1,056) | 43 (4.1) | 3.1% | 2.2% – 4.1% | ||
| Middle Upper Quartile (1,067) | 46 (4.3) | 2.9% | 1.8% – 4.1% | ||
| Highest Quartile (1,125) | 48 (4.3) | 3.9% | 2.5% – 5.3% | ||
| Dietary Carbohydrates Intake (gm) (4,621) | 0.3406 | ||||
| Lowest Quartile (1,001) | 43 (4.3) | 3.3% | 2.1% – 4.5% | ||
| Middle Lower Quartile (1,135) | 52 (4.6) | 3.7% | 2.4% – 5.0% | ||
| Middle Upper Quartile (1,207) | 40 (3.3) | 2.4% | 1.4% – 3.4% | ||
| Highest Quartile (1,278) | 55 (4.3) | 3.7% | 2.6% – 4.9% | ||
| Dietary Total Protein Intake (gm) (4,621) | 0.3989 | ||||
| Lowest Quartile (770) | 35 (4.5) | 3.6% | 1.9% – 5.3% | ||
| Middle Lower Quartile (1,028) | 38 (3.7) | 2.8% | 1.7% – 3.9% | ||
| Middle Upper Quartile (1,311) | 64 (4.9) | 4.0% | 2.8% – 5.1% | ||
| Highest Quartile (1,512) | 53 (3.5) | 2.9% | 2.0% – 3.8% | ||
| Dietary Total Fat Intake (gm) (4,621) | 0.1299 | ||||
| Lowest Quartile (1,021) | 49 (4.8) | 4.4% | 2.8% – 5.9% | ||
| Middle Lower Quartile (1,047) | 48 (4.6) | 3.3% | 2.3% – 4.4% | ||
| Middle Upper Quartile (1,193) | 41 (3.4) | 2.4% | 1.6% – 3.2% | ||
| Highest Quartile (1,360) | 52 (3.8) | 3.3% | 2.4% – 4.2% | ||
Multivariable Analysis of all individuals
On multivariable analysis, (Table 3) increased age (prevalence odds ratio (POR) 1.17 for each additional decade of age, p = 0.003), female gender (POR 2.09, p = 0.007), living below two times the poverty level (POR 0.64 for living above two times poverty level, p = 0.029), presence of urinary urge incontinence (POR 2.34, p < 0.0001), diarrhea (POR 3.45, p < 0.0001), and increased stool frequency (AOR 1.08 for each additional stool per week, p < 0.0001) all remained as predictors of fecal urgency. None of the dietary factors were associated with fecal urgency on multivariate analysis of all patients.
Table 3.
POR for Factors Associated with Urgent Need to Empty the Bowels among the U.S. Population from NHANES 2009–2010.
| Variables | POR | [95% Conf. Interval] | P-value | |
|---|---|---|---|---|
| Age (decade) | 1.17 | 1.06 | 1.28 | 0.003 |
| Female gender | 2.09 | 1.26 | 3.49 | 0.007 |
| Ethnicity | ||||
| Caucasian | 0.77 | 0.45 | 1.32 | 0.321 |
| African American | 1.11 | 0.57 | 2.14 | 0.749 |
| Hispanics | 0.66 | 0.37 | 1.17 | 0.145 |
| Higher education | 1.10 | 0.73 | 1.66 | 0.642 |
| Living above 2× poverty income | 0.64 | 0.43 | 0.95 | 0.029 |
| Obese BMI | 1.04 | 0.61 | 1.80 | 0.869 |
| Feeling down, depressed, hopeless | 1.73 | 0.92 | 3.25 | 0.083 |
| Self-rated health (fair/poor) | 1.43 | 0.93 | 2.19 | 0.098 |
| Urinary Urge incontinence | 2.34 | 1.72 | 3.18 | <0.0001 |
| Heavy/moderate alcohol drinker | 0.96 | 0.51 | 1.80 | 0.890 |
| High caffeine intake | 1.19 | 0.41 | 3.46 | 0.728 |
| Frequent milk drinker | 1.07 | 0.71 | 1.62 | 0.720 |
| Highest quartile Fiber intake | 0.69 | 0.38 | 1.24 | 0.195 |
| Highest quartile Liquid intake | 0.85 | 0.52 | 1.40 | 0.505 |
| Highest quartile Carbohydrates intake | 1.29 | 0.63 | 2.64 | 0.460 |
| Highest quartile Sugar intake | 1.30 | 0.68 | 2.49 | 0.410 |
| Highest quartile Protein intake | 0.93 | 0.48 | 1.80 | 0.823 |
| Highest quartile Fat intake | 1.29 | 0.78 | 2.13 | 0.297 |
| Diarrhea BSFS 6 & 7 | 3.45 | 1.96 | 6.06 | <0.0001 |
| Stool Frequency (continuous) | 1.08 | 1.04 | 1.12 | <0.0001 |
| Fecal Incontinence | 1.41 | 0.64 | 3.13 | 0.369 |
Multivariable Analysis of individuals based on presence or absence of diarrhea
Multivariable analysis was used to evaluate individuals with and without diarrhea separately. Individuals with and without diarrhea were similar with regards to all demographic and dietary parameters (results not shown). 56 out of 378 (14.8%) individuals with diarrhea reported fecal urgency. Increased age (POR 1.35 for each additional decade, p = 0.043) and stool frequency (POR 1.13 for each additional increase in stool per week, p < 0.001) remained strongly associated with fecal urgency among individuals with diarrhea. Being in the highest quartile of carbohydrate intake was also associated with fecal urgency among individuals with diarrhea (POR 6.68, p = 0.006), while being in the highest quartile of fiber intake was negatively associated (POR 0.13, p = 0.002) (Table 4).
Table 4.
POR for Factors Associated with Urgent Need to Empty the Bowels among Diarrhea (BSFS 6 or 7) and Non-Diarrhea in the U.S. Population from NHANES 2009–2010.
| Diarrhea (n = 378) | Non-Diarrhea (n = 4,276) | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | POR | [95% Conf. Interval] |
P- value |
POR | [95% Conf. Interval] |
P- value |
||
| Age (continuous) | 1.35 | 1.01 | 1.79 | 0.043 | 1.15 | 1.05 | 1.27 | 0.005 |
| Female gender | 2.22 | 0.51 | 9.55 | 0.265 | 2.14 | 1.30 | 3.52 | 0.005 |
| Ethnicity | ||||||||
| Caucasian | 2.68 | 0.51 | 14.04 | 0.225 | 0.57 | 0.33 | 1.00 | 0.052 |
| African American | 2.62 | 0.41 | 16.99 | 0.290 | 1.01 | 0.49 | 2.08 | 0.977 |
| Hispanics | 1.14 | 0.20 | 6.68 | 0.876 | 0.60 | 0.30 | 1.22 | 0.148 |
| Higher education | 0.97 | 0.33 | 2.87 | 0.947 | 1.21 | 0.69 | 2.12 | 0.489 |
| Living above 2× poverty income | 0.70 | 0.30 | 1.62 | 0.381 | 0.54 | 0.38 | 0.78 | 0.002 |
| Obese BMI | 1.01 | 0.44 | 2.35 | 0.977 | 0.99 | 0.60 | 1.65 | 0.979 |
| Feeling down, depressed, hopeless | 1.05 | 0.41 | 2.71 | 0.912 | 2.11 | 1.11 | 4.02 | 0.026 |
| Self-rated health (fair/poor) | 2.07 | 0.81 | 5.31 | 0.121 | 1.27 | 0.71 | 2.26 | 0.402 |
| Urinary Urge incontinence | 2.78 | 0.86 | 9.02 | 0.084 | 2.35 | 1.74 | 3.19 | <0.0001 |
| Heavy/moderate alcohol drinker | 0.83 | 0.19 | 3.71 | 0.795 | 0.96 | 0.42 | 2.21 | 0.916 |
| High caffeine intake | 0.39 | 0.08 | 1.91 | 0.229 | 1.48 | 0.48 | 4.55 | 0.474 |
| Frequent milk drinker | 2.04 | 0.72 | 5.73 | 0.164 | 0.92 | 0.58 | 1.46 | 0.722 |
| Highest quartile Fiber intake | 0.13 | 0.04 | 0.43 | 0.002 | 0.96 | 0.49 | 1.89 | 0.908 |
| Highest quartile Liquid intake | 1.43 | 0.47 | 4.32 | 0.501 | 0.88 | 0.50 | 1.56 | 0.640 |
| Highest quartile Carbohydrates intake | 6.68 | 1.85 | 24.07 | 0.006 | 0.81 | 0.36 | 1.79 | 0.577 |
| Highest quartile Sugar intake | 0.75 | 0.21 | 2.62 | 0.630 | 1.57 | 0.76 | 3.23 | 0.202 |
| Highest quartile Protein intake | 1.23 | 0.33 | 4.55 | 0.742 | 0.96 | 0.53 | 1.77 | 0.902 |
| Highest quartile Fat intake | 0.57 | 0.23 | 1.42 | 0.208 | 1.52 | 0.95 | 2.42 | 0.076 |
| Stool Frequency (continuous) | 1.13 | 1.07 | 1.18 | <0.0001 | 1.07 | 1.02 | 1.12 | 0.007 |
| Fecal Incontinence | 0.97 | 0.32 | 2.92 | 0.956 | 1.73 | 0.76 | 3.94 | 0.178 |
134 out of 4,276 (3.1%) individuals without diarrhea reported fecal urgency. Increased age (POR 1.15 for each additional decade, p = 0.005), female gender (POR 2.14, p = 0.005), presence of urinary urge incontinence (POR 2.35, p < 0.001), increased stool frequency (POR 1.07 for each additional stool per week, p = 0.007), and feeling down/depressed/hopeless (POR 2.11, p = 0.026) were all associated with fecal urgency in individuals without diarrhea, while living above two times the poverty level carried a negative association (POR 0.54, p = 0.002) (Table 3).
Discussion
In our study, we observed that fecal urgency was present in 3.3% of a representative sample of the general US population. Fecal urgency was more common in women and older individuals, and among individuals with diarrhea. While there was greater prevalence of fecal urgency in individuals with diarrhea, the overall majority with fecal urgency did not have diarrhea, and their most common reported stool type was BSFS type 4. We observed different predictors of fecal urgency in individuals with and without diarrhea.
Only a limited number of studies have estimated the prevalence of fecal urgency. In the only other population based study, which surveyed 1644 predominantly white individuals living in Rochester MN, Talley et al. reported a prevalence of 18%.14 In a study of younger individuals (mean age of 24.7, 64.5% of whom were female), Drossman et al cited a prevalence of 14.4%.15 In another study of younger individuals (age ranging from 20–44 years, all of whom were female), Heaton et al reported fecal urgency rates of 65% in patients being followed in gastroenterology clinic for IBS, 26% in individuals with IBS-type symptoms not reported to a physician, and 11% in individuals with no abdominal pain symptoms.16
The difference in the cited prevalence of urgency in these prior studies compared to ours is likely due to differences in sample populations, and in how restrictively the relevant survey question was worded. The studies of Talley et al and Heaton et al both reported the proportion of individuals reporting a sensation of urgency more than 25% of the time.14,16 Drossman et al. asked individuals “Do you frequently have an urgent need to go to the bathroom to have a bowel movement?”15 In this study, NHANES survey participants were asked to specify whether urgent bowel movements occurred “always” or “most of the time,” and were also specifically asked about symptoms over the past 12 months. We followed this more restrictive approach in order to study patients with the most bothersome symptoms of fecal urgency. We observed a stepwise increase in the prevalence of diarrhea among patients with increasing reported frequency of fecal urgency (Supplemental Figure 2).
Among individuals with diarrhea, multivariable analysis demonstrated that those in the highest quartile for fiber intake were 83% less likely to report fecal urgency compared to those with lower fiber intake. Those in the highest quartile for carbohydrate intake were over five times more likely to report fecal urgency compared to those with lower carbohydrate intake. There was no association between dietary factors and fecal urgency in individuals without diarrhea on multivariable analysis. Increased fiber is often used in clinical practice to treat fecal urgency and incontinence by improving stool consistency and reducing the frequency of liquid stools.17,18 A low carbohydrate intake (particularly, low in Fermentable, Oligosaccharides, Disaccharides, and Monosaccharides and Polyols – i.e. FODMAPs) has also been shown to decrease stool frequency and improve stool consistency among those with underlying IBS and/or Fructose malabsorption.19,20 We examined dietary factors in order to identify modifiable risk factors for fecal urgency. Our findings suggest that increasing fiber intake and decreasing carbohydrate intake are useful therapeutic adjuncts in treating this symptom in individuals with diarrhea, but are less likely to benefit individuals without diarrhea. A potential area of future study would be to analyze dietary patterns (rather than specific dietary factors) associated with fecal urgency.
The majority of patients with urgency did not have diarrhea (~70%), consistent with Drossman’s findings.15 Older age, female sex, poverty, and presence of urinary urge incontinence remained significantly associated with fecal urgency on multivariable analysis of these patients. Older age and urinary urge incontinence trended towards being predictors of urgency in individuals with diarrhea as well (the lack of statistical significance was likely due to the smaller number of individuals with diarrhea). The presence of depression was a predictor of fecal urgency in individuals without diarrhea, but did not demonstrate a trend towards being a predictor of fecal urgency among those without diarrhea. Despite the previously noted association between fecal urgency and fecal incontinence (confirmed on univariable analysis in this study), fecal incontinence was not an independent predictor of fecal urgency on multivariable analysis. This suggests that both fecal urgency and fecal incontinence are driven by common factors already controlled for on multivariable analysis. Indeed, fecal incontinence was a significant predictor of fecal urgency on multivariable analysis when age, stool frequency, and stool consistency were removed from the regression model reported in table 3 (data not shown).
The mechanism of association between urinary urge incontinence and fecal urgency is not entirely clear. Previous research has reported an association between fecal incontinence and urinary incontinence,21 and fecal urgency is also a frequent symptom among patients followed in urogynecology clinic for pelvic floor disorders.22 While pelvic organ prolapse can be associated with urinary incontinence and various defecatory symptoms that include urgency,23 urinary urge incontinence was a significant predictor of fecal urgency in male but not in female patients in this study (Supplemental Tables 1 and 2). This argues against pelvic organ prolapse as the common driver of fecal urgency and urinary incontinence in our study population. A more likely driver of combined urinary and bowel symptoms is visceral hypersensitivity, which is a known contributor to both IBS24 and fecal urgency.25 Visceral hypersensitivity may also lead to bladder complaints due to shared peripheral innervation and central nervous system processing of the anorectum and bladder.26
Depression was also associated with fecal urgency in patients without diarrhea. This is a novel finding and aligns with prior studies indicating that psychological factors can alter rectal perception and sensory thresholds,27–29 and modulate visceral sensation.30 Our finding that depression was associated with urgency only among patients without diarrhea also argues against the association between fecal urgency and depression being due to reverse causality (with urgency contributing to depression through its effect on individuals’ day-to-day quality of life), or to increased reporting of urgency in individuals with depression (possibly due to somatization or recall bias in depressed patients). Were this the case, the association between depression and urgency would be expected in the general patient population as well, and not simply in those without loose stools. Whether effective treatment of depression leads to improvement in fecal urgency symptoms in individuals without diarrhea is an important area of future investigation. We also noted an association between poverty and fecal urgency on multivariable analysis. This is a notable finding that suggests the need for further investigation on the effect of socioeconomic variables on bowel symptoms, particularly given that lower income indivduals are frequently underrepresented in clinical studies.
A major strength of this study is the utilization of survey data of a large population sample that was weighted to represent the general US population. Weaknesses of this study are related to the NHANES design, with all data being self-reported (and thus prone to recall bias), as well as the cross sectional nature of the NHANES, which precludes clear demonstration of causation. Our definition of fecal urgency (classified as those with urgency “always” or “most of the time”) has also not been previously validated, although it did show good correlation with diarrhea. Additionally, the answer format was different for various questions in the survey (yes/no versus frequency scale), potentially complicating analysis of associations between variables. Finally, the presence of diarrhea was defined on the basis of an individual’s “usual or most common stool type,” which may not be a complete reflection of a particular individual’s underlying bowel habits.
In summary, in the first population based study of its kind, we demonstrated a 3.3% weighted prevalence of fecal urgency in a representative sample of US adults, and that the majority of individuals with fecal urgency do not have diarrhea. After adjusting for covariates, we demonstrated that among individuals with baseline diarrhea, increased carbohydrate intake and decreased fiber intake were unique predictors of fecal urgency, while depression and urinary urge incontinence were unique predictors among patients without diarrhea.
Supplementary Material
Supplemental Figure 1: Flow Diagram of Study Participants
Supplemental Figure 2: Non-weighted Prevalence of Diarrhea According to Self-Reported Frequency of Fecal Urgency
Supplemental Table 1. POR for Factors Associated with Urgent Need to Empty the Bowels among the U.S. Female Population from NHANES 2009–2010.
Supplemental Table 2. POR for Factors Associated with Urgent Need to Empty the Bowels among the U.S. Male Population from NHANES 2009–2010.
Acknowledgments
Grant Support: Research reported in this publication was supported by the National Institutes of Health under award number R01AT00857303 and T32DK007760
Abbreviations
- AOR
Adjusted Odds Ratio
- BSFS
Bristol Stool Form Score
- BMI
Body Mass Index
- CI
Confidence Interval
- IBS
Irritable Bowel Syndrome
- NHANES
National Health and Nutrition Examination Survey
- POR
Prevalence Odds Ratio
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: None of the authors have any conflicts of interest to disclose
Writing assistance: None
Author Contributions: VR: analysis and interpretation of data, drafting of the manuscript; SM: analysis and interpretation of data, statistical analysis; PS: analysis and interpretation of data, critical revision of the manuscript for important intellectual content; SB: analysis and interpretation of data, critical revision of the manuscript for important intellectual content; WH: critical revision of the manuscript for important intellectual content; TS: critical revision of the manuscript for important intellectual content; JN: critical revision of the manuscript for important intellectual content, JI: critical revision of the manuscript for important intellectual content, AL: study concept and design, critical revision of the manuscript for important intellectual content, study supervision.
References
- 1.Mangel AW, Wang J, Sherrill B, et al. Urgency as an Endpoint in Irritable Bowel Syndrome. Gastroenterology Res. 2011;4(1):9–12. doi: 10.4021/gr283e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harding JP, Hamm LR, Ehsanullah RS, et al. Use of a novel electronic data collection system in multicenter studies of irritable bowel syndrome. Aliment Pharmacol Ther. 1997;11(6):1073–6. doi: 10.1046/j.1365-2036.1997.00256.x. [DOI] [PubMed] [Google Scholar]
- 3.Mangel AW, Northcutt AR. Review article: the safety and efficacy of alosetron, a 5-HT3 receptor antagonist, in female irritable bowel syndrome patients. Aliment Pharmacol Ther. 1999;13(Suppl 2):77– 82. doi: 10.1046/j.1365-2036.1999.00010.x. [DOI] [PubMed] [Google Scholar]
- 4.Ihana-Sugiyama N, Nagata N, Yamamoto-Honda R, et al. Constipation, hard stools, fecal urgency, and incomplete evacuation, but not diarrhea is associated with diabetes and its related factors. World J Gastroenterol. 2016;22(11):3252–60. doi: 10.3748/wjg.v22.i11.3252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bezerra LR, Vasconcelos Neto JA, Vasconcelos CT, et al. Prevalence of unreported bowel symptoms in women with pelvic floor dysfunction and the impact on their quality of life. Int Urogynecol J. 2014;25(7):927–33. doi: 10.1007/s00192-013-2317-2. [DOI] [PubMed] [Google Scholar]
- 6.Lundby L, Krogh K, Jensen VJ, et al. Long-term anorectal dysfunction after postoperative radiotherapy for rectal cancer. Dis Colon Rectum. 2005;48(7):1343–9. doi: 10.1007/s10350-005-0049-1. [DOI] [PubMed] [Google Scholar]
- 7.Bharucha AE, Dunivan G, Goode PS, et al. Epidemiology, pathophysiology, and classification of fecal incontinence: state of the science summary for the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) workshop. Am J Gastroenterol. 2015;110(1):127–36. doi: 10.1038/ajg.2014.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitehead WE, Borrud L, Goode PS, et al. Pelvic Floor Disorders Network. Fecal incontinence in US adults: epidemiology and risk factors. Gastroenterology. 2009;137(2):512–7. 517.e1–2. doi: 10.1053/j.gastro.2009.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bharucha AE, Fletcher JG, Melton LJ, 3rd, et al. Obstetric trauma, pelvic floor injury and fecal incontinence: a population-based case-control study. Am J Gastroenterol. 2012;107(6):902–11. doi: 10.1038/ajg.2012.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Simrén M, Palsson OS, Heymen S, et al. Fecal incontinence in irritable bowel syndrome: Prevalence and associated factors in Swedish and American patients. Neurogastroenterol Motil. 2017;29(2):e12919. doi: 10.1111/nmo.12919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Atarodi S, Rafieian S, Whorwell PJ. Faecal incontinence-the hidden scourge of irritable bowel syndrome: a cross-sectional study. BMJ Open Gastroenterol. 2015;1(1):e000002. doi: 10.1136/bmjgast-2014-000002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mangel AW, Northcutt AR. Review article: the safety and efficacy of alosetron, a 5-HT3 receptor antagonist, in female irritable bowel syndrome patients. Aliment Pharmacol Ther. 1999;13(Suppl 2):77– 82. doi: 10.1046/j.1365-2036.1999.00010.x. [DOI] [PubMed] [Google Scholar]
- 13.Chang L, Ameen VZ, Dukes GE, et al. A dose-ranging, phase II study of the efficacy and safety of alosetron in men with diarrhea-predominant IBS. Am J Gastroenterol. 2005;100(1):115–23. doi: 10.1111/j.1572-0241.2005.40365.x. [DOI] [PubMed] [Google Scholar]
- 14.Talley NJ, Weaver AL, Zinsmeister AR, et al. Self-reported diarrhea: what does it mean? Am J Gastroenterol. 1994;89(8):1160–4. [PubMed] [Google Scholar]
- 15.Drossman DA, Sandler RS, Broom CM, et al. Urgency and fecal soiling in people with bowel dysfunction. Dig Dis Sci. 1986;31(11):1221–5. doi: 10.1007/BF01296523. [DOI] [PubMed] [Google Scholar]
- 16.Heaton KW, Ghosh S, Braddon FE. How bad are the symptoms and bowel dysfunction of patients with the irritable bowel syndrome? A prospective, controlled study with emphasis on stool form. Gut. 1991;32(1):73–9. doi: 10.1136/gut.32.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Markland AD, Burgio KL, Whitehead WE, et al. Loperamide Versus Psyllium Fiber for Treatment of Fecal Incontinence: The Fecal Incontinence Prescription (Rx) Management (FIRM) Randomized Clinical Trial. Dis Colon Rectum. 2015;58(10):983–93. doi: 10.1097/DCR.0000000000000442. [DOI] [PubMed] [Google Scholar]
- 18.Bliss DZ, Jung HJ, Savik K, et al. Supplementation with dietary fiber improves fecal incontinence. Nurs Res. 2001;50(4):203–13. doi: 10.1097/00006199-200107000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Shepherd SJ, Gibson PR. Fructose malabsorption and symptoms of irritable bowel syndrome: guidelines for effective dietary management. J Am Diet Assoc. 2006;106(10):1631–9. doi: 10.1016/j.jada.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 20.Böhn L, Störsrud S, Liljebo T, et al. Diet low in FODMAPs reduces symptoms of irritable bowel syndrome as well as traditional dietary advice: a randomized controlled trial. Gastroenterology. 2015;149(6):1399–1407. doi: 10.1053/j.gastro.2015.07.054. [DOI] [PubMed] [Google Scholar]
- 21.Roberts RO, Jacobsen SJ, Reilly WT, et al. Prevalence of combined fecal and urinary incontinence: a community-based study. J Am Geriatr Soc. 1999;47(7):837–41. doi: 10.1111/j.1532-5415.1999.tb03841.x. [DOI] [PubMed] [Google Scholar]
- 22.Bezerra LR, Vasconcelos Neto JA, Vasconcelos CT, et al. Prevalence of unreported bowel symptoms in women with pelvic floor dysfunction and the impact on their quality of life. Int Urogynecol J. 2014;25(7):927–33. doi: 10.1007/s00192-013-2317-2. [DOI] [PubMed] [Google Scholar]
- 23.Jelovsek JE, Maher C, Barber MD. Pelvic organ prolapse. Lancet. 2007;369(9566):1027–38. doi: 10.1016/S0140-6736(07)60462-0. [DOI] [PubMed] [Google Scholar]
- 24.Kanazawa M, Hongo M, Fukudo S. Visceral hypersensitivity in irritable bowel syndrome. J Gastroenterol Hepatol. 2011;26(Suppl 3):119–21. doi: 10.1111/j.1440-1746.2011.06640.x. [DOI] [PubMed] [Google Scholar]
- 25.Grinsvall C, Törnblom H, Tack J, et al. Psychological factors selectively upregulate rectal pain perception in hypersensitive patients with irritable bowel syndrome. Neurogastroenterol Motil. 2015;27(12):1772–82. doi: 10.1111/nmo.12689. [DOI] [PubMed] [Google Scholar]
- 26.Kaplan SA, Dmochowski R, Cash BD, et al. Systematic review of the relationship between bladder and bowel function: implications for patient management. Int J Clin Pract. 2013;67(3):205–16. doi: 10.1111/ijcp.12028. [DOI] [PubMed] [Google Scholar]
- 27.Whitehead WE, Palsson OS. Is rectal pain sensitivity a biological marker for irritable bowel syndrome: psychological influences on pain perception. Gastroenterology. 1998;115(5):1263–71. doi: 10.1016/s0016-5085(98)70099-x. [DOI] [PubMed] [Google Scholar]
- 28.Posserud I, Syrous A, Lindström L, et al. Altered rectal perception in irritable bowel syndrome is associated with symptom severity. Gastroenterology. 2007;133(4):1113–23. doi: 10.1053/j.gastro.2007.07.024. [DOI] [PubMed] [Google Scholar]
- 29.Posserud I, Agerforz P, Ekman R, et al. Altered visceral perceptual and neuroendocrine response in patients with irritable bowel syndrome during mental stress. Gut. 2004;53(8):1102–8. doi: 10.1136/gut.2003.017962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elsenbruch S. Abdominal pain in Irritable Bowel Syndrome: a review of putative psychological, neural and neuro-immune mechanisms. Brain Behav Immun. 2011;25(3):386–94. doi: 10.1016/j.bbi.2010.11.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1: Flow Diagram of Study Participants
Supplemental Figure 2: Non-weighted Prevalence of Diarrhea According to Self-Reported Frequency of Fecal Urgency
Supplemental Table 1. POR for Factors Associated with Urgent Need to Empty the Bowels among the U.S. Female Population from NHANES 2009–2010.
Supplemental Table 2. POR for Factors Associated with Urgent Need to Empty the Bowels among the U.S. Male Population from NHANES 2009–2010.