Abstract
Several cognitive mechanisms have been proposed to account for the relationship between exposure to traumatic life events (TLEs) and the entire psychosis spectrum. However, only few of these mechanisms have been empirically tested and those that have been tested have not considered multiple mechanisms simultaneously. The purpose of this study was to examine whether perceived stress, dissociation, negative self-schemas, negative other-schemas, and/or external locus of control mediated the association between TLEs and psychotic-like experiences (PLEs). An undergraduate sample of 945 individuals completed a battery of self-report questionnaires. We found significant indirect effects from TLE exposure to PLEs through perceived stress, dissociation, external locus of control, negative self-schemas, and negative other-schemas. When controlling for comorbid psychological symptoms, only the indirect effect from TLE exposure to PLEs through dissociation continued to be significant. Targeting stress sensitivity, maladaptive schemas, dissociative tendencies, and externalizing attributional styles may prove useful in the amelioration of risk for various psychopathologies (e.g., mood, psychosis) in the aftermath of TLE exposure. Findings underscore the importance of targeting trauma-related cognitions in the prevention or reduction of psychotic-like experiences or disorders.
Keywords: psychotic-like experiences, trauma exposure, dissociation, negative schemas, stress sensitivity, locus of control
1. Introduction
Although genetic factors appear to be substantially related to the etiology of psychotic disorders, evidence suggests that the environment also influences the development and course of psychosis (Schlosser et al., 2012). Among the environmental contributors to psychotic disorders, traumatic life events (TLEs) have been consistently associated with the entire spectrum of psychosis outcomes, including risk and severity of psychotic disorders and psychotic-like experiences (PLEs), the latter which are considered attenuated (i.e., less frequent, severe, distressing or convincing) positive psychotic symptoms (Gracie et al., 2007; Heins et al., 2011; Spauwen et al., 2006; Thompson et al., 2009). TLEs have been defined in various ways depending on the literature (e.g., adversity, negative life events, abuse, neglect), but PLES have been associated with TLEs regardless of the definition (for a discussion of this issue, see Gibson et al., 2016). For the purposes of this study, we define TLEs as physical, sexual, and emotional abuse, as well as neglect experiences. Considered part of the extended psychosis phenotype, PLEs have been found to occur in 5-8% of non-clinical populations and have been linked to both risk for developing a psychotic disorder and with many of the same risk factors as psychotic disorders, such as cannabis use and exposure to TLEs (Kaymaz et al., 2012; Reeves et al., 2014; van Os et al., 2009; van Os & Linscott, 2012).
A recent meta-analysis indicated that the magnitude of the relation between trauma exposure and subclinical psychotic experiences is fairly large (with odds ratios ranging from 3 to 11), even after controlling for demographic factors and comorbid mental disorders (Janssen et al., 2004; Varese et al., 2012a). The impact of the TLE and psychosis association is emphasized by findings that TLE exposure predates the onset of psychosis (Arseneault et al., 2011; Kelleher et al., 2013; Mackie et al., 2011), and that having a history of TLEs in the context of psychosis is linked to a worse disorder course (e.g., worse symptomatology, cognitive deficits, and treatment resistance; Hassan & De Luca, 2015; Schenkel et al., 2005). Collectively, these findings suggest that TLEs are likely to influence the pathways to, and course of, psychotic experiences.
Despite the robust TLE and psychosis association, the psychological mechanisms by which trauma influences the development of psychosis remain unclear. However, several theoretical models focused on cognitive mechanisms have been suggested (Bentall & Fernyhough, 2008; Morrison et al., 2003; Read et al., 2005; van Winkel et al., 2013). Specific underlying mechanisms that have been proposed to account for this relationship include locus of control, stress sensitivity, negative schemas, and dissociation (Anglin et al., 2014; Fisher et al., 2012; Fisher et al., 2013; Gibson et al., 2014). However, the majority of the empirical data has investigated these mechanisms in isolation rather than simultaneously, the latter of which takes a much more conservative approach (Bebbington et al., 2011; Fisher et al., 2012; Fisher et al., 2013; Freeman & Fowler, 2009; Gracie et al., 2007; Perona-Garcelán et al., 2012).
The importance of perceived stress in the relationship between TLEs and PLEs has been highlighted by research showing that many individuals display heightened physiological or subjective reactivity to lab-induced or environmental stressors, particularly individuals who have been exposed to TLEs (Glaser et al., 2006) and those experiencing symptoms along the entire psychosis continuum (Aiello et al., 2012; Collip et al., 2013a; Lardinois et al., 2011; Lataster et al., 2009; Myin-Germeys et al., 2001). Further, in a sample of university undergraduates, greater perceived stress was found to mediate the association between TLEs and PLEs (Gibson et al., 2014). We wished to extend these findings to determine whether perceived stress remained a significant mediator in the context of other explanatory variables.
Another cognitive mechanism implicated in the pathogenesis of psychosis stemming from TLEs is negative schemas (i.e., negative global beliefs about oneself, others, and the world). Negative schemas are associated with both strict and broad definitions of psychosis (Addington & Tran, 2009; Bortolon et al., 2013; Fowler et al., 2011) and have been found to predict PLEs (Gracie et al., 2007). Negative schemas also have been found to mediate the relationship between TLEs and paranoia (Fisher et al., 2012). Our study intends to expand this research by including other explanatory variables in the mediation model, and by assessing attenuated psychosis more broadly.
Experiencing TLEs also has been hypothesized to lead to dissociative symptoms (e.g., difficulty distinguishing between whether something an individual remembers was reality or a dream) that subsequently lead to psychosis-proneness (Anketell et al., 2010; Moskowitz & Corstens, 2008). Not only have dissociative experiences been consistently associated with a TLE history (Ogawa et al., 1997), but they have been significantly linked to subclinical and clinical psychotic symptoms (Braehler et al., 2013; Schroeder et al., 2016). Dissociation also has been implicated as a significant independent mediator of the TLE-PLE relationship (Anglin et al., 2014; Perona-Garcelán et al., 2012; Varese et al., 2012b), although to our knowledge, no study has investigated this construct in the context of both attenuated hallucinatory and delusional experiences with a more conservative definition of TLEs (i.e., endorsement of at least moderate to severe exposure), gaps this study addresses.
Individuals along the psychosis continuum also appear more likely to make external attributions for their private and public experiences (i.e., manifesting an external locus of control) than those endorsing lower levels of psychotic experiences, to the extent that they interpret their environment as controlled more by outside sources like chance, luck, fate, or powerful others rather than the self (Bentall & Fernyhough, 2008; Candido & Romney, 1990; Cooper et al., 2008; Frenkel et al., 1995; Kaney & Bentall, 1989; Levine et al., 2004; Rosenbaum & Hadari, 1985; Thompson et al., 2011). Possessing an external locus of control was found to be one of the strongest longitudinal predictors of psychotic disorder development (Frenkel et al., 1995), has been found to prospectively mediate the relationship between TLE exposure and attenuated psychosis (Fisher et al., 2013), and has been linked to worse disorder phenomenology and prognosis (Ciufolini et al., 2015). Our study appears to be the first to investigate external locus of control as a mediator of the TLE-PLE relationship in the context of many commonly reported TLEs (e.g., emotional, physical, and sexual abuse), as the TLEs measured in the Fisher et al. (2013) mediation study were exposure to bullying, harsh parenting, and domestic violence.
Given that perceived stress, negative schemas, dissociation, and locus of control have been linked to both TLE exposure and the full spectrum of psychotic experiences, we hypothesized that they would each act as independent putative mediators of the association between TLEs and PLEs, as well as significant explanatory mechanisms in the multiple mediation model, which accounts for the presence of all other putative mediators in a single model. We also conducted analyses to determine which mediators were specific to PLEs by controlling for comorbid psychological symptoms.
2. Method
2.1. Participants and Procedure
Undergraduate students (N = 945) between the ages of 18 and 34 (M = 20.13; SD = 2.47) were from a socioeconomically and racially diverse urban university in the United States. Participants were recruited from courses across multiple disciplines via an online recruitment website and received course credit for their participation. The study protocol received Institutional Review Board approval from the university and informed consent was obtained from all participants prior to participation. After consenting, participants were directed to a laboratory computer where they completed self-report questionnaires and experimental paradigms. Participants beyond the typical age of onset for schizophrenia spectrum disorders (i.e., ages 18 to 35) were excluded from the study in order to capture individuals at peak age for the emergence of psychotic symptoms (American Psychiatric Association, 2013).
2.2. Measures
The Childhood Trauma Questionnaire Short-Form (CTQ; Bernstein et al., 1994; Bernstein & Fink, 1998) measured TLEs. The CTQ is a self-report inventory for ages 12 and up that assesses five maltreatment types (emotional, physical and sexual abuse, and emotional and physical neglect). The CTQ has been found to display good sensitivity and specificity, criterion validity, internal consistency, and convergent reliability across clinical and general population samples (Bernstein & Fink, 1998). Each of the five scales has a cutoff score, including “none to low”, “low to moderate”, “moderate to severe”, and “severe to extreme” exposure. Similar to other studies, the TLE+ group was comprised of individuals who endorsed at least one of the five TLEs at or above the “moderate to severe” cutoff and the TLE- group was comprised of individuals who had scores below the cutoffs (Bendall et al., 2013; Heim et al., 2009; Klewchuk et al., 2007).
The 45 positive items of the 92-item Prodromal Questionnaire (PQ) were used to measure the number of PLEs endorsed in the past month outside the influence of drugs, alcohol, or other medications (Loewy et al., 2005; Loewy et al., 2007). This scale has been found to have moderate concurrent validity and specificity and strong sensitivity when compared to other semi-structured interviews that assess psychosis (Kline et al., 2012; Miller et al., 2002).
Perceived stress was evaluated with the Perceived Stress Scale (PSS; Cohen et al., 1983). The PSS is a 14-item measure of perceived global stress and coping ability that focuses on the predictability and controllability of events in the past month. This scale has established high concurrent and predictive validity with health outcomes, psychiatric outcomes, and with other measures of stress, as well as moderate internal and test-retest reliability (Cohen et al., 1983; Cohen, 1988; Cohen et al., 1993; Hewitt et al., 1992). Higher PSS scores have discriminated between those at risk for psychosis or with first-episode psychosis and controls, and have been associated with schizotypy (Horan et al., 2007; Mondelli et al., 2010; Palmier-Claus et al., 2012).
Negative self-schemas and negative other-schemas were assessed with the Brief Core Schema Scale (BCSS), which is a 24-item assessment of positive and negative schemas concerning the self and others, such as “I am weak” and “Other people are truthful” (Fowler et al., 2006). This scale has been found to be discrete from traditional measures of self-esteem and mood, to be associated with several psychosis outcomes, to demonstrate good internal consistency and test-retest reliability, and moderate to strong concurrent and discriminant validity with self-esteem and depression measures (Addington & Tran, 2009; Fowler et al., 2006; Stowkowy et al., 2016). The negative-self (six items) and negative-others (six items) scores constituted independent putative mediators for the present study.
Dissociation was measured with the Dissociative Experiences Scale (DES; Bernstein & Putnam, 1986), which is a 28-item instrument that assesses dissociative symptoms and experiences (e.g., “Some people have the experience of being in a familiar place but finding it strange and unfamiliar”). The DES is regarded as the gold standard for evaluating dissociation, demonstrating good reliability and validity, and has been associated with various psychosis outcomes (Braehler et al., 2013). The outcome from the DES was the average of the summed score.
The Rotter I-E Scale (Rotter, 1966) measured locus of control, a concept that assesses individuals’ beliefs about how reinforcement is controlled in the world and the degree to which they believe that they can control events happening around them. Higher scores indicate a more external locus of control (i.e., perceiving that reward/reinforcement is not connected to one’s own behavior, but controlled by outside sources). This 23-item instrument has been found to have good test-retest reliability, internal consistency, and concurrent validity with other locus of control measures (Lange & Tiggemann, 1981; Zerega et al., 1976).
To partially address the issue of specificity of the putative mediators on the TLE-PLE relationship, our supplementary analyses tested whether the main mediation model persisted when controlling for depressive symptoms, generalized anxiety symptoms, and substance use given the association between TLEs and these constructs (Green et al., 2010). Depressive symptoms were measured with the brief version of the Center for Epidemiologic Studies-Depression Scale (Radloff, 1977). Generalized anxiety was assessed with the State Trait Anxiety Inventory Trait Form Anxiety Subscale with a version that excluded items from the depression factor (Bieling et al., 1998; Spielberger et al., 1983). The Drug Use Frequency Measure assessed the frequency of use of various substances in the past three months on a scale ranging from “never” to “daily” (O’Farrell et al., 2003). Cannabis and other drug use (i.e., amphetamines, opioids/heroin, and hallucinogens) was dichotomized into a “high” versus “low” use category based on a previous study using the same sample (Reeves et al., 2014). All three scales have been found to demonstrate strong psychometric properties (Bieling et al., 1998; O’Farrell et al., 2003; Radloff, 1977; Rule & Traver, 1983; Spielberger et al., 1983).
2.3. Statistical Analysis
After listwise deletion of missing data, the multiple mediator model included 941 participants. The continuous dependent variable, PLEs, was log-transformed (ln + 1 to address zero values) because of positive skew observed via visual inspection. Bivariate analyses among the demographic, predictor (i.e., TLEs) and outcome (i.e., PLEs) variables involved: chi-square tests when both variables were categorical, Pearson correlations when both variables were continuous, ANOVA when there was a categorical predictor and continuous outcome, and logistic regression (expressed as odds ratios) when there was a continuous predictor and binary outcome. Age, race, and gender were considered covariates if they were related to both the independent and dependent variables.
To examine the indirect effects of the five mediators on the relationship between TLEs and PLEs, we used Hayes (2013) regression-based PROCESS macro. The PROCESS macro tests the direct and indirect effects, as well as provides point estimates (unstandardized effects) and bias-corrected 95% bootstrapped confidence interval (CI) estimates around the indirect effect. The CIs for the indirect effects that do not include zero are considered significant. As per Hayes’ (2013) recommendation, effect sizes were measured with the partially standardized indirect effect of X on Y and were available only for the multiple mediation model (Hayes, 2013). Statistical analyses were conducted using SPSS Version 22.
We also ran three supplementary models: 1) controlling for comorbid symptoms (i.e., depressive and anxiety symptoms, as well as substance use in the past three months) to isolate the specificity of the putative mediators for the TLE and PLE relationship, 2) examining the influence comorbid depressive and anxiety symptoms might have as potential mediators rather than confounders, and 3) exploring the differential impact of TLE type (i.e., running neglect as a separate model from sexual, physical, and emotional abuse experiences).
3. Results
3.1. Demographics
Demographic and clinical characteristics for this sample are presented in Table 1. There was no observed difference for gender between those in the TLE- compared to the TLE+ groups (p = 0.66) and gender was not significantly associated with PLEs (p = 0.17). There was an observed difference among the racial groups depending on TLE status (X2= 55.11, p < 0.0001); however, race was not associated with PLEs (p = 0.27). Although older individuals were significantly more likely to be in the TLE+ group (OR = 1.07, p = 0.02), age was not associated with PLEs (p = 0.09). Therefore, we did not control for gender, race, or age.
Table 1.
Descriptive Characteristics
| Demographics | Overall sample (N = 945) |
|---|---|
| Male, n (%) | 231 (24.40) |
| Age (years), mean (SD) [range] | 20.13 (2.47) [18–34] |
| Race, n (%) | |
| Non-Hispanic White | 520 (55.00) |
| African-American/African | 169 (17.90) |
| Asian/Pacific Islander | 145 (15.30) |
| Multiracial | 48 (5.10) |
| Other | 63 (6.70) |
| Clinical Characteristics, mean (SD) [range] | |
| Receiving or seeking treatment, n (%) | 124 (13.0) |
| PLEs | 9.92 (7.69) [0–44] |
| PSS | 25.22 (8.14) [2–55] |
| BCSS-Self | 2.84 (3.88) [0–24] |
| BCSS-Others | 6.83 (5.38) [0–24] |
| DES | 2.28 (1.23) [1–8] |
| Rotter I-E | 12.43 (3.56) [3–23] |
| TLEs | 0.62 (1.07) [0–5] |
| TLE+, n, % | 312 (33.0) |
| Childhood Emotional Abuse, n, % | 147, 15.6 |
| Childhood Physical Abuse, n, % | 100, 10.6 |
| Childhood Sexual Abuse, n, % | 100, 10.6 |
| Childhood Emotional Neglect, n, % | 118, 12.5 |
| Childhood Physical Neglect, n, % | 119, 12.6 |
TLEs= Traumatic Life Events; TLE+ = Participants who endorsed a history of trauma; PLEs= Psychotic-like Experiences; PSS = Perceived Stress Scale; BCSS = Brief Core Schema Scale; DES = Dissociative Experiences Scale; Rotter I-E = Rotter Internal External Locus of Control Scale
3.2. Bivariate Analyses
The a paths (TLEs to the mediators), b paths (mediators to PLEs), and c path (TLEs to PLEs), were significant in both the independent and multiple mediation models (see Figure 1; supplementary analyses include a correlation matrix for the main independent, mediator, and dependent variables). Perceived stress was significantly associated with TLEs (F[1, 943] = 54.79, p < 0.0001) and PLEs (r = 0.43, p < 0.0001. Dissociation was significantly related to TLEs (F[1, 940] = 55.08, p < 0.0001) and PLEs (r = 0.45, p < 0.0001). External locus of control was significantly associated with the predictor variable, TLEs (F[1, 940] = 8.42, p = 0.004), and the outcome variable, PLEs (r = 0.23, p < 0.0001). Negative self-schemas also were significantly related to TLEs (F[1, 939] = 80.02, p < 0.0001) and PLEs (r = 0.36, p < 0.0001), as were negative other-schemas (F[1, 939] = 14.63, p < 0.001 for TLEs and r = 0.24, p < 0.0001 for PLEs). Lastly, TLE status was significantly associated with PLEs (F[1, 943] = 44.23, p < 0.0001).
Figure 1.
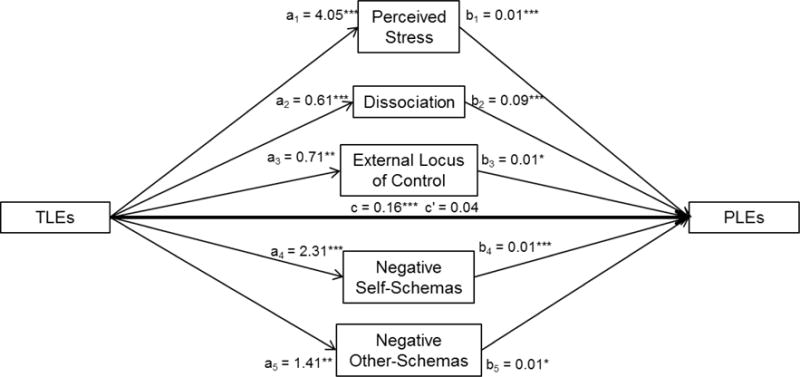
Effect of Multiple Mediators on the Relationship Between Traumatic Life Events (TLEs) and Psychotic-Like Experiences (PLEs). a = effect of TLEs on mediators; b = effect of mediators on PLEs; c = direct effect of TLEs on PLEs; c’ = indirect effect of TLEs on PLEs through the five mediators; *p < 0.05; **p < 0.01; ***p < 0.001. Values are unstandardized coefficients.
3.3. Indirect Effects
Results for the full mediation model are presented in Figure 1. Indirect effects indicated that greater perceived stress, dissociation, external locus of control, and negative self- and other-schemas were significant putative mediators in the relationship between TLE exposure and higher PLE endorsement (see Table 2). When exploring the independent contribution of each mediator, all five variables statistically mediated the association between TLEs and PLEs (see Table 2).
Table 2.
Summary of Indirect Effects from Independent and Multiple Mediation Models
| Multiple mediation model* | Unstandardized estimate | 95% CI** | Partially standardized indirect effect | 95% CI* |
|---|---|---|---|---|
| TLE→ perceived stress→ PLEs | 0.04 | 0.0227 – 0.0525 | 0.10 | 0.0623 – 0.1428 |
| TLE→ dissociation→ PLEs | 0.05 | 0.0368 – 0.0748 | 0.15 | 0.1036 – 0.2016 |
| TLE→ external locus of control→ PLEs | 0.005 | 0.0008 – 0.0120 | 0.01 | 0.0020 – 0.0318 |
| TLE→ negative self-schemas→ PLEs | 0.03 | 0.0143 – 0.0426 | 0.07 | 0.0373 – 0.1166 |
| TLE→ negative other-schemas→ PLEs | 0.01 | 0.0018 – 0.0156 | 0.02 | 0.0047 – 0.0435 |
| Independent mediation model | Unstandardized estimate | 95% CI* | ||
| TLE→ perceived stress→ PLEs | 0.07 | 0.0522 – 0.0961 | ||
| TLE→ dissociation→ PLEs | 0.08 | 0.0558 – 0.1048 | ||
| TLE→ external locus of control→ PLEs | 0.02 | 0.0053 – 0.0288 | ||
| TLE→ negative self-schemas→ PLEs | 0.07 | 0.0536 – 0.0927 | ||
| TLE→ negative other-schemas→ PLEs | 0.02 | 0.0101 – 0.0359 |
TLE = traumatic life events; PLEs = Psychotic-Like Experiences;
Model represents the effect of each mediator in the context of the other mediators.
95% Confidence Interval of the indirect effect effects derived from 1,000 bias-corrected bootstrapped samples (log-transformed); CIs that do not include zero are considered significant and are bolded.
3.4. Supplementary Analyses
Our first supplementary analysis adjusted the models for depressive and anxiety symptoms, as well as substance use, and indicated that dissociation was the only variable to persist in statistically mediating the TLE-PLE relationship. Our second supplementary model included depressive and anxiety symptoms as potential mediators rather than as confounders. Results from this model showed that dissociation, depression, and anxiety symptoms, but not perceived stress, locus of control, or negative-self and other schemas, mediated the relationship between TLEs and PLEs. Lastly, our supplementary analyses indicated that differentiating between any abuse (i.e., childhood emotional, physical, and sexual abuse experiences) versus any neglect (i.e., physical and emotional neglect experiences) does not influence the overall pattern of results given that all five cognitive constructs significantly mediated the relationship between abuse/neglect and PLEs. Data from all supplementary models available upon request.
4. Discussion
This is the first study, to our knowledge, to find that multiple cognitive variables are involved in the relationship between TLEs and PLEs. Specifically, we found that perceived stress, dissociation, external locus of control, negative self-schemas, and negative other-schemas yielded significant indirect effects (both independently and in the multiple mediator model) on the association between TLE and PLEs. However, specificity analyses indicated that dissociation was the only significant mediator that held up after adjusting for comorbid symptoms. These results underscore the salience of dissociation as a critical cognitive style in the TLE-PLE relationship since this was the only variable to persist in its significance across the adjusted models. Although external locus of control, negative schemas, and stress sensitivity are important cognitive constructs to factor into posttraumatic symptomatology assessment and treatment, they may be more salient mediators for phenotypes that commonly occur in the course of psychosis (e.g., depression).
The results of our main model, which highlight the putative role of dissociation, negative schemas, stress sensitivity, and external locus of control, are consistent with research finding the TLE-psychosis relation through indirect effects involving cognitive based mechanisms (Anglin et al., 2014; Fisher et al., 2012; Fisher et al., 2013; Gibson et al., 2014; Gracie et al., 2007; Varese et al., 2012b). Additionally, differentiating between childhood abuse and childhood neglect experiences did not alter the overall influence of the mediators. Each of the mediators in the current study has implications for how reality distortions that might emerge in the aftermath of TLEs could influence the onset of psychotic experiences. It is imperative that future studies assess whether the proposed cognitive styles are a consequence or antecedent of PLEs, a time course this study could not rule out due to the cross-sectional design.
Paralleling other studies was our finding that dissociation was a significant putative mediator of the link between TLEs and PLEs (Anglin et al., 2014; Perona-Garcelán et al., 2012; Varese et al., 2012b). Our study extended these findings in that the strength of dissociation as a potential mediator is underscored by its persistent mediation in the full model, and in that we defined our TLE variable based on higher severity scores versus a one-item binary TLE versus no TLE outcome. Further, we assessed the specificity of this mechanism to PLEs by controlling for several comorbid symptoms, and dissociation was the only variable to hold up to this conservative adjustment. Several researchers have proposed that individuals may respond to TLEs with dissociative experiences (e.g., derealization) that can involve an individual’s personality becoming divided into fragmented selves (e.g., a trauma versus current, daily functioning version of themselves; Anketell et al., 2010; Liotti & Gumley, 2008; Van der Hart et al., 2006). These split versions of the selves are thought to conflict, with the ‘trauma’ focused version being experienced as atypical and unfamiliar to the person and inducing psychotic-like interpretations or “tuning out” experiences (Braehler et al., 2013; Van der Hart et al., 2006). Overall, it appears that dissociation may be a critical feature of posttraumatic event processing that makes it more likely that an individual experiences their environment in an unintegrated, disjointed manner, subsequently increasing their vulnerability to psychotic experiences and interpretations of their world.
Perceived stress appears to be important in increasing risk for psychosis, particularly given an adverse life experience history (Lardinois et al., 2011; Gibson et al., 2014; Trotman et al., 2014). One possible interpretation of our results is that as a result of experiencing trauma, heightened levels of perceived stress that correspond to a reduced sense of controllability and predictability may increase vulnerability to psychotic-symptoms or disorders. In a similar vein, it is possible that a diminished sense of power over one’s experiences may be more likely to manifest or be exacerbated by exposure to TLEs (Erickson et al., 2013; Karstoft et al., 2015). Our supplementary results highlight the transdiagnostic significance of stress sensitivity, such that this construct may be present in the context of other psychological reactions to TLEs (e.g., depressive, anxious, or substance use reactions) rather than unique to psychotic-like presentations.
Subsequent to experiences of victimization, externalizing explanatory styles may be activated or intensified, which may then lead to anticipating threat or to paranoid interpretations of the world (Bentall & Fernyhough, 2008; van Winkel et al., 2013). Consistent with this possibility, we found that having an externalizing locus of control mediated the TLE-PLE relationship. However, the role of locus of control was not as strong as other mediators (see Table 2). Supplementary analyses demonstrated that although locus of control most likely has its place as a putative mediator of the TLE-PLE relationship, its effect on this relationship may be diluted by comorbid psychological symptoms that also are associated with a history of trauma.
Finally, we found that negative schemas, particularly toward the self rather than others, mediated the TLE-PLE relation. This finding suggests that negative beliefs about oneself (e.g., I am vulnerable) or the world (e.g., other people are devious) may be likely to emerge post-childhood trauma, which may make these individuals more prone to psychotic-like explanations or filters (Gracie et al., 2007). Specifically, early adversities have been conceptualized to facilitate negative schemas about the self and others involving vulnerability, humiliation, and subordination (e.g., that one is vulnerable to being harmed due to the hostile intentions of others), which are then thought to increase psychotic symptom development in those with genetic predispositions (Garety et al., 2001). It is also important to note that the significant effect of negative schemas as a mediator of the association between TLEs and PLEs became non-significant when comorbid symptoms were included as either control variables or as potential mediators, potentially given the high co-occurrence between negative schemas and comorbid symptoms, such as depression and anxiety (Calvete et al., 2013).
Despite the potential interpretations of how the mediators may influence PLEs in the aftermath of TLE exposure, reverse directionality issues (i.e., other models) cannot be ruled out. Thus, future studies are warranted that 1) help determine whether TLEs predate the proposed cognitive mediators, and whether psychotic-like symptoms are a consequence of this admixture of experiences, and 2) narrow which psychopathologies these mediators exert their most potent influence post-trauma.
The advantages of exploring the aforementioned variables in a full mediation model is that, while many of them have been individually found to mediate the TLE-psychosis link, it is important to determine the independent strength of specific indirect effects in the context of one another. Hayes (2013) contends that examining multiple mechanisms in an integrated model is preferred given that one mediator is not likely to be the sole way through which a predictor has an effect on the outcome. Indeed, it is more likely that the relationship between TLE exposure and psychosis is impacted by various processes, including others that were not measured by the current study (e.g., social defeat; van Winkel et al., 2013).
There are several methodological limitations to the current study. Most importantly, the study design was cross-sectional, and thus, reverse directionality poses a concern. As mentioned above, the cross-sectional nature of the design does not preclude the existence of other models not tested in this study. Future studies that explore the temporal precedence of TLEs and these five mediators in a longitudinal capacity among a nationally representative or clinical sample are necessary. Nevertheless, previous longitudinal studies implicate a timeline whereby TLEs predate some of the mediators of the current study (e.g., locus of control or self-esteem, the latter which may represent a proxy for negative self-schemas), after which time psychotic-like symptoms have been observed (Fisher et al., 2013). Further, another longitudinal study found a bidirectional relationship between physical abuse and PLEs with abuse experiences strongly predicting PLEs (Kelleher et al., 2013). Despite these findings, the temporal nature of the other mediators should be assessed in future studies. To address reverse directionality, we analyzed supplementary models that swapped the order of the dependent and mediator variables (data available upon request). These independent models led to us not being able to rule out the possibility that three of the cognitive styles that were originally proposed as mediators (i.e., negative self- and other-schemas, as well as perceived stress) are a result of psychotic-like experiences rather than antecedents. Nevertheless, these alternative models explored independent, not multiple, mediation. Future studies considering these cognitive styles as multiple outcome variables (adjusting for one another) are warranted.
We also primarily focused on cognitive mechanisms when we acknowledge that a variety of other potential mechanism are likely at play in the development of PLEs following exposure to TLEs, particularly via genetic and affective pathways. Genetic influences likely moderate the effects of traumatic experiences in increasing risk for psychotic symptoms (Collip et al., 2013b), and some genes may predispose an individual to developing certain cognitive styles, such as perceived stress, and psychotic experiences. As such, future studies that include genetic/biomarker collection from participants may be able to better elucidate the potential role of genetic confounds. With regard to affective mechanisms, our supplementary findings highlight the importance of depressive and anxiety symptoms in explaining the relationship between TLEs and PLEs, which is consistent with other studies that find affective and cognitive factors operating in parallel to exert their influence on psychotic-like symptoms in the context of TLE exposure (Bebbington et al., 2007; Fisher at al., 2012; Fisher et al., 2013).
An additional limitation is that the sample was comprised of undergraduate students, which may limit how translatable these findings are to general population samples. Nevertheless, the sample was socioeconomically and racially diverse, which may help to counter this limitation to some degree. Assessing nuanced demographic factors (e.g., gender, race) that may influence vulnerability and/or predispose someone to increased risks (e.g., increased perceived stress) for certain cognitive styles after childhood trauma is an important area in need of investigation, and future longitudinal studies may be better able to address these potential interactions.
Another limitation involves the nature of our assessment. First, TLE assessment was retrospective. However, concerns about the reliability of TLE recall have been challenged by findings that TLE reporting among psychotic samples tends to be underestimated, stable, and in sync with corroborating reports (Cutajar et al., 2010; Fisher et al., 2011). Second, the retrospective nature of childhood maltreatment measurement may have resulted in false negatives (i.e., non-exposed TLE group being misclassified), especially given that prospective studies have been found to identify different groups of individuals as maltreated than retrospective studies (Newbury et al., 2018). Third, assessment of symptoms and TLEs was also limited to self-report. These assessment limitations would ideally be addressed in future studies by matching self-report data to experimental- or interview-based measurements of relevant constructs.
Lastly, this study examined the dimensional nature of psychotic and other psychiatric symptoms rather than those that solely meet clinical diagnostic threshold for psychosis-risk and/or psychiatric disorders (diagnostic information was also not available for the full sample). It would be useful for future studies to examine whether and how results vary for those who have crossed the diagnostic threshold for a psychotic or other psychiatric disorder, as well as for individuals engaged in mental health treatment, particularly since individuals with a TLE history were more likely to endorse being in or seeking mental health treatment in the past month (X2 = 18.62, p < 0.0001). We also acknowledge that schizophrenia is only one outcome of PLEs, and would look to additional studies to explore the potential influence of these mediators on other psychological constructs (e.g., depression, posttraumatic stress symptoms) instead of PLEs.
In conclusion, this study highlights the importance of several cognitive mechanisms in the relationship between TLEs and PLEs, which may be amenable to psychological intervention, such as targeting trauma-related cognitions that are linked to psychotic-like appraisals of oneself, others, and the world (Sherrer, 2011). Various treatment options have been found to be efficacious for reducing some of the negative effects of the mediators shown in this study, such as Schema Therapy to address maladaptive schemas (Young et al., 2003). Community-based preventative measures to reduce TLE exposure are also warranted given the vast psychological sequelae that have been found to stem from TLEs, such as PLEs (Kelleher et al., 2013). Nuanced clinical assessments that capture TLE histories and how the content and attribution of the specific TLE may manifest in the phenomenology of psychotic symptoms may also constitute a useful avenue of intervention.
Acknowledgments
We thank all of the people who chose to participate in this study. We also thank Seth Maxwell and all of the research assistants for their help in various aspects of the study.
Role of Funding Source
Funding for this study was provided by Temple University’s College of Liberal Arts Research Award, a University Start-Up Fund both awarded to Lauren Ellman, PhD, and the following grants awarded to LME from NIMH: R01MH096478 & R01MH112613.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Author Gibson primarily designed the study, performed the statistical analyses, and wrote the first draft of the manuscript. Authors Reeves and Cooper provided scientific oversight and edited the manuscript. Author Olino provided scientific and statistical analysis support. Author Ellman wrote the original study protocol for the larger study, contributed to all aspects of the current study, provided conceptual and scientific oversight of the study protocol, analyses, and writing of the manuscript, and edited the manuscript. All authors contributed to and have approved the final manuscript.
Conflict of Interest
None of the authors declare any conflicts of interest.
References
- Addington J, Tran L. Using the Brief Core Schema Scales with individuals at clinical high risk of psychosis. Behav Cogn Psychother. 2009;37:227–231. doi: 10.1017/S1352465809005116. [DOI] [PubMed] [Google Scholar]
- Aiello G, Horowitz M, Hepgul N, Pariante CM, Mondelli V. Stress abnormalities in individuals at risk for psychosis: a review of studies in subjects with familial risk or with “at risk” mental state. Psychoneuroendocrinology. 2012;37(10):1600–1613. doi: 10.1016/j.psyneuen.2012.05.003. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders: DSM-5. 5th. Arlington, VA: American Psychiatric Publishing, Inc.; 2013. [Google Scholar]
- Anglin DM, Polanco-Roman L, Lui F. Ethnic variation in whether dissociation mediates the relation between traumatic life events and attenuated positive psychotic symptoms. J Trauma Dissociation. 2014;16(1):68–85. doi: 10.1080/15299732.2014.953283. [DOI] [PubMed] [Google Scholar]
- Anketell C, Dorahy MJ, Shannon M, Elder R, Hamilton G, Corry M, MacSherry A, Curran D, O’Rawe B. An exploratory analysis of voice hearing in chronic PTSD: Potential associated mechanisms. J Trauma Dissociation. 2010;11(1):93–107. doi: 10.1080/15299730903143600. [DOI] [PubMed] [Google Scholar]
- Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A. Childhood trauma and children’s emerging psychotic symptoms: a genetically sensitive longitudinal cohort study. Am J Psychiatry. 2011;168(1):65–72. doi: 10.1176/appi.ajp.2010.10040567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bebbington P, Jonas S, Kuipers E, King M, Cooper C, Brugha T, Meltzer H, McManus S, Jenkins R. Childhood sexual abuse and psychosis: data from a cross-sectional national psychiatric survey in England. Br J Psychiatry. 2011;199(1):29–37. doi: 10.1192/bjp.bp.110.083642. [DOI] [PubMed] [Google Scholar]
- Bendall S, Hulbert CA, Alvarez-Jimenez M, Allott K, McGorry PD, Jackson HJ. Testing a model of the relationship between childhood sexual abuse and psychosis in a first-episode psychosis group: the role of hallucinations and delusions, posttraumatic intrusions, and selective attention. J Nerv Ment Dis. 2013;201(11):941–947. doi: 10.1097/NMD.0000000000000033. [DOI] [PubMed] [Google Scholar]
- Bentall RP, Fernyhough C. Social predictors of psychotic experiences: specificity and psychological mechanisms. Schizophr Bull. 2008;34(6):1012–1020. doi: 10.1093/schbul/sbn103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis. 1986;174(12):727–735. doi: 10.1097/00005053-198612000-00004. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, Sapareto E, Ruggiero J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151:1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L. Childhood trauma questionnaire: A retrospective self-report: Manual. Psychological Corporation 1998 [Google Scholar]
- Bieling PJ, Antony MM, Swinson RP. The State–Trait Anxiety Inventory, Trait version: structure and content re-examined. Behav Res Ther. 1998;36(7):777–788. doi: 10.1016/s0005-7967(98)00023-0. [DOI] [PubMed] [Google Scholar]
- Bortolon C, Capdevielle D, Boulenger JP, Gely-Nargeot MC, Raffard S. Early maladaptive schemas predict positive symptomatology in schizophrenia: A cross-sectional study. Psychiatry Res. 2013;209(3):361–366. doi: 10.1016/j.psychres.2013.03.018. [DOI] [PubMed] [Google Scholar]
- Braehler C, Valiquette L, Holowka D, Malla AK, Joober R, Ciampi A, Pawliuk N, King S. Childhood trauma and dissociation in first-episode psychosis, chronic schizophrenia and community controls. Psychiatry Res. 2013;210(1):36–42. doi: 10.1016/j.psychres.2013.05.033. [DOI] [PubMed] [Google Scholar]
- Calvete E, Orue I, Hankin BL. Transactional relationships among cognitive vulnerabilities, stressors, and depressive symptoms in adolescence. J of Abnorm Child Psychol. 2013;41(3):399–410. doi: 10.1007/s10802-012-9691-y. [DOI] [PubMed] [Google Scholar]
- Candido CL, Romney DM. Attributional style in paranoid vs. depressed patients. Br J Med Psychol. 1990;63(4):355–363. doi: 10.1111/j.2044-8341.1990.tb01630.x. [DOI] [PubMed] [Google Scholar]
- Ciufolini S, Morgan C, Morgan K, Fearon P, Boydell J, Hutchinson G, Demjaha A, Girardi P, Doody GA, Jones PB, Murray R, Dazzan P. Self esteem and self agency in first episode psychosis: Ethnic variation and relationship with clinical presentation. Psychiatry Res. 2015;227(2):213–218. doi: 10.1016/j.psychres.2015.03.030. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- Cohen S. Psychosocial models of the role of social support in the etiology of physical disease. Health Psychol. 1988;7(3):269–297. doi: 10.1037//0278-6133.7.3.269. [DOI] [PubMed] [Google Scholar]
- Cohen S, Tyrrell DA, Smith AP. Negative life events, perceived stress, negative affect, and susceptibility to the common cold. J Pers Soc Psychol. 1993;64(1):131–140. doi: 10.1037//0022-3514.64.1.131. [DOI] [PubMed] [Google Scholar]
- Collip D, Myin-Germeys I, Wichers M, Jacobs N, Derom C, Thiery E, Lataster T, Simons C, Delespaul P, Marcelis M, van Os J, van Winkel R. FKBP5 as a possible moderator of the psychosis-inducing effects of childhood trauma. Br J Psychiatry. 2013a;202(4):261–268. doi: 10.1192/bjp.bp.112.115972. [DOI] [PubMed] [Google Scholar]
- Collip D, Wigman JT, Myin-Germeys I, Jacobs N, Derom C, Thiery E, Wichers M, Van Os J. From epidemiology to daily life: linking daily life stress reactivity to persistence of psychotic experiences in a longitudinal general population study. PloS One. 2013b;8(4):e62688. doi: 10.1371/journal.pone.0062688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper F, Morgan C, Morgan K, Dazzan P, Doody G, Hutchinson G, Jones P, Murray R, Fearon P. Locus of control and psychotic-like symptoms in the Aesop study. Schizophr Res. 2008;102(1):135. [Google Scholar]
- Cutajar MC, Mullen PE, Ogloff JR, Thomas SD, Wells DL, Spataro J. Schizophrenia and other psychotic disorders in a cohort of sexually abused children. Arch Gen Psychiatry. 2010;67(11):1114–1119. doi: 10.1001/archgenpsychiatry.2010.147. [DOI] [PubMed] [Google Scholar]
- Erickson LD, Hedges DW, Call VR, Bair B. Prevalence of and Factors Associated With Subclinical Posttraumatic Stress Symptoms and PTSD in Urban and Rural Areas of Montana: A Cross-Sectional Study. J Rural Health. 2013;29(4):403–412. doi: 10.1111/jrh.12017. [DOI] [PubMed] [Google Scholar]
- Fisher HL, Craig TK, Fearon P, Morgan K, Dazzan P, Lappin J, Hutchinson G, Doody GA, Jones PB, McGuffin P, Murray RM, Leff J, Morgan C. Reliability and comparability of psychosis patients’ retrospective reports of childhood abuse. Schizophr Bull. 2011;37:546–553. doi: 10.1093/schbul/sbp103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher HL, Appiah-Kusi E, Grant C. Anxiety and negative self-schemas mediate the association between childhood maltreatment and paranoia. Psychiatry Res. 2012;196(2):323–324. doi: 10.1016/j.psychres.2011.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher HL, Schreier A, Zammit S, Maughan B, Munafò MR, Lewis G, Wolke D. Pathways between childhood victimization and psychosis-like symptoms in the ALSPAC birth cohort. Schizophr Bull. 2013;39(5):1045–1055. doi: 10.1093/schbul/sbs088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler D, Freeman D, Smith B, Kuipers E, Bebbington P, Bashforth H, Coker S, Hodgekins J, Gracie A, Dunn G, Garety P. The Brief Core Schema Scales (BCSS): psychometric properties and associations with paranoia and grandiosity in nonclinical and psychosis samples. Psychol Med. 2006;36(06):749–759. doi: 10.1017/S0033291706007355. [DOI] [PubMed] [Google Scholar]
- Fowler D, Hodgekins J, Garety P, Freeman D, Kuipers E, Dunn G, Smith B, Bebbington PE. Negative cognition, depressed mood, and paranoia: a longitudinal pathway analysis using structural equation modeling. Schizophr Bull. 2011;38(5):1063–1073. doi: 10.1093/schbul/sbr019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman D, Fowler D. Routes to psychotic symptoms: trauma, anxiety and psychosis-like experiences. Psychiatry Res. 2009;169(2):107–112. doi: 10.1016/j.psychres.2008.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenkel E, Kugelmass S, Nathan M, Ingraham LJ. Locus of control and mental health in adolescence and adulthood. Schizophr Bull. 1995;21(2):219–226. doi: 10.1093/schbul/21.2.219. [DOI] [PubMed] [Google Scholar]
- Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31(02):189–195. doi: 10.1017/s0033291701003312. [DOI] [PubMed] [Google Scholar]
- Gibson LE, Anglin DM, Klugman JT, Reeves LE, Fineberg AM, Maxwell SD, Kerns CM, Ellman LM. Stress sensitivity mediates the relationship between traumatic life events and attenuated positive psychotic symptoms differentially by gender in a college population sample. J Psychiatr Res. 2014;53:111–118. doi: 10.1016/j.jpsychires.2014.02.020. [DOI] [PubMed] [Google Scholar]
- Gibson LE, Alloy LB, Ellman LM. Trauma and the psychosis spectrum: A review of symptom specificity and explanatory mechanisms. Clin Psychol Rev. 2016;49:92–105. doi: 10.1016/j.cpr.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser JP, Van Os J, Portegijs PJ, Myin-Germeys I. Childhood trauma and emotional reactivity to daily life stress in adult frequent attenders of general practitioners. J Psychosom Res. 2006;61(2):229–236. doi: 10.1016/j.jpsychores.2006.04.014. [DOI] [PubMed] [Google Scholar]
- Gracie A, Freeman D, Green S, Garety PA, Kuipers E, Hardy A, Ray K, Dunn G, Bebbington P, Fowler D. The association between traumatic experience, paranoia and hallucinations: a test of the predictions of psychological models. Acta Psychiatr Scand. 2007;116(4):280–289. doi: 10.1111/j.1600-0447.2007.01011.x. [DOI] [PubMed] [Google Scholar]
- Hassan AN, De Luca V. The effect of lifetime adversities on resistance to antipsychotic treatment in schizophrenia patients. Schizophr Res. 2015;161(2-3):496–500. doi: 10.1016/j.schres.2014.10.048. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; 2013. [Google Scholar]
- Heim C, Nater UM, Maloney E, Boneva R, Jones JF, Reeves WC. Childhood trauma and risk for chronic fatigue syndrome: association with neuroendocrine dysfunction. Arch Gen Psychiatry. 2009;66(1):72–80. doi: 10.1001/archgenpsychiatry.2008.508. [DOI] [PubMed] [Google Scholar]
- Heins M, Simons C, Lataster T, Pfeifer S, Versmissen D, Lardinois M, Marcellis M, Delespaul P, Krabbendam L, Myin-Germeys I. Childhood trauma and psychosis: a case-control and case-sibling comparison across different levels of genetic liability, psychopathology, and type of trauma. Am J Psychiatry. 2011;168(12):1286–1294. doi: 10.1176/appi.ajp.2011.10101531. [DOI] [PubMed] [Google Scholar]
- Hewitt PL, Flett GL, Mosher SW. The Perceived Stress Scale: Factor structure and relation to depression symptoms in a psychiatric sample. J Psychopathol Behav Assess. 1992;14(3):247–257. [Google Scholar]
- Horan WP, Brown SA, Blanchard JJ. Social anhedonia and schizotypy: the contribution of individual differences in affective traits, stress, and coping. Psychiatry Res. 2007;149(1):147–156. doi: 10.1016/j.psychres.2006.06.002. [DOI] [PubMed] [Google Scholar]
- Janssen I, Krabbendam L, Bak M, Hanssen M, Vollebergh W, Graaf RD, Van Os J. Childhood abuse as a risk factor for psychotic experiences. Acta Psychiatr Scand. 2004;109(1):38–45. doi: 10.1046/j.0001-690x.2003.00217.x. [DOI] [PubMed] [Google Scholar]
- Kaney S, Bentall RP. Persecutory delusions and attributional style. Br J Med Psychol. 1989;62(2):191–198. doi: 10.1111/j.2044-8341.1989.tb02826.x. [DOI] [PubMed] [Google Scholar]
- Karstoft KI, Armour C, Elklit A, Solomon Z. The role of locus of control and coping style in predicting longitudinal PTSD-trajectories after combat exposure. J Anxiety Disord. 2015;32:89–94. doi: 10.1016/j.janxdis.2015.03.007. [DOI] [PubMed] [Google Scholar]
- Kaymaz N, Drukker M, Lieb R, Wittchen HU, Werbeloff N, Weiser M, Lataster T, Van Os J. Do subthreshold psychotic experiences predict clinical outcomes in unselected non-help-seeking population-based samples? A systematic review and meta-analysis, enriched with new results. Psychol Med. 2012;42(11):2239–2253. doi: 10.1017/S0033291711002911. [DOI] [PubMed] [Google Scholar]
- Kelleher I, Keeley H, Corcoran P, Ramsay H, Wasserman C, Carli V, Sarchiapone M, Hoven C, Wasserman D, Cannon M. Childhood trauma and psychosis in a prospective cohort study: cause, effect, and directionality. Am J Psychiatry. 2013;170(7):730–741. doi: 10.1176/appi.ajp.2012.12091169. [DOI] [PubMed] [Google Scholar]
- Klewchuk EM, McCusker CG, Mulholland C, Shannon C. Cognitive biases for trauma stimuli in people with schizophrenia. Br J Clin Psychol. 2007;46(3):333–345. doi: 10.1348/014466507X173385. [DOI] [PubMed] [Google Scholar]
- Kline E, Wilson C, Ereshefsky S, Denenny D, Thompson E, Pitts SC, Bussell K, Reeves G, Schiffman J. Psychosis risk screening in youth: a validation study of three self-report measures of attenuated psychosis symptoms. Schizophr Res. 2012;141(1):72–77. doi: 10.1016/j.schres.2012.07.022. [DOI] [PubMed] [Google Scholar]
- Lange RV, Tiggemann M. Dimensionality and reliability of the Rotter IE locus of control scale. J Pers Assess. 1981;45(4):398–406. doi: 10.1207/s15327752jpa4504_9. [DOI] [PubMed] [Google Scholar]
- Lardinois M, Lataster T, Mengelers R, Van Os J, Myin-Germeys I. Childhood trauma and increased stress sensitivity in psychosis. Acta Psychiatr Scand. 2011;123(1):28–35. doi: 10.1111/j.1600-0447.2010.01594.x. [DOI] [PubMed] [Google Scholar]
- Lataster T, Wichers M, Jacobs N, Mengelers R, Derom C, Thiery E, Van Os J, Myin- Germeys I. Does reactivity to stress cosegregate with subclinical psychosis? A general population twin study. Acta Psychiatr Scand. 2009;119(1):45–53. doi: 10.1111/j.1600-0447.2008.01263.x. [DOI] [PubMed] [Google Scholar]
- Levine E, Jonas H, Serper MR. Interpersonal attributional biases in hallucinatory-prone individuals. Schizophr Res. 2004;69(1):23–28. doi: 10.1016/S0920-9964(02)00493-0. [DOI] [PubMed] [Google Scholar]
- Liotti G, Gumley A. An attachment perspective on schizophrenia: the role of disorganized attachment, dissociation and mentalization. In: Moskowitz A, Schäfer I, Dorahy MJ, editors. Psychosis, Trauma and Dissociation: Emerging Perspectives on Severe Psychopathology. John Wiley & Sons, Ltd.; Chichester, UK: 2008. pp. 117–133. [Google Scholar]
- Loewy RL, Bearden CE, Johnson JK, Raine A, Cannon TD. The prodromal questionnaire (PQ): preliminary validation of a self-report screening measure for prodromal and psychotic syndromes. Schizophr Res. 2005;79(1):117–125. [PubMed] [Google Scholar]
- Loewy RL, Johnson JK, Cannon TD. Self-report of attenuated psychotic experiences in a college population. Schizophr Res. 2007;93(1):144–151. doi: 10.1016/j.schres.2007.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackie CJ, Castellanos-Ryan N, Conrod PJ. Developmental trajectories of psychotic-like experiences across adolescence: impact of victimization and substance use. Psychol Med. 2011;41(01):47–58. doi: 10.1017/S0033291710000449. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Somjee L, Markovich PJ, Stein K, Woods SW. Prospective diagnosis of the initial prodrome for schizophrenia based on the Structured Interview for Prodromal Syndromes: preliminary evidence of interrater reliability and predictive validity. Am J Psychiatry. 2002;159(5):863–865. doi: 10.1176/appi.ajp.159.5.863. [DOI] [PubMed] [Google Scholar]
- Mondelli V, Dazzan P, Hepgul N, Di Forti M, Aas M, D’Albenzio A, Di Nicola M, Fisher H, Handley R, Marques TR, Morgan C, Navari S, Taylor H, Papadopoulos A, Aitchison KJ, Murray RM, Pariante CM. Abnormal cortisol levels during the day and cortisol awakening response in first-episode psychosis: the role of stress and of antipsychotic treatment. Schizophr Res. 2010;116(2):234–242. doi: 10.1016/j.schres.2009.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison AP, Frame L, Larkin W. Relationships between trauma and psychosis: a review and integration. Br J Clin Psychol. 2003;42(4):331–353. doi: 10.1348/014466503322528892. [DOI] [PubMed] [Google Scholar]
- Moskowitz A, Corstens D. Auditory hallucinations: Psychotic symptom or dissociative experience? Psychol Trauma. 2008;6(2-3):35–63. [Google Scholar]
- Myin-Germeys I, Van Os J, Schwartz JE, Stone AA, Delespaul PA. Emotional reactivity to daily life stress in psychosis. Arch Gen Psychiatry. 2001;58(12):1137–1144. doi: 10.1001/archpsyc.58.12.1137. [DOI] [PubMed] [Google Scholar]
- Newbury JB, Arseneault L, Moffitt TE, Caspi A, Danese A, Baldwin JR, Fisher HL. Measuring childhood maltreatment to predict early-adult psychopathology: Comparison of prospective informant-reports and retrospective self-reports. J Psychiatr Res. 2018;96:57–64. doi: 10.1016/j.jpsychires.2017.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Fals-Stewart W, Murphy M. Concurrent validity of a brief self-report Drug Use Frequency measure. Addict Behav. 2003;28:327–337. doi: 10.1016/s0306-4603(01)00226-x. [DOI] [PubMed] [Google Scholar]
- Ogawa JR, Sroufe L, Weinfield NS, Carlson EA, Egeland B. Development and the fragmented self: Longitudinal study of dissociative symptomatology in a nonclinical sample. Dev Psychopathol. 1997;9(04):855–879. doi: 10.1017/s0954579497001478. [DOI] [PubMed] [Google Scholar]
- Palmier-Claus JE, Dunn G, Lewis SW. Emotional and symptomatic reactivity to stress in individuals at ultra-high risk of developing psychosis. Psychol Med. 2012;42(05):1003–1012. doi: 10.1017/S0033291711001929. [DOI] [PubMed] [Google Scholar]
- Perona-Garcelán S, Carrascoso-López F, García-Montes JM, Ductor-Recuerda MJ, López Jiménez AM, Vallina-Fernández O, Perez-Alvarez M, Gómez-Gómez MT. Dissociative experiences as mediators between childhood trauma and auditory hallucinations. J Trauma Stress. 2012;25(3):323–329. doi: 10.1002/jts.21693. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- Read J, Van Os JV, Morrison AP, Ross CA. Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiatr Scand. 2005;112(5):330–350. doi: 10.1111/j.1600-0447.2005.00634.x. [DOI] [PubMed] [Google Scholar]
- Reeves LE, Anglin DM, Heimberg RG, Gibson LE, Fineberg AM, Maxwell SD, Kerns CM, Ellman LM. Anxiety mediates the association between cannabis use and attenuated positive psychotic symptoms. Psychiatry Res. 2014;218(1):180–186. doi: 10.1016/j.psychres.2014.03.040. [DOI] [PubMed] [Google Scholar]
- Rosenbaum M, Hadari D. Personal efficacy, external locus of control, and perceived contingency of parental reinforcement among depressed, paranoid, and normal subjects. J Pers Soc Psychol. 1985;49(2):539–547. doi: 10.1037//0022-3514.49.2.539. [DOI] [PubMed] [Google Scholar]
- Rotter JB. Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs: General and Applied. 1966;80(1):1–28. [PubMed] [Google Scholar]
- Rule W, Traver MD. Test-retest reliabilities of State-Trait Anxiety Inventory in a stressful social analogue situation. J Pers Assess. 1983;47:276–277. doi: 10.1207/s15327752jpa4703_8. [DOI] [PubMed] [Google Scholar]
- Schenkel LS, Spaulding WD, DiLillo D, Silverstein SM. Histories of childhood maltreatment in schizophrenia: relationships with premorbid functioning, symptomatology, and cognitive deficits. Schizophr Res. 2005;76(2):273–286. doi: 10.1016/j.schres.2005.03.003. [DOI] [PubMed] [Google Scholar]
- Sherrer MV. The role of cognitive appraisal in adaptation to traumatic stress in adults with serious mental illness: A critical review. Trauma Violence Abuse. 2011;12(3):151–167. doi: 10.1177/1524838011404254. [DOI] [PubMed] [Google Scholar]
- Schlosser DA, Pearson R, Perez VB, Loewy RL. Environmental risk and protective factors and their influence on the emergence of psychosis. Adolesc Psychiatry. 2012;2(2):163–171. doi: 10.2174/2210676611202020163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeder K, Langeland W, Fisher HL, Huber CG, Schäfer I. Dissociation in patients with schizophrenia spectrum disorders: what is the role of different types of childhood adversity? Compr Psychiatry. 2013;68:201–208. doi: 10.1016/j.comppsych.2016.04.019. [DOI] [PubMed] [Google Scholar]
- Spauwen J, Krabbendam L, Lieb R, Wittchen HU, Van Os J. Impact of psychological trauma on the development of psychotic symptoms: relationship with psychosis proneness. Br J Psychiatry. 2006;188(6):527–533. doi: 10.1192/bjp.bp.105.011346. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press; Palo Alto, CA: 1983. [Google Scholar]
- Stowkowy J, Liu L, Cadenhead KS, Cannon TD, Cornblatt BA, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Bearden CE, Mathalon DH, Heinssen R, Addington J. Core schemas in youth at clinical high risk for psychosis. Behav Cogn Psychother. 2016;44(02):203–213. doi: 10.1017/S1352465815000144. [DOI] [PubMed] [Google Scholar]
- Thompson JL, Kelly M, Kimhy D, Harkavy-Friedman JM, Khan S, Messinger JW, Schobel S, Goetz R, Malaspina D, Corcoran C. Childhood trauma and prodromal symptoms among individuals at clinical high risk for psychosis. Schizophr Res. 2009;108(1):176–181. doi: 10.1016/j.schres.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson A, Sullivan S, Lewis G, Zammit S, Heron J, Horwood J, Thomas K, Gunnell D, Hollis C, Wolke D, Harrison G. Association between locus of control in childhood and psychotic symptoms in early adolescence: results from a large birth cohort. Cogn Neuropsychiatry. 2011;16(5):385–402. doi: 10.1080/13546805.2010.546077. [DOI] [PubMed] [Google Scholar]
- Trotman HD, Holtzman CW, Walker EF, Addington JM, Bearden CE, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen RK, Mathalon DH, Tsuang MT, Perkins DO, Seidman LJ, Woods SW, McGlashan TH. Stress exposure and sensitivity in the clinical high-risk syndrome: initial findings from the North American Prodrome Longitudinal Study (NAPLS) Schizophr Res. 2014;160(1):104–109. doi: 10.1016/j.schres.2014.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Hart O, Nijenhuis E, Steele K. The haunted self: Structural dissociation and the treatment of chronic traumatization. New York: Norton; 2006. [Google Scholar]
- Van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness–persistence–impairment model of psychotic disorder. Psychol Med. 2009;39(02):179–195. doi: 10.1017/S0033291708003814. [DOI] [PubMed] [Google Scholar]
- Van Os J, Linscott RJ. Introduction: the extended psychosis phenotype—relationship with schizophrenia and with ultrahigh risk status for psychosis. Schizophr Bull. 2012;38(2):227–230. doi: 10.1093/schbul/sbr188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Winkel R, Van Nierop M, Myin-Germeys I, Van Os J. Childhood trauma as a cause of psychosis: linking genes, psychology, and biology. Can J Psychiatry. 2013;58(1):44–51. doi: 10.1177/070674371305800109. [DOI] [PubMed] [Google Scholar]
- Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, Read J, Van Os J, Bentall RP. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective-and cross-sectional cohort studies. Schizophr Bull. 2012a;38(4):661–671. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varese F, Barkus E, Bentall RP. Dissociation mediates the relationship between childhood trauma and hallucination-proneness. Psychol Med. 2012b;42(05):1025–1036. doi: 10.1017/S0033291711001826. [DOI] [PubMed] [Google Scholar]
- Young JE, Klosko JS, Weishaar ME. Schema Therapy: a practitioner’s guide. Guilford Press; New York: 2003. [Google Scholar]
- Zerega WD, Tseng MS, Greever KB. Stability and concurrent validity of the Rotter internal-external locus of control scale. Educ Psychol Meas. 1976;36(2):473–475. [Google Scholar]


