Abstract
Background.
This study examined language development in young children with hearing loss and different types of additional disabilities (ADs).
Method.
A population-based cohort of 67 children who were enrolled in the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study took part. Language ability was directly assessed at 3 and 5 years of age using the Preschool Language Scale 4th edition (PLS-4) and the Peabody Picture Vocabulary Test 4th edition (PPVT-4). Standard scores were used to enable comparison with age-based expectations for typically developing children.
Results.
ANOVA showed that, across the total cohort, children’s language scores remained stable over the 2-year period. However, this overall stability masked a significant difference between children with different types of ADs; in particular, children with autism, cerebral palsy, and/or developmental delay showed a decline in standard scores, whereas children with other disabilities showed a relative improvement. In addition larger improvements in receptive vocabulary were associated with use of oral communication only.
Conclusions.
The results suggest that type of AD can be used to gauge expected language development in the population of children with hearing loss and ADs when formal assessment of cognitive ability is not feasible.
Keywords: Deafness, hearing loss, intellectual disability, language development, children
Approximately 20 to 40% of children born with a permanent hearing loss have one or more additional disabilities (ADs; Cupples et al., 2016; Gallaudet Research Institute, 2011; Picard, 2004). Understanding the achievements of this large subgroup of children is essential in order to develop a comprehensive account of expected language outcomes in the wider population of children who are deaf or hard-of-hearing (DHH). With this aim in mind, the current study examined language development from 3 to 5 years of age in a large, population-based sample of DHH children with ADs who received a hearing aid (HA) or cochlear implant (CI) prior to 3 years of age. This approach differs from that most commonly adopted in previous studies, which compared children’s performance prior to cochlear implantation with their performance at one or more time-points post-implantation, regardless of chronological age.
Language outcomes for DHH children with ADs
Previous research shows that auditory-linguistic abilities generally improve following cochlear implantation in DHH children with ADs (e.g., Beer et al., 2012; Berrettini et al., 2008; Holt & Kirk, 2005; Lee et al., 2010; Palmieri et al., 2014; Wakil et al., 2014; Waltzman et al., 2000; Yang et al., 2004). However, the use of raw scores and a primarily descriptive approach to data analysis limits the extent to which many of these studies reflect on children’s language development relative to typical, age-based expectations. Nevertheless, several findings are worth noting.
Holt and Kirk (2005) reported on 19 children with intellectual disability (ID), who were assessed at 6-monthly intervals on a battery of tests that included measures of receptive and expressive language. According to the researchers, children’s language quotients (developmental age / chronological age) showed small gains across the 3-year period of the study, although individual scores reported in the paper reveal considerable variation between participants. On the other hand, Lee et al. (2010) reported a longitudinal study of 15 DHH children with ID whose receptive and expressive language development was below expectations in the first two years post-implantation. During this period, language age improved from 15 months to just 18 months receptively, and from 15 to 24 months expressively. Finally, Beer et al. (2012) reported that, although average receptive language quotients on the Preschool Language Scale Fourth edition (PLS-4; Zimmerman et al., 2002) increased from pre- to post-cochlear-implantation for seven DHH children with ADs and seven children without ADs, expressive language quotients decreased for both groups.
Taken together, the findings from these three studies indicate the variable nature of language development post-implantation in DHH children with ADs. One factor that might contribute to this variation is the extent to which cognitive ability differs across individual children or groups of children. A number of past studies provide evidence of better language outcomes in DHH children with ADs who have higher levels of cognitive ability (e.g., Beer et al., 2012; Lee et al., 2010; Meinzen-Derr et al., 2010; Wakil et al., 2014).
Other demographic factors might also play a role in determining the rate at which language develops in these children. Cupples et al. (2016) described absolute 5-year language outcomes in a large, population-based cohort of children participating in the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study (Ching et al., 2013). Regression analyses showed that better scores on the PLS-4 were associated with higher nonverbal ability, but also with milder hearing losses, use of oral communication in early intervention, higher levels of maternal education, and earlier intervention with the child’s current audiological device (Cupples et al., 2016). In a previous investigation of 3-year-old outcomes, Cupples et al. (2014) reported that children with autism (ASD), cerebral palsy (CP), and/or developmental delay (DD) achieved significantly poorer scores on the PLS-4 than children with other disabilities (which included visual or speech impairment, syndromes not entailing DD, and medical conditions). The question arises as to whether this observed group difference is the result of variation in cognitive ability or disability type per se.
In addition to difficulties with interpreting the outcomes achieved by DHH children with ADs in relation to typical, age-based expectations, longitudinal studies in this field suffer from a number of other limitations. First, most studies included fewer than 30 participants with ADs who had usable outcome data (e.g., Beer et al., 2012; Lee et al., 2010). Second, variable follow-up periods both within and across studies complicates comparison and interpretation of longitudinal findings (e.g., Waltzman et al., 2000). Third, the use of a retrospective design in many past studies limited the data to those collected previously (e.g., Holt & Kirk, 2005; Wakil et al., 2014).
The current study
The current study addresses these perceived weaknesses while building on findings described previously by Cupples et al. (2014) in relation to the influence of disability type on absolute language outcomes. The aim was to examine longitudinal data on language development across a 2-year period for a large, population-based sample of DHH children with different types of ADs who were enrolled in the LOCHI study and assessed at both 3 and 5 years of age. The potential association between nonverbal cognitive ability and absolute language outcomes was not evaluated at 3 years due to the absence of an appropriate assessment measure in the test battery, but this omission was addressed at 5 years of age, through administration of the Wechsler Nonverbal scale of ability (WNV; Wechsler & Naglieri, 2006).
Research questions
Three research questions were addressed.
Do DHH children with different types of ADs show similar development in language skills from 3 to 5 years of age when compared to norms for typically developing peers without hearing loss?
Which demographic variables are associated with language development from 3 to 5 years of age in DHH children with ADs?
Does type of AD account for unique variance in language development after controlling for nonverbal cognitive ability?
In accordance with Cupples et al. (2014), we hypothesised first, that language development from 3- to 5-years-old would differ according to type of AD. Our second hypothesis was that, in addition to type of AD, the demographic variables identified by Cupples et al. (2016) as predicting absolute 5-year outcomes would also be associated with language development from 3 to 5. Finally, in the absence of strong evidence to the contrary, we predicted that type of AD would account for unique variance in language development after controlling for variation in nonverbal ability.
Method
Participants
Participants were members of a population-based cohort taking part in the LOCHI study. They were children born with permanent hearing loss between 2002 and 2007 in the Australian states of New South Wales, Victoria, and Queensland. All children who were diagnosed with hearing loss and presented at Australian Hearing, the government-funded hearing service provider for all children in Australia, before 3 years of age were invited to participate. The LOCHI study was approved by the Australian Hearing Ethics Committee. Parents provided written informed consent for participation. As part of the study, caregivers were asked to indicate whether their child had been diagnosed with a disability in addition to hearing loss by a qualified professional. A total of 180 children, approximately 39% of the total LOCHI population, were diagnosed with an AD by the age of 5 years. Data were available at both 3 and 5 years of age for 67 of these children. Most cases of missing data were due to children’s inability to cope with the demands of formal testing (including use of nonstandard administration, such as simultaneous communication, which combines speech with sign). In other cases, children were unavailable, unaided, or non-compliant at the time of assessment, spoke a language other than English, or had withdrawn from the study.
Types of AD.
The 67 included participants were allocated to disability subtypes according to the diagnoses they received from qualified medical professionals as reported by parents. These diagnoses were not made as part of the LOCHI study itself. The classification system was devised by Cupples et al. (2014). Each child was allocated to a single category, although diagnoses sometimes overlapped; for instance, developmental delay (DD) was reported in two children with ASD, six children with CP, and with other named disabilities or syndromes, such as Cornelia de Lange and Charge (category 4). DD was also reported as some children’s only disability (category 5). The remaining four disability subtypes encompassed disorders of vision, speech output (difficulties producing clear, fluent speech), a variety of syndromes not necessarily entailing DD, and a diverse set of medical disorders, often affecting major body organs or motor skills (see Table 1).
Table 1.
Number and percent of included participants and mean IQs according to disability
| Type of disability | n | % | IQ (n; Range) |
|---|---|---|---|
| 1. Autism Spectrum Disorder (ASD) | 6 | 9.0 | 96.4 (n=5; 90–104) |
| 2. Cerebral Palsy (CP) | 7 | 10.4 | 86.7 (n=6; 60–118) |
| 3. ASD plus CP | 1 | 1.5 | 39.0 (n=1; n/a) |
| 4. Developmental delay + syndrome(s) - not ASD or CP | 10 | 14.9 | 82.1 (n=7; 58–96) |
| 5. Developmental delay only | 5 | 7.5 | 83.5 (n=4; 65–93) |
| Disability Group A | 29 | 84.8 (n=23; 39–118) | |
| 6. Visiona | 9 | 13.4 | 109.9 (n=8; 94–128) |
| 7. Speechb | 6 | 9.0 | 101.8 (n=6; 78–118) |
| 8. Other syndromes - not entailing developmental delayc | 13 | 19.4 | 98.7 (n=11; 72–115) |
| 9. Medicald | 10 | 14.9 | 106.2 (n=9; 76–120) |
| Disability Group B | 38 | 103.9 (n=34; 72–128) |
Note. WNV scores were not available for all participants - the number of available scores is indicated in parentheses.
Category 6 contains children with a visual disability only (n = 8) or a combined visual/medical disability (n = 1). Children who had a visual disability combined with ASD, CP, DD or another syndrome were included in categories 1, 2, 3, 4 or 8 as appropriate.
Category includes children who have difficulties producing clear, fluent speech.
Category includes: Treacher-Collins (n = 3), Waardenburg (n = 2), Pendred (n = 2), OSMED, Goldenhar, Stickler, proximal symphalangism, glycogen storage disorder, and oppositional defiance disorder (n = 1 each).
Category includes disorders of the head (microcephaly), heart, kidneys, thyroid, bones, muscles, and nervous system. Microcephaly is included in this category because it is essentially a medical condition in which a baby’s head is smaller than normal (https://www.cdc.gov/ncbddd/birthdefects/microcephaly.html); and although it can be associated with developmental delay, it is not always (https://www.ninds.nih.gov/Disorders/All-Disorders/Microcephaly-Information-Page).
Also included in Table 1 are mean standard scores on the WNV (Wechsler & Naglieri, 2006). Although these scores were not used to determine group membership, they are consistent with the allocation of participants to disability groups, in that group A children (with ASD, CP, and/or DD) achieved lower average standard scores than children in group B (t (55) = 4.70, p < .001).
Table 2 presents relevant background data on included participants. The only significant group difference was in communication mode used during early intervention (χ2 = 4.259, p = .039). Group A children used more mixed communication modes than children in group B. In both groups, however, most children who were using mixed modes were reported to use speech and sign, or speech and Auslan more specifically (n = 6 for group A; n = 5 for group B). Of the remaining 5 children in group A, 3 used Makaton, 1 an AAC system, and 1 was not further specified. In group B, the sixth and final child used Makaton. Audiological information was collected from the databases of Australian Hearing and relevant intervention agencies. Hearing loss is represented as a four-frequency-average in the better ear (4FAHL). On average, children were diagnosed with a hearing loss at 5.4 months of age (SD = 7.9, range = 0 – 32), and first fitted with HAs approximately 3 months later (M = 7.9, SD = 7.8 for group A; M = 9.3, SD = 10.6 for group B; t < 1). For children using CIs, devices were first switched-on between 5 and 30 months of age (M = 15.0, SD = 6.8 for group A; M = 17.1, SD = 9.0 for group B; t < 1). In regard to spoken language, all children used English, with a small percentage (n = 6, 9.0%) using another spoken language as well.
Table 2.
Background characteristics at 5 years of age for 67 included participants according to disability group
| Disability Group | |||||
|---|---|---|---|---|---|
| Group A (ASD, CP, DD) |
Group B (Other) |
||||
| Number | (Percent) | Number | (Percent) | χ2 (p) | |
| Total participants | 29 | 38 | |||
| Gender | |||||
| Male | 18 | (62.1) | 22 | (57.9) | χ2 = 0.119 |
| Female | 11 | (37.9) | 16 | (42.1) | (p = .730) |
| Degree of hearing loss (4FAHL) | |||||
| Mild (≤ 40 dB) | 7 | (24.1) | 5 | (13.2) | χ2 = 1.882 |
| Moderate (41–60 dB) | 12 | (41.4) | 19 | (50.0) | (p = .597) |
| Severe (61–80 dB) | 5 | (17.2) | 9 | (23.7) | |
| Profound (> 80 dB) | 5 | (17.2) | 5 | (13.2) | |
| Device | |||||
| Hearing aid(s) | 24 | (82.8) | 27 | (71.1) | χ2 = 1.240 |
| Cochlear implant(s) | 5 | (17.2) | 11 | (28.9) | (p = .265) |
| Maternal Education | |||||
| University | 9 | (31.0) | 17 | (44.7) | χ2 = 3.553 |
| Certificate/diploma | 8 | (27.6) | 14 | (36.8) | (p = .169) |
| ≤ 12 years | 11 | (37.9) | 7 | (18.4) | |
| Missing data | 1 | (3.4) | 0 | (0.0) | |
| Communication mode (Early Intn) | |||||
| Oral | 18 | (62.1) | 32 | (84.2) | χ2 = 4.259 |
| Mixed (speech + sign) | 11 | (37.9) | 6 | (15.8) | (p = .039) |
Note. ASD = autism spectrum disorder; CP = cerebral palsy; DD = developmental delay; Other = disorders of vision or speech output, a variety of syndromes that do not necessarily entail DD, and a diverse set of medical disorders; 4FAHL = 4 frequency average hearing loss in the better ear at 5 years of age.
Evaluation Tools
Evaluation tools included direct assessments of receptive and expressive language and nonverbal cognitive ability. Language measures included the PLS-4 (Zimmerman et al., 2002), and the PPVT-4 (Dunn & Dunn, 2007). Nonverbal cognitive ability was assessed using the WNV (Wechsler & Naglieri, 2006).
The PLS-4 provides a formal assessment of children’s overall receptive and expressive language abilities. At 5 years of age, verbal tasks are used to evaluate children’s understanding of and ability to produce English language structures including semantics, morphology, and syntax. Interactive play, picture pointing, and verbal elicitation activities are used at 3 years of age. The PPVT-4 uses a four-alternative, forced-choice, picture-selection format to obtain a measure of children’s receptive vocabulary. For both language measures, raw scores are converted to standard scores using published normative data with a mean of 100 and SD of 15.
Nonverbal cognitive ability was assessed using the WNV, which was designed for linguistically diverse populations, including people with hearing loss. It contains four subtests, which combine to provide a full-scale IQ score (standard score with a mean of 100 and SD of 15). For children ages 4;0 – 7;11 (years;months) the relevant subtests are matrices, coding, object assembly, and recognition.
Procedure
The test batteries administered to LOCHI participants at 3 and 5 years of age included assessments of language at both time points, and nonverbal cognitive ability at 5 years only. For the current sample, PLS-4 data were collected when children were 37.3 months old on average (SD = 1.6; range = 34 – 42) and 61.7 months on average (SD = 1.6, range = 60 – 66). PPVT-4 data were collected when children were 37.6 months on average (SD = 1.8, range = 34 – 42) and 61.8 months on average (SD = 1.5, range = 60 – 66). WNVs were administered between 56 and 95 months of age, with the majority (45 out of 57 or 79%) conducted within a 1-year age bracket, from 60 to 72 months.
A team of research speech pathologists directly assessed children in a location of best convenience for the families (including homes, schools, early intervention centres, childcare centres, or Australian Hearing offices). During evaluation, children wore their HAs or CIs at the settings prescribed by their audiologist. As far as possible, research speech pathologists were blinded to children’s age of intervention and severity of hearing loss. The WNV was administered in a separate session by a professional psychologist. Tasks were administered according to instructions in their respective manuals where each child’s abilities allowed. Thus, language scores included here were obtained using oral communication only.
Reliability
Inter-rater reliability was computed for the group of participants in the larger LOCHI study. Assessments were video/audio recorded, and randomly selected samples were subjected to a second, independent scoring by a member of the research speech pathologist team who was not involved in the initial test administration or scoring. Approximately 5–10% of PLS-4 and PPVT-4 assessments administered at 3 and 5 years of age were double-scored. Agreement was uniformly high on test items administered for PLS-4 (98.6% at 3 years and 98.9% at 5 years) and PPVT-4 (98.1% at 3 years and 99.8% at 5 years).
Statistical considerations
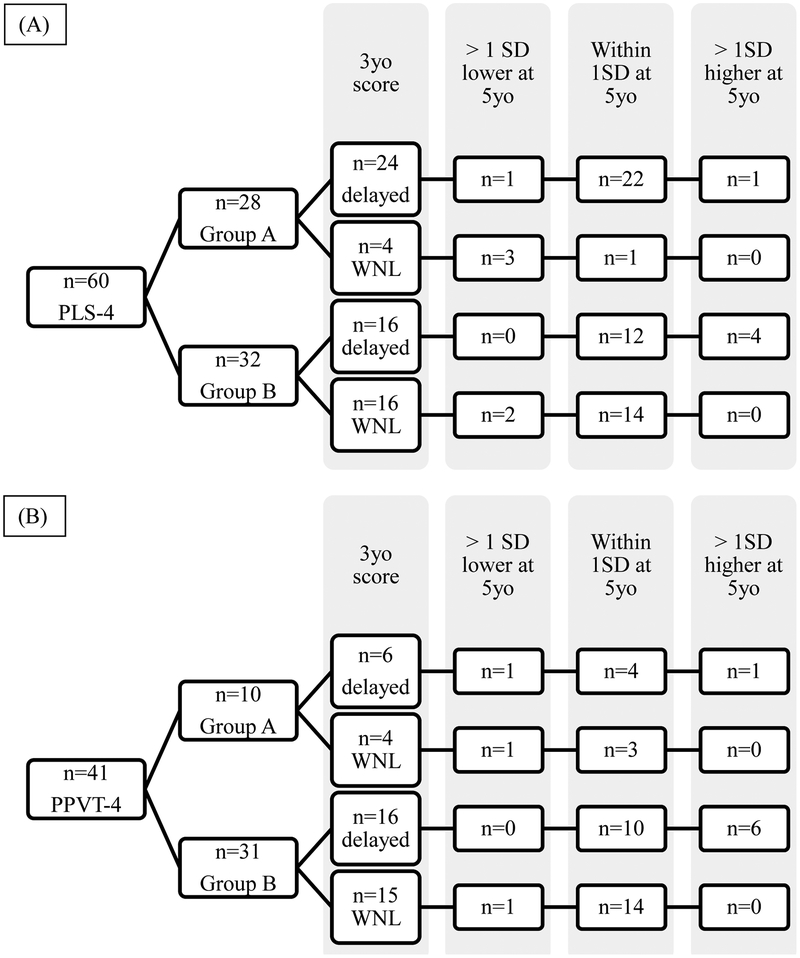
Our first hypothesis, that children’s language development would differ according to type of AD, was tested in two ways. First, the mean standard scores achieved at 3 and 5 years of age by children in each disability group were compared using a two-way, mixed-measures ANOVA. Second, individual children were classified according to how their standard scores compared at 3 and 5 years of age. Children were classified as: “improving” if their standard score at 5 exceeded their 3-year-old score by more than one SD; “declining” if their 5-year-old score was more than one SD below their 3-year-old score; and “holding steady” if their 5-year-old score was within one SD of their 3-year-old score.
Our second hypothesis concerned the variables associated with language development from 3 to 5, and was assessed using two multiple regressions. The dependent variable in each case was a 5-year-old language score (on PLS-4 or PPVT-4), and the first step in the regression analysis was to partial out performance on the same language measure at 3 years of age. Only participants with complete data (i.e., valid scores on the dependent variable and all predictors) were included in individual regression analyses. Two regression models were fitted for each dependent variable. Model 1 included three continuous and four categorical variables. The continuous variables were 3-year-old language (on PLS-4 or PPVT-4), 4FAHL, and age at audiological intervention with the current device (i.e., age at first fitting of HAs for children using HAs, and age at CI switch-on for children using CIs). The categorical variables were gender, hearing device (HA or CI), communication mode in early intervention (oral or mixed), and maternal education (recoded as two binary variables using university as the reference category). In the second model the categorical variable of disability group was added.
Our third and final hypothesis was that disability group and nonverbal cognitive ability would each account for unique variance in language development after controlling for the other. This prediction could have been tested by including both WNV and disability group as predictors in the multiple regression analyses described above. However, missing WNV data would have reduced the size of the included participant sample with a consequent reduction in power. To avoid this problem, we used four additional multiple regressions. The dependent variable was always a 5-year-old language score (PLS-4 or PPVT-4), and the first step in the regression analysis was to partial out 3-year-old performance on the same measure. Disability group and WNV standard score were then entered into each regression equation sequentially (either disability group first and nonverbal ability second, or vice versa).
A Type I error rate of α = .05 was adopted for all statistical analyses, which were performed using IBM SPSS statistics version 24.0 (IBM Corp., 2016).
Results
Table 3 shows the mean language scores achieved by children in groups A (ASD, CP, and/or DD) and B (other disabilities) at 3 and 5 years of age. The results confirm a different developmental trend for the two groups. In group A, children’s average scores dropped by approximately 5 standard score points on both language measures over the 2-year period; whereas in group B, there was a corresponding increase of 5 to 8 standard score points. The interaction between age at testing and disability group was significant in the analysis of both PLS-4 scores (F (1, 58) = 8.48, p = .005) and PPVT-4 scores (F (1, 39) = 7.74, p = .008). The main effect of age was not significant in either analysis (both Fs < 1). Despite this variation in average scores, there was a strong tendency for children who performed well at 3 years of age to also perform well at 5 years. This pattern is reflected in the generally strong positive correlations between scores attained at the two time points, the one exception being group A’s performance on the PPVT-4.
Table 3.
Mean standard scores on language measures according to age and disability group
| Assessment | n | 3yo Mean (SD) | 5yo Mean (SD) | r | p-value |
|---|---|---|---|---|---|
| PLS-4 | |||||
| Group A (ASD, CP, DD) | 28 | 64.00 (16.22) | 59.04 (13.56) | .70 | < .001 |
| Group B (other disabilities) | 32 | 85.59 (24.35) | 90.38 (17.09) | .83 | < .001 |
| PPVT-4 | |||||
| Group A (ASD, CP, DD) | 10 | 86.50 (17.12) | 80.20 (17.16) | .09 | .799 |
| Group B (other disabilities) | 31 | 85.74 (18.94) | 94.16 (14.88) | .83 | < .001 |
Note. PLS-4 = Preschool Language Scales 4th edition; PPVT-4 = Peabody Picture Vocabulary Test 4th edition.
Due to the small number of participants with PPVT-4 scores in disability group A, the correlation was repeated using the nonparametric Spearman’s rho, with no change to the results (rho = .22, p = .551).
While the data in Table 3 provide important information regarding average changes in children’s language outcomes, they do not indicate how many children developed language at a level commensurate with, above, or below the normative sample. This question was investigated by assigning children to subgroups according to their difference scores on each language outcome (see figure 1). In around 75 to 80% of cases on average, children’s 5-year-old scores were “holding steady” (i.e., within 1SD of their 3-year-old scores). This pattern was evident for children in group A (with ASD, CP, and/or DD) and group B (with other disabilities). There was, however, an apparent group difference in the frequency with which members of the two disability groups were classified as “improving” or “declining.” Averaging across the two language outcome measures, 17.2% of group A children attained a 5-year-old score more than 1 SD below their 3-year-old score (declining), whereas the corresponding figure for group B was just 4.8%. On the other hand, approximately 16.0% of group B children scored more than 1 SD higher at 5 than at 3 years of age (improving), compared to just 6.8% of children in Group A.
Figure 1.
Number of children whose standard scores on the PLS-4 (A) and the PPVT-4 (B) declined, held steady, or improved from 3 to 5 years of age according to disability group and 3-year-old scores. (Note. Group A = ASD, CP, and/or DD; Group B = other disabilities; delayed = more than 1 SD below the mean; WNL = within or above 1 SD of the mean.)
The second primary aim of this research was to investigate the predictors of language development. Summary results from two multiple regressions, are presented in Table 4. The outcome measures were scores obtained on the PLS-4 and PPVT-4 at 5 years of age. Three-year-old scores were included in the regression models as covariates. The results show first, that children’s language scores at 3 years of age were highly predictive of their scores at 5 years. They also show that greater improvements in spoken language outcomes are associated with an absence of group A disabilities (ASD, CP, DD) and use of an oral only communication mode (especially, for receptive vocabulary).
Table 4.
Summary table for multiple regressions predicting language development from 3 to 5 years of age
| Language outcome measure | ||||
| PLS-4 @ 5yo | PPVT-4 @ 5yo | |||
| R2 change for model 2 (significance) | ||||
| PLS-4 or PPVT-4 @ 3yoa | .67 (< .001) | .35 (< .001) | ||
| Gender, 4FAHL, MatEd, Mode, Device, AgeHAorCI | .03 (.567) | .30 (.004) | ||
| Disability Group | .12 (< .001) | .04 (.050) | ||
| Total R2 | .83 (< .001) | .70 (< .001) | ||
| N | 60 | 40 | ||
| Regression coefficients (significance) | ||||
| Model 1 | Model 2 | Model 1 | Model 2 | |
| PLS-4 or PPVT-4 @ 3yoa | 0.699 (< .001) | 0.538 (< .001) | 0.513 (< .001) | 0.509 (< .001) |
| Gender | 1.789 (.640) | −0.100 (.973) | 7.932 (.048) | 6.733 (.080) |
| 4FA HL | −0.005 (.972) | −0.044 (.689) | −0.159 (.224) | −0.144 (.249) |
| Mat Ed (ref: university) | ||||
| Certificate/diploma | 3.968 (.361) | 1.999 (.555) | 4.921 (.260) | 3.548 (.398) |
| ≤ 12 years | −4.734 (.326) | −2.575 (.493) | −0.305 (.952) | −1.899 (.697) |
| Mode (ref: oral) | −4.088 (.068) | −2.417 (.168) | −9.900 (.001) | −8.945 (.002) |
| Device (HA or CI) | −1.495 (.845) | −1.354 (.820) | 4.572 (.455) | 3.328 (.570) |
| AgeHAorCI | −0.014 (.942) | −0.037 (.802) | 0.241 (.191) | 0.121 (.508) |
| Disability Group | ----b | 17.99 (< .001) | ----b | 9.255 (.050) |
Note. PLS-4 = Preschool Language Scales 4th edition; PPVT-4 = Peabody Picture Vocabulary Test 4th edition; Bold font indicates p < .05; 4FA HL = four-frequency average hearing loss in the better ear; Mode = Communication mode in early intervention; MatEd = Maternal education (coded as two binary variables using university education as the reference category); AgeHAorCI = Age of intervention with current device; Disability Group = Group A (ASD, CP, DD) versus Group B (other disabilities).
To predict language development from 3 to 5 years of age, 5-year-old scores on a given measure served as the dependent variable and 3-year-old scores on the same measure were partialled out at step one.
Disability group was not included in model 1.
Finally, four multiple regressions addressed the third research question, concerning whether effects of disability group on language outcome could be explained by variation in nonverbal IQ. Two predictors, WNV standard score and disability group, were entered sequentially after partialling out the variance associated with 3-year-old outcomes on the same language measure. Both predictors, when entered first, accounted for significant variance in language development. Disability group accounted for 13% of variance in PLS-4 scores (p < .001) and 15% in PPVT-4 scores (p = .003). WNV accounted for 8% of variance in PLS-4 scores (p < .001) and 20% in PPVT-4 scores (p = .001). The results were less clear when predictors were entered into the regression equation second. When entered after WNV, disability group accounted for 7% of additional variance in PLS-4 scores (p < .001) but only a marginally significant 5% in PPVT-4 scores (p = .050). When WNV was entered after disability group, it accounted for just 2% of variance in PLS-4 scores (p = .016), compared to 10% in PPVT-4 scores (p = .010).
Discussion
The aims of this research were: first, to describe language development over a 2-year period, from 3 to 5 years of age, in a population-based sample of DHH children with ADs; second, to identify the variables associated with language development in this participant sample; and third, to determine whether type of AD would account for unique variance in language development after controlling for variation in nonverbal cognitive ability. Two directly administered standardised assessments of receptive and expressive language (PLS-4) and receptive vocabulary (PPVT-4) were used to measure the development of children’s language skills relative to published norms.
With regard to the first aim, there was no significant change in average language test scores from 3 to 5 years of age for the total cohort of children with ADs. As predicted, however, children with different types of ADs show different developmental trends. Average language scores for children with ASD, CP, and/or DD declined in comparison to norms for typically developing peers, whereas average scores for children with other disabilities improved. These findings are consistent with those reported by Cupples et al. (2014), which showed that children with different types of ADs attained different absolute language outcomes at 3 years of age. They suggest that differences between previous published studies might be due partly to the inclusion of participant samples that vary with respect to their ratio of different disability types. Certainly, had the nature of children’s ADs not been considered in the current research, our conclusions would have been very different. Furthermore, the finding that a subgroup of DHH children with ADs show signs of “catching up” to their typically developing peers stands in contrast to frequent suggestions in the literature that these children generally develop language skills more slowly than expected (e.g., Waltzman et al., 2000).
In regard to the second aim, of identifying the child- and family-related variables that predict language development in DHH children with ADs, the results were partly consistent with our hypothesis. Disability group accounted for a significant 12% of variance in PLS-4 scores; and a similar, but weaker, association was evident for PPVT-4 scores, with 4.2% of variance explained (p = .050). However, of the child- and family-related variables that predicted absolute 5-year language outcomes in Cupples et al. (2016), only communication mode predicted language development from 3 to 5 here; and then, only for the PPVT-4.
In interpreting these findings, we consider first why the effect of disability group was stronger in the analysis of outcomes for PLS-4 than PPVT-4. This difference might reflect a reduction of power in the analysis of PPVT-4 scores, brought about by the smaller number of participants with complete data, and/or the imbalance in participant numbers across disability groups; in particular, that the number of participants with complete PPVT-4 data was smaller in the group of children with ASD, CP and/or DD than the group with other disabilities (see figure 1). Interestingly, Donaldson et al. (2004) reported a similar difficulty with the PPVT-4 for children with ASD in particular, with only 2 of their 7 participants able to complete the test. We infer, therefore, that the PLS-4 provides a better measure of language ability in this population at this age.
Another factor that might have contributed to the somewhat unexpected results lies in our use of previous findings for absolute 5-year-old outcomes to arrive at hypotheses for development. Palmieri et al. (2012) suggested that improvements shown post-CI could be less influenced than absolute scores by factors such as IQ and age. This suggestion is consistent with our finding of fewer significant predictors here than for absolute 5-year-old outcomes described previously (Cupples et al., 2016).
Nevertheless, one predictor variable was significant in regression analyses of PPVT-4 outcomes. Children using oral communication only in early intervention showed an advantage over children using mixed mode (typically speech plus sign). Although a causal interpretation cannot be attributed to this association, it is in the expected direction given that the ability to recognise and assign meaning to spoken words constitutes an essential component of oral communication.
In regard to the third and final aim, our hypothesis was confirmed, in that type of AD accounted for unique variance in language scores, most notably on the PLS-4, after controlling for nonverbal ability. This result presumably reflects the fact that some diagnoses, such as ASD and CP, involve aspects other than (or in addition to) cognitive delay. It provides some support for including both disability type and nonverbal ability in subsequent studies of language development in DHH children with ADs. However, given the marginal significance of the current results for receptive vocabulary, future research is recommended to confirm the independent contributions of these variables to language development.
Clinical Implications
The current findings underscore the importance of acknowledging the nature of a child’s AD in predicting whether s/he might achieve a typical trajectory in language development from 3 to 5 years of age. They also point to the necessity of providing extra support for children with ADs in order to optimise language outcomes, support that will vary from child to child and depend on the establishment of effective collaborations among relevant professionals with specialist knowledge of particular disability types. Finally, the finding that nonverbal ability or type of AD can be used to predict language development suggests that type of AD provides a useful additional, or alternative, predictor of expected language development in this population.
Strengths and Limitations
When compared to previous studies, the current research has a number of strengths, including: a large sample of 67 children, with a diverse range of ADs, all of whom were assessed at the same ages with a consistent 2-year gap. However, 180 LOCHI children were diagnosed with an AD by 5 years of age, and missing data mean that our conclusions are based on results from less than half of that larger cohort. Furthermore, missing data were not evenly spread across children with different types of ADs, resulting in potential bias. Any conclusions must be tempered in light of these limitations.
Conclusion
In conclusion, DHH children with ADs differ in the extent to which they show a typical trajectory of language development from 3 to 5 years of age. Children with ASD, CP, and/or DD showed an average decline in language ability relative to norms, whereas children with other disabilities showed an average improvement. The results suggest that type of AD can be used to gauge expected language development in this population when formal assessment of cognitive ability is not feasible. Findings also suggest an association between use of oral only communication and enhanced development of receptive spoken vocabulary, although the nature of any causal link between these variables cannot be inferred.
Footnotes
Conflict of interest statement
We have no conflicts of interest to disclose.
References
- Beer J, Harris MS, Kronenberger WG, Holt RF, & Pisoni DB (2012). Auditory skills, language development, and adaptive behaviour of children with cochlear implants and additional disabilities. International Journal of Audiology, 51, 491–498. DOI: 10.3109/14992027.2012.664291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrettini S, Forli F, Genovese E, Santarelli R, Arslan E, et al. (2008). Cochlear implantation in deaf children with associated disabilities: challenges and outcomes. International Journal of Audiology, 47, 199–208. DOI: 10.1080/14992020701870197 [DOI] [PubMed] [Google Scholar]
- Ching TYC, Dillon H, Marnane V, Hou S, Day J, et al. (2013). Outcomes of early- and late-identified children at 3 years of age: findings from a prospective population-based study. Ear and Hearing, 34, 535–552. DOI: 10.1097/AUD.0b013e3182857718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cupples L, Ching TYC, Crowe K, Seeto M, Leigh G, et al. (2014). Outcomes of 3-year-old children with hearing loss and different types of additional disabilities. Journal of Deaf Studies and Deaf Education, 19, 20–39. DOI: 10.1093/deafed/ent039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cupples L, Ching TYC, Button L, Leigh G, Marnane V, Whitfield J, Gunnourie M, & Martin L (2016). Language and speech outcomes of children with hearing loss and additional disabilities: Identifying the variables that influence performance at 5 years of age. International Journal of Audiology. First published online September 14 2016. DOI: 10.1080/14992027.2016.1228127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson AI, Heavner KS, & Zwolan TA (2004). Measuring progress in children with Autism Spectrum Disorder who have cochlear implants. JAMA Otolaryngology - Head & Neck Surgery, 130, 666–671. DOI: 10.1001/archotol.130.5.666 [DOI] [PubMed] [Google Scholar]
- Dunn LM, & Dunn DM (2007). Peabody Picture Vocabulary Test (4th ed.). Minneapolis, MN: Pearson Assessments. [Google Scholar]
- Gallaudet Research Institute (2011). Regional and national summary report of data from the 2009–10 annual survey of deaf and hard of hearing children and youth. Washington, DC: GRI, Gallaudet University; Retrieved from: http://research.gallaudet.edu/Demographics/2010_National_Summary.pdf [Google Scholar]
- Holt R, & Kirk KI (2005). Speech and language development in cognitively delayed children with cochlear implants. Ear and Hearing, 26, 132–148. [DOI] [PubMed] [Google Scholar]
- Corp IBM. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp. [Google Scholar]
- Lee Y-M, Kim L-S, Jeong S-W, Kim J-S, & Chung S-H (2010). Performance of children with mental retardation after cochlear implantation: Speech perception, speech intelligibility, and language development. Acta Otolaryngology, 130, 924–934. DOI: 10.3109/00016480903518026 [DOI] [PubMed] [Google Scholar]
- Meinzen-Derr J, Wiley S, Grether S, & Choo DI (2010). Language performance in children with cochlear implants and additional disabilities. Laryngoscope, 120, 405–413. DOI: 10.1002/lary.20728 [DOI] [PubMed] [Google Scholar]
- Palmieri M, Berrettini S, Forli F, Trevisi P, Genovese E, et al. (2012). Evaluating benefits of cochlear implantation in deaf children with additional disabilities. Ear and Hearing, 33, 721–730. DOI: 10.1097/AUD.0b013e31825b1a69 [DOI] [PubMed] [Google Scholar]
- Palmieri M, Forli F, & Berrettini S (2014). Cochlear implantation outcome for deaf children with additional disabilities: A systematic review. Hearing Balance and Communication, 12, 6–19. DOI: 10.3109/21695717.2014.883205 [DOI] [Google Scholar]
- Picard M (2004). Children with permanent hearing loss and associated disabilities: Revisiting current epidemiological data and causes of deafness. Volta Review, 104, 221–236. [Google Scholar]
- Wakil N, Fitzpatrick EM, Olds J, Schramm D, & Whittingham J (2014). Long-term outcome after cochlear implantation in children with additional developmental disabilities. International Journal of Audiology, 53, 587–594. DOI: 10.3109/14992027.2014.905716 [DOI] [PubMed] [Google Scholar]
- Waltzman SB, Scalchunes V, & Cohen NL (2000). Performance of multiply handicapped children using cochlear implants. American Journal of Otology, 21, 329–335. [DOI] [PubMed] [Google Scholar]
- Wechsler D, & Naglieri JA (2006). Wechsler Nonverbal Scale of Ability. San Antonio, TX: PsychCorp. [Google Scholar]
- Yang H-M, Lin C-Y, Chen Y-J, & Wu J-L (2004). The auditory performance in children using cochlear implants: effects of mental function. Int J Pediatr Otorhinolaryngol, 68, 1185–1188. DOI: 10.1016/j.ijporl.2004.04.011 [DOI] [PubMed] [Google Scholar]
- Zimmerman IL, Steiner VG, & Pond RE (2002). Preschool Language Scale (4th ed.). San Antonio, TX: The Psychological Corporation. [Google Scholar]