Abstract
Objective/Background
Improvements in curative treatments for many types of cancer have emerged over the past several decades, resulting in a growing population of long-term cancer survivors—of both adult and childhood cancers. Despite this incredible medical achievement, long-term survivors of cancer face a unique fear: the fear of relapse.
Methods
We conducted a review of the literature for data on fear of relapse among cancer survivors.
Results
The fear of cancer recurrence is present in survivors of childhood and adult cancers as well as family members and often leads to psychological sequelae.
Conclusion
Literature on the fear of cancer recurrence has begun to emerge. However, herein we provide a unique approach through the use of a metaphor: Cicero’s story of Damocles’ sword. We aim to outline the many fear-related and emotional challenges faced by cancer survivors with an extensive review of studies demonstrating such challenges.
Keywords: anxiety, cancer, fear of recurrence, relapse, survivorship
Introduction
The Roman philosopher Cicero wrote about Dionysus, the tyrant king of Syracuse. In one story, the courtier Damocles expresses his belief that Dionysus is the most fortunate man in the world. Wishing to teach him a lesson, Dionysus allows Damocles to sit on his throne, giving him all of his riches. In the midst of Damocles’ enjoyment, Dionysus suspends a sword over Damocles’ neck, dangling by a single horsehair. Preoccupied with the danger of the sword, Damocles is no longer able to enjoy the beauty around him. No longer wishing to be so fortunate, he begs Dionysus to take back his throne.
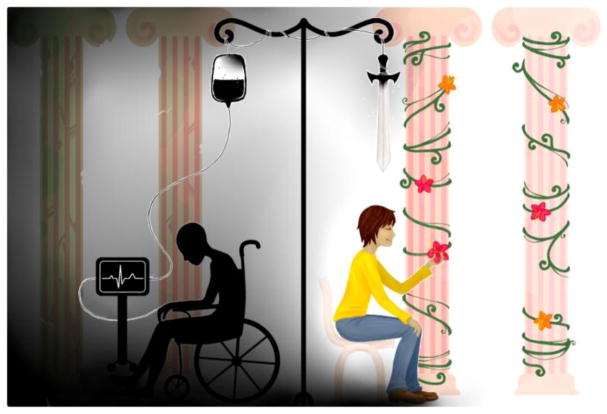
For Damocles, great fortune was not worth the unrelenting fear that accompanied it. Damocles’ outlook is shared today by many, particularly survivors of childhood or adult cancers. The “mixed blessings” consequences faced by survivors of childhood cancer were first described using the story of “Damocles’ Sword” as an analogy in the early 1980s.1 Survivors are given a new lease on life, but also persisting fears of recurrence, subsequent malignancies, and long-term health sequelae after cancer treatment. The cancer survivor experiences hope and celebration as well as uncertainty, fear, and hypervigilance to new symptoms.2 New cancer treatments and increasing recommendations for watchful waiting in lieu of active treatment leave even more survivors with Damocles’ view of their futures (Figure 1).
Figure 1.
An artistic depiction of a cancer survivor who lives in the constant shadow of a previous cancer diagnosis.
Childhood cancer survivors
Awareness of this phenomenon—what we call the “Damocles’ sword effect” (DSE)—is pertinent due to an increasing number of survivors previously treated for childhood and adolescent cancer. According to a 2014 report,3 the overall survival rate for all childhood and adolescent cancers is nearly 85%. It is now both possible and imperative to focus on quality of life (QoL) among these survivors. In 1998, the American Cancer Society Task Force on Children and Cancer reported, “the progress achieved in attaining 80% survival among children and adolescents and young adults with cancer can be justified only if their physical, emotional, and social QoL also are protected.”4 We agree with this statement. Previous reports have summarized many of the hardships faced by survivors of childhood and adolescent cancer as they age.5–8 These include lack of follow-up care, long-term health sequelae, and psychosocial challenges.
While many studies have attempted to quantify the mental health disparities among childhood and adolescent cancer survivors using surveys, no known studies have specifically addressed the association of the fear of recurrence (FoR) with health-related sequelae among childhood cancer survivors. Data from many studies imply the presence of the DSE. A meta-analysis of studies addressing psychosocial adjustment among adolescent survivors of pediatric cancer suggested that increased anxiety existed in this population due to FoR.9 Multiple studies have found post-traumatic stress disorder (PTSD) to be more prevalent among survivors of pediatric cancer.10 Compared with controls, greater anxiety and depression exist among pediatric cancer patients following completion of cancer therapies, with higher rates after the end of therapy than during treatment.11 Anxiety disorders are also significantly more common among long-term survivors of cancer during adolescence.12 Compared with their siblings, survivors of childhood leukemia and lymphoma have significantly increased risk of depression and somatic distress.13 Survivors of childhood cancer also have increased rates of suicidal ideation, anxiety, and global distress.14
This picture is complicated due to conflicting data. Many survivors of childhood cancer appear to be psychologically similar to healthy controls. Psychological QoL is reportedly similar between survivors and sibling controls in all areas except in physical domains.15 Certain subsets of the survivor population may be more susceptible to the DSE than others. A study of young adult cancer survivors found 16% of survivors to have PTSD.16 Another study found that most survivors lead “normal adult lives,” while a small subset demonstrates anxiety, depression, and/or FoR or a subsequent malignancy.17 These sequelae were associated with female sex, lower socioeconomic status, unemployment, and poor education.17
A study of the psychological consequences of surviving childhood cancer concluded that psychological outcome was only impacted among certain groups, including bone and brain malignancies.18 This might be due to the length of therapy required for these types of cancer when compared with others, such as Hodgkin’s lymphoma. Survivors diagnosed as adolescents have significantly greater psychological distress than those diagnosed at a younger age.19 Adult survivors of childhood cancer are at increased risk for suicidal ideation.20 These findings suggest that the consequences of living with uncertainty go well beyond FoR.
Studies of childhood cancer survivors have identified subsets of survivors with psychological and social difficulties many years beyond completion of therapy, stemming from PTSD, impaired self-esteem/body image, and employment/health insurance discrimination.2 Although some data indicate that many survivors of childhood cancer grow in positive ways from their experiences with cancer and are psychologically well adjusted, even these survivors express concerns about the potential for recurrence or other late complications of their treatments.
Despite a mixed picture of psychological outcomes, children with cancer benefit from comprehensive behavioral support in the form of psychiatry, psychology, child life therapy, education, chaplaincy, social work, and career counseling.21 Children who survive cancer and their families must undergo a unique transition and period of psychosocial adaptation,21 with needs that may reawaken anxiety and worry at future developmental points in their lives.
Family stress reactions
Apart from survivors of childhood and adolescent cancer themselves, families—including parents and siblings—are greatly impacted by the shift in lifestyle necessitated by pediatric cancer. Adolescent survivors of childhood malignancies have lower levels of family cohesion than controls.22 The cancer patient’s needs and QoL become a preoccupation and priority for many parents.23 Both mothers and fathers of children newly diagnosed with cancer report significantly altered perceptions of self and family functioning when compared with controls.24 Marriages are often altered. The prevalence of PTSD among mothers of pediatric cancer survivors has been compared with that of mothers of children without chronic illnesses.25 More than half (54%) of the mothers of survivors had lifetime diagnosis of PTSD, compared with 4% among the control group. Interviews reflected that the PTSD resulted from the stress associated with parenting a child with cancer.
Siblings also struggle. Children with siblings with chronic illnesses have more behavioral problems.26 As parents dedicate increased time and attention to the patient, many siblings of cancer patients develop conduct problems, psychosomatic problems, and behavioral issues within 3 months of diagnosis.27 Even 2 years after diagnosis, siblings of cancer patients demonstrate reduced QoL compared with age-matched controls, reporting emotions of fear, isolation, jealousy, and guilt.28
Adult cancer survivors
Although the Damocles’ effect was originally described in pediatric cancer survivors, survivors of adult cancers face similar challenges in living with uncertainty and fear. The most abundant data on FoR are found among breast cancer survivors, in which FoR is highly prevalent and has a negative impact on QoL. The prevalence of PTSD among survivors of breast cancer is elevated.29 A systematic review found that up to 32.3% of patients with breast cancer develop PTSD.30 In a multicenter study of 2,671 women evaluated for FoR, 99% of women reported FoR.31 Substantial proportions experienced moderate (11%) and high (6%) FoR. Higher FoR was associated with both depression and poorer QoL.
A systematic review of quantitative studies concluded that adult cancer survivors consider FoR as one of their top concerns and the most frequently endorsed unmet need.32 Because of significant advancements in cancer therapeutics, certain adult cancers are now considered to be chronic diseases rather than life-threatening or terminal diagnoses.33 Chronic myelogenous leukemia and multiple myeloma, in particular, can be treated by targeted therapies with relatively few side effects.34 Despite a near normal lifespan in the majority of these survivors, there are no data regarding their FoR. There are, however, data regarding the development of PTSD among survivors of hematological malignancies.35 A relationship exists between FoR and the development of PTSD in this population. Evaluation of FoR along with QoL should thus be one of the priorities of survivorship research across survivors of all cancers.
Keeping the sword at bay: coping mechanisms
Because of many clinicians’ familiarity with the phenomenon of FoR among cancer survivors, an increasing number of investigations have addressed coping mechanisms for patients who suffer from the DSE. Listed in Table 1, these coping mechanisms can be thought of as strategies to remove the sword that hangs over the patient—or at least keep the sword at bay.
Table 1.
Tools for Coping with Damocles’ Sword Syndrome
| Type of Intervention | |
|---|---|
| Psychological interventions | Cognitive behavioral therapy
|
| Cognitive-existential therapy | |
| Group therapy | |
| Pharmacological interventions | Selective serotonin reuptake inhibitors
|
Serotonin and norepinephrine reuptake inhibitors
| |
Tricyclic antidepressants
| |
Antiepileptics
| |
Atypical neuroleptic agents
| |
| Complementary and alternative interventions | Treatments
|
Practices
|
|
Studies on both the general population and cancer patients specifically have proven the efficacy of cognitive behavioral therapy (CBT) in treating anxiety. CBT is a type of psychological therapy that has been utilized for a range of symptoms and emotional distress among cancer patients both during and after the end of treatment.36 It has also been studied as a treatment for FoR. In a recent randomized controlled trial among survivors of breast, prostate, and colorectal cancers, CBT significantly reduced cancer anxiety among 29% of recipients.37 This type of therapy has also been successful in treating anxiety and PTSD among childhood and adolescent cancer survivors of every age.38
When FoR contributes to an anxiety disorder, pharmacological treatments may be needed as well. Although CBT has received the most empirical support for the treatment of anxiety disorders, combining pharmacological treatments with psychological treatment is thought to be even more effective.39 The first line of pharmacological therapy for anxiety is typically a selective serotonin reuptake inhibitor. Serotonin and norepinephrine reuptake inhibitors are often used after failure or inadequate response to a selective serotonin reuptake inhibitor. If these options are ineffective, other medications may be helpful (Table 1).40
Additional nonpharmacological treatments and practices may be particularly useful for patients with FoR, as they often contribute to empowerment, confidence, and mindfulness (Table 1).
Conclusion
Improved cancer survival in the current era of immunotherapies and personalized medicine without long-term data on outcomes in both pediatric and adult cancers are driving a revolution in the cancer survivorship paradigm. This increased longevity comes with a price of escalating rates of certain late effects, particularly psychosocial comorbidities. This review focuses on the DSE, related to FoR, but extending beyond recurrence to the other uncertain consequences after survival is uncharted territory. There are many useful coping mechanisms that are helpful in treating patients with FoR, including but not limited to CBT. These tools should be provided to patients as soon as possible to keep Damocles’ sword at bay. In the current era of patient-centered care, it is imperative that the scientific and clinical communities study and provide solutions for all issues on survivorship health, including FoR, so that Damocles’ sword does not hang over the lives of millions of cancer survivors.
Acknowledgments
The featured original artwork was designed, drafted, and digitally created by Courtney Cittadino Link.
Footnotes
Conflicts of interest statement
There are no conflicts of interest to disclose from any authors.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Koocher GP, O’Malley JE. The Damocles syndrome: psychosocial consequences of surviving childhood cancer. New York: McGraw-Hill; 1981. [Google Scholar]
- 2.Zebrack BJ, Zeltzer LK. Living beyond the sword of Damocles: surviving childhood cancer. Expert Rev Anticancer Ther. 2001;1:163–4. doi: 10.1586/14737140.1.2.163. [DOI] [PubMed] [Google Scholar]
- 3.Ward E, DeSantis C, Robbins A, Kohler B, Jemal A. Childhood and adolescent cancer statistics, 2014. CA Cancer J Clin. 2014;64:83–103. doi: 10.3322/caac.21219. [DOI] [PubMed] [Google Scholar]
- 4.Haase GM, Mauer AM, Reaman GH. Survivorship in childhood cancer: a case statement for enhancement of the role of the American Cancer Society. Task Force on Children and Cancer of the American Cancer Society. Cancer. 1998;83:821–3. doi: 10.1002/(sici)1097-0142(19980815)83:4<821::aid-cncr29>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 5.Cupit MC, Duncan C, Savani BN, Hashmi SK. Childhood to adult transition and long-term follow-up after blood and marrow transplantation. Bone Marrow Transplant. 2016;51:176–81. doi: 10.1038/bmt.2015.228. [DOI] [PubMed] [Google Scholar]
- 6.Huang IC, Brinkman TM, Armstrong GT, Leisenring W, Robison LL, Krull KR. Emotional distress impacts quality of life evaluation: a report from the Childhood Cancer Survivor Study. J Cancer Surviv. 2017;11:309–19. doi: 10.1007/s11764-016-0589-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yeh JM, Hanmer J, Ward ZJ, Leisenring WM, Armstrong GT, Hudson MM, et al. Chronic conditions and utility-based health-related quality of life in adult childhood cancer survivors. J Natl Cancer Inst. 2016:108. doi: 10.1093/jnci/djw046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Phillips SM, Padgett LS, Leisenring WM, Stratton KK, Bishop K, Krull KR, et al. Survivors of childhood cancer in the United States: prevalence and burden of morbidity. Cancer Epidemiol Biomarkers Prev. 2015;24:653–63. doi: 10.1158/1055-9965.EPI-14-1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McDonnell G, Baily C, Schuler T, Verdeli H. Anxiety among adolescent survivors of pediatric cancer: a missing link in the survivorship literature. Palliat Support Care. 2015;13:345–9. doi: 10.1017/S1478951514000297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bruce M. A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clin Psychol Rev. 2006;26:233–56. doi: 10.1016/j.cpr.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 11.von Essen L, Enskar K, Kreuger A, Larsson B, Sjoden PO. Self-esteem, depression and anxiety among Swedish children and adolescents on and off cancer treatment. Acta Paediatr. 2000;89:229–36. doi: 10.1080/080352500750028889. [DOI] [PubMed] [Google Scholar]
- 12.Seitz DC, Besier T, Debatin KM, Grabow D, Dieluweit U, Hinz A, et al. Posttraumatic stress, depression and anxiety among adult long-term survivors of cancer in adolescence. Eur J Cancer. 2010;46:1596–606. doi: 10.1016/j.ejca.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Zebrack BJ, Zeltzer LK, Whitton J, Mertens AC, Odom L, Berkow R, et al. Psychological outcomes in long-term survivors of childhood leukemia, Hodgkin’s disease, and non-Hodgkin’s lymphoma: a report from the Childhood Cancer Survivor Study. Pediatric. 2002;110:42–52. doi: 10.1542/peds.110.1.42. [DOI] [PubMed] [Google Scholar]
- 14.Bitsko MJ, Cohen D, Dillon R, Harvey J, Krull K, Klosky JL. Psychosocial late effects in pediatric cancer survivors: a report from the Children’s Oncology Group. Pediatr Blood Cancer. 2016;63:337–43. doi: 10.1002/pbc.25773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zeltzer LK, Recklitis C, Buchbinder D, Zebrack B, Casillas J, Tsao JC, et al. Psychological status in childhood cancer survivors: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2009;27:2396–404. doi: 10.1200/JCO.2008.21.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rourke MT, Hobbie WL, Schwartz L, Kazak AE. Posttraumatic stress disorder (PTSD) in young adult survivors of childhood cancer. Pediatr Blood Cancer. 2007;49:177–82. doi: 10.1002/pbc.20942. [DOI] [PubMed] [Google Scholar]
- 17.Massimo L, Zarri D, Caprino D. Psychosocial aspects of survivors of childhood cancer or leukemia. Minerva Pediatr. 2005;57:389–97. [PubMed] [Google Scholar]
- 18.Eiser C, Hill JJ, Vance YH. Examining the psychological consequences of surviving childhood cancer: systematic review as a research method in pediatric psychology. J Pediatr Psychol. 2000;25:449–60. doi: 10.1093/jpepsy/25.6.449. [DOI] [PubMed] [Google Scholar]
- 19.Kazak AE, Derosa BW, Schwartz LA, Hobbie W, Carlson C, Ittenbach RF, et al. Psychological outcomes and health beliefs in adolescent and young adult survivors of childhood cancer and controls. J Clin Oncol. 2010;28:2002–7. doi: 10.1200/JCO.2009.25.9564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Recklitis CJ, Diller LR, Li X, Najita J, Robison LL, Zeltzer L. Suicide ideation in adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2010;28:655–61. doi: 10.1200/JCO.2009.22.8635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Askins MA, Moore BD., 3rd Psychosocial support of the pediatric cancer patient: lessons learned over the past 50 years. Curr Oncol Rep. 2008;10:469–76. doi: 10.1007/s11912-008-0072-1. [DOI] [PubMed] [Google Scholar]
- 22.Rait DS, Ostroff JS, Smith K, Cella DF, Tan C, Lesko LM. Lives in a balance: perceived family functioning and the psychosocial adjustment of adolescent cancer survivors. Fam Process. 1992;31:383–97. doi: 10.1111/j.1545-5300.1992.00383.x. [DOI] [PubMed] [Google Scholar]
- 23.Giammona AJ, Malek DM. The psychological effect of childhood cancer on families. Pediatr Clin North Am. 2002;49:1063–81. x. doi: 10.1016/s0031-3955(02)00036-6. [DOI] [PubMed] [Google Scholar]
- 24.Pai AL, Greenley RN, Lewandowski A, Drotar D, Youngstrom E, Peterson CC. A meta-analytic review of the influence of pediatric cancer on parent and family functioning. J Fam Psychol. 2007;21:407–15. doi: 10.1037/0893-3200.21.3.407. [DOI] [PubMed] [Google Scholar]
- 25.Pelcovitz D, Goldenberg B, Kaplan S, Weinblatt M, Mandel F, Meyers B, et al. Posttraumatic stress disorder in mothers of pediatric cancer survivors. Psychosomatics. 1996;37:116–26. doi: 10.1016/S0033-3182(96)71577-3. [DOI] [PubMed] [Google Scholar]
- 26.Lavigne JV, Ryan M. Psychologic adjustment of siblings of children with chronic illness. Pediatrics. 1979;63:616–27. [PubMed] [Google Scholar]
- 27.Lahteenmaki P, Sjoblom J, Korhonen T, Salmi T. The siblings of childhood cancer patients need early support: a follow up study over the first year. Arch Dis Child. 2004;89:1008–13. doi: 10.1136/adc.2002.012088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Houtzager BA, Grootenhuis MA, Caron HN, Last BF. Quality of life and psychological adaptation in siblings of paediatric cancer patients, 2 years after diagnosis. Psychooncology. 2004;13:499–511. doi: 10.1002/pon.759. [DOI] [PubMed] [Google Scholar]
- 29.Kwakkenbos L, Coyne JC, Thombs BD. Prevalence of posttraumatic stress disorder (PTSD) in women with breast cancer. J Psychosom Res. 2014;76:485–6. doi: 10.1016/j.jpsychores.2014.03.103. [DOI] [PubMed] [Google Scholar]
- 30.Arnaboldi P, Riva S, Crico C, Pravettoni G. A systematic literature review exploring the prevalence of post-traumatic stress disorder and the role played by stress and traumatic stress in breast cancer diagnosis and trajectory. Breast Cancer (Dove Med Press) 2017;9:473–85. doi: 10.2147/BCTT.S111101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koch L, Bertram H, Eberle A, Holleczek B, Schmid-Hopfner S, Waldmann A, et al. Fear of recurrence in long-term breast cancer survivors—still an issue. Results on prevalence, determinants, and the association with quality of life and depression from the cancer survivorship—a multi-regional population-based study. Psychooncology. 2014;23:547–54. doi: 10.1002/pon.3452. [DOI] [PubMed] [Google Scholar]
- 32.Simard S, Thewes B, Humphris G, Dixon M, Hayden C, Mireskandari S, et al. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv. 2013;7:300–22. doi: 10.1007/s11764-013-0272-z. [DOI] [PubMed] [Google Scholar]
- 33.Faiman B, Faiman M. Living with hematologic cancer: recommendations, solutions. Cleve Clin J Med. 2017;84:528–34. doi: 10.3949/ccjm.84a.15159. [DOI] [PubMed] [Google Scholar]
- 34.Hochhaus A. Educational session: managing chronic myeloid leukemia as a chronic disease. Hematology Am Soc Hematol Educ Program. 2011;2011:128–35. doi: 10.1182/asheducation-2011.1.128. [DOI] [PubMed] [Google Scholar]
- 35.Black EK, White CA. Fear of recurrence, sense of coherence and posttraumatic stress disorder in haematological cancer survivors. Psychooncology. 2005;14:510–5. doi: 10.1002/pon.894. [DOI] [PubMed] [Google Scholar]
- 36.Brothers BM, Yang HC, Strunk DR, Andersen BL. Cancer patients with major depressive disorder: testing a biobehavioral/cognitive behavior intervention. J Consult Clin Psychol. 2011;79:253–60. doi: 10.1037/a0022566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van de Wal M, Thewes B, Gielissen M, Speckens A, Prins J. Efficacy of blended cognitive behavior therapy for high fear of recurrence in breast, prostate, and colorectal cancer survivors: the SWORD study, a randomized controlled trial. J Clin Oncol. 2017;35:2173–83. doi: 10.1200/JCO.2016.70.5301. [DOI] [PubMed] [Google Scholar]
- 38.Kazak AE. Evidence-based interventions for survivors of childhood cancer and their families. J Pediatr Psychol. 2005;30:29–39. doi: 10.1093/jpepsy/jsi013. [DOI] [PubMed] [Google Scholar]
- 39.Tatrow K, Montgomery GH. Cognitive behavioral therapy techniques for distress and pain in breast cancer patients: a meta-analysis. J Behav Med. 2006;29:17–27. doi: 10.1007/s10865-005-9036-1. [DOI] [PubMed] [Google Scholar]
- 40.Bystritsky A, Khalsa SS, Cameron ME, Schiffman J. Current diagnosis and treatment of anxiety disorders. P T. 2013;38:30–57. [PMC free article] [PubMed] [Google Scholar]