Abstract
Introduction
Childhood obesity is one of the most serious global public health challenges. However, obesity and its consequences are largely preventable. As parents play an important role in their children's weight‐related behaviours, good communication between parents and health care professionals (HCPs) is essential. This systematic review provides a meta‐synthesis of qualitative studies exploring the barriers and facilitators experienced by HCPs when discussing child weight with parents.
Methods
Searches were conducted using the following databases: MEDLINE (OVID), Psych INFO (OVID), EMBASE (OVID), Web of Knowledge and CINAHL. Thirteen full‐text qualitative studies published in English language journals since 1985 were included. Included studies collected data from HCPs (e.g., nurses, doctors, dieticians, psychologists, and clinical managers) concerning their experiences of discussing child weight‐related issues with parents. An inductive thematic analysis was employed to synthesize findings.
Findings
Emerging subthemes were categorized using a socio‐ecological framework into intra/interpersonal factors, organizational factors, and societal factors. Perceived barriers and facilitators most commonly related to intra/interpersonal level factors, that is, relating to staff factors, parental factors, or professional–parent interactions. HCPs also attributed a number of barriers, but not facilitators, at the organizational and societal levels.
Conclusion
The findings of this review may help to inform the development of future weight‐related communication interventions. Whilst intra/interpersonal interventions may go some way to improving health care practice, it is crucial that all stakeholders consider the wider organizational and societal context in which these interactions take place.
Statement of contribution.
What is already known on the subject?
Childhood obesity is one of the United Kingdom's most serious current public health challenges.
Health care professionals are in a prime position to identify child weight issues during routine consultations.
However, they often feel unable or unequipped to raise the topic and provide information on child weight management.
What does this study add?
To our knowledge, this is the first review to synthesize barriers and facilitators to discussing child weight.
This review interprets key barriers and facilitators in the context of the socio‐ecological model.
Supports the development of interventions matched to the appropriate level of the socio‐economic model.
Keywords: child weight, health care communication, health care professionals, meta‐synthesis, obesity, qualitative, review
Background
Childhood obesity is one of the most serious current global public health challenges (WHO, 2014). Overweight children are at greater risk of health problems later in life, both physical (e.g., asthma, type 2 diabetes) and psychological (e.g., low self‐esteem, loneliness) (van Grieken, Renders, Wijtzes, Hirasing, & Raat, 2013). Obesity and its consequences are associated with factors that are amenable to change such as dietary and physical activity (PA) behaviours. Addressing these lifestyle behaviours with parents early in children's lives could help prevent obesity and its health‐related consequences.
Effective communication is the foundation of therapeutic relationships in health care (Windover et al., 2014) and can positively influence health outcomes (e.g., emotional wellbeing and pain control (Street, Makoul, Arora, & Epstein, 2009)). Doctors and nurses talk and listen to patients more often than they perform any other procedure (Fallowfield & Jenkins, 1999). A good health care professional (HCP)–patient relationship is associated with greater patient recall and satisfaction than written instructions or time spent with the clinician (Levetown, 2008). Complaints about HCPs tend to focus on communication failures rather than clinical competencies (Moore, Wilkinson, & Rivera Mercado, 2004). In child weight management, a good therapeutic relationship between parents and HCPs is essential, as parental attitudes and behaviours influence the dietary and PA practices of their children (Farnesi, Ball, & Newton, 2012; Golan & Weizman, 2001).
The factors that are predictive of effective communication in health care include the HCP's demonstration of interest, care, warmth, responsiveness, and trust (Fallowfield & Jenkins, 2004). Despite communication skills being an essential component of most current health care training programmes (Moore, Rivera Mercado, Grez Artigues, & Lawrie, 2013), communication continues to present challenges in child weight management. For parents, child weight is a complex and sensitive topic associated with much stigma and negative perceptions (Chadwick, Sacher, & Swain, 2008), particularly if parents have weight issues themselves (Edvardsson, Edvardsson, & Hörnsten, 2009).
The challenges of professional–parent relationships have been reported by both parents and HCPs. Parents express dissatisfaction with primary care experiences, sometimes finding advice unhelpful or judgemental (Edmunds, Rudolf, & Mulley, 2007). Meanwhile, HCPs can feel uncomfortable, unable, or ill‐equipped to provide information about child weight and its management (Steele et al., 2011; Turner, Owen, & Watson, 2016). Reasons for HCP discomfort include the following: a lack of understanding of the complexities of childhood obesity; a lack of confidence; feelings of intimidation; and limited child weight‐related training and protocols (Rudolf, Hunt, George, Hajibagheri, & Blair, 2010; Teachman & Brownell, 2001; Turner et al., 2016; Willis, Potrata, Hunt, & Rudolf, 2012). The professional–parent relationship may be further complicated by some HCP beliefs that a lack of willpower contributes to obesity (Ljungkrona‐Falk, Brekke, & Nyholm, 2014), often attributing childhood obesity to family characteristics (e.g., lack of motivation to change, concern about weight, and cultural factors (Bonde, Bentsen, & Hindhede, 2014; Fisher & Kral, 2008; Isma, Bramhagen, Ahlstrom, Östman, & Dykes, 2012; Trigwell, Watson, Murphy, Stratton, & Cable, 2014; Turner et al., 2016)). If HCPs anticipate a negative reaction from parents, they may prioritize relationships over addressing children's weight (Chadwick et al., 2008; Regber, Mårild, & Hanse, 2013; Walker, Strong, Atchinson, Saunders, & Abbott, 2007).
Review rationale
Despite the interest in child weight‐related communication, to our knowledge no systematic review of published literature exists. It was decided to restrict the review to qualitative research, due to the potential range and depth of data generated by qualitative methodologies. In addition, synthesizing qualitative research is increasingly recognized as an effective way of informing appropriate health care interventions (Thomas & Harden, 2008). By undertaking a synthesis of qualitative study findings, it is possible to draw robust conclusions about the key barriers and facilitators HCPs encounter when discussing child weight with parents and the implications of these in improving future health care.
This meta‐synthesis explores barriers and facilitators experienced by HCPs when discussing child weight‐related information with parents. Since the focus of this review is on communicating with parents, rather than children themselves, the use of the term ‘children’ will refer to individuals under 18 years of age (as adopted in Oude Luttikhuis et al., 2009).
By synthesizing the available literature, we aim to:
Appraise the methodological quality of published studies;
Make recommendations for future practice and research to improve HCPs’ weight‐related communication with parents.
Methods
Search strategy and selection criteria
The research team (DB, AC, PW, CB, NB, SB) with support from an evidence synthesis and specialist support librarian developed the search terms (see Appendix). DB conducted searches in November 2016 using databases: MEDLINE (OVID), Psych INFO (OVID), EMBASE (OVID), Web of Knowledge, and CINAHL. Search strategies were adapted as appropriate for each database. Truncations, synonyms, and American medical terms were used where appropriate to ensure all relevant studies were identified. Forward and backward citation searches were undertaken, and literature known to the research team but not yet available through online searches was checked for eligibility. Where potentially relevant conference abstracts were identified, abstract authors were contacted to enquire whether full articles had been produced. Studies were included if they collected data from HCPs about their experiences of discussing child weight‐related issues (i.e., any health behaviours that can influence weight, for example, nutrition, physical activity, sedentary behaviour) with parents. For this study, an HCP was defined as ‘an individual who provides preventative or curative health care services to children and families of children’. Only full‐text qualitative studies published in an English language journal since 1985 were included, because child overweight began to rise steeply in the 1980s (von Hippel & Nahhas, 2013). Where parent data were also included in studies, only HCP data were extracted and analysed (see Table 1 for full eligibility criteria).
Table 1.
Study inclusion/exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
Data collection and analysis
Study screening and selection
Figure 1 provides an overview of the study screening and selection process. DB independently conducted the searches using the predefined search terms (Appendix). Screening of studies occurred in two stages. The first stage involved a broad eligibility screening based on titles and abstracts, where studies deemed obviously irrelevant to the research question were excluded. Where eligibility could not be determined, or where title and abstracts were ambiguous, full texts were obtained. To assess for inclusion/exclusion and establish reliability of eligibility criteria, 1,500 studies were randomly selected from 14,481 records and reviewed by NB and SB. Where there was any ambiguity over the inclusion/exclusion, the studies were discussed (DB, NB, SB) until a decision was made. This resulted in 100% agreement. DB and SB subjected the remaining 30 papers to a detailed full‐text review against the pre‐determined inclusion/exclusion criteria (Table 1). Any disagreements were discussed with a third author (AC) until a consensus was reached. Seventeen studies were excluded at this stage (for reasons see Figure 1). Thirteen studies were identified for inclusion in the review.
Figure 1.
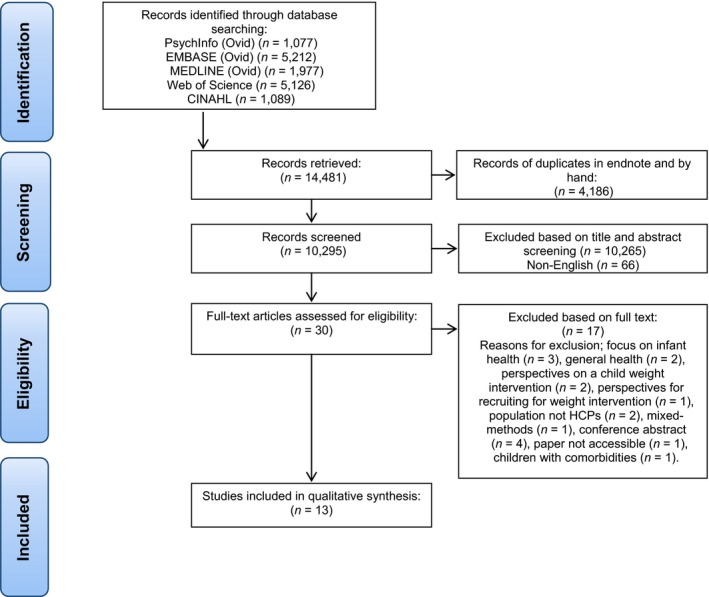
Study flow. [Colour figure can be viewed at http://wileyonlinelibrary.com]
Assessment of study quality
Quality of the included studies was assessed independently by three reviewers (DB, AC, PW), using the 14‐item National Institute of Clinical Excellence (NICE) quality appraisal checklist for qualitative studies (NICE, 2012). DB reviewed all 13 studies, with two authors (AC and PB) reviewing 6 and 7 studies, respectively. Initial inter‐rater reliability between DB and AC was k = .88; and DB and PW k = .64. According to the proposed standards by Landis and Koch (1977), the strength of agreement for DB and AC is ‘almost perfect’ (k = .81 to 1) and ‘substantial’ for DB and PW (k = .61 to .80). All three reviewers met to discuss any disagreements in the quality assessments and resolve any remaining ambiguities. This resulted in redefining the quality thresholds. The checklist stated that studies should be rated as ‘++’ if all or most of the criteria of the checklist have been fulfilled, ‘+’ if some of the criteria have been fulfilled (but where they have not adequately been fulfilled it is unlikely to affect the conclusion), and ‘−’ where few or no items on the checklist have been fulfilled. However, to ensure additional rigour, it was decided to only award a study ++ if it had met all of the criteria.
Data extraction
DB and SB extracted the following information from included studies: the country of study; study characteristics; population characteristics; and methodological aspects. The two reviewers (DB and SB) assessed the findings of each paper independently and data relating to HCP experiences of discussing child weight‐related information with parents were extracted. Where the authors were unsure or disagreed, discussions were held with the full research team to reach a consensus.
Data synthesis
The synthesis of data occurred in two stages: firstly, an inductive thematic analysis was employed to synthesize the findings of the included journal articles (Thomas & Harden, 2008), allowing common ideas to emerge directly from the data. Both narratives (i.e., text in analysis sections) and direct participant data (i.e., quotes) were coded ensuring analysis of all relevant data. Thematic analysis enabled data to be analysed, organized, and described in detail, and this data‐driven approach allowed the results to be strongly grounded within the data (Braun & Clarke, 2006). Initial coding was undertaken by one reviewer (DB) using NVivo 12 software. A second reviewer (SB) ensured the consistency of the key themes and subthemes that emerged by coding a random subset (four) of the papers. After all studies had been coded, codes were redefined by DB and similar codes combined to create new broader codes. Authors (DB, SB) then reviewed and organized these broader codes into themes and subthemes. The themes and subthemes were further defined in discussions with other team members (DB, AC, PW) and displayed with associated illustrative quotes. At this stage, these emergent themes and subthemes were identified by the research team as being broadly consistent with the levels of the socio‐ecological model (SEM) (Bronfenbrenner, 1992; Davison & Birch, 2001). The SEM has been previously applied to research in child weight (Davison & Birch, 2001; Huang & Glass, 2008; Steele et al., 2011). By highlighting the importance of considering influences at the intrapersonal, interpersonal, and organizational/societal levels (Neuhauser & Kreps, 2003), the model helps to conceptualize the range of factors that contribute to this complex topic and identify potential areas for change within a particular organization/setting.
The second stage of the synthesis involved grouping these subthemes into the SEM, thereby allowing the range of barriers and facilitators to be identified at the appropriate SEM level (i.e., inter/intrapersonal, organizational, societal). These groupings were then reviewed by the wider research team. A narrative account of the synthesis was prepared, and quotations were taken directly from the included studies to illustrate each theme.
Results
Thirteen studies were included in this review (Table 2). Six were conducted in the United States; two in the United Kingdom, Australia, and Sweden; and one in Canada, all between 2002 and 2016. Three data collection methods were used: interviews, focus groups, and open‐ended questionnaires. Consistent with qualitative research, the sample sizes were small ranging from 8 to 26 participants. Participants were HCPs working across a wide range of health care settings (see Table 2). As there were no noticeable differences between professions during the data analysis, all participants are discussed under the term ‘HCPs’.
Table 2.
Description of included studies
| Study | Country | Data collection methods | Participants | Recruitment source | Study Setting | Analysis methods | Quality assessment |
|---|---|---|---|---|---|---|---|
| Barlow, Richert, and Baker (2007) | United States | Interviews | Eight paediatricians (three female, five male) | American Medical Association database to represent a variety of demographic backgrounds in the St. Louis area | Paediatrician office visits | Deductive focused coding | − |
| Chamberlin, Sherman, Jain, Powers, and Whitaker (2002) | United States | Interviews, focus groups | 19 health care professionals; seven with clinical nutrition backgrounds 12 nursing backgrounds (all female) | Professionals who counsel on the Nutrition Programme for Women, Infants and Children (WIC) | Special Supplemental Nutrition Programme for Women Infants and Children (WIC) | Qualitative synthesis, specific analytic method unclear | + |
| Farnesi et al. (2012) | Canada | Focus groups | 12 clinicians; exercise specialist, dietician, nurse, paediatrician, psychiatrist, psychologist (13 females, one male) | Clinicians working in the field of paediatric weight | Multidisciplinary settings at specialized clinics | Thematic analysis | + |
| Findholt et al. (2013) | United States | Interviews | 13 clinicians; four family medicine physicians, two paediatricians, one paediatric nurse practitioner, two physician assistants (seven male six female) | Telephone book and database from the Oregon Rural Practice‐Based Research Network | Paediatric or family practice | Focused coding and grounded theory | + |
| Gilbert and Fleming (2006) | United States | Interviews | 24 paediatricians (42% male) | Paediatricians within the general paediatrics division of the University of Wisconsin | A mixture of community practice and academic settings overseeing residents | Editing analysis | + |
| Isma et al. (2012) | Sweden | Interviews | 17 Child Health Care nurses (CHC) | Child Care Centres in southern Sweden | Child Health Care Centres | Phenomenographic approach | + |
| Jones, Dixon, and Dixon (2014) | Australia | Interviews | 10 GPs | Convenience sample | General Practices | Thematic analysis | − |
| King et al. (2007) | Australia | Focus groups | 26 GPs (mix of males and females) | Three metropolitan and 1 rural area of New South Wales | General Practices | Content analysis | + |
| Morrison‐Sandberg, Kubik, and Johnson, (2011) | United States | Interviews | 21 school nurses | Minnesota Department of Education website and school district website | Elementary schools | Content analysis | + |
| Regber et al. (2013) | Sweden | Interviews | 15 nurses; six paediatric nurses, nine district nurses (all female) | Child health centres in south west Sweden | Child Health Centres | Content analysis | ++ |
| Steele et al. (2011) | United States | Focus groups | 22 school nurses | Midwestern School districts | Elementary, Middle and High Schools | Inductive content analysis | + |
| Turner et al. (2016) | United Kingdom | Interviews, focus groups, open‐ended questionnaires | 26 school health professionals; three service managers, 16 school nurses, seven child health practitioners | Staff employed in study location in city in North West England | Primary Schools | Thematic analysis | + |
| Walker et al. (2007) | United Kingdom | Interviews | 18 health care professionals; 12 GPs (11 male, one female), six nurses (female) | Rotherham Primary Health Care | General Practices | Framework analysis | + |
Using the NICE quality appraisal checklist for qualitative studies, 10 of the 13 studies included in the review were categorized as ‘+’, one as ‘++’, and 2 as ‘−’. For a full overview of study quality, see Table 2. A cross‐study summary of the scores for each quality component of the NICE appraisal checklist is presented in Table 3.
Table 3.
Quality assessment by individual quality appraisal item
| Quality appraisal item | Percentage meeting criteria across studies |
|---|---|
| 1. Is a qualitative approach appropriate? | 100 |
| 2. Is the study clear in what it seeks to do? | 76.9 |
| 3. How defensible/rigorous is the research design/methodology? | 76.9 |
| 4. How well was the data collection carried out? | 61.5 |
| 5. Is the role of the research clearly described? | 23.1 |
| 6. Is the context clearly described? | 92.3 |
| 7. Were the methods reliable? | 84.6 |
| 8. Is the data analysis sufficiently rigorous? | 46.2 |
| 9. Is the data rich? | 53.8 |
| 10. Is the analysis reliable? | 69.2 |
| 11. Are the findings convincing? | 76.9 |
| 12. Are the findings relevant to the aims of the study? | 100 |
| 13. Conclusions | 84.6 |
| 14. How clear and coherent is the reporting of ethics? | 100 |
An overview of the emergent themes and subthemes is provided in Tables 4 and 5 with verbatim quotes and participant identifiers, or narrative data where illustrative quotes and page numbers are identified. The results are presented for barriers (Table 4) and facilitators (Table 5), under themes and subthemes. Subthemes are highlighted in ‘italics’ throughout the text discussion.
Table 4.
Themes, subthemes, a selection of illustrative verbatim quotes and narrative data reflecting the identified barriers to discussing child weight with parents
| Themes | Subthemes | Data extracts |
|---|---|---|
| Intra/interpersonal factors | ||
| Staff factors | Knowledge and perceived competence | ‘I know what [the dietary] recommendations are, but only on a broad basis and not on a “well,… show me your dietary diary and let's see if…. “I can pick out some things to give them advice about, but I'm not going to presume to be a dietician and… have at my immediate recall a repertoire of dietary plans that might work for different situations…. I don't have that training’ (Paediatric physician, 5; Findholt et al., 2013) |
| Personal weight challenges | ‘I personally get the feeling that the parents are thinking, ‘how can you be talking about this, you're fat yourself’. (School nurse; Steele et al., 2011) | |
| Sense of futility | ‘I just feel kind of powerless… what more can I do? Well, if I was really having an impact, tomorrow I should see less obese people than I see today, and that ain't so. I mean I see just as many tomorrow, perhaps more’ (Paediatrician; Barlow 2007) | |
| Parental factors | Unmotivated to change | Parents [are a barrier.] …. the kids are overweight, the parents are overweight, and you try to reassure them, you try to get them educated on healthy diet and that kind of stuff… but it rarely makes any difference…. [S]o I would say… a lack of motivation to actually change lifestyle… [is] the biggest barrier I see. (Family practice physicians assistant, 6; Findholt et al.2013) |
| Parents overweight | ‘The issue also is that the kids with obesity problems, the parents usually do also and so identifying and helping… the parent understands that they can't just focus on their child, they have to focus on their whole family’ (School nurse; Morrison‐Sandberg et al. 2011) | |
| Complex family situations | ‘Nurses noted that some children with weight problems had complicated family situations that made it more difficult for nurses to consider intervening’ (School nurse; Steele et al., 2011 p. 132) | |
| Lack of acceptance | ‘Parents do not always accept that their child has a weight issue and decline onward referral or further monitoring’, (School nurse, 15; Turner et al., 2016) | |
| Professional–parent interaction | Fear of parent reactions | ‘Should we? [bring up the issue of a child's weight] Probably yes, but we don't. Usually because the response back is very negative. (GP, 3; Walker et al., 2007) |
| Risk to professional‐parent relationship | ‘One mother stated very clearly that “I find it so hard to come to you because you always bring this up.” She got up and left’ (Child health centre nurse; Regber et al., 2013) | |
| Fear of harm to child | ‘… chose not to discuss the issue in front of the child because it could lead to an eating disorder or depression’ (GP, 3; Jones et al. 2014) | |
| Cultural factors | It was also regarded as a communication problem when parents from certain cultures held a view of a healthy child and a healthy life that does not match the view held by the Child Health Care nurse (Isma et al., 2012; p. 7) | |
| Inconsistent messages | ‘We're telling them one thing, the family doctor may tell them something, and then what they read on that baby food jar or at the store is different. So they're getting conflicting information.’ (WIC health professional; Chamberlin et al., 2002) | |
| Organizational factors | Time | ‘You only have ten minutes; you just can't do it’ (GP, 2; Walker et al., 2007) |
| Organizational support | “If you get the principals on board you can make anything happen. But if the principals aren't on board, you can forget it, they're going to shut it down. “ (School nurse; Steele et al., 2011) | |
| Few contact opportunities | ‘We don't meet our children. We meet the kids quite regularly during the first year, perhaps at 15 months, then 18 months, then 2½ years, 4 years, and then 5½. So much can happen between those ages’ (Child health centre nurse; Regber et al., 2013) | |
| Lack of clear referral protocols | ‘It's alright identifying the problem but… where do we refer to, what do we do with them’, (Child health practitioner, 2; Turner et al., 2016) | |
| Limited resources | ‘Were unable to find relevant information to hand to families” (GP, 6; Jones et al. 2014) | |
| Societal factors | Normalization of overweight | ‘It is normal to be slightly overweight, really. We have changed our values somewhat. One doesn't quite react as quickly as before when children are chubby’ (Child health centre nurse; Regber et al., 2013) |
| Cultural perceptions of weight | ‘But, some parents felt that their child “being chubby represented good health’ (GP, 10; Jones et al., 2014) | |
| Economic environment | ‘… [inability to pay] is a huge issue because there are a lot of people hurting right now with the way the economy is…. So, to ask them to come back to do a separate assessment is kind of a challenge. I will tend not to do that unless I felt that the child was at a big enough risk that it needed to be addressed immediately’. (Family practice physicians assistant, 10; Findholt et al. 2013) | |
Table 5.
Themes, subthemes, a selection of illustrative verbatim quotes and narrative data reflecting the identified facilitators to discussing child weight with parents
| Themes | Subthemes | Verbatim quotes |
|---|---|---|
| Intra/interpersonal factors | ||
| Staff factors | Knowledge and perceived confidence | ‘I feel quite confident in speaking to them [parents]…. That may be because of my background’ (School nurse, 12; Turner et al., 2016) |
| Parental factors | Parents seeking help | ‘(When the parents seek help themselves) they embrace what you talk about, changing the diet and trying to assimilate the tips and advice that I have given ……..the easiest ones are the parents that say ‘help me’. They're definitely the easiest’ (Child health centre nurse; Regber et al., 2013) |
| Professional–parent interaction | Opportunity for health promotion | ‘Sometimes opportunities come, like the child is obese, and they come with some aches and pains in joints and… asthma [and ask] how do we prevent that? …. Say ‘you do this’ and she [the mother] is more likely to do it’ (GP Focus group 2; King et al. 2007) |
| Language | ‘I will never use the word overweight or obese’ (WIC health professional; Chamberlin et al., 2002) | |
| Good relationship | ‘I think the biggest thing is to keep a good relationship with the families, so that you can introduce little things and they're never afraid to come back because you're going to yell at them’ (Paediatrician; Gilbert & Fleming, 2006) | |
| Assessment tools | ‘Well, I think really the growth chart helps because you can show them. It's not just talking, you can show them where they should be and where they are’. (WIC health professional; Chamberlin et al., 2002) | |
| Regular monitoring and follow‐up | Ongoing monitoring and evaluation were identified as catalysis's for interactions between clinicians and parents … Many clinicians mentioned that encouraging families to monitor their behaviours and share these data with them gave them some objective evidence upon which to help with goal setting and recommendations (Farnesi et al., 2012 p. 14) | |
| Family‐centred goals | Counselling sessions needed to involve changing behaviour in small increments with short‐term goals that were established in conjunction with the client. The health care professionals also felt that the process of setting nutritional goals should be respectful of the client's social circumstances. Failing to focus on short‐term, achievable, client centred goals was likely to make the client feel overwhelmed and uninterested (Chamberlin et al. p. 666) | |
Barriers to discussing weight
Table 4 provides an overview of barriers to discussing child weight at the intra/interpersonal, organizational, and societal levels (Table 4). Intra/interpersonal barriers are further grouped into staff factors, parental factors, and professional–parent interactions.
Intra/interpersonal factors
Staff factors
A lack of knowledge and perceived competence in discussing weight‐related health posed a barrier to discussing weight in most studies. HCPs were unsure of the factors associated with weight‐related health or how to approach discussing a child's weight with parents. Furthermore, they did not feel confident in their ability to work with and motivate parents to change their family's lifestyles. This insufficient knowledge was attributed to a lack of appropriate training. HCPs’ own personal weight challenges were sometimes perceived as a barrier that resulted in a reluctance to discuss a child's weight with parents. A sense of futility was experienced by some HCPs who felt that they could not cope with the scale of the problem, and that they had little, if any influence on parents’ behaviour.
Parental factors
Parents being perceived as unmotivated to change provided an obstacle for most HCPs, inhibiting attempts to work with the family to promote lifestyle change. It was widely acknowledged that children with weight problems tend to come from inactive families with poor diets and overweight parents. Helping these parents to understand the scale of the problem and the risks associated with increased weight was perceived as an overwhelming task. Complex family situations, including safeguarding issues, difficult family dynamics and emotional or behavioural problems also occasionally presented barriers. HCPs felt some families had too many competing demands to try to tackle their lifestyles. When HCPs raised a child's weight, the parents were often unaware of, or unable to recognize, the problem. This parental lack of acceptance impeded further attempts to discuss the weight issue.
Professional–parent interaction
Health care professionals often indicated a fear of parent reactions when discussing a child's weight. They were anxious that parents might feel they were personally criticizing their lifestyle or parenting skills. Past experiences where parents had reacted badly during similar discussions contributed to these fears. As a result, some HCPs reported avoiding the topic altogether. A few HCPs highlighted that discussing a child's weight may risk professional–parent relationships. This was a particular concern given the HCP perceptions of the importance of parental involvement and trust when working with children. Due to the stigma attached to weight, some HCPs expressed a fear of harm to the child should they raise weight with children present, fearing that drawing attention to a child's weight could result in psychological problems.
Cultural factors such as language barriers, parental beliefs, and an HCP lack of awareness of specific cultural practices limited the extent to which HCPs felt able to discuss weight‐related health with parents. Additionally, parents receiving inconsistent messages around lifestyle change and recommendations from different sources (e.g., family, media, nurses, GPs, dieticians) risked making messages appear less credible.
Organizational factors
Irrespective of professional roles, insufficient time to discuss weight was cited in almost all studies as an organizational barrier to discussing weight and weight‐related health. The time available for providing counselling was limited by lack of capacity and competing priorities such as administrative burdens. Irrespective of the service setting, time constraints were coupled with a lack of organizational support, which led HCPs to feel as though they were working alone without support from their managers. Additionally, HCPs felt they had few contact opportunities to identify weight issues due to limited routine contact opportunities (e.g., immunizations), and potential long gaps between contacts (e.g., for acute illness). When they did see children with weight issues, almost half of HCPs described a lack of clear referral protocols. They were unsure where to refer children and what support was available for families. HCPs were dissatisfied with the lack of feedback they received after onward referral. Limited resources were often cited as a further barrier, such as lack of access to computerized BMI charts and few appropriate health promotion materials.
Societal factors
The normalization of overweight was seen as a barrier to communication with parents. Since HCPs perceived that both parents and themselves viewed being ‘bigger’ as being ‘normal’, issues were less likely to be picked up, discussed in consultations and actions taken. Differences in cultural perceptions of healthy weight were also identified. HCPs perceived different cultures as having differing perceptions of healthy body size and shape and reported increased prevalence of health problems in particular cultural groups. The economic environment was also identified as a barrier, particularly in studies conducted in countries where health care insurance was required. Often those families most in need of support did not have the resources to attend appointments, thus reducing the opportunity for weight issues to be discussed and followed up.
Facilitators to discussing weight
A number of facilitators emerged at the intra/interpersonal level (Table 5), which are again grouped into staff factors, parental factors, and professional–parent interactions. No organizational or societal level facilitators were reported.
Intra/interpersonal factors
Staff factors
Studies identified HCPs’ knowledge and perceived confidence as a facilitator to discussing a child's weight with parents. This included HCPs’ knowledge around weight‐related health (e.g., PA and nutrition guidelines for children) as well as personal experiences which increased their confidence in facilitating weight‐related discussions.
Parental factors
Parents seeking help provided a major facilitator to weight‐related conversations. HCPs believed that when parents themselves raised concerns about their child's weight, they would not perceive the HCP as being critical or judgemental. They were also more likely to be receptive to weight‐related discussions and to try to implement changes at home.
Professional–parent interaction
A number of HCPs noted that focussing on an associated health condition (e.g., family history of disease, or child's asthma) or current health behaviours (e.g., screen time or lack of routine exercise) and the impact this could have on the child offered an opportunity for health promotion and facilitated subsequent discussions around weight‐related health. The importance of language was highlighted, with HCPs preferring subtle approaches, neutral terminology, and avoiding the words ‘overweight’ and ‘obese’. A good relationship with parents was seen as making it easier to raise weight, resulting in parents being more receptive to discussions and more likely to adhere to lifestyle changes.
The use of assessment tools was identified by some as a facilitator. The use of objective tools such as BMI charts, growth charts, and questionnaires enabled HCPs to discuss weight objectively and therefore reduce blame or stigma. The charts also helped aid family understanding of weight issues. Regular monitoring and follow‐up provided a weight‐specific opportunity where the HCP could provide ongoing behavioural change support. It was widely acknowledged that the whole family's lifestyle and willingness to change impacts on a child's weight. Thus, setting family‐centred goals was perceived to be important, with a focus on short‐term goals that were realistic, conducive to the family's needs, and matched to their stage of change.
Discussion
This meta‐synthesis sought to explore HCPs’ perceptions of barriers and facilitators to discussing child weight with parents. The review identified 13 qualitative studies published between 2002 and 2016. There was a high degree of consistency across studies and no noteworthy differences between professions. Barriers and facilitators were most commonly cited at the intra/interpersonal level incorporating staff factors, parental factors, and the interactions between two. HCPs also attributed barriers to organizational factors and societal factors. However, there were no facilitators identified at the organizational and societal levels.
Both barriers and facilitators most commonly emerged at the intra/interpersonal level. At the staff level, HCPs saw the presence of knowledge and competence as a facilitator to discussing child weight and their absence as a barrier. Although this absence was sometimes blamed on insufficient training, when knowledge and competence were identified as a facilitator, the value of training was not explicitly acknowledged. Some participants indicated they would draw on knowledge from personal experiences which may be less grounded in evidence‐based practice (Turner et al., 2016).
Health care professionals in this study highlighted the role societal factors may play in interpersonal situations. It has been suggested that the general population is poor at recognizing overweight (Johnson, Cooke, Croker, & Wardle, 2008). This means parents may be less likely to see weight management as personally relevant (Towns & D'auria, 2009). HCPs themselves may also be poor at visually recognizing a child's overweight (Robinson, 2017; Smith, Gately, & Rudolf, 2008), so unless they employ objective tools the opportunity for weight‐related discussions may be missed. Whilst HCPs in this review were cognizant of the impact of societal perceptions of overweight on their interactions with parents, they seemed less concerned with the impact of their own weight and lifestyle (personal weight challenges were only cited in 1/13 studies (Steele et al., 2011)). Health professionals may often be overweight themselves, not always eating a healthy diet or partaking in sufficient PA (Esposito & Fitzpatrick, 2011; Kaur & Walia, 2008). However, research findings into the impact of HCP weight in weight management settings are equivocal. Some studies suggest that HCPs may give little consideration to how their own weight could affect conversations with patients (Fie, Norman, & While, 2013; Howe et al., 2010; Mikhailovich & Morrison, 2007), whereas others indicate that HCPs are in fact conscious of the impact of their body size in interactions with patients (Brown, 2007).
Health care professionals often felt that parents did not accept the messages being conveyed (i.e., that their child was overweight), or the extent of their parental role in weight management. Some HCPs regarded parents as being unmotivated to change, potentially leading to a belief that their professional efforts had minimal impact on lifestyle change. This perception of parental factors posing a barrier to discussing weight‐related health could be seen to suggest a lack of HCP ownership of their own responsibility in delivering effective behaviour change interventions. Regardless of the health care system, or country, most HCPs cited time and lack of clear referral protocols as barriers. They tended to focus on the lack of referral and service options rather than concentrating their efforts on health promotion or lifestyle behaviour change interventions prior to onward referral (as recommended by current paediatric weight management guidance (e.g., NICE, 2013)). Similarly, research in other areas of health communication (e.g., psoriasis) has found that whilst clinicians recognize lifestyle change as important they do not believe facilitating this is their role (Nelson et al., 2014). These beliefs may be underpinned by limited knowledge and behaviour change skills. Parents actively seeking help for their child's weight are seen as facilitating weight discussions, as their awareness of their child's weight problem makes them more receptive to these conversations. Applying the health action process approach of behaviour change (Schwarzer, 1992), these parents are more likely to respond positively to interventions directed at taking action to address the weight problem and may be more successful in the long term (Watson, 2012).
Health care professionals expressed fears of parental reactions when raising a child's overweight and the negative impact these discussions could have on the professional–parent relationship. The importance of professional–patient relationships and their influence on patient outcomes is well established (Street et al., 2009; Windover et al., 2014). However, concerns about raising weight may be misguided, since evidence from adult weight management shows patients do want professionals to raise weight and that it may not damage the relationship (Hart, Yelland, Mallinson, Hussain, & Peters, 2016). Furthermore, research from both adult (Potter, Vu, & Croughan‐Minihane, 2001) and child (Booth, King, Pagnini, Wilkenfeld, & Booth, 2009) weight management settings shows if health professionals do not raise weight as an issue, patients may not feel there is any problem with their (child's) weight and are therefore less likely to implement change. Evidence from parents themselves suggests the way in which HCPs bring up weight issues is important. Empathic nonjudgemental approaches encourage favourable responses and more ‘dictatorial’ approaches elicit anger (Watson, 2012).
Health care professionals’ interventions often appeared to rely on information giving. However, provision of information alone does not elicit lifestyle changes (Eccles et al., 2012; Miller & Rollnick, 2012). In some instances, HCPs would work in a more structured way citing strategies consistent with behaviour change techniques (e.g., regular monitoring, specific weight‐related follow‐up, and goal setting). Consistent with previous research, the importance of setting realistic achievable goals was emphasized (Golley, Hendrie, Slater, & Corsini, 2011).
Findings from this review highlighted a number of societal factors that posed barriers to weight‐related discussions. Cultural beliefs have been shown to affect the way parents view their child's weight (Towns & D'auria, 2009) with parents from cultures where weight is highly valued (i.e., as an indicator of wealth and health) more likely to view overweight children as healthy and believe they will outgrow their weight (Trigwell et al., 2014). For HCPs, however, specific cultural knowledge is not always essential. Empathy, respect, and a recognition of the role culture can play in health may play a greater part in child weight management (Leonard, 2001; Purnell, 2012). The economic environment was also identified as a societal barrier. In studies conducted in countries where health care has financial implications (e.g., North America), HCPs were less likely to discuss weight if the consequences of longer consultations or subsequent clinic visits would pressure already limited family resources.
It is notable that although several organizational and societal level barriers were identified no facilitators emerged at these levels. This finding might be explained from the perspective of attribution theory (Heider, 1958), which is concerned with how people use information to develop causal explanations in order to make sense of their social world. Organizational and societal factors are external to the individual, suggesting HCPs viewed barriers at this level as being out of their control. HCPs attributed intrapersonal barriers related to themselves to external factors (e.g., lack of training) whilst at the same time attributing intrapersonal barriers related to parents to internal factors (e.g., lack of parental motivation). In underestimating the importance of external influences (e.g., family pressures, lack of education, or financial resources) on parents’ behaviours and overestimating the contribution of internal factors, HCPs may have been exhibiting what is termed the ‘fundamental attribution error’. This may have contributed to their sense of futility in that they believed they were already doing all they could (hence citing a number of intra/interpersonal level facilitators) whilst perceiving parents and their employing organizations as doing little.
Strengths and Limitations
This review is, to the best of our knowledge, the first in this area. The inclusion of in‐depth qualitative studies ensures a rich yet focused dataset. The use of established analysis principles (Braun & Clarke, 2006) allowed for a rigorous thematic analysis and exploration into the insights of health professionals (Braun & Clarke, 2014). This, along with the application of the SEM allows for the identification of multiple level factors to inform future interventions by both practitioners and policymakers.
The review synthesizes findings from 13 studies, differing in methodological quality and rigour. Due to the inclusion of all studies that met the inclusion criteria, there may be a compromise in the quality of the studies synthesized. Similar limitations in the quality appraisal process have previously been reported (Thomas & Harden, 2008). However, it is deemed that ‘poor quality’ studies are less likely to add to, and, thus be a smaller component of the synthesis. Including studies that were purely qualitative provides the potential to miss key findings that have emerged through mixed methods and quantitative studies in this area. An additional methodological limitation is that a second reviewer coded only 25% of the review studies.
In this article, we use a broad definition of children to indicate under 18 years. One methodological flaw common across studies was the failure to explicitly report the age of the children. Given that health care practices may differ depending on children's ages (e.g., discussions with children or adolescents as opposed to parents), this may compromise attempts to generalize or compare findings with other published literature. However, studies were only included if HCPs were discussing weight with parents (rather than with children), suggesting children were likely of primary school age or younger. Time was consistently identified as a barrier regardless of profession. However, studies did not report the length of consultations. Despite the different geographical locations of the studies, findings were generally consistent. However, as the studies were all conducted in developed Western cultures, findings may not be applicable elsewhere. The restriction to studies published in English may have resulted in overlooking rich research published in other languages.
Conclusion and recommendations
This review synthesized the key barriers and facilitators faced by HCPs in discussing child weight with parents. Displaying barriers and facilitators in the context of the socio‐ecological model highlights the complexities of discussing child weight and in turn allows for the identification of the levels at which it might be useful to intervene. Barriers and facilitators were most commonly reported at the intra/interpersonal level. Whilst this is to be expected (as HCPs were delivering individual health care services), this finding suggests that staff‐level interventions have a role in overcoming these barriers. Training focussed on increasing skills, knowledge, and confidence in having conversations about child weight could enable practitioners routinely to raise and discuss the topic with families. Additionally, improving HCPs’ knowledge of, and ability to use evidence‐based behaviour change techniques may enhance the provision of weight‐related care for children and families. Training might also include increasing HCPs’ awareness of the role of attributional bias in child weight management.
The number of societal and organizational barriers cited suggests intra/interpersonal level interventions may be only part of the solution. Future research in child weight management should consider the social ecology of the issue (i.e., taking into account the wide range of factors that contribute to childhood overweight) and explore means of developing consistent child weight management pathways with clear responsibilities and referral mechanisms. In order to address the multifaceted and complex nature of child weight, interventions must occur at multiple levels of the socio‐ecological model and consider the need for wider systems change.
Conflict of interest
All authors declare no conflict of interest.
Key search terms:
Barrier* OR facilitate* OR ability* OR skill* Opportun* OR time* OR motivate* OR competenc* OR self‐efficac* OR auton* OR ‘needs support*’ OR intent* OR perc* OR attitude*
AND
communicat* OR interact* OR advi* OR ‘behavio?r change talk’ OR counsel* OR discuss* OR ‘obesity counsel*’ OR address* OR educat*
AND
Weight* OR ‘weight manag*’ OR obes* OR diet* OR nutrit* OR exercise* OR ‘physical activit*’
AND
‘health care profession*’ OR doctor* OR nurs* OR ‘general practition*’ OR clinician* OR practition* OR physician*
AND
Child* OR pe?d* OR pre‐school* OR school*
AND
Famil* OR parent* OR caregiv*
AND
Qualitative* OR interview* OR focus group* OR interpret* OR view* OR explor* OR experienc* OR narrative*
References
- Bonde, A. H. , Bentsen, P. , & Hindhede, A. L. (2014). School nurses’ experiences with motivational interviewing for preventing childhood obesity. The Journal of School Nursing, 30, 448–455. 10.1177/1059840514521240 [DOI] [PubMed] [Google Scholar]
- Barlow, S. , Richert, M. , & Baker, E. (2007). Putting context in the statistics: Paediatricians’ experiences discussing obesity during office visits. Child: Care, Health and Development, 33(4), 416–423. [DOI] [PubMed] [Google Scholar]
- Booth, M. L. , King, L. A. , Pagnini, D. L. , Wilkenfeld, R. L. , & Booth, S. L. (2009). Parents of school students on childhood overweight: The Weight of Opinion Study. Journal of Paediatrics and Child Health, 45, 194–198. 10.1111/j.1440-1754.2008.01453.x [DOI] [PubMed] [Google Scholar]
- Braun, V. , & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Braun, V. , & Clarke, V. (2014). What can thematic analysis offer health and wellbeing researchers? International Journal of Qualitative Studies on Health and Well‐being, 9, 26152 10.3402/qhw.v9.26152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner, U. (1992). Ecological systems theory. London, UK: Jessica Kingsley Publishers. [Google Scholar]
- Brown, I. A. T. J. (2007). Primary care nurses’ attitudes, beliefs and own body size in relation to obesity management. Journal of Advanced Nursing, 60, 535–543. 10.1111/j.1365-2648.2007.04450.x [DOI] [PubMed] [Google Scholar]
- Chadwick, P. , Sacher, P. , & Swain, C. (2008). Talking to families about overweight children. British Journal of School Nursing, 3, 271–276. 10.12968/bjsn.2008.3.6.31696 [DOI] [Google Scholar]
- Chamberlin, L. A. , Sherman, S. N. , Jain, A. , Powers, S. W. , & Whitaker, R. C. (2002). The challenge of preventing and treating obesity in low‐income, preschool children: perceptions of WIC health care professionals. Archives of Pediatrics & Adolescent Medicine, 156(7), 662–668. [DOI] [PubMed] [Google Scholar]
- Davison, K. K. , & Birch, L. L. (2001). Childhood overweight: A contextual model and recommendations for future research. Obesity Reviews, 2, 159–171. 10.1046/j.1467-789x.2001.00036.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccles, M. P. , Grimshaw, J. M. , MacLennan, G. , Bonetti, D. , Glidewell, L. , Pitts, N. B. , & Johnston, M. (2012). Explaining clinical behaviors using multiple theoretical models. Implementation Science, 7(1), 99 10.1186/1748-5908-7-99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmunds, L. , Rudolf, M. , & Mulley, B. (2007). How should we tackle obesity in the really young. Archives of Disease in Childhood, 92(Suppl 1), A75. [Google Scholar]
- Edvardsson, K. , Edvardsson, D. , & Hörnsten, Å. (2009). Raising issues about children's overweight–maternal and child health nurses’ experiences. Journal of Advanced Nursing, 65, 2542–2551. 10.1111/j.1365-2648.2009.05127.x [DOI] [PubMed] [Google Scholar]
- Esposito, E. M. , & Fitzpatrick, J. J. (2011). Registered nurses’ beliefs of the benefits of exercise, their exercise behaviour and their patient teaching regarding exercise. International Journal of Nursing Practice, 17(4), 351–356. 10.1111/j.1440-172X.2011.01951.x [DOI] [PubMed] [Google Scholar]
- Fallowfield, L. , & Jenkins, V. (1999). Effective communication skills are the key to good cancer care. European Journal of Cancer, 35, 1592–1597. 10.1016/S0959-8049(99)00212-9 [DOI] [PubMed] [Google Scholar]
- Fallowfield, L. , & Jenkins, V. (2004). Communicating sad, bad, and difficult news in medicine. The Lancet, 363, 312–319. 10.1016/S0140-6736(03)15392-5 [DOI] [PubMed] [Google Scholar]
- Farnesi, B. C. , Ball, G. , & Newton, A. (2012). Family–health professional relations in pediatric weight management: An integrative review. Pediatric Obesity, 7, 175–186. 10.1111/j.2047-6310.2012.00029.x [DOI] [PubMed] [Google Scholar]
- Fie, S. , Norman, I. J. , & While, A. E. (2013). The relationship between physicians’ and nurses’ personal physical activity habits and their health‐promotion practice: A systematic review. Health Education Journal, 72(1), 102–119. 10.1177/0017896911430763 [DOI] [Google Scholar]
- Findholt, N. E. , Davis, M. M. , & Michael, Y. L. (2013). Perceived barriers, resources, and training needs of rural primary care providers relevant to the management of childhood obesity. The Journal of Rural Health, 29(s1), s17–s24. [DOI] [PubMed] [Google Scholar]
- Fisher, J. O. , & Kral, T. V. (2008). Super‐size me: Portion size effects on young children's eating. Physiology and Behavior, 94(1), 39–47. 10.1016/j.physbeh.2007.11.015 [DOI] [PubMed] [Google Scholar]
- Gilbert, M. J. , & Fleming, M. F. (2006). Pediatricians’ approach to obesity prevention counseling with their patients. WMJ‐MADISON‐, 105(5), 26. [PubMed] [Google Scholar]
- Golan, M. , & Weizman, A. (2001). Familial approach to the treatment of childhood obesity: Conceptual model. Journal of nutrition education, 33, 102–107. 10.1016/S1499-4046(06)60173-5 [DOI] [PubMed] [Google Scholar]
- Golley, R. , Hendrie, G. , Slater, A. , & Corsini, N. (2011). Interventions that involve parents to improve children's weight‐related nutrition intake and activity patterns–what nutrition and activity targets and behaviour change techniques are associated with intervention effectiveness? Obesity Reviews, 12(2), 114–130. 10.1111/j.1467-789X.2010.00745.x [DOI] [PubMed] [Google Scholar]
- Hart, J. , Yelland, S. , Mallinson, A. , Hussain, Z. , & Peters, S. (2016). When is it ok to tell patients they are overweight? General public's views of the role of doctors in supporting patients’ dieting and weight management. Journal of Health Psychology, 21, 2098–2107. 10.1177/1359105315571974 [DOI] [PubMed] [Google Scholar]
- Heider, F. (1958). The psychology of interpersonal relations. New York, NY. [Google Scholar]
- Howe, M. , Leidel, A. , Krishnan, S. M. , Weber, A. , Rubenfire, M. , & Jackson, E. A. (2010). Patient‐related diet and exercise counseling: Do providers’ own lifestyle habits matter? Preventive Cardiology, 13, 180–185. 10.1111/j.1751-7141.2010.00079.x [DOI] [PubMed] [Google Scholar]
- Huang, T. T.‐K. , & Glass, T. A. (2008). Transforming research strategies for understanding and preventing obesity. JAMA, 300, 1811–1813. 10.1001/jama.300.15.1811 [DOI] [PubMed] [Google Scholar]
- Isma, G. E. , Bramhagen, A.‐C. , Ahlstrom, G. , Östman, M. , & Dykes, A.‐K. (2012). Swedish Child Health Care nurses conceptions of overweight in children: A qualitative study. BMC Family Practice, 13(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, F. , Cooke, L. , Croker, H. , & Wardle, J. (2008). Changing perceptions of weight in Great Britain: Comparison of two population surveys. BMJ, 337, a494 10.1136/bmj.a494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, K. M. , Dixon, M. E. , & Dixon, J. B. (2014). GPs, families and children's perceptions of childhood obesity. Obesity Research & Clinical Practice, 8(2), e140–e148. [DOI] [PubMed] [Google Scholar]
- Kaur, J. , & Walia, I. (2008). Bodymass index among nursing students. Nursing and Midwifery Research, 4, 110–116. [Google Scholar]
- King, L. A. , Loss, J. H. , Wilkenfeld, R. L. , Pagnini, D. L. , Booth, M. L. , & Booth, S. L. (2007). Australian GPs’ perceptions about child and adolescent overweight and obesity the Weight of Opinion study. British Journal of General Practice, 57(535), 124–129. [PMC free article] [PubMed] [Google Scholar]
- Landis, J. R. , & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33, 159–174. 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- Leonard, B. (2001). Quality nursing care celebrates diversity. Online Journal of Issues in Nursing, 6(2), 1–16. [PubMed] [Google Scholar]
- Levetown, M. (2008). Communicating with children and families: From everyday interactions to skill in conveying distressing information. Pediatrics, 121(5), e1441–e1460. 10.1542/peds.2008-0565 [DOI] [PubMed] [Google Scholar]
- Ljungkrona‐Falk, L. , Brekke, H. , & Nyholm, M. (2014). Swedish nurses encounter barriers when promoting healthy habits in children. Health Promotion International, 29, 730–738. 10.1093/heapro/dat023 [DOI] [PubMed] [Google Scholar]
- Mikhailovich, K. , & Morrison, P. (2007). Discussing childhood overweight and obesity with parents: A health communication dilemma. Journal of Child Health Care, 11(4), 311–322. 10.1177/1367493507082757 [DOI] [PubMed] [Google Scholar]
- Miller, W. R. , & Rollnick, S. (2012). Motivational interviewing: Helping people change. New York, NY: Guilford Press. [Google Scholar]
- Moore, P. M. , Rivera Mercado, S. , Grez Artigues, M. , & Lawrie, T. A. (2013). Communication skills training for healthcare professionals working with people who have cancer. The Cochrane Library. [DOI] [PMC free article] [PubMed]
- Moore, P. M. , Wilkinson, S. S. , & Rivera Mercado, S. (2004). Communication skills training for health care professionals working with cancer patients, their families and/or carers. Cochrane Database Systematic Review, 2. [DOI] [PubMed] [Google Scholar]
- Morrison‐Sandberg, L. F. , Kubik, M. Y. , & Johnson, K. E. (2011). Obesity prevention practices of elementary school nurses in Minnesota: Findings from interviews with licensed school nurses. The Journal of School Nursing, 27(1), 13–21. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence, N. (2012). Methods for the development of NICE public health guidance (third edition). Retrieved from https://www.nice.org.uk/process/pmg4/chapter/appendix-f-quality-appraisal-checklist-quantitative-intervention-studies [PubMed]
- National Institute for Health and Care Excellence, N. (2013). Weight management: Lifestyle services for overweight or obese children and young people. Retrieved from https://www.nice.org.uk/guidance/ph47/chapter/6-glossary#obesity-care-or-weight-management-pathway
- Nelson, P. , Keyworth, C. , Chisholm, A. , Pearce, C. , Griffiths, C. , Cordingley, L. , & Bundy, C. (2014). ‘In someone's clinic but not in mine’–clinicians’ views of supporting lifestyle behaviour change in patients with psoriasis: A qualitative interview study. British Journal of Dermatology, 171, 1116–1122. 10.1111/bjd.13231 [DOI] [PubMed] [Google Scholar]
- Neuhauser, L. , & Kreps, G. L. (2003). Rethinking communication in the e‐health era. Journal of Health Psychology, 8(1), 7–23. 10.1177/1359105303008001426 [DOI] [PubMed] [Google Scholar]
- Oude Luttikhuis, H. , Baur, L. , Jansen, H. , Shrewsbury, V. A. , O'Malley, C. , Stolk, R. P. , & Summerbell, C. D. (2009). Cochrane review: Interventions for treating obesity in children. Evidence‐based Child Health: A Cochrane Review Journal, 4, 1571–1729. 10.1002/(ISSN)1557-6272 [DOI] [PubMed] [Google Scholar]
- Potter, M. B. , Vu, J. D. , & Croughan‐Minihane, M. (2001). Weight management: What patients want from their primary care physicians. Journal of Family Practice, 50(6), 513. [PubMed] [Google Scholar]
- Purnell, L. D. (2012). Transcultural health care: A culturally competent approach. Philadelphia, PA: FA Davis. [Google Scholar]
- Regber, S. , Mårild, S. , & Hanse, J. J. (2013). Barriers to and facilitators of nurse‐parent interaction intended to promote healthy weight gain and prevent childhood obesity at Swedish child health centers. BMC Nursing, 12(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson, E. (2017). Overweight but unseen: A review of the underestimation of weight status and a visual normalization theory. Obesity Reviews, 18, 1200–1209. 10.1111/obr.12570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolf, M. , Hunt, C. , George, J. , Hajibagheri, K. , & Blair, M. (2010). HENRY: Development, pilot and long‐term evaluation of a programme to help practitioners work more effectively with parents of babies and pre‐school children to prevent childhood obesity. Child: Care, Health and Development, 36, 850–857. [DOI] [PubMed] [Google Scholar]
- Schwarzer, R. (1992). Self‐efficacy in the adoption and maintenance of health behaviours Theoretical approaches and a new model In Schwarzer R. (Ed.), Self‐efficacy: Thought control of action. Washington, DC: Hemisphere. [Google Scholar]
- Smith, S. M. , Gately, P. , & Rudolf, M. (2008). Can we recognise obesity clinically? Archives of Disease in Childhood, 93(12), 1065–1066. 10.1136/adc.2007.134486 [DOI] [PubMed] [Google Scholar]
- Steele, R. G. , Wu, Y. P. , Jensen, C. D. , Pankey, S. , Davis, A. M. , & Aylward, B. S. (2011). School nurses’ perceived barriers to discussing weight with children and their families: A qualitative approach. Journal of School Health, 81(3), 128–137. 10.1111/j.1746-1561.2010.00571.x [DOI] [PubMed] [Google Scholar]
- Street, R. L. , Makoul, G. , Arora, N. K. , & Epstein, R. M. (2009). How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient Education and Counseling, 74(3), 295–301. 10.1016/j.pec.2008.11.015 [DOI] [PubMed] [Google Scholar]
- Teachman, B. A. , & Brownell, K. D. (2001). Implicit anti‐fat bias among health professionals: Is anyone immune? International Journal of Obesity, 25, 1525–1531. 10.1038/sj.ijo.0801745 [DOI] [PubMed] [Google Scholar]
- Thomas, J. , & Harden, A. (2008). Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Medical Research Methodology, 8(1), 45 10.1186/1471-2288-8-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towns, N. , & D'auria, J. (2009). Parental perceptions of their child's overweight: An integrative review of the literature. Journal of Pediatric Nursing, 24(2), 115–130. 10.1016/j.pedn.2008.02.032 [DOI] [PubMed] [Google Scholar]
- Trigwell, J. , Watson, P. , Murphy, R. , Stratton, G. , & Cable, N. (2014). Ethnic differences in parental attitudes and beliefs about being overweight in childhood. Health Education Journal, 73(2), 179–191. 10.1177/0017896912471035 [DOI] [Google Scholar]
- Turner, G. L. , Owen, S. , & Watson, P. M. (2016). Addressing childhood obesity at school entry: Qualitative experiences of school health professionals. Journal of Child Health Care, 20(3), 304–313. 10.1177/1367493515587061 [DOI] [PubMed] [Google Scholar]
- van Grieken, A. , Renders, C. M. , Wijtzes, A. I. , Hirasing, R. A. , & Raat, H. (2013). Overweight, obesity and underweight is associated with adverse psychosocial and physical health outcomes among 7‐year‐old children: The “Be active, eat right” study. PLoS ONE, 8(6), e67383 10.1371/journal.pone.0067383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Hippel, P. T. , & Nahhas, R. W. (2013). Extending the history of child obesity in the United States: The fels longitudinal study, birth years 1930‐1993. Obesity, 21, 2153–2156. 10.1002/oby.20395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker, O. , Strong, M. , Atchinson, R. , Saunders, J. , & Abbott, J. (2007). A qualitative study of primary care clinicians’ views of treating childhood obesity. BMC Family Practice, 8(1), 50 10.1186/1471-2296-8-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson, P. M. (2012). Feasibility evaluation and long‐term follow up of a family‐based behaviour change intervention for overweight children (GOALS). PhD thesis: Liverpool John Moores University.
- Willis, T. , Potrata, B. , Hunt, C. , & Rudolf, M. (2012). Training community practitioners to work more effectively with parents to prevent childhood obesity: The impact of HENRY upon Children's Centres and their staff. Journal of Human Nutrition and Dietetics, 25(5), 460–468. 10.1111/j.1365-277X.2012.01247.x [DOI] [PubMed] [Google Scholar]
- Windover, A. K. , Boissy, A. , Rice, T. W. , Gilligan, T. , Velez, V. J. , & Merlino, J. (2014). The REDE model of healthcare communication: Optimizing relationship as a therapeutic agent. Journal Patient Experience, 1, 8–13. 10.1177/237437431400100103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) (2014). Global Strategy on Diet, Physical Activity and Health. Childhood overweight and obesity. Retrieved from http://www.who.int/dietphysicalactivity/childhood/en/


