Abstract
Objective:
As part of a quality improvement process, we propose a model of routinely monitoring electroconvulsive therapy (ECT) in Canadian provinces using linked health administrative databases to generate provincial periodic reports, influence policy, and standardise ECT practices.
Methods:
ECT practice in Quebec was studied from 1996 to 2013, using longitudinal data from the Quebec Integrated Chronic Disease Surveillance System of the Institut National de Santé Publique du Québec, which links 5 health administrative databases. The population included all persons, aged 18 y and over, eligible for the health insurance registry, who received an ECT treatment at least once during the year.
Results:
Among recorded cases, 75% were identified by physician claims and hospitalisation files, 19% exclusively by physician claims, and 6% by hospitalisation files. From 1996 to 2013, 8,149 persons in Quebec received ECT with an annual prevalence rate of 13 per 100,000. A decline was observed, which was more pronounced in women and in older persons. On average, each patient received 9.7 treatments of ECT annually. The proportion of acute ECT decreased whereas maintenance treatment proportions increased. A wide variation in the use of ECT was observed among regions and psychiatrists.
Conclusion:
This study demonstrates the profitable use of administrative data to monitor ECT use in Quebec, and provides a reliable method that could be replicated in other Canadian provinces. Although Quebec has one of the lowest utilisation rates reported in industrialized countries, regional disparities highlighted the need for a deeper examination of the quality and monitoring of ECT care and services.
Keywords: Electroconvulsive therapy, mental illness, prevalence, surveillance system, survey, practice variation, Quebec, epidemiology
Abstract
Objectif:
Dans le cadre d’un processus d’amélioration de la qualité, nous proposons un modèle de surveillance provinciale de l’électroconvulsivothérapie (ECT), basé sur l’utilisation des données médico-administratives, qui permettrait de produire régulièrement des rapports provinciaux, d’influencer les politiques et standardiser les pratiques d’ECT.
Méthodes:
La pratique d’ECT a été étudiée à partir des données longitudinales issues du Système intégré de surveillance des maladies chroniques du Québec de l’Institut national de santé publique du Québec, qui regroupe cinq bases de données médico-administratives. La population incluait l’ensemble des personnes admissibles à la Régie de l’assurance maladie du Québec, âgées de 18 ans et plus, ayant eu de l’ECT au cours de l’année.
Résultats:
Parmi les cas répertoriés, 75 % ont été identifiés à la fois par le fichier des services médicaux rémunérés à l’acte et par le fichier des hospitalisations, 19 % exclusivement identifiés par le fichier des services médicaux et 6 % exclusivement par le fichier des hospitalisations. De 1996 à 2013, 8 149 personnes du Québec ont reçu de l’ECT avec une prévalence annuelle de 13 par 100 000. Une baisse d’utilisation, plus prononcée chez les femmes et les personnes âgées, a été observée. En moyenne, chaque personne a reçu 9.7 séances d’ECT par année. L’administration d’ECT en phase aiguë a sensiblement diminué durant cette période, contrairement à l’ECT d’entretien qui a augmenté. Une grande variation de l’utilisation de l’ECT entre les régions et les psychiatres a été constatée.
Conclusion:
Cette étude démontre l’avantage de l’utilisation des données administratives pour surveiller l’usage de l’ECT au Québec, et offre une méthode fiable qui pourrait être reproduite dans les autres provinces canadiennes. Bien que le Québec ait un taux d’utilisation parmi les plus faibles reportés dans les pays industrialisés, les disparités régionales souligne la nécessité de mettre en place un système de suivi plus élaboré de la qualité des soins et des services d’ECT.
Electroconvulsive therapy (ECT) is an effective and safe medical intervention, designed to induce a convulsion in the brain to treat some of the most resistant forms of specific psychiatric illnesses.1,2 First used in 1938, this therapy was frequently administered before the development of psychiatric medications in the 1960s.3 Since then, its use varies greatly across countries.4,5
To our knowledge, the first assessment of the practice of ECT in the province of Quebec was published in 2002 by the Agence d’évaluation des technologies et des modes d’intervention en santé (Health Technology Assessment Agency of Quebec, or AETMIS), part of the International Network of Agencies for Health Technology Assessment.6 Analysis of the physician billing data derived from the Régie de l’assurance maladie du Quebec (Quebec’s health insurance board, or RAMQ) showed an increase in ECT treatment from 1988 to 1996 and then a stabilisation until 2001.6 The AETMIS report did not indicate the number of people who received ECT, or standardised prevalence. The interprovincial comparison was therefore based on the number of hospitalisations associated with ECT from The Canadian Institute for Health Information (CIHI). Great variability was observed based on these data, with prevalence ranging from 15 to 140 hospitalisations per 100,000 inhabitants. A marked heterogeneity in ECT utilisation was reported among the different regions of Quebec and also among the Canadian provinces.6 Interestingly, Quebec and Ontario had among the lowest prevalence rates in Canada between 1999 and 2000, with 26 and 37 hospitalisations per 100,000 inhabitants, respectively.5,6 This variability seems, in part, due to differences in the accessibility of this therapy.6–8 A recent meta-analysis, addressing the international prevalence of ECT since 1973, estimated the use of ECT at 16.9 treated persons per 100,000 inhabitants globally, with a decreased trend over time and a higher ECT utilisation rate in higher-income countries.5
There are serveral limitations of using only data from hospitalisations or only data from physicians’ billings to analyse ECT utilisation rates. The hospitalisation rate does not make it possible to estimate the number of people treated, as the same patient may have been hospitalised and treated by ECT several times in the same year. This rate also does not include outpatient ECT treatments (performed in outpatient clinics), with one study6 reporting that outpatient ECT rates increased by 18% to 28% between 1988 and 2001. Likewise, estimations based on billing data may underestimate ECT use by not considering ECTs administered by physicians under remuneration by the hour. Linking different health administrative databases, including hospital and physician payment data, could thus lead to a more accurate estimate of ECT use.
As part of a quality improvement process, the main objectives of this study were to assess the profile of ECT use from 1996 to 2013 and propose a model for routinely monitoring ECT in Canada’s provinces. The secondary objectives were to estimate the overall ECT utilisation prevalence, treatment indications, ECT practices, and the regional volumes of ECT by clinic and by psychiatrist.
Methods
Data Sources
Estimates on ECT use were gathered using data from linked health administrative databases which together make up the Quebec Integrated Chronic Disease Surveillance System (QICDSS). These databases include the health insurance registry, the physician claims database, the hospitalization database, the vital statistics death database, and the pharmaceutical services database.9 Vital statistics and pharmaceutical databases were not used for this study. The process of creating the QICDSS and data access meet stringent standards of security and privacy, as QICDSS was evaluated and approved by the public health ethics committee and the Commission d’accès à l’information du Québec. The health insurance registry provides information on demographic and geographic data as well as periods of health insurance eligibility. Quebec, like other Canadian provinces, operates a public-managed care system10; over 98% of the Quebec population are registered under this plan. The physician claims compile all fee-for-service payment claims billed to the Quebec’s public health plan agency (RAMQ). Each record includes the fee code associated with the service rendered and, optionally—in about 95% of claims submitted by psychiatrists—the most relevant diagnostic code. The hospitalisation database identifies the primary and secondary diagnoses associated with each hospital admission. Diagnostic codes are based on the International Classification of Diseases, 9th Revision (ICD-9) in the physician claims database for the entire observation period, as well as on the hospitalisation database up until 31 March 2006; since 1 April 2006, the codes of the Canadian enhancement of the Tenth Revision (ICD-10-CA) have been used in the hospitalisation database. Intervention codes in the hospitalisation database are based on the Canadian Classification of Diagnostics, Therapeutic and Surgical Procedures (CCP), in conjunction with ICD-9,11 and the Canadian Classification of Health Interventions (CCI),12 in conjunction with ICD-10-CA.10
Population and Case Identification
The population studied included all Quebec residents eligible for health insurance, aged 18 y and over during the study period of 1 April 1996 to 31 March 2013; this means between 5.5 and 6.6 million people each year, with an annual average of 6.0 million people for the entire province.
To be considered as having received an ECT, an individual must have received at least one ECT during a given year (April 1 to March 31) on physician billing procedures with a fee code of ECT as an inpatient (08977) or as an outpatient (08987); or at least one ECT on physician billing procedures or ECT on hospitalisation separation procedure codes with CCP intervention code of electroconvulsive therapy not otherwise classified (0838), or a CCI code of stimulation, brain, using external electrical stimulation for shock or convulsion (1AN09JADV).
An ECT treatment was defined as acute if it was given less than 6 d before or after any other ECT treatment. An ECT treatment was defined as maintenance if it was given 7 d or more before or after any other ECT treatment.
Hospitals and psychiatrists delivering ECT were identified through an anonymized identification number recorded in physician claims and hospitalisation files.
Treatment indications were classified into 6 diagnostic categories grouping ICD-9 and ICD-10 codes: substance abuse, schizophrenia and related disorders, affective disorders, anxiety disorders, personality disorders, and other diagnoses.13
Data Analysis
The analysis period began 1 April 1996 and ended 31 March 2013. To simplify presentation, yearly results are identified by the first 9 mo of the calendar year. For example, results covering April 1996 to March 1997 are identified as 1996. Comparisons over time and between regions were made using age-adjusted measures, obtained with direct standardisation using the age structure of the population of Quebec in 2001. Though all regions of Quebec were included in the provincial analysis, data from the Outaouais region were not disclosed because of its borderline position with Ontario and the cross-border health care exchanges. Similarly, data from Northern regions of Quebec were not included because such a small volume could lead to unreliable estimates and fail to preserve anonymity. However, these regions were added to the total of the Province of Quebec.
Results were stratified according to 3 age groups. Hospitals and psychiatrists were classified according to the volume of ECT treatments delivered over a 5-y period, from 2008 to 2012.
Tests for trends were made by fitting negative binomial regression models. According to the trend studied, the dependent variables were either annual prevalence or mean annual treatments of acute and maintenance ECT and the year was the independent variable. The percent change in the expected number of the dependent variables was calculated for a 1-y increase with a 95% confidence interval.
Results
According to the selected case definition used in this study, 8,149 individuals received at least one ECT between 1 April 1996 and 31 March 2013 in Quebec. Among the recorded cases, 75% were identified by both physician claims and hospitalisation files, 19% exclusively by physician claims, and 6% exclusively by hospitalisation files.
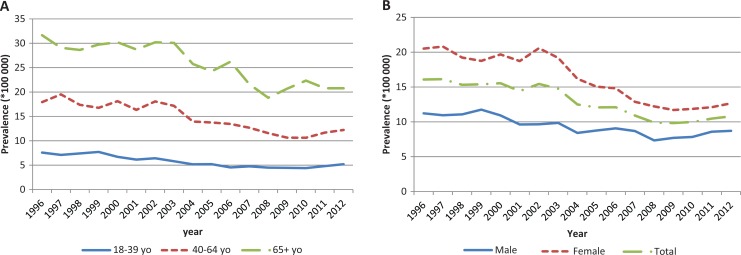
Figure 1 presents the annual prevalence rate of individuals who received ECT from 1996–1997 to 2012–2013 by sex (Figure 1a) and age group (Figure 1b). Over the entire study period, the age-standardised annual rate for ECT utilisation was 13 per 100,000 inhabitants. Table 1 presents the number of people who received ECT, providing absolute numbers for the region, and the age-standardised rates, which can be used for regional, temporal, inter-provincial, and international comparisons. A downward trend was observed in the 15 y of the study, with age-standardised rates decreasing from 15 per 100,000 for 1997 to 2002 to 10 per 100,000 for 2008 to 2013 (33% decrease; Figure 1 and Table 1). Crude rates were similar to standardised rates (1998 to 2002: 15.3 [14.9–15.8]; 2003 to 2007: 12.9 [12.5–13.3] and 2008 to 2012: 10.8 [10.4–11.2]).
Figure 1.
Annual prevalence of persons receiving ECT, per 100,000 inhabitants, according to age (a) and sex (b); Québec, 1996 to 2012.
Table 1.
Number of Cases and Standardised Prevalence Rates of Persons Receiving ECT per 100,000 Inhabitants, Per 5 Y Periods, According to the Health Administrative Region of Quebeca, 1998 To 2012.
| 1998–2002 | 2003–2007 | 2008–2012 | ||||
|---|---|---|---|---|---|---|
| RSS | Number of cases | Standardised rates (95% CI) | Number of cases | Standardised rates (95% CI) | Number of cases | Standardised rates (95% CI) |
| Bas-Saint-Laurent | 70 | 8.8 (6.9 to 11.1) | 110 | 12.6 (10.3 to 15.3) | 100 | 12.0 (9.7 to 14.7) |
| Saguenay–Lac-Sait-Jean | 245 | 21.8 (19.2 to 24.7) | 180 | 15.7 (13.5 to 18.2) | 130 | 10.6 (8.8 to 12.6) |
| Capitale-Nationale | 675 | 25.6 (23.7 to 27.6) | 420 | 14.6 (13.2 to 16.1) | 350 | 11.4 (10.2 to 12.7) |
| Mauricie et Centre-du-Québec | 280 | 14.1 (12.5 to 15.9) | 340 | 16.1 (14.4 to 17.9) | 420 | 19.0 (17.2 to 21.0) |
| Estrie | 160 | 13.9 (11.9 to 16.3) | 180 | 14.6 (12.6 to 17.0) | 295 | 22.5 (20.0 to 25.3) |
| Montréal | 1435 | 19.0 (18.0 to 20.0) | 1180 | 15.2 (14.3 to 16.1) | 935 | 11.7 (11.0 to 12.5) |
| Abitibi-Témiscamingue | 30 | 6.1 (4.2 to 8.5) | 65 | 10.7 (8.2 to 13.8) | 55 | 8.5 (6.4 to 11.2) |
| Côte-Nord | 60 | 15.8 (12.1 to 20.4) | 75 | 19.1 (15.0 to 24.1) | 55 | 12.9 (9.6 to 17.1) |
| Gaspésie—Îles-de-la-Madeleine | 95 | 21.8 (17.6 to 26.8) | 85 | 19.2 (15.3 to 24.1) | 35 | 6.5 (4.5 to 9.3) |
| Chaudière-Appalaches | 190 | 12.4 (10.7 to 14.2) | 140 | 8.4 (7.0 to 9.9) | 70 | 3.9 (3.1 to 5.0) |
| Laval | 145 | 10.3 (8.6 to 12.1) | 140 | 9.1 (7.7 to 10.8) | 135 | 7.8 (6.5 to 9.2) |
| Lanaudière | 140 | 8.9 (7.5 to 10.6) | 130 | 7.2 (6.0 to 8.6) | 85 | 4.3 (3.5 to 5.4) |
| Laurentides | 60 | 3.4 (2.6 to 4.4) | 65 | 3.4 (2.7 to 4.4) | 60 | 2.6 (2.0 to 3.4) |
| Montérégie | 630 | 12.5 (11.5 to 13.5) | 570 | 10.3 (9.4 to 11.1) | 475 | 7.8 (7.1 to 8.5) |
| Province of Quebec | 4465 | 15.2 (14.8 to 15.7) | 3940 | 12.5 (12.1 to 12.8) | 3460 | 10.2 (9.9 to 10.6) |
95%CI: 95% confidence interval
aOutaouais and Northern Quebec regions are presented in the total of Quebec.
This decrease was observed for all age groups and in both sexes. The prevalence of ECT was higher among women (Figure 1a) and among persons aged 65 y and over (Figure 1b). The decrease in ECT prevalence was also higher among these 2 categories. Regression analyses estimated the annual decrease in the annual prevalence at −3.4% (95%CI, −4.0 to −2.8). For age groups, the annual decrease was estimated at –3.8% (–4.6 to –3.1), –3.5% (–4.3 to –2.8), –2.9% (–3.5 to 2.3), respectively, for age ranges 18 to 39 y, 40 to 64 y and 65 y and over. The annual decrease was estimated at –4.0% (–4.7 to –3.2) for women and –2.3% (–2.9% to –1.8%) for men.
The analysis of prevalent cases and prevalence rates of individuals who received ECT by health region corroborates this downward trend across all regions, except for 2 regions (Mauricie et Centre-du-Québec, Estrie), where the age-standardised prevalence rate increased constantly by 35% and 62%, respectively, between 1997 and 2012. Bas-Saint-Laurent and Abitibi-Témiscamingue also increased but only between 1998–2002 and 2003–2007 (Table 1). A wide variation in the use of ECT was also observed among regions, with prevalence rates varying between 3 per 100,000 to 23 per 100,000 inhabitants for the period between 2008 and 2012.
Characteristics of ECT by Treatment Type (Acute ECT Treatment v. Maintenance Treatment)
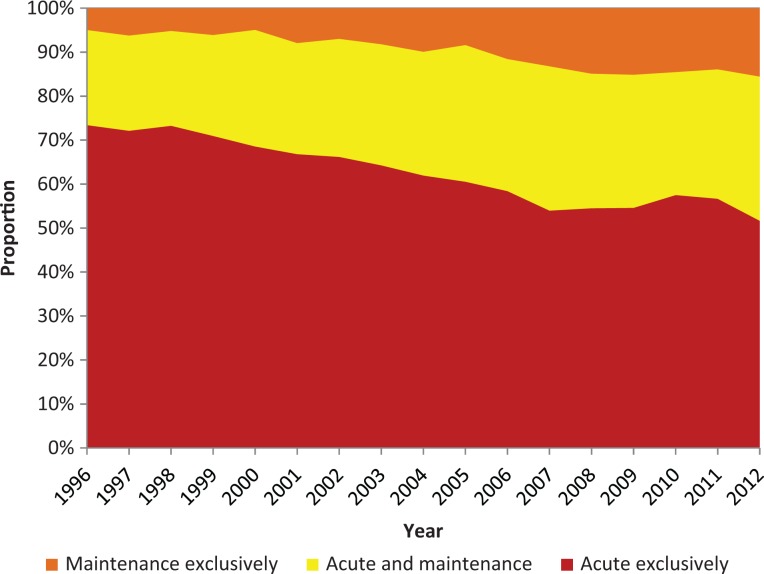
The proportion of individuals who exclusively received maintenance treatments increased during the study period, shifting from 5% in 1996 to 16% in 2012. In contrast, the proportion of individuals who exclusively received acute treatments decreased from 72% to 52% over the same period (Figure 2). Overall, the proportion of individuals treated by both acute and maintenance ECT increased from 22% to 33% during the study period.
Figure 2.
Annual proportion of persons receiving exclusively acute ECT treatments, exclusively maintenance ECT treatments, or both; Québec, 1996 to 2012.
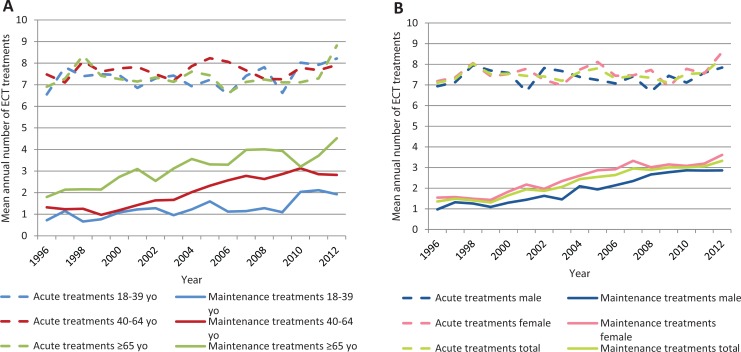
The individual annual mean of acute treatments remained stable during the study period, with an average of 7.1 treatments in 1996 and 8.3 in 2012 (Figure 3a). The individual annual mean of maintenance treatments rose from 1.4 to 3.3 during the study period; this increase was observed for all age groups (Figure 3b).
Figure 3.
Mean annual number of acute and maintenance ECT treatments per year according to age (a) and sex (b); Québec, 1996 to 2012.
The mean number of maintenance treatments increased with age, with averages of 1.2, 2.0, and 3.1 for age groups 18 to 39 y, 40 to 64 y and 65 y and over, respectively. Besides, the individual mean of maintenance treatments was lower than the mean of acute treatments. Regression models estimated a stable number of acute treatments and an increased number of maintenance treatments over time. The average annual increase in mean acute treatments was estimated at 0.2% (95%CI, −0.2% to 0.6%), with similar results estimated by sex and age groups. The average annual increase in maintenance treatments was estimated at 6.4% (5.5% to 7.2%) with estimations, by age group, respectively of 5.5% (3.5% to 7.5%), 7.4% (6.1% to 8.7%) and 4.8% (3.6% to 5.9%) for 18 to 39 y, 40 to 64 y and 65 y and over. The annual average increase was estimated at 6.1% (5.1% to 7.1%) for women and 7.3% (6.3% to 8.2%) for men.
ECT Diagnostic Categories
Overall, 74% of ECT treatments were dispensed for affective disorders, 19% for schizophrenia and related psychotic disorders, 2.6% for anxiety disorders, and 1.1% for personality disorders. Finally, 2.6% of medical claims were classified as “other diagnosis”. This distribution remained stable over time.
Characteristics of Hospitals and Psychiatrists Giving ECT in Quebec
Overall, 66 hospitals administered ECT in Quebec between 2008 and 2012. Given that the province of Quebec adopted a policy of hospital mergers in the final years of the study, the number of hospitals that delivered ECT varied. In 2012, there were 46 hospitals. About one-quarter of hospitals administered nearly three-quarters of all treatments and had treated two-thirds of the patients. Yet, over the same period, 16 hospitals administered less than 24 ECT treatments, corresponding to 1.7% of all patients who received ECT. This distribution was stable throughout the study period (Table 2).
Table 2.
Number of ECT Treatments According to ECT Volume Per Hospital and Psychiatrist, Quebec, 2008 To 2012.
| Number of ECTs Per Hospital or Psychiatrist | Number of Hospitals or Psychiatrists | Total Number of ECT Treatments | Proportion of ECT Treatments (%) | |
|---|---|---|---|---|
| Hospitals | 1 to 24 | 16 | 55 | 0.2 |
| 25 to 159 | 15 | 1297 | 3.7 | |
| 160 to 524 | 20 | 7,051 | 20.3 | |
| ≥525 | 15 | 26,357 | 75.8 | |
| Psychiatrists | 1 to 10 | 64 | 246 | 0.7 |
| 11 to 35 | 64 | 1,247 | 3.6 | |
| 36 to 110 | 68 | 4,687 | 13.5 | |
| ≥111 | 78 | 28,580 | 82.2 |
The number of psychiatrists who administered ECT varied little during the study period, from 329 psychiatrists in the period of 1998–2001, to 340 in 2003–2006, and 274 in 2008–2012. Over the period of 1997 to 2012, about one-quarter of the psychiatrists administered 10 treatments or less whereas another one-quarter, more than 111 treatments (Table 2).
Discussion
Our study shows for the first time in Canada that it is feasible to monitor ECT use based on medico-administrative data like the QICDSS. The overall prevalence of ECT use in Quebec between 1996 and 2012 was estimated at 13 per 100,000 inhabitants. This report highlighted a decrease in this prevalence over the study period for both men and women of all ages. Women and patients aged 65 y and over remained the population for which ECT was most often dispensed, and the main indications for ECT were affective disorders, followed by non-affective psychosis in 20% of cases. Although most ECT treatments were given for acute treatment, we noticed an increase in ECT treatments given as maintenance therapy. Finally, ECT is provided in all regions of Quebec province; for the period of 1997 to 2012, this involved 66 separate establishments, and for the year 2012 to 2013, 274 of the 1,212 (22.6%) active, registered psychiatrists.14 Regional disparities in the rates of utilisation were observed.
The CIHI reported in 2003 that 871 people received ECT in Quebec.15 This figure is comparable with that found in our study, since CIHI used only hospital separations as a source. The study by Martin et al.8 surveyed all Canadian hospital centres (including Quebec) that provided ECT in the calendar year 2006. They estimated that, in Canada, 24 people received ECT per 100,000 inhabitants, and that the prevalence in ECT treatment was 212 treatments per 100,000 inhabitants. Considering we found an average of 8.3 acute and 3.1 maintenance treatments for a total of 11.4 treatments per patient, the number of treatments found in the study by Martin et al.8 would be equivalent to 18.6 patients per 100,000 inhabitants per year in Quebec. This overestimation in the study by Martin et al.8 may be explained by the fact that their 1-y projection of population rates was derived from a projection of non-responding centres and was not age-standardised. To date, only one Canadian study in Ontario has reported the number of patients treated with ECT based on administrative physician payment data.16 This Ontario study showed that ECT prevalence remained relatively stable between 1992 and 2004. Our study is also the first to use both physician payment data and hospital data to assess ECT in Canada, considering inpatients and outpatients who received ECT, and is also the first study to use age-standardised prevalence rates. Of the cases listed, 75% were identified by both the hospitalisation database and physician claims database, 19% were exclusively identified by the physician claims database, and 6% exclusively by the hospitalisation database. Note that by using only physician claims or only hospitalisation data, 6% and one-fifth of ECT cases, respectively, would not have been captured. By linking health administrative databases, we prevented underestimating the prevalence.
Medico-administrative databases provide the opportunity to perform pan-Canadian analyses on population health and the use of health services. The Canadian Chronic Disease Surveillance System (CCDSS) is a collaborative network of provincial and territorial chronic disease surveillance systems. It has been established to merge the data after homogenisation of the provincial systems. Like the QICDSS, the CCDSS provides longitudinal data on chronic disease prevalence and incidence using physician billing claims and hospital discharge abstract records linked to provincial and territorial health insurance registries. Our algorithm for case identification in the QICDSS may be replicated in most surveillance system of other provinces; it could also provide the opportunity to study ECT use nationally and compare ECT use across Canada.
The estimated prevalence appeared to be comparable with the results found by the AETMIS in 2002.6 We report a decline in the rate of ECT use in Quebec since 2002 to 2003. Several assumptions can be made to explain this decrease: the increased use of alternative psychotropic drug treatments; the increased awareness of alternative treatments; as well as the amalgamation of hospitals and the impact of the AETMIS report, published in 2002, that supported ECT as an effective treatment, but noted inconsistent utilisation across the province, raising questions about standardisation.
Differences by gender and age were highlighted in the characteristics of patients treated with ECT. Observed repartition by gender was similar to that found in most Western countries, including Canada. Women are more likely to receive ECT than men.1,4,6,16,17 This could be explained in part by the fact that major depression affects more women than men.18–20 The strong representation of older adults may be partly due to the difficulty of treating major depression for this age group.21,22
Our results also showed that indication and practices of ECT were consistent with established international guidelines.1,23,24 Depressive disorders, such as major depression, constituted the main indication, corresponding to 75% of ECT use. This corresponds to practices observed in Western countries.4 However, this therapy remains an exceptional treatment for mental disorders. For example, based on our results, of the 900,000 people treated for mental disorders each year in Quebec,25 only 0.08% received ECT. Most ECT treatment was given at an acute phase. Finally, we observed an increase in the use of ECT as a maintenance therapy during the study period. Although this issue is poorly documented, maintenance treatments appear to be an alternative treatment, especially for patients with high risk of relapse or recurrence, such as the older patients, for whom ECT is advocated.1,6,26–29
ECT was provided by many health care institutions and psychiatrists in all regions of Quebec. Regional disparities were observed with differences in overall prevalence as well as in prevalence reduction across regions. The annual volume of ECT treatments given by psychiatrists varied considerably, with almost one-quarter of psychiatrists delivering about 4 treatments of ECT over 5 y, and another one-quarter administering an average of 366 treatments for the same period. As with any specialized medical intervention, it is necessary to question how to ensure that the skills required to administer ECT are of adequate quality and maintained by psychiatrists and other practioners in facilities that rarely administer this treatment. Our observations also led us to wonder about equality in accessing ECT and about the optimal use of ECT in the treatment of hospitalised patients suffering from serious mental disorders. Regional variations in the use of ECT do not appear to be due to the number of psychiatrists who can provide ECT, as more than one-quarter of psychiatrists provide it each year in all regions of Quebec. Its health technology agency, AETMIS, already recommended in its 2002 report that improved training of psychiatrists and nurses, as well as the improved dissemination of information to patients and relatives, patient committees, and advocacy groups during hospitalisation could improve the quality of ECT practices.
There were several limitations to our study. The first limitation was the risk of underestimating ECT prevalence due to the absence of data on general practitioner (GP) procedures in the physician claims database. Indeed, unlike psychiatrists, GPs providing ECT are not fee-for-services physicians and, thus, their ECTs are not registered among the physician claims. However, our estimates were based on physician payment data and hospital separation data, the latter adding 6% more cases than if the source would have been only physician payment data. Further, 19% of cases had no evidence of hospitalisation. We tentatively explain this discrepancy in two ways: 1) maintenance ECT may be given without hospital admission; 2) there are alternative payment methods. However, the characteristics of the QICDSS provide an opportunity to reliably monitor ECT utilisation in Quebec. It covers 98% of all insured people, who represent 99% of the Quebec population, and contains systematic data both on inpatient and outpatient treatments, diagnosis, procedures, patients and healthcare providers.9
A previous national survey, the Canadian Electroconvulsive Therapy Survey, also provided interesting information on ECT practices in Canada.7,8,24,30 Geographical access to ECT in Canada was good, with 84% of Canadians living within 1 h of an ECT facility; however, the study identified other limitations to optimal access, such as organizational, logistical, and staffing difficulties.30 We observed wide variations in ECT caseload per hospital across the country.8 Based on these observations, the authors7,8,24 concluded that an accreditation process and a standardisation of collected data would be necessary to ensure high-quality practices. Establishing a national registry on ECT in Quebec would also respond to this advocacy. An exhaustive register would provide additional information not currently available in health administrative databases, such as the technical parameters of ECT, clinical efficacy assessed using standardised scales, side effects, or adherence to treatment. This would enable us to follow ECT practices more precisely in each region of Quebec, to develop training activities on ECT according to the highest standards, and to fit the needs of Quebec health professionals.
This attention to improved quality could also lead to improved outcomes. An audit of all hospital-based suicides between 1986 and 1991 showed that 17% could have benefited from ECT at a time when ECT was used more in Quebec than elsewhere.31 In the United Kingdom, the audits of the National Confidential Enquiry on Suicide in patients who received ECT showed increased suicide risk attributed to inadequate discharge planning and community care.32 But this does not answer whether ECT made a difference in this high-risk group, nor does it allow for estimates on the loss of benefits of decreased ECT use. QICDSS data could be used to demonstrate the better outcome of hospitalised patients exposed to ECT, and how many patients could have benefited if it were provided; for instance, studies using linked administrative databases have demonstrated the benefit of anti-psychotic medication33 for patients with schizophrenia but the dangers of tranquilizers in the same patients.34
Conclusion
This study provided a detailed picture of ECT use in Quebec from 1996 to 2012 and demonstrated the feasibility of using the QICDSS to identify ECT usage rates. A decrease in the use of ECT has been observed in Quebec for both men and women of all ages. However, regional disparities in ECT use call for a deeper examination of the practice of ECT in Quebec and in Canada.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. American Psychiatric Association. American Psychiatric Association Task Force report on electroconvulsive therapy. Washington (DC): American Psychiatric Association; 2001. [Google Scholar]
- 2. Milev RV, Giacobbe P, Kennedy SH, et al. ; CANMAT Depression Work Group. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 4. Neurostimulation treatments. Can J Psychiatry. 2016;61(9):561–575. doi:10.1177/0706743716660033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McCall WV. Electroconvulsive therapy in the era of modern psychopharmacology. Int J Neuropsychopharmacol. 2001;4(3):315–324. [DOI] [PubMed] [Google Scholar]
- 4. Leiknes KA, Jarosh-von Schweder L, Høie B. Contemporary use and practice of electroconvulsive therapy worldwide. Brain Behav. 2012;2(3):283–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lesage A, Lemasson M, Medina K, et al. The prevalence of electroconvulsive therapy use since 1973: a meta-analysis. J ECT. 2016;32(4):236–242. [DOI] [PubMed] [Google Scholar]
- 6. Agence d’évaluation des technologies et des modes d’intervention en santé (AETMIS). 2002. L’utilisation des électrochocs au Québec. Rapport préparé par Reiner Banken (AETMIS 02-05 RF) Montréal (Canada): AETMIS; 2002. p xvii–103. [Google Scholar]
- 7. Gosselin C, Graf P, Milev R, et al. Delivery of electroconvulsive therapy in Canada: a first national survey report on devices and technique. J ECT. 2013;29(3):225–230. [DOI] [PubMed] [Google Scholar]
- 8. Martin BA, Delva NJ, Graf P, et al. Delivery of electroconvulsive therapy in Canada: a first national survey report on usage, treatment practice, and facilities. J ECT. 2015;31(2):119–124. [DOI] [PubMed] [Google Scholar]
- 9. Blais C, Jean S, Sirois C, et al. Quebec Integrated Chronic Disease Surveillance System (QICDSS), an innovative approach. Chronic Dis Inj Can. 2014;34(4):226–235. [PubMed] [Google Scholar]
- 10. Mossialos E, Wenzl M, Osborn R, et al. 2015 International profiles of health care systems. The Commonwealth Fund; 2016 Available from: http://www.commonwealthfund.org/publications/fund-reports/2016/jan/international-profiles-2015. Accessed October 16, 2017. [Google Scholar]
- 11. Canadian Institute for Health Information, International Statistical Classification of Disease [cited 2017 Jun 08]. Available from: https://www.cihi.ca/en/submit-data-and-view-standards/icd-9ccp-and-icd-9-cm.
- 12. Canadian Institute for Health Information, Canadian Classification of Health Information [cited 2017 Jun 8]. Available from: https://www.cihi.ca/en/submit-data-and-view-standards/codes-and-classifications/cci.
- 13. Canadian Institute for Health Information, Technical Note: 30-Day Mental Illness Readmission Rate. 2012. [cited 2017 Sep 20]. Available from: http://indicatorlibrary.cihi.ca/display/HSPIL/30-Day+Readmission+for+Mental+Illness.
- 14. RAMQ website. [cited 2017 Apr 21]. Available from: https://www4.prod.ramq.gouv.qc.ca/IST/CD/CDF_DifsnInfoStats/CDF1_CnsulInfoStatsCNC_iut/DifsnInfoStats.aspx?ETAPE_COUR=2&LANGUE=fr-CA.
- 15. Hoag H. Inducing seizures among seniors. CMAJ Can Med Assoc J. 2008;178(10):1264–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rapoport MJ, Mamdani M, Herrmann N. Electroconvulsive therapy in older adults: 13-year trends. Can J Psychiatry Rev Can Psychiatr. 2006;51(9):616–619. [DOI] [PubMed] [Google Scholar]
- 17. Smith WE, Richman A. Electroconvulsive therapy: a Canadian perspective. Can J Psychiatry Rev Can Psychiatr. 1984;29(8):693–699. [DOI] [PubMed] [Google Scholar]
- 18. Weissman MM, Klerman GL. Sex differences and the epidemiology of depression. Arch Gen Psychiatry. 1977;34(1):98–111. [DOI] [PubMed] [Google Scholar]
- 19. Kuehner C. Gender differences in unipolar depression: an update of epidemiological findings and possible explanations. Acta Psychiatr Scand. 2003;108(3):163–174. [DOI] [PubMed] [Google Scholar]
- 20. Fleury MJ, Grenier G. État de situation sur la santé mentale au Québec et réponse du système de santé et des services sociaux. Québec (Canada): Commissaire à la santé et au bien-être; 2012. [Google Scholar]
- 21. Baldwin RC, Chiu E, Katona C, et al. Guidelines on depression in older people: practising the evidence. London (GB: ): Martin Dunitz Ltd; 2002. [Google Scholar]
- 22. Coalition canadienne par la santé mentale des personnes âgées (CCSMPA). Lignes directrices nationales. La santé mentale de la personne âgée. Toronto (ON): CCSMPA; 2006. Available from: www.ccsmh.ca. Accessed March 21, 2017. [Google Scholar]
- 23. Enns MW, Reiss JP, Chan PK. Electroconvulsive therapy. Can J Psychiatry. 2010;55(6 Suppl):1–12. [Google Scholar]
- 24. Chan P, Graf P, Enns M, et al. The Canadian Survey of Standards of Electroconvulsive Therapy Practice: a call for accreditation. Can J Psychiatry Rev Can Psychiatr. 2012;57(10):634–642. [DOI] [PubMed] [Google Scholar]
- 25. Institut National de Santé Publique du Québec (INSPQ): Lesage A. D., Émond V. Number 6: Surveillance of Mental Disorders in Québec: Prevalence, Mortality and Service Utilization Profile. Chronic Disease Surveillance. Québec (Canada): INSPQ; 2013. Report No.: ISBN: 978-2-550-68121-2 (PDF). Available from: https://www.inspq.qc.ca/pdf/publications/1662_SurvMentalDisorQc_PrevMortServUtiliProfile.pdf. [Google Scholar]
- 26. Brown ED, Lee H, Scott D, et al. Efficacy of continuation/maintenance electroconvulsive therapy for the prevention of recurrence of a major depressive episode in adults with unipolar depression: a systematic review. J ECT. 2014;30(3):195–202. [DOI] [PubMed] [Google Scholar]
- 27. Kellner CH, Kaicher DC, Banerjee H, et al. Depression severity in electroconvulsive therapy (ECT) versus pharmacotherapy trials. J ECT. 2015;31(1):31–33. [DOI] [PubMed] [Google Scholar]
- 28. Petrides G, Tobias KG, Kellner CH, et al. Continuation and maintenance electroconvulsive therapy for mood disorders: review of the literature. Neuropsychobiology. 2011;64(3):129–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rabheru K. Maintenance electroconvulsive therapy (M-ECT) after acute response: examining the evidence for who, what, when, and how? J ECT. 2012;28(1):39–47. [DOI] [PubMed] [Google Scholar]
- 30. Delva NJ, Graf P, Patry S, et al. Access to electroconvulsive therapy services in Canada. J ECT. 2011;27(4):300–309. [DOI] [PubMed] [Google Scholar]
- 31. Proulx F, Lesage AD, Grunberg F. One hundred in-patient suicides. Br J Psychiatry J Ment Sci. 1997;171(3):247–250. [DOI] [PubMed] [Google Scholar]
- 32. Hunt IM, Windfuhr K, Swinson N, et al. Electroconvulsive therapy and suicide among the mentally ill in England: a national clinical survey. Psychiatry Res. 2011;187(1–2):145–149. [DOI] [PubMed] [Google Scholar]
- 33. Vanasse A, Blais L, Courteau J, et al. Comparative effectiveness and safety of antipsychotic drugs in schizophrenia treatment: a real-world observational study. Acta Psychiatr Scand. 2016;134(5):374–384. [DOI] [PubMed] [Google Scholar]
- 34. Tiihonen J, Mittendorfer-Rutz E, Torniainen M, et al. Mortality and cumulative exposure to antipsychotics, antidepressants, and benzodiazepines in patients with schizophrenia: an observational follow-up study. Am J Psychiatry. 2016;173(6):600–606. [DOI] [PubMed] [Google Scholar]