Abstract
Background
The 10/66 Dementia Research Group developed and validated a culture and education fair battery of cognitive tests for diagnosis of dementia in population‐based studies in low‐income and middle‐income countries including India.
Aims
This study examined the association between individual domains of the 10/66 battery of cognitive tests and ‘disability’ and ‘functional impairment’ in community‐dwelling older adults in South India.
Methods
One hundred twenty‐nine adults aged 60–90 years residing in Karunapura, in the city of Mysore, were interviewed in their own homes. Cognitive functioning was measured by administering the 10/66 battery of cognitive tests that composes of Community Screening Instrument for Dementia (CSI'D' COGSCORE), verbal fluency (VF) and word list memory recall (WLMR). A reliable informant was interviewed to ascertain if the subject's cognitive problems have resulted in functional impairment. Disability was measured by WHO Disability Schedule‐II (DAS).
Results
The women had significantly lower CSI'D' COGSCORE score when compared with men (p = 0.002). The presence of ‘functional impairment’ resulting from cognitive decline was significantly associated with lower scores on VF (p = 0.03), WLMR (p = 0.03) and CSI'D' COGSCOREs (p < 0.01). There was a significant inverse association between WHO DAS II score and WLMR (p = 0.004), VF (0.006) and CSI'D' COGSCORE scores (p ≤ 0.001) even after adjusting for self‐reported ischaemic heart disease, stroke, chronic obstructive airway disease, hypertension and diabetes.
Conclusions
Lower scores on individual domains of the 10/66 battery of cognitive tests are associated with higher levels of disability and functional impairment in community‐dwelling older adults. These culture and education fair tests are suitable for use in population‐based research in India. Copyright © 2015 John Wiley & Sons, Ltd.
Keywords: late life, cognitive function, disability, validation, 10/66 Dementia Research
Background
Neurocognitive disorders are a major cause of disability and mortality in late life and are associated with high costs for health systems and society (Mathers and Leonardi, 2000; Revised Global Burden of Disease (GBD) 2002 Estimates, 2004; The Dementia India Report, 2010; WHO Report, 2001). Population‐based studies in India report 7.5% and 10.6% prevalence for dementia in those aged above 60 years in urban and rural areas, respectively (Prince, 2009; The Dementia India Report, 2010). The proportion of persons with dementia is expected to increase twofold by 2030 because of the steady growth in the older population and stable increments in life expectancy (Ferri et al., 2006; Link to World Alzheimer's Report, 2009; The Dementia India Report, 2010). Although neurocognitive disorders are the second highest source of burden after tropical diseases, research in India remains minimal (Murray and Lopez, 1996).
The Global Burden of Disease report identifies cognitive impairment as one of the main causes of disability, and this has a disproportionate impact on the capacity for independent living in later life. Co‐morbidity with cardiometabolic disorders is common and interacts in complex ways to create disability and dependence (Lozano et al., 2012). Therefore, it is important to understand the contribution of cognitive disorders, relative to that of other chronic diseases, to disability and dependence.
The population‐based studies by 10/66 Dementia Research Group have assessed the impact of dementia and mild cognitive impairment on disability and dependence in late life in low‐income and middle‐income countries (LMICs) including India (Sousa et al., 2009; Sosa et al., 2012). Those with greater disability and need for care were characterised by co‐morbidity between cognitive impairment and physical and mental disorders. Dementia emerged as the leading independent cause of both disability and dependence, followed by limb weakness, stroke, depression, eyesight problems and arthritis. Neither ischaemic heart disease (IHD) nor hypertension or even chronic obstructive pulmonary disease was associated with disability or dependence. (Sousa et al., 2009; Sosa et al., 2012).
A culture and education fair battery of cognitive tests was developed, validated and normed for use in LMICs (including South India) by the 10/66 Dementia Research Group. This is suitable for use in people with little or no education (Prince et al., 2003). The 10/66 battery of cognitive tests comprises the Community Screening Instrument for Dementia (CSI'D') incorporating the Consortium to Establish a Registry for Alzheimer's Disease (CERAD) animal naming verbal fluency (VF) task, the modified CERAD 10 word list learning task with delayed recall and an informant interview for evidence of cognitive and functional decline (Prince et al., 2003; Prince et al., 2007). In the 10/66 pilot studies, the CSI'D', informant interview and the modified CERAD 10 word list learning task were independently able to predict the diagnosis of dementia (Prince et al., 2003).
The ecological validity and relationship between the individual domains of the 10/66 battery of cognitive tests and disability have not been examined in community‐dwelling older adults in India. Ecological validity refers to the extent to which the findings of a research study are able to be generalised to real‐life settings.
This study examined the association between individual domains of the 10/66 battery of cognitive tests [word list memory and recall (WLMR), VF and a global cognitive function score derived from the Community Screening Instrument for Dementia (CSI'D' COGSCORE)] and ‘disability’ and ‘functional impairment’ in community‐dwelling older adults in the city of Mysore, South India. The mediating effect of self‐reported chronic non‐communicable diseases is examined. In addition, we explored the feasibility of administering the 10/66 battery cognitive tests to an older person and a reliable informant in their own homes.
Methods
Design and setting
This single‐phase cross‐sectional validation study was carried out at the Epidemiology Research Unit, Holdsworth Memorial Hospital, Mysore, South India. The study was approved by the Ethics and Research Committee at Holdsworth Memorial Hospital.
Adults aged 60 years and above and residing at Karunapura (colony number 1), a mainly Christian community in the inner city of Mysore, were eligible to participate. All households in the study area (n = 186) were approached by a door‐to‐door survey, and study information was provided. One hundred fifty‐one individuals aged 60 years and above were identified from 138 households. One hundred twenty‐nine of them agreed to participate and were recruited along with a reliable informant after obtaining written consent. Individuals who were close to the subjects and knew them for most of their lives (spouse, relative or a friend) were considered reliable informants. If the participant was illiterate, verbal consent was obtained, which was witnessed and signed by a relative. If individuals were unable to consent (because of severe cognitive problems), assent was obtained from their nearest/authorised relative, which was witnessed.
Instruments
-
Cognitive function tests: Cognitive functioning as a continuous measure was obtained by administering the Kannada (local language) version of the 10/66 cognitive assessment battery. This is drawn principally from CSI'D' developed by the Ibadan–Indianapolis study group (Hall et al., 2000) specifically for use in cross‐cultural research and in low education settings and from the CERAD (Morris et al., 1989). The aim of the translation process was to achieve a Kannada version of the English 10/66 battery of cognitive tests that was conceptually equivalent to the study setting and practically perform in the same way. The focus was cross‐cultural and conceptual rather than on linguistic or literal equivalence. This was achieved by using forward translation (by author MK) and back translation (by authors EB and SA) methods. This battery comprises the following:
Global cognitive function measured by administering the CSI'D' to the subjects (Hall et al., 2000). This includes a 32‐item cognitive test assessing orientation, comprehension, memory, naming and language expression, which generates a global cognitive score (CSI'D' COGSCORE).
The CSI'D' was from the outset intended to be used across cultures with the minimal adaptation. It was developed and first validated among Cree American Indians (Nath et al., 1993; Hendrie et al., 1995), further validated and used in population‐based research among Nigerians in Ibadan, African Americans in Indianapolis and White Canadians in Winnipeg and in Jamaica in conjunction with the CERAD battery (Hendrie et al., 1995; Unverzagt et al., 1999; Hall et al., 2000). The CSI'D' test score distributions among those with dementia and controls and the degree of discrimination provided were remarkably consistent across the aforementioned cultural settings (Unverzagt et al., 1999).
Verbal fluency is measured by the animal naming VF task from the CERAD (Hall et al., 2000; Morris et al., 1989). After a brief practice, naming items from another category (clothing), participants are encouraged to name as many different animals as they can in the space of 1 min. The instructions read out to the participant stipulate the following: ‘think of any kinds of animal in the air, on land, in the water, in the forest, all the different animals’. If the participant stops before the allotted time has elapsed, they are encouraged to continue. The score is one point for each valid name.
Memory is measured by the modified WLMR test to evaluate immediate and delayed recall, respectively. WLMR has been reported to be of particular value in distinguishing early dementia from normal ageing (Welsh et al., 1991). WLMR is taken from the adapted CERAD 10‐word list learning task used in the Indo–US Ballabgarh dementia study (Ganguli et al., 1996). Six words—butter, arm, letter, queen, ticket and grass—were taken from the original CERAD battery English language list (Guruje et al., 1995). Pole, shore, cabin and engine were replaced with corner, stone, book and stick, which were deemed more cross‐culturally applicable (Prince et al., 2003). In the learning phase, the list is read out to the participant from a green card, who is then asked to recall straight away the words that they remember. This process is repeated three times, giving the subject a score out of 30. Approximately 5 min later, after a series of unrelated CSI'D' questions (name registration, object naming, object function and repetition), the participant is again asked to recall the 10 words with prompting that they were read from a green card, giving a recall score out of 10. This makes the total WLMR score of 40.
The CSI'D' informant interview: In the informant section of the CSI'D', a reliable informant is asked about declining memory in general and the frequency of six specific and characteristic memory lapses: forgetting where he or she has put things, where things are kept, names of friends, names of family, when he or she last saw informant and what happened the day before. If the subject was receiving care, the primary caregiver was considered as a reliable informant. The 26 items from the interview seek for evidence of cognitive and functional decline (Nath et al., 1993; Hendrie et al., 1995; Prince et al., 2003). The response to each item is weighted, and for the purpose of this study, a summative score (CSI'D' RELSCORE) of more than 2 was considered as indicative of cognitive decline resulting in ‘functional impairment’. The 10/66 battery of cognitive tests in English is provided in the Appendix, and the Kannada version will be shared upon request by interested readers.
The following instruments were administered to the participant, and if they were unable to provide accurate information (for example, because of cognitive problems or following a stroke), they were administered to the reliable informant.
Socio‐demographic questionnaire collecting information on age, sex, marital status, level of education (none; some, but did not complete primary; completed primary; completed secondary; completed tertiary or further education) and living circumstances (living with children, yes/no) (Prince et al., 2007).
Medical history questionnaire: Hypertension and diabetes were ascertained by a positive answer to the question ‘have you ever been told you had diabetes or hypertension?’ The ascertainment of previous episodes of stroke or IHD was based on self‐report (‘have you ever been told by a doctor that you had a stroke/angina/heart attack?’). Stroke was coded only if there was a clear history of sudden onset of unilateral paralysis, loss of speech or blindness lasting for more than 24 h, hence excluding previous episodes of transient ischaemic attack. Chronic obstructive airway disease (COAD) was diagnosed in people who responded ‘yes’ to the question ‘do you usually cough up phlegm from your chest first thing in the morning?’ and whose answer to the question ‘for how many months of the year does this usually happen?’ was 3 months or more (Prince et al., 2007).
Physical health impairment schedule: This is a self‐reported list of 12 commonly occurring physical impairments, a measure of health impairment (Duke University Centre for the Study of Aging and Human Development: Multidimensional Functional Assessment, 1978). They include arthritis/rheumatism, eyesight problems, hearing difficulty or deafness, persistent cough, breathlessness/asthma, high blood pressure, heart trouble/angina, stomach problems, intestine problems, faints/blackouts, skin disorders and paralysis/weakness or loss of one leg or an arm. Impairments were rated as present if they interfered with activities ‘a little’ or ‘a lot’, as opposed to ‘not at all’.
WHO Disability Schedule‐II: The degree of disability was measured by administering the WHO Disability Schedule‐II (WHO DAS II) (Rehm et al., 2000). It was developed by the WHO as a culture–fair assessment tool for use in cross‐cultural comparative epidemiological and health services research to measure activity limitation and participation restriction. The 12 items assess five activity limitation domains (communication, physical mobility, self‐care, interpersonal interaction, life activities and social participation). Each domain is covered by two questions, with scores ranging from 0 (no difficulty) to 4 (extreme difficulty or cannot do) and yielding a total score between 0 and 48.
Data collection
A clinical psychologist (EB) was trained by MK, a member of the 10/66 Dementia Research Group to administer the instruments in subjects' own homes. The interviews for participants and a key informant were carried out separately, but this was not always feasible. The data were manually collected on paper and then entered into the Epidata‐driven (version 3) database developed by the 10/66 Dementia Research Group. These files have in‐built checks to minimise errors and thereby assist in cleaning of the data. The data were double entered, cleaned and directly exported to spss version 19 for analysis.
Statistics
A power calculation was not carried out before commencing the study, as no study had previously examined the association between individual domains of the 10/66 cognitive battery and disability in an older adult population from this region. A post hoc power calculation indicated that our sample size had more than 90% power to detect a correlation of at least 0.20 between disability and exposure variables (WLMR, VF and CSI'D' COGSOCRE) significance at the 5% level (Table 1).
Descriptive statistics were performed to calculate mean, standard deviation and proportions. Independent samples t‐tests were used to test for differences in socio‐demographics, cognitive function, health impairment and disability scores between men and women. Multiple linear regression was used to examine the association between the dependent variables (WHO DAS II score) and independent variables/predictors (WLMR, VF and CSI'D' COGSCORE). The cognitive scores were adjusted for age, education and gender. The regression analyses were adjusted to examine the mediating effect of self‐reported chronic non‐communicable disorders (diabetes, hypertension, stroke, COAD and IHD).
Table 1.
Post hoc power calculation
| Dependent variable | Independent | R 2 | Effect size | Number of predictors | α | Sample size | Power |
|---|---|---|---|---|---|---|---|
| Disability | Word list memory recall | 0.245 | 0.32450 | 8 | 0.05 | 129 | 0.9987834 |
| Verbal fluency | 0.292 | 0.41243 | 8 | 0.05 | 129 | 0.9999228 | |
| CSI'D' COGSCORE | 0.281 | 0.39082 | 8 | 0.05 | 129 | 0.9998448 |
CSI'D', Community Screening Instrument for Dementia.
Results
The 129 participants included 42 men and 87 women aged between 60 and 90 years. Table 2 shows their characteristics. The women had significantly lower levels of literacy and were more likely to be widowed when compared with men (p = <0.001). Table 2 provides mean scores on individual cognitive tests, health impairment and disability for men and women.
Table 2.
General characteristics of the study participants
| Characteristics | Male (N = 42) | Female (N = 87) | p‐value |
|---|---|---|---|
| Age mean (SD) | 67.81 (6.64) | 69.46 (7.30) | 0.22 |
| Education | |||
| None | 1 (2.4%) | 28 (32.2%) | ≤0.001 |
| Some, but did not complete primary | 5 (11.9%) | 5 (5.7%) | |
| Completed primary | 5 (11.9%) | 18 (20.7%) | |
| Completed secondary (metric) | 15 (35.7%) | 24 (27.6%) | |
| Completed tertiary (college) | 16 (38.1%) | 12 (13.8%) | |
| Marital status | |||
| Never married | — | 4 (4.6%) | ≤0.001 |
| Married/co‐habiting | 31 (73.8%) | 27 (31.0%) | |
| Widowed | 11 (26.2%) | 56 (64.4%) | |
| Religion | |||
| Roman Catholic | 3 (7.1%) | 2 (2.3%) | 0.304 |
| Anglican/Protestant | 23 (54.8%) | 39 (44.8%) | |
| Muslim | 2 (4.8%) | 6 (6.9%) | |
| Hindu | 14 (33.3%) | 40 (46.0%) | |
| Job | |||
| Paid full‐time work | 3 (7.1%) | 3 (3.4%) | ≤0.001 |
| Paid part‐time work | 4 (9.5%) | 0 (0%) | |
| Housewife/husband | 4 (9.5%) | 45 (51.7%) | |
| Retired | 30 (71.4%) | 35 (40.2%) | |
| Hypertension | 6 (14.3%) | 11 (12.6%) | 0.834 |
| Ischaemic heart disease | 6 (14.3%) | 11 (12.6%) | 0.834 |
| Stroke | 2 (4.8%) | 1 (1.1%) | 0.197 |
| Diabetes | 16 (38.1%) | 27 (31.0%) | 0.478 |
| Chronic obstructive airway disease | 4 (9.5%) | 6 (6.9%) | 0.641 |
| Smoking (ever) | 7 (16.7%) | 2 (2.3%) | 0.007 |
| Alcohol (ever) | 5 (11.9%) | 0 (0%) | |
| Alcohol (present) | 5 (11.9%) | 0 (0%) | |
| Cognitive function | |||
| CSI'D' COGSCORE | 37.46 (4.27) | 34.61 (5.10) | 0.002 |
| Verbal fluency | 13.76 (4.0) | 12.03 (4.85) | 0.047 |
| Word list memory recall | 19.43 (7.23) | 17.56 (6.70) | 0.150 |
| Physical health impairment schedule score | 12.48 (1.90) | 13.18 (1.90) | 0.05 |
| WHO Disability Assessment II score | 1.76 (5.09) | 2 .29 (3.01) | 0.464 |
CSI'D', Community Screening Instrument for Dementia; SD, standard deviation.
The CSI'D' informant interview identified 33 of the 129 subjects as having cognitive decline severe enough to cause ‘functional impairment’ (i.e. CSI'D' RELSCORE of 2 or more). The associations of functional impairment and cognitive function score are provided in Table 3.
Table 3.
Association between cognition and functional impairment
| Cognitive function | Functional impairment (n = 23) | No functional impairment (n = 106) | p‐value |
|---|---|---|---|
| CSI'D' COGSCORE | 32.82 (5.61) | 36.47 (4.44) | <0.01 |
| Verbal fluency | 11.0 (4.52) | 13.40 (4.52) | 0.03 |
| Word list memory recall | 15.94 (6.38) | 18.94 (6.94) | 0.03 |
CSI'D', Community Screening Instrument for Dementia.
The association between cognitive function and disability score (WHO DAS II) was examined in regression analyses (Table 4). The analyses were adjusted for age, education and gender. There was a significant inverse association between WHO DAS II score and WLMR (p = 0.004), VF (0.006) and CSI'D' COGSCORE scores (p ≤ 0.001) even after adjusting for self‐reported IHD, stroke, COAD, hypertension and diabetes.
Table 4.
Association between cognition and disability
| Dependent variable | Predictors | Beta coefficient | 95% CI value | p‐values |
|---|---|---|---|---|
| WHO DAS II score | CSI'D' COGSCORE | −0.282 | −0.408, −0.155 | ≤0.001 |
| Verbal fluency | −0.215 | −0.366, −0.064 | 0.006 | |
| Word list memory and recall | −0.150 | −0.25, −0.05 | 0.004 |
CI, confidence interval; CSI'D', Community Screening Instrument for Dementia; WHO DAS II, WHO Disability Assessment Score Version II.
Predictors are adjusted for age, education and gender. The regression analyses were adjusted for ischaemic heart disease, stroke, chronic obstructive airway disease, hypertension and diabetes.
Discussion
Lower scores on individual domains of the 10/66 battery of cognitive tests are associated with higher levels of disability and functional impairment in community‐dwelling older adults in Mysore, South India. This is the first population‐based ecological validation study of the 10/66 instruments in India to examine these associations. The association between CSI'D' COGSCORE, VF, WLMR scores and disability was strong and independent of self‐reported chronic non‐communicable disorders. The associations between lower cognitive function scores and disability in late life were not attenuated after adjusting for chronic non‐communicable disorders. Our finding is similar to the observation by the 10/66 Dementia Research Group that dementia and amnesic mild cognitive impairment independently predict disability in late life (Sosa et al., 2012). Unlike the previous 10/66 research reports from India that examined the impact of diagnostic categories of cognitive impairment (amnesic mild cognitive impairment and dementia) on disability, this study examined cognitive function as a continuous variable.
Independently, all three cognitive function tests were able to identify individuals with ‘functional impairment’ because of cognitive problems in this sample of community‐dwelling older adult population where nearly a third of them were illiterates. This reconfirms ‘culture and education fair’ properties of the 10/66 cognitive tests and that these are well suited for identification of older adults with cognitive and functional impairment at a population level in LMIC setting.
In this study, women had significantly lower global cognitive function score (CSI'D' COGSCORE) than men. This may be due to lower education levels attained by the women in the study. Interestingly, despite lower attained educational levels and lower CSI'D' COGSCORE, there were no significant gender differences in disability. This may be partly explained by the fact that health impairment between men and women was the same, but this needs to be examined further.
It was feasible to administer the 10/66 instruments in participants' own homes, and all assessments were completed. Administering a battery of cognitive tests to an older adult and interviewing an informant in their own homes have its strengths and weaknesses. It was a challenge to administer cognitive tests in a standardised manner while strictly adhering to the test protocol. The reasons include the following: limited physical space, lack of privacy, poor lighting, noise levels and in some instances family members and friends attempting to prompt or answer for the subject despite clear instructions not to do so. However, being at the participants' own home provided an opportunity to observe them in familiar surroundings, and it was easier to identify reliable informants. The informants were generally reluctant to report certain information like toileting needs, getting lost in the neighbourhood and needing assistance with personal care out of respect to their elders. This may have potentially resulted in underreporting of cognitive and functional decline by the informants.
Strengths
This study was carried out in an inner city area of the district with even distribution of families across various socio‐economic classes. Therefore, the sample is likely to represent normal community‐dwelling older adults in Mysore. A reliable informant was interviewed for all the participants. In those who were receiving care, the main ‘hands on’ caregiver was interviewed. The few refusals to participate were mainly due to social inconvenience (e.g. visitors at home, festivities and ceremonies) and not genuine unwillingness to participate. The clinical psychologist was supervised to ensure that tests were administered in a standardised manner. There were no missing data, and all analyses are complete.
Limitations
The major limitation of this validation study is that no diagnostic interview schedule was administered to determine if the participants had a diagnosable mental disorder particularly depression and dementia. Depression is a common co‐morbidity with cognitive disorders and enhances the resulting impairment and disability in late life. This limitation was partly overcome by administering a CSI'D' informant interview that generated a final score indicating if the subjects' cognitive problems were severe enough to impair the subject's activities of daily life and any other functional impact. All chronic diseases were self‐reported with a negligible few having any medical records to verify.
Abbreviations
- CSI'D'
Community Screening Instrument for Dementia
- WHO DAS II
WHO Disability Assessment Score Version II
- COAD
chronic obstructive airway disease
- VF
verbal fluency
- WLMR
word list memory recall
- CERAD
The Consortium to Establish a Registry for Alzheimer's Disease
Conflict of interest
None of the authors have any conflict of interest to declare.
Key points.
10/66 cognitive tests are well suited for identification of older adults with cognitive and functional impairment at a population level in LMIC setting.
Lower scores on individual domains of the 10/66 battery of cognitive tests are associated with higher levels of disability and functional impairment.
It is feasible to administer 10/66 cognitive assessments in participant's own homes in India.
10/66 cognitive tests are education and culture fair, suitable for use in population‐based research in India.
Acknowledgements
This study was funded by the Wellcome DBT India Alliance as an Early Career Research Fellowship to Dr Murali Krishna. Our sincere thanks go to the participants and their families for taking part in this study. We thank Mr Kiran K Nagaraj, CSI Holdsworth Memorial Hospital, for his assistance with data management.
Appendix Appendix. The Community Screening Instrument for Dementia (CSI‐D)
WORD LIST LEARNING
I am now going to read out a list of words. Please listen carefully, as I will ask you to repeat them back to me when I have finished. The words are on this green card
Read out the ten words, pausing for one second between each. Score correct words on the grid below
| 1ST | 2ND | 3RD | ||
| BUTTER | BUTTER | |||
| ARM | ARM | |||
| LETTER | LETTER | |||
| QUEEN | QUEEN | |||
| TICKET | TICKET | |||
| GRASS | GRASS | |||
| CORNER | CORNER | |||
| STONE | STONE | |||
| BOOK | BOOK | |||
| STICK | STICK | |||
| TOTAL SCORE |
1st trial
1. {LEARN1} ###
Now please tell me all the words you can remember
Interviewer—Score total number of words correctly recalled
2nd trial
Thank you. Now I will read out the words to you one more time. Again, please listen carefully, as I will ask you to repeat the words when I have finished.
Interviewer—Read out the ten words, pausing for one second between each.
2. {LEARN2} ##
Now please tell me all the words you can remember
Interviewer—Score total number of words correctly recalled
3rd trial
Thank you. Now I will read out the words to you one last time. Again, please listen carefully, as I will ask you to repeat the words when I have finished.
Interviewer—Read out the ten words, pausing for one second between each.
3. {LEARN3} ##
Now please tell me all the words you can remember
Interviewer—Score total number of words correctly recalled.
4. {NAME} #
I'd like you to remember my name.
My last name is xxxxxxxxx. Can you repeat that please?
- Cannot repeat name
0
- Successfully repeats name
1
We will begin with naming things. I will point to something and i would like you to tell me the name of the object. For example
5. {PENCIL} #
(Interviewer shows a pencil)
What is this called?
- Incorrect
0
- Correct
1
6. {WATCH} #
(Interviewer points to their watch)
What is this?
- Incorrect
0
- Correct
1
7. {CHAIR} #
(Interviewer pats chair)
What about this?
- Incorrect
0
- Correct
1
8. {SHOES} #
(Interviewer points to shoes [or socks or stockings if they have left shoes outside])
And these?
- Incorrect
0
- Correct
1
9. {KNUCKLE} #
(Interviewer shows their knuckles)
What do we call these?
- Incorrect
0
- Correct
1
10. {ELBOW} #
(Interviewer points to their elbow)
What do we call this?
- Incorrect
0
- Correct
1
11. {SHOULD} #
(Interviewer points to their shoulder)
What do we call this?
- Incorrect
0
- Correct
1
I was just showing you things and you told me what we call them. Now i will tell you the name of something and i want you to describe what it is. For example
12. {BRIDGE} #
What is a bridge?
Incorrect 0
Correct* 1
*Correct answers: to walk across water, to climb up, etc.
13. {HAMMER} #
What do you do with a hammer?
- Incorrect
0
- Correct*
1
*Correct answers: to drive a nail into something
14. {PRAY} #
What do people do in a church/ temple/ mosque(as appropriate)
- Incorrect
0
- Correct*
1
*Correct answers: to pray, to wed
15. {CHEMIST} #
Where do we go to buy medicine?
- Incorrect
0
- Correct*
1
*Correct answers: chemist, pharmacy, etc. (accept locally appropriate answers)
16. {REPEAT} #
Now I would like you to repeat what I say.
(Only one presentation is allowed, so the interviewer must read the phrase clearly and slowly enunciating carefully)
‘No ifs, ands or buts’
- Incorrect
0
- Correct
1
(exact phrase only)
WORD LIST LEARNING—delayed recall
Do you remember that I readout to you a list of words on a green card? How many of those words do you remember now? Could you please tell me all the words you can remember?
Interviewer—Score correct words in the grid below
| BUTTER | |
| ARM | |
| LETTER | |
| QUEEN | |
| TICKET | |
| GRASS | |
| CORNER | |
| STONE | |
| BOOK | |
| STICK | |
| TOTAL SCORE |
17. {RECALL} ##
Total number of words correctly recalled
18. {NRECALL} #
Do you remember my name? What is it?
- Incorrect
0
- Correct
1
(allow minor errors)
19. Now we are going to do something a little different, I am going to give you a category, and I want you to name, as fast as you can, all of the things that belong in that category. For example, if I say ‘articles of clothing’ you could say shirt, tie or hat. Can you think of other articles of clothing.
Wait for the subject to give two words. If the subject succeeds, indicate that the responses were correct and proceed to the test itself. If the subject gives an inappropriate word or reply, correct the response and repeat the instructions. If it becomes clear that the subject still does not understand the instruction, terminate this task and explain why this is so. After you are satisfied that the subject understands the task and has given two words naming articles of clothing, say:
That's fine. I want you to name things that belong to another category, ‘animals’. I want you to think about all the many different kinds of animal you know. Think of any kinds of animal in the air, on land, in the water, in the forest, all the different animals. Now I would like for you to tell the names for as many different animals as you can. You will have a minute to do this. Are you ready? Let's begin.
Allow one minute precisely. If the subject stops before the end of the time, encourage them to try to find more words. If they are silent for 15 seconds repeat the basic instruction (‘I want you to tell me all the animals you can think of’). No extension on the time limit is made in the event that the instruction has to be repeated.
(The score is the sum of acceptable animals. Any member of the animal kingdom, real or mythical, is scored correct, except repetitions and proper nouns. Specifically, each of the following gets credit: a species name and any accompanying breeds within the species; male, female and infant names within the species).
19. {ANIMALS}##
Number of animals in one minute
20. Now I am going to tell you three words and I would like you to repeat them after me.
Boat
House
Fish
Interviewer—Score one point for each correct word on first attempt
20.1 {WORDIMM}#
First trial score
- No words remembered
0
- 1. word remembered
1
- 2. words remembered
2
- 3. words remembered
3
Then go on to repeat the three words, up to a total of six times until the subject has remembered them all correctly
20.2 {TRIALNO} #
Record number of trials until repeated successfully
Very good, now try to remember these words because I will be asking you later.
21. {TOWN} #
What is the name of this city/town/village (as appropriate)?
- Incorrect
0
- Correct
1
22. {CHIEF} #
What is the name of the mayor/village head (as appropriate)?
- Incorrect
0
- Correct
1
23. {STREET} #
What are the names of two main streets near here?
Or (if inappropriate)
What is the name of a river near here?
- Incorrect
0
- Correct
1
24. {STORE} #
Where is the local market/ local store?
- Incorrect
0
- Correct
1
25. {ADDRESS} #
What is your address?
Or (if inappropriate)
Who lives next door?
- Incorrect
0
- Correct
1
26. {WORDDEL} #
Do you remember the three words I told you a few minutes ago?
- No words remembered
0
- 1. word remembered
1
- 2. words remembered
2
- 3. words remembered
3
27. {LONGMEM} #
Long term memory
Construct a locally appropriate equivalent of
- USA
What is the name of the civil rights leader who was assassinated in Memphis in 1968?
- Nigeria
Who was the military leader of the Ibos during the Nigerian Civil war fought between 1967–1970?
- Incorrect
0
- Correct
1
The key to this is to give the participant the date and the event and ask them for the identity of the famous person who was involved. The event should be so well known that practically no non‐demented person should get it wrong!
Now I would like to ask some questions about time
28. {MONTH} #
What month is it?
- Incorrect
0
- Correct
1
29. {DAY} #
What day of the week?
- Incorrect
0
- Correct
1
30. {YEAR} #
What year is it?
- Incorrect
0
- Correct
1
(within one year)
31. {SEASON} #
What season is it?
- Incorrect
0
- Correct
1
(Wet and dry were the appropriate alternatives in Nigeria)
I am going to ask you to carry out some actions so please listen carefully, because I will only tell you one time
(Interviewer—Give complete instructions at one time, do not give step by step)
32. {NOD} #
Please nod your head
- Incorrect
0
- Correct
1
33. {POINT} #
Please point first to the window and then to the door
- Incorrect
0
- Correct
1
34. {PAPER} #
I'm going to give you a piece of paper. When I do, take the paper in your right hand, fold the paper in half with both hands, and put the paper down on your lap.
Score one point for each component carried out correctly
Completely incorrect 0
Uses right hand 1
Folds in two 1
Places in lap 1
(maximum score = 3)
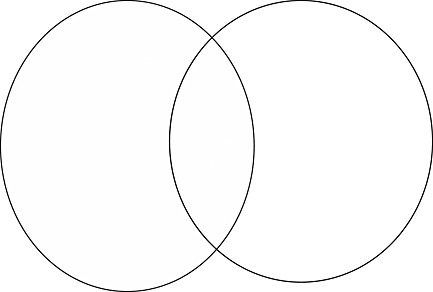
35. Now I would like you to take my pencil and copy these figures in the space given below them on the sheet
See figures on next two sheets
35.1 {CIRCLE} #
Score for circles
- Incorrect
0
- Correct
1
Score one if two vaguely circular objects intersect to form a meniscus
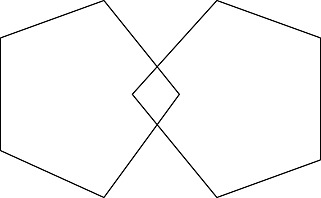
35.2 {PENTAG} #
Score for pentagons
- Incorrect
0
- Correct
1
Score one if two five sided objects intersect to form a diamond shape
36. Now I will tell a short story, then I will ask you to repeat as much of the story as you can remember. I want you to listen very carefully because I want you to try to tell me the whole story with as many details as you can remember.
Three children were alone at home and the house caught on fire. A brave man managed to climb in a back window and carry them to safety. Aside from minor cuts and bruises, all were well.
Now I would like you tell me the story in as much detail as possible
36. {STORY} #
Story recall – total items recalled
Interviewer—Score one point for each component correctly recalled
3 children 1
house on fire 1
brave man climbed 1
children rescued 1
minor injuries 1
everyone well 1
(maximum score = 6)
Krishna, M. , Beulah, E. , Jones, S. , Sundarachari, R. , A, S. , Kumaran, K. , Karat, S. C. , Copeland, J. R. M. , Prince, M. , and Fall, C. (2016) Cognitive function and disability in late life: an ecological validation of the 10/66 battery of cognitive tests among community‐dwelling older adults in South India. Int J Geriatr Psychiatry, 31: 879–891. doi: 10.1002/gps.4404.
References
- Duke University Centre for the Study of Aging and Human Development: Multidimensional Functional Assessment . 1978. The OARS Methodology. Duke University: Durham NC. [Google Scholar]
- Ferri C, Prince M, Brayn C, et al. 2006. Global prevalence of dementia: a Delphi consensus study. Lancet 366: 2112–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganguli M, Chandra V, Gilby JE, et al. 1996. Cognitive test performance in a community based non‐demented elderly sample in rural India: the Indo‐U.S. Cross‐national Dementia Epidemiology Study. Int Psychogeriatr 8(4): 507–524. DOI: 10.1016/S0140-6736(14)61682-2. [DOI] [PubMed] [Google Scholar]
- Guruje O, Unverzargt FW, Osuntokun BO, et al. 1995. The CERAD neuropsychological test battery: norms from a Yoruba‐speaking Nigerian sample. West Afr J Med 14(1): 29–33. [PubMed] [Google Scholar]
- Hall KS, Gao S, Emsley CL, et al. 2000. Community screening interview for dementia (CSI'D'); performance in five disparate study sites. Int J Geriatr Psychiatry 15(6): 521–531. [DOI] [PubMed] [Google Scholar]
- Hall KS, Hendrie HC, Brittain HM, et al. 1993. The development of a dementia screening interview in two distinct languages. Int J Methods Psychiatr Res 3: 1–28. [Google Scholar]
- Hendrie HC, Osuntokun BO, Hall KS, Ogunniyi AO, et al. 1995. Prevalence of Alzheimer's disease and dementia in two communities: Nigerian Africans and African Americans. Am J Psychiatr 152: 1485–1492. [DOI] [PubMed] [Google Scholar]
- Link to World Alzheimer's Report, 2009. Available at: http://www.alz.co.uk/research/files/WorldAlzheimerReport.pdf.
- Lozano R, Naghavi M, Foreman K, et al. 2012. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859): 2095–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathers C, Leonardi M. 2000. Global Burden of Dementia in the Year 2000 Summary of Methods and Data Sources. World Health Organization: Geneva. [Google Scholar]
- Morris JC, Heyman A, Mohs RC, et al. 1989. The Consortium to Establish a Registry for Alzheimer's Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer's disease. Neurology 39(9): 1159–1165. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. 1996. The global burden of disease In A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries and Risk Factors in 1990 and Projected to 2020. Harvard School of Public Health, Harvard University Press: Boston. [Google Scholar]
- Nath A, Blue A, Kaufert J, et al. 1993. Alzheimer's disease is rare in Cree. Int Psychogeriatr 5(1): 5–14. [DOI] [PubMed] [Google Scholar]
- Prince M, Acosta D, Chiu H, et al. 2003. Dementia diagnosis in developing countries: a cross‐cultural validation study. Lancet 361(9361): 909–917. [DOI] [PubMed] [Google Scholar]
- Prince M, Ferri CP, Acosta D, et al. 2007. The protocols for the 10/66 Dementia Research Group population‐based research programme. BMC Public Health 7: 165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince M. 2009. The 10/66 Dementia Research Group—10 years on. Indian J Psychiatr 51(5): 8–15. [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Ustun TB, Saxena S. 2000. On the development and psychometric testing of the WHO screening instrument to assess disablement in the general population. Int J Methods Psychiatr Res 8: 110–122. [Google Scholar]
- Revised Global Burden of Disease (GBD) 2002 Estimates . 2004. 2004 World Health Report. World Health Organization: Geneva. [Google Scholar]
- Sosa AL, Albanese E, Stephan BC, et al. 2012. Prevalence, distribution, and impact of mild cognitive impairment in Latin America, China, and India: a 10/66 population‐based study. PLoS Med 9(2): e1001170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sousa RM, Ferri CP, Acosta D, et al. 2009. Contribution of chronic diseases to disability in elderly people in countries with low and middle incomes: a 10/66 Dementia Research Group population‐based survey. Lancet 28(9704)374: 1821–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Dementia India Report . 2010. Prevalence, Impact, Costs and Services for Dementia, Shaji KS, Jotheeswaran AT, Girish N, et al. (eds.). Alzheimer's and Related Disorders Society India: New Delhi. [Google Scholar]
- Unverzagt FW, Morgan OS, Thesiger CH, et al. 1999. Clinical utility of CERAD neuropsychological battery in elderly Jamaicans. J Int Neuropsychol Soc 5(3): 255–259. [DOI] [PubMed] [Google Scholar]
- Welsh K, Butters N, Hughes J, et al. 1991. Detection of abnormal memory decline in mild cases of Alzheimer's disease using CERAD neuropsychological measures. Arch Neurol 48(3): 278–281. [DOI] [PubMed] [Google Scholar]
- Report WH. 2001. Mental Health: New Understanding, New Hope. World Health Organization: Geneva. [Google Scholar]


