Abstract
Objectives
Health care professionals and the health care environment play a central role in protecting pregnant and post‐partum women and their infants from smoking‐related harms. This study aimed to better understand the health professional's perspective on how interactions between women, health care professionals, and the environment influence how smoking is managed.
Design
Semi‐structured interviews and focus groups.
Methods
Data were from 48 health care staff involved in antenatal or post‐partum care at two UK sites, including midwives, obstetricians, health visitors, GPs, pharmacists, service commissioners, and Stop Smoking Service (SSS) advisors and managers. Thematic analysis was guided by a social–ecological framework (SEF).
Results
Themes were divided across three SEF levels and represented factors connected to the management of smoking in the health care context and the beliefs and behaviour of pregnant or post‐partum smokers. Organizational level: Service reconfigurations, ‘last resort’ nicotine replacement therapy prescribing policies, and non‐mandatory training were largely negative factors. There were mixed views on opt‐out referral pathways and positive views on carbon monoxide monitoring. Interpersonal level: Protection of client–professional relationships often inhibited frank discussions about smoking, and weak interservice relationships affected SSS referral motivation and quality. Individual level: Professionals felt community midwives had primary responsibility for managing smoking, although midwives felt underskilled doing this. Midwives’ perceived priority for addressing smoking was influenced by the demands from unrelated organizational initiatives.
Conclusions
Opportunities to improve clinical support for pregnant smokers exist at organizational, interservice, and health care professional levels. Interactions between levels reflect the importance of simultaneously addressing different level‐specific barriers to smoking cessation in pregnancy.
Statement of contribution.
What is already known on this subject?
Few health care professionals discuss smoking cessation support with pregnant or post‐partum women.
Identified health care professional‐related barriers to supporting pregnant and post‐partum women to stop smoking include deficits in knowledge and confidence, perceived lack of time, and concerns about damaging client relationships.
There is currently a gap in understanding regarding the barriers and facilitators to supporting this group and how interactions between the health care environment and health care professionals influence the way smoking is addressed.
What does this study add?
This study identifies modifiable factors that can influence cessation support delivery to pregnant and post‐partum women.
These factors are mapped across organizational, interpersonal, and individual health care professional levels.
Service structure, communication pathways, and policies appear to influence what cessation support is offered.
Interpersonal and individual factors influence how this support is delivered.
Keywords: health professional, postpartum, pregnancy, qualitative, smoking, smoking cessation, social‐ecological model
Background
Antenatal smoking is strongly associated with health complications including miscarriage (Pineles, Park, & Samet, 2014), stillbirth (Flenady et al., 2011), spontaneous preterm birth, small for gestational age (Moore, Blatt, Chen, Van, & Defranco, 2016), asthma (Moshammer et al., 2006), and childhood obesity (Oken, Levitan, & Gillman, 2008). In the United Kingdom, approximately 12% of women smoke throughout pregnancy (Health and Social Care Information Centre, 2016; The NHS Information Centre, 2011). Rates of smoking in pregnancy vary significantly between countries, with prevalence close to zero in some lower income countries, to as high as one in three in more disadvantaged populations or among women with mental health or substance use problems in some high‐income countries (Bloch et al., 2008; Centers for Disease Control and Prevention, 2012). Smoking is closely linked with deprivation in high‐income countries, with tobacco use rates around five times higher among the most deprived compared with the least deprived women in the United Kingdom (Raisanen et al., 2014; The NHS Information Centre, 2011).
While many pregnant and post‐partum smokers or ex‐smokers report positive smoking cessation support from health care professionals (Flemming, McCaughan, Angus, & Graham, 2015), some professionals’ actions or lack of action is perceived as a barrier to quitting. These include a perceived reticence to discuss smoking, reinforcing and praising cutting down behaviour, and failing to provide practical help or revisit smoking at subsequent appointments (Flemming et al., 2015; Lendahls, Ohman, Liljestrand, & Hakansson, 2002; Naughton, Eborall, & Sutton, 2013). From the perspective of pregnant or recently pregnant women, therefore, the way health care professionals manage smoking, and health care organizations support their staff to do so, could be improved.
Most clinicians working with pregnant women (such as midwives, GPs, and obstetricians) perceive addressing smoking to be part of their role (Beenstock et al., 2012; Glover, Paynter, Bullen, & Kristensen, 2008; Roske, Hannover, Thyrian, John, & Hannich, 2009) and report that they routinely ask about or record women's smoking status (Glover et al., 2008; Jordan, Dake, & Price, 2006; Roske et al., 2009). Surveys indicate, however, that only around one‐third of professionals across these groups routinely discuss support or treatment options for cessation and less than one quarter follow up women to ask about their smoking after an initial discussion (Abatemarco, Steinberg, & Delnevo, 2007; Jordan et al., 2006; Price, Jordan, & Dake, 2006b). Although midwives are reported to be more likely to provide risk information than other pregnancy‐orientated health care professionals (Abatemarco et al., 2007; Chang et al., 2013), they are much less likely to recommend that women abstain from smoking completely (Glover et al., 2008). This matches the experience reported by pregnant smokers (Owen & Penn, 1999; Ussher, Etter, & West, 2006).
Several qualitative studies have explored the factors that influence health care professionals’ decisions about, and management of, antenatal smoking. Professionals commonly report feeling that they lack the skills, confidence, motivation, and the time to address, discuss, and advise on smoking (Colomar et al., 2015; Flemming et al., 2016; Herberts & Sykes, 2012). These are not clearly addressed by training in brief advice (Althabe et al., 2016). Health care professionals, particularly midwives, also express concern that discussing smoking could negatively affect the therapeutic relationship between them and their clients (Flemming et al., 2016; Herberts & Sykes, 2012; Reardon & Grogan, 2016). Few studies, however, have investigated the interactions between the health care environment and health care professionals and how this influences the way antenatal smoking is addressed.
Understanding this is likely to be of high importance. For example, previous research has suggested that the type of team a midwife works in (community/integrated vs. hospital/clinic) is far more important in determining smoking cessation referral behaviour than the cessation training received or length of time they have worked as a midwife (Beenstock et al., 2012). A further perceived barrier to addressing prenatal smoking is lacking a cohesive and coordinated interorganizational strategy and the funding to implement it (Borland, Babayan, Irfan, & Schwartz, 2013). A lack of service protocols to implement cessation interventions has also been highlighted as an inhibiter of support access (Colomar et al., 2015).
In the United Kingdom, based on national guidance (National Institute for Health and Care Excellence, 2010), many maternity teams have implemented an ‘opt‐out’ referral pathway. This means that all pregnant women are screened at maternity booking appointments for carbon monoxide (CO) exposure, using CO monitors, with the most likely source being active smoking. In the absence of any objection, those identified as smokers are automatically referred to specialist cessation support. Where this pathway has been implemented, both staff and pregnant women considered it broadly acceptable (Campbell et al., 2017) although less so the automatic referral component (Sloan et al., 2016). Despite growing implementation of the opt‐out protocol, comparatively little is known about the views of health care professionals on this intervention. While the implementation of an opt‐out pathway has been associated with a twofold increase in support access and cessation during pregnancy (Bell et al., 2017; Campbell et al., 2017), only a minority of pregnant smokers ultimately have access to this pathway (Health and Social Care Information Centre, 2015). Therefore, it is important to increase our understanding of interactions between health care professionals and pregnant smokers generally, as well as those connected with opt‐out referrals.
We undertook a qualitative study that aimed to fill the gaps in our understanding outlined above. Specifically, we set out to explore the psychological, social, and environmental factors that influence the behaviour of health care professionals regarding smoking and smoking cessation in pregnancy. To obtain a range of views and experiences, we interviewed staff from two sites in different parts of the United Kingdom – one in Scotland (smoking rates in pregnancy 17.3%) (Salomi Barkat et al., 2015) and one in England (smoking rate at the time of delivery 13.7%) (Office for National Statistics, 2013) with different referral pathways to specialist smoking cessation support.
Methods
Design and participants
All interviews and focus groups were guided by a semi‐structured topic guide. Participants were health care staff (hereafter referred to as health care professionals) who had a significant role in the provision of care or smoking cessation support to women during pregnancy or immediately after delivery in one of two National Health Service (NHS) sites. Due to the small number of some types of staff, the specific locations of these two sites will remain confidential to preserve anonymity. Recruitment was guided by a target quota determined by the level of involvement for each health care role in smoking in pregnancy and to reflect perspectives of a range of professional groups. We aimed to recruit midwives and midwifery managers (target n = 18), obstetricians (target n = 2), health visitors (target n = 4), primary care physicians (GPs) (target n = 2), pharmacists (target n = 2), smoking cessation service managers and advisors (target n = 10), and service commissioners (target n = 2). Inclusion criteria were 16 years old or over and English speaking.
Participants were recruited through health care organizations using a multichannel approach, including attendance at team meetings, contact with team leaders, and use of email invitations. Due to this approach, the exact number of health professionals approached, and therefore recruitment rate, could not be reliably calculated. Relationships with participants were not established prior to the study. Recruitment took place between October 2013 and July 2014. This manuscript adheres to the COREQ checklist (Tong, Sainsbury, & Craig, 2007).
Procedure
Health care professionals at both sites were approached by a researcher and provided with a participant information sheet. Those agreeing to participate gave written informed consent prior to interviews or focus groups. All interviews and focus groups were conducted by female researchers: LB (PhD), LS (BSc), JM (MSc), and DM (RN, MSc). Researchers had varied research experience, including extensive experience of addictive behaviour and smoking in pregnancy (LB, LS, JM) and qualitative methods (LB, JM & DM). Four professionals participated in a telephone interview and all others in a face‐to‐face interview/focus group in their workplace, with no non‐participants present. Focus groups were conducted where there was a significant number of relevant staff in similar roles, for example, smoking cessation advisors and midwives. The topic guide used was informed by the theory of planned behaviour (TPB) (Ajzen, 1988) and the research team's previous and ongoing research into smoking and pregnancy. The topic guide included questions focused on caring for pregnant and post‐partum smokers and in particular focused on health care professionals’ attitudes towards smoking and its impact on maternal health, prior experience and confidence in discussing smoking and providing advice and support, relevant training received, and perceived barriers to and facilitators of providing cessation support. Participants were also asked about their perception of what they think pregnant women expect in terms of a discussion on smoking, their perception of the effectiveness of available smoking cessation interventions, and the clinical importance of addressing smoking in pregnancy relative to other risk factors (Appendix S1).
Participants were informed that the researchers had a broad interest in this topic and simply sought out their views. All interviews and focus groups were audio‐recorded and transcribed verbatim; no field notes were taken. Individual interviews ranged from 17 min to an hour and a quarter, and focus groups and paired interviews lasted approximately 1 hr. This variation was influenced by work schedules and the extent to which smoking cessation was part of each professional's role.
Analysis
Analysis was guided by Braun and Clarke's phases of thematic analysis (Braun & Clarke, 2006) and set within the interpretivist paradigm. This paradigm considers participant accounts elicited during research interactions as representing one of many possible ‘truths’ and that interpretations of these interactions are influenced by the researchers’ knowledge, beliefs, and values. We did not specifically analyse dynamics between participants in the focus groups. NVivo (version 10) (QSR International, 2012) was used to facilitate the coding and analysis.
While the TPB informed the topic guide, during data collection it became apparent that this framework was not optimal for representing, describing, and understanding the data. Instead, a social–ecological framework (SEF) (Schneider & Stokols, 2009) was chosen to represent participant views and experiences, which were structured according to multiple layers of influence. An SEF conceptualizes behaviour as the outcome of an individual's interactions with their environment. It places the individual in the middle of a series of concentric rings, each one representing a layer of influence from the micro (individual) to the macro (society) level (Figure 1). We adopted an SEF that covered three levels of influence: the individual health care professional, their interpersonal relationships with pregnant women and other professionals, and the organization within which they worked, including their policies, guidelines, and cultures. While some uses of an SEF include community and societal levels, little relevant data were collected at these levels in this study. After familiarization, several transcripts were microcoded and identified codes were categorized into one of three SEF levels. Several additional transcripts were then coded using the draft framework with any new identified concepts added. Coding consistency was assessed through five instances of dual coding among three researchers. NVivo's coding consistency queries were used to help identify codes with potentially poor overlap between coders, using alpha <0.7 as a cut‐off for further investigation. This identified several codes that had been inconsistently applied. The researchers then discussed these and made changes to the coding framework to improve coherence and validity (Figure S1). Once all transcripts had been coded, the researchers read and re‐read the coded content and summarized the emerging key findings into higher order categories. Consistent with ‘axial coding’ (Strauss & Corbin, 1998), the researchers explored how categories were interrelated, leading to the emergence of preliminary themes. Through exploration, discussion, and mapping back onto the coded and raw data, each of the themes was refined and integrated into one of the three levels of the SEF. During the analysis, where appropriate, particular attention was paid to the similarities and differences in views of different types of health care professional and also to any ‘deviant’ or ‘negative’ views (Green & Thorogood, 2014). No repeat interviews were undertaken and participant feedback on the findings was not invited due to resource constraints.
Figure 1.
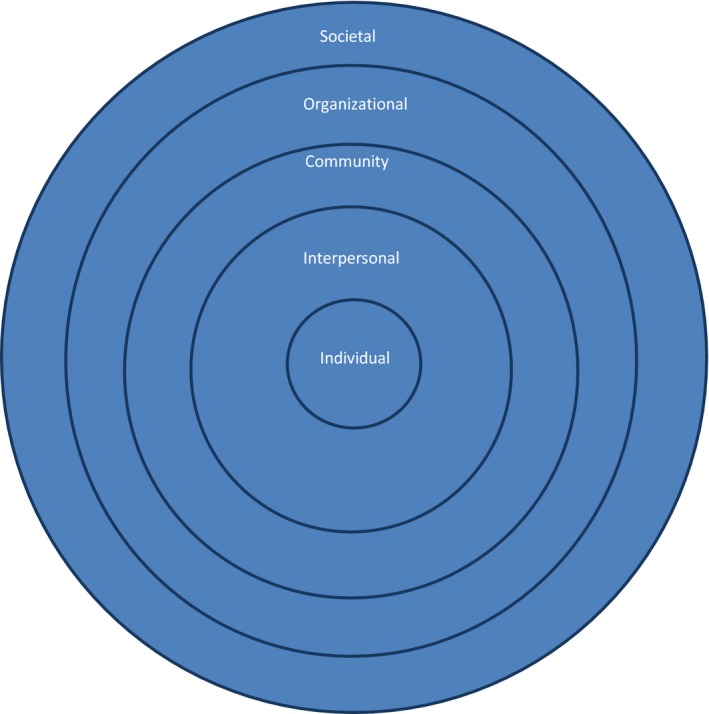
A social–ecological framework for smoking cessation in pregnancy: spheres of influence on barriers and facilitators. [Colour figure can be viewed at http://wileyonlinelibrary.com]
Findings
Forty‐eight health care professionals participated in the study: 22 across four focus groups, four in paired interviews, and 22 in one‐to‐one interviews (including four by telephone). Participants were midwives/midwifery managers (n = 17), health visitors (n = 4), Stop Smoking Service (SSS) advisors/managers (n = 19), obstetricians (n = 2), GPs (n = 2), service commissioners (n = 2), and community pharmacists (n = 2). Only one participant was male. There was a wide range of professional experience ranging from those who had worked in the NHS for several decades to staff who were newly qualified. Similarly, age ranged from early twenties to mid‐sixties.
The findings are divided into three main ‘levels’ of the SEF used: ‘organizational’, ‘interpersonal’, and ‘individual’. While these levels are presented separately, interactions between the different levels emerged, some of which are integrated into the findings and others are described in the discussion.
Organizational
Participants stated that overall organizational support available for pregnant smokers was heavily influenced by funding and local and national priorities. One overarching factor was the multiple service and role reconfigurations that occurred over time, which was felt to inhibit services’ ability to have ‘a cohesive run at how we deal with pregnant women’ (Area A SSS group 1):
The constant changes in commissioner, the constant changes in geography, well it doesn't do anyone any favours, because you spend half your time trying to catch up to where you were, rather than actually developing the service… (Area B Commissioner 1)
Participants discussed a number of specific protocols and processes at the organizational level that affected the cessation‐related support offered to women, including referral, carbon monoxide (CO) monitoring, nicotine replacement therapy (NRT) prescribing, and training.
Referral
Most non‐SSS participants described their role in smoking in pregnancy as focused on raising the issue with women and potentially referring to the SSSs rather than discussing smoking in depth. Participants identified prompts in paperwork and clinical systems as useful cues that ‘allow for the conversation’ (Area A HV1) on smoking and increased their confidence in raising the issue. Views on different referral pathways were mixed. While pharmacists were largely positive about an opt‐out pathway, some midwives indicated they felt uncomfortable referring women who were not at the ‘right stage’ for stopping smoking. Other midwives, however, described the opt‐out process positively, viewing it as ‘pretty straight forward’ (Area A Midwife group 2).
SSS advisors also had mixed views about the opt‐out pathway. For example, some felt that it clashed with their service's philosophy of choice, and suggested that it risked being coercive by putting women ‘under pressure’:
We are not here to tell people ‘stop smoking’. We are here to help people who have decided that they want to quit. (Area B SSS Advisor 2)
Some advisors in the area with an opt‐out pathway noted that referral rates were lower than expected and that referral information at times lacked the necessary detail. Additionally when women were referred, some were not interested in stopping smoking and this increased workload:
It would be nice to say to us lot I'm not interested, but [the women] just let you go through that process and you wait for them to come along and then you have got to chase them and you, they don't answer their phone. (Area A SSS group 2)
Despite these issues, advisors indicated that the process offered an effective way to engage women with support who might not otherwise have attended:
…there is always somebody that's pleasantly surprised that we are non‐judgemental and we are there just to accept them kind of warts and all. (Area A SSS group 1)
Carbon monoxide (CO) monitoring
In general, health care professionals with experience of CO monitoring felt that it was acceptable to pregnant women and feasible to undertake as ‘it does only take seconds’ (Area B Midwife group 1). CO monitoring was described as a useful visual tool, a method of establishing honesty with smoking, a powerful motivator for quitting, and an opportunity for discussing harm from smoking. Repeated testing was described as a positive way for pregnant smokers to see the benefits of abstinence from smoking, or as an opportunity to highlight why cutting down did not necessarily reduce health risks.
Some midwives, primarily those in the study area where CO monitoring was not routine, expressed concerns about the time CO monitoring would take and the perceived damage it may do to the practitioner–client relationship:
I am not quite sure how I feel about doing it. I don't know whether it might come across as a bit bullying by using them maybe. (Area B Midwife 3)
Among SSS advisors, concerns were expressed that midwives may increase client disengagement with poorly explained CO readings. Improved training, information sheets, and standardized responses were suggested as ways to reduce this risk.
NRT prescribing
Most non‐SSS professionals seemed very cautious about the use of NRT in pregnancy and expressed uncertainty about safety, including the erroneous belief that patches were not licensed for use in pregnancy in the United Kingdom. For SSS staff, where the local policy specified that pregnant smokers could only be offered NRT after a failed quit attempt (Area A), advisors felt this risked disengagement. They suggested that the offer of NRT sooner would increase successful quitting:
…I always thought if you could give them the patches straightaway you would be half way there. (Area A SSS group 2)
Training
Attending training on smoking cessation in pregnancy was described as a voluntary activity among non‐SSS participants. Much of the available training described was not nationally recognized, instead coming from pharmacists, pharmaceutical companies, or experienced midwives. While some appreciated the discretion to choose whether to attend training or not, others described lack of opportunities to attend. One midwife suggested that unless mandatory, midwives might not proactively seek smoking cessation training opportunities.
Several SSS advisors reported that without adequate training, professionals might give mixed messages around smoking in pregnancy, prompting pregnant smokers to either adopt the views of people in their social network over health care professionals or ‘push’ away guidance entirely:
…I think sometimes you know they get mixed messages from like their family, from their doctor, from the midwife and it's, you know, who do they listen to really. (Area A SSS group 2)
Interpersonal
Relationships with pregnant smokers
Positive relationships were seen by all professional groups as highly important for facilitating discussions about smoking with pregnant smokers:
… the key thing is first with the pregnant clients, developing that rapport with them and developing that strong relationship. (Area B SSS Advisor 1)
Paradoxically, however, motivation to maintain positive relationships appeared at times to generate reluctance to raise and discuss smoking, with some participants describing ‘backing off’ if they feel clients could get upset by discussing it. Relationship concerns also seemed to affect how health care professionals delivered risk information, with several disinclined to link smoking with specific outcomes, or to emphasize the importance of abstinence. Instead, professionals often used the language of ‘choice’ and ‘trying’, congratulating women who reported cutting down. Post‐partum, participants, particularly health visitors, often focused on reducing infant second‐hand smoke exposure, rather than quitting. Some believed that this reluctance could cause risk information to get lost or misunderstood:
…nobody wants to say to women if you smoke your baby might die. What we say is if you smoke you will have a smaller baby and we've all done it…and actually that has been turned on its head and that's been turned into a positive. (Area B Midwife 3)
From the commissioners’ perspective, it was felt that many professionals were overly cautious around giving risk information and providing firm advice to quit. It was felt that pregnant smokers expected, and often wanted, a clear message about smoking in pregnancy:
I sometimes feel that we tread on egg shells a little bit, around, is it OK to bring it up…I'm not negating what midwives say about their relationships with pregnant mums…but actually there is a reasonable amount of evidence base that says that they are expecting to be asked, women, it isn't going to damage the relationship if you ask, or talk about smoking. (Area B Commissioner 1)
Interservice relationships
The relationship between non‐SSS professionals and SSS staff seemed to influence the support that pregnant smokers received. In general, GPs and pharmacists described being satisfied with their relationship and level of contact with SSSs. For midwives and health visitors, perceptions of the relationship were mixed, with some describing limited or no contact with SSS staff. Meanwhile, although sympathetic to workload demands, SSS advisors described frustration that smoking was not given greater priority by antenatal professionals.
Where interservice communication was limited, confidence in the referral process appeared lacking from both perspectives:
I: Do you hear back when you refer people on, do you hear anymore about how it's gone along?
P: No, and that is frustrating too,
I: Would you like to?
P: Yes of course I would because if I am referring in and then it goes no further than that, that becomes a bit of a pointless process’. (Area B Health Visitor 2)
… if somebody doesn't turn up and we phone the midwife and say could you just remind them, you often get yeah, yeah, yeah, oh well. You are pretty sure they don't. (Area A SSS group 2)
Aware of this issue, commissioners expressed a keen wish to improve interagency working, and several professionals felt that improved communication would benefit both the referral process and the support offered. Suggestions included a regular newsletter, opportunities to attend each other's team meetings, and better joined‐up care:
So it's getting everyone on board at the hospital, your GP practice, your midwives, all healthcare professionals trained up to the same level, consistent messages and referrals into the specialist service. (Area B Commissioner 2)
Individual
Non‐SSS participants generally lacked confidence in discussing smoking in pregnancy and varied in how much they saw it as part of their role. Some, including GPs and obstetricians, reported that they might only raise smoking if it was relevant to the appointment, perceiving midwives to be better placed to discuss smoking routinely. Generally, hospital midwives felt that community midwives were better placed to discuss smoking. While some community midwives indicated they felt addressing smoking in pregnancy was very much part of their role, others were less committed. The community midwives often described feeling underskilled to explore smoking in detail, and, most prominently in areas where an opt‐in referral pathway was operating, felt they might only discuss it briefly if time allowed:
If we have time we will take the information, find one of the old forms that we have and contact the smoking cessation service. But most often we are asking the women to do that themselves, encouraging them to do it themselves. (Area B Midwife 1)
Where an opt‐out pathway was in place, it seemed that midwives were more likely to prioritize smoking.
In some cases, the priority individuals gave to smoking seemed connected with external influences such as the availability of NHS information, including for other health behaviours, or the political fashion at the time:
Now obesity is a big one…especially [area B] have had a new obesity guideline come in and leaflets. And that I think is one of the key sorts of things at the moment because it is one of the new things…and I would say that smoking is probably near the bottom. (Area B Midwife 4)
Discussion
This study reports the views and experiences of health care professionals involved in addressing smoking in pregnancy and in the post‐partum period in the United Kingdom. Participants represented a broad range of professions who had routine contact with pregnant and post‐partum women. To our knowledge, this study represents the largest qualitative investigation to date examining this topic anywhere in the world. The SEF‐guided analysis revealed a number of areas where participants felt service and professional issues had an important influence. Service structure, communication pathways, and policies appeared to influence what, if anything, is offered to women in terms of smoking cessation dialogue and support. Interpersonal and individual factors, such as protection of the professional–client relationship and perceived priority of smoking, seemed to affect how this support was delivered. A strength of using an SEF to guide analysis was its ability to help identify interactions between phenomena identified at the different SEF levels and thus potentially recognize ‘high‐impact leverage points’ (Schneider & Stokols, 2009). In our study, interlevel interactions provided insight into the influence of the health care environment on health care professional behaviour and indirectly on the beliefs and behaviour of pregnant and post‐partum women.
Many health care professionals reported a lack of knowledge and confidence around raising and delivering information about smoking in pregnancy. Deficits in knowledge and confidence to advise about smoking in pregnancy is a perennial issue that has been identified by studies in a number of countries (Colomar et al., 2015; Flemming et al., 2016; Price et al., 2006b). Conventionally, such deficits are addressed by training. But unlike many aspects of clinical care, smoking in pregnancy training opportunities appeared to be limited and non‐mandatory for our participants, as reported elsewhere (Abatemarco et al., 2007; Flemming et al., 2016). Non‐mandatory training may influence professional beliefs about the relative importance of smoking in pregnancy compared to other risk factors for which training is mandatory. Where training was available, it was often not nationally accredited and was perceived to be accessed primarily by highly self‐motivated individuals.
Other important organizational factors were service priorities and information campaigns. For example, a recent focus on tackling obesity in pregnancy appeared to reduce the perceived priority of smoking among antenatal professionals. Low prioritization of smoking cessation has been identified previously as a barrier (Abatemarco et al., 2007; Colomar et al., 2015), and our findings provide new insight into how priorities may be affected inadvertently by new initiatives targeting other health behaviours. Many parallels with smoking in pregnancy can be drawn with midwives’ experience of discussing obesity with pregnant women and referring them to weight management services (Atkinson, French, Ménage, & Olander, 2017). This includes not raising the topic when a negative reception is anticipated and variable rates of referral due to the offer of choice (opt‐in) or not (opt‐out). Addressing either smoking or obesity is likely to be compounded by the perceived lack of time among health care professionals, particularly midwives, to address lifestyle behaviour change (Abatemarco et al., 2007; Herberts & Sykes, 2012) and a prioritization for discussing the clients’ concerns, usually about labour (Flemming et al., 2016), during consultations.
The importance placed on a positive professional–client relationship emerged as having a likely influence on pregnant women's smoking beliefs and behaviour. Most midwives described a ‘catch‐22’ situation: They reported the need for an established positive relationship to discuss the consequences of smoking, yet would protect this relationship by avoiding discussion of any risks that could potentially be upsetting or damage the relationship. The consequences of protecting the relationship included downplaying risks, reinforcing cutting down and, among health visitors, focusing on post‐partum environmental tobacco smoke avoidance rather than cessation. Midwives’ tendency to promote reduction over abstinence is also found outside of the United Kingdom (Flemming et al., 2016; Glover et al., 2008), although likely reasons for this have not before now been described. Promoting reduction over abstinence can increase ambivalence and reduce motivation to quit for some women (Flemming et al., 2015; Naughton et al., 2013), although others report it as supportive as it recognizes the difficulty they have in stopping smoking (Flemming et al., 2015).
New insights were also generated about views of opt‐out referral pathways combined with routine CO monitoring. This is important as this pathway is relatively new in the United Kingdom and not in place in other countries. Some midwives felt that opt‐out referral pathways simplified referral and increased access to support, whereas others highlighted concerns about referring women who they felt were not motivated to quit, as did some SSS advisors. Some pregnant smokers with experience of an opt‐out referral have reported being unhappy with the lack of choice with some even describing powerlessness and resentment (Sloan et al., 2016). Yet opt‐out pathways have been shown to increase support, access, and abstinence (Bell et al., 2017; Campbell et al., 2017). Informing health care professionals of the potential benefits of opt‐out over opt‐in referrals, including emphasizing that many pre‐implementation concerns do not emerge post‐implementation (Campbell et al., 2016), could help with adoption and delivery (Jordan et al., 2006). Furthermore, CO monitoring could be promoted to health care professionals as a positive way of initiating a discussion about smoking with clients, given the positive experiences of using CO monitors among our participants and that many pregnant women find this a useful and positive motivational tool (Sloan et al., 2016).
The ‘last resort’ policy for the provision of NRT at one site, where NRT is provided only when other options have been tried and failed, was considered to facilitate pregnant women to disengage from cessation support. This type of policy, which was often ignored by the cessation advisor participants, may in part help explain why health care professionals continue to be highly cautious about the appropriateness of NRT in pregnancy and sometimes hold erroneous beliefs about its safety (Flemming et al., 2016; Glover et al., 2008; Herbert, Coleman, & Britton, 2005; Price, Jordan, & Dake, 2006a). This view prevails in the United Kingdom despite near universal provision of NRT to pregnant women in the SSSs (Fahy, Cooper, Coleman, Naughton, & Bauld, 2014). It is no surprise, therefore, that pregnant women are uncertain about the safety of NRT in pregnancy (Flemming et al., 2015) and some perceive the risks of NRT to be equal to tobacco (Naughton et al., 2013). This may extend to new nicotine‐containing devices such as e‐cigarettes, which, unlike NRT, are not licensed as medicines (Oncken et al., 2017).
While we set out to understand barriers and facilitators to the provision of support for smokers in the post‐partum period as well as the prenatal period, our sample had limited experience of supporting women during this time and so little data were collected on this. This in itself highlights how little smoking‐related support activity occurs during the post‐partum period and remains an important focus for future investigation. Furthermore, views from some health professionals interviewed, such as GPs, obstetricians, and pharmacists, were less informative for the main themes identified as their role had little involvement in addressing smoking in pregnancy. Increasing the involvement of these professionals in supporting smoking cessation in pregnancy is a further area for future research.
Clinical implications
The findings identified a number of areas for clinical improvement, at organizational, interpersonal, and individual levels, some of which have been discussed above. At an organizational level, building on existing models of care rather than continually changing the model could help support a more effective and coordinated cessation support service. Enabling staff members to be more fully involved in service development could also potentially enable the service to make better use of staff expertise, increase staff buy‐in, improve communication pathways, and reduce the feeling among some staff that changes are imposed on them. In combination with this, efforts may be required to ensure health services continually promote smoking in pregnancy‐related policies and practices to ensure any new initiatives focused on other areas of care do not reduce the perceived priority of smoking. Regarding interservice relationships, bilateral improvements in communication between clinical services and the SSSs also emerged as important targets for improving the overall management of antenatal smoking.
Improved access to or mandatory training and updates for staff who encounter antenatal smoking should help improve the quality of smoking management. This should also help improve the consistency of health messages around smoking delivered to pregnant smokers. Training of antenatal staff can increase the assessment of smoking and provision of support to pregnant women (Althabe et al., 2016), even when part of opt‐out referral pathways (Campbell et al., 2017).
Prompts to remind HPs to record and discuss smoking also emerged as useful aids in our study. While some health care professionals view such prompts as promoting a prescriptive rather than sensitive approach to discussing smoking (Flemming et al., 2016), our participants indicated that improved prompts could help encourage and inform smoking discussions. Integrating agreed scripts to aid discussion around smoking could help professionals present a clear and comprehensive picture of the risks and avoid the common practice of raising only certain risks to minimize upset, which is largely at odds with the information preferences of pregnant smokers (Arborelius & Nyberg, 1997; Lendahls et al., 2002). Health care professionals have reported interest in scripts for discussing smoking with pregnant women (Colomar et al., 2015), and a midwife‐delivered standardized ‘risk perception’ intervention has already been implemented in North East England as part of an opt‐out referral pathway (‘BabyClear’) (Bell et al., 2017).
Conclusion
Health care professionals described multiple factors affecting pregnant and post‐partum smokers’ capacity to quit smoking, both directly, through the advice or support provided, and indirectly, through the care structure and environment. In general, midwives in the United Kingdom were considered to have the key role in addressing prenatal smoking, but protection of their client relationships, lack of skills, knowledge and training opportunities, and changing service priorities and policies were all barriers to managing women's smoking. Routine CO monitoring and opt‐out referrals to specialist cessation advisors were considered effective, although some professionals believed that this constrained personal choice. Balancing the need to provide interventions that will improve maternal and child health while respecting the autonomy of women remains an ongoing challenge. The findings highlight the importance of addressing health care professional beliefs and behaviours alongside simultaneously tackling organizational barriers to bring about significant and lasting change.
Conflict of interest
All authors declare no conflict of interest.
Supporting information
Figure S1. Coding framework.
Appendix S1. Interview schedules.
Acknowledgements
The authors would like to thank the participants for the time they took out of their busy schedules to participate. The authors would also like to thank Carol Anne Greenan and Aileen Paton at the University of Stirling and Sally Stephenson at the University of York for their administrative support. Particular thanks also go to Helena Connelly and Dermot Gorman who helped with the original design of the study, identified areas for investigation, and assisted with recruiting health professionals to participate in interviews. This study was funded by the NIHR Health Technology Assessment programme. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme, or the Department of Health. The views and opinions expressed by the interviewees in verbatim quotes are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme, or the Department of Health.
The Institute for Social Marketing is a member of the UK Centre for Tobacco and Alcohol Studies (UKCTAS; http://www.ukctas.ac.uk). Funding for UKCTAS from the British Heart Foundation, Cancer Research UK, the Economic and Social Research Council, the Medical Research Council, and the National Institute for Health Research, under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- Abatemarco, D. J. , Steinberg, M. B. , & Delnevo, C. D. (2007). Midwives’ knowledge, perceptions, beliefs, and practice supports regarding tobacco dependence treatment. Journal of Midwifery and Women's Health, 52(5), 451–457. 10.1016/j.jmwh.2007.03.019 [DOI] [PubMed] [Google Scholar]
- Ajzen, I. (1988). Attitudes, personality and behavior. Milton Keynes, UK: Open University Press. [Google Scholar]
- Althabe, F. , Aleman, A. , Berrueta, M. , Morello, P. , Gibbons, L. , Colomar, M. , & Buekens, P. M. (2016). A multifaceted strategy to implement brief smoking cessation counseling during antenatal care in Argentina and Uruguay: A cluster randomized trial. Nicotine and Tobacco Research, 18, 1083–1092. 10.1093/ntr/ntv276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arborelius, E. , & Nyberg, K. (1997). How should midwives discuss smoking behaviour in pregnancy with women of low educational attainment? Midwifery, 13, 210–215. 10.1016/S0266-6138(97)80008-3 [DOI] [PubMed] [Google Scholar]
- Atkinson, L. , French, D. P. , Ménage, D. , & Olander, E. K. (2017). Midwives’ experiences of referring obese women to either a community or home‐based antenatal weight management service: Implications for service providers and midwifery practice. Midwifery, 49, 102–109. 10.1016/j.midw.2016.10.006 [DOI] [PubMed] [Google Scholar]
- Beenstock, J. , Sniehotta, F. F. , White, M. , Bell, R. , Milne, E. M. , & Araujo‐Soares, V. (2012). What helps and hinders midwives in engaging with pregnant women about stopping smoking? A cross‐sectional survey of perceived implementation difficulties among midwives in the North East of England. Implementation Science, 7, 36 10.1186/1748-5908-7-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell, R. , Glinianaia, S. V. , Waal, Z. V. , Close, A. , Moloney, E. , Jones, S. , & Rushton, S. (2017). Evaluation of a complex healthcare intervention to increase smoking cessation in pregnant women: Interrupted time series analysis with economic evaluation. Tobacco Control, 27(1), 90–98. 10.1136/tobaccocontrol-2016-053476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloch, M. , Althabe, F. , Onyamboko, M. , Kaseba‐Sata, C. , Castilla, E. E. , Freire, S. , … Goldenberg, R. (2008). Tobacco use and second hand smoke exposure during pregnancy: An investigative survey of women in 9 developing nations. American Journal of Public Health, 98, 1833–1840. 10.2105/AJPH.2007.117887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland, T. , Babayan, A. , Irfan, S. , & Schwartz, R. (2013). Exploring the adequacy of smoking cessation support for pregnant and postpartum women. BMC Public Health, 13, 472 10.1186/1471-2458-13-472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun, V. , & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. [Google Scholar]
- Campbell, K. A. , Bowker, K. A. , Naughton, F. , Sloan, M. , Cooper, S. , & Coleman, T. (2016). Antenatal clinic and stop smoking services staff views on “opt‐out” referrals for smoking cessation in pregnancy: A framework analysis. International Journal of Environmental Research and Public Health, 13(10), 1004 10.3390/ijerph13101004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, K. A. , Cooper, S. , Fahy, S. J. , Bowker, K. , Leonardi‐Bee, J. , McEwen, A. , & Coleman, T. (2017). ‘Opt‐out’ referrals after identifying pregnant smokers using exhaled air carbon monoxide: Impact on engagement with smoking cessation support. Tobacco Control, 26(3), 300–306. 10.1136/tobaccocontrol-2015-052662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2012). Current tobacco use and secondhand smoke exposure among women of reproductive age–14 countries, 2008–2010. Morbidity and Mortality Weekly Report (MMWR), 2, 877–882. 10.1001/jama.2012.91588 [DOI] [PubMed] [Google Scholar]
- Chang, J. C. , Alexander, S. C. , Holland, C. L. , Arnold, R. M. , Landsittel, D. , Tulsky, J. A. , & Pollak, K. I. (2013). Smoking is bad for babies: Obstetric care providers’ use of best practice smoking cessation counseling techniques. American Journal of Health Promotion, 27, 170–176. 10.4278/ajhp.110624-QUAL-265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colomar, M. , Tong, V. T. , Morello, P. , Farr, S. L. , Lawsin, C. , Dietz, P. M. , & Althabe, F. (2015). Barriers and promoters of an evidenced‐based smoking cessation counseling during prenatal care in Argentina and Uruguay. Maternal and Child Health Journal, 19, 1481–1489. 10.1007/s10995-014-1652-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fahy, S. J. , Cooper, S. , Coleman, T. , Naughton, F. , & Bauld, L. (2014). Provision of smoking cessation support for pregnant women in England: Results from an online survey of NHS stop smoking services for pregnant women. BMC Health Services Research, 14, 107 10.1186/1472-6963-14-107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flemming, K. , Graham, H. , McCaughan, D. , Angus, K. , Sinclair, L. , & Bauld, L. (2016). Health professionals’ perceptions of the barriers and facilitators to providing smoking cessation advice to women in pregnancy and during the post‐partum period: A systematic review of qualitative research. BMC Public Health, 16, 290 10.1186/s12889-016-2961-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flemming, K. , McCaughan, D. , Angus, K. , & Graham, H. (2015). Qualitative systematic review: Barriers and facilitators to smoking cessation experienced by women in pregnancy and following childbirth. Journal of Advance Nursing, 71, 1210–1226. 10.1111/jan.12580 [DOI] [PubMed] [Google Scholar]
- Flenady, V. , Koopmans, L. , Middleton, P. , Froen, J. F. , Smith, G. C. , Gibbons, K. , & Ezzati, M. (2011). Major risk factors for stillbirth in high‐income countries: A systematic review and meta‐analysis. Lancet, 377, 1331–1340. 10.1016/S0140-6736(10)62233-7 [DOI] [PubMed] [Google Scholar]
- Glover, M. , Paynter, J. , Bullen, C. , & Kristensen, K. (2008). Supporting pregnant women to quit smoking: Postal survey of New Zealand general practitioners and midwives’ smoking cessation knowledge and practices. New Zealand Medical Journal, 121, 53–65. [PubMed] [Google Scholar]
- Green, J. , & Thorogood, N. (2014). Qualitative methods for health research (3rd ed.). London, UK: Sage. [Google Scholar]
- Health and Social Care Information Centre (2015). Statistics on NHS Stop Smoking Services in England, April 2014 to March 2015. The Health and Social Care Information Centre.
- Health and Social Care Information Centre (2016). Statistics on Women's Smoking Status at Time of Delivery, England – Quarter 4, 2015‐16. The Health and Social Care Information Centre.
- Herbert, R. , Coleman, T. , & Britton, J. (2005). U.K. general practitioners’ beliefs, attitudes, and reported prescribing of nicotine replacement therapy in pregnancy. Nicotine and Tobacco Research, 7(4), 541–546. 10.1080/14622200500186015 [DOI] [PubMed] [Google Scholar]
- Herberts, C. , & Sykes, C. (2012). Midwives’ perceptions of providing stop‐smoking advice and pregnant smokers’ perceptions of stop‐smoking services within the same deprived area of London. Journal of Midwifery and Women's Health, 57(1), 67–73. 10.1111/j.1542-2011.2011.00072.x [DOI] [PubMed] [Google Scholar]
- Jordan, T. R. , Dake, J. R. , & Price, J. H. (2006). Best practices for smoking cessation in pregnancy: Do obstetrician/gynecologists use them in practice? Journal of Women's Health, 15(4), 400–441. 10.1089/jwh.2006.15.400 [DOI] [PubMed] [Google Scholar]
- Lendahls, L. , Ohman, L. , Liljestrand, J. , & Hakansson, A. (2002). Women's experiences of smoking during and after pregnancy as ascertained two to three years after birth. Midwifery, 18(3), 214–222. 10.1054/midw.2002.0312 [DOI] [PubMed] [Google Scholar]
- Moore, E. , Blatt, K. , Chen, A. , Van, H. J. , & Defranco, E. A. (2016). Relationship of trimester specific smoking patterns and risk of preterm birth. American Journal of Obstetrics and Gynecology, 215(1), 109 10.1016/j.ajog.2016.01.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moshammer, H. , Hoek, G. , Luttmann‐Gibson, H. , Neuberger, M. A. , Antova, T. , Gehring, U. , & Fletcher, T. (2006). Parental smoking and lung function in children: An international study. American Journal of Respiratory and Critical Care Medicine, 173(11), 1255–1263. 10.1164/rccm.200510-1552OC [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (NICE) (2010). Quitting smoking in pregnancy and following childbirth. National Institute for Health and Care Excellence, 6–9. Retrieved from http://nice.org.uk/guidance/ph26
- Naughton, F. , Eborall, H. , & Sutton, S. (2013). Dissonance and disengagement in pregnant smokers: A qualitative study. Journal of Smoking Cessation, 8(1), 24–32. 10.1017/jsc.2013.4 [DOI] [Google Scholar]
- Office for National Statistics (ONS) (2013). Data from Integrated Household Survey: Smoking prevalence among adults aged 18+ by region and local authority. January‐December 2012. Retrieved from http://www.ons.gov.uk/ons/rel/integrated-household-survey/integrated-household-survey/index.html
- Oken, E. , Levitan, E. B. , & Gillman, M. W. (2008). Maternal smoking during pregnancy and child overweight: Systematic review and meta‐analysis. International Journal of Obesity, 32(2), 201–210. https://doi.org/0.1038/sj.ijo.0803760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oncken, C. , Ricci, K. A. , Kuo, C. L. , Dornelas, E. , Kranzler, H. R. , & Sankey, H. Z. (2017). Correlates of electronic cigarettes use before and during pregnancy. Nicotine and Tobacco Research, 19(5), 585–590. 10.1093/ntr/ntw225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen, L. , & Penn, G. (1999). Smoking and pregnancy: A survey of knowledge, attitudes and behaviour 1992–1999. London, UK: Health Education Authority. [Google Scholar]
- Pineles, B. L. , Park, E. , & Samet, J. M. (2014). Systematic review and meta‐analysis of miscarriage and maternal exposure to tobacco smoke during pregnancy. American Journal of Epidemiology, 179(7), 807–823. 10.1093/aje/kwt334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price, J. H. , Jordan, T. R. , & Dake, J. A. (2006a). Obstetricians and gynecologists’ perceptions and use of nicotine replacement therapy. Journal of Community Health, 31, 160–175. 10.1007/s10900-005-9009-x [DOI] [PubMed] [Google Scholar]
- Price, J. H. , Jordan, T. R. , & Dake, J. A. (2006b). Perceptions and use of smoking cessation in nurse‐midwives’ practice. Journal of Midwifery and Women's Health, 51, 208–215. 10.1016/j.jmwh.2005.12.003 [DOI] [PubMed] [Google Scholar]
- QSR International (2012). Retrieved from http://www.qsrinternational.com/products_nvivo.aspx.
- Raisanen, S. , Kramer, M. R. , Gissler, M. , Saari, J. , Hakulinen‐Viitanen, T. , & Heinonen, S. (2014). Smoking during pregnancy was up to 70% more common in the most deprived municipalities – a multilevel analysis of all singleton births during 2005–2010 in Finland. Preventive Medicine, 67, 6–11. 10.1016/j.ypmed.2014.06.026 [DOI] [PubMed] [Google Scholar]
- Reardon, R. , & Grogan, S. (2016). Talking about smoking cessation with pregnant women: Exploring midwives’ accounts. British Journal of Midwifery, 24(1), 38–42. 10.12968/bjom.2016.24.1.38 [DOI] [Google Scholar]
- Roske, K. , Hannover, W. , Thyrian, J. R. , John, U. , & Hannich, H. J. (2009). Smoking cessation counselling for pregnant and postpartum women among midwives, gynaecologists and paediatricians in Germany. International Journal of Environmental Research and Public Health, 6(1), 96–107. 10.3390/ijerph6010096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomi Barkat, S. , Karanwal, S. , Lawder, R. , MacKinnon, A. , Stockton, D. , & Moore, F. (2015). ScotPHO tobacco profiles (Second release). Retrieved from http://www.scotpho.org.uk/opt/Reports/scotpho-tobacco-profiles-secondrelease2015-overview-report.pdf
- Schneider, M. , & Stokols, D. (2009). Multilevel theories of behavior change: A Social Ecological Framework In Shumaker S. A., Ockene J. K. & Riekert K. A. (Eds.), The handbook of health behavior change (4th ed.) (pp. 85–105). London, UK: Springer. [Google Scholar]
- Sloan, M. , Campbell, K. A. , Bowker, K. , Coleman, T. , Cooper, S. , Brafman‐Price, B. , & Naughton, F. (2016). Pregnant women's experiences and views on an “opt‐out” referral pathway to specialist smoking cessation support: A qualitative evaluation. Nicotine and Tobacco Research, 18, 900–905. 10.1093/ntr/ntv273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss, A. , & Corbin, J. (1998). Basics of qualitative research: Techniques and procedures for developing grounded theory (Vol. 2). London: Sage. [Google Scholar]
- The NHS Information Centre (2011). Infant feeding survey 2010: Early results. York, UK: Author. [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32‐item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19, 349–357. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Ussher, M. , Etter, J. F. , & West, R. (2006). Perceived barriers to and benefits of attending a stop smoking course during pregnancy. Patient Education and Counselling, 61(3), 467–472. 10.1016/j.pec.2005.06.021 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Coding framework.
Appendix S1. Interview schedules.


