INTRODUCTION
Persistent pain after breast surgery for cancer is observed in more than 60% patients.[1] Although opioids have been mainstay for managing postoperative pain, they have undesirable side effects such as constipation, sedation, respiratory depression, urinary retention, postoperative nausea and vomiting, and pruritus. Opioid-induced hyperalgesia or opioid paradox has been described as increased perception of pain after opioid-based anaesthesia and surgery.[2] We used opioid-free general anaesthesia (OFGA) technique in five patients who underwent modified radical mastectomy along with a preoperative ultrasound (US)-guided erector spinae plane (ESP) block under local anaesthesia.
CASE REPORT
We selected five female patients with carcinoma breast (American Society of Anesthesiologists' physical status I/II, ASA) who were posted for modified radical mastectomy with axillary dissection. Demographic details (age, weight, ASA status, side of surgery) are shown in Table 1a. Unilateral ESP block under US guidance with OFGA was planned after obtaining an informed consent. All patients were evaluated at preanaesthesia clinic for fitness. A 12-lead electrocardiogram and two-dimensional echocardiogram were advised if they had received anthracycline-based chemotherapy preoperatively. After confirming nil by mouth status and securing intravenous (IV) access on contralateral hand, patients were shifted to operating room. Noninvasive blood pressure (NIBP), heart rate (HR), and oxygen saturation (SPO2) were noted. T4 spinous process was marked after counting down from C7 spinous process with the patient in sitting position. A linear array high-frequency probe (SonositeM-Turbo Inc., USA) was used, which was placed in craniocaudal orientation in midline and was moved laterally to identify T4 transverse process (TP). TP is usually at 2.5–3 cm from spinous process laterally. Erector spinae muscle (ESM), rhomboidus major, and trapezius muscle were identified. Under aseptic technique and after skin infiltration with 2% lidocaine, 18 G Tuohy needle was introduced in-plane craniocaudally and under vision navigated till the TP was encountered. Hydrodissection with 2 ml normal saline was done to confirm separation of ESM from TP. 30 ml 0.25% bupivacaine was injected under vision in aliquots of 5 ml after negative aspiration [Figure 1a]. The drug spread was seen in the ESP plane craniocaudally. In the supine position, patients were premedicated with IV 0.03 mg/kg midazolam and 2 mg/kg lidocaine. Loading dose of 1 μg/kg dexmedetomidine was started after the block over 15 min followed by a maintenance of 0.5 μg/kg/h till skin closure. Intraoperative monitoring as per ASA standards (electrocardiogram, NIBP, SPO2, and end-tidal carbon dioxide) was done for all cases. Anaesthesia was induced with 2–2.5 mg/kg IV propofol. Airway was secured with appropriate-sized supraglottic airway device (SAD – AMBUR Aura40™), and neuromuscular blockade was achieved with 0.5 mg/kg atracurium. GA was maintained with oxygen: air (total fresh gas flow of 1 l) and isoflurane titrated for a minimum alveolar concentration of 1.0. All patients received 0.1 mg/kg dexamethasone, 0.5 mg/kg ketamine, 30 mg ketorolac, 2 gm magnesium, and 1 gm paracetamol IV intraoperatively. Baseline vitals (HR, NIBP) and at skin incision were noted. There was no haemodynamic response to incision in any patient [Table 1b]. One patient had a low HR (<50/min) with blood pressure of 100/70 mm Hg during dexmedetomidine infusion, which was treated with 0.2 mg IV glycopyrrolate. At the end of surgery, SAD was removed after reversing neuromuscular blockade with 0.05 mg/kg neostigmine and 0.01 mg/kg glycopyrrolate.
Table 1a.
Comparison of age, weight, side, comorbidities, and body mass index (BMI)
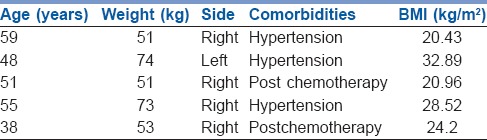
Figure 1.
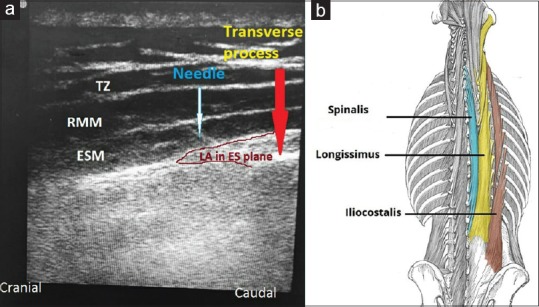
(a) ESP block given under US guidance at T4 level. Image also shows local anaesthetic in ESP with the muscle getting pushed above (ESM: erector spinae muscle, RMM: rhomboidus major muscle, TZ: trapezius muscle). (b) The three muscles: iliocostalis, longissimus, and spinalis, which forms the ESM along with its attachment to the vertebral column and other bones (Image source: The image has been submitted after permission from Dr. Oliver Jones from the site: http://teachmeanatomy.info/)
Table 1b.
Comparison of vital parameters at baseline, at skin incision, postoperative VAS and events in five patients
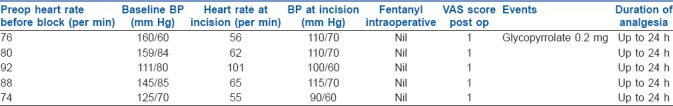
Patients were monitored in recovery room and were transferred to ward later. Visual analogue scale (VAS) score was noted every 1, 3, and 6 h after surgery and rescue analgesia of 3 mg IV morphine was ordered if VAS was more than 4. All patients were prescribed 1 gm paracetamol every 6th hourly, ibuprofen 400 mg every 8th hourly, gabapentin 300 mg per orally every 12th hourly. Rescue analgesic was not required in any patient.
DISCUSSION
Perioperative use of potent opioids-like morphine have been implicated for cancer recurrence; however the clinical evidence is lacking.[3] Avoiding opioids is indicated in obesity, patients with obstructive sleep apnea, and opioid addicts.[4] Thoracic epidural anaesthesia used for unilateral breast surgery is technically challenging too.[5] Thoracic paravertebral block when used with GA or as the sole anaesthetic has been found to provide better postoperative pain relief but adverse events such as accidental pneumothorax and vascular puncture are known problems.[6] Pectoral blocks and serratus anterior plane blocks have been used with variable efficacy with GA but have its limitations as it causes sparing of supraclavicular nerves, intercostobrachial nerve and also disrupts surgical planes.[7] Forero et al. described ESP block for treating thoracic neuropathic pain with encouraging results.[8] Erector spinae (ES) consists of three columns of muscles: iliocostalis, longissimus, and spinalis, which run parallel to each other along the vertebra and extends from lower back of the skull down to the pelvis [Figure 1b]. ESP is a potential space deep to ES muscle, where the injected local anaesthetic (LA) spreads cranio-caudally up to several levels as the ES fascia extends from nuchal fascia cranially to the sacrum caudally (C7-T2 cranially and L2-L3 caudally), as demonstrated by Chin et al. in cadavers.[9] LA gains entry into the thoracic paravertebral space by reaching the costotransverse foramina and thereby blocks ventral rami, dorsal rami of spinal nerves, and rami communicantes that transmit sympathetic fibers. In this way the block covers somatic and visceral pain during breast surgery. The dermatomes covered by the injection depend on the point of entry and the volume of LA used. Bilateral ESP block can be as effective as an epidural anaesthetic.[10] Postoperatively all our patients had unilateral T1-T6 dermatomal sensory block.
CONCLUSION
OFGA was safe, effective, and provides good postoperative morphine sparing analgesia, facilitates early recovery and discharge after breast surgeries. ESP block is a good addition to the current multimodal analgesia regimen for breast surgeries.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Wang L, Guyatt GH, Kennedy SA, Romerosa B, Kwon HY, Kaushal A, et al. Predictors of persistent pain after breast cancer surgery: A systematic review and meta-analysis of observational studies. CMAJ. 2016;188:E352–61. doi: 10.1503/cmaj.151276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heeseung Lee. Opioid-induced hyperalgesia is a paradox for perioperative physician. Korean J Anesthesiol. 2013;64:1–2. doi: 10.4097/kjae.2013.64.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fodale V, D'Arrigo MG, Triolo S, Mondello S, La Torre D. Anesthetic techniques and cancer recurrence after surgery. Sci World J. 2014;2014:328513. doi: 10.1155/2014/328513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar K, Kirksey MA, Duong S, Wu CL. A review of opioid-sparing modalities in perioperative pain management: Methods to decrease opioid use postoperatively. Anesth Analg. 2017;125:1749–60. doi: 10.1213/ANE.0000000000002497. [DOI] [PubMed] [Google Scholar]
- 5.Doss NW, Ipe J, Crimi T, Rajpal S, Cohen S, Fogler RJ, et al. Continuous thoracic epidural anaesthesia with 0.2% ropivacaine versus general anaesthesia for perioperative management of modified radical mastectomy. Anesth Analg. 2001;92:1552–7. doi: 10.1097/00000539-200106000-00041. [DOI] [PubMed] [Google Scholar]
- 6.Schnabel A, Reichl SU, Kranke P, Pogatzki-Zahn EM, Zahn PK. Efficacy and safety of paravertebral blocks in breast surgery: A meta-analysis of randomized controlled trials. Br J Anaesth. 2010;105:842–52. doi: 10.1093/bja/aeq265. [DOI] [PubMed] [Google Scholar]
- 7.Woodworth GE, Ivie RMJ, Nelson SM, Walker CM, Maniker RB. Perioperative breast analgesia: A qualitative review of anatomy and regional techniques. Reg Anesth Pain Med. 2017;42:609–31. doi: 10.1097/AAP.0000000000000641. [DOI] [PubMed] [Google Scholar]
- 8.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: A novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–7. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 9.Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017;72:452–60. doi: 10.1111/anae.13814. [DOI] [PubMed] [Google Scholar]
- 10.Restrepo-Garces CE, Chin KJ, Suarez P, Diaz A. Bilateral continuous erector spinae plane block contributes to effective postoperative analgesia after major open abdominal surgery: A case report. Case Rep. 2017;9:319–21. doi: 10.1213/XAA.0000000000000605. [DOI] [PubMed] [Google Scholar]


