Abstract
Background and Aims:
The preservation of recurrent laryngeal nerve (RLN) is an essential part of thyroid surgery. The various methods to test the normal functionality of vocal cords (VCs) include direct visualisation under the fiber bronchoscope, indirect laryngoscopy, laryngeal muscles electromyography, computed tomography (CT), and magnetic resonance imaging (MRI). We aimed to assess the usefulness of ultrasound (USG) in the examination of VC morphology and movement.
Methods:
After Institutional Ethical Committee (IEC) clearance, 65 American Society of Anesthesiologists physical status I/II patients between the age group 18 and 60 years scheduled for thyroid surgery were enrolled in this observational study. All patients underwent USG examination before, immediately after and 2 days after thyroidectomy. The vocal fold (VF) displacement velocity (VFDV) was recorded and analysed. If any VF disorder was detected, the patients underwent two additional examinations: 2 and 3 months after thyroidectomy. All the findings were correlated with those of video rhinolaryngoscope (VRL).
Results:
The visualisation rate of the VCs with USG was 96.9% whereas with VRL was 100%. Two patients had preoperative VC palsy that was picked up by USG and confirmed by VRL. The sensitivity and specificity of USG as a tool to detect paralysis were 100% CI = (0.34, 1.00) and 93.44% CI = (0.84, 0.97), respectively.
Conclusion:
USG examination can prove to be a good, noninvasive, cheap alternative to VRL in examination for functionality of VCs perioperatively.
Key words: Thyroid surgery, ultrasound, video rhinolaryngoscope, vocal fold displacement velocity
INTRODUCTION
The preservation of recurrent laryngeal nerve (RLN) is an essential part of thyroid surgery. The functionality of the nerve is assessed preoperatively and is attempted to be preserved during surgery.[1,2] Various methods have been described to monitor the function of the RLN: (1) direct visualisation of vocal cord movement under the fiber bronchoscopy; (2) indirect laryngoscopy (IDL); (3) palpation of the larynx during stimulation of the RLN; (4) laryngeal muscle electromyography; (5) electromyography with orotracheal tube inserted electrodes; (6) computed tomography (CT), and magnetic resonance imaging (MRI).[3] Transcutaneous ultrasound (USG) is a cheap, noninvasive alternative to the above methods.[4] The development of gray-scale, real-time, high-resolution, B-mode USG helps in visualisation of the normal anatomy of the larynx, and the movements of the true and false cords.[5] It can offer to be an alternative to the more invasive direct visualisation of VCs using DL/video rhinolaryngoscope (VRL). Hence, we hypothesised that USG can be useful in assessment of the functionality of VCs after thyroid surgery.
METHODS
After Institutional Ethical Committee (IEC) clearance, the study was registered in clinical trial registry of India (CTRI) CTRI/2017/02/007868. As it was a pilot study, 65 consecutive patients scheduled to undergo thyroid surgery (benign or malignant) were enrolled in this observational study. All these patients were American Society of Anesthesiologists physical status I/II and belonged to the age group 18–60 years. Informed consent was taken and the patients were explained various manoeuvres like: (1) Valsalva manoeuvre, (2) coughing, (3) phonation, during the time of counselling itself. They were also explained about VRL (Karl Storz, Germany) examination. ASA III or more, patients with psychiatric disorder, preexisting neurological disease affecting VC functions, patients with a diagnosis of primary untreated laryngeal/hypopharyngeal cancer, laryngeal trauma were excluded.
All patients underwent USG examination of the VCs before, immediately after and 2 days after thyroidectomy. An anaesthesiologist with an experience of at least 3 years in USG scanned all the patients. If any vocal fold (VF) disorder was detected, the patients underwent two additional examinations: 2 and 3 months after thyroidectomy. [Figure 1] All the findings were correlated with the findings of VRL, which the patients underwent at the same time. An independent anaesthesiologist not involved in USG scanning performed VRL in the patients. The results were correlated by an independent anaesthesiologist not involved in the study.
Figure 1.
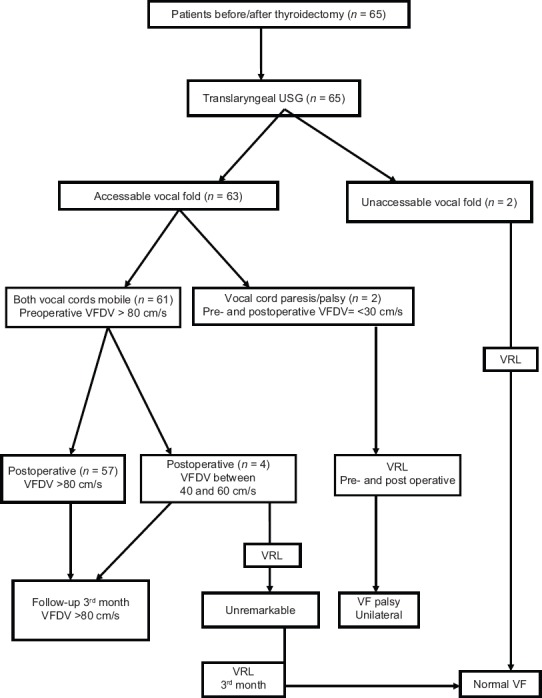
Flow diagram showing sequential assessment of patients
During USG (Sonosite, USA) scanning, the patients were in recumbent position with neck hyperextended. A high frequency linear probe (frequency: 8–12 Hz) was used to scan the anterior neck. The various structures identified were carotid artery, jugular vein, tracheal ring, thyroid cartilage, arytenoids, and VFs. Thereafter the probe was kept transversely over the thyroid cartilage to view the VFs movements. False VCs appear as hyperechoic structures whereas true cords are hypoechoic. Normal VC movement was defined as “symmetrically abductive and adductive motion of the true VCs during quiet respiration.” After localizing the VCs, the system was switched to pulsed Doppler and the Doppler gate set on the VF vibrating part. The range of tissue velocity was recorded and analysed.[6] The following parameters were assessed:
Morphology and bilateral movement of VCs during phonation: patient was made to say “Ah”
Color Doppler imaging (CDI) to quantify tissue displacement velocity in the vibrating section of VF
Adduction of VCs during Valsalva manoeuvre and coughing.
The primary objective was to assess the morphology of the VCs using both the modalities. The secondary objective was to assess the vocal fold displacement velocity (VFDV) of the patients using USG.
RESULTS
The study group included 47 females (72.3%) and 18 male patients (27.6%) scheduled for thyroidectomy for various reasons: multinodular goiter (36 patients), colloid goiter (18 patients), medullary carcinoma (4 patients), and Graves' disease (7 patients). The median age of presentation was 44 years (23–60 years) and the mean weight was 62.246 ± 9.48 kg.
Preoperatively, VF was visualised in all patients using VRL, but only in 63 of 65 patients using USG (96.9%) In 57 patients, the morphology and movement remained the same pre- and postoperatively (true negative) [Figure 2]. VRL also revealed the same morphological findings. VFDV as measured with USG ranged from 80 to 150 cm/s (mean = 104.1875 ± 12.450) and not much change was observed postoperatively.
Figure 2.

Normal morphology and vocal fold displacement velocity (VFDV)
Preoperatively two patients had a significant decrease in VF size and mobility. On VRL examination, the VF paralysis was confirmed (true positive) [Figure 3]. The VFDV was 16.8 cm/s [Figure 4] and 21.2 cm/s, which remained the same postoperatively.
Figure 3.
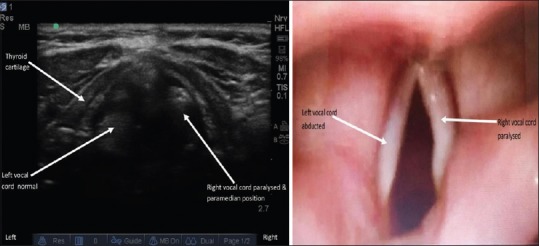
Vocal fold palsy as seen on video rhinolaryngoscope (VRL)
Figure 4.

Vocal fold palsy on ultrasound
In four other patients, where the VRL and USG visualisation of VF suggested normal findings, there was a transient decrease in VFDV <60 cm/s postoperatively. This change was transient and it returned to its normal values in 3 months (false positive).
The sensitivity and specificity of USG as a tool to detect paralysis were 100% (CI = [0.34, 1.00]) and 93.44% (CI = [0.84, 0.97]), respectively.
DISCUSSION
Assessing the functionality of RLN and preserving it intraoperatively is of utmost importance in thyroid surgeries. Even if the patient has unilateral RLN paralysis, the surgeon tries to preserve the contralateral side to prevent any airway related complications. As few of these patients with unilateral palsy might be asymptomatic, knowing the functional status of VFs becomes mandatory. Among all the modalities used, USG is a noninvasive, simple, safe, and radiation free alternative.[4] Flexible VRL has been used, but may have limited usage in pediatric patients because of the lack of cooperation. This is the first observational study correlating the findings of anaesthesiologist aided USG and VRL in Indian subpopulation.
On USG examination, the false VCs appear as hyperechoic structures whereas true cords are hypoechoic. Movements of the VFs occur during quiet respiration and phonation.[7] When air flows through the trachea and larynx, there is vibration and creation of mucosal wave. CDI can be used to visualise color images of mucosa-air interface and hence to deduce wavelength, frequency, and mean mucosal wave velocity.[8] Any disorders due to mass lesions, and nerve palsies present as irregular vibrations and altered mucosal wave velocity.
Dedecjus et al. evaluated VF movements in 50 thyroidectomy patients perioperatively with both USG and DL.[6] In two patients with VF paralysis, the VFDV decreased below 30 cm/s. The paralysis was confirmed using DL examination. VFDV decreased by 50% in eight patients postoperatively. This change was transitional in nature and subsided after 3 months. They concluded that USG can be used for detecting postoperative VF dysfunction. In our patients, we encountered 35–45% decrease in four patients that recovered in 3 months. VRL examination was unremarkable in these patients. This transient decrease could be attributed to temporary disturbances in the laryngeal mechanical framework or extralaryngeal scarring not evident on VRL.[9]
Ooi et al. used CDI of the VF in patients with known VF palsy.[10] They identified VF palsy in six patients using USG, which was confirmed with direct and indirect laryngoscopies. They concluded that layngeal USG can be as accurate as DL to detect VF palsies. In our study VF palsy was picked up in two patients with reduced VFDV and was confirmed using VRL.
Wang et al. used USG in 705 patients and could evaluate VC motion in 87% of them. Visualisation of VCs was better in females and young patients.[3] They concluded that USG can prove to be useful in unavailability or inexpertise in using DL. We were unable to visualise the VF in two patients using USG. Both the patients were elderly males and inability could be due to calcification of the cartilage causing an acoustic shadow underneath.[11]
About 1–5% patients scheduled for thyroid surgeries have RLN injury intraoperatively. Extensive lymphadenopathy, carcinoma, Graves' disease, and redo surgeries have a higher risk for palsies. RLN palsy can result in hoarseness and breathiness, but this usually does not occur due to slow progression of palsy with good compensation from contralateral side.[9] Also other causes of breathy voice like atrophic corditis or sulcus vocalis have to be ruled out. Hence, voice quality is not a reliable indicator of pre- or postoperative RLN involvement. USG along with VFDV can be successfully used for this purpose as shown in our observational study. The only way to confirm the results is through VRL as done in our study.
The major limitation of this study is the low number of patients with VF palsy, which might affect the sensitivity of USG. Our study was a pilot study; hence a study with larger sample size might be beneficial. We documented VFDV in all patients, but as the sample size was small with only two cases of palsy, we cannot generalise our criteria of VFDV reduction of less than 60 cm/s to all the patients. We would require a larger sample size to come to a cutoff value for palsy.
Also, there were no criteria for transitional or permanent nature of the palsy. USG as a diagnostic tool can be further studied in cord clinics and comparisons made with indirect laryngoscopy. There was inability to visualise the cords in few patients due to ossification of the cartilage. An age-related study with a larger sample would help to ascertain the effect of age on visualisation.
Fiber-optic and VRL visualization of the cords are established methods to check for the intergrity of the nerves. Though, there are numerous studies highlighting the use of USG to visualise the VC, its use remains underutilised in Indian scenario.[3,4,6,12] Our study suggests that USG might prove to be an easy, handy alternative to invasive fiber-optic/VRL to visualise VF in thyroid surgeries. More studies with larger sample size are required to substantiate the results.
CONCLUSION
USG might prove to be a noninvasive alternative to VRL to visualise the VCs in perioperative period. Future studies can help to substantiate results of this pilot study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Revised American Thyroid Association Management Guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–214. doi: 10.1089/thy.2009.0110. [DOI] [PubMed] [Google Scholar]
- 2.Shaha AR. Routine laryngoscopy in thyroid surgery: A valuable adjunct. Surgery. 2007;142:865–6. doi: 10.1016/j.surg.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Méndez Garrido S, Ocete Pérez RF. Causes and imaging manifestations of paralysis of the recurrent laryngeal nerve. Radiologia. 2016;58:225–34. doi: 10.1016/j.rx.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Wang CP, Chen TC, Yang TL, Chen CN, Lin CF, Lou PJ, et al. Transcutaneous ultrasound for evaluation of vocal fold movement in patients with thyroid disease. Eur J Radiol. 2012;81:e288–91. doi: 10.1016/j.ejrad.2011.09.020. [DOI] [PubMed] [Google Scholar]
- 5.Sabaretnam M, Ramakant P, Abraham DT, Paul MJ. Preoperative ultrasonography assessment of vocal cord movement during thyroid and parathyroid surgery. World J Surg. 2013;37:1740. doi: 10.1007/s00268-013-1921-0. [DOI] [PubMed] [Google Scholar]
- 6.Dedecjus M, Adamczewski Z, Brzeziński J, Lewiński A. Real-time, high-resolution ultrasonography of the vocal folds – A prospective pilot study in patients before and after thyroidectomy. Langenbecks Arch Surg. 2010;395:859–64. doi: 10.1007/s00423-010-0694-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Linares JP. Use of ultrasound in evaluation of vocal cords post thyroidectomy. Rev Colomb Anestesiol. 2014;42:238–42. [Google Scholar]
- 8.Shau YW, Wang CL, Hsieh FJ, Hsiao TY. Noninvasive assessment of vocal fold mucosal wave velocity using color Doppler imaging. Ultrasound Med Biol. 2001;27:1451–60. doi: 10.1016/s0301-5629(01)00453-7. [DOI] [PubMed] [Google Scholar]
- 9.Maeda T, Saito M, Otsuki N, Morimoto K, Takahashi M, Iwaki S, et al. Voice quality after surgical treatment for thyroid cancer. Thyroid. 2013;23:847–53. doi: 10.1089/thy.2012.0060. [DOI] [PubMed] [Google Scholar]
- 10.Ooi LL, Chan HS, Soo KC. Color Doppler imaging for vocal cord palsy. Head Neck. 1995;17:20–3. doi: 10.1002/hed.2880170105. [DOI] [PubMed] [Google Scholar]
- 11.Bozzato A, Zenk J, Gottwald F, Koch M, Iro H. Influence of thyroid cartilage ossification in laryngeal ultrasound. Laryngorhinootologie. 2007;86:276–81. doi: 10.1055/s-2006-945029. [DOI] [PubMed] [Google Scholar]
- 12.Wang LM, Zhu Q, Ma T, Li JP, Hu R, Rong XY, et al. Value of ultrasonography in diagnosis of pediatric vocal fold paralysis. Int J Pediatr Otorhinolaryngol. 2011;75:1186–90. doi: 10.1016/j.ijporl.2011.06.017. [DOI] [PubMed] [Google Scholar]


