Abstract
Background:
Behavioral and geographical factors may play a role in the acquisition of scrub typhus infection. In this prospective case–control study, we studied the factors associated with infection.
Patients and Methods:
Consecutive adult patients admitted with scrub typhus infection over 10 months were recruited. For every case, a geographical control from the same area and a gender-matched clinical control admitted with acute febrile illness were enrolled. The risk factors, which included sanitation, environment, activity, and protective measures, were compared between cases and controls using univariable and multivariable conditional logistic regression analysis and expressed as odds ratio (OR) with 95% confidence interval (CI).
Results:
The study cohort (n = 225; 132 female) aged 44 ± 17 years comprised of 75 cases and 150 controls from mid to low socioeconomic background. When compared with clinical controls, on univariable conditional regression analysis, cases were more likely to be involved in farming or gardening and less likely to have a toilet within the house. On multivariate regression analysis, only involvement in farming or gardening was associated with infection (OR: 4.2, 95% CI: 1.5–11.5). When compared with geographical controls, on univariable conditional regression analysis, cases were less likely to change undergarments or clothes before sleeping (OR: 3.5, 95% CI: 1.3–9.5) and more likely to have rodents in their house (OR: 2.5, 95% CI: 1–6.4) and rest on grass/mud without a mat (OR: 2.4, 95% CI: 1.1–5.3). On multivariate regression analysis, not changing undergarments or clothes tended to be associated with infection (OR: 2.7, 95% CI: 0.98–7.3).
Conclusion:
Certain behavioral factors predisposed our cohort to develop scrub typhus infection. Lifestyle changes may reduce the burden of scrub typhus in South India.
Keywords: Case–control, risk factors, scrub typhus, South India
INTRODUCTION
Scrub typhus, a zoonotic rickettsial infection caused by Orientia tsutsugamushi and transmitted through the bite of the larvae (chigger) of the Trombiculid mite, affects close to a million people annually in the endemic area called the tsutsugamushi triangle.[1] In some centers, it is an important cause of acute undifferentiated febrile illness with multiorgan dysfunction[2,3] that may be associated with significant morbidity and mortality. The presence of an eschar at the site of the bite, in some individuals, helps in the clinical recognition of the disease.
The mite species identified in India are Leptotrombidium deliense and Shoengastiella ligula.[4] The bacteria are maintained in the mite population by transovarian spread. The chiggers (larvae of the mite) rest on low-lying scrubs and grass in groups called islands of chiggers. They sense carbon dioxide generated by approaching warm-blooded animals, and this increases their activity. They drop off leaves onto their host and attach themselves to the hosts’ skin. Then, they feed on dead epidermal cells and fluids. After feeding for 2–3 days, the chigger gets engorged and falls off the host.[5] Thus, unlike other zoonosis, the vector does not seek out its host; the hosts put themselves at risk of a chigger bite through various activities. Increased exposure to the vector due to urbanization, development of antibiotic resistance, and significant morbidity and mortality in those who develop scrub typhus infection make preventive measures to reduce disease burden imperative.[6,7]
Previous studies from Asia have shown that exposure to scrubland, exposure of skin during working, and lack of use of protective gear are the key factors for the spread of this disease.[8,9,10,11] However, this does not explain the occurrence of the disease in urban areas or among people not engaged in farming. Although some factors described above are common in our setting, other features peculiar to people living in South India, such as the use of outdoor make-shift toilets (even among urban families), squatting in the outdoor, and cooking and drying clothes on open grass, may favor acquisition of scrub typhus in our setting. This study was therefore conducted to look at the environmental factors and the activities that put people at risk of acquiring scrub typhus in a semi-urban area in South India.
PATIENTS AND METHODS
Setting
This hospital-based, prospective case–control study was done in a tertiary care teaching hospital in South India. Consecutive patients admitted to the general medical wards and Intensive Care Unit from January to October 2013 were considered for inclusion.
Study cohort
Cases were patients who presented to the hospital with an acute febrile illness (AFI) and who fulfilled the modified World Health Organization case definition for scrub typhus.[12] Patients <18 years and those who did not have an appropriate geographic control were excluded. For every case, a geographical control and a clinical control were enrolled. A geographical control was the first gender-matched relative who came to visit the patient from the same neighborhood or district. The clinical control was the next, gender-matched patient, admitted in any of the medical wards with an AFI of <2 weeks with a diagnosis other than scrub typhus. Matching of gender was done as activities may be influenced by gender-defined roles. The rationale for the geographical control was that they would share a similar environment as the case so that the activities that put cases at risk of scrub typhus may be studied. Clinical controls were taken as they would have similar health-seeking behavior as the cases, and they would allow for comparison of risk factors in the environment and activities between the two groups.
Data collection
Before initiation of the study, field visits were conducted in the homes of three patients with proven scrub typhus infection. All were from a semi-urban area. They lived in thatched houses with mud flooring and had piles of wood outside their house. There was dense scrub vegetation within the compounds. None of the homes had a toilet inside the house; however, one had a thatched toilet in the backyard. The homes had wooden stoves (Chulha) on the floor, placed outside the house. In general, women wore saris with short-sleeved blouses while men wore sleeveless vests and a dhoti.
Based on the field visits and data from other studies on the pathogenesis of scrub typhus, a standardized questionnaire with the proposed risk factors was developed. This was administered to four patients admitted with AFI and simplified based on the pilot test. The principal investigator administered the questionnaire to every case and control individually, after obtaining written informed consent. However, when a patient was too sick to be interviewed, the interview was postponed until before discharge. If the patient was clinically deteriorating and deemed unlikely to survive the illness, the questionnaire was administered to the next of kin who lived with the patient. After the interviews, a health education session on prevention of scrub typhus was done, and pamphlets in vernacular were distributed. The study was approved by the Institutional Review Board and Ethics Committee (Ref no: 8112, dated January 2013).
Statistical aspects
Lauritsen JM. (Editor) EpiData version 3.1 (The EpiData Association, Denmark) Data Entry, Data Management and basic Statistical Analysis System. Odense Denmark, EpiData Association, 2000-2008. (Available from http://www.epidata.dk) was used for entering data, and analysis was done SPSS Inc. Released 2008. SPSS Statistics for Windows, Version 17.0. SPSS Inc., Chicago, IL, USA). Mean and standard deviation (SD) were calculated for continuous variables; for categorical variables, frequencies and percentages were recorded. Conditional univariate logistic regression analyses were used for identifying the risk factors relating to scrub typhus with a significance level of 0.20 and were included in the multivariable conditional logistic regression model and expressed as odds ratio (OR) with 95% confidence interval (CI).
RESULTS
During the study period, 75 consecutive patients with scrub typhus and 150 controls were recruited. The mean (SD) age of the entire cohort was 44 ± 17 years. There was a female preponderance (58.7%). More than half of the patients (53%) were from an urban area. A majority (88%) belonged to the low and middle socioeconomic strata and lived in thatched or mud houses. Most patients were from the local district (45.3%) while 38.7% were from a neighboring district situated about 30 km from our hospital. Only about 20% of the patients presented from a radius of over 70 km from the hospital. The mean (SD) age was similar in cases (44.5 ± 17.2), geographical controls (38.1 ± 10.6), and clinical controls (44.9 ± 17.5).
Climatic conditions
It was observed that there were only a few cases during the summer months. However, during the rainy season, the number of cases increased. The change in a number of cases corresponded to the rise in the humidity rather than to variations in the temperature [Figure 1].
Figure 1.
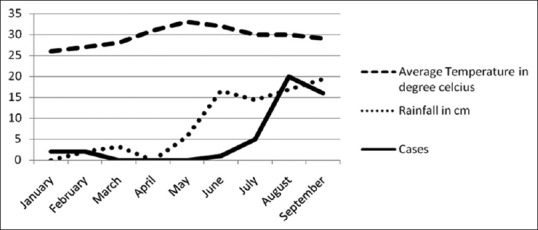
Incidence of scrub typhus cases over the study period (January to September 2013) and their relation to rainfall and temperature
Comparisons
The cases were compared to their clinical controls and geographical controls independently. The univariate analysis is summarized in Tables 1 and 2 and the multivariable conditional logistic regressions in Table 3.
Table 1.
Univariate analysis comparing sanitation and surroundings related risk factors in cases to clinical and geographical controls
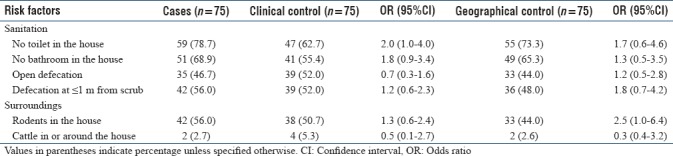
Table 2.
Univariate analysis comparing activity related risk factors and protective measures in cases to clinical and geographical controls
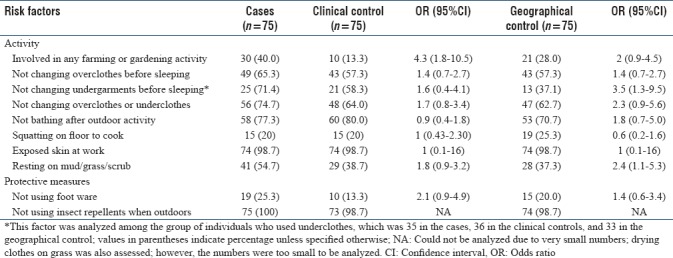
Table 3.
Multiple variable conditional logistic regression analysis of risk factors in case versus clinical and case versus geographical controls
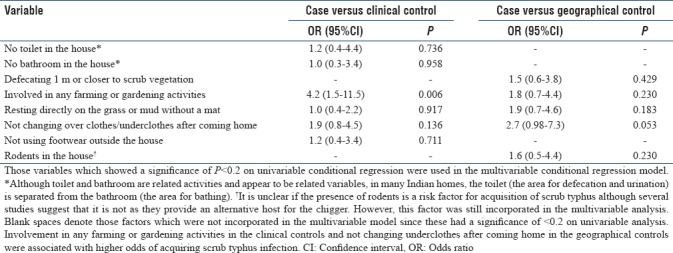
When compared with clinical controls, cases were more likely to be involved in farming or gardening activities (OR: 4.3, 95% CI: 1.8–10.5) and spend time resting directly, without a mat, on grass and mud (OR: 1.8, 95% CI: 0.9–3.2) and were also more likely to have no toilets within their houses (OR: 2.0, 95% CI: 1–4). The environmental risk factors (surroundings) were similar in the two groups. The use of protective measures was similar in the two groups [Tables 1 and 2]. The multiple variable conditional logistic regression analysis showed that involvement in any farming or gardening activity was associated with a 4 times higher risk of acquiring scrub typhus [Table 3], with an OR of 4.2 (95% CI: 1.5–11.5, P = 0.006).
When compared with geographical controls [Tables 1 and 2], cases were less likely to change undergarments before sleeping (OR: 3.5, 95% CI: 1.3–9.5) and more likely to rest directly, without a mat, on the grass or mud (OR: 2.4, 95% CI: 1.1–5.3). The presence of rodents in the house was also associated with higher odds of scrub typhus (OR: 2.5, 95% CI: 1.0–6.4). On multiple variable conditional logistic regression analysis [Table 3], not changing overclothes or underclothes after returning home tended to be associated with a higher risk of acquiring scrub typhus (OR: 2.7, 95% CI: 0.98–7.3, P = 0.053).
DISCUSSION
Scrub typhus is transmitted to humans either when a man/woman is exposed to the mite through certain activities or while dwelling in proximity to the vectors’ habitat. Every year, there is a surge of patients admitted with scrub typhus during the rainy season that claims many lives. Although the treatment of scrub typhus is relatively simple and inexpensive, comprising of a short course of doxycycline, about 30% develop severe illness necessitating intensive care treatment.[3] This adds to the financial strain on the limited resources in a developing country. Reports of doxycycline-resistant infection[7] further add to the concern. Given this background, it is important to study the factors associated with the acquisition of scrub typhus and determine if certain factors can be modified to tackle this problem.
The role of climatic conditions in the acquisition of scrub typhus is known. The increase in the number of cases in our study, during certain months, appeared to be a function of rainfall and humidity rather than temperature per se [Figure 1]. Similar observations were made by Li et al., who found that an increase of 1 mm of rainfall resulted in an increase of up to 1% cases in South China.[13] The changing global climatic conditions may lead to further increase in cases in the coming years. Although climate is a nonmodifiable factor, the observed incidence pattern of this disease during the rainy season could result in the implementation of certain public health measures (control of vector, reduction of scrub, and health education) during this season, particularly in highly endemic regions. This may impact the burden of disease.
The development of infection in young individuals, predominantly women from the middle and lower socioeconomic strata of society, is not surprising. In Korea, women are at a higher risk of acquiring Scrub typhus as they work in the farm in a squatting position and use their bare hands. This is unlike the men who stand while working and use tools.[8] In our cohort, apart from farming activity, the predilection of disease in women may be due to the lack of indoor toilets and the practice of open defecation since women are likely to go deeper into scrub vegetation when compared to men. In addition, women squat on the ground outdoors while cooking, and this could also contribute to acquisition of infection.
There are some differences in the risk factors observed in our study as compared with other studies. Factors such as presence of scrub vegetation around the house, presence of wood piles around the house, and presence of cattle around the house have been shown to be prominent factors for the acquisition of scrub typhus in previous studies.[9,10] However, these were not associated with infection in our study. If we look at geographical controls, where the environment is likely to be similar between cases and controls, not changing underclothes and overclothes before sleeping, resting on mud or grass, and presence of rodents in the house were associated with risk of infection on univariate analysis [Tables 1 and 2]. However, on multivariable analysis, not changing underclothes after coming home was the only factor that tended to be significant after adjusting for other factors [Table 3]. This observation is supported by work by Sharma et al., who observed this phenomenon in the Northern part of India, in Darjeeling.[10] This finding suggests that in a geographical environment that is endemic for scrub typhus, certain behavioral factors such as that observed in our study may put a patient at risk for developing infection.
If we look at clinical controls versus cases, the lack of toilets in the house, involvement in farming or gardening activities, and resting on mud or grass were associated with infection on univariate analysis. However, on multivariate analysis, only involvement in farming was associated with risk of infection. Out of 75 cases, 40 (53.3%) were from an urban area. This was not surprising since this group consisted mainly of daily wage laborers who usually leave their homes in villages to find work in the cities and live on the fringes of cities. These people work not only in the city when jobs are available in the city but also work in the farms during the rainy season when crops such as paddy, sugarcane, and groundnut are planted. This may explain the risk of scrub typhus in those involved with farming or gardening activities. Resting directly on mud or grass without a mat being a risk factor is again not surprising, since workers during long hours of work, rest in areas adjoining their workplace which often is close to scrub vegetation. This factor has been shown to be a risk factor in studies from Korea as well.[8] Resting on grass could lead to chiggers attaching onto the human host and subsequently infecting them, particularly if they do not change their clothes once they return from work.
The lack of toilets at home, in our study, was found to be a risk factor on univariate analysis. Open defecation has been shown to be a risk factor in South Korea.[8] Open defecation has to be looked at in terms of local cultural beliefs. In South India, there is a notion that the presence of toilets in the home is defiling. Hence, in many households, a bathroom is constructed within the house, whereas the toilet is either a shack within the compound of the house, outside the main structure of the house, or practiced as open defecation in the fields.
The study must be looked at in the light of some limitations. This was a prospective, hospital-based case–control study with two different controls for each case. Thus, it may not truly represent the entire community. Consecutive patients were recruited to overcome selection bias. Data was collected by administering a questionnaire and not by direct observation, and this might have introduced ascertainment bias. Although clinical cases were meant to recruit patients from a different geographical location, unfortunately, most patients (81%) in the study happened to be from within a 30 km radius from the hospital. This inadvertent overmatching could have resulted in not identifying multiple risk factors for disease acquisition since they are likely to have come from similar microenvironments. However, this overmatching in a scrub typhus endemic area probably adds strength to the observation that it is certain activities and behavioral factors such as involvement in farming and not changing undergarments and overclothes after coming home that are independent risk factors for scrub typhus infection and not the environment per se.
CONCLUSION
In a scrub typhus endemic area, certain activities such as farming and gardening and behavioral factors such as not changing garments after returning from work are associated with higher risk of acquiring scrub typhus infection. Public health interventions such as vector control, particularly during the rainy season, reduction of scrub vegetation, particularly in areas of farming or gardening, and health education may translate to reduction of burden of scrub typhus in South India.
Financial support and sponsorship
The study was supported by the Institutional Fluid Research Grant.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mccrumb FR, Jr, Stockard JL, Robinson CR, Turner LH, Levis DG, Maisey CW. Leptospirosis in Malaya. I. Sporadic cases among military and civilian personnel. Am J Trop Med Hyg. 1957;6:238–56. [PubMed] [Google Scholar]
- 2.Chrispal A, Boorugu H, Gopinath KG, Chandy S, Prakash JA, Thomas EM, et al. Acute undifferentiated febrile illness in adult hospitalized patients: The disease spectrum and diagnostic predictors - An experience from a tertiary care hospital in South India. Trop Doct. 2010;40:230–4. doi: 10.1258/td.2010.100132. [DOI] [PubMed] [Google Scholar]
- 3.Varghese GM, Trowbridge P, Janardhanan J, Thomas K, Peter JV, Mathews P, et al. Clinical profile and improving mortality trend of scrub typhus in South India. Int J Infect Dis. 2014;23:39–43. doi: 10.1016/j.ijid.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 4.Tilak R, Kunwar R, Wankhade UB, Tilak VW. Emergence of Schoengastiella ligula as the vector of scrub typhus outbreak in Darjeeling: Has Leptotrombidium deliense been replaced? Indian J Public Health. 2011;55:92–9. doi: 10.4103/0019-557X.85239. [DOI] [PubMed] [Google Scholar]
- 5.Traub R, Wisseman CL. Ecological considerations in scrub typhus. Bull World Health Organ. 1968;39:219–30. [PMC free article] [PubMed] [Google Scholar]
- 6.Kim MS, Baek JH, Lee JS, Chung MH, Lee SM, Kang JS, et al. High in vitro infectivity of a doxycycline-insensitive strain of Orientia tsutsugamushi. Infect Chemother. 2013;45:431–4. doi: 10.3947/ic.2013.45.4.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Watt G, Chouriyagune C, Ruangweerayud R, Watcharapichat P, Phulsuksombati D, Jongsakul K, et al. Scrub typhus infections poorly responsive to antibiotics in Northern Thailand. Lancet. 1996;348:86–9. doi: 10.1016/s0140-6736(96)02501-9. [DOI] [PubMed] [Google Scholar]
- 8.Kweon SS, Choi JS, Lim HS, Kim JR, Kim KY, Ryu SY, et al. A community-based case-control study of behavioral factors associated with scrub typhus during the autumn epidemic season in South Korea. Am J Trop Med Hyg. 2009;80:442–6. [PubMed] [Google Scholar]
- 9.Lyu Y, Tian L, Zhang L, Dou X, Wang X, Li W, et al. A case-control study of risk factors associated with scrub typhus infection in Beijing, China. PLoS One. 2013;8:e63668. doi: 10.1371/journal.pone.0063668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma PK, Ramakrishnan R, Hutin YJ, Barui AK, Manickam P, Kakkar M, et al. Scrub typhus in Darjeeling, India: Opportunities for simple, practical prevention measures. Trans R Soc Trop Med Hyg. 2009;103:1153–8. doi: 10.1016/j.trstmh.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 11.Kim DM, Kim KY, Nam HS, Kweon SS, Park MY, Ryu SY, et al. Risk-factors for human infection with Orientia tsutsugamushi: A case-control study in Korea. Clin Microbiol Infect. 2008;14:174–7. doi: 10.1111/j.1469-0691.2007.01901.x. [DOI] [PubMed] [Google Scholar]
- 12. [Last accessed on 2016 Jul 03]. WHO_CDS_CSR_ISR_99.2.pdf. Available from: http://www.apps.who.int/iris/bitstream/10665/65517/1/WHO_CDS_CSR_ISR_99.2.pdf .
- 13.Li T, Yang Z, Dong Z, Wang M. Meteorological factors and risk of scrub typhus in Guangzhou, Southern China, 2006-2012. BMC Infect Dis. 2014;14:139. doi: 10.1186/1471-2334-14-139. [DOI] [PMC free article] [PubMed] [Google Scholar]


