Abstract
RNAi is emerging as a powerful approach in cancer treatment. siRNA is an important RNAi tool that can be designed to specifically silence the expression of genes involved in drug resistance and chemotherapeutic inactivity. Combining siRNA and other therapeutic agents can overcome the multi-drug resistance phenomenon by simultaneously silencing genes and enhancing chemotherapeutic activity. Moreover, the therapeutic efficiency of anti-cancer drugs can be significantly improved by additive or synergistic effects induced by siRNA and combined therapies. Co-delivery of these diverse anti-cancer agents, however, requires specially designed nanocarriers. This review highlights the recent trends in siRNA/anti-cancer drug co-delivery systems under the major categories of liposomes/lipid, polymeric, and inorganic nanoplatforms. The objective is to discuss the strategies for nanocarrier-based co-delivery systems using siRNA/anti-cancer drug combinations, emphasizing various siRNA targets that help overcome multi-drug resistance and enhance therapeutic efficiency.
Keywords: Cancer therapy, Chemotherapeutic, Co-delivery, Liposome, Nanoparticle, siRNA
Introduction
Worldwide, there is a continuing interest in identifying new strategies for cancer treatment [1,2]. Finding and modulating the genes responsible for cancer pathology is one such approach. A growing number of studies have suggested that RNA interference (RNAi) as a promising gene manipulation technique with therapeutic potential, when used alone or in conjunction with other treatments [3–5]. However, siRNA or shRNA-based therapy relies on successful delivery to the target [6,7]. Hence, these approaches require a safe and efficient carrier system for in vivo use.
The use of viral vectors for therapeutic gene delivery has been controversial because of possible immunogenic and undesirable gene mutation effects [8]. The availability of various non-viral, nanoparticle-based delivery systems has contributed to tremendous advancements in siRNA-based therapeutics for cancer [9]. It has been shown that nanoparticle delivery systems improve the systemic stability of siRNA, prevent premature degradation and rapid in vivo clearance of siRNAs, and enhance selectivity towards the target [10–12].
In addition, siRNA has been widely explored for use in combination therapy [13–16]. Combination therapy relies on the simultaneous action of multiple therapeutic entities to exploit additive or synergistic effects and enhance therapeutic efficiency. In clinical settings, combination chemotherapy refers to the grouping of multiple chemotherapeutic agents that use different mechanisms to treat cancer. The combination strategy not only enhances therapeutic efficiency, but also reduces the risk of severe side effects caused by cytotoxicity of individual drugs [17]. The use of siRNA in combination with other anti-cancer therapeutics has been shown to improve outcomes by either increasing the sensitivity of cancer towards a therapeutic modality, or by working in an additive or synergistic fashion [18].
Advancements in nano-drug delivery systems improved the co-delivery of siRNA and other therapeutic agents [19]. Nanoparticle carriers supporting the combination of anti-cancer therapeutics, such as chemotherapy agents, photodynamic sensitizers, or small molecule inhibitors, with siRNA have been developed. This review primarily focuses on the nanodelivery system advancements for siRNA-chemotherapeutic combination(s) in cancer treatment.
Significance of siRNA in combination with other therapeutics
Cancers are highly heterogenic in nature and often become resistant to therapies [20]. Resistance may develop towards different treatment modalities, including chemotherapy, radiation therapy, and photodynamic therapy (PDT). The mechanisms of treatment resistance are complex, although several molecular mechanisms have been elucidated [21].
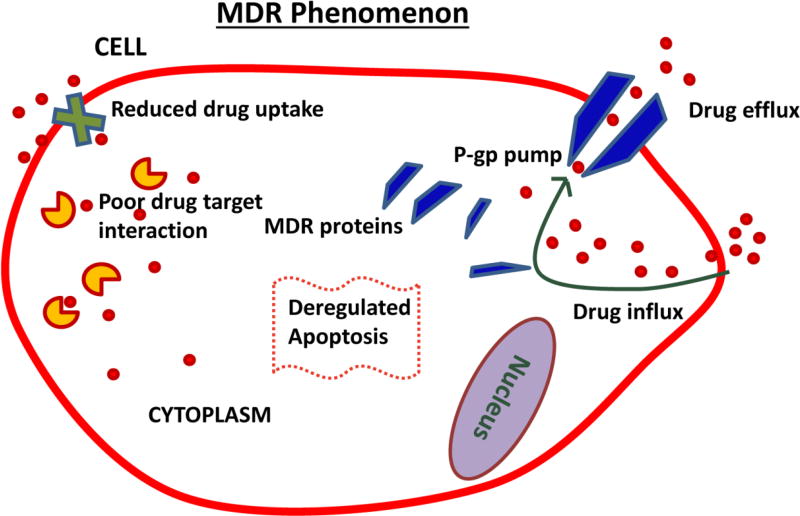
The development of multi-drug resistance (MDR) poses a significant challenge. Many researchers have comprehensively reviewed the molecular mechanisms of MDR in cancer [21–23]. Increased drug efflux, altered levels of intracellular target, and overexpression of resistance-related, anti-apoptotic genes leading to the expression of MDR proteins are prominent mechanisms of MDR in cancer cells (Figure 1). MDR ultimately results in a lower cellular concentration of drug, which limits apoptosis and prevents other cytotoxic events. siRNA-based gene therapy has been shown to effectively overcome MDR in cancer, when combined with chemotherapeutics [5,24–26]. The suppression of genes related to MDR may increase the chemosensitivity of cancer cells and improve treatment efficacy.
Figure 1.
Illustration depicts multi-drug resistance (MDR) mechanisms in cancer cells. Enhanced drug efflux, expression of MDR proteins, reduced drug uptake, poor drug target interaction, and deregulated apoptosis are some of the important mechanisms.
PDT involves the treatment of cancer with multiple components, including light, photosensitizers, and oxygen [27]. The localized excitation of photosensitizer molecules by light results in conversion of molecular oxygen to reactive oxygen species, which interact with biomolecules in cancer cells and kill them by triggering apoptosis. The combination of siRNA with PDT enhances therapeutic responses in cancer [28,29]. Many studies demonstrated that autophagy-related genes are major targets for siRNAs to improve cancer cells’ response to PDT [30,31]. Co-delivery of a photosensitizer and siRNA via nanoparticles might be an important treatment strategy. PDT combined with siRNA has also been utilized in cancer immunotherapy [32,33]. Activating human immune cells (T-cells) to attack cancer cells is a strategic way of utilizing the body’s own immune system against cancer. By suppressing certain genes in immune inhibitory pathways with siRNA, it is possible to safely and effectively render T-cells immunogenic against cancer.
SiRNA therapy complements radiation therapy by targeted suppression of specific genes that cause radiation resistance, resulting in an enhanced tumor response to radiation [34–36]. The AMPK pathway has been shown to be upregulated in tumors that exhibit radiation therapy resistance [37]. Recent reports suggest that the overexpression of proteins like PD-L1, HuR, and Ape-1 causes radiation resistance in some cancers [34,36,38]. Increased DNA damage repair machinery is also a prominent mechanism of radiation resistance. Although new developments in nanomedicine have explored the use of nanoparticles for radio-sensitization [39], there are not extensive investigations on radionuclide/siRNA co-delivery using nanoparticle drug delivery systems, until now.
To achieve the best therapeutic efficiency out of combination of siRNA and other therapeutics precise and efficient nanoparticle delivery systems are required. The following section discusses various nanoparticle systems that have been particularly investigated for siRNA-based combination therapy in cancer.
Nanoparticle-assisted co-delivery of siRNA and other chemotherapy agents
Chemotherapeutic drugs have been used as front-line treatment for many cancers. However, tumor heterogeneity and the development of drug resistance have resulted in the reduced effectiveness of numerous cancer drugs that are commonly used in the clinic [40]. Nucleic acid therapeutics in combination with drugs compliment chemotherapy in various ways such as silencing specific genes involved in drug resistance and anti-apoptosis mechanism, by restoring tumor suppresser genes and by introducing apoptotic genes. The combination of chemotherapy with RNAi can be achieved by either co-treatment with individual therapeutic agents [41] or by co-delivery of chemotherapeutics and siRNA via a single carrier [42]; the latter known to be more efficient [43,44].
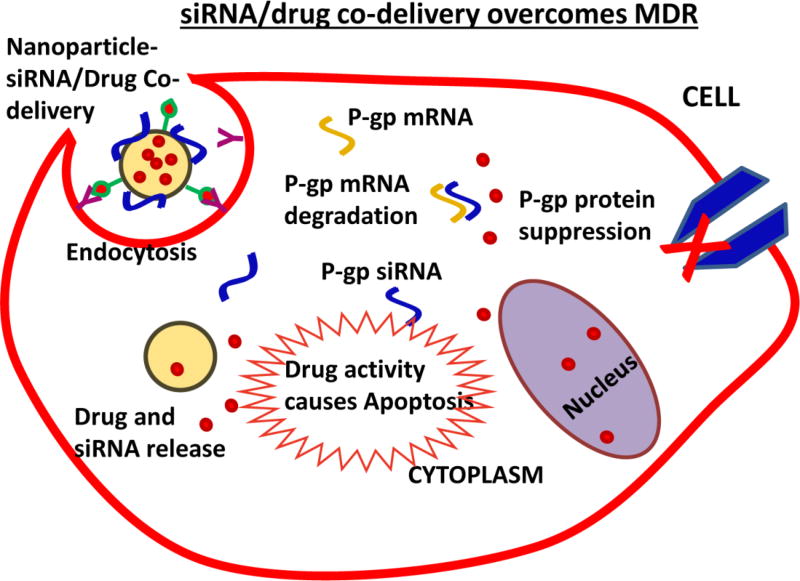
Co-delivery of multiple agents can be achieved with nanoparticle carriers that have the capability of packaging and releasing individual therapeutic agents in a controlled fashion at the desired site [44]. Various nanoparticle carriers, such as liposomes, polymer-based nanoparticles, and inorganic nanoparticles, have been introduced for co-delivery of siRNA and chemotherapeutics. The co-delivery of siRNA and chemotherapeutics by nanoparticles results in a combined therapeutic response due to siRNA-based target gene silencing and cytotoxic drug activity (Figure 2).
Figure 2.
Nanoparticle-based co-delivery of siRNA and chemotherapeutic drug overcomes MDR by siRNA-mediated p-glycoprotein (p-gp) suppression. Increased drug accumulation in cells triggers apoptosis mechanisms.
The next section discusses some successful strategies in nanoparticle-based nucleic-chemotherapeutic co-delivery systems. Relevant examples of siRNA in combination with PDT, immunotherapy, and radiotherapy are also mentioned.
Liposomes or lipid-based nanoparticles
Liposomes are well known for their ability to carry nucleic acid therapeutics and/or chemotherapeutic agents [45]. The easy manipulation of the lipid components to suit nucleic acid interaction and co-encapsulation of one or multiple drugs make liposomes advantageous for combination drug delivery. Co-delivery efficiency may depend on how the anti-cancer agents are packaged and their interaction with the lipid components of the carrier [46]. Cationic liposomes usually utilize ionic interactions between the positively charged liposome surface and the negatively charged siRNA to form a siRNA-liposome complex [47]. However, if the carrier liposome is anionic or neutrally charged, siRNAs may be encapsulated in the aqueous core [48]. Proper packaging of nucleic acid in liposomes can also occur through condensation using cationic polymers like protamine [48] or PEI [49], which enhances siRNA stability. Depending on the solubility, chemotherapy drugs are either encapsulated in the aqueous core or embedded in the lipid bilayer during liposome preparation. Therefore, the solubility and stability of nucleic acid and chemotherapeutics are important factors.
Lipid-based nanoparticles typically harness the cationic property of lipids by modifying the physicochemical properties of nanoparticles made of different materials. For example, calcium phosphate nanoparticles use lipid to support the delivery of nucleic acid therapeutics [50]. Such nanoparticles that utilize the properties of multiple materials during fabrication are generally categorized as hybrid nanoparticles for specific drug delivery applications.
Liposomal nanocarriers have benefitted from more advancement in their application as co-delivery systems. Simple PEGylated liposomes [51], advanced stimuli-responsive liposomes [52,53], and targeting liposomes [54,55] have all been constructed for siRNA/chemotherapeutic co-delivery in cancer. Using a PEGylated liposome to co-deliver, BCL2 siRNA with docetaxel successfully inhibited lung cancer in vitro and in vivo [51]. The PEGylation of the liposomal carrier prolonged the circulation time of liposomes in vivo and facilitated passive co-delivery of BCl2 siRNA and docetaxel to the tumor. Synergism was reported between these therapeutic molecules in an A549 xenograft model upon successful co-delivery using liposomes [51]. Another study by Yao et al. [53] used a pH-sensitive liposome to co-deliver sorafenib and a therapeutic siRNA in cell culture and a mouse model of liver cancer. The pH-sensitive liposome was constructed by modifying pH-sensitive carboxymethyl chitosan onto a liposome preloaded with siRNA and sorafenib. Drug release was pH-sensitive, and the liposome successfully co-delivered siRNA and sorafenib. Peng et al. [52] developed a thermosensitive magnetic liposome for co-delivery of shRNA and doxorubicin in gastric cancer in vitro and in vivo. This advantageous system combined magnetic targeting, thermosensitive controlled release, and synergistic anti-tumor efficacy [52].
The functionalization of lipids with small molecule ligands for active targeting of specific receptors overexpressed in cancer cells offers significant advantages for cancer treatment. Recently, ligand conjugated liposomal systems have been optimized for targeted delivery of a combination of siRNA and chemotherapeutic drug(s). Yang et al. [55] reported the use of folic acid-modified liposomes for the targeted co-delivery of Bmi1 siRNA and doxorubicin in KB, HeLa, and Hep3B cancer cells, and a KB xenograft tumor model. They observed folic acid receptor (FR)-expression-dependent cell uptake of folic acid-modified liposomes (DOTAP/Chol/mPEG-DSPE/FA-PEG-Chol) in cancer cells. In vivo administration resulted in effective Bmi1 gene silencing, and enhanced doxorubicin’s cytotoxicity. The combination of doxorubicin and Bmi1 siRNA delivered via folate-liposome had an enhanced therapeutic effect against cancer, compared with individual agents. Since this liposomal carrier enhanced hepatic accumulation, the co-delivery strategy may be useful against liver cancer; however, this approach remains to be investigated.
Another study demonstrated the targeted co-delivery of siRNA and chemotherapeutic agent to liver tumors [54]. A liposomal carrier for the co-delivery of vimentin siRNA and doxorubicin was prepared from a mixture of lipids: DMKE (O,O’-dimyristyl-N-lysyl glutamate), cholesterol, galactosylated ceramide, POPC (1-palmitoyl-2-oleoyl-sn-glycero-3-phosphocholine), and PEG2000-DSPE (distearoyl phosphatidyl ethanolamine). Targeting was conducted by modifying the nanoparticle system with galactosyl ligand targeted to asialoglycoprotein receptors (ASGPR) expressed in hepatic cancer cells. This Gal-DOX-siRNA-L co-delivery system demonstrated great potential for synergistic antitumor therapy.
Modifying liposomal carriers using multiple targeting moieties might be a feasible option in co-delivering siRNA and chemotherapeutic. This strategy was successfully used by Yang et al. [56] to treat brain tumors in vitro and in vivo. The cationic liposome was modified using dual-peptides that targeted the LDL-protein receptor-related protein receptor (Angiopep-2) and the neuropilin-1 receptor. The liposome loaded with VEGF siRNA and docetaxel (DTX) was targeted against glioma, and the peptide-mediated cell penetration enhanced the co-delivery of VEGF siRNA and DTX to the tumor cells. Anti-angiogenesis and cellular apoptosis effects were combined with this approach. The synergism between siRNA and the chemotherapeutic agent effectively inhibited tumor growth.
Lipid-based nanoparticles have also been used in a combination of siRNA and PDT to treat some cancers. In a typical study, Chen et al. [57] demonstrated that a combination of HIF-1α siRNA-loaded lipid-calcium phosphate nanoparticle (LCP) and photosan-mediated PDT significantly inhibited head and neck tumor growth in vitro and in vivo. The anisamide-modified LCP nanoparticles/HIF-1α siRNA, which significantly inhibited cell growth and enhanced cell death and proliferation when combined with PDT, were targeted to cancer cells overexpressing sigma receptors. When systemically administered, LCP nanoparticles/HIF-1α siRNA reduced HIF-1α expression in mouse xenograft tumors. When PDT was combined with this siRNA based gene silencing, tumor regression was significantly enhanced. The combination of LCP-based HIF-1α delivery and photosan-mediated PDT was more effective than HIF1α siRNA or PDT alone. A recent study demonstrated that LCP nanoparticle delivery of VEGF-siRNA combined with photosan-mediated PDT significantly reduced tumor growth in xenograft models of human head and neck squamous cell carcinoma (HNSCC) [58]. This LCP nanoparticle was also modified with anisamide to target sigma receptors in cancer cells.
The anti-tumor efficacy of small molecule inhibitors is enhanced upon co-delivery of therapeutic siRNA using a single liposomal vehicle. Inhibition of the Ras group of oncoproteins is considered difficult. However, scientists have developed MEK inhibitors that act downstream of Ras in the MAP kinase pathway, indirectly targeting Ras [4] Golan et al, 2015]. The effect of these MEK inhibitors was further enhanced by co-delivery of Mcl1-specific siRNA via a cationic liposome [59]. The hydrophobic MEK inhibitor molecules were encapsulated in the lipid bilayer, and were then complexed with the Mcl1 siRNA and co-delivered to achieve enhanced antitumor effects in cell culture and a mouse model. Cationic liposomes have also been used to combine multiple siRNAs with a chemotherapeutic agent. Saad et al. [60] used this strategy to co-deliver MRP1 and BCl2 siRNAs with doxorubicin to overcome MDR and to target different pathways or cell growth inhibition mechanisms.
Hence the application of liposomes in co-delivery of siRNA and other therapeutics have a major impact in experimental and translational cancer therapeutics. Some of the well-known challenges with liposomes are their unsatisfactory in vivo stability and burst release of loaded drug. Many of these challenges have been addressed to a great extent by modification of liposome surface or bilayer with additional components [61–64]. The limitations still existing in liposomal platforms may be improved by newer technological advances that may allow continued translational success in cancer therapy.
As alternative to liposomes, niosomes are widely-used drug delivery carriers because of their similar properties [65–67]. Niosomes are known for more than two decades in drug delivery applications [67–69]. Niosomes are formed by the self-association of nonionic surfactants and cholesterol in an aqueous phase and have shown good physico-chemical stability and excellent loading efficiency of drugs of both hydrophilic and hydrophobic nature and also oligonucleotides [65, 66, 70]. The biodegradable, biocompatible and nontoxic nature of niosomes and their easy manipulation with targeting ligands makes them attractive drug delivery systems for cancer therapy [71]. In an earlier study, the hydrophilic anti-cancer agent doxorubicin was encapsulated in niosomes for studying its metabolism, tissue distribution and anti-tumor activity in a mouse model [68]. Niosomes were prepared from sorbitan monostearate (Span 60), cholesterol and choleth-24 (a 24 oxyethylene cholesteryl ether) in typical molar ratios and used as a carrier for doxorubicin for treating MAC 15A subcutaneously implanted tumor in mice. This niosomal formulation enhanced the tumor accumulation of doxorubicin compared to free doxorubicin, leading to doubling of tumoricidal activity. Later the same group studied the doxorubicin containing niosomal formulation in ovarian tumor models in mice [69]. The C16G2 (a hexadecyl diglycerol ether) based niosomes were equally potent when compared with free doxorubicin. Further the study also demonstrated that span 60 niosomes were able to reduce the IC50 value of doxorubicin, though modestly, as compared to C16G2 niosomes and free doxorubicin. Niosomes were also efficiently delivered oligonucleotides to mammalian cells. In a typical study, niosomes were prepared by synthetic aminolipid, 2,3-di(tetradecyloxy)propan-1-amine and polysorbate-80 for delivery of antisense oligonucleotides against Renilla luciferase mRNA in HeLa cells [72]. The niosomes were not cytotoxic and efficiently transfected HeLa cells using oligonucleotides when used at a charge ratio of 1:14, in comparison with cytotoxic commercial transfection reagent, lipofectamine.
Recently, niosomes have explored for combinatorial drug delivery for cancer therapy. For instance, Rajput et al [73] demonstrated that an acidic milieu-sensitive multi-lamellar gold niosomes (Nio-Au) were able to co-deliver Akt-siRNA and thymoquinone (TQ) in tamoxifenresistant and Akt-overexpressing MCF7 breast cancer cells. TQ was encapsulated in hydrophobic core of the niosomes whereas siRNA was electrostatically bound with cationic niosomes. This combination delivery strategy enhanced the sensitivity of breast cancer cells to tamoxifen by efficient knockdown of Akt expression. Studies in xenograft tumor models in mice revealed that niosome formulation of Akt siRNA and TQ combination enhanced the apoptosis and MDM2 inhibition in therapy-resistant cancer [73]. These studies suggest that niosomes are promising alternative to liposomes which is capable of delivering drug or gene or a combination of both, in cancer therapy.
Polymer nanoparticles
Polymers offer a promising nanoparticle platform for siRNA/anticancer drug co-delivery. These materials have been extensively studied as a delivery system for siRNA and chemotherapy [74,75]. Polymer nanoparticles can be easily fine-tuned for any size and allow good packaging of the payload by physical or ionic interactions. They are ideal platforms with which to construct core-shell nanoparticles, allowing them to carry multiple agents, such as siRNA, plasmid DNA, and chemotherapeutic drugs, simultaneously [24]. Cationic polymers, including polyethylene imine, chitosan, and poly-l-lysine, are commonly employed for gene delivery applications because of their strong ionic interaction with nucleic acids to form polyplexes. Nanoparticles fabricated from amphiphilic polymers, like PLGA and atellocollagen, have also shown promise as drug and gene delivery vehicles. Due to the distinct physicochemical properties of different polymers, most co-delivery strategies use multiple polymers in the nanoformulation process [76,77].
In contrast to the soft nature of liposomes, polymer nanoparticles are solid particles that carry drugs in their network or matrix, and are more stable. Due to these properties, the entrapped or encapsulated drugs show more sustained and controlled release patterns over time. However, drug release also depends on the type of interaction between the drug and the polymer backbone of the nanoparticle [78]. Physically conjugated drug may result in slower and more controlled release, usually over many days, in contrast to the fast, but time-dependent, release of weakly bound drug. Nevertheless, the desired controlled release properties can be achieved for each individual payload based on how the nanoparticle co-delivery system was formulated.
Polylactic acid-co-glycolic acid (PLGA) or polylactic acid (PLA) nanoparticles are sought-after platforms for co-delivery of siRNA and chemotherapeutics. PLGA nanoparticles have a well-defined spherical and nano-capsular structure, and are biocompatible. These nanoparticles offer high drug loading capacity and are easy to manipulate to carry siRNA therapeutics. PEI modified PLGA nanoparticles are attractive nanoparticle platform for carrying siRNA and combination drugs as demonstrated by Su et al. [79]. PLGA nanoparticles carrying paclitaxel with PEI as a co-polymer was synthesized, and the siRNA was electrostatically adsorbed onto its surface. Since STAT3 overexpression is implicated in paclitaxel resistance in lung cancer, they combined STAT3 siRNA with paclitaxel in the same nanoparticle carrier. The co-delivery efficiency of this nanoparticle system was monitored in A549 lung cancer cells with Oregon green paclitaxel and cy5-labelled STAT3 siRNA. The researchers concluded that STAT3 siRNA co-delivered PLGA-PEI nanoparticles exerted higher cytotoxicity than their STAT3 siRNA-free counterpart. Moreover, sensitivity to treatment increased in paclitaxel-resistant A549 lung cancer cells after the co-delivery of STAT3 siRNA and paclitaxel by PLGA-PEI nanoparticles [79].
In a similar approach Patil et al. [80] designed PLGA-PEI nanoparticles for siRNA/drug co-delivery for lung cancer therapy in vitro and in vivo. They in-situ-coated PEI to PLGA in the nanoparticle preparation itself, instead of coating PEI into the preformed PLGA nanoparticle with loaded drug [80]. Biotin, the target ligand, was introduced into the PLGA-PEI nanoparticle system as a PLA-PEG-Biotin conjugate. The resulting nanoparticle system loaded with paclitaxel and p-gp siRNA was used to treat biotin-receptor-overexpressing, drug-resistant JC (mammary adenocarcinoma) tumors in BALB/C mice. They observed that paclitaxel, either in its free form or as encapsulated in PLGA-PEI nanoparticles, did not suppress tumor growth, while the co-delivery of paclitaxel with p-gp siRNA effectively silenced the specific gene and enhanced the tumor’s response to paclitaxel.
Recently, we demonstrated the efficacy of chitosan-coated polylactic acid nanoparticles as co-delivery vehicles for P62 siRNA, Beta-5 plasmid DNA (pDNA), and cisplatin (CDDP) in cisplatin-resistant ovarian cancer cells [24]. The CDDP was encapsulated in the PLA core, and the siRNA/pDNA was adsorbed onto the cationic-chitosan coating of the nanoparticle through electrostatic interaction. By suppressing the autophagy regulatory protein P62 using siRNA and restoring the proteasome Beta-5 function using pDNA via chitosan-coated, CDDP-loaded PLA nanoparticles, the sensitivity of ovarian cells to CDDP significantly improved.
Chitosan is a biodegradable and biocompatible polymer with attractive properties for the delivery of nucleic acids in combination with chemotherapeutics. This polymer is a well-known gene delivery vehicle that forms rapid, self-assembled complexes with siRNA or DNA to form nano-sized particles. The presence of many free amino groups allows chitosan to undergo a crosslinking reaction with counter ions, such as thiamine pyrophosphate or tri polyphosphate, resulting in ionic gelation of chitosan and production of nanoparticles under optimal cation-to-anion ratios. siRNA or drug may be entrapped in the crosslinked chitosan network, increasing particle stability, but decreasing the rate of drug release. Since most chemotherapeutic drugs are hydrophobic, the co-delivery of chemotherapeutics would be difficult without chemically modified chitosan or supporting chitosan with other hydrophobic polymers.
Recently, Wei et al. [81] introduced a modified chitosan-based nanoparticle system for co-delivery of mTERT siRNA and paclitaxel. The nanoparticle platform was fabricated using N-((2-hydroxy-3-trimethylammonium) propyl) chitosan chloride (HTCC) with a positive charge for interaction with siRNA. This system efficiently delivered siRNA in vivo. This chitosan-based nanoparticle was then developed into a two-in-one co-delivery system encapsulating paclitaxel and mTERT siRNA. This co-delivery strategy using an HTCC nanoparticle enhanced the efficacy of paclitaxel due to simultaneous delivery with mTERT siRNA, resulting in significant tumor suppression in vivo. Importantly, this chitosan-based nanoparticle system assisted the synergistic activity of paclitaxel and mTERT siRNA, and thereby shows promise for the delivery of a siRNA/hydrophobic drug combination in cancer therapy [81].
Chitosan is also useful in the co-delivery of hydrophilic drug and siRNA. In a recent study, a carboxymethyl chitosan nanoparticle was designed to co-deliver siRNA towards IL17RB (associated with cell growth, proliferation migration, and poor prognosis in patients with breast cancer) and doxorubicin in breast cancer cells [82]. Simultaneous delivery of IL17RB siRNA and doxorubicin was possible with this carboxymethyl chitosan nanoparticle, and resulted in efficient suppression of IL17RB-related genes, like NF-kB and Bcl-2, apoptosis, and inhibited migration of MDA-MB361 breast cancer cells.
In addition, chitosan is used as a prominent component of co-delivery vehicles due to its high biocompatibility. In a typical study, a chitosan-based triblock micellar structure was prepared for the co-delivery of p-glycoprotein siRNA and doxorubicin to overcome MDR in a liver tumor model in vivo [76]. The N-succinyl chitosan–PLL–palmitic acid (NSC–PLL–PA) nanoparticles, in which n-succynyl chitosan served as a hydrophilic shell, improved the half-life of micelles and reduced the toxicity of poly-l-lysine (PLL). Doxorubicin was encapsulated in the palmitic acid core, and siRNA was adsorbed onto the micelles using a PLL skeleton. The co-delivery of p-gp siRNA and doxorubicin using NSC–PLL–PA nanoparticles bypassed drug efflux transporters by downregulating p-gp expression, and increased doxorubicin accumulation in the cancer cells. This chitosan-micelle-based co-delivery strategy ultimately improved the antitumor activity through the synergistic activity of p-gp siRNA and doxorubicin.
Various polymers with distinct physicochemical properties are being used together to fabricate nanoparticles with interesting features for co-delivery of nucleic acid therapeutics and anticancer drugs. Among the cationic polymers, polyethyleneimine has been extensively used, alone or in combination with other polymers, in siRNA co-delivery systems. Shen et al. [42] designed a poly(D,L-lactide-co-glycolide) (PLGA) nanoparticle bearing disulfide-linked reducible polyethyleneimine (PEIs) covered by hyaluronic acid (HA) for co-delivery of COX-2 siRNA and docetaxel. The hydrophobic drug docetaxel was incorporated into the PLGA core, and the siRNA was electrostatically linked to the cationic PEI layer of the nanoparticle. The presence of HA was used to target the therapeutic agents towards CD44-overexpressing gastric cancer cells. This co-delivery strategy suppressed COX2 gene expression in the target cells. This PEI-based nanoparticle system has promise as an excellent co-delivery system targeting CD44-overexpressing tumors, as supported by in vivo biodistribution data showing that the HA-modified nanoparticle system allowed enhanced docetaxel accumulation in tumors, compared with RES organs.
The presence of numerous free amino groups allows PEI to be conjugated with various moieties to improve its physicochemical properties for co-delivery formulation. Recently, Xu et al. [83] prepared a pH-sensitive nano-formulation using PEI for co-delivery of siRNA and doxorubicin in models of metastatic lung cancer. Doxorubicin was conjugated to PEI using a pH-sensitive hydrazine bond; the system was complexed with BCl2 siRNA. The pH-sensitive linkage in nanoparticles allowed controlled, pH-responsive release of doxorubicin in vivo. The combination with BCL2 siRNA enhanced the therapeutic efficiency of doxorubicin in a B16F10 lung tumor model. This PEI-based nanoparticle system is a promising strategy for pulmonary co-delivery of siRNA and chemotherapeutic agent(s) to treat lung cancer.
Triblock co-polymer systems are also attractive delivery systems for siRNA/chemotherapeutic combinations [84]. It was shown that triblock co-polymer methoxy-poly(ethyleneglycol)-block-poly(L-glutamate-hydrazide)-block-poly(N,N-dimethylaminopropyl methacrylamide) was functionalized with folate (FA/m-PEG-b-P(LG-Hyd)-b-PDMAPMA) for co-delivery of p-gp siRNA and doxorubicin [85]. Doxorubicin was conjugated to the poly(L-glutamate-hydrazide) blocks using a pH-sensitive linkage. The nanoparticles were formed by self-assembly of these polymers and doxorubicin. The p-gp siRNA was then electrostatically bound to cationic poly(N,N-dimethylaminopropyl methacrylamide) (PDMAPMA) blocks to form nanocomplexes. The drug and siRNA release in vitro was pH-dependent. The nanoparticles were targeted by FA towards MCF-7 cells and showed enhanced cell uptake and cytotoxicity.
Biswas et al. [86] demonstrated a different triblock co-polymer nanoparticle system based on poly(amidoamine) dendrimer (generation 4)-poly(ethylene glycol)-1,2-dioleoyl-sn-glycero-3-phosphoethanolamine (G(4)-D-PEG-2K-DOPE) for co-delivery of siRNA and anti-cancer drug. The lipid modification of the nanoparticle system enhanced the binding, protection, and transfection efficiency of model siRNA (siGFP), promoting a high level of target gene suppression by siRNA. The co-delivery of doxorubicin with siRNA was efficiently achieved by dendrimer-based triblock co-polymer complex (G(4)-D-PEG-2K-DOPE) or dendrimer-micelle formulation, as measured by the cell uptake experiment. Thus, novel triblock co-polymers are consistently developed and tested. Although many studies are in the preliminary stages, triblock co-polymers appear to be promising for co-delivery of siRNA and chemotherapy agents.
Inorganic nanoparticles
Inorganic nanoparticles are reliable systems for co-delivery of siRNA and other therapeutics. They have unique physicochemical properties, including small size, large surface-area-to-volume ratio, stability in a biological environment, a surface that is easily functionalized for ligand or therapeutic molecules, and optical or magnetic properties [87]. Common inorganic nanoplatforms include gold, iron oxide, mesoporous silica, calcium phosphate nanoparticles, carbon nanotubes (CNTs), and quantum dots.
Recent studies suggest that gold nanoparticles or nanorods (AuNP) are excellent gene delivery systems, due to their stability, biocompatibility, and ability to undergo surface modifications and conjugations [87–89]. SiRNA can be directly conjugated to gold nanoparticles via electrostatic interactions or thiol bonds, or can be adsorbed to a layer of cationic polymer coated onto gold nanoparticle surfaces. However, for co-delivery purposes, the polymer coating strategy has been useful [90]. A recent example demonstrated the co-delivery of doxorubicin, ASCL1 siRNA, and octreotide (targeting ligand) using a gold nanorod targeted at neuroendocrine (NE) cancer cells [91]. The doxorubicin was conjugated to the gold nanoparticle via a pH-sensitive hydrazone linker; siRNA was complexed by poly-l-arginine coating. The targeting ligand octreotide was also attached to the poly-l-arginine polymer. Treatment of NE cells with this multi-component co-delivery system resulted in efficient targeted cell uptake, enhanced ASCL1 gene silencing, and effective cell proliferation inhibition. Hence, targeted delivery of ASLC1 siRNA and doxorubicin using Au nanorods could be a potential strategy for effective NE tumor treatment. Recently, Esteban-Fernández et al. [92] developed a gold nanowire-based system, optimized for ultrasound micromotor-propelled gene silencing, to deliver siRNA in HEK-293 and MCF-7 cell lines. The novel technology uses a rolling circle amplification (RCS) DNA strand to wrap the gold nanowire as an anchor to siRNA for delivery. This system shows promise for efficient siRNA delivery.
Mesoporous silica nanoparticle (MSN) is a widely investigated platform for drug and gene delivery applications. MSNs are chemically stable, biocompatible, and non-toxic. The physicochemical properties of mesoporous silica nanoparticles favor the development of co-delivery platforms for siRNA and other cancer therapeutics [15, 93]. A recent study reported the development of functionalized mesoporous silica nanoparticle for co-delivery of siRNA and a chemotherapeutic agent [94]. MSNs were modified with PEI-PEG and loaded with epirubicin and BCl2 siRNA for simultaneous delivery. The release of BCL2 siRNA from MSN was pH-dependent. Compared with free epirubicin, MSN carrying epirubicin, or siRNA alone, the MSN BCL2-siRNA/epirubicin co-delivery system exhibited cytotoxicity in vitro and enhanced therapeutic efficiency in vivo. The therapeutic effect was synergistic.
Another strategy for co-delivering siRNA and chemotherapeutics utilized hollow silica nanoparticles [95]. The hollow MSN achieved high drug loading and controlled release of doxorubicin. BCl2 siRNA was electrostatically adsorbed to the folic acid-PEI modified MSN containing doxorubicin for targeted co-delivery into HeLa cells. The pH-responsive cellular release of siRNA/doxorubicin may help prevent their premature release and possible side effects caused by non-specific activity. Upon targeting folic-acid-receptor-overexpressing Hela cells, the simultaneous delivery of BCL2 siRNA and doxorubicin resulted in effective BCl2 gene silencing and enhanced cytotoxicity. Using hollow MSNs may enhance the potential of anti-cancer therapy.
Recent studies show that calcium phosphate nanoparticles may be an excellent alternative for siRNA and chemotherapeutic delivery system [96–99]. These nanoparticles are non-toxic and biocompatible, and are in the generally regarded as safe for human use as per FDA. These advantages may facilitate rapid clinical translation for drug and gene delivery applications. Recent studies show the possibility of incorporating siRNA (or any nucleic acid therapeutic) and other agents into calcium phosphate nanoparticles [96, 97]. For siRNA co-delivery purpose, calcium phosphate nanoparticles may be modified to improve the physicochemical characteristics. For instance, Zhang et al. [100] encapsulated VEGF siRNA and gemcitabine into calcium phosphate nanoparticles. The calcium phosphate nanoparticles were prepared using a microemulsion technique, encapsulating VEGF siRNA and gemcitabine together. Then, the siRNA/drug-loaded calcium phosphate nanoparticle was coated with high-density lipid-PEG (DSPE-PEG). Systemic administration of this LCP nanoparticle resulted in targeted co-delivery of VEGF siRNA and doxorubicin to subcutaneous and orthotopic NSCLC tumor xenograft models. The strategy significantly enhanced apoptosis and reduced cell proliferation, leading to a dramatic reduction in tumor growth. Importantly, the in vivo toxicity of the LCP co-delivery system was minimal, while the VEGF silencing and apoptotic induction demonstrated the feasibility of this system as a successful siRNA/small molecule drug co-delivery vehicle. The same group extended the use of LCP to co-delivering a combination of cmyc-siRNA targeting the myc oncogene and gemcitabine to H460 and A549 NSCLC tumor cells [50]. These studies revealed that nucleic acid therapeutics can be efficiently combined with small molecule drugs in LCP nanoparticles for cancer therapy.
Functionalized carbon nanotubes have also emerged as a unique gene delivery system [101,102]. Carbon nanotubes (CNTs) have high mechanical strength and the ability to transport across the cell membrane without undergoing endocytosis. Due to their intrinsic hydrophobic nature, CNTs must be functionalized for drug delivery applications. Pereira et al. [103] investigated the use of ammonium-functionalized, multi-walled nanotubes (NTs)/cationic liposome hybrid to co-deliver Polo-1 kinase siRNA and doxorubicin. They tested a series of functionalized (f) MWNT-DOTAP:Chol liposome hybrid formulations for optimal in vitro transfection efficiency, gene silencing, and doxorubicin delivery. The F-MWNT-liposome nanoparticles loaded with doxorubicin and complexed with PLK1 siRNA efficiently co-delivered drug and siRNA to A549 lung cancer cells. The two therapeutic agents evoked cytotoxicity synergistically. Although recent advancements that identify newer CNT-based drug and gene delivery systems have been made, the research data are limited, perhaps indicating that challenges to therapeutic applications remain. Additional studies are required to improve the pharmacokinetics and toxicity profile of CNT-based drug delivery vectors.
Although most of these inorganic nanoparticle platforms have shown potential as co-delivery vehicles for siRNA and other anti-cancer agents, most have not been evaluated for material-related toxicity. Most of these inorganic nanoparticles were only tested in vitro. The lack of information regarding the in vivo toxicity and efficiency is considered a major issue that hinders the path forward for inorganic nanoparticles as drug delivery systems for cancer therapy. Systemic studies regarding the safety, pharmacokinetics, and mechanism of toxicities for inorganic nanoparticles are warranted.
Apart from siRNAs these nanoparticle systems such as liposomes, polymers or inorganic systems have been utilized in exploring combinations of miRNA or plasmid DNA therapeutics with chemotherapeutics or other therapeutic agents, including siRNA. Table 1 provides examples of miRNA, plasmid DNA, and combinations, some using siRNA as a co-delivery agent, have also been co-delivered with other cancer therapeutics via a variety of nanoparticles.
Table 1.
Co-delivery of miRNA, miRNA inhibitor, or plasmid DNA with other cancer therapeutic agents via nanoparticles
| Nanoparticle | miRNA/pDNA/ Inhibitor |
Co-delivered Therapeutic |
Target Cancer | Reference |
|---|---|---|---|---|
| Methoxy poly(ethylene glycol)-block-poly(2-methyl-2-carboxyl-propylenecarbonate-graft-dodecanol-graft-tetraethylene-pentamine): micelle | miR-let7B | GDC-0449-Hedgehog signaling inhibitor | Pancreatic ductal adenocarcinoma | [104] |
| GC4 svFv-liposome-polycation-hyaluronic acid (LPH) nanoparticle | miR-34a | siRNAs (c-Myc, MDM2, VEGF) | Lung metastasis of murine B16F10 melanoma | [105] |
| Chitosan-coated polylactic acid nanoparticle | Proteasome Beta subunit 5 (β5) pDNA | Cisplatin, P62 siRNA | Ovarian cancer cells | [24] |
| Mesoporous silica nanoparticle | Model single strand DNA (ssDNA) | Doxorubicin | HeLa cells | [106] |
| PAMAM modified NIR-responsive hollow gold nanoparticle | miR-21 inhibitor | Doxorubicin | Breast cancer cells and breast cancer stem cells. | [107] |
| Hyaluronic acid-coated PEI-PLGA nanoparticle | miR-542-3p | Doxorubicin | Triple negative breast cancer (MDA-MB-231) | [108] |
| Solid lipid nanoparticle | Plasmid EGFP (model DNA) | Doxorubicin | NSCLC cells/tumor: A549 | [109] |
| Cationic core-shell nanoparticle | IL-12 pDNA or BCL-2 siRNA | Paclitaxel | 4T1 mouse breast cancer model | [110] |
| Heparin–Biotin/Heparin/Calcium carbonate/Calcium Phosphate | p53 pDNA | Doxorubicin | HeLa cells | [111] |
| Calcium Phosphate polymer hybrid nanoparticles | miR-221/222 Inhibitors | Paclitaxel | Triple-negative breast cancer (MDA-MB-231) | [112] |
| Alginate/Calcium carbonate hybrid nanoparticles | p53 pDNA | Doxorubicin | HeLa cells | [113] |
Conclusions
Nanoparticles are versatile platforms used to deliver nucleic acid therapeutics and other anti-cancer drugs. The advantages of nanoparticles include improved drug stability, protection from rapid bio-clearance or bio-degradation, altered pharmacokinetics, enhanced bioavailability, promotion of the preferential accumulation of drugs in tumor sites via enhanced permeation and retention (EPR) effects, and increased therapeutic index. Over the last decade, nanoparticle systems have been successfully harnessed for the co-delivery of multiple anti-cancer agents. Co-delivery improves the therapeutic efficiency by achieving additive or synergistic effects and/or by overcoming MDR. The use of siRNA in combination with other anticancer agents is advantageous since multiple pathways or regulatory proteins involved in cancer cell growth, progression, metastasis, or drug resistance can be simultaneously manipulated to achieve an enhanced therapeutic response. Many liposomal, polymer-based, and inorganic nanoparticles have been proposed for use in co-delivery of siRNA with chemotherapeutics, small molecule inhibitors, or photodynamic agents. In addition to siRNA, other nucleic acid therapeutics, such as miRNA and pDNA, have been under investigation for co-delivery with anti-cancer agents. Many of the nanoparticle co-delivery systems using siRNA and anticancer drugs show great promise and high efficiency in treating cancers.
Although recent advancements using nanoparticle-based co-delivery have been made, challenges remain. One important issue may be the increased complexity of these systems, especially when multiple components are used in carrier fabrication. The material safety of each component should be validated before their application in drug delivery systems. Once a multicomponent system is created, multiple levels of safety evaluation must be carried out to monitor and prevent off-target effects or undesired toxicity. To quickly translate these co-delivery systems into clinical settings, the use of FDA-approved materials in their fabrication is recommended. By modifying nanoparticles with targeting ligands and molecules against specific receptors that are overexpressed in cancer cells, the efficiency of siRNA/cancer therapeutic co-delivery can be significantly enhanced. These strategies may also increase the potential of siRNA/drug combination delivery systems in overcoming drug resistance.
Acknowledgments
This work was supported in part by a grant received from the National Institutes of Health (NIH) R01 CA167516, and by funds received from the Presbyterian Health Foundation Seed Grant, Presbyterian Health Foundation Bridge Grant, Stephenson Cancer Center Seed Grant, and from the Jim and Christy Everest Endowed Chair in Cancer Developmental Therapeutics, the University of Oklahoma Health Sciences Center. The authors thank Ms. Kathy Kyler at the office of Vice President for Research, OUHSC, for editorial assistance. Rajagopal Ramesh is an Oklahoma TSET Research Scholar and holds the Jim and Christy Everest Endowed Chair in Cancer Developmental Therapeutics.
Footnotes
Disclosure Statement
The authors declare no competing financial interests.
References
- 1.Yap T, Omlin A, de Bono JS. Development of Therapeutic Combinations Targeting Major Cancer Signaling Pathways. J Clin Oncol. 2013;31:1592–1605. doi: 10.1200/JCO.2011.37.6418. [DOI] [PubMed] [Google Scholar]
- 2.Tong R, Kohane DS. New Strategies in Cancer Nanomedicine. Ann Rev Pharmacol Toxicol. 2016;56:41–57. doi: 10.1146/annurev-pharmtox-010715-103456. [DOI] [PubMed] [Google Scholar]
- 3.Mansoori B, Shotorbani SS, Baradaran B. RNA Interference and its Role in Cancer Therapy. Adv Pharm Bull. 2014;4:313–321. doi: 10.5681/apb.2014.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Golan T, Khvalevsky EZ, Hubert A, et al. RNAi therapy targeting KRAS in combination with chemotherapy for locally advanced pancreatic cancer patients. Oncotarget. 2015;6:24560–24570. doi: 10.18632/oncotarget.4183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ganesh S, Iyer AK, Weiler J, et al. Combination of siRNA-directed Gene Silencing With Cisplatin Reverses Drug Resistance in Human Non-small Cell Lung Cancer. Mol Ther. Nucleic Acids. 2013;2:e110. doi: 10.1038/mtna.2013.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanasty R, Dorkin JR, Vegas A, et al. Delivery materials for siRNA therapeutics. Nat Mater. 2013;12:967–977. doi: 10.1038/nmat3765. [DOI] [PubMed] [Google Scholar]
- 7.Vorhies JS, Nemunaitis J. Nonviral delivery vehicles for use in short hairpin RNA-based cancer therapies. Expert Rev Anticancer Ther. 2007;7:373–382. doi: 10.1586/14737140.7.3.373. [DOI] [PubMed] [Google Scholar]
- 8.Thomas CE, Ehrhardt A, Kay MA. Progress and problems with the use of viral vectors for gene therapy. Nat Rev Genet. 2003;4:346–358. doi: 10.1038/nrg1066. [DOI] [PubMed] [Google Scholar]
- 9.Yin H, Kanasty RL, Eltoukhy AA, et al. Non-viral vectors for gene-based therapy. Nat Rev Genetics. 2014;15:541–555. doi: 10.1038/nrg3763. [DOI] [PubMed] [Google Scholar]
- 10.Young SW, Stenzel M, Yang JL. Nanoparticle-siRNA: A potential cancer therapy? Crit Rev Oncol Hematol. 2016;98:159–169. doi: 10.1016/j.critrevonc.2015.10.015. [DOI] [PubMed] [Google Scholar]
- 11.Williford JM, Wu J, Ren Y, et al. Recent advances in nanoparticle-mediated siRNA delivery. Annu Rev Biomed Eng. 2014;16:347–370. doi: 10.1146/annurev-bioeng-071813-105119. [DOI] [PubMed] [Google Scholar]
- 12.Whitehead KA, Langer R, Anderson DG. Knocking down barriers: advances in siRNA delivery. Nat Rev Drug Discov. 2009;8:129–138. doi: 10.1038/nrd2742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Esmaeili MA. Combination of siRNA-directed gene silencing with epigallocatechin-3-gallate (EGCG) reverses drug resistance in human breast cancer cells. J Chem Biol. 2015;9:41–52. doi: 10.1007/s12154-015-0144-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dong H, Yao L, Bi W, et al. Combination of survivin siRNA with neoadjuvant chemotherapy enhances apoptosis and reverses drug resistance in breast cancer MCF-7 cells. J Can Res Ther. 2015;11:717–722. doi: 10.4103/0973-1482.147764. [DOI] [PubMed] [Google Scholar]
- 15.Meng H, Mai WX, Zhang H, et al. Codelivery of an optimal drug/siRNA combination using mesoporous silica nanoparticles to overcome drug resistance in breast cancer in vitro and in vivo. ACS Nano. 2013;7:994–1005. doi: 10.1021/nn3044066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu Y, Zhang Y, Zhang W, et al. Reversing of multidrug resistance breast cancer by co-delivery of P-gp siRNA and doxorubicin via folic acid-modified core-shell nanomicelles. Colloids Surf B Biointerfaces. 2016;138:60–69. doi: 10.1016/j.colsurfb.2015.11.041. [DOI] [PubMed] [Google Scholar]
- 17.Komarova NL, Boland CR. Cancer: Calculated treatment. Nature. 2013;499:291–292. doi: 10.1038/499291a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiao B, Ma L, Merlin D. Nanoparticle-mediated co-delivery of chemotherapeutic agent and siRNA for combination cancer therapy. Expert Opin Drug Deliv. 2016;6:1–9. doi: 10.1080/17425247.2016.1205583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saraswathy M, Gong S. Recent developments in the co-delivery of siRNA and small molecule anticancer drugs for cancer treatment. Mater Today. 2014;17:298–306. [Google Scholar]
- 20.Marusyk A, Polyak K. Tumor heterogeneity: causes and consequences. Biochim Biophys Acta. 2010;1805:105. doi: 10.1016/j.bbcan.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gillet JP, Gottesman MM. Mechanisms of multidrug resistance in cancer. Methods Mol Biol. 2010;596:47–76. doi: 10.1007/978-1-60761-416-6_4. [DOI] [PubMed] [Google Scholar]
- 22.Krishna R, Mayer LD. Multidrug resistance (MDR) in cancer. Mechanisms, reversal using modulators of MDR and the role of MDR modulators in influencing the pharmacokinetics of anticancer drugs. Eur J Pharm Sci. 2000;11:265–283. doi: 10.1016/s0928-0987(00)00114-7. [DOI] [PubMed] [Google Scholar]
- 23.Pérez-Tomás R. Multidrug resistance: retrospect and prospects in anti-cancer drug treatment. Curr Med Chem. 2006;13:1859–1876. doi: 10.2174/092986706777585077. [DOI] [PubMed] [Google Scholar]
- 24.Babu A, Wang Q, Muralidharan R, et al. Chitosan coated polylactic acid nanoparticle-mediated combinatorial delivery of cisplatin and siRNA/Plasmid DNA chemosensitizes cisplatin-resistant human ovarian cancer cells. Mol Pharm. 2014;11:2720–2733. doi: 10.1021/mp500259e. [DOI] [PubMed] [Google Scholar]
- 25.Yang H, Ding R, Tong Z, et al. siRNA Targeting of MDR1 Reverses Multidrug Resistance in a Nude Mouse Model of Doxorubicin-resistant Human Hepatocellular Carcinoma. Anticancer Res. 2016;36:2675–2682. [PubMed] [Google Scholar]
- 26.Nascimento AV, Singh A, Bousbaa H, et al. Overcoming cisplatin resistance in non-small cell lung cancer with Mad2 silencing siRNA delivered systemically using EGFR-targeted chitosan nanoparticles. Acta Biomater. 2016:S1742–7061. 30518–30519. doi: 10.1016/j.actbio.2016.09.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Agostinis P, Berg K, Cengel KA, et al. Photodynamic therapy of cancer: an update. CA Cancer J Clin. 2011;61:250–281. doi: 10.3322/caac.20114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen WH, Lecaros RL, Tseng YC, et al. Nanoparticle delivery of HIF1α siRNA combined with photodynamic therapy as a potential treatment strategy for head-and-neck cancer. Cancer Lett. 2015;359:65–74. doi: 10.1016/j.canlet.2014.12.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang X, Liu K, Yang G, et al. Near-infrared light triggered photodynamic therapy in combination with gene therapy using upconversion nanoparticles for effective cancer cell killing. Nanoscale. 2014;6:9198–9205. doi: 10.1039/c4nr02495h. [DOI] [PubMed] [Google Scholar]
- 30.Xue LY, Chiu SM, Oleinick NL. Atg7 deficiency increases resistance of MCF-7 human breast cancer cells to photodynamic therapy. Autophagy. 2010;6:248–255. doi: 10.4161/auto.6.2.11077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim J, Lim H, Kim S, et al. Effects of HSP27 downregulation on PDT resistance through PDT-induced autophagy in head and neck cancer cells. Oncol Rep. 2016;35:2237–2245. doi: 10.3892/or.2016.4597. [DOI] [PubMed] [Google Scholar]
- 32.Mao CP, Hung CF, Wu TC, et al. Immunotherapeutic strategies employing RNA interference technology for the control of cancers. J Biomed Sci. 2007;14:15–29. doi: 10.1007/s11373-006-9131-5. [DOI] [PubMed] [Google Scholar]
- 33.Ghafouri-Fard S, Ghafouri-Fard S. siRNA and cancer immunotherapy. Immunotherapy. 2012;4:907–917. doi: 10.2217/imt.12.87. [DOI] [PubMed] [Google Scholar]
- 34.Naidu MD, Mason JM, Pica RV, et al. Radiation resistance in glioma cells determined by DNA damage repair activity of Ape1/Ref-1. J Radiat Res. 2010;51:393–404. doi: 10.1269/jrr.09077. [DOI] [PubMed] [Google Scholar]
- 35.Higgins GS, Prevo R, Lee YF, et al. A siRNA screen of genes involved in DNA repair identifies tumour specific radiosensitisation by POLQ Knockdown. Cancer Res. 2010;70:2984–2993. doi: 10.1158/0008-5472.CAN-09-4040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mehta M, Basalingappa K, Griffith JN, et al. HuR silencing elicits oxidative stress and DNA damage and sensitizes human triple-negative breast cancer cells to radiotherapy. Oncotarget. 2016;7:64820–64835. doi: 10.18632/oncotarget.11706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jin H, Gao S, Guo H, et al. Re-sensitization of radiation resistant colorectal cancer cells to radiation through inhibition of AMPK pathway. Oncol Lett. 2016;11:3197–3201. doi: 10.3892/ol.2016.4339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gong X, Li X, Zhou C. 81P - Radiation resistance induced immunity evasion by evoking PD-L1 expression. J Thoracic Oncol (suppl 4) 2016;11:S57–S166. [Google Scholar]
- 39.Retif P, Pinel S, Toussaint M, et al. Nanoparticles for Radiation Therapy Enhancement: the Key Parameters. Theranostics. 2015;5:1030–1044. doi: 10.7150/thno.11642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dexter DL, Leith JT. Tumor heterogeneity and drug resistance. J Clin Oncol. 1986;4:244–257. doi: 10.1200/JCO.1986.4.2.244. [DOI] [PubMed] [Google Scholar]
- 41.Tekedereli I, Alpay SN, Akar U, et al. Therapeutic Silencing of Bcl-2 by Systemically Administered siRNA Nanotherapeutics Inhibits Tumor Growth by Autophagy and Apoptosis and Enhances the Efficacy of Chemotherapy in Orthotopic Xenograft Models of ER (−) and ER (+) Breast Cancer. Mol Ther Nucleic Acids. 2013;2:e121. doi: 10.1038/mtna.2013.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shen Y, Wang J, Li Y, et al. Co-delivery of siRNA and paclitaxel into cancer cells by hyaluronic acid modified redox-sensitive disulfide-crosslinked PLGA–PEI nanoparticles. RSC Adv. 2015;5:46464–46479. [Google Scholar]
- 43.Creixell M, Peppas NA. Co-delivery of siRNA and therapeutic agents using nanocarriers to overcome cancer resistance. Nano Today. 2012;7:367–379. doi: 10.1016/j.nantod.2012.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Godsey ME, Suryaprakash S, Leong KW. Materials innovation for co-delivery of diverse therapeutic cargos. RSC Adv. 2013;3:24794–24811. doi: 10.1039/C3RA43094D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kang L, Gao Z, Huang W, et al. Nanocarrier-mediated co-delivery of chemotherapeutic drugs and gene agents for cancer treatment. Acta Pharmaceutica Sinica B. 2015;5:169–175. doi: 10.1016/j.apsb.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bozzuto G, Molinari A. Liposomes as nanomedical devices. Int J Nanomedicine. 2015;10:975–999. doi: 10.2147/IJN.S68861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shim G, Kim MG, Park JY, et al. Application of cationic liposomes for delivery of nucleic acids. A J Pharm Sci. 2013;8:72–80. [Google Scholar]
- 48.Bender HR, Kane S, Zabel MD. Delivery of Therapeutic siRNA to the CNS Using Cationic and Anionic Liposomes. J Vis Exp. 2016;113 doi: 10.3791/54106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ko YT, Bickel U. Liposome-Encapsulated Polyethylenimine/Oligonucleotide Polyplexes Prepared by Reverse-Phase Evaporation Technique. AAPS PharmSciTech. 2012;13:373–378. doi: 10.1208/s12249-012-9757-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang Y, Peng L, 1 Mumper RJ, et al. Combinational delivery of c-Myc siRNA and nucleoside analogues in a single, synthetic nanocarrier for targeted cancer therapy. Biomaterials. 2013;34:8459–8468. doi: 10.1016/j.biomaterials.2013.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Qu MH, Zeng RF, Fang S, et al. Liposome-based co-delivery of siRNA and docetaxel for the synergistic treatment of lung cancer. Int J Pharm. 2014;474:112–122. doi: 10.1016/j.ijpharm.2014.08.019. [DOI] [PubMed] [Google Scholar]
- 52.Peng Z, Wang C, Fang E, et al. Co-delivery of doxorubicin and SATB1 shRNA by thermosensitive magnetic cationic liposomes for gastric cancer therapy. Plos One. 2014 doi: 10.1371/journal.pone.0092924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yao Y, Su Z, Liang Y, et al. pH-Sensitive carboxymethyl chitosan-modified cationic liposomes for sorafenib and siRNA co-delivery. Int J Nanomedicine. 2015;10:6185–6197. doi: 10.2147/IJN.S90524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Oh HR, Jo HY, Park JS, et al. Galactosylated Liposomes for targeted co-delivery of doxorubicin/vimentin siRNA to hepatocellular carcinoma. Nanomaterials. 2016;6:141. doi: 10.3390/nano6080141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yang T, Li B, Qi S, et al. Co-delivery of doxorubicin and Bmi1 siRNA by folate receptor targeted liposomes exhibits enhanced anti-tumor effects in vitro and in vivo. Theranostics. 2014;4:1096–1011. doi: 10.7150/thno.9423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yang ZZ, Li JQ, Wang ZZ, Dong DW, et al. Tumor-targeting dual peptides-modified cationic liposomes for delivery of siRNA and docetaxel to gliomas. Biomaterials. 2014;35:5226–5239. doi: 10.1016/j.biomaterials.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 57.Chen WH, Lecaros RLG, Tseng YC, et al. Nanoparticle delivery of HIF1α siRNA combined with photodynamic therapy as a potential treatment strategy for head-and-neck cancer. Cancer Letters. 2015;359:65–74. doi: 10.1016/j.canlet.2014.12.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lecaros RLG, Huang L, Lee TC, et al. Nanoparticle delivered VEGF-A siRNA enhances photodynamic therapy for head and neck cancer treatment. Mol Ther. 2016;24:106–116. doi: 10.1038/mt.2015.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kang SH, Cho HJ, Shim G, et al. Cationic liposomal co-delivery of small interfering RNA and a MEK inhibitor for enhanced anticancer efficacy. Pharm Res. 2011;28:3069–3078. doi: 10.1007/s11095-011-0569-4. [DOI] [PubMed] [Google Scholar]
- 60.Saad M, Garbuzenko OB, Minko T. Co-delivery of siRNA and an anticancer drug for treatment of multidrug-resistant cancer. Nanomedicine (Lond) 2008;3:761–776. doi: 10.2217/17435889.3.6.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ha J, Cho SK, Park ES, et al. Enhanced Stability of Hydroxyapatite-coated Liposomes for Ultrasound-triggered Drug Release. Bull Korean Chem. Soc. 2015;36:83–87. [Google Scholar]
- 62.Sévin DC, Sauer U. Ubiquinone accumulation improves osmotic-stress tolerance in Escherichia coli. Nat Chem Biol. 2014;10:266–272. doi: 10.1038/nchembio.1437. [DOI] [PubMed] [Google Scholar]
- 63.Hernández AV, Eriksson EK, Edwards K. Ubiquinone-10 alters mechanical properties and increases stability of phospholipid membranes. Biochim Biophys Acta. 2015;1848(10Pt A):2233–2243. doi: 10.1016/j.bbamem.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 64.Kang SN, Honga S-S, Kima S-Y, et al. Enhancement of liposomal stability and cellular drug uptake by incorporating tributyrin into celecoxib-loaded liposomes. Asian J Pharm Sci. 2013;8:128–133. [Google Scholar]
- 65.Pawar S, Shevalkar G, Vavia P. Glucosamine-anchored doxorubicin-loaded targeted nano-niosomes: pharmacokinetic, toxicity and pharmacodynamic evaluation. J Drug Target. 2016;8:730–743. doi: 10.3109/1061186X.2016.1154560. [DOI] [PubMed] [Google Scholar]
- 66.Sharma V, Anandhakumar S, Sasidharan M. Self-degrading niosomes for encapsulation of hydrophilic and hydrophobic drugs: An efficient carrier for cancer multi-drug delivery. Mater Sci Eng. 2015;56:393–400. doi: 10.1016/j.msec.2015.06.049. [DOI] [PubMed] [Google Scholar]
- 67.Namdeo A1, Jain NK. Niosomal delivery of 5-fluorouracil. J Microencapsul. 1999;16:731–40. doi: 10.1080/026520499288672. [DOI] [PubMed] [Google Scholar]
- 68.Uchegbu IF, Double JA, Turton JA, et al. Distribution, metabolism and tumoricidal activity of doxorubicin administered in sorbitan monostearate (Span 60) niosomes in the mouse. Pharm Res. 1995;12:1019–1024. doi: 10.1023/a:1016210515134. [DOI] [PubMed] [Google Scholar]
- 69.Uchegbu IF, Double JA, Kelland LR, et al. The activity of doxorubicin niosomes against an ovarian cancer cell line and three in vivo mouse tumour models. J Drug Targ. 1996;3:399–409. doi: 10.3109/10611869608996831. [DOI] [PubMed] [Google Scholar]
- 70.Huang Y, Chen J, Chen X, et al. PEGylated synthetic surfactant vesicles (Niosomes): novel carriers for oligonucleotides. J Mater Sci: Mater Med. 2008;19:607–614. doi: 10.1007/s10856-007-3193-4. [DOI] [PubMed] [Google Scholar]
- 71.Tavano L, Muzzalupo R, Mauro L, et al. Transferrin-conjugated pluronic niosomes as a new drug delivery system for anticancer therapy. Langmuir. 2013;29:12638–12646. doi: 10.1021/la4021383. [DOI] [PubMed] [Google Scholar]
- 72.Grijalvo S, Alagia A, Puras G, et al. Cationic vesicles based on non-ionic surfactant and synthetic aminolipids mediate delivery of antisense oligonucleotides into mammalian cells. Colloids Surf B Biointerfaces. 2014;119:30–37. doi: 10.1016/j.colsurfb.2014.04.016. [DOI] [PubMed] [Google Scholar]
- 73.Rajput S, Puvvada N, Kumar BN, et al. Overcoming Akt Induced Therapeutic Resistance in Breast Cancer through siRNA and Thymoquinone Encapsulated Multilamellar Gold Niosomes. Mol Pharm. 2015;12:4214–4225. doi: 10.1021/acs.molpharmaceut.5b00692. [DOI] [PubMed] [Google Scholar]
- 74.Tamura A, Nagasak Y. Smart siRNA delivery systems based on polymeric nanoassemblies and nanoparticles. Nanomedicine. 2010;5:1089–1102. doi: 10.2217/nnm.10.76. [DOI] [PubMed] [Google Scholar]
- 75.Shroff K, Vidyasagar A. Polymer nanoparticles: newer strategies towards targeted cancer therapy. J Phys Chem Biophys. 2013;3:125. [Google Scholar]
- 76.Zhang CG, Zhu WJ, Liu Y, et al. Novel polymer micelle mediated co-delivery of doxorubicin and P-glycoprotein siRNA for reversal of multidrug resistance and synergistic tumor therapy. Sci Rep. 2016;6:23859. doi: 10.1038/srep23859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hao S, Yan Y, Ren X, et al. Candesartan-graft-polyethyleneimine cationic micelles for effective co-delivery of drug and gene in anti-angiogenic lung cancer therapy. Biotechnol Bioprocess Eng. 2015;20:550–560. [Google Scholar]
- 78.Fu Y, Kao WJ. Drug release kinetics and transport mechanisms of non-degradable and degradable polymeric delivery systems. Expert Opin Drug Deliv. 2010;7:429–444. doi: 10.1517/17425241003602259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Su WP, Cheng FY, Shieh DB, et al. PLGA nanoparticles codeliver paclitaxel and Stat3 siRNA to overcome cellular resistance in lung cancer cells. Int J Nanomedicine. 2012;7:4269–4283. doi: 10.2147/IJN.S33666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Patil YB, Swaminathan SK, Sadhukha T, et al. The use of nanoparticle-mediated targeted gene silencing and drug delivery to overcome tumor drug resistance. Biomaterials. 2010;31:358–365. doi: 10.1016/j.biomaterials.2009.09.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wei W, Lv PP, Chen XM. Codelivery of mTERT siRNA and paclitaxel by chitosan-based nanoparticles promoted synergistic tumor suppression. Biomaterials. 2013;34:3912–923. doi: 10.1016/j.biomaterials.2013.02.030. [DOI] [PubMed] [Google Scholar]
- 82.Alinejad V, Somi MH, Baradaran B, et al. Co-delivery of IL17RB siRNA and doxorubicin by chitosan-based nanoparticles for enhanced anticancer efficacy in breast cancer cells. Biomed Pharmacother. 2016;83:229–224. doi: 10.1016/j.biopha.2016.06.037. [DOI] [PubMed] [Google Scholar]
- 83.Xu C, Tian H, Sun H, et al. A pH sensitive co-delivery system of siRNA and doxorubicin for pulmonary administration to B16F10 metastatic lung cancer. RSC Adv. 2015;5:103380–103385. [Google Scholar]
- 84.Zhu C, Jung S, Luo S, et al. Co-delivery of siRNA and paclitaxel into cancer cells by biodegradable cationic micelles based on PDMAEMA-PCL-PDMAEMA triblock copolymers. Biomaterials. 2010;31:2408–2416. doi: 10.1016/j.biomaterials.2009.11.077. [DOI] [PubMed] [Google Scholar]
- 85.Xu M, Qian J, Suo A, et al. Co-delivery of doxorubicin and P-glycoprotein siRNA by multifunctional triblock copolymers for enhanced anticancer efficacy in breast cancer cells. J Mater Chem B. 2015;3:2215–2228. doi: 10.1039/c5tb00031a. [DOI] [PubMed] [Google Scholar]
- 86.Biswas S, Deshpande PP, Navarro G, et al. Lipid modified triblock PAMAM-based nanocarriers for siRNA drug co-delivery. Biomaterials. 2013;34:1289–1301. doi: 10.1016/j.biomaterials.2012.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jiang Y, Huo S, Hardie J, et al. Progress and perspective of inorganic nanoparticle-based siRNA delivery systems. Expert Opin Drug Deliv. 2016;13:547–559. doi: 10.1517/17425247.2016.1134486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bishop CJ, Tzeng SY, Green JJ. Degradable polymer-coated gold nanoparticles for co-delivery of DNA and siRNA. Acta Biomater. 2015;11:393–403. doi: 10.1016/j.actbio.2014.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ding Y, Jiang Z, Saha K, et al. Gold Nanoparticles for Nucleic Acid Delivery. Mol Ther. 2014;22:1075–1083. doi: 10.1038/mt.2014.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Guo S, Huang Y, Jiang Q, et al. Enhanced Gene Delivery and siRNA Silencing by Gold Nanoparticles Coated with Charge-Reversal Polyelectrolyte. ACS Nano. 2010;4:5505–5511. doi: 10.1021/nn101638u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Xiao Y, Jaskula-Sztul R, Javadi A, et al. Co-delivery of doxorubicin and siRNA using octreotide-conjugated gold nanorods for targeted neuroendocrine cancer therapy. Nanoscale. 2012;4:7185–7193. doi: 10.1039/c2nr31853a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Esteban-Fernández AB, Angell C, Soto F, et al. Acoustically propelled nanomotors for intracellular siRNA delivery. ACS Nano. 2016;10:4997–5005. doi: 10.1021/acsnano.6b01415. [DOI] [PubMed] [Google Scholar]
- 93.Meng H, Liong M, Xia T, et al. Engineered design of mesoporous silica nanoparticles to deliver doxorubicin and P-glycoprotein siRNA to overcome drug resistance in a cancer cell line. ACS Nano. 2010;4:4539–4550. doi: 10.1021/nn100690m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hanafi-Bojd MY, Jaafari MR, Ramezanian N, et al. Co-delivery of Epirubicin and siRNA using functionalized mesoporous silica nanoparticles enhances in vitro and in vivo drug efficacy. Curr Drug Deliv. 2015;13:1176–1182. doi: 10.2174/1567201813666151231094056. [DOI] [PubMed] [Google Scholar]
- 95.Ma X, Zhao Y, Ng KW, et al. Integrated hollow mesoporous silica nanoparticles for target drug/siRNA co-delivery. Chem Eur J. 2013;19:15593–15603. doi: 10.1002/chem.201302736. [DOI] [PubMed] [Google Scholar]
- 96.Lee MS, Lee JE, Byun E, et al. Target-specific delivery of siRNA by stabilized calcium phosphate nanoparticles using dopa-hyaluronic acid conjugate. J Control Release. 2014;192:122–130. doi: 10.1016/j.jconrel.2014.06.049. [DOI] [PubMed] [Google Scholar]
- 97.Lee K, Oh MH, Lee MS, et al. Stabilized calcium phosphate nano-aggregates using a dopa-chitosan conjugate for gene delivery. Int J Pharm. 2013;445:196–202. doi: 10.1016/j.ijpharm.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 98.Cheng X, Kuhn L. Chemotherapy drug delivery from calcium phosphate nanoparticles. Int J Nanomedicine. 2007;2:667–674. [PMC free article] [PubMed] [Google Scholar]
- 99.Jun W, Lin L, Yurong C, et al. Recent advances of calcium phosphate nanoparticles for controlled drug delivery. Mini Rev Med Chem. 2013;13:1501–1507. doi: 10.2174/13895575113139990059. [DOI] [PubMed] [Google Scholar]
- 100.Zhang Y, Schwerbrock NM, Rogers AB, et al. Codelivery of VEGF siRNA and gemcitabine monophosphate in a single nanoparticle formulation for effective treatment of NSCLC. Mol Ther. 2013;21:1559–1569. doi: 10.1038/mt.2013.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Varkouhi AK, Foillard S, Lammers T, et al. SiRNA delivery with functionalized carbon nanotubes. Int J Pharm. 2011;416:419–425. doi: 10.1016/j.ijpharm.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 102.Siu KS, Zhang Y, Zheng X, et al. Non-Covalently Functionalized of Single-Walled Carbon Nanotubes by DSPE-PEG-PEI for SiRNA Delivery. Methods Mol Biol. 2016;1364:151–63. doi: 10.1007/978-1-4939-3112-5_13. [DOI] [PubMed] [Google Scholar]
- 103.Pereira S, Lee J, Rubio N, et al. Cationic liposome- multi-walled carbon nanotubes Hybrids for dual siPLK1 and doxorubicin delivery in vitro. Pharm Res. 2015;32:3293–3308. doi: 10.1007/s11095-015-1707-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kumar V, Mondal G, Slavik P, et al. Codelivery of small molecule hedgehog inhibitor and miRNA for treating pancreatic cancer. Mol Pharm. 2015;12:1289–1298. doi: 10.1021/mp500847s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Chen Y, Zhu X, Zhang X, et al. Nanoparticles modified with tumor-targeting scFv deliver siRNA and miRNA for cancer therapy. Mol Ther. 2010;18:1650–1656. doi: 10.1038/mt.2010.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ma X, Nguyen KT, Borah P, et al. Chung Yen Ang, Yanli Zha. Functional silica nanoparticles for redox-triggered drug/ssDNA co-delivery. Adv Health Care Mater. 2012;1:690–697. doi: 10.1002/adhm.201200123. [DOI] [PubMed] [Google Scholar]
- 107.Ren Y, Wang R, Gao L, et al. Sequential co-delivery of miR-21 inhibitor followed by burst release doxorubicin using NIR-responsive hollow gold nanoparticle to enhance anticancer efficacy. J Control Release. 2016;28:74–86. doi: 10.1016/j.jconrel.2016.03.008. [DOI] [PubMed] [Google Scholar]
- 108.Wang S, Zhang J, Wang Y, et al. Hyaluronic acid-coated PEI-PLGA nanoparticles mediated co-delivery of doxorubicin and miR-542-3p for triple negative breast cancer therapy. Nanomedicine. 2016;12:411–420. doi: 10.1016/j.nano.2015.09.014. [DOI] [PubMed] [Google Scholar]
- 109.Han Y, Zhang P, Chen Y, et al. Co-delivery of plasmid DNA and doxorubicin by solid lipid nanoparticles for lung cancer therapy. Int J Mol Med. 2014;34:191–196. doi: 10.3892/ijmm.2014.1770. [DOI] [PubMed] [Google Scholar]
- 110.Wang Y, Gao S, Ye WH, et al. Co-delivery of drugs and DNA from cationic core–shell nanoparticles self-assembled from a biodegradable copolymer. Nat Mater. 2006;5:791–796. doi: 10.1038/nmat1737. [DOI] [PubMed] [Google Scholar]
- 111.Liang P, Wang CQ, Chen H, et al. Multi-functional heparin–biotin/heparin/calcium carbonate/calcium phosphate nanoparticles for targeted co-delivery of gene and drug. Polym Int. 2104;64 doi: 10.1002/pi.4824. [DOI] [Google Scholar]
- 112.Zhou Z, Kennella C, Lee JY, et al. Calcium phosphate-polymer hybrid nanoparticles for enhanced triple negative breast cancer treatment via co-delivery of paclitaxel and miR-221/222 inhibitors. Nanomedicine. 2017;2:403–410. doi: 10.1016/j.nano.2016.07.016. [DOI] [PubMed] [Google Scholar]
- 113.Zhao D, Liu CJ, Zhuo RX, et al. Alginate/CaCO3 hybrid nanoparticles for efficient codelivery of antitumor gene and drug. Mol Pharm. 2012;9:2887–2893. doi: 10.1021/mp3002123. [DOI] [PubMed] [Google Scholar]