Abstract
Objective
To examine the impact from Family Foundations, a transition-to-parenting intervention, on parent and child outcomes 2 years after birth.
Background
Couples transitioning to parenthood face many stressors and challenges that are not typically addressed through commonly available childbirth preparatory classes. The Family Foundations program was designed for couples expecting their first child and addresses family stressors related to coparenting, parenting, and mental health.
Method
The recruited sample of 399 couples expecting their first child were randomly assigned to intervention or control conditions. Data were obtained through home observation and parent surveys before and after intervention.
Results
Intent-to-treat analyses indicated effects on several targeted domains including coparenting, parenting, and relationship quality, as well as on child sleep habits and internalizing behavior problems at 2 years of age. Effects for several outcomes were larger for those couples at greater risk based on pretest observed negative dyadic communication styles.
Conclusion
Longer term impact found here on parent and child outcomes provides new evidence of the effectiveness of this program for first-time parents.
Implications
Programs directed toward broader issues related to aspects of coparenting, parenting, and mental health have the potential to have longer term positive impact on the couples and the developing child.
Keywords: coparenting, program development & evaluation, transition to parenthood, child development
The transition to parenthood is a challenging and stressful period for many couples. Interventions and other resources to help parents navigate these challenges have the potential to provide great benefit (Belsky, 1984; Dennis & Dowswell, 2013; Morrill, Hines, Mahmood, & Cordova, 2010; Sanders & Morawska, 2006). For instance, in two-parent families, improved ability of the coparents to minimize daily stress, negative affect, and conflict in their relationship can provide a more stable and enriching context for their developing child (Margolin, Gordis, & John, 2001). However, few studies have demonstrated that couple-focused programs can generate sustained, positive results for new parents (Pinquart & Teubert, 2010). Moreover, this limited evidence on long-term effects precludes the study of how couple-focused programs may be more effective for some families and less effective for others.
The preventative intervention Family Foundations (FF)—a couple-focused program addressing the transition to parenthood—has demonstrated long-term positive effects for improving parent, couple, and child outcomes (Feinberg et al., 2016; Feinberg, Jones, Kan, & Goslin, 2010; Feinberg, Jones, Roettger, Solmeyer, & Hostetler, 2014). The program, which was created to support new parents as they manage the transition to parenthood, is delivered through a brief series of classes designed for the general population of couples expecting their first child. The program was designed to enhance coparenting relationships, which in turn bolsters both parent mental health and healthy parenting practices. Multiple evaluations of the original trial demonstrated intervention effects in all targeted domains: coparenting, parent mental health, parenting, and child behavior and adjustment (Feinberg et al., 2010, 2014; Feinberg & Kan, 2008; Feinberg, Kan, & Goslin, 2009). Sustained impacts on child outcomes from birth to middle childhood are especially salient given the potential developmental implications for lifelong benefits: Evaluation of the first trial of the program revealed long-term impact on child developmental outcomes at 3 years of age (Feinberg et al., 2010) that were also still evident at early school-age (Feinberg et al., 2014). Moreover, the program structure and content has proven flexible as we have adapted the original, group-based, universal FF program for delivery by different modalities to support specific groups; versions of the program have been developed for teens in either health settings or high school, for military families via an online platform, for high-risk families delivered through home visitors, and parents with a young child recently diagnosed with autism, and the effectiveness of these versions are currently being tested.
Here, we examine outcomes of the second trial, using observed family interaction data and parent reports of self- and child adjustment at 2 years postpartum. This second trial is needed to investigate whether longer term impact demonstrated through evaluation of the original intervention is replicated with different participants comprising a larger sample (Ioannidis, 2005). This study of longer term impact is also important given a slight change in intervention delivery for this second trial. Specifically, childbirth education material is now incorporated into the prenatal FF classes to reduce the need for parents to enroll in more than one prenatal preparation program (to accommodate this material, some prenatal material from the original intervention was condensed for the revised implementation).
In two earlier papers examining short-term outcomes of the second trial, we reported positive impact that replicated findings from the first trial: improved birth outcomes for women at risk and enhanced parent, child, and family relationship adjustment at 10 months postpartum (Feinberg, Jones, Hostetler, et al., 2016; Feinberg, Jones, Roettger, et al., 2016). Therefore, the first question we address in this article is whether FF yields sustained, long-term impact in this second, larger trial as in the first. At 2 years postpartum, we expected to see observable enhanced coparenting and parenting skills among intervention participants in contrast to the control group. It is also important to assess whether intervention impact on child adjustment outcomes evident in the first trial is replicated with the second trial. The second question we address in this study is whether the program is more or less effective for some families based on initial couple relationship risk during pregnancy. Postnatal, coparental functioning is linked to prenatal relationship quality (Le, McDaniel, Leavitt, & Feinberg, 2016); thus, intervention effects may differ across families with varying levels of risk. In what follows, we provide a brief description of the program’s background, review key findings from prior evaluations, and introduce the outcomes and analytic strategy used to assess long-term intervention impact from the second trial.
Family Foundations: First Trial
FF was designed to be delivered efficiently within a health care or community setting and is carried out through a series of classes held before and after birth. Instruction in the classes focuses on coparental conflict resolution, problem-solving, and communication and mutual-support strategies around raising an infant. Prior investigations of program effects have included extensive reviews of the literature demonstrating the need for FF and the basis for what key elements were incorporated into program curriculum (Feinberg, 2002, 2003; Feinberg et al., 2009). Programs aimed at coparenting skills and relationship issues often require more time and commitment than most new parents have available (Schulz, Cowan, & Cowan, 2006; Wood, Moore, Clarkwest, Killewald, & Monahan, 2012). Thus, the FF program was designed to provide sufficient information but still be practical with regard to working parents’ time constraints.
On the basis of a review of the literature and the development of theoretical models regarding both the components of coparenting and the role of coparenting in influencing child well-being, the FF program aims to enhance the coparental relationship and, in turn, improve parents’ stress management, mental health, and parenting quality (Feinberg & Kan, 2008). These factors are especially important during the infancy and early childhood period, as the transition to parenthood is linked to increased conflict and difficulties in couple relationships, lack of sleep and irritability, and depression (Cowan & Cowan, 1995; Shapiro, Gottman, & Carrere, 2000). Thus, some scholars suggest that establishing healthy coparenting patterns early can reduce conflict in the couple relationship and increase mutual support with positive effects for each parent’s mental health (McHale, Kuersten-Hogan, Lauretti, & Rasmussen, 2000; Van Egeren, 2004). Although more than 30 years of research has shown that couple conflict is linked to disrupted parenting and child adjustment difficulties (Buehler & Gerard, 2002; Kaczynski, Lindahl, Malik, & Laurenceau, 2006; Kelly, 2000), researchers have since discovered that coparenting conflict is more detrimental to child adjustment than general couple conflict (Abidin & Brunner, 1995; Feinberg, Kan, & Hetherington, 2007; Frosch, Mangelsdorf, & McHale, 2000).
The importance of coparenting quality both for parents’ and children’s adjustment may relate to its central function in nuclear families. The parental couple was viewed by influential family therapists as the joint “executive” team that set the tone for and managed family relationships (Minuchin, 1985). During the transition to parenthood, new parents are required to take on a substantial and often overwhelming new responsibility for the 24-hour care of their newborn. Care for this vulnerable, prized, and often unpredictable new family member requires new skills and the development of new psychological resources (e.g., patience in the face of insistent crying). Uncertainty and feelings of inadequacy arise frequently (Feinberg, 2003); in this context, the coparent is the figure available to provide either support or critical reproach. For this reason, the coparenting relationship is a strong factor influencing parental adjustment (Weissman & Cohen, 1985). As a result, coparenting also influences parenting quality: It is difficult to be patient, sensitive, and warm as a new parent when in conflict with one’s partner, feeling undermined and criticized in one’s parenting role, or resentful of a seemingly unfair division of the parenting workload (Feinberg, 2003). Children’s emotional security is a critical influence on developmental outcomes (e.g., psychopathology) and is predicted by the quality of overall family functioning and parent–child attachment. Marital argument and conflict threatens the security perceived by infants and young children and, therefore, increases the chances of negative child outcomes (Cummings & Davies, 2011).
In reality, meaningful improvement in these areas may not require monumental effort or resources if efficient delivery of brief program services can be achieved (Cummings & Davies, 2011; Cummings, Faircloth, Mitchell, Cummings, & Schermerhorn, 2008; Feinberg et al., 2009; Jones, Feinberg, & Hostetler, 2014; Mejia, Calam, & Sanders, 2015). We originally hypothesized that coparenting, parent adjustment, and parenting could be influenced positively through the FF program design, and evaluation of the first trial indicated that this was the case (Feinberg & Kan, 2008; Feinberg et al., 2009, 2010). Positive effects on parent outcomes were detected immediately after program completion but also as late as 3 years post-intervention for the original trial of the program. At posttest (i.e., 6 months postpartum), we found program impact on self-reported maternal depression and anxiety as well as on both parents’ self-reported coparenting support. Intervention couples also indicated less dysfunction in parent–child interactions as well as longer infant duration of attention (Feinberg & Kan, 2008). Using observational data from 12 months postpartum, examinations revealed lower levels of negative coparenting behavior between intervention couples and greater parenting positivity (Feinberg et al., 2009).
Follow-up assessment when the child was 3 years old revealed sustained impact from the initial program. Intervention parents indicated better levels of parenting adjustment, greater satisfaction with coparenting, and improved parenting—including lower rates of corporal punishment—compared with a control group (Feinberg et al., 2010). Depression was found to be statistically lower among single mothers who received the program. Perhaps most notably, long-term effects on child outcomes were observed in the initial trial of the program at the 3-year assessment: Mothers of boys in the intervention group indicated better externalizing and internalizing behavior, although the same effect was not found for girls (Feinberg et al., 2010). These findings were echoed in a subsequent assessment when children had reached early school-age. Teachers rated intervention boys as lower on externalizing behavior, corresponding to parent report at 3 years of age. Interestingly, teachers rated intervention children as lower on internalizing symptoms regardless of gender (Feinberg et al., 2014).
Family Foundations: Second Trial
The second trial of FF was intended to validate the findings from the first trial by assessing impact as the child develops. Our recent evaluation of outcomes at the 10-month-posttest assessment replicated and extended findings from the first trial on multiple domains (Feinberg et al., 2016). This assessment included improved parent mental health (i.e., depression, anxiety), lower levels of parent-reported family aggression, and more positive coparenting and parenting behaviors demonstrated in observational measures. Effects were also detected for parent-reported child sleep habits and soothability. Some effects were found to be greater or only evident as pre-intervention risk increased; risk factors were represented through observer-coded negative communication styles and self-reported levels of depression during pregnancy.
Considering effects from the original trial on child behavioral outcomes, we were interested in understanding whether these child effects were evident through the 2-year follow-up assessment. Given the finding of positive impact on child sleep habits at the posttest evaluation and the importance of sleep as an influence on well-being (Feinberg et al., 2016; Sepa, Frodi, & Ludvigsson, 2004), we assessed impact on child sleep. Although detecting the impact on child emotional and behavioral adjustment at 2 years of age can be difficult given issues in assessing adjustment in children so young (Shepard, Kagan, & Wurtz, 1998), it is important to consider when such effects may first be evident. Assessing sleep at this age is important when considering possible precursors to behavioral problems (Sadeh et al., 2015) that may be better assessed at older ages.
A thorough understanding of intervention effects includes addressing the question of moderation (i.e., for whom is an intervention most or least beneficial). Thus, we were interested in assessing whether variability in program impact across families may be systematically related to pretest family characteristics. For example, families under more stress or struggling with relationship conflict during pregnancy may particularly benefit from a supportive preventive intervention. In our analysis, we were interested in whether a demonstrated effect on a study outcome found for all families is actually stronger for higher or lower risk families or, alternatively, whether the effect is only detected among families with particular characteristics. Because our focus in the program was on coparenting, couple-relationship risk before intervention could have moderated findings. Couples who were able to communicate and problem-solve well before the program might not have needed as much support. However, an alternative hypothesis is that the presence of risk factors during pregnancy might have undermined the ability of couples to take advantage of the tools and strategies offered in the intervention classes. Given prior evidence that intervention impact on some outcomes was greater among couples demonstrating relationship stress (Feinberg et al., 2014; Kan & Feinberg, 2014), we hypothesized that couple conflict would be associated with larger intervention effects in this case as well. Thus, we assessed whether intervention effects were moderated by pre-intervention levels of risk as measured by couple conflict.
Method
The evaluation of this trial of FF comprises 399 heterosexual couples recruited through hospitals in three northeastern and one southwestern state. To participate, couples were required to be living together, expecting their first child together, and at least 18 years of age at the time of enrollment. No mothers in the study had given birth before recruitment. The study was advertised through childbirth education programs and obstetrician and gynecological clinics located in or near regional hospitals. At enrollment, the mean age of expectant mothers and fathers was 29.1 years (SD = 4.4) and 31.1 years (SD = 5.4), respectively; mean education level was 15.7 years (SD = 1.5), median annual household income was $85,000 (ranging from $5,000 to $162,500), and 87% of couples were married. Most participants (81%) indicated their race as non-Hispanic White; minority racial and ethnic categories included 7% Hispanic, 6% Black, and 4% Asian, and 2% indicated multiple races or ethnicities. Separate cohorts of participants were recruited in succession across the study sites, joining the study beginning in the fall of 2008, and the last couples were recruited roughly 4 years later.
The program was delivered through a series of five prenatal and four postnatal classes. More background information on the theoretical model is available in (Feinberg, 2003). (Information for parents and professionals can be found at http://famfound.net.) The classes were led by a mixed-gender pair of trained group leaders. Classes included 8 to 12 couples with content delivery comprising presentations, group discussion, couple and group skill-building exercises (e.g., role-plays), and video vignettes. Training of group leaders involved 3 full days at each site, with supervision provided by the research team after each session until familiarity and competence with the intervention model was achieved. To enhance participant interest and reduce burden, the prenatal classes also included educational material on standard childbirth so that participants did not need to attend a separate class series for childbirth preparation. Families assigned to the control group received mailed written materials on selecting high-quality childcare and the stages of child development. More than half of intervention couples attended at least eight of the nine classes (Mprenatal = 4.4, SD = 1.2; Mpostnatal = 2.3, SD = 1.7), which signifies high engagement compared with typical engagement rates for family-focused interventions (Ingoldsby, 2010). Nine families assigned to the intervention (4%) did not attend any of the sessions but were included in analyses given our intent-to-treat approach. One prenatal and one postnatal class for each cohort were video recorded and rated by a trained, reliable observer for implementation quality.
Pretest data were collected during a home visit when mothers were at a mean of 22.8 weeks’ gestation. During this visit, video recordings of the couples interacting during a structured discussion session provided information on dyadic communication styles. Each expectant parent then completed a set of questionnaires privately. Couples were randomly assigned to intervention or control conditions after this interview using a random number generator.
At roughly 2 years postpartum (post-intervention), staff members returned to couples’ homes for a follow-up assessment of intervention impact. These visits involved similar home-interview procedures although with multiple video-recorded family interactions. Institutional review boards at the Pennsylvania State University and participating hospitals approved the study, and participants signed informed consent forms before participating.
Measures
Parent Observational Measures
The follow-up interview included a similar protocol as the posttest assessment carried out at 10 months postpartum, in which the families (both parents and the child) engaged in two interactions as a triad while being video recorded. The first interaction lasted 12 minutes and involved free play with provided toys; the second interaction lasted 6 minutes and involved the parents teaching their child to accomplish a set of developmentally difficult tasks (e.g., stringing wooden beads). Trained research assistants blind to intervention condition coded these interactions using codes with 5- to 7-point ordinal response scales. An experienced coder served as a criterion coder. Roughly 25% of randomly selected cases were coded by at least two raters to determine reliability with the criterion coder; interrater intraclass correlations ranged from .66 to .85. More information on the video procedures can be found in our evaluation of posttest outcomes (Feinberg et al., 2016).
Aggregation of codes into index variables was based on conceptual alignment between specific scales that was confirmed through factor analyses. Individual codes were standardized (M = 0) before combining them into composite scores. Coparenting positivity combined three separate codes for parent-observed coparenting styles: coparental warmth, cooperation, and inclusiveness (α = .63 for mothers and .69 for fathers). Measures of coparenting negativity included separate ratings of observed coparental triangulation, competition, withdrawal, hostility, and endorsement of the partner (which was reverse scored). A triadic relationship quality code represented overall quality of the mother, father, and child triadic interactions. Separate parenting indices were also created for each parent. A positivity aggregate combined three codes: affection, sensitivity, and support for exploration (α = .82 for mothers and .86 for fathers). Parenting negativity was created from codes for parental rejection and observed negative affect toward the child (α = .80 for mothers and .76 for fathers).
Parent Report of Self and Child
A total score for parental depressive symptoms was derived using a 14-item version of the Center for Epidemiological Studies Depression Scale (Radloff, 1977). Individual questions inquired about respondents’ feelings and outlook within the past week, using four response options ranging from rarely/none of the time (scored as 1) to always/most of the time (4). In the present study, internal reliability (Cronbach’s α) scores were .85 for mothers and .83 for fathers. Anxiety was obtained from a revised version of the Penn State Worry Questionnaire (Beck, Stanley, & Zebb, 1995; Meyer, Miller, Metzger, & Borkovec, 1990); the revised version used seven of the original 16 items. Internal reliability scores in the present study were .94 for mothers and .93 for fathers. Collectively, these questions assessed how typical excessive and uncontrollable worries were for respondents, soliciting reflection on thought processes ranging from not at all typical (1) to very typical (5). Children’s behavior at roughly 2 years of age was gauged using the 100-item Child Behavior Checklist (CBCL) for ages 1.5 to 5 (Achenbach & Rescorla, 2000) using two broadband scales for externalizing and internalizing behavior based on conventional methods for the measure. Raw scores were used without normalizing based on age per recommendations in the CBCL manual for use in analysis. Both mothers and fathers reported the degree to which children demonstrated certain behaviors using an ordinal scale ranging from not true (0) to very/often true (2). Mothers reported on two items from the Child Sleep Questionnaire (Seifer, Sameroff, Dickstein, & Hayden, 1996) representing sleep habits at 2 years of age: the typical number of nighttime wakings and total duration of child nighttime sleep.
Control Variables
Following analyses reported for the first trial and prior reports from this trial, we included several control variables representing characteristics of the parents and their context. These included study site, age, gender, family income, marital status, and reported financial strain. The latter involved a composite score created from three items asking (a) how much a respondent has had to reduce standard of living recently, (b) inability to afford certain essentials, and (c) difficulty living on current income (α = .69 for mothers and .65 for fathers). A measure of social desirability was also included to control for potential response bias on self-report outcomes (α = .64 for mothers and .65 for fathers). An indicator for site served as a control variable referring to the different healthcare facilities that housed the program. We included the corresponding pretest measure of the outcome as a control variable if available (e.g., parenting or child outcomes were not measured at pretest). Child age (in months) and gender were included as controls in analyses of child outcomes, but gender was not included for models assessing child sleep outcomes.
Moderator
For all study outcomes at follow-up, we employed separate regression models to assess potential moderated effects. We focused on whether level of initial risk moderated intervention impact. This investigation is based on prior findings both in the original trial of FF (Feinberg et al., 2014) as well as from moderated impact demonstrated for this (the second) trial observed at posttest (Feinberg et al., 2016). Specifically, we selected the negative-communication style derived from observed couple interactions during the pretest interview. As noted earlier, the pretest home interview included a couple-relationship discussion task, where couples were asked to discuss issues they would like to change in each other. Video recordings were later coded by trained raters (see Feinberg et al., 2016) for more information on coder training). A negative communication score comprised mean scores across separate codes for demonstrated aggression and anger in the discussion. This composite score was characterized by positive skew; to remove the influence of extreme values from this score in assessments of moderation, we set extreme values at a capped maximum based on box-plots indicating outliers, which altered values in data for three mothers and four fathers.
We also considered gender—gender of the parent for parent outcomes and gender of the child for child outcomes—as a potential moderator of intervention impact. For all models presented, we tested for gender moderation by adding a Gender × Condition term to the model, except for outcomes representing the couple (e.g., observed triadic relationship quality). In no case did we find evidence of gender moderating intervention impact; thus, we do not present those results. Finally, we also tested and found no evidence that marital status moderated intervention effects, although a low sample size among the nonmarried couples limited statistical power to detect these effects in this study.
Analytic Models
We used separate regression models to test the main effect of the condition (intervention = 1; control = 0) for each outcome as well as separate regression models to assess potential moderated effects. For parent-specific outcomes nested within dyads, we used multilevel regression models with a random intercept specified to represent couple-level shared variance. Where both parents reported on the child (i.e., CBCL outcomes), we included mother and father report; thus, the model assessed perception of child behavior separately for each parent. Ordinary regression models were used for outcomes available only at the family level: mother-reported child sleep (fathers did not report on child sleep) and observed triadic relationship quality. A count-based regression model (negative binomial) was used for analysis of the number of wakings (child) outcome.
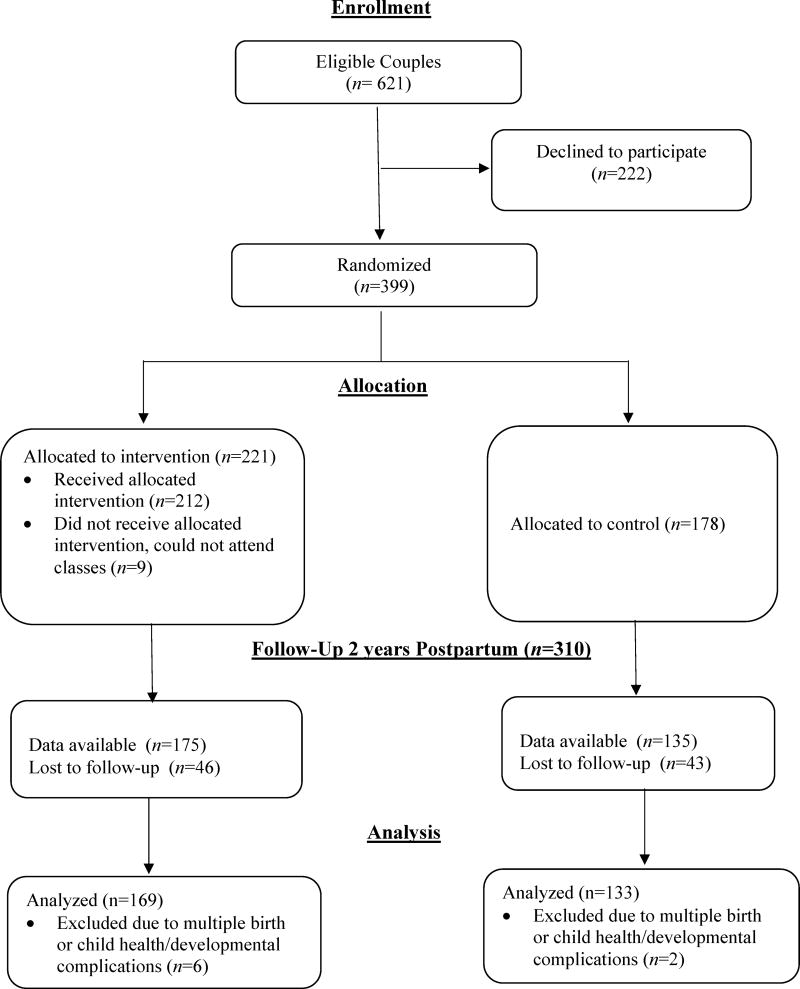
Eight families were excluded from analyses (six intervention and two control) because of severe parent or infant medical problems (e.g., severe congenital defect, poor maternal health), developmental disorders (e.g., autism, Down syndrome), or multiple births. Follow-up data collection was also subject to some attrition of participants across the 2.5-year period, which is to be expected for families transitioning to parenthood (e.g., see Deke, Sama-Miller, & Hershey, 2015). Specifically, for the home interview 310 mothers and 295 fathers provided data, an attrition rate of 21% and 24%, respectively. The attrition rate was higher for observational data because families could decline even if participating in other aspects of the data collection. In all, roughly 240 families provided observational data (i.e., 38% original sample did not participate). See Figure 1 for a Consolidated Standards of Reporting Trials (CONSORT) flow diagram showing the sample sizes for intervention and control groups for the present study.
Figure 1.
Flow of participants through each stage of the second trial of the Family Foundations program evaluations.
Because of missing data, it was necessary to investigate whether the data were missing at random and also to accommodate missing data in our analytic approach. We conducted binary logistic regressions examining multivariable prediction of posttest participation by follow-up; interaction terms between condition and specific predictors were included to test for differential attrition. Predictors included baseline characteristics of the participants/couples, representing stress, mental health, relationship qualities, and demographic factors (e.g., socioeconomic status, marital status). Through these sets of analyses, we found no evidence of differential attrition between conditions. Missing data models were employed to gain full-sample model estimates given problems with relying on complete case analyses (Little & Rubin, 2014). This approach is an efficient technique for accommodating missing data, even when attrition rates are relatively high (Schafer & Olsen, 1998). Multiple imputation techniques involving standard procedures were used to derive 60 imputed datasets for all regression analyses of study outcomes. Missing data models were carried out separately by intervention group to preserve our ability to assess moderated intervention effects. In addition to the follow-up outcomes and relevant covariates, these models included dozens of baseline predictors including demographic variables (e.g., socioeconomic status), mental health and stress levels, couple relationship quality, and other factors representing parental interactions.
Results
Table 1 provides descriptive statistics for all pretest control variables and study outcomes by condition. Table 2 provides regression results for tests of overall intervention effect on study outcomes. We found evidence of a statistically significant intervention impact on three of the five observational outcomes in the coparenting and parenting domains. Families from the intervention condition demonstrated statistically greater overall triadic relationship quality in observed family interactions as well as statistically lower levels of coparenting negativity and parenting negativity. The fourth outcome, parenting positivity, did not have a statistical effect in these data but the observed direction of effect was consistent with the other statistically significant effects. There was no statistical or meaningful difference between conditions on coparenting positivity scores.
Table 1.
Means and Standard Deviations for Control Variables and Study Outcomes at Follow-Up Assessment
| Characteristic | Mothersa
|
Fathers
|
||||||
|---|---|---|---|---|---|---|---|---|
| Intervention
|
Control
|
Intervention
|
Control
|
|||||
| M | SD | M | SD | M | SD | M | SD | |
| Control variables | ||||||||
| Marital status: marriedbc | .88 | — | .84 | — | ||||
| Household income (divided by 10,000) | 8.67 | 3.71 | 8.59 | 3.92 | ||||
| Child age, at follow-up assessment | 2.13 | 0.19 | 2.14 | 0.21 | ||||
| Child gender: femalec | .51 | — | .49 | — | ||||
| Age | 29.42 | 4.33 | 28.53 | 4.33 | 31.59 | 5.59 | 30.38 | 4.95 |
| Perceived economic strain | 0.04 | 2.39 | −0.08 | 2.18 | −0.05 | 2.01 | 0.1 | 2.62 |
| Social desirability index | 7.72 | 2.55 | 7.90 | 2.68 | 8.10 | 2.43 | 8.07 | 2.76 |
| Observed negative couple communication | −0.04 | 0.77 | 0.00 | 0.81 | −0.09 | 0.71 | 0.07 | 0.89 |
| Observed measures | ||||||||
| Coparenting: triadic relationship qualitya | 0.16 | 0.81 | −0.21 | 0.97 | — | — | ||
| Coparenting: positivity aggregate | 0.06 | 0.64 | −0.06 | 0.53 | 0.03 | 0.62 | −0.03 | 0.64 |
| Coparenting: negativity aggregate | −0.06 | 0.35 | 0.09 | 0.65 | −0.09 | 0.34 | 0.12 | 0.65 |
| Parenting: positivity aggregate | 0.07 | 0.68 | −0.12 | 0.78 | 0.03 | 0.76 | −0.06 | 0.80 |
| Parenting: negativity aggregate | −0.10 | 0.41 | 0.16 | 1.12 | −0.08 | 0.56 | 0.13 | 0.98 |
| Parent outcomes (self-report) | ||||||||
| Depressive symptoms | 0.44 | 0.37 | 0.41 | 0.32 | 0.42 | 0.36 | 0.50 | 0.38 |
| Anxiety | 14.74 | 6.28 | 14.85 | 6.38 | 11.50 | 5.02 | 12.19 | 5.54 |
| Child outcomes (parent report) | ||||||||
| CBCL: externalizing | 9.81 | 6.41 | 10.50 | 6.41 | 10.35 | 6.38 | 10.60 | 6.53 |
| CBCL: internalizing | 5.37 | 4.04 | 5.84 | 4.45 | 5.33 | 4.17 | 6.44 | 5.71 |
| Number of night wakings | 0.83 | 1.31 | 1.11 | 1.55 | — | — | ||
| Hours child sleeps during night | 9.96 | 1.81 | 10.02 | 1.22 | — | — | ||
Note. CBCL = Child Behavior Checklist.
Also includes family and child variables, where appropriate.
Measured using combined score from mother, father, and child reports.
Numbers represent proportions of the sample.
Table 2.
Regression Coefficients and Standard Errors for Intervention Effects Moderated by Pretest Levels of Observed Couple Negative Communication for Expectant Parents
| Predictors | B | p | d or IRRa | 95% CI |
|---|---|---|---|---|
| Observed measures | ||||
| Coparenting: positivity aggregate | 0.08 | .230 | [0.05, 0.21] | |
| Coparenting: negativity aggregate | −0.16 | .001 | 0.38 | [−0.25, −0.07] |
| Coparenting: triadic relationship quality | 0.36 | .001 | 0.39 | [0.15, 0.58] |
| Parenting: positivity aggregate | 0.13 | .054 | 0.18 | [0.00, 0.27] |
| Parenting: negativity aggregate | −0.20 | <.001 | 0.41 | [−0.29, −0.11] |
| Parent self-report: parent adjustment | ||||
| Depressive symptoms | −0.03 | .284 | [−0.09, 0.03] | |
| Anxiety | −0.50 | .280 | [−1.25, 0.36] | |
| Parent self-report: Child outcomes | ||||
| CBCL: Externalizing | −0.78 | .210 | [−2.00, 0.44] | |
| CBCL: Internalizing | −0.93 | .043 | 0.19 | [−1.84, −0.03] |
| Number of night wakings (mother-report) | −0.35 | .030 | 0.30a | [−0.66, −0.33] |
| Hours child sleeps during night (mother-report) | 0.05 | .779 | [−0.28, 0.37] |
Note. CBCL = Child Behavior Checklist; CI = confidence interval for B; IRR = incidence ratio rate. All models include controls for site location and pretest characteristics of informant: family income, economic strain, and age. Parent-report outcome models also include a control for social desirability. Child outcome models include a control for child age; child gender was added as a control for CBCL outcomes. Multilevel modeling was used if data were available from each parent.
Effect sizes are Cohen’s d (model-adjusted standardized group mean differences) except for number of night wakings; for that outcome, a multilevel negative binomial regression model was used, and an IRR is provided for effect size.
In contrast to outcomes based on observational parenting domains, we did not find statistically significant intervention effects for the full sample on the self-report parent outcomes. These findings included null effects for both scores representing parental adjustment (i.e., levels of depression and anxiety). However, a statistically significant intervention impact was found on parent reports of two child outcomes: Intervention children were reported by parents to demonstrate lower internalizing problems and reported by mothers to have fewer nighttime wakings. There were no overall intervention effects found for child externalizing problems or the total number of hours the child sleeps. As noted earlier, we found no evidence of child’s gender moderating the impact of intervention on behavior.
Separate analyses revealed a pattern in which intervention impact was moderated by pretest levels of observed couple negative communication, consistent with results from prior assessments of the effects of this intervention (Feinberg et al., 2016). This pattern was demonstrated through five of the nine study outcomes (Table 3). For observed positive and negative parenting, results indicated a statistically significant overall intervention impact that was larger for families at higher risk (i.e., that had higher levels of negative communication) at baseline. This pattern was also found for two of the three observed coparenting scores: negativity (see Figure 2) and triadic relationship quality. A similar result was found for mother-reported child wakings, where the intervention impact was greater as pretest observed dyadic negative communication increased in the sample. Finally, although the main effect of anxiety was not statistically related to group membership, we found an intervention effect on anxiety as prenatal parental risk increased.
Table 3.
Regression Models Predicting Participation in the Intervention Program, Moderated by Pretest Levels of Observed Couple Negative Communication
| Variable | Coparenting negativity
|
Relationship quality
|
Parenting positivity
|
Parenting negativity
|
Anxiety
|
Night wakings
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | 95% CI | p | B | 95% CI | p | B | 95% CI | p | B | 95% CI | p | B | 95% CI | p | B | 95% CI | p | |
| Condition | −0.19 | [−0.28, −0.10] | <.001 | 0.35 | [0.14, 0.56] | .001 | 0.13 | [0.00, 0.26] | .058 | −0.19 | [−0.28, −0.10] | <.001 | −0.38 | [−1.20, 0.44] | .364 | −0.26 | [−0.59, 0.06] | .112 |
| Negative Communication | 0.14 | [0.06, 0.21] | .001 | −0.32 | [−0.55, −0.09] | .006 | −0.20 | [−0.31, −0.09] | .001 | 0.14 | [0.06, 0.21] | .001 | 0.88 | [−0.03, 1.78] | .057 | 0.16 | [−0.05, 0.37] | .135 |
| Condition × Negative Communication | −0.13 | [−0.23, −0.02] | .016 | 0.33 | [0.02, 0.65] | .038 | 0.24 | [0.08, 0.41] | .004 | −0.13 | [−0.23, −0.02] | .016 | −1.95 | [−3.10, −0.79] | .001 | −0.45 | [−0.85, −0.06] | .025 |
Note. CI = confidence interval.
All models include controls for site location and pretest characteristics of informant: family income, economic strain, age, child age (for wakings) and social desirability (for parent report). Multilevel modeling was used if data were available from each parent. The moderator was centered before analysis to aid in coefficient interpretation.
Figure 2.
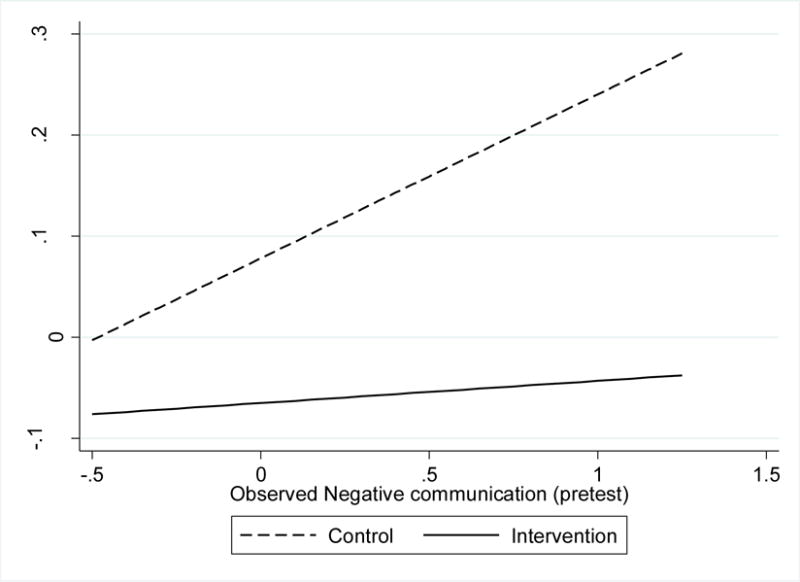
Moderation of intervention impact on observed negative coparenting at follow-up, across level of pretest observed negative couple communication style.
Discussion
The findings presented here represent new evidence on the effectiveness of the FF program. These results from the second trial of the program demonstrate longer term impact observed at 2 years postpartum. The data used here enabled a final assessment of sustained program impact across multiple key outcome domains for the planned evaluation period. Our analyses confirmed that the improvements in parenting and coparenting behaviors found previously at approximately 1-year postpartum (Feinberg et al., 2016) were sustained a year later. Likewise, the intervention effect on improved child sleep patterns found at posttest continued to be demonstrated in terms of reduced number of night wakings at the 2-year follow-up assessment. Most notably, we detected an intervention effect on child adjustment at 2 years of age, as reported by parents. This evidence of impact on child adjustment is consistent with results from the first trial, which were based on parent report at 3 years of age and again by teacher report at 7 years of age. The present results indicate that impact on child adjustment is demonstrated roughly as soon as child internalizing and externalizing adjustment can be reliably assessed. Further, the finding of fewer nighttime wakings is important given the link between sleep problems and future behavior problems (Sadeh et al., 2015). Overall, demonstration of program impact on child outcomes across multiple ages and trials of the program suggests that an effective but efficient intervention for parents can have impact throughout a critical developmental period.
Although we found no evidence of a differential program effect dependent on child gender in the present study, we will continue to investigate potential variation based on gender in future work given findings for stronger impact among boys from the initial trial based on child adjustment outcomes at 3 years of age (Feinberg et al., 2010). It is possible that gender moderation of intervention impact has not emerged by 2 years of age. In general, more research is needed to improve understanding for how a program such as FF can positively influence early child behavior indirectly.
Results presented here are generally consistent with prior evaluation of this trial at 10 months postpartum (Feinberg et al., 2016), although some differences are worth considering. Consistent with the earlier results, we found lower levels of observed negativity in both coparenting and parenting domains as well as higher overall coparenting relationship quality. Interestingly, levels of observed positivity were not found to be statistically higher among intervention parents for coparenting and parenting domains, as had been found at posttest (albeit the latter had an intervention impact effect size (d) of 0.18, which could emerge as statistically significant with a higher powered study). This could be an indication that the intervention is more effective at reducing observable negativity in couple interactions in a sustained way compared with positivity. It may also be the case that differences in positive behaviors are less discernible in the observational measurement setting (compared with negative behaviors) as the child gets older.
We did not find the same evidence of intervention impact on parent mental health that was evident at the earlier assessment for this trial (Feinberg et al., 2016). We detected lower levels of anxiety among the intervention parents as pretest risk increased, which has implications for health among parents with greater burdens, given the physiological effects of stress (Brosschot, Van Dijk, & Thayer, 2007). However, we did not find continued impact on depressive symptoms for the whole sample at 2 years postpartum. In the first trial, we found short-term impact on depressive symptoms for all mothers, whereas long-term impact was maintained over time only among nonmarried mothers (Feinberg et al., 2010). We did not find similar impact in the present study, although the low percentage of nonmarried parents in the second trial (roughly 14% at pretest) may have limited our ability for obtaining precise effects in assessment of moderation by marital status. However, the lack of overall program impact on long-term depressive symptoms as a result of this brief transition to parenthood program is not surprising. Depressive symptoms may change considerably across the 2 postpartum years as some mothers recover, perhaps due to benefitting from other familial support or medical assistance. Research has demonstrated that postpartum depression is linked to poor long-term child outcomes, even controlling for the presence or absence of later bouts of maternal depression (Murray, Halligan, Adams, Patterson, & Goodyer, 2006). Although not as extensively studied, paternal mental health is also an important factor for the developing infant (Garfield et al., 2014; Ramchandani et al., 2008). Thus, short-term intervention impact on depressive symptoms in participating parents may be important for long-term child well-being even if program impact is not maintained longer term among parents.
Although our outcome measures, as is common in the field, do not provide precise information on clinical significance, and acknowledging that interpretation of obtained effect sizes is much more complex than usually discussed (Ferguson, 2009), we see the largely moderate-sized effects of FF in this study as representing substantial practical benefits for families. No other transition to parenthood program focused on couples has been able to achieve such levels of impact across outcome domains or across time (i.e., persisting effects after posttest). In our first trial, we found that moderate-sized impacts on family factors led to important mental health, behavioral, and academic outcomes reported by teachers when children were 7 years old (Feinberg et al., 2014). And in our analyses of mediation pathways in this trial, we found that program impact on child outcomes is mediated by several factors (e.g., parent adjustment, parenting, coparenting) working in concert rather than by a single common pathway (e.g., parenting; Feinberg, Jones, & Hostetler, 2017). Thus, achieving moderate-sized impact on several mediating, and reciprocally interacting, childrearing environment factors represents an important approach to enhancing children’s well-being.
The issue of program impact for families across levels of risk is critical because those parents at the highest levels of risk are more likely to be aggressive with each other as well as both psychologically and physically abusive toward the child (Slep & O’Leary, 2005; Tolan, Gorman-Smith, & Henry, 2006). Findings of greater program impact among those at higher risk at baseline have been demonstrated for the FF program in the original trial (Feinberg et al., 2014; Feinberg, Roettger, Jones, Paul, & Kan, 2015) as well as in this second trial for both birth (Feinberg et al., 2015) and short-term outcomes (Feinberg et al., 2016). Our approach here included an exploration of moderated program impact considering all study outcomes. The program was designed for all first-time parents but could feasibly have greater impact among those with higher levels of risk due to factors such as low financial resources or high relationship distress. Statistical models in the present assessment echoed those found more proximal to intervention completion, showing that effects on several key outcomes were stronger among those at greater risk, as represented here by relatively higher levels of observed couple negative communication during pregnancy. For most outcomes, results indicated that the overall (main) effect of the program was statistically significant and that this effect was stronger as baseline risk increased among the sample. We note that with the typical randomized controlled trial (RCT) design, we cannot disentangle whether such families benefited more from program exposure simply due to the greater amount of improvement possible or because of specific program factors—for example, whether the social support and role-modeling among participants that occurs within face-to-face, group format programs is particularly salient for such families.
The finding of moderated program impact has important implications for planning future implementations and evaluation. For example, if FF did not provide greater benefit to families at higher risk, then such families would continue to require additional support or intervention to reduce disparities and “level the playing field.” Generalizing the risk moderation effects from this or other trials of universal programs is likely not a valid approach at this point. We do not understand the specific program factors that would lead families to benefit more, similarly, or less than other families. Thus, exploring whether such youth and families derive more versus less benefit from universal programs is an important consideration with practical implications that should be reported for all trials of universal programs.
Moreover, further focus should be directed toward understanding the degree to which families at greater risk can be reached by programs such as this and whether more enhanced program versions (e.g., using home visiting or tailoring program content for higher levels of risk) may be more successful. In other words, the additional impact (and reach) of such tailored program versions should be compared with the benefits higher risk families derive from inclusion in a universal program version. For instance, modified versions of FF are currently underway that are designed to support new parents who are burdened with higher risk factors compared with the general population, such as poor parents, adolescent parents, military families, and families with health challenges. In such efforts, we attend to potential iatrogenic results as the negative consequences of a high-risk tailored program approach, including possible social reinforcement among higher risk participants of maladaptive tendencies (Dishion, McCord, & Poulin, 1999), as well as stigmatization if indicated or selected program versions are viewed as designed for families outside the mainstream. Yet, to guide further development of programs and policy-making around community-level implementation, it is important to consider the trade-offs between possibly greater reach and the impact of tailored versions for higher risk groups against the more effortful and expensive implementation of a spectrum of program versions (universal, indicated, selected) relative to a single universal version.
Further, RCT findings can obscure the potential for universal programs such as FF to improve outcomes among higher risk families via community-level impacts. Universal prevention programs such as FF can enhance the general level of family functioning and well-being among parents and children within a community. Such community-wide effects can support higher risk families through a higher level of peer (family to family) social support and role-modeling throughout community settings. Gradual improvement of children’s peer contexts (in day care, preschool, school, neighborhood play, and youth recreation and afterschool settings) by way of reduced behavior and emotional problems and greater social competence among children in general might be an additional community-level outcome. Enhanced peer contexts would likely present fewer stressors for children at higher risk and greater opportunities for social integration and learning prosocial relationship skills; such peer-setting impacts would then likely lead to reduced stress and conflict within higher risk families when children return home. The empirical basis for such community-based effects is only slowly emerging; see, for example, our prior work on the diffusion pathways of substance use prevention operating through both the parenting of children’s friends’ parents and the attitudes and behaviors of the youth themselves (Cleveland, Feinberg, Osgood, & Moody, 2012; Rulison, Feinberg, Gest, & Osgood, 2015).
Finally, the results from this evaluation provide additional evidence that this program can work in different contexts. The first trial was implemented in two medium-sized cities in central Pennsylvania (Feinberg et al., 2010). The second trial reported in the present study was implemented in multiple settings across the country. Demonstrated effects in multiple trials and regions support the original intention for program dissemination (i.e., that it can be installed and effectively delivered in various settings using different program implementers). The program was designed to be disseminated broadly and manualized in a way that allows for its use in health care settings across the country. Replication of impact across two trials on parenting and coparenting behaviors—and in turn, child outcomes—shows that these important outcomes can be improved using an effective but efficient approach (Jones et al., 2014) implemented across different settings. Efficiency is especially relevant for considering policy implications, as preliminary assessment of the program’s potential return on investment suggests that monetary benefits of the outcomes of the program are roughly three times greater than the initial cost of implementing the program (Jones, 2015).
Certain limitations are worth noting with respect to the present investigation. Although we attempted to control for some bias through inclusion of a social desirability scale, parent-report data are still subject to reporter bias. As noted, subgroup analyses were sometimes limited by smaller sample sizes (e.g., for unmarried participants). Compared with the general population, the sample was more likely to be married, Caucasian, and have higher household income. Some lack of representativeness to the general population may be due to the nature of the study, which relies on recruiting from health care facilities where certain families (e.g., married) may be more likely to agree to participate in group-based instructional classes and research procedures. We could not assess variation of program impact based on racial and ethnic characteristics given that more than 80% of the sample was Caucasian. Intervention impact could be different (and possibly greater, given our findings about risk) among families with lower socioeconomic status or other relative disadvantage than the families in our sample tended to experience. In short, although our results represent new parents from diverse settings across four regions, they may not generalize to the entire population. Further, our results are based on an intent-to-treat analytic approach; statistical results may differ among those families who are more or less engaged with the intervention. We leave such investigation for future research.
Conclusion
The goal of the FF program is to improve parenting and coparenting strategies, thereby achieving positive developmental benefits for children. A secondary goal is to demonstrate that these changes can be achieved through a program that is feasible for new parents (e.g., low time commitment) and for public health providers (e.g., readily installed, relatively low cost). The results of the present study indicate that key initial positive findings in this trial at 10 months postpartum continue to be evident more than a year later and translate to important benefits in terms of child adjustment. These findings are consistent with results from evaluations of the original trial of the program—implemented in different settings—that demonstrated long-term program impact on both family and child outcomes. More research is needed to understand the long-term implications of effective programs that target these early family relationships and to understand how such programs can be implemented more broadly for the sake of improved public health.
Acknowledgments
This research was supported by a grant from the National Institute of Child Health and Human Development (NICHD; HD058529), Mark Feinberg, Principal Investigator. The views expressed in this article are those of the authors and do not necessarily represent the views of NICHD or Penn State University. Dr. Feinberg created Family Foundations and is the owner of a private company that disseminates the program.
Footnotes
Dr. Feinberg’s company has been reviewed by the Institutional Review Board and the Conflict of Interest Committee at Penn State University for potential financial gain. The other authors declare no potential conflict of interest.
Contributor Information
Damon Jones, The Pennsylvania State University.
Mark Feinberg, The Pennsylvania State University.
Michelle Hostetler, The Pennsylvania State University.
Michael Roettger, The Australian National University.
Ian M. Paul, The Pennsylvania State University
Deborah B. Ehrenthal, The University of Wisconsin–Madison
References
- Abidin RR, Brunner JF. Development of a parenting alliance inventory. Journal of Clinical Child Psychology. 1995;24:31–40. doi: 10.1207/s15374424jccp2401_4. [DOI] [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA preschool forms & profiles. Burlington: University of Vermont Department of Psychiatry; 2000. [Google Scholar]
- Beck JG, Stanley MA, Zebb BJ. Psychometric properties of the Penn State Worry Questionnaire. Journal of Clinical Geropsychology. 1995;1:33–42. [Google Scholar]
- Belsky J. The determinants of parenting: A process model. Child Development. 1984;55:83–96. doi: 10.2307/1129836. [DOI] [PubMed] [Google Scholar]
- Brosschot JF, Van Dijk E, Thayer JF. Daily worry is related to low heart rate variability during waking and the subsequent nocturnal sleep period. International Journal of Psychophysiology. 2007;63:39–47. doi: 10.1016/j.ijpsycho.2006.07.016. [DOI] [PubMed] [Google Scholar]
- Buehler C, Gerard JM. Marital conflict, ineffective parenting, and children’s and adolescents’ maladjustment. Journal of Marriage and Family. 2002;64:78–92. doi: 10.1111/j.1741-3737.2002.00078.x. [DOI] [Google Scholar]
- Cleveland MJ, Feinberg ME, Osgood DW, Moody J. Do peers’ parents matter? A new link between positive parenting and adolescent substance use. Journal of Studies on Alcohol and Drugs. 2012;73:423–433. doi: 10.15288/jsad.2012.73.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowan PC, Cowan PA. Interventions to ease the transition to parenthood: Why they are needed and what they can do. Family Relations. 1995;44:412–423. doi: 10.2307/584997. [DOI] [Google Scholar]
- Cummings EM, Davies PT. Marital conflict and children: An emotional security perspective. New York, NY: Guilford Press; 2011. [Google Scholar]
- Cummings EM, Faircloth WB, Mitchell PM, Cummings JS, Schermerhorn AC. Evaluating a brief prevention program for improving marital conflict in community families. Journal of Family Psychology. 2008;22:193–202. doi: 10.1037/0893-3200.22.2.193. [DOI] [PubMed] [Google Scholar]
- Deke J, Sama-Miller E, Hershey A. Addressing attrition bias in randomized controlled trials: Considerations for systematic evidence reviews. Princeton, NJ: Mathematica Policy Research; 2015. [Google Scholar]
- Dennis CL, Dowswell T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database of Systematic Reviews. 2013;2:CD001134. doi: 10.1002/14651858.CD001134.pub3. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, McCord J, Poulin F. When interventions harm: Peer groups and problem behavior. American Psychologist. 1999;54:755–764. doi: 10.1037/0003-066X.54.9.755. [DOI] [PubMed] [Google Scholar]
- Feinberg ME. Coparenting and the transition to parenthood: A framework for prevention. Clinical Child & Family Psychology Review. 2002;5:173–195. doi: 10.1023/A:1019695015110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME. The internal structure and ecological context of coparenting: A framework for research and intervention. Parenting: Science and Practice. 2003;3:95–131. doi: 10.1207/S15327922PAR0302_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Jones DE, Hostetler M. Experimental support for a family systems approach to understanding child development: Multiple mediators of intervention effects across the transition to parenthood. 2017 doi: 10.1037/cfp0000100. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Jones DE, Hostetler ML, Roettger ME, Paul IM, Ehrenthal DB. Couple-focused prevention at the transition to parenthood, a randomized trial: Effects on coparenting, parenting, family violence, and parent and child adjustment. Prevention Science. 2016;17:751–764. doi: 10.1007/s11121-016-0674-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Jones DE, Kan ML, Goslin MC. Effects of family foundations on parents and children: 3.5 years after baseline. Journal of Family Psychology. 2010;24:532–542. doi: 10.1037/a0020837. [DOI] [PubMed] [Google Scholar]
- Feinberg ME, Jones DE, Roettger ME, Hostetler M, Sakuma K, Paul IM, Ethrenthal D. Preventive effects on birth outcomes: Buffering impact of maternal stress, depression, & anxiety. Maternal and Child Health Journal. 2016;20:56–65. doi: 10.1007/s10995-015-1801-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Jones DE, Roettger ME, Solmeyer A, Hostetler ML. Long-term follow-up of a randomized trial of family foundations: Effects on children’s emotional, behavioral, and school adjustment. Journal of Family Psychology. 2014;28:821–831. doi: 10.1037/fam0000037. [DOI] [PubMed] [Google Scholar]
- Feinberg ME, Kan ML. Establishing Family Foundations: Intervention effects on coparenting, parent/infant well-being, and parent–child relations. Journal of Family Psychology. 2008;22:253–263. doi: 10.1037/0893-3200.22.2.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Kan ML, Goslin MC. Enhancing coparenting, parenting, and child self-regulation: Effects of Family Foundations 1 year after birth. Prevention Science. 2009;10:276–285. doi: 10.1007/s11121-009-0142-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Kan ML, Hetherington EM. The longitudinal influence of coparenting conflict on parental negativity and adolescent maladjustment. Journal of Marriage and the Family. 2007;69:687–702. doi: 10.1111/j.1741-3737.2007.00400.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Roettger M, Jones DE, Paul IM, Kan ML. Effects of a psychosocial couple-based prevention pogram on averse birth outcomes. Maternal and Child Health Journal. 2015;19:102–111. doi: 10.1007/s10995-014-1500-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson CJ. An effect size primer: A guide for clinicians and researchers. Professional Psychology: Research and Practice. 2009;40 doi: 10.1037/a0015808. [DOI] [Google Scholar]
- Frosch CA, Mangelsdorf SC, McHale JL. Marital behavior and the security of preschooler–parent attachment relationships. Journal of Family Psychology. 2000;14:144–161. doi: 10.1037/0893-3200.14.1.144. [DOI] [PubMed] [Google Scholar]
- Garfield CF, Duncan G, Rutsohn J, McDade TW, Adam EK, Coley RL, Chase-Lansdale PL. A longitudinal study of paternal mental health during transition to fatherhood as young adults. Pediatrics. 2014;133:836–843. doi: 10.1542/peds.2013-3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingoldsby EM. Review of interventions to improve family engagement and retention in parent and child mental health programs. Journal of Child and Family Studies. 2010;19:629–645. doi: 10.1007/s10826-009-9350-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ioannidis JP. Contradicted and initially stronger effects in highly cited clinical research. Journal of the American Medical Association. 2005;294:218–228. doi: 10.1001/jama.294.2.218. [DOI] [PubMed] [Google Scholar]
- Jones DE. return on investment from family-focused prevention. University Park, PA: Prevention Research Center, Penn State University; 2015. [Google Scholar]
- Jones DE, Feinberg ME, Hostetler ML. Costs to implement an effective transition-to-parenthood program for couples: Analysis of the Family Foundations program. Evaluation and Program Planning. 2014;44:59–67. doi: 10.1016/j.evalprogplan.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaczynski KJ, Lindahl KM, Malik NM, Laurenceau JP. Marital conflict, maternal and paternal parenting, and child adjustment: A test of mediation and moderation. Journal of Family Psychology. 2006;20:199–208. doi: 10.1037/0893-3200.20.2.199. [DOI] [PubMed] [Google Scholar]
- Kan ML, Feinberg ME. Can a family-focused, transition-to-parenthood program prevent parent and partner aggression among couples with young children? Violence and Victims. 2014;29:967–980. doi: 10.1891/0886-6708.VV-D-12-00162. [DOI] [PubMed] [Google Scholar]
- Kelly J. Children’s adjustment in conflicted marriage and divorce: A decade review of research. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:963–973. doi: 10.1097/00004583-200008000-00007. [DOI] [PubMed] [Google Scholar]
- Le Y, McDaniel BT, Leavitt CE, Feinberg ME. Longitudinal associations between relationship quality and coparenting across the transition to parenthood: A dyadic perspective. Journal of Family Psychology. 2016;30:918–926. doi: 10.1037/fam0000217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. Hoboken, NJ: Wiley; 2014. [Google Scholar]
- Margolin G, Gordis EB, John RS. Coparenting: A link between marital conflict and parenting in two parent families. Journal of Family Psychology. 2001;15:3–21. doi: 10.1037/0893-3200.15.1.3. [DOI] [PubMed] [Google Scholar]
- McHale JP, Kuersten-Hogan R, Lauretti A, Rasmussen JL. Parental reports of coparenting and observed coparenting behavior during the toddler period. Journal of Family Psychology. 2000;14:220–236. doi: 10.1037/0893-3200.14.2.220. [DOI] [PubMed] [Google Scholar]
- Mejia A, Calam R, Sanders MR. A pilot randomized controlled trial of a brief parenting intervention in low-resource settings in Panama. Prevention Science. 2015;16:707–717. doi: 10.1007/s11121-015-0551-1. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behavior Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Minuchin P. Families and individual development: Provocations from the field of family therapy. Child Development. 1985;56:289–302. doi: 10.2307/1129720. [DOI] [PubMed] [Google Scholar]
- Morrill MI, Hines DA, Mahmood S, Cordova JV. Pathways between marriage and parenting for wives and husbands: The role of coparenting. Family Process. 2010;49:59–73. doi: 10.1111/j.1545-5300.2010.01308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray L, Halligan SL, Adams G, Patterson P, Goodyer IM. Socioemotional development in adolescents at risk for depression: The role of maternal depression and attachment style. Development and Psychopathology. 2006;18:489–516. doi: 10.1017/S0954579406060263. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Teubert D. Effects of parenting education with expectant and new parents: A meta-analysis. Journal of Family Psychology. 2010;24:316–327. doi: 10.1037/a0019691. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Ramchandani PG, Stein A, O’Connor TG, Heron JON, Murray L, Evans J. Depression in men in the postnatal period and later child psychopathology: A population cohort study. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:390–398. doi: 10.1097/CHI.0b013e31816429c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rulison KL, Feinberg M, Gest SD, Osgood DW. Diffusion of intervention effects: The impact of a family-based substance use prevention program on friends of participants. Journal of Adolescent Health. 2015;57:433–440. doi: 10.1016/j.jadohealth.2015.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeh A, De Marcas G, Guri Y, Berger A, Tikotzky L, Bar-Haim Y. Infant sleep predicts attention regulation and behavior problems at 3–4 years of age. Developmental Neuropsychology. 2015;40:122–137. doi: 10.1080/87565641.2014.973498. [DOI] [PubMed] [Google Scholar]
- Sanders MR, Morawska A. Towards a public health approach to parenting. The Psychologist. 2006;19:476–479. [Google Scholar]
- Schafer JL, Olsen MK. Multiple imputation for multivariate missing data problems: A data analysts’ perspective. Multilevel Behavioral Research. 1998;33:545–571. doi: 10.1207/s15327906mbr3304_5. [DOI] [PubMed] [Google Scholar]
- Schulz MS, Cowan CP, Cowan PA. Promoting healthy beginnings: A randomized controlled trial of a preventive intervention to preserve marital quality during the transition to parenthood. Journal of Consulting and Clinical Psychology. 2006;74:20–31. doi: 10.1037/0022-006X.74.1.20. [DOI] [PubMed] [Google Scholar]
- Seifer R, Sameroff AJ, Dickstein S, Hayden LC. Parental psychopathology and sleep variation in children. Child and Adolescent Psychiatric Clinics of North America. 1996;5:715–727. [Google Scholar]
- Sepa A, Frodi A, Ludvigsson J. Psychosocial correlates of parenting stress, lack of support and lack of confidence/security. Scandinavian Journal of Psychology. 2004;45:169–179. doi: 10.1111/j.1467-9450.2004.00392.x. [DOI] [PubMed] [Google Scholar]
- Shapiro AF, Gottman JM, Carrere S. The baby and the marriage: Identifying factors that buffer against decline in marital satisfaction after the first baby arrives. Journal of Family Psychology. 2000;14:59–70. doi: 10.1037/0893-3200.14.1.59. [DOI] [PubMed] [Google Scholar]
- Shepard L, Kagan SL, Wurtz E. Principles and recommendations for early childhood assessments. Washington, DC: National Goals Panel; 1998. [Google Scholar]
- Slep AM, O’Leary SG. Parent and partner violence in families with young children: Rates, patterns, and connections. Journal of Consulting and Clinical Psychology. 2005;73:435–444. doi: 10.1037/0022-006X.73.3.435. [DOI] [PubMed] [Google Scholar]
- Tolan P, Gorman-Smith D, Henry D. Family violence. Annual Review of Psychology. 2006;57:557–583. doi: 10.1146/annurev.psych.57.102904.190110. [DOI] [PubMed] [Google Scholar]
- Van Egeren LA. The development of the coparenting relationship over the transition to parenthood. Infant Mental Health Journal. 2004;25:453–477. doi: 10.1002/imhj.20019. [DOI] [Google Scholar]
- Weissman S, Cohen RS. The parenting alliance and adolescence. Adolescent Psychiatry. 1985;12:24–45. [PubMed] [Google Scholar]
- Wood RG, Moore Q, Clarkwest A, Killewald A, Monahan S. The long-term effects of Building Strong Families: A relationship skills education program for unmarried parents. Washington, DC: U.S. Department of Health and Human Services, Administration for Children and Families; 2012. [Google Scholar]