Abstract
In vitro studies of gastric wound repair typically involves the use of gastric cancer cell lines in a scratch-wound assay of cellular proliferation and migration. One critical limitation of such assays, however, is their homogenous assortment of cellular types. Repair is a complex process which demands the interaction of several cell types. Therefore, to study a culture devoid of cellular subtypes, is a concern that must be overcome if we are to understand the repair process. The gastric organoid model may alleviate this issue whereby the heterogeneous collection of cell types closely reflects that of the gastric epithelium or other native tissues in vivo. Demonstrated here is a novel, in vitro scratch-wound assay derived from human or mouse 3-dimensional organoids which can then be transferred to a gastric epithelial monolayer as either intact organoids or as a single cell suspension of dissociated organoids. The goal of the protocol is to establish organoid-derived gastric epithelial monolayers that can be used in a novel scratch-wound assay system to study gastric regeneration.
Keywords: Immunology and Infection, Issue 135, scratch-wound assay, gastric organoids, stem cells, repair, regeneration, epithelial monolayer
Introduction
The use of scratch-wound assays is a popular method for studying repair and regeneration1,2,3,4,5,6. The proposed methodology may be used to specifically study gastric regeneration and Helicobacter pylori colonization. In the past, gastric cancer cell lines have been used as a means to study Helicobacter pylori (H. pylori) infection1,2 and up until recently gastric cancer cell lines such as AGS cells were favored1,2,3,4. One limitation of the gastric cancer cell cultures is their failure to recapitulate the cellular diversity of the gastric epithelium. To try to address this limitation, demonstrated here is the establishment and transfer of primary human- and mouse-derived 3-dimensional fundic gastric organoids (FGOs) to a gastric epithelial monolayer for wound healing assays based on a modified method first described by Schlaermann et al.7 We demonstrate that gastric epithelial monolayers derived from sheared 3D gastric FGOs or FGO-derived single cells retain a polarized cellular composition that closely represents that of the gastric epithelium in vivo. Given that gastric cancer cell lines do not demonstrate the cell composition this technique displays, the current protocol has an advantage over alternative scratch-wound assay methods. This methodology has been optimized whereby monolayers can be established from whole organoids or from a single cell suspension from dissociated organoids and plated using a basement membrane matrix or collagen-coating. The overall goal of this protocol is to establish an organoid derived gastric epithelial monolayer cultures for a novel wound healing assay.
Protocol
To avoid contamination, perform protocol in its entirety within a sterile tissue culture hood. Human fundic tissue was collected from patients undergoing sleeve gastrectomy according to the approved University of Cincinnati IRB protocol (IRB protocol number: 2015 - 4869). All mouse studies were approved by the University of Cincinnati Institutional Animal Care and Use Committee (IACUC) that maintains an American Association of Assessment and Accreditation of Laboratory Animal Care (AAALAC) facility.
1. Establishing Human-derived 3D Gastric Fundic Organoids
NOTE: This protocol is based upon research previously published in this lab8.
- Prepare 3D organoid media which consists of 50% Wnt-conditioned and 20% R-spondin conditioned media.
- Prepare Wnt conditioned media, culture the L cells in Wnt growth medium (Dulbecco's modified Eagle Medium (DMEM), 10% fetal bovine serum (FBS), 1% Penicillin/streptomycin) for 7 days, harvest the medium, and filter using a 0.22 µm filter.
- Prepare R-spondin conditioned media. Grow a modified HEK-293T R-spondin secreting cell line in R-spondin growth medium (Dulbecco's modified Eagle Medium (DMEM), 10% fetal bovine serum (FBS), 1% Penicillin/streptomycin). Upon attachment after 2 h, change the medium from these cells to OPTIMEM growth medium, 1% Penicillin/Streptomycin. Culture the cells for 7 days. Then harvest the R-spondin conditioned media and filter using a 0.22 µm filter. NOTE: This protocol has been published previously and for a more detailed protocol refer to 6,7,8.
Thaw the growth factor reduced, phenol red-free basement membrane matrix for 16 h on the ice at 4 °C. Collect the tissue in the ice cold Ca2+/Mg2+-free DBPS in a large plastic container. Store on the ice until beginning step 1.4. NOTE: Tissue is collected from patients undergoing sleeve gastrectomy.
Using forceps, wash the tissue vigorously in a sterile beaker containing 100 mL Ca2+/Mg2+-free Dulbecco's Phosphate Buffered Saline (DPBS). Wash for approximately 30 s or until the debris and the blood has been removed. Next, using sterile gauze, wipe away the mucous layer from the epithelium.
Using large forceps, firmly grasp the muscle layer of the tissue and with force, scrape away the epithelium using the large curved hemostatic forceps. Collect the scraped epithelial fragments into a sterile, polystyrene petri dish.
Mince the epithelial tissue into approximately 2.0 x 2.0 mm2 sized fragments using razors to optimize tissue digestion. Wash the tissue fragments with Ca2+/Mg2+ -free DBPS supplemented with antibiotics (Ca2+/Mg2+ -free DPBS, 1% Penicillin/Streptomycin, 0.25 mg/mL Amphotericin B /10 mg/mL Gentamicin, 50 mg/mL Kanamycin), until the wash is free of blood. Perform multiple washes if needed. Discard off the wash by carefully filtering the wash through a sterile gauze into a waste beaker.
Collect washed fragments into a 125 mL glass round bottom flask with a 25 mm stir bar and pre-warmed incubation media (basal media supplemented with 2 mM L-glutamine, 1% Penicillin/Streptomycin, 10 mM HEPES Buffer, 1 mg/mL Collagenase Type 1, 2 mg/mL cell culture grade Bovine Serum Albumin). Seal the round bottom flask with rubber septa.
Insert a 20 G spinal needle into the septa and connect it to an oxygen tank with rubber hosing. To filter out any contaminants, insert tissue paper into the tubing to create a filter. Turn on the oxygen outflow on low. Insert 10 - 15 outflow needles into the septa to avoid the rupture of septa.
Secure the set up to a ring stand using clamps and place it in a water bath calibrated to 37 °C with a stir plate for 30 - 45 min. After the tissue has been incubating for 15 min, remove 50 µL of incubation media and check visually for dissociated glands. If glands are not dense or have not separated from the tissue, leave for an additional 5 - 10 min.
Immediately following incubation, add 50 mL pre-heated DMEM/F12 to incubation media using a sterile serological pipette or by pouring directly into the incubation mixture.
Filter the gland mixture through a sterile gauze into four 50 mL conical tubes. Keep the filtrate on ice for 15 min to allow extracted glands to settle to the bottom of the conical tube. Be careful not to disturb the settled glands, remove and discard off the top 40 mL of supernatant using a serological pipette. Resuspend the remaining 10 mL in 10 mL of DPBS supplemented with antibiotics.
Distribute the mixture evenly into 5 mL cell culture test tubes. Centrifuge for 5 min at 65 x g at 4 °C and remove the supernatant carefully using a pipette. Resuspend the gland pellet in thawed basement membrane matrix using either a pipette or a 200 µL wide pipette tip. Mix until homogeneous. NOTE: It is crucial to perform this step on the ice and to avoid polymerization of basement membrane matrix while mixing. Additionally, it is important to visually inspect the gland density by sampling for 50 µL. The optimal density is ~70% confluency.
Next, plate the glands in 50 µL of basement membrane matrix using a wide-tipped pipette. Avoid producing any bubbles while plating.
To allow basement membrane matrix to polymerize, incubate for 10 - 15 min at 37 °C. If plating in a 12-well culture plate, add 1 mL of hFGO media (Advanced Dulbecco's modified Eagle medium/F12 medium supplemented with 2mM L-glutamine, 1% Penicillin/Streptomycin, 0.25 mg/mL Amphotericin B /10 mg/mL Gentamicin, 50 mg/mL Kanamycin, 10 mM HEPES Buffer, 1 mM n-Acteylcystine, 1 x N2, 1 x B27, 50% Wnt-conditioned medium, 20% R-spondin-conditioned medium supplemented with 100 ng/mL bone morphogenetic protein inhibitor, 1 nM gastrin, 50 ng/mL Epidermal Growth Factor, 200 ng/mL Fibroblast growth factor 10, 10 mM Nicotinamide, and 10 µM Y-27632 ROCK inhibitor) per well. If not using a 12-well culture plate add enough media to submerge the basement membrane matrix bubble.
Culture the cells at 37 °C in a 5% CO2 humidified cell culture incubator. Change media every 4-5 days.
2. Establishing Mouse-derived 3D Gastric Fundic Organoids
NOTE: This protocol has been previously published 6. Thaw basement membrane matrix on the ice and prepare all reagents before beginning.
Sacrifice mice using a method approved by the research institution where research is being performed. Remove the stomach from the mouse and dissect according to the previously published protocols 6. Wash in 20 mL ice cold Ca2+/Mg2+-free DBPS. NOTE: C57BL/6 mice, aged 8 - 10 weeks, are used for fundic gastric organoid cultures. Mice were euthanized by inhalation of carbon dioxide followed by manual cervical dislocation before stomach removal.
Strip the muscle layer from the stomach and any visible blood vessels as previously published 6.
Separate the fundus from the antrum and forestomach using a sterile razor blade. Cut fundus using small surgical scissors into fragments approximately 2.0 x 2.0 mm. Using forceps, collect the fragments into a 15 mL conical tube containing EDTA incubation buffer (Ca2+/Mg2+-free DPBS, 5mM EDTA) and incubate at 4 °C for 2 h with gentle agitation.
In a sterile hood, leave conical tube and fragments on ice for approximately 5 min. Use a pipette to remove as much incubation buffer as possible leaving fragments untouched. Add 5 mL shaking buffer (1 g D-Sorbitol, 1.47 g sucrose in 100 mL Ca2+/Mg2+-free DPBS) and shake by hand with a force for 2 min. Allow the large fragments to settle and with haste, using a 1000p pipette, remove the small fragments that have yet to settle in the top layer.
Spin the removed fragments for 5 min at 4 °C at 65 x g.
While avoiding air bubbles, remove the supernatant, resuspend in the basement membrane matrix and mix until it is homogenous.
Use a wide tip pipette to plate the basement membrane matrix at 50 µL per well and then incubate at 37 °C for 20 min.
Add enough mFGO growth media (Advanced Dulbecco's modified Eagle medium/F12 medium supplemented with 2mM L-glutamine, 1% Penicillin/Streptomycin, 10 mM HEPES Buffer, 1mM n-Acteylcystine, 1 x N2, 1 x B27, 50% Wnt-conditioned medium, 20% R-spondin-conditioned medium supplemented with 100 ng/mL bone morphogenetic protein inhibitor, 10 nM gastrin, 50ng/mL Epidermal Growth Factor, 10 ng/mL Fibroblast growth factor 10, and 10 µM Y-27632 ROCK inhibitor) to submerge the bubble.
Culture the cells at 37 °C, 5% CO2 humidified cell culture incubator. Change the media every 4 - 5 days.
3. Collagen Coating for 2D Transfer
NOTE: Perform all procedures in a sterile tissue culture hood unless otherwise specified. Begin collagen coating 24 h before transferring 3D organoids to the monolayer. Keep the rat tail collagen on the ice and shielded from light. Collagen coated plates are good for up to 2 weeks. If not using the coated plates immediately, wrap the plate in parafilm and store at 4 °C until needed.
Dilute the rat tail collagen to 50 µg/mL using 20 mM acetic acid.
Sufficiently cover the surface of the well with diluted collagen. For one well in a standard 12-well plate, coat with approximately 1 mL of collagen. Leave overnight at room temperature in a sterile hood.
Wash twice with 1 mL Ca2+/Mg2+-free DPBS per well and leave uncovered for 2 h at room temperature in a sterile hood.
4. Basement Membrane Matrix Coating for 2D Transfer
NOTE: Perform all procedures in a sterile tissue culture hood unless otherwise specified. Begin basement membrane matrix coating 2 h before transferring 3D organoids to the monolayer. Keep the basement membrane matrix on ice. Coated plates are to be used immediately and cannot be stored for an extended period of time.
Dilute the basement membrane matrix in a 15 mL conical tube with a cell culture grade water at a 1:10 ratio. Dilute on ice.
Using a pipette add 100 µL of diluted basement membrane matrix to each well of a standard 12-well plate. Using a cell scraper, evenly distribute the diluted basement membrane matrix throughout the well for an even coat.
Incubate at 37 °C for 1 h.
Remove the residual water using a pipette and dry at room temperature for 1 h before transferring 3D organoids.
5. Transfer of 3D m/hFGOs to 2D Gastric Epithelial Cell Monolayers
After 3D mouse- or human-derived FGOs have been cultured for 6 - 7 days, begin the transfer of 3D organoids to the 2D monolayer. NOTE: For each well of a monolayer required it is recommended to use 300 intact organoids or single cells derived from 300 organoids. In a robust culture it is expected to obtain approximately 150 organoid/well within a 12 well culture plate.
Be sure plates are coated before transferring. NOTE: The basement membrane matrix coated plates have a translucent gel layer, however, collagen coated plates will not have any obvious indication of the coating.
Dislodge the 3D basement membrane matrix bubble from the plate by directly pipetting 1 mL sterile Ca2+/Mg2+-free DBPS onto the center of the bubble.
Using a pipette, collect the basement membrane matrix and organoid mixture into cell culture test tubes. Collect at a ratio of 2 basement membrane matrix bubbles per tube. Centrifuge for 5 min at 40 x g and 4 °C.
Using a vacuum system, remove the supernatant and as much basement membrane matrix as possible. Resuspend in 4 mL of Ca2+/Mg2+-free DBPS, remove the supernatant, and repeat 2 - 3 times. For the whole organoid transfer protocol, proceed to step 5.10. Continue to step 5.7 for the single cell suspension protocol.
Pre-warm cell detachment solution to 37 °C and add 1 mL to each test tube. Gently mix by either inverting tubes or pipetting up and down with a pipette. Incubate for 10 min at 37 °C.
Add 2 mL of Ca2+/Mg2+-free DBPS directly to each test tube.
Use a 26 G needle and syringe the mixture 2 - 3 times. Visually check for single cells. Syringe 1 - 2 more times if there are still organoids or clusters of cells.
Centrifuge at 40 x g for 5 min at 4 °C. Resuspend the pellet in 2D FGO media (2D mouse FGO growth medium: Advanced Dulbecco's modified Eagle medium/F12 medium supplemented with 2mM L-glutamine, 10 mM Penicillin/Streptomycin, 10% Fetal Calf Serum, 10 mM HEPES Buffer, 1 x N2, 1 x B27, supplemented with 10 nM gastrin, 50 ng/mL Epidermal Growth Factor, 1 µM TGF-β inhibitor, and 10 µM Y-27632 ROCK inhibitor. 2D human FGO growth medium: Advanced Dulbecco's modified Eagle medium/F12 medium supplemented with 2mM L-glutamine, 1% Penicillin/Streptomycin, 10 mM HEPES Buffer, 10% Fetal Calf Serum, 10 mM Nicotinamide, 1 x N2, 1 x B27, supplemented with 50 mg/mL Kanamycin, 50 ng/mL Epidermal Growth Factor, and 10 µM Y-27632 ROCK inhibitor, 1 µM TGF-β inhibitor).
Plate the resuspension on coated plates. Incubate plates at 37 °C. Replace media every 4 days or earlier if media turns yellow. Monolayer requires approximately 4 days to form.
6. Scratch Wound Assay Using 2D Gastric Epithelial Cell Monolayers
Using a razor blade, scratch the monolayer when the culture has reached 100% confluency.
Fix monolayers using 3.7% formaldehyde for 15 min at room temperature. Permeabilize with 0.5% non-ionic detergent/PBS for 20 min at room temperature.
Next block monolayers with 2% donkey serum for 1 h at room temperature and incubate with 1:1000 dilution of H+,K+-ATPase primary antibody overnight at 4 °C, wash with 0.1% non-ionic detergent/PBS and incubate with 1:100 dilution of donkey anti-mouse 488 secondary antibody and 10μg/mL of Hoechst cell nuclei stain for 1 h at room temperature.
To identify the surface mucous pit cells in 2D human-derived gastric monolayer cultures, stain cells with 20 μg /mL of Ulex europaeus (UEAI) FITC conjugate. Image monolayers on a confocal microscope.
Take images of wound every few h. Scratch will re-epithelialize between 24 - 48 h depending on the quality of the monolayer and variation between patients.
Representative Results
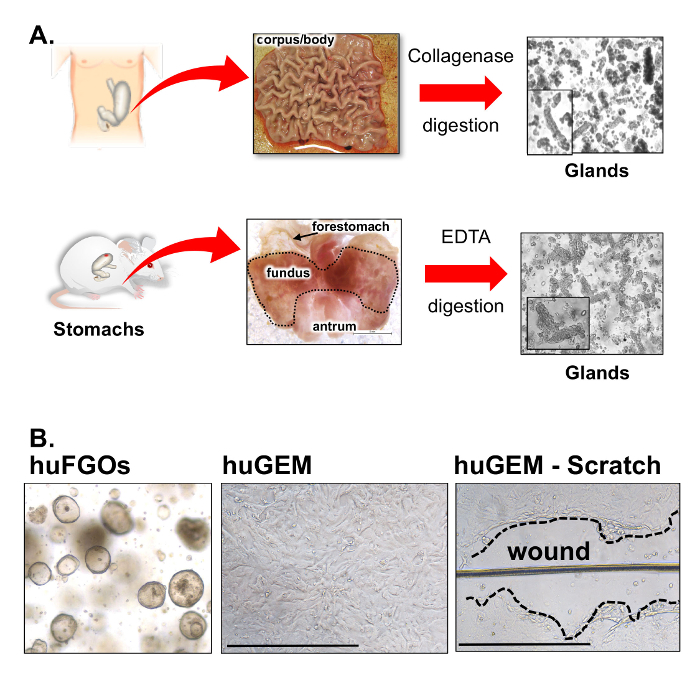
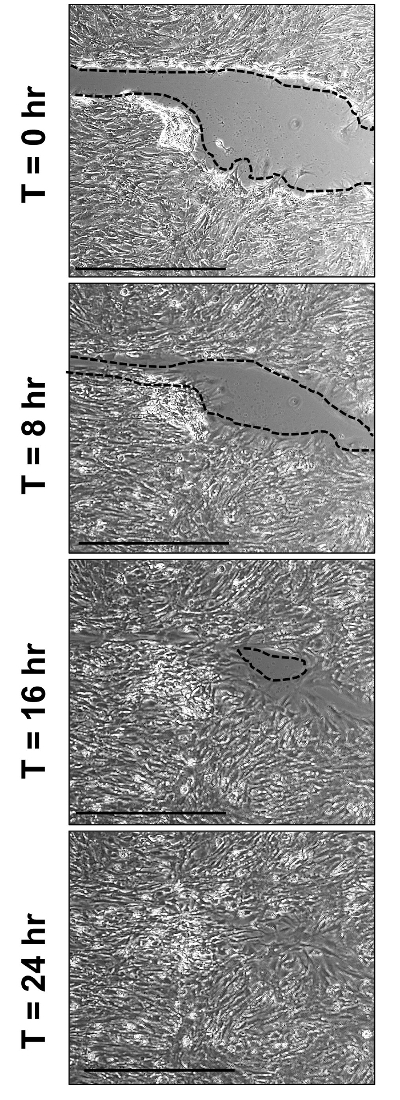
Organoids were derived from either the corpus/body of the human or fundus of the mouse stomach tissues (Figure 1A). After either collagenase or EDTA digestion of human- or mouse-derived stomach tissue respectively, glands are embedded into basement membrane matrix and cultured for 6 - 7 days (Figure 1A). Figure 1B demonstrates the formation of human-derived gastric organoids (huFGOs) that have then been transferred to a gastric epithelial monolayer (huGEM) on basement membrane matrix-coated chamber slides. After 4 days of culture, confluent huGEMs were used for scratch wound assays (Figure 1B). Images collected from a time lapse analysis of the huGEM showed wound closure within the culture over a period of 24 hours (Figure 2).
HuGEMs were found to express the major cell lineages found in the native stomach tissue. Immunofluorescence staining revealed the expression of a polarized E cadherin-positive monolayer that consisted of the parietal (Figure 3B, C) and the surface mucous (Figure 3B, D) cells. PCR analysis using RNA collected from these monolayers confirmed the expression of parietal and surface mucous cells, in addition to the chief and mucous neck cells (Figure 3E). Confluent huGEMs also expressed few proliferating cells (Figure 3F). Analysis of these major cell lineages within the scratch wound assay revealed sustained expression of parietal, chief, mucous neck surface mucous cells over a 24 hour time period (Figure 4A, B). Collectively, these data demonstrate the use of huGEMs as novel culture system to study gastric regeneration in vitro.
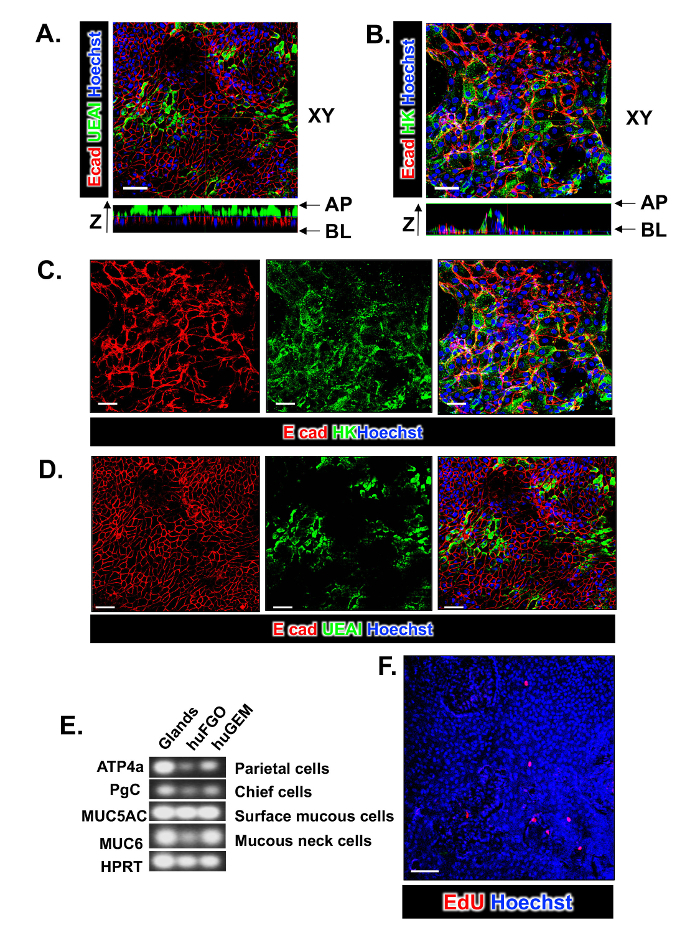
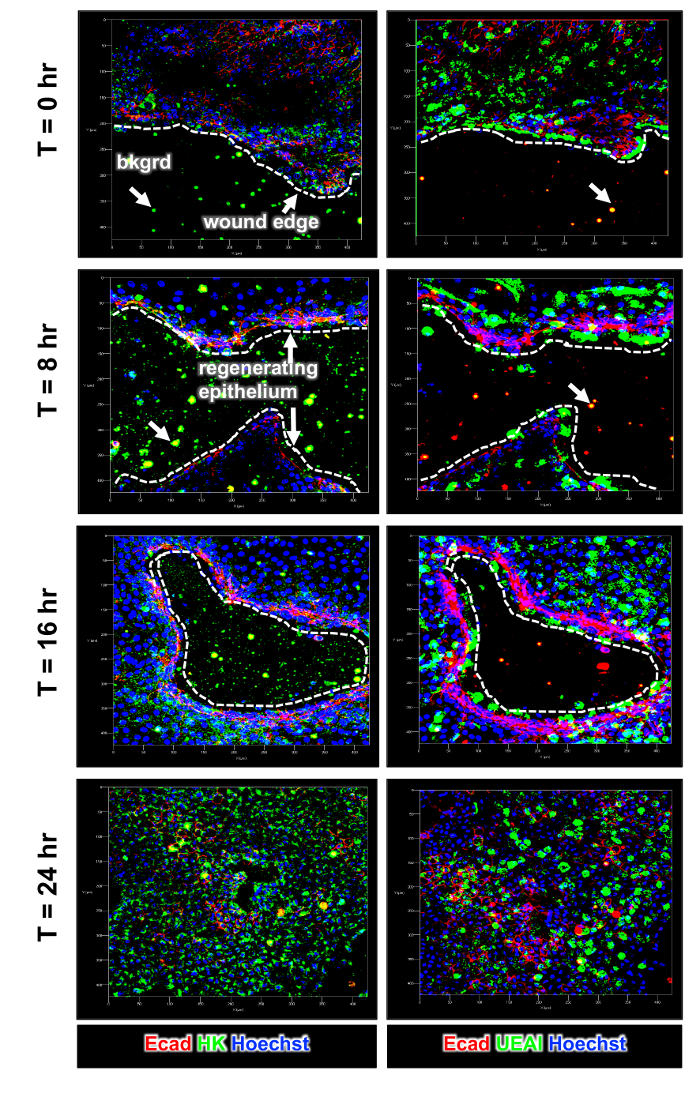
Figure 1: Generation of human-derived gastric organoids (huFGO) and primary gastric epithelial monolayers (huGEM). (A) Representative images of human gastric tissue and mouse stomach used to generate glands for organoid culture. Outlined area indicates fundic region of the mouse stomach. (B) Generation of human-derived gastric organoids (huFGOs) that are used for the culture of human-derived gastric epithelial monolayers (huGEMs). Representative image of huGEM after scratch showing the wounded area. Scale bar = 500 μm Please click here to view a larger version of this figure.
Figure 2: Scratch-wound assay. Representative images collected from a time lapse experiment using huGEM 0, 8, 16, and 24 h after scratch wound. Scale bar = 500 μm Please click here to view a larger version of this figure.
Figure 3: Expression of major cell lineages in huGEM cultures. Immunofluorescence staining of huGEM cultures demonstrating the expression of (A) E cadherin (Ecad, red), surface mucous cells (UEAI, green) and nuclei (Hoechst, blue), and (B) E cadherin (Ecad, red), parietal cells (HK, green) and nuclei (Hoechst, blue). Separate channels are shown in (C) and (D). (E) RT-PCR was performed using RNA extracted from huGEMs for the expression of H+K+-ATPase (ATP4a), pepsinogen C (PgC), MUC5AC, and MUC6. (F) Proliferating cells within the huGEM culture determined by EdU (red) uptake. Scale bar (A-D) = 50 μm, Scale bar (F) = 100 μm. Please click here to view a larger version of this figure.
Figure 4: Changes in cell lineage expression in the scratch-wound assay. Immunofluorescence staining of huGEM cultures demonstrating the expression of E cadherin (Ecad, red) or surface mucous cells (UEAI, green) or parietal cells (HK, green) and nuclei (Hoechst, blue) using slides collected from huGEM cultures 0, 8, 16, and 24 hrs post scratch-wound. Bkgrd = background staining of basement membrane matrix on slides. XY-axis scale bar from 0 - 400 μm. Please click here to view a larger version of this figure.
| Mouse 3D Media | Stock Solution | Working Concentration |
| nAcetylcysteine | Powder | 1 mM |
| Gastrin | 10 µM | 10 nM |
| EGF | 500 µg/mL | 50 ng/mL |
| Noggin | 100 µg/mL | 100 ng/mL |
| FGF10 | 100 µg/mL | 100 ng/mL |
| YCMD | 10 mM | 10 µM |
| B27 | 50x | 1x |
| N2 | 100x | 1x |
| Pen/Strep | 1 M | 10 mM |
| HEPES | 1 M | 10 mM |
| Glutamax | 200 mM | 2 mM |
| WNT | 50% v/v | |
| R-Spondin | 10% v/v |
Table 1: Mouse 3D Media Components.
| Mouse 2D Media | Stock Solution | Working Concentration |
| FCS | 100% | 10% |
| YCMPD | 10 mM | 10 µM |
| Gastrin | 10 µM | 10 nM |
| EGF | 500 µg/mL | 50 ng/mL |
| B27 | 50x | 1x |
| N2 | 100x | 1x |
| Pen/Strep | 1 M | 10 mM |
| HEPES | 1 M | 10 mM |
| Glutamax | 200 mM | 2 mM |
| TGF-β inhibitor | 10 mM | 1 µM |
Table 2: Mouse 2D Media Components.
| Human 3D Media | Stock Solution | Working Concentration |
| Nicotinamide | Powder | 10 mM |
| nAcetylcysteine | Powder | 1 mM |
| Gastrin | 10 µM | 1 nM |
| EGF | 500 µg/mL | 50 ng/mL |
| Noggin | 100 µg/mL | 100 ng/mL |
| FGF10 | 100 µg/mL | 200 ng/mL |
| YCMD | 10 mM | 10 µM |
| B27 | 50x | 1x |
| N2 | 100x | 1x |
| Pen/Strep | 1 M | 10 mM |
| HEPES | 1 M | 10 mM |
| Glutamax | 200 mM | 2 mM |
| Kanamycin | 1 M | 10 mM |
| Amphotericin B/Gentamycin | 125 µg/mL | 1 mM |
| WNT | 50% v/v | |
| R-Spondin | 10% v/v |
Table 3: Human 3D Media Components.
| Human 2D Media | Stock Solution | Working Concentration |
| FCS | 100% | 10% |
| YCMPD | 10 mM | 10 µM |
| Gastrin | 10 µM | 1 nM |
| EGF | 500 µg/mL | 50 ng/mL |
| B27 | 50x | 1x |
| N2 | 100x | 1x |
| Pen/Strep | 1 M | 10 mM |
| HEPES | 1 M | 10 mM |
| Glutamax | 200 mM | 2 mM |
| TGF-β inhibitor | 10 mM | 1 µM |
| Nicotinamide | Powder | 10 mM |
| Kanamycin | 1 M | 10 mM |
Table 4: Human 2D Media Components.
| Experimental Problem | Troubleshooting Tip |
| Monolayers fail to form from organoids | 1) Optimal culturing conditions for this protocol vary between experimental needs. Human and mouse monolayers derived from organoids should be cultured using diluted basement membrane matrix when using glass or plastic culture dishes. However, rat tail collagen is optimal for monolayer experiments of mouse or human origin that require polyester membrane inserts. 2) Optimal culturing conditions vary depending on the experimental set up. Cultures using single cell suspension are ideally cultured with 3D FGO media whereas intact organoids are cultured with 2D FGO media. |
| Monolayers derived from aged patients (>55 years) or mice (>18 months) failed to grow and reach confluency | If using stomach tissue collected from aged mice (>18 months) or patients (>55 years) the density of organoids used for the generation of the monolayer should be doubled given that the growth efficiency of organoids is decreased. |
| Organoids fail to form from glands | It is recommended that fresh (newly purchased if possible) gastrin be used. Use freshly re-suspended gastrin every 4 months. |
| Organoids fail to attach and form monolayers | Ensure that efficient removal of basement membrane matrix has been achieved after harvesting organoids for the transfer to culture plates for monolayers. |
| Cultures derived from aged patients (>55 years) or mice (>18 months) fail | During the digestion and incubation periods, 15 - 30 min of initial incubation followed by 5 min intervals of incubation as necessary is sufficient. It should be noted that patients greater than 55 years of age may have glands that are more easily dissociated and therefore require less digestion. Similarly, FGOs derived from aged patients have displayed slower growth time and increased sensitivity to centrifugation. To obtain the best results, limit any excess centrifugation when working with aged tissue and replace media in a timely manner. |
Table 5: Troubleshooting Tips. Encountered issues and recommended resolutions for optimal establishment and culture of human or mouse gastric monolayers.
Discussion
The current protocol details the establishment of human- and mouse-derived gastric epithelial monolayers that can be used for scratch-wound assays. The protocol depends on the concept of resident stem cell isolation from primary human (or mouse) tissues and is a modified protocol first published by Schlaermann et al7. In particular, we have optimized the protocol here to establish a confluent and polarized gastric epithelial monolayer which expresses the major cell lineages which can be found within the gastric epithelium in vivo. Gastric ulcer repair is a complex process that involves tissue re-epithelialization, regeneration, and proliferation9,10,11. In particular, our laboratory has reported that regeneration of the gastric epithelium coincides with the emergence of spasmolytic polypeptide/trefoil factor (TFF) 2-expressing metaplasia (SPEM) at the ulcer margin within the regenerating gastric glands12,13. SPEM is defined as the transdifferentiation of the chief cell lineage into a mucous cell metaplasia14 that emerges with injury and disappears when the mucosa returns to its normal cellular composition12. Thus, to study such a mechanism in an in vitro system, it is essential that the major cell lineages, such as the chief cells, are present within the culture.
The use of scratch-wound assays have been extensively used for the study of repair and regeneration, and up until recently, gastric cancer cell lines were used1,2,3,4. While fundamental mechanisms have been revealed using gastric cancer cells lines, these cultures are transformed and lack the cellular diversity of the native stomach tissue. HuGEMs are shown to retain a polarized and diverse cellular composition that closely recapitulates the gastric epithelium in vivo. Additionally, after reaching confluency huGEM cultures can be maintained for up to one month in optimal conditions. Extended cultures allow for long term experiments. Thus, future applications of the huGEMs that may be considered include monolayer/immune cell co-cultures and long term experiments for the study of Helicobacter pylori pathogenesis.
There are important technical aspects to note in the current protocol. The first technical point is that the choice of basement membrane component varies depending on the cell culture surface that is to be used for experiments. To ensure that optimum monolayer conditions are reached, it is recommended that collagen is used when experiments with monolayers require plates with polyester membrane inserts. However, if monolayer experiments require glass or plastic culture surfaces, diluted basement membrane matrix is the optimal choice of coating. Second, the density of organoids required to reach a confluent monolayer must be adjusted depending on the age of the patient from which the gastric tissue is collected. For tissue collected from aged mice (>18 months) or patients (>55 years), the organoid density used should be increased twofold when transferring to a monolayer due to the decreased growth capacity in aged individuals. During digestion and incubation of human tissue derived from aged patients, glands may be more susceptible to dissociation and centrifugation and therefore: 1) should be centrifuged as sparingly as possible, 2) media replaced diligently, and 3) during digestion incubations of 15 to 30 minutes with incremental digestions of 5 minutes afterwards will decrease the likelihood of over digestion. Finally, when forming monolayers from organoid-derived single cell suspensions, 3D FGO media is most optimal for proper formation of monolayers whereas when culturing from intact organoids, 2D FGO media has been observed to yield the highest efficiency.
Disclosures
The authors have nothing to disclose.
Acknowledgments
This work was supported by NIH (NIDDK) 5 R01 DK083402-07 grant (YZ).
References
- Nagy TA, et al. Helicobacter pylori regulates cellular migration and apoptosis by activation of phosphatidylinositol 3-kinase signaling. J Infect Dis. 2009;199(5):641–651. doi: 10.1086/596660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mnich E, et al. Impact of Helicobacter pylori on the healing process of the gastric barrier. World J Gastroenterol. 2016;22(33):7536–7558. doi: 10.3748/wjg.v22.i33.7536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, et al. Bm-TFF2, a toad trefoil factor, promotes cell migration, survival and wound healing. Biochem Biophys Res Commun. 2010;398(3):559–564. doi: 10.1016/j.bbrc.2010.06.118. [DOI] [PubMed] [Google Scholar]
- Crabtree J. Role of cytokines in pathogenesis of Helicobacter pylori-induced mucosal damage. Dig Dis Sci. 1998;43(Supplement):46S–53S. [PubMed] [Google Scholar]
- Riahi R, Yang Y, Zhang DD, Wong PK. Advances in wound-healing assays for probing collective cell migration. J Lab Autom. 2012;17(1):59–65. doi: 10.1177/2211068211426550. [DOI] [PubMed] [Google Scholar]
- Zhang M, Li H, Ma H, Qin J. A simple microfluidic strategy for cell migration assay in an in vitro wound-healing model. Wound Repair Regen. 2013;21(6):897–903. doi: 10.1111/wrr.12106. [DOI] [PubMed] [Google Scholar]
- Schlaermann P, et al. A novel human gastric primary cell culture system for modelling Helicobacter pylori infection in vitro. Gut. 2016;65(2):202–213. doi: 10.1136/gutjnl-2014-307949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertaux-Skeirik N, et al. CD44 plays a functional role in Helicobacter pylori-induced epithelial cell proliferation. PLoS Pathog. 2015;11(2):e1004663. doi: 10.1371/journal.ppat.1004663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarnawski AS. Cellular and molecular mechanisms of gastrointestinal ulcer healing. Dig Dis Sci. 2005;50(Suppl 1):S24–S33. doi: 10.1007/s10620-005-2803-6. [DOI] [PubMed] [Google Scholar]
- Wright NA, Pike C, Elia G. Induction of a novel epidermal growth factor-secreting cell lineage by mucosal ulceration in human gastrointestinal stem cells. Nature. 1990;343:82–85. doi: 10.1038/343082a0. [DOI] [PubMed] [Google Scholar]
- Wright CL, Riddell RH. Histology of the stomach and duodenum in Crohn's disease. Am J Surg Pathol. 1998;22(4):383–390. doi: 10.1097/00000478-199804000-00001. [DOI] [PubMed] [Google Scholar]
- Engevik AC, et al. The Development of Spasmolytic Polypeptide/TFF2-Expressing Metaplasia (SPEM) During Gastric Repair Is Absent in the Aged Stomach. CMGH. 2016. In Press. [DOI] [PMC free article] [PubMed]
- Bertaux-Skeirik N, et al. CD44 variant isoform 9 emerges in response to injury and contributes to the regeneration of the gastric epithelium. Journal of Pathology. 2017;242(4):463–475. doi: 10.1002/path.4918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nam KT, et al. Mature chief cells are cryptic progenitors for metaplasia in the stomach. Gastroenterology. 2010;139(6):2028–2037. doi: 10.1053/j.gastro.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]


