Abstract
The following is a training platform to allow robotic surgeons to develop the skills necessary to lead an interprofessional team in emergency undocking of a robotic system. In traditional robotic training for surgeons, a brief web based overview of performing an emergency undocking is provided during initial introductory training to the robotics system. During such a process, there is no training in delineation of interdisciplinary roles for operating room (OR) personnel. The training presented here uses formative simulation and debriefing followed by a lecture. For the simulation, a modified gynecologic simulator is draped in a steep trendelenburg position consistent with most gynecologic laparoscopic surgery. The training torso is modified using tubing hooked to pressure bags of red food colored IV fluid used to simulate a catastrophic vessel injury on demand. Positioned throughout the operating room setting is an interprofessional team consisting of embedded standardized persons (ESPs) to fulfill the roles of a circulating nurse, scrub nurse, anesthesiologist, and bedside assist surgeon. Robotic surgeons are presented a case scenario necessitating emergency undocking, and given control of the robotic instruments. The scenario is terminated following either successful completion of an emergency undock, or at five minutes due to the emergent nature of the case. A debriefing session with hands on training of the steps to emergency undocking, necessary equipment, troubleshooting techniques, and operating room personnel roles follows the simulation. The learners are presented with a short lecture reemphasizing the material presented in the debriefing for their own self-study. This training results in improved time accessing the patient, improved knowledge, confidence, and completion of critical actions, and can be replicated in most institutions. All robotic surgeons should be able to demonstrate competence in this crucial intervention. A limitation of the curriculum is ability to access the in-situ environment for training purposes.
Keywords: Medicine, Issue 135, Robotic surgery, simulation, surgical education, emergency undocking, training, curriculum, gynecology
Introduction
The purpose of this training is to improve robotic surgeons' confidence, knowledge, and proficiency of performing an emergency undocking of the robotic system, and to improve the surgeon's ability to lead an interprofessional team through effective communication of clearly delineated roles in the event of an emergency undocking. Despite the abundance of personnel and equipment in the operating room, there is a lack of experience managing these crises1,2. Current training requirements of online course work and a short period of proctored cases leave many surgeons feeling their training is inadequate3. Regardless of these feelings of inadequacy, prior studies have established that surgeons will encounter at least 1 OR emergency in their career4. Strategies to improve on these feelings of inadequacy include increasing usage of simulation training5. It is well established that simulation training is becoming inseparable from surgical education6. Prior studies have determined that simulation-based team training is an invaluable tool in helping learners overcome cognitive and behavioral gaps in surgical education and is useful as a tool to allow trainees in sessions with other team members the ability to demonstrate baselines for knowledge and communication skills, while improving performance following combining simulation exercises and debriefing4,7,8,9,10,11.
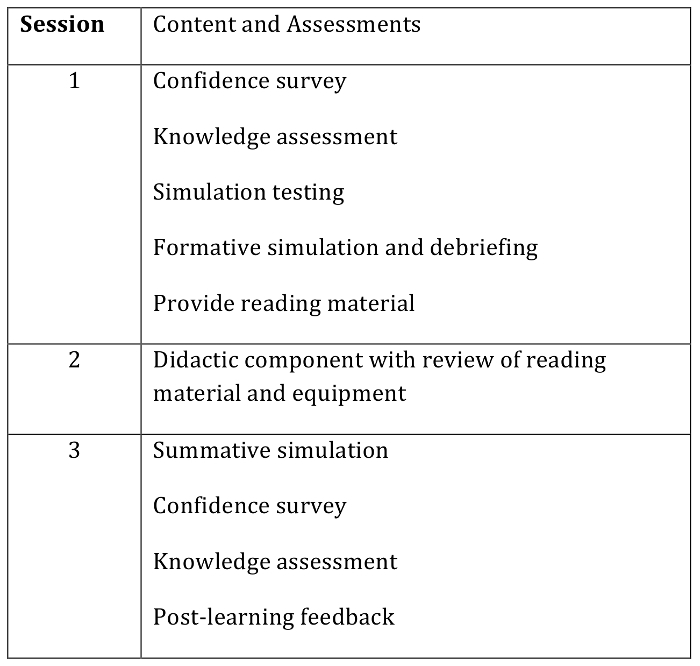
To improve robotic crisis management, various simulator-training scenarios have been developed1,12,13. While there have been numerous studies examining the effects of team training, there is a dearth of research analyzing training on complex OR scenarios4. During complex OR emergencies, checklists and the clear delineations of roles through effective communication are of paramount importance. In robotic surgery, there is a paucity of literature available outlining protocols or training for this procedure14. Simulation has proven effective in validating checklists for use during operating-room crises to improve surgical care15. Here, we present a training curriculum to allow robotic surgeons to develop the skills necessary to lead an interprofessional team in an emergency undocking of a robotic system. Implementation of this curriculum takes place over three sessions in an in-situ environment, as laid out in Figure 1, and can be used to provide training, demonstrate skills for credentialing, and is easily reproducible in any hospital with a robotic system.
Protocol
The IRB determined that this project was exempt from IRB review in accordance with federally defined categories of exempt review per 45 CFR 46.101 Category 2.
1. Gather and Prepare Materials
Collect materials for the training curriculum, including a robotic system with 2 training arms (see Table of Materials), 3 trocars, and a laparoscope.
In the hollow training torso, create at least 3 separate incisions with a scalpel to place laparoscopic instrument trocars. Ensure that the incisions are consistent with those found in robotic surgery, i.e., one above the umbilicus, and one in each the right and left lower quadrant large enough to accommodate a trocar.
- To simulate a vessel and subsequent vessel injury, create a vessel using rubber tubing. Tubing from a water seal chest drain functions well.
- Cut a separate tube for the vena cava and descending aorta.
- Connect two shorter pieces replicating the right and left common iliac veins and two shorter pieces replicating the common iliac arteries to the vena cava and aorta, respectively, using a Y-connector.
- Create a notch at the distal end of the common iliac artery to allow for simulated blood to escape in the case of a vessel injury.
- Place the vessels against the posterior wall of the torso and secure using glue. Protrude the access point to the vessel through the cephalad portion of the torso to allow for instillation of red food colored fluid.
- Color as necessary for realism with oil base red and blue paint for artery and vein respectively. Coat with a protective clear enamel spray for durability.
Obtain a 1-liter bag of IV fluid. Inject red food coloring until the fluid has a color consistent with blood. Hook this bag to the previously assembled vessel.
Drape the torso with operating room drapes used for laparoscopic surgery or laparotomy. Ensure that the drape covers the entire OR table.
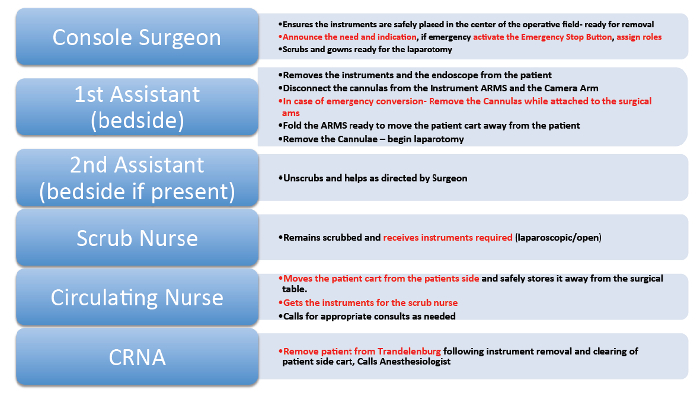
Have embedded standardized persons (ESPs) or confederates fulfill the roles laid out in the emergency undocking protocol (Figure 2). A minimum of 4 individuals is required. Alternatively, OR personnel can be employed to perform their actual roles.
2. Setup of the Operating Room
Place the training torso, complete with vessel and IV tubing, and connect it to an IV fluid bag on the OR table. Place the table in a steep trendelenburg position, then drape using OR drapes.
Place the laparoscopic trocars into the training torso through the incisions made previously. Move the robotic patient side cart to the bedside, and attach robotic arms to trocars. Once attached, dock robotic training instrument and camera to torso using trocars.
Place ESPs or OR staff in desired roles as described in Figure 2. Have the surgeon console on and ready for surgeon to assume control of robotic instruments.
3. Simulation and Debriefing
Have the surgeon enter the room and position at the surgeon's console. Instruct the surgeon to adjust positional settings, but not take control of the instruments until completion of orientation to the case.
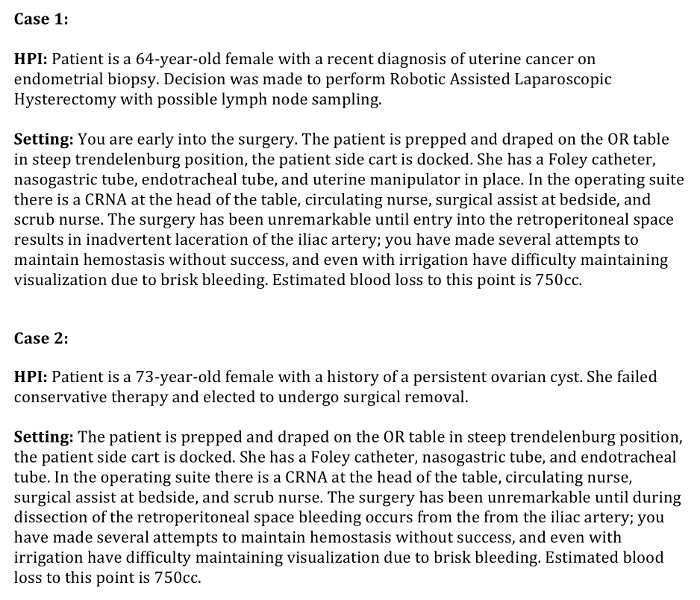
Introduce the ESPs or OR staff to the surgeon. Read one of the case stems presented in Figure 3. Then, instruct the surgeon to take control of the instruments following completion of the case stem.
Have the anesthesia ESP initiate bleeding from the vessel via pressure bag or manual pumping of fluid bag once the case stem is completed. The IV tubing should be wide open, allowing for brisk bleeding. Allow the surgeon up to 5 minutes to complete emergency undocking.
Following the case (or after 5 minutes), proceed with debriefing and didactic component of the scenario and procedure. During the debriefing emphasize key points of personnel roles as listed in Figure 2, key equipment including instrument arms and patient side cart, and use of closed loop communication.
Reposition ESPs or OR staff, and run a second case to reinforce the lessons taught during debriefing. Following the case, reiterate any points missed during the second case.
Representative Results
By incorporating this curriculum as outlined in Figure 1 and the undocking protocol outlined in Figure 2 during training in robotic-assisted surgery, our study demonstrated an overall improvement in the confidence, knowledge, and critical actions performed by the surgeon as demonstrated in Figure 3. Baseline measurements in knowledge and confidence were collected on all participants immediately prior to participation in the curriculum. A 20 question multiple-choice exam and a 6-item Likert confidence scale ranging from very uncomfortable to very comfortable provided this baseline. This was illustrated by the significant increase in the baseline level of knowledge of robotic surgeons after our training curriculum was implemented (p = 0.001; Wilcoxon signed rank test of median change equal to 0), and our results also demonstrated an increase in the confidence of surgeons when faced with an emergency undocking after completion of our curriculum (p = 0.003) (Table 1, Figure 4). This may indicate that utilizing robotic surgery simulation during training can be advantageous to robotic surgeons by boosting confidence and familiarity with the emergency protocol. There was also an improvement in the undocking times (p <0.001) and increase in the critical actions performed out of 7 possible measured actions (p = 0.002) (Table 2, Figure 4). This likely represents a combination of the robotic surgeon's ability to recognize the need for an emergency undocking sooner and having the opportunity to simulate the entire emergency undocking process while leading a team in an in situ environment with immediate feedback from content experts after completing the curriculum. It is important to be consistent in training personnel in the execution of this protocol in order to ensure consistency among surgeons and to maximize effectiveness in a real life scenario.
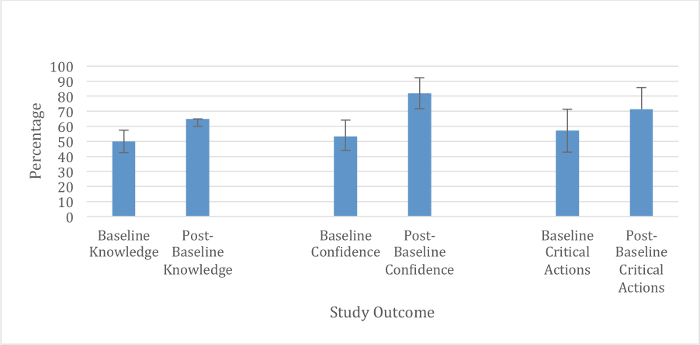
Figure 1: Curricular outline of the pre-training simulation, debriefing and didactic component, and post-training simulation. Please click here to view a larger version of this figure.
Figure 2: Emergency undocking roles. Please click here to view a larger version of this figure.
Figure 3: Case stems read to initiate simulation. Please click here to download this file.
Figure 4: Summary graph of statistically significant results (median ± interquartile range). Please click here to view a larger version of this figure.
| Study Cohort | |
| Variable/Statistic | (n = 21) |
| Baseline Knowledge Score (out of 20) | |
| Mean (SD) | 10.0 (1.82) |
| Median (IQR) | 10 (8.5 - 11.5) |
| Range | 7 - 13 |
| Post-Baseline Knowledge Score (out of 20) | |
| Mean (SD) | 12.4 (1.29) |
| Median (IQR) | 13 (12 - 13) |
| Range | 9 - 14 |
| Change in Knowledge Score | |
| Mean (SD) | 2.4 (2.20) |
| Median (IQR) | 3 (1 - 4.5) |
| Range | -2 - 5 |
| p | 0.001 |
| Baseline Total Confidence (maximum 75) | |
| Mean (SD) | 38.5 (12.43) |
| Median (IQR) | 40 (33 - 48) |
| Range | 15 - 62 |
| Post-Baseline Total Confidence (out of 75) | |
| Mean (SD) | 58.9 (13.65) |
| Median (IQR) | 61.5 (53.75 - 69.25) |
| Range | 25 - 74 |
| Change in Total Confidence | |
| Mean (SD) | 20.1 (19.93) |
| Median (IQR) | 18 (6 - 30.5) |
| Range | -15 - 58 |
| p | 0.003 |
Table 1: Baseline/Post-simulation knowledge and total confidence of participants. p from Wilcoxon signed rank test of median change equal to 0.
| Study Cohort | |
| Variable/Statistic | (n = 21) |
| Baseline Undocking Time (secs) | |
| Mean (SD) | 146.1 (40.01) |
| Median (IQR) | 139 (116.5 - 169) |
| Range | 88 - 254 |
| Post-Baseline Undocking Time (secs) | |
| Mean (SD) | 89.6 (18.20) |
| Median (IQR) | 89 (76 - 104.5) |
| Range | 59 - 120 |
| Change in Undocking Time (secs) | |
| Mean (SD) | -56.5 (41.95) |
| Median (IQR) | -50 (-81.5 - -23.5) |
| Range | -151 - -2 |
| p | <0.001 |
| Baseline Critical Actions Performed (out of 7) | |
| Mean (SD) | 4.3 (1.06) |
| Median (IQR) | 4 (3 - 5) |
| Range | 3 - 6 |
| Post-Baseline Critical Actions Performed (out of 7) | |
| Mean (SD) | 5.3 (0.78) |
| Median (IQR) | 5 (5 - 6) |
| Range | 3 - 6 |
| Change in Critical Actions Performed | |
| Mean (SD) | 1.0 (1.05) |
| Median (IQR) | 1 (0 - 2) |
| Range | -1 - 3 |
| p | 0.002 |
Table 2: Baseline/Post-simulation undocking times and completion of critical actions. p from Wilcoxon signed rank test of median change equal to 0.
Discussion
Incorporating this curriculum into training necessitates adherence to the protocol as outlined previously. Ensuring practice through hands on training of both the technical aspects of emergency undocking, as well as delineation of roles of OR personnel, is essential towards successful training. All three sessions of pre-training simulation, debriefing, and post-training simulation are likely required to ensure maximal benefit to the learner.
An attempt should be made to create as realistic a learning environment as possible. Although use of an in-situ environment is not mandatory, it is encouraged in order to identify any logistical hurdles or latent safety threats in an actual OR environment that might inhibit completion of the emergency undocking. Another important detail is the vessel used during the training scenarios. Choosing a durable and realistic material is essential as the learners may try any number of techniques to obtain hemostasis depending on their skill level. An ideal vessel design should be able to withstand repeated simulations.
A major limitation to instituting this curriculum is lack of faculty or staff with training in simulation or debriefing. Part of the goal of this curriculum is to clearly layout what is required regarding material and set up to ensure a successful simulation. The availability of the OR to perform training may be a limitation, but the importance of in-situ practice for identifying unanticipated obstacles in the actual clinical environment in case of an emergency undocking is invaluable. The resource of a pelvic model could also be a limitation for some. Although the modification to the model was designed for repeated use, some institutions may not have a training model. There are a number of affordable alternatives to the one mentioned specifically in the study.
The significance of this training curriculum is that it is a single tool used to teach not only procedural skills for emergency undocking, but also establishment of roles for the entire interprofessional team. The in-situ environment adds a level of realism to the simulation, and hands-on training provides a proven tool for solidifying knowledge of the procedure.
This curriculum can be used for future applications including modification for use with other case scenarios involving catastrophic events in robotic surgery. Although this curriculum was focused towards OBGYN robotic surgeons, it can be expanded to use with urology and general surgery robotic surgeons. The modified torso can be used for teaching OR emergencies for any laparoscopic surgery, not only robotic surgery.
Disclosures
The authors have nothing to disclose.
Acknowledgments
The authors wish to thank medical simulation technician Jared Hammond for design of the modified torso, and the Summa Health, Akron Campus operating room personnel. There was no outside funding for this project.
References
- Huser AS, et al. Simulated life-threatening emergency during robot-assisted surgery. J Endourol. 2014;28(6):717–721. doi: 10.1089/end.2013.0762. [DOI] [PubMed] [Google Scholar]
- Berry WR. Cardiac resuscitation in the operating room: reflections on how we can do better. Can J Anaesth. 2012;59(6):522–526. doi: 10.1007/s12630-012-9697-5. [DOI] [PubMed] [Google Scholar]
- Shaligram A, Meyer A, Simorov A, Pallati P, Oleynikov D. Survey of minimally invasive general surgery fellows training in robotic surgery. J Robot Surg. 2013;7(2):131–136. doi: 10.1007/s11701-012-0355-2. [DOI] [PubMed] [Google Scholar]
- Acero NM, et al. Managing a surgical exsanguination emergency in the operating room through simulation: an interdisciplinary approach. J Surg Educ. 2012;69(6):759–765. doi: 10.1016/j.jsurg.2012.06.022. [DOI] [PubMed] [Google Scholar]
- Hoffman M. Simulation of robotic radical hysterectomy using the porcine model. J Robot Surg. 2012;6(3):237–239. doi: 10.1007/s11701-011-0303-6. [DOI] [PubMed] [Google Scholar]
- Goonewardene SS, Cahill D. Robotic surgery, skills and simulation: a technical sport. J Robot Surg. 2016;10(1):85–86. doi: 10.1007/s11701-015-0544-x. [DOI] [PubMed] [Google Scholar]
- Meier M, Horton K, John HDaVinci©. Skills Simulator™: is an early selection of talented console surgeons possible. J Robot Surg. 2016;10(4):289–296. doi: 10.1007/s11701-016-0616-6. [DOI] [PubMed] [Google Scholar]
- Gaba DM. The future vision of simulation in health care. Qual Saf Health Care. 2004;13(Suppl 1):i2–i10. doi: 10.1136/qshc.2004.009878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas E, Wilson KA, Burke CS, Priest HA. Using simulation-based training to improve patient safety: what does it take? Jt Comm J Qual Patient Saf. 2005;31(7):363–371. doi: 10.1016/s1553-7250(05)31049-x. [DOI] [PubMed] [Google Scholar]
- McGaghie WC, Siddall VJ, Mazmanian PE, Myers J, Committee ACoCPHaSP. Lessons for continuing medical education from simulation research in undergraduate and graduate medical education: effectiveness of continuing medical education: American College of Chest Physicians Evidence-Based Educational Guidelines. Chest. 2009;135(3 Suppl):62S–68S. doi: 10.1378/chest.08-2521. [DOI] [PubMed] [Google Scholar]
- Paige JT, et al. High-fidelity, simulation-based, interdisciplinary operating room team training at the point of care. Surgery. 2009;145(2):138–146. doi: 10.1016/j.surg.2008.09.010. [DOI] [PubMed] [Google Scholar]
- Moitra VK, Gabrielli A, Maccioli GA, O'Connor MF. Anesthesia advanced circulatory life support. Can J Anaesth. 2012;59(6):586–603. doi: 10.1007/s12630-012-9699-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziewacz JE, et al. Crisis checklists for the operating room: development and pilot testing. J Am Coll Surg. 2011;213(2):212–217. doi: 10.1016/j.jamcollsurg.2011.04.031. [DOI] [PubMed] [Google Scholar]
- O'Sullivan OE, O'Sullivan S, Hewitt M, O'Reilly BA. Da Vinci robot emergency undocking protocol. J Robot Surg. 2016;10(3):251–253. doi: 10.1007/s11701-016-0590-z. [DOI] [PubMed] [Google Scholar]
- Arriaga AF, et al. Simulation-based trial of surgical-crisis checklists. N Engl J Med. 2013;368(3):246–253. doi: 10.1056/NEJMsa1204720. [DOI] [PubMed] [Google Scholar]


