Abstract
Since there is no cure for glioblastoma multiforme (GBM), the goal of treatment becomes prolonging the survival through cytoreduction while minimising neurological deficits. In this case report, laser interstitial thermal therapy (LITT) was used once the tumour progressed into the isthmus of the cingulate gyrus. One year after temporal lobectomy, disorders of memory, emotion, personality and navigation, likely related to limbic system involvement along with hallucinations and fluctuating cognition occurred as the tumour progressed. After ablation of the posterior cingulum, worsening of topographical disorientation was observed.
Per literature review, delirium has been noted in patients with strokes involving the right-sided temporo-parieto-occipital junction, and topographical disorientation has been associated with lesions of the right posterior cingulum. Alternative causes of these deficits were ruled out, leaving structural changes as the primary explanation. This is the first report of the neurological deficits associated with tumour progression and vasogenic oedema in this region.
Keywords: cancer intervention, delirium, neurosurgery
Background
Median survival after diagnosis of glioblastoma multiforme (GBM) in patients who are able to tolerate the standard therapy of maximal safe resection followed by external beam radiation therapy (EBRT) and adjuvant temozolamide is 14.6 months.1 The increased survival with more complete laser ablation or surgical resection must be balanced with iatrogenic worsening of neurological deficits.2 As an alternative to biopsy alone, a less invasive approach utilising laser interstitial thermal therapy (LITT) to ablate neoplastic tissue achieving immediate cytoreduction is being used more frequently when patients are not candidates for surgical resection.3 The most commonly reported permanent complication of LITT is worsening of a pre-existing neurological deficit which has been reported in 0%–6% of cases.2 3
In this case report, the risk of successive surgical treatments of a mesial temporal GBM were carefully weighed against progressive confusion believed to be resulting from tumour progression. Acute delirium associated with right-sided temporo-parieto-occipital junction in ischaemic and haemorrhagic strokes has been described; however, this is the first report of progression and treatment of a tumour in this region resulting in delirium.4–6 Likewise, topographical disorientation has been described as a result of a stroke of the posterior cingulum but has not been described before resulting from tumour progression and treatment.7
The minimally invasive nature of LITT made it a desirable treatment modality over open craniotomy as the tumour progressed into the deeper mesial temporal structures. This case report serves as a guide to council patients with tumours in the same location who might be experiencing similar symptoms.
Case presentation
A 68-year-old right-handed male with a medical history of migraines, hypertension, type II diabetes mellitus and atrial fibrillation presented with generalisation of a partial seizure. Prior to his brain tumour diagnosis, he was a practising lawyer with no personal or family history of psychiatric disease. MRI revealed a non-enhancing temporal lobe mass.
Investigations
Continuous electroencephalogram (EEG) was negative for epileptiform activity. Cerebrospinal fluid (CSF) was negative for infection, including Lyme disease, syphilis, herpes simplex, varicella zoster, Epstein-Barr, cytomegalovirus and West Nile virus. An autoimmune panel, including paraneoplastic antibodies, ACE, immunoglobulin (Ig)G index, was negative except for the non-specific finding of oligoclonal bands.
Treatment
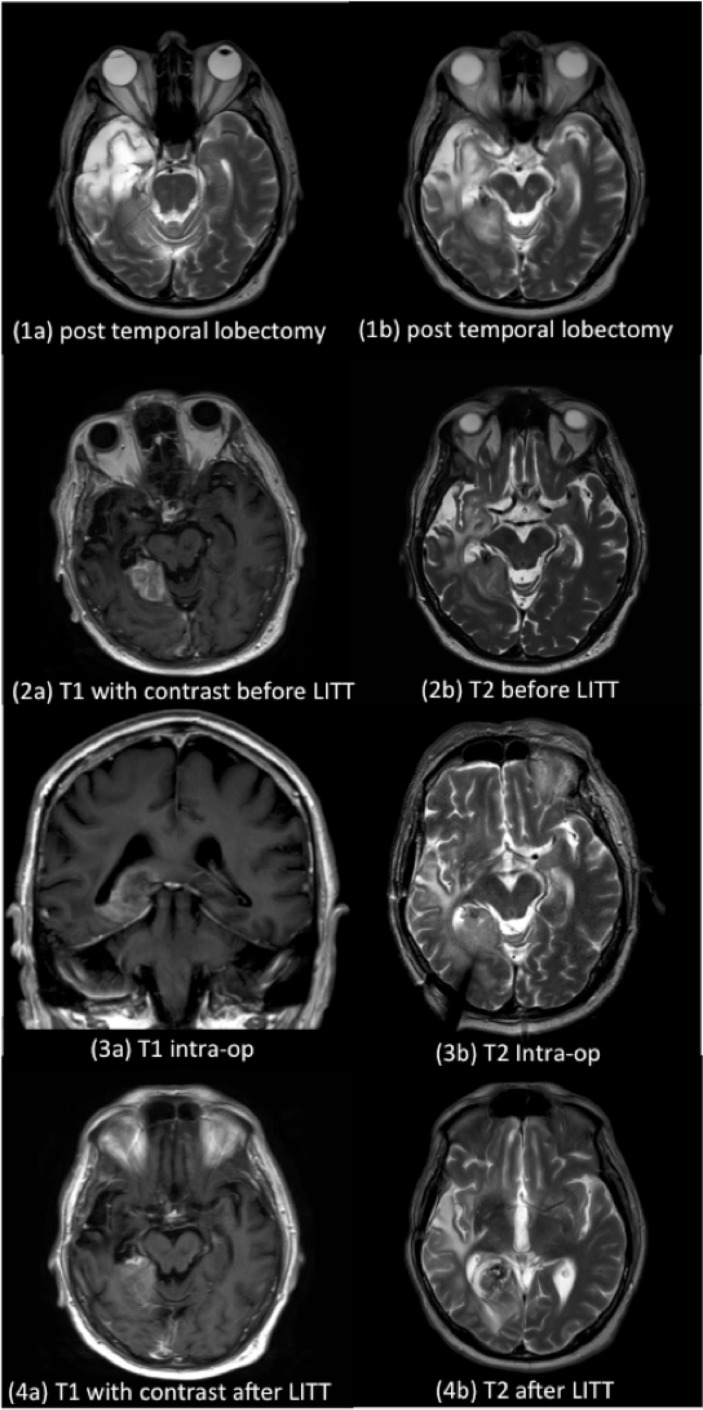
The patient initially underwent uncomplicated surgical excision of the anterior temporal pole, the extent of which is shown in figure 1. Subsequent treatment included concurrent temozolamide and external beam radiation therapy followed by metronomic temozolamide as per Stupp protocol. He recovered without a notable deficit on standard neurological examination. Follow-up MRI 1 year later showed increasing enhancement along the right temporal mesial structures extending back to level of the tectum with local oedema and minimal mass effect. He elected for LITT over open craniotomy.
Figure 1.
The extent of initial tumour resection (1a and 1b), tumour progression prior to LITT (2a and 2b), intra-ablation (3a and 3b) and post-LITT (4a and 4b) extent of cytoreduction. MR images are arranged in pairs and are in ascending chronological order from top to bottom. (1a and 1b) T2 MRI without contrast illustrates the extent of temporal lobe resection after craniotomy for tumour resection. (2a and 2b) T1 with contrast MRI shows the tumour progression (2a) and associated vasogenic oedema (2b) prior to the second round of LITT. This MRI was performed at the onset of associated delirium. An enhancing mass primarily in the posterior mesial temporal lobe is seen with associated vasogenic oedema extending along the white matter tracks of the temporo-parieto-occipital junction. (3a and 3b) Intraoperative MRI illustrates the catheter trajectory as it extends into the mass located in the isthmus of the right-sided cingulate gyrus. A coronal section is included to illustrate the axial extent of the postablative zone centred medial to the atrium lateral ventricles. (4a and 4b) Decreased contrast enhancement in comparison to preoperative images.
Stereotactic biopsy followed by laser interstitial thermal ablation using the Medtronic Visualase (Minneapolis, Minnesota, USA) platform was undertaken. Intraoperative navigation involved a preoperative CT fused to preoperative MRI using BrainLAB system and Varioguide biopsy platform. Subsequent ablation was confirmed through intraoperative MRI and he recovered uneventfully. A gross total ablation of the contrast enhancing mass, of which biopsy showed radiation treatment effect, was performed without complication.
One year later, progressive delusions and paranoia occurred requiring hospitalisation. He experienced fluctuating restlessness, confusion and visual hallucination along with paranoid delusions including that he was kidnapped. Repeat MRI showed progression of disease into the posterior border of the previous ablation zone extending to the isthmus of the cingulate gyrus (figure 1). Repeat LITT was then performed with Monteris Neuroblate (Plymouth, Minnesota, USA) system. Two ablation zones, 1 cm apart were targeted, effectively treating 90% of the enhancing region (figure 1). He was placed on 16 mg/day of dexamethasone in anticipation of postoperative oedema. The delirium was first treated through avoidance of benzodiazepines and anticholinergic medications and maintenance of an appropriate sleep–wake cycle. Next, dexamethasone was tapered to 1 mg twice daily and levetiracetam was replaced with divalproex. While these medications can cause altered mental status, he was treated with these medication since his original diagnosis 2 years prior without significant side effects. EEG and CSF laboratories were unremarkable. He was treated with risperidone and divalproex and was discharged home.
Outcome and follow-up
Over the following week, the delirium improved; however, he continued to have behavioural changes and topographical disorientation. He developed an insatiable appetite and was convinced that his blood glucose levels were low along with agitation. Despite not exhibiting focal weakness on neurological examination, he had difficulty with spatial tasks such as misjudging the distance to a chair and repeatedly falling when attempting to sit. He also experienced difficulty with the orientation of clothing such as putting a shirt on backwards. On examination, he was oriented with intact recall, strength, coordination, and on cranial nerve examination, however, he was unable to determine differentiated sidedness of hearing.
He was eventually rehospitalised for worsening delirium and taken into the care of a hospice team. Two months after the last treatment with LITT, he expired at home 2 years after initial diagnosis.
Discussion
The right temporo-parieto-occipital cortex was first associated with delirium in a study of patients with ischaemic stroke.5 6 More recently, haemorrhagic strokes affecting the parahippocampal gyrus has been implicated.4 This region is involved in conscious awareness as it contains long-track transcortical connections important for attention, which may explain why when dysfunction of this region occurs, a delirium-like state ensues. Additionally, the hippocampus, parahippocampal gyrus and cingulate gyrus have been implicated in awareness, specifically with respect to operations that support declarative memory.8 9 Disruption of regions which project hippocampal connections with the prefrontal cortex has been associated with disease states such as Alzheimer’s, schizophrenia and depression among others.10
As the tumour progressed into the isthmus of the cingulate gyrus, profound changes in awareness occurred. In the Papez circuit, the cingulum links the parahippocampal gyrus and hippocampus with the limbic system, which are involved in memory, emotion and navigation.10 Thus, it is conceivable that damage to this region could explain the psychological changes which occurred. Additionally, he experienced topographical disorientation, which is defined as inability to judge the distance and direction of objects.11 In one case report, this was also seen in a patient who suffered a stroke of the isthmus of the right cingulate gyrus.7
While the goal of therapy is to prevent tumour progression, worsening of neurological deficits, sometimes seen with especially in the immediate postoperative period is a known risk of LITT. As LITT is an emerging therapy in patients with GBM, research is limited to case series and review articles.12 13 Although there is currently no class I or II evidence for its efficacy, it has the potential to prolong life via cytoreduction in selected patients with GBM with tumours that are surgically inaccessible or in whom a larger operation is not feasible. This technique works through delivering photons via an optical fibre to attain a temperature threshold where proteins are irreversibly denatured without vaporisation. This system has been coupled with elegant software and imaging modalities to allow for real-time temperature mapping MRI feedback and modulation to allow for precise ablation boundaries.14
In this case, precise ablation of enhancing tissue located in the posterior cingulate gyrus was achieved; however, despite this, worsening of topographical disorientation was observed. This was coupled with delirium as tumour-associated oedema tracked into the right temporo-parieto-occipital junction in the setting of pre-existing atrophy from EBRT and prior surgical temporal lobe resection. Corroboration of our report in future cases would be important to confirm the validity of these findings along with more detailed testing of special memory and perception in patients with similar lesions.
Learning points.
Delirium is defined as a waxing and waning confusion characterised by agitation, delusions, illusions and incoherence that is treated through correction of the underlying illness. There are many causes of delirium in hospitalised patients including prescription drug use and withdrawal, electrolyte disturbances, infection, intoxication, stress and alterations in the sleep–wake cycle.
On a molecular level, acetylcholine deficiency and dopamine excess is seen in the state of delirium. Acetylcholine deficiency is associated with attention deficits, classically seen as slowing on electroencephalogram.15 The cholinergic pathways travel in discrete bundles through the white matter tracks, so there is a greater threat to the balance of neurotransmitter pathways when tumour invasion occurs.
A lesion of the right temporo-parieto-occipital cortex may also be associated with delirium.
A lesion of the isthmus of the cingulate gyrus may result in topographical disorientation.
Acknowledgments
We would like to acknowledge Dr Jack Rock for his expertise in neuroanatomy.
Footnotes
Contributors: TMZ was responsible for primary authorship, bibliography compilation, consent and IRB approval for publication. AMR was responsible for review, extensive edits, intellectual content and expertise in oncological neurosurgery. IL was responsible for the project oversight and attending neurosurgeon of the patient who is presented in the report and provided significant contributions to review and edits.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Next of kin consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Stupp R, Mason WP, van den Bent MJ, et al. . Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 2005;352:987–96. 10.1056/NEJMoa043330 [DOI] [PubMed] [Google Scholar]
- 2.Schwarzmaier HJ, Eickmeyer F, von Tempelhoff W, et al. . MR-guided laser irradiation of recurrent glioblastomas. J Magn Reson Imaging 2005;22:799–803. 10.1002/jmri.20446 [DOI] [PubMed] [Google Scholar]
- 3.Mohammadi AM, Hawasli AH, Rodriguez A, et al. . The role of laser interstitial thermal therapy in enhancing progression-free survival of difficult-to-access high-grade gliomas: a multicenter study. Cancer Med 2014;3:971–9. 10.1002/cam4.266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naidech AM, Polnaszek KL, Berman MD, et al. . Hematoma locations predicting delirium symptoms after intracerebral hemorrhage. Neurocrit Care 2016;24:1–7. 10.1007/s12028-015-0210-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Posner J, clifford S, schiff N, et al. . Posner’s diagnosis of stupor and coma. 4th ed. [Google Scholar]
- 6.Peroutka SJ, Sohmer BH, Kumar AJ, et al. . Hallucinations and delusions following a right temporoparietooccipital infarction. Johns Hopkins Med J 1982;151:181–5. [PubMed] [Google Scholar]
- 7.Katayama K, Takahashi N, Ogawara K, et al. . Pure topographical disorientation due to right posterior cingulate lesion. Cortex 1999;35:279–82. 10.1016/S0010-9452(08)70801-3 [DOI] [PubMed] [Google Scholar]
- 8.Radua J, Phillips ML, Russell T, et al. . Neural response to specific components of fearful faces in healthy and schizophrenic adults. Neuroimage 2010;49:939–46. 10.1016/j.neuroimage.2009.08.030 [DOI] [PubMed] [Google Scholar]
- 9.Weiner KS, Zilles K. The anatomical and functional specialization of the fusiform gyrus. Neuropsychologia 2016;83 10.1016/j.neuropsychologia.2015.06.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bubb EJ, Kinnavane L, Aggleton JP. Hippocampal-diencephalic-cingulate networks for memory and emotion: An anatomical guide. Brain Neurosci Adv 2017;1:239821281772344 10.1177/2398212817723443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aguirre GK, D’Esposito M. Topographical disorientation: a synthesis and taxonomy. Brain 1999;122:1613–28. 10.1093/brain/122.9.1613 [DOI] [PubMed] [Google Scholar]
- 12.Elder JB, Chiocca EA. Editorial: Glioblastoma multiforme and laser interstitial thermal therapy. J Neurosurg 2013;118:1199–201. 10.3171/2012.9.JNS121563 [DOI] [PubMed] [Google Scholar]
- 13.Masters A, Steger AC, Lees WR, et al. . Interstitial laser hyperthermia: a new approach for treating liver metastases. Br J Cancer 1992;66:518–22. 10.1038/bjc.1992.305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Norred SE, Johnson JA. Magnetic resonance-guided laser induced thermal therapy for glioblastoma multiforme: a review. Biomed Res Int 2014;2014:1–9. 10.1155/2014/761312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trzepacz PT. Is there a final common neural pathway in delirium? Focus on acetylcholine and dopamine. Semin Clin Neuropsychiatry 2000;5:132–48. 10.153/SCNP00500132 [DOI] [PubMed] [Google Scholar]