Abstract
Proliferating trichilemmal tumours are benign but locally aggressive skin neoplasms arising from hair follicles. Rarely, they can become malignant and must be appropriately managed to prevent recurrence and metastasis. One must have a low threshold for diagnosing this rare neoplasm.
Keywords: skin, plastic and reconstructive surgery
Background
Proliferating trichilemmal tumours (PTTs) were originally described by Jones in 1966 as benign but locally aggressive skin neoplasms arising from the outer root sheath of hair follicles.1 They usually develop in pre-existing trichilemmal cysts (TCs) and present as rapid growth from previously singular, asymptomatic lesions.2 Very rarely, they may develop into malignant PTTs (MPTTs).
Case presentation
A 56-year-old female Caucasian presented with a nodular lesion on the left parietal scalp. This lesion progressively increased in size over 1 year. There was no history of prior trauma or travel and no similar lesions elsewhere. The patient reported no pertinent personal or family medical history and had never smoked, and a systems review was negative. Physical examination revealed a 1.8 cm diameter nodular lesion with no exudate, sensorimotor deficit or cervical or peripheral lymphadenopathy.
Investigations
Blood results were normal and tissue cultures revealed only skin commensals. The lesion was presumed to be a sebaceous cyst and was excised under local anaesthetic. Macroscopically, the lesion was encapsulated, homogenous grey-white in colour and nodular in consistency and with no exudate. The histology report identified a benign pilar cyst comprised sharply circumscribed nodules showing little cytonuclear atypia, with incomplete excision margins (figure 1). Given the benign nature of the lesion at the time, it was decided to adopt a conservative approach and review the patient in outpatient clinic in 6 months time to see if further excision would be warranted.
Figure 1.
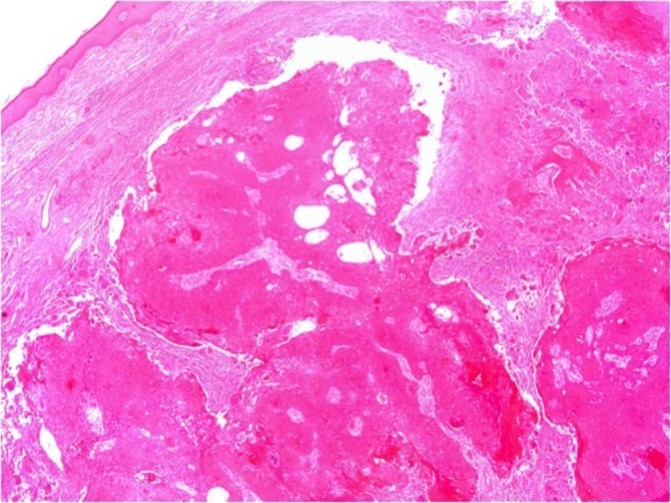
Histology micrograph (×2.5) showing benign pilar cyst comprised sharply circumscribed nodules showing little cytonuclear atypia, with incomplete excision margins.
Differential diagnosis
Differential diagnoses of a scalp lesion include sebaceous cysts, lipomas, infectious pathologies such as kerions, neoplasms such as trichoblastomas, spiradenomas, cylindromas, squamous cell carcinomas (SCCs), basal cell carcinomas, melanomas and metastases.
Treatment
Six months on the area had been slow to heal, the lesion regrew, increased in tenderness and was now accompanied by local alopecia (figure 2). A subsequent excision biopsy was undertaken. Macroscopically, the lesion was again encapsulated, nodular in consistency and had a homogenous grey-white cut surface but this time with foci of necrosis and haemorrhage.
Figure 2.
Recurrence of malignant proliferating trichilemmal tumour with local alopecia.
The histology reported skin incorporating a lobulated dermal tumour with a focally cystic architecture, with foreign body-type granulomatous inflammation, indicating previous rupture of some of the cystic areas. The lesion is composed of stratified squamous epithelium with trichilemmal pilar keratinisation. Most of the nodules are sharply circumscribed and show little cytonuclear atypia; however, there are areas where the lesion has moderate cytonuclear atypia and a distinct infiltrative architecture. Single cells are seen in the dermis eliciting a desmoplastic stromal reaction. Focally, the tumour displays cytonuclear atypia and there are small islands of atypical squamous cells and single keratinocytes within the dermal stroma surrounded by stromal reaction. These histological features are those of a malignant proliferating pilar tumour (figures 3–4). Given the excision margins were narrow at 0.2 mm, the patient underwent subsequent Mohs surgery.
Figure 3.
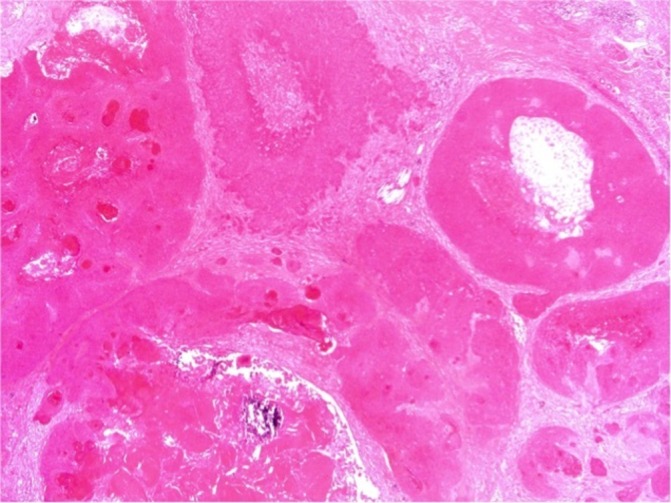
Histology findings (×2.5) showing foci of tumour with an infiltrative architecture.
Figure 4.
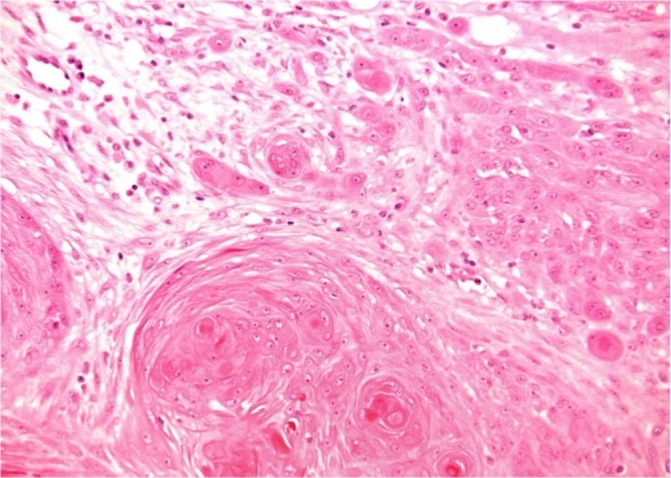
Histology findings (×20) showing invasive malignant proliferating trichilemmal tumour carcinoma with cytonuclear atypia, infiltrative architecture, trichilemmal keratinisation and atypical squamous cells and keratinocytes in the dermis surrounded by desmoplastic stromal reaction.
A staging CT scan was not done as there was no clinical impression of metastatic spread. Further direct imaging of the lesion was not deemed necessary.
Outcome and follow-up
The patient has been free from recurrence at 1 year follow-up.
Discussion
TCs occur in 5%–10% of the population, with 2% developing into PTTs and MPTTs being even rarer.3 PTTs can develop from foci of proliferating epithelial cells in TCs secondary to trauma or chronic inflammation, or may arise de novo.4 They have a female to male preponderance of 6% to 1% and 90% are located on the scalp with increased density of hair follicles and chronic sun exposure cited as explanation.3 5 PTTs have been reported infrequently in other body regions and comprise 0.1% of all skin malignancies.6 There are few reported cases of MPTTs in the literature,3 7–15 and although rare, they can present similarly to benign PTTs.16 Satyaprakash et al report complete surgical excision is warranted for TCs, PTTs and MPTTs and cite a PTT local recurrence rate of 3.7% after conservative local excision.2 17–19 Local recurrence rate for MPTT has been shown to be 25%.18 Uchida et al report an MPTT in the breast which was misdiagnosed as a breast carcinoma and excised, and she remains healthy at follow-up.10 Deshmukh et al report a scalp MPTT which was again treated by wide local excision, and advise that the efficacy of alternative treatments for cannot be safely evaluated given the small number of reported cases.11 Shetty et al and Alici et al report scalp MPTTs which were successfully excised with a wide local excision and 1 cm margin.3 9 Saida et al report a patient with multiple TCs which were excised with a wide margin, but later presented with metastases in regional lymph nodes with the same histological findings, suggesting that the original TCs may have been misdiagnosed and were in fact MPTTs.12 Rao et al report a patient with a scalp PTT which was excised but recurred and displayed characteristics of MPTT and so was excised with a 2 cm margin.13 From the few cases in the literature, the treatment of choice seems to be wide local excision and monitoring for recurrence. Fieleke et al however report a case of MPTT with incomplete margins who underwent Mohs surgery until clear margins were obtained, and propose it as a more effective and tissue sparing approach.15 However, there is insufficient evidence in the literature to suggest whether MPTTs are, or are not, contiguous. Non-contiguous lesions negate the benefit of Mohs surgery as skip lesions can produce inaccurate clearance margins. In MPTTs therefore, the gold standard treatment remains wide local excision with a clear margin of healthy tissue.
Gross examination of excised lesions in other reported cases of MPTTs is similar to our case, with the lesion presenting as a nodular, encapsulated mass with a homogenous grey-white cut surface containing foci of necrosis and haemorrhage.2 Histologically, PTTs are characterised by ‘trichilemmal keratinisation’ involving an abrupt transition of nucleated to anucleated keratinised epithelium without a granular layer.2
PTTs can evolve into MPTTs by invading neighbouring tissues with the propensity to metastasise.20 Histologically, they demonstrate markers of malignancy such as nuclear polymorphism, atypical mitosis, foci of single cell necrosis, abrupt keratinisation and lymphovascular invasion.9 11 MPTTs can arise de novo, but most occur due to malignant transformation of pre-existing PTTs via a sequential adenomatous–epitheliomatous–carcinomatous progression.18
Ye et al classified PTTs into three groups based on their clinicopathological characteristics18:
PTTs (benign)—Well-circumscribed lesion with pushing margins; mild nuclear atypia, absence of mitoses, necrosis or neurovascular invasion.
MPTTs (low grade)—Similar to ‘Benign’ but manifest as irregular, locally invasive silhouettes with involvement of the deep dermis and subcutis.
MPTTs (high grade)— Invasive growth patterns, marked nuclear atypia, pathological mitotic forms and necrosis, with or without neurovascular invasion.
Imaging can be a useful adjunct when clinically necessary. If there is evidence of metastatic spread, a staging CT scan would be useful to determine the extent. If the lesion is firmly adherent on the scalp and suggestive of infiltration into cranium, or if there is any focal neurology, a CT head scan would be useful to illustrate this. MRI can subsequently be used to better evaluate soft tissue infiltration, and MPTTs show up as poorly marginated, ovoid, soft-tissue masses showing isointense signal on T1 weighting and hyperintense signal on T2 weighting relative to muscle.21
MPTTs can resemble SCCs both clinically and histologically,18 and trichilemmal keratinisation is an important indicator in differentiating PTTs from SCCs but there is no definitive recognised treatment algorithm for MPTTs as there is for SCC.2 If MPTT is diagnosed with evidence of metastatic spread, adjuvant treatments such as nodal dissections, radiotherapy and chemotherapy can be considered in addition to wide local excision or Mohs resection.2 Adjuvant chemotherapy is not thought to be superior to adequate surgery alone.22 The CAV regimen (cisplatin, adriamycin and vindesine) used for advanced SCC has shown only limited benefit.23 In addition, Takenaka et al report a case of MPTT resistant to radiotherapy, chemotherapy (cisplatin, bleomycin, adriamycin) and intralesional ethanol.24 It is difficult to evaluate alternative treatments given the scarcity of this tumour in the literature. Nevertheless, radiotherapy has been used effectively to reduce the size of the lesion, especially where the lesion is particularly large,15 18 20 22 25 and also has the potential to reduce recurrence rate and has been used with curative intent in one case.25
In contrast, the treatment algorithm for SCCs is more established, with either surgery or radiotherapy used as first-line treatment, followed by adjuvant chemotherapy, molecular therapy or additional radiotherapy depending on staging.26 Misdiagnosing MPTT as SCC could alter management and prognosis.
The treatment of choice is wide local surgical excision with clear margins of at least 1 cm.2 11 Mohs surgery may provide a better cosmetic outcome but with equivalent recurrence rates as wide local excision. Further studies and cases need to be published to provide a thorough evidence base for the management of MPTTs.15
Learning points.
Proliferating trichilemmal tumours (PTTs) are aggressive skin neoplasms arising from hair follicles.
PTTs exist on a spectrum ranging from benign and locally aggressive PTTs to high-grade malignant PTTs with significant recurrence and metastatic potential.
Wide local excision with a margin of healthy tissue is the gold standard.
Alternative therapies such as radiotherapy and chemotherapy have been shown to be effective and are useful adjuncts to surgical excision.
Footnotes
Contributors: PS: planning, organisation of patient care, collaboration with histopathology and follow-up review of the patient and literature review and writing of manuscript. AU: care of the patient, literature review, discussions in multidisciplinary team, design of case report and writing and editing of the manuscript. LM: role in MDT meetings and reviewing histopathology, literature review and editing of manuscript. IK: consultant responsible for patient care, coordinating MDT, literature review and case identification for write-up, editing and review of manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Jones EW. Proliferating epidermoid cysts. Arch Dermatol 1966;94:11–19. 10.1001/archderm.1966.01600250017002 [DOI] [PubMed] [Google Scholar]
- 2.Satyaprakash AK, Sheehan DJ, Sangüeza OP. Proliferating trichilemmal tumors: a review of the literature. Dermatol Surg 2007;33:1102–8. 10.1111/j.1524-4725.2007.33225.x [DOI] [PubMed] [Google Scholar]
- 3.Shetty PK, Jagirdar S, Balaiah K, et al. Malignant proliferating trichilemmal tumor in young male. Indian J Surg Oncol 2014;5:43–5. 10.1007/s13193-013-0259-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rahbari H, Mehregan AH. Development of proliferating trichilemmal cyst in organoid nevus. Presentation of two cases. J Am Acad Dermatol 1986;14:123–6. [DOI] [PubMed] [Google Scholar]
- 5.Morgan RF, Dellon A, Hoopes JE. Pilar tumors. Plast Reconstr Surg 1979;63:520–4. 10.1097/00006534-197904000-00013 [DOI] [PubMed] [Google Scholar]
- 6.Siddha M, Budrukkar A, Shet T, et al. Malignant pilar tumor of the scalp: a case report and review of literature. J Cancer Res Ther 2007;3:240–3. [DOI] [PubMed] [Google Scholar]
- 7.Capurso-García MA, Bautista-Piña V, Pomerantz A, et al. Atypical proliferating trichilemmal cyst with malignant breast skin transformation: A case report and review of the literature. Case Rep Oncol Med 2016;2016:1–4. 10.1155/2016/7481569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goyal S, Jain BB, Jana S, et al. Malignant proliferating trichilemmal tumor. Indian J Dermatol 2012;57:50–2. 10.4103/0019-5154.92679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alici O, Keles MK, Kurt A. A rare cutaneous adnexal tumor: malignant proliferating trichilemmal tumor. Case Rep Med 2015;2015:1–4. 10.1155/2015/742920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uchida N, Tsuzuki Y, Ando T, et al. Malignant proliferating trichilemmal tumor in the skin over the breast: a case report. Breast Cancer 2000;7:79–82. 10.1007/BF02967193 [DOI] [PubMed] [Google Scholar]
- 11.Deshmukh BD, Kulkarni MP, Momin YA, et al. Malignant proliferating trichilemmal tumor: a case report and review of literature. J Cancer Res Ther 2014;10:767–9. 10.4103/0973-1482.136036 [DOI] [PubMed] [Google Scholar]
- 12.Saida T, Oohara K, Hori Y, et al. Development of a malignant proliferating trichilemmal cyst in a patient with multiple trichilemmal cysts. Dermatologica 1983;166:203–8. 10.1159/000249868 [DOI] [PubMed] [Google Scholar]
- 13.Rao S, Ramakrishnan R, Kamakshi D, et al. Malignant proliferating trichilemmal tumour presenting early in life: an uncommon feature. J Cutan Aesthet Surg 2011;4:51–5. 10.4103/0974-2077.79196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mathis ED, Honningford JB, Rodriguez HE, et al. Malignant proliferating trichilemmal tumor. Am J Clin Oncol 2001;24:351–3. 10.1097/00000421-200108000-00006 [DOI] [PubMed] [Google Scholar]
- 15.Fieleke DR, Goldstein GD. Malignant proliferating trichilemmal tumor treated with Mohs surgery: proposed protocol for diagnostic work-up and treatment. Dermatol Surg 2015;41:292–4. 10.1097/DSS.0000000000000269 [DOI] [PubMed] [Google Scholar]
- 16.Al-Khateeb TH, Al-Masri NM, Al-Zoubi F. Cutaneous cysts of the head and neck. J Oral Maxillofac Surg 2009;67:52–7. 10.1016/j.joms.2007.05.023 [DOI] [PubMed] [Google Scholar]
- 17.Sau P, Fau GJ, Helwig EB. Proliferating epithelial cysts. Clinicopathological analysis of 96 cases. [DOI] [PubMed] [Google Scholar]
- 18.Ye J, Nappi O, Swanson PE, et al. Proliferating pilar tumors: a clinicopathologic study of 76 cases with a proposal for definition of benign and malignant variants. Am J Clin Pathol 2004;122:566–74. 10.1309/21DK-LY2R-94H1-92NK [DOI] [PubMed] [Google Scholar]
- 19.Tellechea O, Cardoso JC, Reis JP, et al. Benign follicular tumors. An Bras Dermatol 2015;90:780–98. 10.1590/abd1806-4841.20154114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lobo L, Amonkar AD, Dontamsetty VV. Malignant proliferating trichilemmal tumour of the scalp with intra-cranial extension and lung metastasis-a case report. Indian J Surg 2016;78:493–5. 10.1007/s12262-015-1427-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim HJ, Kim TS, Lee KH, et al. Proliferating trichilemmal tumors: CT and MR imaging findings in two cases, one with malignant transformation. AJNR Am J Neuroradiol 2001;22:180–3. [PMC free article] [PubMed] [Google Scholar]
- 22.Markal N, Kurtay A, Velidedeoğlu H, et al. Malignant transformation of a giant proliferating trichilemmal tumor of the scalp: patient report and literature review. Ann Plast Surg 1998;41:314–6. [DOI] [PubMed] [Google Scholar]
- 23.Hayashi I, Harada T, Muraoka M, et al. Malignant proliferating trichilemmal tumour and CAV (cisplatin, adriamycin, vindesine) treatment. Br J Dermatol 2004;150:156–7. 10.1111/j.1365-2133.2004.05670.x [DOI] [PubMed] [Google Scholar]
- 24.Takenaka H, Kishimoto S, Shibagaki R, et al. Recurrent malignant proliferating trichilemmal tumour: local management with ethanol injection. Br J Dermatol 1998;139:726-9. [PubMed] [Google Scholar]
- 25.Sutherland D, Roth K, Yu E. Malignant proliferating trichilemmal tumor treated with radical radiotherapy: a case report and literature review. Cureus 2017;9:e999 10.7759/cureus.999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parikh S, Patel V, Ratner D. Advances in the management of cutaneous squamous cell carcinoma. F1000Prime Rep 2014;6:6–70. 10.12703/P6-70 [DOI] [PMC free article] [PubMed] [Google Scholar]



